Abstract
Purpose
To evaluate whether intraoperative ventilation using lower driving pressure decreases the risk of nonhome discharge.
Methods
We conducted a historical cohort study of patients aged ≥ 60 yr who were living at home before undergoing elective, noncardiothoracic surgery at two tertiary healthcare networks in Massachusetts between 2007 and 2018. We assessed the association of the median driving pressure during intraoperative mechanical ventilation with nonhome discharge using multivariable logistic regression analysis, adjusted for patient and procedural factors. Contingent on the primary association, we assessed effect modification by patients’ baseline risk and mediation by postoperative respiratory failure.
Results
Of 87,407 included patients, 12,584 (14.4%) experienced nonhome discharge. In adjusted analyses, a lower driving pressure was associated with a lower risk of nonhome discharge (adjusted odds ratio [aOR], 0.88; 95% confidence interval [CI], 0.83 to 0.93, per 10 cm H2O decrease; P < 0.001). This association was magnified in patients with a high baseline risk (aOR, 0.77; 95% CI, 0.73 to 0.81, per 10 cm H2O decrease, P-for-interaction < 0.001). The findings were confirmed in 19,518 patients matched for their baseline respiratory system compliance (aOR, 0.90; 95% CI, 0.81 to 1.00; P = 0.04 for low [< 15 cm H2O] vs high [≥ 15 cm H2O] driving pressures). A lower risk of respiratory failure mediated the association of a low driving pressure with nonhome discharge (20.8%; 95% CI, 15.0 to 56.8; P < 0.001).
Conclusions
Intraoperative ventilation maintaining lower driving pressure was associated with a lower risk of nonhome discharge, which can be partially explained by lowered rates of postoperative respiratory failure. Future randomized controlled trials should target driving pressure as a potential intervention to decrease nonhome discharge.
Résumé
Objectif
Évaluer si la ventilation peropératoire utilisant une pression motrice plus faible diminue le risque de congé hors domicile.
Méthode
Nous avons réalisé une étude de cohorte historique de patients âgés de ≥ 60 ans vivant à la maison avant de bénéficier d’une chirurgie non cardiothoracique non urgente dans deux réseaux de soins de santé tertiaires du Massachusetts entre 2007 et 2018. Nous avons évalué l’association entre la pression motrice médiane pendant la ventilation mécanique peropératoire et le congé ailleurs qu’au domicile à l’aide d’une analyse de régression logistique multivariable, ajustée pour tenir compte des facteurs liés aux patients et à l’intervention. En fonction de l’association primaire, nous avons évalué la modification de l’effet par le risque initial des patients et la médiation par l’insuffisance respiratoire postopératoire.
Résultats
Sur les 87 407 patients inclus, 12 584 (14,4 %) ont reçu leur congé ailleurs qu’au domicile. Dans les analyses ajustées, une pression motrice plus faible était associée à un risque réduit de congé hors domicile (rapport de cotes ajusté [RCa], 0,88; intervalle de confiance [IC] à 95 %, 0,83 à 0,93, par diminution de 10 cm H2O; P < 0,001). Cette association a été amplifiée chez les patients présentant un risque initial élevé (RCa, 0,77; IC 95 %, 0,73 à 0,81, par diminution de 10 cm H2O, P-pour-interaction < 0,001). Les résultats ont été confirmés chez 19 518 patients appariés pour la compliance initiale de leur système respiratoire (RCa, 0,90; IC 95 %, 0,81 à 1,00; P = 0,04 pour des pressions motrices faibles [< 15 cm H2O] vs élevées [≥ 15 cm H2O]). Un risque plus faible d’insuffisance respiratoire a entraîné une association entre une faible pression motrice et un congé à l’extérieur du domicile (20,8 %; IC 95 %, 15,0 à 56,8 ; P < 0,001).
Conclusion
La ventilation peropératoire maintenant une pression motrice plus faible a été associée à un risque plus faible de congé hors domicile, ce qui peut s’expliquer en partie par des taux réduits d’insuffisance respiratoire postopératoire. Les futures études randomisées contrôlées devraient cibler la pression motrice comme intervention potentielle pour réduire les congés hors domicile.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Over 300 million patients undergo surgery with anesthesia worldwide each year.1 Postoperative nonhome discharge to a long-term care facility or nursing home is an important adverse outcome, and its avoidance highly prioritized by patients and their families.2,3 This unfavorable endpoint is associated with a higher risk of hospital readmission and increased overall healthcare costs.4 For example, the cost of long-term care in a nursing home is estimated at 349 to 397 CAD per patient per day, resulting in more than 137,000 CAD (conversion rate 1.37 from USD) annually for every patient admitted to a nursing home.5
While many screening tools have been derived and validated to reliably identify patients at high risk of nonhome discharge,6,7,8,9,10 clinicians still lack a thorough understanding of modifiable intraoperative risk factors and related interventions that can decrease rates of nonhome discharge. Postoperative programs including targeted mobilization may increase patients’ functional status, potentially avoiding nonhome discharge.11,12 Few intraoperative interventions are known that help prevent this unfavourable outcome.
Previous research has suggested that postoperative respiratory failure is associated with an increased risk of nonhome discharge.13 In addition, avoiding postoperative respiratory complications can mitigate intensive care unit admission and hospitalization,14 favoring maintenance of patient autonomy after surgery. Multiple studies have found that intraoperative mechanical ventilation can decrease the risk of postoperative respiratory complications,15 particularly when lower driving pressures are maintained.16,17,18 A meta-analysis showed that the beneficial effects of low intraoperative tidal volume were completely mediated by lower driving pressure,19 which imposes lung tissue damage through stretch and strain.20,21,22 Mechanical injury increases the release of inflammatory mediators that can lead to systemic inflammation, reduced functional status, and multiorgan impairment, translating into a higher incidence of nonhome discharge.20,23,24
In this study, we sought to investigate the hypothesis that a lower driving pressure during intraoperative ventilation is associated with a lower risk of nonhome discharge, and that this effect could be explained by a lower risk of postoperative respiratory failure.
Methods
Study design
In this historical cohort study, we analyzed data from cases of surgery performed between January 2007 and December 2018 at two academic hospital networks in Massachusetts, USA: Beth Israel Lahey Health (Beth Israel Deaconess Medical Center) and Mass General Brigham (Massachusetts General Hospital and its affiliated community hospitals). Ethical approval for this study (Institutional Review Board numbers, 2021P000494 and 2021P001727) was provided by the Committee on Clinical Investigations affiliated with the Beth Israel Lahey Health Network in June 2021 and by the Mass General Brigham Institutional Review Board in July 2021, with waivers of informed consent.
Data sources used to establish the dataset are described in the Electronic Supplementary Material (ESM), eAppendix 1. This manuscript complies with the Strengthening the Reporting of Observational Studies in Epidemiology guidelines.25
Study population
Patients aged 60 yr and older who underwent noncardiothoracic surgery under general anesthesia were eligible for inclusion if they lived at home prior to surgery and had available electronic documentation of exposure and primary outcome variables. Patients undergoing emergency procedures and those with an American Society of Anesthesiologists (ASA) Physical Status classification of V or higher were excluded. Patients undergoing laparoscopic or microlaryngoscopic surgery were also excluded as driving pressure recordings from these procedures are likely to be subject to overestimation. Observations with missing data for potential confounding variables were excluded and the primary analysis was performed using the complete-case method.
Primary analysis
The primary exposure variable was the median driving pressure during intraoperative mechanical ventilation. Driving pressure was calculated as the difference between median plateau pressure (Pplat) and median positive end-expiratory pressure (PEEP). In cases without available plateau pressure, the peak inspiratory pressure was used to estimate Pplat. The primary outcome was nonhome discharge after surgery (previously also referred to as “adverse discharge”6,26 or “loss of the ability to live independently”11), defined as discharge to a skilled nursing home or long-term care facility, discharge to hospice care, or in-hospital death.27
In the primary analysis, we assessed the association between lower intraoperative driving pressure and nonhome discharge using multivariable logistic regression analysis adjusted a priori for defined confounding variables based on a literature review and clinical plausibility.6,7,8,28 Potential confounding variables included admission type, year of surgery, patient’s a priori risk for postoperative respiratory complications, and nonhome discharge based on the individual predictors29 of the Score for Prediction of Postoperative Respiratory Complications (SPORC)28,30 and of the Discharge Prediction for Patients Undergoing Inpatient Surgery (DEPENDENSE) score.8 We further adjusted for anesthesia-related factors and markers of procedural severity, including the duration of surgery, work relative value units, hypotension (time with mean arterial pressure [MAP] < 55 mm Hg), vasopressor dose (mg norepinephrine equivalents), administered fluid volume, dose of nondepolarizing neuromuscular blocking agents (effective dose [ED]95 equivalents), dose of long- and short-acting opioids (mg oral morphine equivalents), neostigmine dose,31,32 age-adjusted minimum alveolar concentration of volatile anesthetics and nitrous oxide,33 and intraoperative blood transfusions.34 The healthcare network was additionally included to address potential bias arising from the multicentre design of this study. Details on exposure, outcome, and confounding variables are provided in the ESM eAppendix 1. We then applied path mediation analysis to evaluate whether the association between low (< 15 cm H2O) vs high (≥ 15 cm H2O) driving pressure and nonhome discharge was mediated by lower rates of postoperative respiratory failure, defined as reintubation within seven days after surgery or oxygen saturation below 90% during the first ten minutes after extubation.35,36 Details on the mediation analysis are provided in the ESM eAppendix 2.
Secondary and exploratory analyses
In a key secondary analysis, we matched patients receiving high vs low driving pressure based on their baseline respiratory system compliance (defined as the median compliance during the first ten minutes after intubation, normalized to ideal body weight) using a 1:1 scheme and a caliper of 0.005 mg·kg–1/cm H2O. The goal of this procedure was to create two cohorts with different driving pressures but identical respiratory system compliance. This analysis was conducted in a subgroup of patients with available minute-by-minute recordings of respiratory parameters. We estimated the risk of nonhome discharge in the matched cohort for patients receiving low vs high driving pressure using multivariable logistic regression analysis adjusted for the aforementioned potential confounding variables.
We then applied interaction term analysis to assess a potential effect modification of the primary association by a high baseline risk of nonhome discharge, defined as a DEPENDENSE score8 above the median in the cohort.
To assess potential variability in the application of intraoperative driving pressure across anesthesia providers, we calculated the mean predicted probability of using low vs high driving pressure for each individual provider, adjusted for patient-, anesthesia-, and procedure-related factors.37
With exploratory intent, we assessed whether a lower driving pressure was associated with intraoperative hypotension, defined as a MAP < 55 mm Hg for ≥ five cumulative minutes, and with major postoperative complications within 30 days.38 Further, we investigated the primary association in subgroups of hospitalized patients, patients with an ASA Physical Status classification of III or higher, and patients with a prior diagnosis of chronic obstructive pulmonary disease. In post hoc exploratory analyses, we investigated a possible mediation of the association of low driving pressure with nonhome discharge by postextubation oxygen desaturation (defined as peripheral oxygen saturation < 90% within ten minutes after extubation),13 the requirement of reintubation or noninvasive ventilation within seven days after surgery,35,36,39,40 and major postoperative complications within 30 days.38 Details of secondary and exploratory analyses are provided in the ESM eAppendices 3 and 4.
Sensitivity analyses
The primary model was designed to provide estimates of the relationship between lower driving pressure ventilation and nonhome discharge. Sensitivity analyses were conducted to test the robustness of the primary analysis, including 1) multiple imputation of missing Pplat; 2) multiple imputation of missing data for confounding variables; 3) estimation of driving pressure from peak inspiratory pressure; 4) propensity score matching; 5) inverse probability of treatment weighting; 6) effect modification analyses by airway device, body mass index (BMI), surgical complexity, and long-acting opioids; 7) mixed-effects logistic regression analysis including individual anesthesia providers as random effects to account for variability in using low driving pressure across providers; 8) recategorization of the primary exposure and outcome based on quantiles and clinical definitions; 9) adjustment for the interaction of surgical service and work relative value units; 10) adjustment for the administration of sugammadex; 11) removal of neostigmine dose and duration of surgery from the confounder model; 12) removal of all intraoperative factors from the confounder model; 13) removal of variables with a high variance inflation factor from the confounder model; and 14) Lasso regression of the primary analysis. Details on all sensitivity analyses are provided in the ESM eAppendix 5.
Statistical analyses
All analyses were performed retrospectively with prespecified endpoints and statistical methods. Exploratory analyses were conducted after the results of the main analyses became available. The effect of lower driving pressure ventilation on nonhome discharge was tested using multivariable logistic regression and results are reported as adjusted odds ratios (aORs) with corresponding 95% confidence intervals (CIs). Possible adjusted fractional polynomial models were assessed.41 A P value of less than 0.05 was considered statistically significant. Path mediation analyses were conducted using single conditional models where each mediator was investigated separately, as previously published.26,42,43,44 Model discrimination of the primary regression model was assessed through the concordance c-statistic. Model calibration of the primary analysis was evaluated using the Hosmer–Lemeshow test and a reliability plot. Statistical analyses were performed using Stata (Version 16.1, StataCorp LLC, College Station, TX, USA) and R statistical software (Version 4.1.0, R Foundation for Statistical Computing, Vienna, Austria). Sample size calculation was done using G*Power (Version 3.1, Heinrich-Heine-University Duesseldorf, Duesseldorf, Germany). Statistical methods are further detailed in the ESM.
Results
Study cohort and characteristics
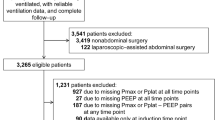
A total of 112,628 surgical patients aged 60 yr and older were screened for inclusion. After application of exclusion criteria and excluding cases with missing confounder data, the study cohort consisted of 87,407 patients (Fig. 1). Missing confounder data were present in 9.9% of the included observations (n = 9,588), with a missing at random pattern. The following variables used as confounders in the primary regression model had missing data: intraoperative hypotension (n = 14), vasopressor dose (n = 502), nondepolarizing neuromuscular blocking agents ED95 dose (n = 575), SPORC (n = 2,474), estimated household income (n = 4,737), BMI < 18.5 kg·m–2 (n = 2,355), BMI > 30 (n = 2,355), ASA Physical Status classification > II (n = 500), work relative value units (n = 187), and federal insurance (n = 70).
Study flow diagram
*Multiple criteria may apply
ED95 = median effective dose required to achieve a 95% reduction in maximal twitch response from baseline; ND-NMBA = nondepolarizing neuromuscular blocking agents; SPORC = Score for Prediction of Postoperative Respiratory Complications; work RVUs = work relative value units.
The median [interquartile range (IQR)] driving pressure in the study cohort was 15.0 [12.0–18.2] cm H2O. Characteristics of patients by a high vs low driving pressure are provided in Table 1. The rates of patients who experienced nonhome discharge by year are displayed in ESM eFig. 1.
Primary analysis
In total, 12,584 (14.4%) patients experienced nonhome discharge. The median [IQR] driving pressure in patients who experienced this endpoint was 16.0 [13.0–19.5] cm H2O vs 14.7 [12.0–18.0] cm H2O in those who did not (P < 0.001). After confounder adjustment, a lower driving pressure was associated with a reduced risk of nonhome discharge (aOR, 0.88; 95% CI, 0.83 to 0.93, per 10 cm H2O decrease; P < 0.001), corresponding to an adjusted risk difference of -1.1% (95% CI, -1.6 to -0.6; P < 0.001) per 10 cm H2O decrease in driving pressure (Fig. 2). This translated to a number needed to treat (NNT) of 92 (95% CI, 64 to 164). A higher order fractional polynomial model showed an equal deviance of 48,660 with insignificant difference in model fitness (P = 0.37) compared with the primary model. The primary model output is given in ESM eTable 1, the calibration plot in ESM eFig. 2, and the receiver operating characteristic (ROC) curve in ESM eFig. 3.
Driving pressure and the probability of nonhome discharge
Predicted probability of nonhome discharge as a function of intraoperatively applied driving pressure in cm H2O. A lower driving pressure was associated with lower predicted probability of nonhome discharge after anesthesia for surgery. The relationship between driving pressure and the outcome was tested for linearity and potential fractional polynomial models were assessed. The best model fit was observed for the linear model. Blue line: mean predicted probability of nonhome discharge; blue area: 95% confidence interval.
Path mediation analysis revealed that ventilation with low driving pressure was associated with lower rates of postoperative respiratory failure, which mediated 20.8% (95% CI, 15.0 to 56.8; P < 0.001) of the effect of lower driving pressure ventilation on nonhome discharge (ESM eFig. 4).
Secondary, exploratory, and sensitivity analyses
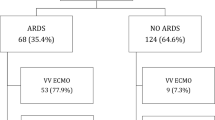
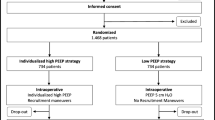
A total of 19,518 patients with low vs high driving pressure ventilation were matched in a 1:1 scheme based on their baseline standardized respiratory system compliance. After matching, the mean (standard deviation [SD]) driving pressure was 19.2 (4.1) cm H2O in patients in the high driving pressure group and 12.0 (2.1) cm H2O in patients in the low driving pressure group (standardized difference, 2.195). The baseline standardized compliance for both groups was 0.65 (0.13) mg·kg–1/cm H2O (standardized difference, 0.001; Fig. 3). In this matched cohort and after confounder adjustment, a low driving pressure was associated with a lower risk of nonhome discharge (aOR, 0.90; 95% CI, 0.81 to 1.00; P = 0.04), corresponding to an adjusted risk difference of -0.9% (95% CI, -1.8 to -0.0; P = 0.04).
Baseline respiratory system compliance in the nonmatched and matched cohorts
Baseline respiratory system compliance, defined as the median respiratory system compliance during the first ten minutes after intubation, for patients whose lungs were ventilated with high (≥ 15 cm H2O, navy) vs low (< 15 cm H2O, maroon) driving pressure, before (A) and after (B) matching for baseline respiratory system compliance.
The primary association between intraoperative low driving pressure ventilation and nonhome discharge was magnified in patients at a high baseline risk, defined as a DEPENDENSE score ≥ 37 (corresponding to a predicted risk of nonhome discharge of ≥ 8.8%) (aOR, 0.77; 95% CI, 0.73 to 0.81, per 10 cm H2O decrease; P < 0.001; P-for-interaction < 0.001). In the subgroup of patients that were at a high baseline risk, the adjusted risk difference was -2.4% (95% CI, -3.3 to -1.5; P < 0.001), translating to a NNT of 42 (95% CI, 31 to 67).
There was wide variability in the use of low (< 15 cm H2O) driving pressure across all 945 individual providers who provided anesthesia care. The adjusted probabilities of using low driving pressure ranged from 13.1% to 82.5% across individual caseloads (Fig. 4).
Variability in the use of low driving pressure across anesthesia providers
Predicted probabilities for the use of low driving pressure (< 15 cm H2O) during anesthesia (mean, black line, and 95% confidence interval, defined by the lines in navy) across individual anesthesia providers were obtained from an adjusted mixed-effects logistic regression model, including individual providers as random effects. The use of low driving pressure during anesthesia was subject to a large interprovider variability, with some providers using low driving pressure rarely (as low as 13.1%) and others more routinely (up to 82.5%).
There was a statistically significant association between lower driving pressure and intraoperative hypotension (aOR, 1.09; 95% CI, 1.05 to 1.14, per 10 cm H2O decrease; P < 0.001). Lower driving pressure ventilation was associated with a lower risk of major postoperative complications (aOR, 0.85; 95% CI, 0.79 to 0.91, per 10 cm H2O decrease; P < 0.001).
In subgroup analyses, lower driving pressure ventilation was significantly associated with a lower risk of nonhome discharge in hospitalized patients (aOR, 0.88; 95% CI, 0.84 to 0.93, per 10 cm H2O decrease; P < 0.001), patients with an ASA Physical Status classification of at least III (aOR, 0.89; 95% CI, 0.83 to 0.94, per 10 cm H2O decrease; P < 0.001), and patients with a prior diagnosis of chronic obstructive pulmonary disease (aOR, 0.81; 95% CI, 0.71 to 0.92, per 10 cm H2O decrease; P = 0.001).
The association of low driving pressure with nonhome discharge was in part mediated by a lower risk of postextubation desaturation (2.8% mediation; P = 0.01), the need for reintubation within seven days after surgery (18.9% mediation; P < 0.001), the need for noninvasive ventilation within seven days after surgery (10.3% mediation; P < 0.001), and a lower risk of major postoperative complications within 30 days of surgery (9.7% mediation; P < 0.001).
Further details on secondary and exploratory analyses are provided in the ESM eAppendices 3 and 4.
Our primary findings remained robust across all sensitivity analyses, as detailed in Table 2 and in the ESM eAppendix 5. Quintiles of driving pressure and nonhome discharge are given in ESM eTable 2, patient characteristics and distribution of variables in the propensity score-matched cohort in ESM eTable 3, and patient characteristics and distribution of variables in the primary cohort by nonhome discharge in ESM eTable 4. A histogram of the variables with missing data and the pattern of missingness are shown in ESM eFig. 5.
Discussion
In this multicentre study of surgical patients aged 60 yr and older, intraoperative mechanical ventilation maintaining lower driving pressure was associated with a lower risk of nonhome discharge, which was more pronounced in patients at a high baseline risk of nonhome discharge. Patients’ respiratory mechanics were further accounted for by matching based on baseline compliance. The association of a low driving pressure with nonhome discharge was partially mediated by a reduction in postoperative respiratory failure.
Previous studies have illustrated the relevance of intraoperative lung-protective ventilation strategies maintaining low inspiratory pressure in avoiding postoperative adverse events including pulmonary and extrapulmonary complications.16,17,18,19,45,46 A secondary analysis of randomized controlled trials found that interventions such as lowering the tidal volume and the application of PEEP mediate their effects on lowering postoperative respiratory complications through a reduction in driving pressure.19 Our study adds to these findings that a lower intraoperative driving pressure might be a potential target for maintaining patients’ functional status and autonomy by mitigating the risk of nonhome discharge. Maintenance of independent living is an important patient-centered outcome and a relevant performance metric after surgery.3,13,47 Opposed to previously identified risk factors,6,7,8,9,10,47,48 our findings suggest that the intraoperative driving pressure might represent one of few modifiable factors associated with nonhome discharge.
While physicians can modify the intraoperative driving pressure by changing the applied tidal volume or adjusting PEEP, the individual patient’s respiratory mechanics, characterized by the compliance of the respiratory system, are an important determinant. Patients with poor respiratory system compliance that increases the driving pressure, for example, through structural lung disease or increased stiffness of the chest wall, are at high risk of postoperative respiratory failure and therefore at increased risk of discharge to a nursing home.14,49 Consequently, the question arises whether a high intraoperative driving pressure reflects pre-existing or developing lung injury characterized by impaired pulmonary mechanics,50 or whether ventilation with high driving pressure is causally related to nonhome discharge. To address this, we matched patients by their standardized respiratory system compliance. In this analysis, we were able to create two groups with comparable baseline compliance, but different driving pressures (12 vs 19 cm H2O). We believe that this was possible because of the variability in driving pressures among anesthesia providers observed in our study, which reflects practice patterns worldwide.51,52 This analysis controlling for patients’ respiratory system mechanics confirmed our primary findings, thereby supporting the conclusion that the intraoperative driving pressure is not merely a reflection of lung disease and poor functional status at baseline but may impact postoperative recovery and maintenance of independence. This is further supported by experimental data linking high driving pressure to pulmonary stress, which can initiate and propagate ventilator-induced lung injury53 and contribute to extrapulmonary organ dysfunction through systemic release of inflammatory mediators.54,55,56 Previous studies further indicated that lung tissue damage is closely related to the amplitude of cyclic stress, depicted by the driving pressure22 and higher driving pressures may decompartmentalize lung tissue, characterized by stress failure of epithelial and endothelial layers with subsequent promotion of organ dysfunction by the systemic release of inflammatory mediators into the lungs and circulation.57 Even in non-injured lungs, overstretching can lead to inhomogeneous recruitment and expansion of lung areas, which can enhance mechanical stress.58 High pressure is further known to damage the fragile pulmonary intercellular matrix structure.59 These injuries to epithelial and endothelial layers might facilitate bacterial translocation, and the presence of postoperative atelectasis might result in more favorable conditions for bacterial growth.19
Our findings may be explained as a result of minimizing ventilator-induced lung injury and extrapulmonary organ dysfunction, which is supported by our finding that the effect of lower intraoperative driving pressure on reduced nonhome discharge was partially mediated by a reduction in postoperative respiratory failure, the occurrence of postextubation oxygen desaturation, the requirement of reintubation or noninvasive ventilation, and major postoperative complications. Based on our results, physicians should establish strategies to measure and reduce intraoperative driving pressure, supporting a recent consensus statement.60 While the effect in our overall cohort was rather small with an NNT of 92, we identified a larger effect size in patients with a high baseline risk for nonhome discharge, reflected by a NNT of 42 (95% upper limit, 67). Nonhome discharge is a serious and potentially devastating event for patients and their families2,3 and our data identify a lower driving pressure as a potential zero-cost intervention. Low driving pressure ventilation can be implemented through judicious application of tidal volume, in particular in patients with impaired respiratory system compliance,61 as well as titration of PEEP to maintain optimum intratidal compliance.19 Recruitment maneuvers after induction of anesthesia might lower the driving pressure by reducing atelectasis and increasing functional lung volume; however, they might threaten hemodynamic stability and are of unproven beneficial effect.62,63 Future randomized controlled studies on nonhome discharge after intraoperative mechanical ventilation are warranted in patients aged 60 yr and older living at home before undergoing noncardiothoracic and nonlaparoscopic surgery with general anesthesia. Assuming the observed incidence of nonhome discharge of 14.4% in our study, a two-sided alpha of 0.05, and the statistical power set to 80%, a sample size of 2,546 would be required in a future clinical trial to detect a difference in the risk of nonhome discharge of at least 15.0%64 between patients who were exposed to high (≥ 15 cm H2O) vs low (< 15 cm H2O) driving pressure (effect size = 0.062). This design could benefit from a pilot study assessing feasibility of applying this protocol if stratification by baseline compliance is used.
Limitations
Limitations arise from the retrospective design of the study as residual unidentified confounding cannot be fully excluded, especially when analyzing routinely collected billing, administrative, and clinical data. We conducted several exploratory and sensitivity analyses to mitigate the inherently arising limitations of working with observational data. Furthermore, data from a limited geographical region were analyzed and data on functional status in patients living at home prior to hospital admission were not readily available. The course of hospital discharge may have further been influenced by distinct insurance plans, and ultimately, being discharged to a nursing facility may still yield independent living in some cases. Nevertheless, the large cohort size allowed for a wide range of confounder adjustments, and the robustness of the results was confirmed in several sensitivity analyses. We calculated driving pressure from data acquired during routine clinical practice, where Pplat might not always be adequate as the duration of the plateau rarely exceeds 10% of inspiratory time with routine ventilator settings. In addition, driving pressure was estimated from peak inspiratory pressure where Pplat was missing. This might have resulted in an overestimation of the driving pressure by including the pressure required to overcome airway resistance. Most accurate data would involve esophageal manometry to estimate pleural pressure and calculate transpulmonary pressure; however, it is important to point out that the vast majority of data on driving pressure from patients with acute respiratory distress syndrome similarly only used data from retrospective datasets.65,66
A major part of causal inference with observational data is identifying and measuring important confounders and including them correctly in the statistical model; however, key sources of bias cannot always be fully excluded.67 Therefore, comparing results across methods with different sources of bias is an important element.68
Despite these limitations, we are convinced that our findings in a large patient collective provide clinically relevant information and identify potential mechanisms as well as patients at high risk and will therefore help inform the design of future randomized controlled trials.
Conclusion
Intraoperative mechanical ventilation maintaining lower driving pressure is associated with a lower risk of nonhome discharge, which can be partially explained by lowered rates of postoperative respiratory failure. This effect is especially relevant in patients with a high baseline risk of nonhome discharge. Future randomized controlled trials should target driving pressure as a potential intervention to decrease nonhome discharge.
References
Weiser TG, Haynes AB, Molina G, et al. Size and distribution of the global volume of surgery in 2012. Bull World Health Organ 2016; 94: 201–9F. https://doi.org/10.2471/blt.15.159293
Weyker PD, Webb CA, Flynn BC. Adverse discharge disposition (ADD): when things do not ADD up after surgery. J Cardiothorac Vasc Anesth 2021; 35: 490–1. https://doi.org/10.1053/j.jvca.2020.09.095
Koppitz AL, Dreizler J, Altherr J, Bosshard G, Naef R, Imhof L. Relocation experiences with unplanned admission to a nursing home: a qualitative study. Int Psychogeriatr 2017; 29: 517–27. https://doi.org/10.1017/s1041610216001964
Xiao R, Miller JA, Zafirau WJ, Gorodeski EZ, Young JB. Impact of home health care on health care resource utilization following hospital discharge: a cohort study. Am J Med 2018; 131: 395–407. https://doi.org/10.1016/j.amjmed.2017.11.010
Genworth. Genworth 2020 cost of care survey: home care providers, adult day health care facilities, assisted living facilities and nursing homes, 2020. https://pro.genworth.com/riiproweb/productinfo/pdf/131168.pdf (accessed October 2022).
Schaefer MS, Hammer M, Platzbecker K, et al. What factors predict adverse discharge disposition in patients older than 60 years undergoing lower-extremity surgery? The adverse discharge in older patients after lower-extremity surgery (ADELES) risk score. Clin Orthop Relat Res 2021; 479: 546–7. https://doi.org/10.1097/corr.0000000000001532
Gosling AF, Hammer M, Grabitz S, et al. Development of an instrument for preoperative prediction of adverse discharge in patients scheduled for cardiac surgery. J Cardiothorac Vasc Anesth 2021; 35: 482–9. https://doi.org/10.1053/j.jvca.2020.08.028
Hammer M, Althoff FC, Platzbecker K, et al. Discharge prediction for patients undergoing inpatient surgery: development and validation of the DEPENDENSE score. Acta Anaesthesiol Scand 2021; 65: 607–17. https://doi.org/10.1111/aas.13778
Wang HT, Carrier FM, Tremblay A, et al. Outcomes of vulnerable elderly patients undergoing elective major surgery: a prospective cohort study. Can J Anesth 2020; 67: 847–56. https://doi.org/10.1007/s12630-020-01646-z
Beggs T, Sepehri A, Szwajcer A, Tangri N, Arora RC. Frailty and perioperative outcomes: a narrative review. Can J Anesth 2015; 62: 143–57. https://doi.org/10.1007/s12630-014-0273-z
Scheffenbichler FT, Teja B, Wongtangman K, et al. Effects of the level and duration of mobilization therapy in the surgical ICU on the loss of the ability to live independently: an international prospective cohort study. Crit Care Med 2021; 49: e247–57. https://doi.org/10.1097/ccm.0000000000004808
Schaller SJ, Anstey M, Blobner M, et al. Early, goal-directed mobilisation in the surgical intensive care unit: a randomised controlled trial. Lancet 2016; 388: 1377–88. https://doi.org/10.1016/s0140-6736(16)31637-3
Rostin P, Teja BJ, Friedrich S, et al. The association of early postoperative desaturation in the operating theatre with hospital discharge to a skilled nursing or long-term care facility. Anaesthesia 2019; 74: 457–67. https://doi.org/10.1111/anae.14517
Sprung J, Gajic O, Warner DO. Review article: age related alterations in respiratory function - anesthetic considerations. Can J Anesth 2006; 53: 1244–57. https://doi.org/10.1007/bf03021586
Bagchi A, Rudolph MI, Ng PY, et al. The association of postoperative pulmonary complications in 109,360 patients with pressure-controlled or volume-controlled ventilation. Anaesthesia 2017; 72: 1334–43. https://doi.org/10.1111/anae.14039
Park M, Ahn HJ, Kim JA, et al. Driving pressure during thoracic surgery: a randomized clinical trial. Anesthesiology 2019; 130: 385–93. https://doi.org/10.1097/aln.0000000000002600
Blum JM, Stentz MJ, Dechert R, et al. Preoperative and intraoperative predictors of postoperative acute respiratory distress syndrome in a general surgical population. Anesthesiology 2013; 118: 19–29. https://doi.org/10.1097/aln.0b013e3182794975
Mazzinari G, Serpa Neto A, Hemmes SN, et al. The association of intraoperative driving pressure with postoperative pulmonary complications in open versus closed abdominal surgery patients - a posthoc propensity score-weighted cohort analysis of the LAS VEGAS study. BMC Anesthesiol 2021; 21: 84. https://doi.org/10.1186/s12871-021-01268-y
Serpa Neto AS, Hemmes SN, Barbas CS, et al. Association between driving pressure and development of postoperative pulmonary complications in patients undergoing mechanical ventilation for general anaesthesia: a meta-analysis of individual patient data. Lancet Respir Med 2016; 4: 272–80. https://doi.org/10.1016/s2213-2600(16)00057-6
Wellman TJ, Winkler T, Costa EL, et al. Effect of local tidal lung strain on inflammation in normal and lipopolysaccharide-exposed sheep. Crit Care Med 2014; 42: e491–500. https://doi.org/10.1097/ccm.0000000000000346
Sweeney FJ, Pereira MJ, Eskra JD, Carty TJ. The use of 12-hydroxyheptadecatrienoic acid (HHT) as an HPLC/spectrophotometric marker for cyclooxygenase pathway activity in resident rat peritoneal cells. Prostaglandins Leukot Med 1987; 26: 171–7. https://doi.org/10.1016/0262-1746(87)90027-8
Tschumperlin DJ, Oswari J, Margulies AS. Deformation-induced injury of alveolar epithelial cells. Effect of frequency, duration, and amplitude. Am J Respir Crit Care Med 2000; 162: 357–62. https://doi.org/10.1164/ajrccm.162.2.9807003
Wolthuis EK, Choi G, Dessing MC, et al. Mechanical ventilation with lower tidal volumes and positive end-expiratory pressure prevents pulmonary inflammation in patients without preexisting lung injury. Anesthesiology 2008; 108: 46–54. https://doi.org/10.1097/01.anes.0000296068.80921.10
Ranieri VM, Giunta F, Suter PM, Slutsky AS. Mechanical ventilation as a mediator of multisystem organ failure in acute respiratory distress syndrome. JAMA 2000; 284: 43–4. https://doi.org/10.1001/jama.284.1.43
von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med 2007; 4: e296. https://doi.org/10.1371/journal.pmed.0040296
Wachtendorf LJ, Azimaraghi O, Rangasamy V, et al. Preoperative treatment of severe diabetes mellitus and hypertension mitigates healthcare disparities and prevents adverse postoperative discharge to a nursing home. Ann Surg 2022; 276: e185–91. https://doi.org/10.1097/sla.0000000000005544
Joseph B, Pandit V, Zangbar B, et al. Superiority of frailty over age in predicting outcomes among geriatric trauma patients: a prospective analysis. JAMA Surg 2014; 149: 766–72. https://doi.org/10.1001/jamasurg.2014.296
Brueckmann B, Villa-Uribe JL, Bateman BT, et al. Development and validation of a score for prediction of postoperative respiratory complications. Anesthesiology 2013; 118: 1276–85. https://doi.org/10.1097/aln.0b013e318293065c
Schneeweiss S, Maclure M. Use of comorbidity scores for control of confounding in studies using administrative databases. Int J Epidemiol 2000; 29: 891–8. https://doi.org/10.1093/ije/29.5.891
Lukannek C, Shaefi S, Platzbecker K, et al. The development and validation of the Score for the Prediction of Postoperative Respiratory Complications (SPORC‐2) to predict the requirement for early postoperative tracheal re‐intubation: a hospital registry study. Anaesthesia 2019; 74: 1165–74. https://doi.org/10.1111/anae.14742
Shaydenfish D, Wongtangman K, Eikermann M, Schaefer MS. The effects of acetylcholinesterase inhibitors on morbidity after general anesthesia and surgery. Neuropharmacology 2020; 173: 108134. https://doi.org/10.1016/j.neuropharm.2020.108134
Rudolph MI, Chitilian HV, Ng PY, et al. Implementation of a new strategy to improve the peri-operative management of neuromuscular blockade and its effects on postoperative pulmonary complications. Anaesthesia 2018; 73: 1067–78. https://doi.org/10.1111/anae.14326
Obeidat SS, Wongtangman K, Blank M, et al. The association of nitrous oxide on length of stay in the postanesthesia care unit: a retrospective observational study. Can J Anesth 2021; 68: 1630–40. https://doi.org/10.1007/s12630-021-02067-2
Stahl DL, Groeben H, Kroepfl D, Gautam S, Eikermann M. Development and validation of a novel tool to estimate peri-operative blood loss. Anaesthesia 2012; 67: 479–86. https://doi.org/10.1111/j.1365-2044.2011.06916.x
Santer P, Zheng S, Hammer M, et al. Ventilatory frequency during intraoperative mechanical ventilation and postoperative pulmonary complications: a hospital registry study. Br J Anaesth 2020; 125: e130–9. https://doi.org/10.1016/j.bja.2020.02.018
Schaefer MS, Hammer M, Santer P, et al. Succinylcholine and postoperative pulmonary complications: a retrospective cohort study using registry data from two hospital networks. Br J Anaesth 2020; 125: 629–36. https://doi.org/10.1016/j.bja.2020.05.059
Althoff FC, Xu X, Wachtendorf LJ, et al. Provider variability in the intraoperative use of neuromuscular blocking agents: a retrospective multicentre cohort study. BMJ Open 2021; 11: e048509. https://doi.org/10.1136/bmjopen-2020-048509
Jones PM, Cherry RA, Allen BN, et al. Association between handover of anesthesia care and adverse postoperative outcomes among patients undergoing major surgery. JAMA 2018; 319: 143–53. https://doi.org/10.1001/jama.2017.20040
Hammer M, Santer P, Schaefer MS, et al. Supraglottic airway device versus tracheal intubation and the risk of emergent postoperative intubation after general anaesthesia in adults: a retrospective cohort study. Br J Anaesth 2021; 126: 738–45. https://doi.org/10.1016/j.bja.2020.10.040
Santer P, Wachtendorf LJ, Suleiman A, et al. Mechanical power during general anesthesia and postoperative respiratory failure: a multicenter retrospective cohort study. Anesthesiology 2022; 137: 41–54. https://doi.org/10.1097/aln.0000000000004256
Royston P, Altman DG. Regression using fractional polynomials of continuous covariates: parsimonious parametric modelling. J R Stat Soc Ser C Appl Stat 1994; 43: 429–53. https://doi.org/10.2307/2986270
Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: new procedures and recommendations. Psychol Methods 2002; 7: 422–45.
Imai K, Keele L, Tingley D. A general approach to causal mediation analysis. Psychol Methods 2010; 15: 309–34. https://doi.org/10.1037/a0020761
Althoff FC, Wachtendorf LJ, Rostin P, et al. Effects of night surgery on postoperative mortality and morbidity: a multicentre cohort study. BMJ Qual Saf 2021; 30: 678–88. https://doi.org/10.1136/bmjqs-2020-011684
Severgnini P, Selmo G, Lanza C, et al. Protective mechanical ventilation during general anesthesia for open abdominal surgery improves postoperative pulmonary function. Anesthesiology 2013; 118: 1307–21. https://doi.org/10.1097/aln.0b013e31829102de
Ladha K, Vidal Melo MF, McLean DJ, et al. Intraoperative protective mechanical ventilation and risk of postoperative respiratory complications: hospital based registry study. BMJ 2015; 351: h3646. https://doi.org/10.1136/bmj.h3646
Mohanty S, Liu Y, Paruch JL, et al. Risk of discharge to postacute care: a patient-centered outcome for the American College of Surgeons national surgical quality improvement program surgical risk calculator. JAMA Surg 2015; 150: 480–4. https://doi.org/10.1001/jamasurg.2014.3176
Hyder JA, Wakeam E, Habermann EB, Hess EP, Cima RR, Nguyen LL. Derivation and validation of a simple calculator to predict home discharge after surgery. J Am Coll Surg 2014; 218: 226–236. https://doi.org/10.1016/j.jamcollsurg.2013.11.002
Chan R, Ueno R, Afroz A, Billah B, Tiruvoipati R, Subramaniam A. Association between frailty and clinical outcomes in surgical patients admitted to intensive care units: a systematic review and meta-analysis. Br J Anaesth 2022; 128: 258–71. https://doi.org/10.1016/j.bja.2021.11.018
Baedorf Kassis E, Loring SH, Talmor D. Mortality and pulmonary mechanics in relation to respiratory system and transpulmonary driving pressures in ARDS. Intensive Care Med 2016; 42: 1206–13. https://doi.org/10.1007/s00134-016-4403-7
Ladha KS, Bateman BT, Houle TT, et al. Variability in the use of protective mechanical ventilation during general anesthesia. Anesth Analg 2018; 126: 503–12. https://doi.org/10.1213/ane.0000000000002343
LAS VEGAS investigators. Epidemiology, practice of ventilation and outcome for patients at increased risk of postoperative pulmonary complications: LAS VEGAS - an observational study in 29 countries. Eur J Anaesthesiol 2017; 34: 492–507. https://doi.org/10.1097/eja.0000000000000646
Webb HH, Tierney DF. Experimental pulmonary edema due to intermittent positive pressure ventilation with high inflation pressures. Protection by positive end-expiratory pressure. Am Rev Respir Dis 1974; 110: 556–65. https://doi.org/10.1164/arrd.1974.110.5.556
Imai Y, Parodo J, Kajikawa O, et al. Injurious mechanical ventilation and end-organ epithelial cell apoptosis and organ dysfunction in an experimental model of acute respiratory distress syndrome. JAMA 2003; 289: 2104–12. https://doi.org/10.1001/jama.289.16.2104
Caironi P, Cressoni M, Chiumello D, et al. Lung opening and closing during ventilation of acute respiratory distress syndrome. Am J Respir Crit Care Med 2010; 181: 578–86. https://doi.org/10.1164/rccm.200905-0787oc
Dreyfuss D, Saumon G. Role of tidal volume, FRC, and end-inspiratory volume in the development of pulmonary edema following mechanical ventilation. Am Rev Respir Dis 1993; 148: 1194–203. https://doi.org/10.1164/ajrccm/148.5.1194
Dos Santos CC, Slutsky AS. Invited review: mechanisms of ventilator-induced lung injury: a perspective. J Appl Physiol 2000; 89: 1645–55. https://doi.org/10.1152/jappl.2000.89.4.1645
Mead J, Takishima T, Leith D. Stress distribution in lungs: a model of pulmonary elasticity. J Appl Physiol 1970; 28: 596–608. https://doi.org/10.1152/jappl.1970.28.5.596
Moriondo A, Pelosi P, Passi A, et al. Proteoglycan fragmentation and respiratory mechanics in mechanically ventilated healthy rats. J Appl Physiol 2007; 103: 747–56. https://doi.org/10.1152/japplphysiol.00056.2007
Young CC, Harris EM, Vacchiano C, et al. Lung-protective ventilation for the surgical patient: international expert panel-based consensus recommendations. Br J Anaesth 2019; 123: 898–913. https://doi.org/10.1016/j.bja.2019.08.017
Suleiman A, Costa E, Santer P, et al. Association between intraoperative tidal volume and postoperative respiratory complications is dependent on respiratory elastance: a retrospective, multicentre cohort study. Br J Anaesth 2022; 129: 263–72. https://doi.org/10.1016/j.bja.2022.05.005
Writing Committee for the PROBESE Collaborative Group of the PROtective VEntilation Network (PROVEnet) for the Clinical Trial Network of the European Society of Anaesthesiology, Bluth T, Serpa Neto A, et al. Effect of intraoperative high positive end-expiratory pressure (PEEP) with recruitment maneuvers vs low PEEP on postoperative pulmonary complications in obese patients: a randomized clinical trial. JAMA 2019; 321: 2292–305. https://doi.org/10.1001/jama.2019.7505
Futier E, Constantin J-M, Paugam-Burtz C, et al. A trial of intraoperative low-tidal-volume ventilation in abdominal surgery. N Engl J Med 2013; 369: 428–37. https://doi.org/10.1056/nejmoa1301082
Wachtendorf LJ, Azimaraghi O, Santer P, et al. Association between intraoperative arterial hypotension and postoperative delirium after noncardiac surgery: a retrospective multicenter cohort study. Anesth Analg 2021; 134: 822–33. https://doi.org/10.1213/ane.0000000000005739
Amato MBP, Meade MO, Slutsky AS, et al. Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med 2015; 372: 747–55. https://doi.org/10.1056/nejmsa1410639
Goligher EC, Costa EL, Yarnell CJ, et al. Effect of lowering vt on mortality in acute respiratory distress syndrome varies with respiratory system elastance. Am J Respir Crit Care Med 2021; 203: 1378–85. https://doi.org/10.1164/rccm.202009-3536oc
Hammerton G, Munafò MR. Causal inference with observational data: the need for triangulation of evidence. Psychol Med 2021; 51: 563–78. https://doi.org/10.1017/s0033291720005127
Richmond RC, Al-Amin A, Smith GD, Relton CL. Approaches for drawing causal inferences from epidemiological birth cohorts: a review. Early Hum Dev 2014; 90: 769–80. https://doi.org/10.1016/j.earlhumdev.2014.08.023
Author contributions
Tim M. Tartler contributed to study concept and design, data collection, data analysis, interpretation of the data, drafting the manuscript, and critical revision of the manuscript. Tim M. Tartler conducted this work in partial fulfillment of the requirements for an MD thesis. Luca J. Wachtendorf, Aiman Suleiman, and Maximilian S. Schaefer contributed to study concept and design, data collection, data analysis, interpretation of the data, drafting the manuscript, critical revision of the manuscript, and final approval of the version to be submitted. Michael Blank, Felix C. Linhardt, and Peter Santer contributed to data collection, data analysis, interpretation of the data, and critical revision of the manuscript. Elena Ahrens contributed to data analysis, interpretation of the data, and critical revision of the manuscript. Friederike C. Althoff and Alexander Nagrebetsky contributed to interpretation of the data and critical revision of the manuscript. Guanqing Chen contributed to study concept and design, data collection, data analysis, interpretation of the data, and critical revision of the manuscript. Matthias Eikermann contributed to study concept and design, interpretation of the data, and critical revision of the manuscript. All authors confirm that they have met the criteria for authorship as established by the ICMJE and believe that the paper represents honest work and are able to verify the validity of the results reported. The manuscript's guarantor is Maximilian S. Schaefer. He affirms that this manuscript is an honest, accurate, and transparent account of the study being reported.
Acknowledgements
We are grateful to Dr. Ricardo Munoz-Acuna for his assistance with the study.
Disclosures
Matthias Eikermann is an Associate Editor of the British Journal of Anaesthesia. Maximilian S. Schaefer is an Associate Editor for BMC Anesthesiology. Tim M. Tartler, Luca J. Wachtendorf, Aiman Suleiman, Michael Blank, Elena Ahrens, Felix C. Linhardt, Friederike C. Althoff, Guanqing Chen, Peter Santer, and Alexander Nagrebetsky have no conflict of interests.
Funding statement
Matthias Eikermann received unrestricted funds from philanthropic donors Jeffrey and Judith Buzen during the study period and has received grants for investigator-initiated trials not related to this manuscript from Merck & Co and serves as a consultant on the advisory board of Merck & Co. The funders had no role in the design and conduct of the study, the collection, management, analysis, and interpretation of the data, the preparation, review, or approval of the manuscript, or the decision to submit the manuscript for publication. Maximilian S. Schaefer has received grants for investigator-initiated trials not related to this manuscript from Merck & Co.
Editorial responsibility
This submission was handled by Dr. Stephan K. W. Schwarz, Editor-in-Chief, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Preliminary data of this study were presented at the International Anesthesia Research Society and Association of University Anesthesiologists meetings in March 2022.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tartler, T.M., Wachtendorf, L.J., Suleiman, A. et al. The association of intraoperative low driving pressure ventilation and nonhome discharge: a historical cohort study. Can J Anesth/J Can Anesth 70, 359–373 (2023). https://doi.org/10.1007/s12630-022-02378-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-022-02378-y