Abstract
Purpose
To assess whether intraoperative use of nitrous oxide (N2O) as an adjunct to general anesthesia is associated with a shorter length of stay in the postanesthesia care unit (PACU).
Methods
We analyzed data from adult patients who underwent non-cardiothoracic surgery under general anesthesia between May 2008 and December 2018. We assessed the association between intraoperative low- and high-dose N2O and PACU length of stay.
Results
A total of 148,284 patients were included in the primary analysis. After adjusting for a priori defined confounders, a high dose of N2O significantly decreased PACU length of stay, with a calculated difference of −9.1 min (95% confidence interval [CI], −10.5 to −7.7; P < 0.001). Patients who received high-dose N2O had a lower incidence of both short- and prolonged-duration of intraoperative hypotension (adjusted odds ratio [aOR], 0.85; 95% CI, 0.83 to 0.88; P < 0.001 and aOR, 0.76; 95% CI, 0.73 to 0.80; P < 0.001, respectively) and received a lower total intraoperative vasopressor dose (−0.04 mg of norepinephrine equivalents; 95% CI, −0.06 to −0.01; P = 0.01). The effect of high-dose N2O on PACU length of stay was modified by surgical complexity (adjusted absolute difference: −26.1 min; 95% CI, −29.2 to −23.1; P < 0.001; P for interaction < 0.001), and most pronounced in patients who underwent complex surgery and received intraoperative antiemetic therapy (adjusted absolute difference: −38.9 min; 95% CI, −43.1 to −34.6; P < 0.001; P for interaction < 0.001).
Conclusions
Nitrous oxide was dose-dependently associated with a decreased PACU length of stay. The effect was clinically relevant (> 30 min difference) in patients who underwent complex surgical procedures and received intraoperative antiemetic therapy.
Résumé
Objectif
L’objectif de cette étude était de déterminer si l’utilisation peropératoire de protoxyde d’azote (N2O) en complément à l’anesthésie générale était associée à une durée de séjour écourtée en salle de réveil (SDR).
Méthode
Nous avons analysé les données de patients adultes qui ont subi une chirurgie non cardiothoracique sous anesthésie générale entre mai 2008 et décembre 2018. Nous avons évalué l’association entre une faible dose et une dose élevée de N2O peropératoire et la durée du séjour en SDR.
Résultats
Au total, 148 284 patients ont été inclus dans notre analyse primaire. Après ajustement tenant compte des facteurs de confusion définis a priori, une dose élevée de N2O a considérablement écourté la durée du séjour en salle de réveil, avec une différence calculée de −9,1 min (intervalle de confiance [IC] à 95 %, −10,5 à −7,7 ; P < 0,001). Chez les patients ayant reçu une dose élevée de N2O, l’incidence d’hypotension peropératoire de courte ou plus longue durée était plus faible (rapport de cotes ajusté [RCA], 0,85; IC 95 %, 0,83 à 0,88; P < 0,001 et RCA, 0,76; IC 95 %, 0,73 à 0,80; P < 0,001, respectivement); en outre, ces patients ont reçu une dose totale de vasopresseurs peropératoires inférieure (−0,04 mg d’équivalents de norépinéphrine; IC 95 %, −0,06 à −0,01; P = 0,01). L’effet d’une dose élevée de N2O sur la durée du séjour en SDR a été modifié par la complexité de la chirurgie (différence absolue ajustée : −26,1 min; IC 95 %, −29,2 à −23,1; P < 0,001; P pour l’interaction < 0,001), et était le plus prononcé chez les patients ayant subi une chirurgie complexe et reçu un traitement antiémétique peropératoire (différence absolue ajustée : −38,9 min; IC 95 %, −43,1 à −34,6; P < 0,001; P pour l’interaction < 0,001).
Conclusion
Le protoxyde d’azote a été associé de façon dose-dépendante à une réduction de la durée du séjour en SDR. L’effet était cliniquement pertinent (différence > 30 minutes) chez les patients qui subissaient des interventions chirurgicales complexes et recevaient un traitement antiémétique peropératoire.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Optimal early postoperative care increases perioperative safety and reduces postoperative morbidity and mortality.1 The length of stay in the postanesthesia care unit (PACU)is dependent on a number of factors, including both medical and non-medical related factors.2 PACUs require large nurse-to-patient ratios similar to an intensive care unit (ICU), which contributes to a high cost of care. Discharge delays can create a PACU wait list, which may affect surgical case volume in specific scenarios.3,4 To optimize early postoperative healthcare utilization, PACU length of stay should be as short as reasonably possible.2,5,6,7
Nitrous oxide has been used in general anesthesia since 1844 and helps to facilitate emergence.8,9,10 It is unclear whether a faster emergence of anesthesia with N2O translates to a shorter length of stay in the PACU, since N2O also dose-dependently increases the risk of postoperative nausea and vomiting (PONV), and its rapid diffusion may increase intraluminal bowel volume.11,12,13,14 In this study, we sought to assess whether intraoperative use of N2O as an adjunct to general anesthesia is associated with a shorter length of stay in the PACU.
Methods
Study design
In this retrospective observational hospital registry study, we analyzed available data of surgical cases performed between May 2008 and December 2018 at an academic teaching hospital (Beth Israel Deaconess Medical Center) in Massachusetts, United States. This study used de-identified data from the institutional Anesthesia Research Data Repository, which was prospectively approved by the local institutional review board (Committee on Clinical Investigations, protocol number 2018P000666). The requirement for informed written consent was waived. Data were collected from multiple hospital databases comprising patient-, surgery-, anesthesia-, ICU-, and outcome-related data. Data sources used in establishing the data repository are described in the Electronic Supplementary Material [ESM], eAppendix 1.
Patient selection
Adult patients undergoing non-cardiothoracic surgery under general anesthesia with sufficient data on PACU length of stay were considered for inclusion in this study. We excluded patients with an American Society of Anesthesiologists (ASA) Physical Status Classification of V and VI, patients who were admitted to the ICU before surgery, and patients who had more than one surgical procedure within the preceding month. Cases with missing data for the primary analysis were excluded and the complete case method was used for the primary analysis.
Exposure and outcome measures
The primary exposure variable was defined a priori as intraoperative use of N2O at any time from induction of anesthesia to emergence as an adjunct to general anesthesia. N2O was categorized into a low-dose and a high-dose group using the median of average end-tidal N2O concentration as a cut-off. The a priori defined primary outcome was PACU length of stay, defined as the time from a patient’s arrival in the PACU until discharge in minutes. Secondary outcomes included the incidence of intraoperative hypotension and the intraoperative use of vasopressors. Intraoperative hypotension was defined as mean arterial pressure below 55 mm Hg and categorized as short (1–15 min) and prolonged (> 15 min) duration.15 The intraoperative use of vasopressors was defined as the total dose of administered vasopressors including phenylephrine, ephedrine, epinephrine, and norepinephrine converted to norepinephrine equivalents in mg.
Confounder model
Analyses were adjusted for a priori defined confounders based on available literature. Confounders included patient demographics (age, sex, body mass index), comorbidities (ASA Physical Status Classification, Charlson Comorbidity Index, high risk of postoperative respiratory complications [defined by Score for Prediction of Postoperative Respiratory Complications ≥ 7], and preoperative opioid prescriptions), procedure-related confounders (type of surgery, emergency surgery, high-risk surgery [i.e., neurosurgery, colorectal, transplant, vascular or burn surgery], admission type, duration of surgery, work relative value units [RVUs], and intraoperative anesthesia-related factors [neuromuscular blocking agent dose, neostigmine dose, intravenous administered fluid volume, and transfused packed red blood cell units]).16,17,18,19,20,21
Primary and secondary analyses
In the primary analysis, we assessed the effect of low and high doses of N2O compared with no administration of N2O on PACU length of stay. We conducted the primary analysis in the full cohort. As a co-primary analysis, we used propensity score matching and compared no N2O vs high-dose N2O (ESM, eAppendix 2).
In secondary analyses, we evaluated the effect of low and high doses of N2O compared with no N2O administration on the incidence of intraoperative hypotension and intraoperative vasopressor use.
Exploratory analyses
With an exploratory intent, we tested whether the association of N2O and PACU length of stay was mediated by intraoperative hypotension or PONV using formal path mediation analysis (ESM, eAppendix 3). To better understand the differences in the effect of N2O on the length of stay in the PACU in various settings, we investigated the effect modification of the primary association by complex surgery, defined as the combination of a high duration of surgery, high work RVUs, and inpatient setting. In addition, we assessed whether intraoperative antiemetic therapy (any type and any dose) had modifying effects on the primary association, and whether the effect of N2O on the length of stay in the PACU was different in complex surgeries with antiemetic therapy compared with complex surgeries without antiemetic therapy. Lastly, we assessed the association between N2O and 30-day hospital readmission after ambulatory procedures, using the PREdicting admission after Outpatient Procedures score as a confounder in the logistic regression model.22
Sensitivity analyses
To evaluate whether the association between N2O and PACU length of stay was modified by surgical factors, we performed effect modification and subgroup analyses. We investigated interaction terms between high-dose N2O and the following dichotomized variables (based on the median as cut-off): duration of surgery (≤ 123 vs > 123 min), work RVUs (≤ 11.92 vs > 11.92) as well as the surgical setting (inpatient vs ambulatory surgery), and the type of abdominal surgery (open vs laparoscopic).
Statistical analyses
The linearity assumption between outcome and confounding variables was tested using scatter plots. To adjust for non-linear relationships, we divided continuous variables into quintiles or clinically relevant groups. We used multivariable zero-truncated negative binomial regression to assess the effect of N2O on PACU length of stay. Multivariable logistic regression was used to assess the effect of N2O on intraoperative hypotension. For continuous outcome data (vasopressor dose in mg norepinephrine equivalents), we performed multivariable linear regression. Results are presented as adjusted incidence rate ratios and adjusted absolute differences (for zero-truncated multivariable negative binomial regression), adjusted odds ratios (aOR) (for multivariable logistic regression), or adjusted coefficients (for multivariable linear regression) with 95% confidence intervals (CI). For mediation analysis, we tested whether the use of N2O was associated with the potential mediator variable and whether the potential mediator variable was associated with the primary outcome, indicating possible effect mediation. Conditional on both associations being significant, we used formal path mediation analysis to estimate incidence rate ratios of the indirect (mediated) effect of the potential mediator and the direct (unmediated) effect of N2O on length of stay in the PACU.23,24,25,26 For effect modification analyses, interaction terms were included separately into the primary regression model. Linear combinations of the respective main effect and interaction term were performed to assess the association between exposure and outcome across different subgroups. A two-tailed P value < 0.05 was considered statistically significant. Statistical analyses were performed using Stata (version 16, StataCorp LLC, College Station, TX, USA). Details of the statistical analyses are described in the ESM document.
Results
Study cohort and characteristics
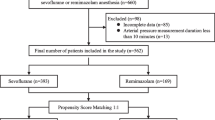
A total of 167,271 patients were considered for analysis. After exclusion of ineligible cases and cases with missing data, the final study cohort consisted of 148,284 patients (Fig. 1). Of these, 67,403 patients received no N2O, 40,441 patients received low N2O doses (average end-tidal N2O ≤ 13.15%), and 40,440 patients received high N2O doses (average end-tidal N2O > 13.15%). In the propensity-score matched cohort, 78,882 patients were included, of which 39,441 received high-dose N2O. Detailed characteristics of the study population are shown in Table 1.
Primary analysis
The median [interquartile range (IQR)] length of stay in the PACU was 176 [132–251] min in patients not receiving N2O, 181 [137–252] min in patients receiving low-dose N2O, and 158 [120–216] min in patients receiving high-dose N2O. After adjusting for a priori defined confounders, the use of both low- and high-dose N2O was associated with a significant decreased in PACU length of stay (Table 2). Compared with patients receiving no N2O, the adjusted absolute decrease of the PACU length of stay was −4.3 min (95% CI, −5.6 to −3.0; P < 0.001) in patients receiving low doses of N2O and −9.1 min (95% CI, −10.5 to −7.7; P < 0.001) in patients receiving high doses of N2O. Similar results were observed in the propensity-score matched cohort: high-dose N2O compared with no N2O significantly decreased PACU length of stay by -11.4 min (95% CI, −12.9 to −9.9; P < 0.001; Table 2).
Secondary analyses
Compared with patients who did not receive N2O, patients receiving high doses of N2O had a significantly decreased chance of experiencing short (1–15 min, median [IQR] 5 [3-8] min; aOR, 0.85; 95% CI, 0.83 to 0.88; P < 0.001) and prolonged (> 15 min, median [IQR] 25 [18-39] min; aOR, 0.76; 95% CI, 0.73 to 0.80; P < 0.001) duration of intraoperative hypotension. Patients who received low doses of N2O had a significantly decreased risk of prolonged intraoperative hypotension (aOR, 0.93; 95% CI, 0.89 to 0.97; P < 0.01) (Table 3).
Patients who received high-dose N2O had a significantly reduced total intraoperative administered dose of vasopressors, with an adjusted absolute difference of −0.04 mg norepinephrine equivalents (95% CI, −0.06 to −0.01; P = 0.01) compared to patients who did not receive N2O (Table 3).
Exploratory analyses
The use of N2O was significantly associated with a shorter duration of intraoperative hypotension (adjusted coefficient, −0.17; 95% CI, −0.2 to −0.13), which in turn was significantly associated with PACU length of stay (adjusted absolute difference: increase in PACU length of stay by 1.4 min per minute of intraoperative hypotension; 95% CI, 1.3 to 1.5; P < 0.001). Formal path mediation analysis revealed a partial mediation of the beneficial effect of N2O administration on PACU length of stay by decreasing the duration of intraoperative hypotension (5.9% indirect effect; P < 0.001) and a partial mediation of the harmful effect of N2O administration on PACU length of stay by increasing PONV (−40% indirect effect; P < 0.001) (ESM, eAppendix 3).
Of the patients in our cohort, 90.9% received intraoperative antiemetic therapy. Intraoperative antiemetic therapy was a significant effect modifier of the primary association (P for interaction < 0.001) for low and high doses of N2O. The beneficial effect of N2O on PACU length of stay was no longer observed in patients who did not receive intraoperative antiemetic therapy (P = 0.81).
The effect of high-dose N2O was more pronounced in patients undergoing complex surgeries (complex surgery: absolute adjusted difference, −26.1 min; 95% CI, −29.2 to −23.1; P < 0.001; non-complex surgery: absolute adjusted difference, −5.0 min; 95% CI, −7.0 to −3.0; P < 0.001; P for interaction < 0.001). This effect was more pronounced in patients undergoing complex surgery with prior intraoperative antiemetic therapy (absolute adjusted difference, −38.9 min; 95% CI, −43.1 to −34.6; P < 0.001) compared with patients undergoing complex surgery without prior intraoperative antiemetic therapy (absolute adjusted difference, −13.9 min; 95% CI, −28.5 to 0.8; P = 0.07) (P for interaction < 0.001). Figure 2 shows the results of the effect modification analyses. Additional exploratory analysis showed that high-dose intraoperative N2O was associated with a lower unplanned 30-day hospital re-admission after ambulatory procedures (aOR, 0.90; 95% CI, 0.82 to 0.98; P = 0.02).
Effect modification of the association between N2O and PACU length of stay by complex surgery and intraoperative antiemetic use. A. The beneficial association of high-dose N2O on PACU length of stay was more pronounced in complex surgery (defined as the combination of a high duration of surgery, high work RVUs, and inpatient setting) (absolute adjusted difference, −26.1 min; 95% CI, −29.2 to −23.1; P < 0.001) compared with non-complex surgery (absolute adjusted difference, −5.0 min; 95% CI, −7.0 to −3.0 min; P < 0.001). B. Intraoperative antiemetic drug therapy modified the association of N2O on PACU length of stay (P for interaction < 0.001). Without intraoperative antiemetic therapy, high-dose N2O did not decrease the PACU length of stay (P = 0.81). C. The beneficial association of N2O was most pronounced in complex surgery with intraoperative antiemetic therapy (adjusted absolute difference, −38.9 min; 95% CI, −43.1 to −34.6; P < 0.001) compared with complex surgery without intraoperative antiemetic therapy (adjusted absolute difference, −13.9 min; 95% CI, −28.5 to 0.8; P = 0.06). CI = confidence interval; N2O = nitrous oxide; PACU = postanesthesia care unit; RVU = relative value unit.
Sensitivity analyses
The association between high-dose N2O and PACU length of stay was modified by duration of surgery, work RVUs, and surgical setting as well as by the type of abdominal surgery (P for interaction < 0.001 for all) (ESM, eTable 2). Subgroup analyses revealed that the beneficial effect of high-dose N2O on PACU length of stay was magnified in surgeries with longer duration (adjusted absolute difference, −16.6 min vs −3.9 min), higher work RVUs (adjusted absolute difference, −18.8 min vs −5.1 min), inpatient surgeries (adjusted absolute difference, −12.7 min vs −4.7 min), and open abdominal surgeries (adjusted absolute difference, −24.1 min vs −2.9 min).
Discussion
In patients undergoing non-cardiothoracic surgery under general anesthesia, we found that N2O was dose-dependently associated with a decrease in PACU length of stay. This effect was magnified in surgeries with higher complexity, longer duration, higher procedural severity, and an inpatient setting. The effect was most pronounced when N2O was combined with intraoperative antiemetic therapy. Patients who received N2O had a lower risk of intraoperative hypotension, which in part mediated the beneficial association of N2O on PACU utilization.
Our data suggest that there are two competing effects of N2O that affect PACU length of stay: increased hemodynamic stability and increased PONV. Several large studies, including some randomized controlled trials, have studied the effects of N2O on hospital utilization and cardiopulmonary complications.27,28 The ENIGMA trial found no difference in hospital length of stay but found an increased risk of postoperative complications including wound infections, fever, pneumonia, atelectasis, and pulmonary complications as well as severe PONV in patients receiving N2O.27 The association of inhalational anesthesia using N2O with PONV was well-described and had led to the decline in the popularity of N2O in the last two decades.29,30,31,32,33 By contrast, a large retrospective study by Turan et al. studying the use of N2O showed a decreased risk of 30-day mortality, in-hospital mortality, and morbidity, as well as lower risks of respiratory complications in patients receiving N2O.28 The highest level of evidence was provided by the ENIGMA-II study, which supports the safety profile of N2O use in major non-cardiac surgery. The emetogenic effect of N2O can be controlled with antiemetic prophylaxis, and a desired effect of reduced volatile agent use was shown.29 In our study, the association of high-dose N2O on PACU length of stay was more pronounced in patients undergoing complex surgeries who received intraoperative antiemetic therapy (any type and any dose). We found that, without intraoperative antiemetic therapy, high-dose N2O did not decrease the PACU length of stay (P = 0.81), which is congruent with the findings of the ENIGMA-II trial that prophylactic intraoperative antiemetic therapy can eliminate the risk of N2O-associated PONV.29 Our study found that a low median dose of N2O is associated with reduced PACU length of stay. This might be explained by the pattern of utilization of N2O in our hospital. Many clinicians take advantage of the unique pharmacological profile of N2O by administering a high dose of N2O for only a brief period at the end of surgery to discontinue the volatile agent administration earlier, resulting in an overall low median dose over the entire case. A smoother emergence and decreased concentration of other anesthetics, which leads to faster recovery from anesthesia, has been reported in the presence of N2O and is due to the second-gas effect.12,13,34 This conclusion is supported by our data.
In our study, patients who received N2O had a lower risk of intraoperative hypotension and recieved lower intraoperative vasopressor doses. A lower incidence of intraoperative hypotension in part mediated the beneficial effect of N2O on PACU utilization. These findings can be explained by the fact that N2O exerts direct effects on the cardiovascular system, as it has been shown that it increases sympathetic outflow, maintains the baroreflex response to hypotension, and increases venous tone and venous return, maintaining hemodynamic stability.9,35,36,37 Nitrous oxide administration reduces the required amount of intraoperative volatile anesthetics, and therefore mitigates the afterload-reducing effects of these agents.13
Our data showed that the beneficial association of N2O on PACU length of stay was more prominent in subgroups of patients undergoing complex surgeries and less relevant in younger patients undergoing less-complex surgeries. The European Society of Anesthesiology task force on the use of N2O in clinical practice concluded, based on expert opinions, that, despite continuously decreasing use, there is no strong evidence for the withdrawal of N2O from anesthesia practice.38 Our data support the view that the supply of N2O in hospitals should be maintained and indicates that not only the emergence in the operating room but also the PACU recovery is shortened with N2O.39 Further research is needed to explore the mechanisms of a shortened PACU length of stay, accounting for earlier recovery of cognitive or motor function, and N2O-independent factors such as bed availability on the surgical ward.
Limitations
The retrospective design of our study raises several limitations. First, our PACU length of stay was long but similar to values observed in Harvard hospitals and other institutions in the United States.40,41,42,43 Second, although the large cohort permitted wide confounder adjustment, residual unmeasured confounding cannot completely be ruled out. In addition, the lack of availability of certain parameters from electronic medical records limited our analyses and prevented us from including potentially important confounders. Third, other potential mediators may have played a role in the mediation analysis that we did not identify in this study. Lastly, our data were limited to a single tertiary referral centre and so we may not be able to generalize our results. Nevertheless, our institution includes different service locations that perform a wide variety of procedures; therefore, we believe that our findings are relevant for a wide spectrum of patients.
Conclusion
The use of N2O as an adjunct to general anesthesia had a dose-dependent association with decreased PACU length of stay. This beneficial association was magnified in complex surgery and most pronounced in complex surgery with intraoperative antiemetic therapy.
References
Bruins SD, Leong PM, Ng SY. Retrospective review of critical incidents in the post-anaesthesia care unit at a major tertiary hospital. Singapore Med J 2017; 58: 497-501.
Waddle JP, Evers AS, Piccirillo JF. Postanesthesia care unit length of stay: quantifying and assessing dependent factors. Anesth Analg 1998; 87: 628-33.
Allen J. American Society of PeriAneshtesia Nurses. Perianeshtesia Nursing Standards, Practice Recommendations and Interpretive Statements 2015; pp. 32-7. Available from URL: http://www.aspan.org/portals/6/docs/clinicalpractice/pr1_2017_2018.pdf?ver=2017-02-09-145204-670 (accessed June 2021).
Lalani SB, Ali F, Kanji Z. Prolonged-stay patients in the PACU: a review of the literature. J Perianesthesia Nurs 2013; 28: 151-5.
Dexter F, Tinker JH. Analysis of strategies to decrease postanesthesia care unit costs. Anesthesiology 1995; 82: 94-101.
Seago JA, Weitz S, Walczak S. Factors influencing stay in the postanesthesia care unit: a prospective analysis. J Clin Anesth 1998; 10: 579-87.
Abeeleh MA, Tareef TM, Hani AB, et al. Reasons for operation cancellations at a teaching hospital: prioritizing areas of improvement. Ann Surg Treat Res 2017; 93: 65-9.
Erving HW. The discoverer of anæsthesia: Dr. Horace Wells of Hartford. Yale J Biol Med 1933; 5: 421-30.
Becker DE, Rosenberg M. Nitrous oxide and the inhalation anesthetics. Anesth Prog 2008; 55: 124-30.
Jain D, Ma HK, Buckley N. Impact of ENIGMA trials on nitrous oxide: a survey of Canadian anesthesiologists and residents. Can J Anesth 2018; 65: 730-1.
Emmanouil DE, Quock RM. Advances in understanding the actions of nitrous oxide. Anesth Prog 2007; 54: 9-18.
Peyton PJ, Stuart-Andrews C, Deo K, et al. Persisting concentrating and second gas effects on oxygenation during N2O anaesthesia. Anaesthesia 2006; 61: 322-9.
Peyton PJ, Chao I, Weinberg L, Robinson GJ, Thompson BR. Nitrous oxide diffusion and the second gas effect on emergence from anesthesia. Anesthesiology 2011; 114: 596-602.
Peyton PJ, Wu CY. Nitrous oxide-related postoperative nausea and vomiting depends on duration of exposure. Anesthesiology 2014; 120: 1137-45.
Wongtangman K, Wachtendorf LJ, Blank M, et al. Effect of intraoperative arterial hypotension on the risk of perioperative stroke after non-cardiac surgery: a retrospective multicenter cohort study. Anesth Analg 2021. DOI: https://doi.org/10.1213/ANE.0000000000005604
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987; 40: 373-83
Brueckmann B, Villa-Uribe JL, Bateman BT, et al. Development and validation of a score for prediction of postoperative respiratory complications. Anesthesiology 2013; 118: 1276-85.
Wynn BO, Burgette LF, Mulcahy AW, et al. Development of a Model for the Validation of Work Relative Value Units for the Medicare Physician Fee Schedule. Rand Heal Q 2015; 5: 5.
McLean DJ, Diaz-Gil D, Farhan HN, Ladha KS, Kurth T, Eikermann M. Dose-dependent association between intermediate-acting neuromuscular-blocking agents and postoperative respiratory complications. Anesthesiology 2015; 122: 1201-13.
Sasaki N, Meyer MJ, Malviya SA, et al. Effects of neostigmine reversal of nondepolarizing neuromuscular blocking agents on postoperative respiratory outcomes: a prospective study. Anesthesiology 2014; 121: 959-68.
Shin CH, Long DR, McLean D, et al. Effects of intraoperative fluid management on postoperative outcomes: a hospital registry study. Ann Surg 2018; 267: 1084-92.
Teja B, Raub D, Friedrich S, et al. Incidence, prediction, and causes of unplanned 30-day hospital admission after ambulatory procedures. Anesth Analg 2020; 131: 497-507.
Wongtangman K, Santer P, Wachtendorf LJ, et al. Association of sedation, coma, and in-hospital mortality in mechanically ventilated patients with coronavirus disease 2019-related acute respiratory distress syndrome: a retrospective cohort study. Crit Care Med 2021. DOI: https://doi.org/10.1097/CCM.0000000000005053
Althoff FC, Wachtendorf LJ, Rostin P, et al. Effects of night surgery on postoperative mortality and morbidity: a multicentre cohort study. BMJ Qual Saf 2020. DOI: https://doi.org/10.1136/bmjqs-2020-011684
Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: new procedures and recommendations. Psychol Methods 2002; 7: 422-45.
Grotta A, Bellocco R. A review of mediation analysis in Stata: principles, methods and applications 2013. Available from URL: https://www.stata.com/meeting/italy13/abstracts/materials/it13_grotta.pdf (accessed June 2021).
Myles PS, Leslie K, Chan MT, et al. Avoidance of nitrous oxide for patients undergoing major surgery: a randomized controlled trial. Anesthesiology 2007; 107: 221–31.
Turan A, Mascha EJ, You J, et al. The association between nitrous oxide and postoperative mortality and morbidity after noncardiac surgery. Anesth Analg 2013; 116: 1026-33.
Myles PS, Leslie K, Chan MT, et al. The safety of addition of nitrous oxide to general anaesthesia in at-risk patients having major non-cardiac surgery (ENIGMA-II): a randomised, single-blind trial. Lancet 2014; 384: 1446–54.
Apfel CC, Heidrich FM, Jukar-Rao S, et al. Evidence-based analysis of risk factors for postoperative nausea and vomiting. Br J Anaesth 2012: 109: 742-53.
Fernandez-Guisasola J, Gómez-Arnau JI, Cabrera Y, Del Valle SG. Association between nitrous oxide and the incidence of postoperative nausea and vomiting in adults: a systematic review and meta-analysis. Anaesthesia 2010; 65: 379-87.
Gan TJ, Diemunsch P, Habib AS, et al. Consensus guidelines for the management of postoperative nausea and vomiting. Anesth Analg 2014; 118: 85-113.
Leslie K, Myles PS, Chan MT, et al. Risk factors for severe postoperative nausea and vomiting in a randomized trial of nitrous oxide-based vs nitrous oxide-free anaesthesia. Br J Anaesth 2008; 101: 498-505.
Peyton PJ, Horriat M, Robinson GJ, Pierce R, Thompson BR. Magnitude of the second gas effect on arterial sevoflurane partial pressure. Anesthesiology 2008; 108: 381-7.
Ebert TJ. Differential effects of nitrous oxide on baroreflex control of heart rate and peripheral sympathetic nerve activity in humans. Anesthesiology 1990; 72: 16-22.
Neukirchen M, Kienbaum P. Sympathetic nervous system: evaluation and importance for clinical general anesthesia. Anesthesiology 2008; 109: 1113-31.
Ko H, Kaye AD, Urman RD. Nitrous oxide and perioperative outcomes. J Anesth 2014; 28: 420-8.
European Society of Anaesthesiology Task Force on Use of Nitrous Oxide in Clinical Anaesthetic Practice; Buhre W, Cerny V, De Hert S, et al. The current place of nitrous oxide in clinical practice: an expert opinion-based task force consensus statement of the European Society of Anaesthesiology. Eur J Anaesthesiol 2015; 32: 517-20.
Buhre W, Disma N, Hendrickx J, et al. European Society of Anaesthesiology Task Force on Nitrous Oxide: a narrative review of its role in clinical practice. Br J Anaesth 2019; 122: 587-604.
Butterly A, Bittner EA, George E, Sandberg WS, Eikermann M, Schmidt U. Postoperative residual curarization from intermediate-acting neuromuscular blocking agents delays recovery room discharge. Br J Anaesth 2010; 105: 304-9.
Ma H, Wachtendorf LJ, Santer P, et al. The effect of intraoperative dexmedetomidine administration on length of stay in the post-anesthesia care unit in ambulatory surgery: a hospital registry study. J Clin Anesth 2021. DOI. https://doi.org/10.1016/j.jclinane.2021.110284
Polshin V, Petro J, Wachtendorf LJ, et al. Effect of peripheral nerve blocks on postanesthesia care unit length of stay in patients undergoing ambulatory surgery: a retrospective cohort study. Reg Anesth Pain Med 2021; 46: 233-9.
Levy N, Santer P, Zucco L, Nabel S, Korsunsky G, Ramachandran SK. Evaluation of early postoperative intravenous opioid rescue as a novel quality measure in patients who receive thoracic epidural analgesia: a retrospective cohort analysis and prospective performance improvement intervention. BMC Anesthesiol 2021. DOI: https://doi.org/10.1186/s12871-021-01332-7
Author contributions
Salameh Sameh Obeidat, Karuna Wongtangman, and Michael Blank contributed equally to this manuscript. Salameh Sameh Obeidat helped conceptualize the paper, performed the literature review, wrote the initial draft of manuscript, and read and approved the final manuscript. Karuna Wongtangman helped conceptualize the paper, analyzed data, wrote the initial draft of manuscript, and read and approved the final manuscript. Michael Blank helped analyze the data, reviewed the manuscript, edited and modified drafts, and read and approved the final manuscript. Luca J. Wachtendorf and Maximilian Hammer helped analyze the data, reviewed the manuscript, edited and modified drafts, and read and approved the final manuscript. Maximilian S. Schaefer and Peter Santer gave suggestions on data analysis, helped interpret the data, reviewed the manuscript, edited and modified drafts, and read and approved the final manuscript. Matthias Eikermann, helped conceptualize the paper, gave suggestions on data analysis, reviewed the manuscript, edited and modified drafts, and read and approved the final manuscript. He is the guarantor of the study and takes responsibility for all parts from conceptualization to publication. Eswar Sundar helped conceptualize the paper, reviewed the manuscript, edited and modified drafts, and read and approved the final manuscript.
Disclosures
Matthias Eikermann has received research support from Merck not related to this manuscript.
Funding statement
This study was supported by Jeffrey and Judith Buzen in an unrestricted grant to Matthias Eikermann.
Editorial responsibility
This submission was handled by Dr. Philip M. Jones, Deputy Editor-in-Chief, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is accompanied by an editorial. Please see Can J Anesth 2021; this issue.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Obeidat, S.S., Wongtangman, K., Blank, M. et al. The association of nitrous oxide on length of stay in the postanesthesia care unit: a retrospective observational study. Can J Anesth/J Can Anesth 68, 1630–1640 (2021). https://doi.org/10.1007/s12630-021-02067-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-021-02067-2