Abstract
Purpose of Review
In cystic fibrosis (CF), the main focus in bronchopulmonary infections is on bacterial pathogens, as they significantly influence lung function and the exacerbation rate. In the last decade, fungal respiratory diseases have been increasingly investigated for their impact on the clinical course of people with CF. This review aims to highlight recent findings in diagnostics and therapeutic approaches in terms of fungal infections in CF.
Recent Findings
We reviewed over 100 publications on fungal species in CF. Studies showed that Aspergillus spp. negatively impact lung function in patients with CF. A summary of these investigations showed that fungal diseases in patients with CF present as colonization, sensitization, bronchitis, pneumonia, allergic bronchopulmonary aspergillosis, and aspergilloma. Two significant fungal infections, pneumonia and bronchitis, are now well-defined, and several studies have established treatment options. The following pathogens are considered the primary cause of bronchitis, i.e., Aspergillus spp. and Exophiala spp., and of pneumonia, i.e., Scdedosporium spp., Apergillus spp., Trichosporon spp., and Candida spp. The main therapeutic innovations highlighted were real-time PCR techniques, DNA chips, and antigen-reactive T cell enrichment assay (ARTE).
Summary
Respiratory fungal infections in CF are a complex task in terms of definition and therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A new era for people with cystic fibrosis (pwCF) has started with the approval and use of highly effective CFTR modulator therapy. In clinically stabalized patients with increasing pulmonary function and an significantly reduced exacerbation rate, the role of bronchopulmonary exacerbations or infections needs to be discussed in a new setting, in particular with regard to fungal infections. In this context, the current challenges in diagnosis and therapy are to be adressed [1,2,3]. In fact, diagnosis of invasive fungal infections (IFI) is often delayed, resulting in inadequate treatment. Fortunately, several studies have been conducted regarding fungal colonization and infection of the airways in pwCF to bring light into a complex topic.
It is known that Aspergillus fumigatus (Af) for filamentous fungi and Candida albicans for yeasts remain by far the most common fungal species in pwCF, but the pattern of fungal species associated with CF has considerably diversified recently [4,5,6,7,8,9,10,11,12,13]. Thus, besides Af, some Scedosporium species (Scedosporium boydii, Scedosporium apiospermum, Scedosporium aurantiacum, Scedosporium minutisporium) and the closely related species Lomentospora prolificans have worldwide been recognized as significant fungal pathogens in CF, potentially causing severe fungal infetions that might be in many cases difficult to treat [11, 14,15,16]. In addition, very rare fungal species such as Exophiala dermatitidis, Arxula adeninivorans, and Trichosporon mycotoxinivorans have also been described causing severe fungal pneumonia in pwCF [17,18,19,20,21,22].
In addition to fungal infections, pwCF commonly experience allergic bronchopulmonary aspergillosis (ABPA) and bronchitis [23,24,25,26,27]. The diagnosis and treatment of Af-related conditions remains a challenge in CF due to overlapping features with other disease and absence of clinical guidelines for these conditions outside of ABPA. The impact of Aspergillus spp. is of high importance and was evidenced in a study from Germany where presentation with a significantly lower forced expiratory volume in 1 s (FEV1) in pwCF was associated with detection of Aspergillus spp. in respiratory samples. In particular, patients without chronic Pseudomonas aeruginosa (Pa) infection had a significantly lower FEV1 in association with one or at least two positive Aspergillus spp. Cultures per year (P < 0.0001). Pulmonary exacerbations requiring antibiotic treatment were experienced by significantly more pwCF with at least two positive Af cultures (53.9% vs. 39.5% with no Aspergillus spp. diagnosis in 2016 and 73.9% vs. 59.2% in 2017; p < 0.0001, respectively) [5]. In addition, a current study from the USA has shown that in people with CF, TH2 inflammation based on serum absolute eosinophil counts and IgE correlated with pulmonary exacerbations requiring hospitalizations and/or intravenous antibiotics, independent of bacterial airway colonization. Furthermore, lung function decline correlated with increased IgE and serum absolute eosinophil counts [28].
Although many patients receive CFTR modulator therapy, the European Cystic Fibrosis Society (ECFS) registry data from 2018, 2019, and 2020 show no recent significant differences in proportion of pwCF with ABPA diagnosis, with 4.75% reported in 2018, 5.12% in 2019, and 4.55% in 2020, respectively [29]. Despite the increasing number of studies adressing fungal pulmonary diseases in CF, there is still a great heterogeneity in the availability of diagnostic tools and diagnostic and therapeutic guidelines [30]. In this review, the definition of fungal infection will be described as well as the diagnostic and therapeutic approaches and challenges.
In this review, both the definition of fungal infections and the diagnostic and therapeutic approaches and challenges will be described.
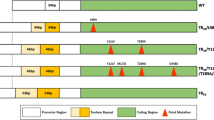
In general in CF, different entities or categories of fungal pulmonary diseases have been discovered [15, 17, 24, 26, 27, 31,32,33,34,35]. In addition to fungal airway colonization, host responses can be divided into two different groups: the allergic and the infectious groups. The allergic group comprises with sensitization, ABPA, or allergic bronchopulmonary mycosis (ABPM). The infectious group includes fungal pulmonary infection, fungal bronchitis, and aspergilloma [7, 8, 15, 26, 27, 31, 36,37,38,39] (Fig. 1).
Fungi can cause different disease entities in people with CF. One direction are allergic entities with fungus sensitization and allergic bronchopulmonary aslergillosis (or allergic bronchopulmonary mycosis caused by fungi other than Aspergillus). The second direction of fungal entity is infection with fungal bronchitis, aspergilloma, and fungal pneumonia. Between these two directions are people with CF who are not colonized with fungi and others who are only colonized with fungi
The Challenge to Detect Fungal Species in Cystic Fibrosis
Culture-Based Methods
Until now, the most common and widely available detection method for fungal species in pwCF is the use of culture-based techniques [30]. In the past, it has already been pointed out that the comparison of data from one study to another might be hampered by the lack of standardization of mycological examination of respiratory secretions [40, 41]. For instance, some laboratories might inoculate the respiratory samples on agar slants which offer a more limited surface for fungal growth compared to agar plates. Some slow-growing or low-prevalent fungal species may therefore be missed in case of mixed fungal populations, which are common in the CF airways. Likewise, great variations may be seen from one laboratory to another in the volume and processing of the sample being analyzed, as well as in the number of culture media inoculated and in incubation time and temperature [40]. Moreover, the microbiological follow-up of CF patients is usually limited to an exhaustive bacteriological analysis of respiratory secretions, and for mycological analysis, samples are inoculated only on Sabouraud dextrose agar supplemented with antibiotics (SDA) [30, 42, 43]. The frequency of indications for excluding or diagnosing fungal species varies between countries [30]. As these differences exist, it is impossible to establish consensus definitions of chronic colonization of the airways with fungal species. Only if respiratory samples are analyzed in a regular and standardized manner to detect bacteria and fungi at the same time can chronic colonizations could be defined. In addition to the lack of standarization, differences in the population studied, in environmental exposure and in lifestyle of the patients, possibly account for part of the differences that can be seen in the prevalence of filamentous fungi from one study to another [44,45,46].
Nevertheless, limitations in the biological diagnosis need to be considered as attested by the recent publication from Reece et al. [47] or the comparison of current practices in clinical laboratories in the UK [48]. This was perfectly illustrated by Hong et al. [43] in Baltimore (MA, USA). During 1 year, consecutive sputa (n = 487) collected from outpatients were inoculated in parallel on bacteriological agar plates, which were incubated for 3 days at 37 °C, or on SDA, brain–heart infusion (BHI) agar plates supplemented with antibiotics and inhibitory mold agar (IMA) plates which were incubated for 2 weeks at 30 °C. Only 48 of the samples (9.8%) revealed to be positive for fungi using bacteriological media, whereas they were about 120 (from 23.8 to 24.8%) on each of the three mycological media incubated at 30 °C. Interestingly, 32% of the samples revealed the presence of fungi when combining the results obtained on SDA, BHI agar, and IMA and the prevalences of Aspergillus and Scedosporium/Lomentospora species were found to be twofold to threefold higher than their reported prevalences in the USA (40.8% vs. 20.4% and 5.2% vs. 1.9%, respectively). Likewise, only 3 out of the 20 Scedosporium/Lomentospora and 1 out of the 17 Trichosporon positive samples were detected using bacteriological media, and none of the Exophiala was a positive sample. Of note, samples were not digested with a mucolyticum nor sonicated or diluted before inoculation of the plates and no Scedosporium-selective culture media were used [43]. Similar results have been reported previously in Germany [49, 50].
Regarding the detection procedures, many countries currently have their own recommendations on detection of fungal species in respiratory samples in pwCF, which vary greatly between them [6]. Nevertheless, this needs to be updated to allow a correct overview of the fungal biota colonizing the CF lungs and airways. In addition, consensus is needed for the frequencies of testing as, for example, fungal surveillance is not routinely performed in most clinical centers in the USA [30]. Therefore, to address these challenges in detecting fungi, improved and consented guidelines for mycological examination of sputum samples from CF patients are urgently needed [51]. With this aim, two multicenter studies were conducted recently within the Fri-CF (fungal respiratory infections in cystic fibrosis) working group launched by both the European Confederation of Medical Mycology (ECMM) and the International Society for Human and Animal Mycology (ISHAM). The studies encompassed 7 CF-care centers from France for the MucoFong project [52] and 19 laboratories (9 from France and 4 from Italy, as well as laboratories from Spain, the UK, Belgium, Austria, Greece and Australia, one each) for the MFIP project [53]. In this study, the same procedure was used for the mycological examination of samples, including inoculation on a wide range of culture media and incubation of agar plates at two different temperatures. From the analysis of the obtained data, a combination of three to four culture media was proposed [52, 53]. In a Dutch study, the inclusion of prior digestion of the sample with a mucolyticum, increased inoculum size, additional culture media (SDA, B + medium, Sce-Sel + and dichloran-glycerol agar), and longer incubation time (3 weeks) was tested [54], noting a marked increase in both the frequency and the diversity of molds. Nevertheless, some semi-selective culture media were not evaluated in these studies, such as dichloranrose bengal-chloramphenicol agar, the aforementioned inhibitory mold agar, or the Scedo-Select III and SceSel + culture [4, 43, 49, 55,56,57]. To enhance the recovery of Exophiala dermatitidis from sputum samples, Burkholderia cepacia-selective agar can also be used [58].
In fact, all growing fungi should be identified, which is not the case presently, for example, because of a lack of consideration of some fungi as potential pathogens, misidentifications using conventional methods, or limits of commercially available databases for MALDI-TOF mass spectrometry. For example, in a questionnaire survey of current practices in UK CF centers, only 7 out of the 11 respondents performed species identification for Exophiala species and only 2 for non-Candida yeasts [59]. Likewise, some molds colonizing the CF airways may be misidentified on the basis of the sole macroscopic and microscopic morphology or when using only commercially available databases for MALDI-TOF mass spectrometry. This is particularly true for Rasamsonia species which are frequently misidentified as Penicillium or Paecilomyces species [60,61,62]. Further multicenter studies comparing these innovative and new culture media with those previously selected [52, 53] and using gold-standard procedures for species identification should be conducted in order to provide evidence-based guidelines in CF.
Culture-Independent Methods
In addition to culture-based methods, molecular approaches are currently being developed based on real-time PCR techniques, or on DNA chips. One limitation of these possible new approaches will be the differenciation between infection, colonization, and transient carriage of recently inhaled fungal spores [12, 51, 63, 64]. If necessary, next-generation sequencing technique for secondary identification of the isolated fungi may be used in reference laboratories [65]. Genotyping of fungal isolates can be applied to describe transmission patterns between patients or to identify an environmental source of contamination at home of the patients, as well as to differenciate between a transient carriage of always distinct genotypes unable to establish in the respiratory tract and a true chronic colonization with the same genotype recovered by culture from successive samples.
In addition, serological tests (for detection of specific IgG antibodies) may be useful, for culture-positive patients, to differenciate an airway colonization from a respiratory infection [24, 26, 66,67,68]. Unfortunately, serological methods for CF-related fungi apart from Aspergillus and Candida are not commercially available.
The Growing Problem of Resistance to Antifungals
Once fungal species are detected, in vitro antifungal susceptibility testing of mold isolates is mandatory because of primary resistance of some fungal species and increasing occurrence of acquired resistance in other species. However, it is not known wether the results can be transferred from in vitro to in vivo, and there might be discrepancies, in particular in triazoles.
Analysis of transcriptomic changes induced in S. apiospermum in response to the particular physicochemical environment encountered by the fungus in the CF airways revealed reprogramming of genes involved in the synthesis of some important cell wall or membrane components, including genes encoding not only the glycosylphosphatidylinositol anchor and sphingolipids, but also ergosterol, with the downregulation of five of the genes involved in ergosterol biosynthesis pathway [69]. These metabolic changes could explain the discrepancies aforementioned regarding triazole drugs, since environmental conditions in CF lungs may lead to a drastic reduction in the ergosterol content of the plasma membrane, maintaining fungal growth despite the inhibition of the azole target, the 14 alpha-demethylase encoded by the gene Cyp51A. In agreement with these data, Mello et al. [70, 71] reported that cultivation of some Scedosporium species under 5% carbon dioxide in a medium mimicking the biochemical composition and viscosity of the CF bronchial mucus resulted in increased resistance to triazole drugs compared to reference growth conditions. In addition, this reseach group could show the influence of biofilm on resistance in Scedosporium species [71].
As azoles are used intensively to treat invasive and chronic aspergillosis, the likelihood for selection of resistant isolates is high. Analysis of isolates collected from respiratory samples of CF patients revealed resistance rates in cyp51A ranging from 5.3 to 13.2%. For example, a resistance rate of up to 8.2% was found for Af isolates collected from pwCF in Italy [72]. In the same line, in Germany, 2888 Af isolates from 961 CF patients were screened prospectively and 101 isolates from 51 of these patients (5.3% of the patients) were found to be azole resistant [73]. Likewise, in the UK, 167 Af isolates collected from 135 pwCF were investigated; resistance to at least one azole drug was confirmed in 22 out of these isolates (13.2%) [74]. Finally, during a 1-year period, similar results were reported in France and in the Netherlands. All Af isolates collected from pwCF in a French reference CF center were investigated prospectively; 23 out of the 355 isolates studied (6.5%) were found to be resistant to at least one triazole drug, leading to a prevalence of 6.8% (6/88 patients) [75]. In the Netherlands, azole-resistant Af isolates were cultured from 7.3% (10/137) of the CF patients [76]. In patients with CF, azole-resistant A. fumigatus strains may be selected during the course of azole therapy, but they also from azolenaïve pwCF, in relation with the extensive use of triazole fungicides in agriculture. The acquired resistance to azole drugs in the course of azole therapy is usually due to point mutations in the cyp51A gene sequence, but analysis of resistant isolates from environmental origin might reveal other mutations such as TR46/Y121F/T289A [73, 75, 77].
The Challenge to Define and Treat Fungal Pneumonia
As bronchopulmonary infections or exacerbations in CF are usually caused by bacteria, no commonly agreed upon definition for pulmonary infections existed in the past. However, in recent years, a definition has been developed and established for fungal pulmonary infection and published by international experts in the field [11, 37, 78, 79]. This definition is as follows:
-
1.
Increased sputum production
-
2.
Multiple isolation of the same fungal species from sputum or bronchoalveolar lavage (≥ twice over a 6-month period)
-
3.
Pulmonary infiltrate(s) on chest computertomography- or magnet resonace imaging or chest X-ray
-
4.
Treatment failure by antibiotic therapy (≥ 2 × antibiotic treatment, duration ≥ 2 weeks)
-
5.
Unclear cause for lung function decline (exclusion of newly diagnosed CF-related diseases, e.g., CF-related diabetes mellitus)
-
6.
Exclusion of new/other bacteria (e.g., non-tuberculous mycobacteria or Pa)
-
7.
Exclusion of ABPA/ABPM
Diagnosis of Fungal Pneumonia
Although this definition probably helps to identify patients with fungal pneumonia, it can still be challenging to confirm the diagnosis. CT or MRI imaging might be a very helpful tool in diagnosing fungal pneumonia. Typical findings for this specific diagnosis — as shown and described in two previous publications [15, 17] — may be ground glass density surrounding a nodule, also known as “halo sign,” or consolidations with internal ground glass density. But other findings like semi-solid and ground glass nodules and, in particular, peripheral well-circumscribed nodules might also be specific hints for severe non-specific pulmonary infections in CF [80, 81]. The definitive diagnosis of IFI is by microbiology or histopathology. However, as many CF patients receive highly effective CFTR modulator therapy, less sputum is produced which makes appropriate collection of sputum samples for analysis difficult, while bronchoalveolar lavage or induced sputum is not feasible in a routine setting. For this reason, new methods to detect microbiological colonization or infections with bacteria or fungi are needed.
A novel diagnostic tool has been proposed in recent years relying on the measurement of fungus-specific host response. This antigen-reactive T cell enrichment assay (ARTE) might be useful to measure fungus-specific T cell responses during the onset of fungal infections [38, 39, 82, 83]. This method reflects the direct host–pathogen reaction, therefore identifying the relevant pathogen in usually co-colonized pwCF could be possible despite negative culture-based detection methods or PCR-based methods from low quality samples.In addition, an easier and less time-consuming diagnostic tool is the above mentioned fungus-specific IgG. In a recent publication, it could be shown that Af-specific IgG might be helpful in the diagnosis and treatment follow-up of Af entities as Af-specific IgG decreases after therapy [24].
Serological techniques such as galactomannan in blood bronchoalveolar lavage or other Aspergillus antigens measured by lateral flow devices have also helped to achieve aspergillosis diagnosis within hours with a specificity and sensitivity of more than 80%, in particular in severe, life-threatening cases [84,85,86]. Although not commercially available, some serological methods have recently also been prposed for Scedosporium/Lomentospora. Two of them based on ELISA system using a total extract or recombinant proteins as antigen [67, 87]. An additional, newly developed assay based on a rapid dot immobinding assay (DIA), which allows the detection of serum IgG against a total extract of these fungi in less than 15 min with a sensitivity and specifity of 90.48% and 79.30%, respectively [123].
Af or non-Aspergillus species pneumonia is a new disease entity in pwCF which is not easy to diagnose as bacteria are the main reason for infections with similar symptoms [88, 89], and it therefore needs the attention of radiologists and clinicians. Usually, the gold standard would be transbronchial biopsy of the region with infiltrate to verfy fungal growth via direct detection [90]. In CF, this intervention is usally too dangerous as pneumothorax might cause severe clinical detoriation [91].
Tratment of Fungal Pneumonia
The treatment of these infections might cause some challenges in this patient population. Infections with Af is usually treated with monotherapy using voriconazole, posaconazole, isavuconazole, caspofungin, micafungin, or lipidic amphotericin B [15, 92]. Susceptibility testing is considered important if clinical response is lacking, particularly as azole resistance has recently been reported [72, 76]. However, treatment of fungal pulmonary infections in CF remains challenging when they are caused by multi-resistant fungi such as Scedosporium species and L. prolificans or the emerging Rasamsonia species. These fungi exhibit a primary resistance or low susceptibility to most available antifungal drugs [9, 60, 93]. In recent years, a lot of efforts have been made performing studies to address this issue. First of all, for all antifungal treatments, susceptibility testing is mandatory as resistance can occur [9, 11, 94]. Single studies on Scedosporium/Lomentospora infections recommend the option of combined anti-fungal therapy. A combination of two or even three different antifungals might be necessary and is therefore recommended for the initial treatment phase [11, 15, 16, 79, 95]. Ideally, it should combine an oral azole (voriconazole, posaconazole, isavuconazole), an intravenous echinocandin (e.g. caspofungin or micafungin), and inhaled lipidic amphotericin B. In Rasamsonia infections, micafungin would be preferred in combination, and in infections with L prolificans, terbinafine might be susceptible as well as miltefosine, in combination with an echinocandin and azole [11, 15, 78, 96]. In the case of E. dermatitidis, antifungal therapy recommendations are mainly focused on therapy with amphotericin B, flucytosine, or azoles [19, 20, 37], but susceptibility testing should also be performed initially as different resistance might occur [18, 19, 97,98,99,100]. In the rare cases caused by T. mycotoxinivorans, recommended treatment regimes are a combination of amphotericin B (intravenous or inhaled) and an azole as with monotherapy; however, breakthrough infections might occur [21, 101,102,103,104]. As recommended for other fungi, it is also crucial to performe susceptibility testing as resistance might occur and cause treatment failure [21, 22, 101, 102, 105].
Candida spp. are the most common yeast isolated in respiratory samples in pwCF, being isolated in a study period of 6 years in microbiology institutes from 9 CF centers in Europe with a range (in mean) of 33.8% up to 77.9% [6]. However, infections caused by this fungus are only rarely described [6, 15]. In fact, the pathogenicity of Candida spp. in CF and their influence on disease progression is less clearly understood than with filamentous fungi and continues to be debated. In the late 1990s, registry data from 7010 pwCF showed the association of Candida spp. and lower FEV1(91), although it is unknown whether his was due to a direct effect of Candida spp.; an observation for its predilection for damaged pulmonary parenchyma or a finding associated with antibiotic treatment used more often in those with greater disease severity is unknown. More recently, the potential of Candida spp. to cause lung function decline, implicating a significant impact in CF, was also demonstrated as well as that the yeast can cause both localized and systemic infections and induce oral and genital thrush, vascular access device-related infections, and post-transplantation complications (108; 109). However, whether treatment against Candida spp. influences the course of disease or the drop in lung function remains unknown and needs further investigation. In the very rare cases of highly probable pulmonary infection due to Candida spp., the accurate identification of the infecting Candida species is crucial in determining which antifungal agent to use, because of the occurrence of fluconazole-resistant Candida species [92]. In C. albicans infections, it is recommended to start with an azole, preferably fluconazole, and to modify treatment if needed according to susceptibility tests. Echinocandins (e.g., caspofungin, anidulafungin, micafungin) are effective drugs for Candida glabrata and Candida tropicalis infections. Amphotericin B is also useful for Candida spp. infections but has the disadvantage of nephrotoxicity, hypokalemia and acute infusion-related side effects [13]. However, Candida spp. are still rarely identified as causing acute pulmonary infection in CF requiring treatment, and further research is needed to determine their true position as pathogenic organisms in CF.
Clinicians have to be aware that all detected fungal species in respiratory samples of pwCF should be considered as potentially pathogenic. The first in-human detection of A. adeninivorans in a pwCF causing a life-threatening invasive pulmonary infection underlines this hypothesis [17].
An additional important question for clinicians is whether colonization without clinical implications should be treated to prevent clinical deterioration and chronic lung damage, in particular if multi-resistant fungi such as L. prolificans are detected, which could be a potential contraindication for lung transplantation. IFI pose a serious threat in CF. Nevertheless, it has been shown that it is complicated to diagnose them and that early initiation of appropriate antifungal therapy is vital for a good outcome [16, 37, 48, 108,109,110,111,112].
The Challenge to Diagnose and Treat Af Bronchitis
Besides ABPA, other diseases, such as aspergilloma, invasive pulmonary aspergillosis, hypersensitivity diseases, and Af bronchitis, may occur [25, 26, 31, 113, 114]. Af bronchitis was first described in 2006 [31]. The main problem in a clinical setting is to distinguish between harmless colonization and clinically relevant bronchitis.
Aspergillus spp. or non-Aspergillus spp. bronchitis is defined as by Aspergillus-positive sputum cultures, respiratory exacerbations unresponsive to antibiotic treatment and successful antifungal treatment, as well as exclusion of ABPA [31]. Further specifications and a modified definition of Aspergillus bronchitis were published in 2013 already by Baxter et al. [26] including a cutoff index of > 0.5 for sputum galactomannan, positive Af-specific PCR, and elevated levels for specific serum IgG antibodies (75 mg/l), in combination with not elevated total serum IgE (whereas a total serum IgE level > 500 IU/ml indicates ABPA) [115] and specific serum IgE [26]. Thus, repeatedly detected Aspergillus spp. in sputum samples without hypersensitivity to Aspergillus spp. and with persistent respiratory symptoms are features of Aspergillus bronchitis in patients with CF [113].
In a recent study, Aspergillus-specific IgGm3 was evaluated in pwCF with ABPA, bronchitis and pneumonia. The results showed that Aspergillus-specific IgGm3 is a good individual biomarker to follow up the patient during and after treatment in order to access treatment response [24]. Once the diagnosis is confirmed, treatment should be started with an azole but susceptibility testing is always recommended [72, 76, 116, 117]. As there are no prospective studies on Aspergillus spp. bronchitis, the duration of treatment is unclear. In a German single center study, the duration of antifungal treatment was 4 ± 1.6 weeks with a range between 2 and 6 weeks. But the treatment in this small study significantly reduced cough (P = 0.0067), sputum production (P < 0.0001) and lung function measures (P = 0.0358) but did not increase physical capacity (P = 0.0794) [27]. In some cases, it might be indicated to continue the treatment longer, and it is not yet known which biomarker might be the most suitable to decide the duration of antifungal treatment, but as mentioned above, the Af-IgG would be a fast and low-cost marker [24].
General Challenges in the Antifungal Treatment of pwCF
CF presents some aspects different from other diseases that make it essential to adjust doses of azoles and to monitor levels in those drugs with a low volume of distribution. These following factors result in a need for potentially higher dosing and highlight the importance of therapeutic drug monitoring delayed absorption of oral antifungal drugs due to pancreatic insufficiency and fat malabsorption, increased total body volume leading to higher volume distribution with low drug concentrations, and enhanced hepatic and renal drug clearance due to hypermetabolic state [118, 119]. In addition, pwCF have usually many co-medications, particularly drugs with severe interactions [120]. Drug–drug interactions with CFTR modulators are typical, and in patients with elaxaftor, tezacaftor, and ivacaftor, the modulator therapy needs to be adjusted to a lower dosage [1, 121, 122].
Mycobiome
To understand more about fungal species in the airways, analysis of the mycobiome becomes important. With new methods such as qPCR and rRNA analyses, it is now feasible to gain data in terms of the total fungal load in particular of the lower airways.
Two metrics, α-diversity and β-diversity, are used to simplify the high-dimension data associated with microbiome analysis into a single metric. Alpha diversity describes the ecological diversity within a certain niche using the Shannon diversity index. This index includes many parameters such as the number of taxa (richness) and the distribution (evenness and dominance) of each taxon. Beta diversity is a measure of the degree of difference in membership or structure between two or more microbiota with many equations and indices existing to measure β-diversity [123, 124]. In a current study from the USA, in the bronchoalveolar lavage of people with CF, differences were observed in the abundance of Aspergillus and Candida in people with CF [125]. More studies are needed to understand the mycobiome in people with CF, in particular in terms of treatment with highly effective modulator therapy. Those studies usually focus only on bacteria such as Pseudomonas aeruginosa or Staphylococcus aureus.
Conclusion
In summary, fungal pulmonary infections are a complex task in terms of definition and therapy. But the efforts of world-wide collaborations (e.g., ECFS Fungal Pathogens Working Group and ISHAM/ECCMID Fungal Respiratory Infections in CF Group) in the last years have led to (i) new diagnostic approaches for detecting the causative fungal pathogen, (ii) new definitions of fungal pneumonia, (iii) definition for fungal bronchitis, and (iv) new recommendations for antifungal treatments. Using these established definitions for different categories of fungal diseases is now strongly recommended and should be taken into account if patients are deterioriating without responding to antibiotic treatment. Furthermore, there is a need for better data to determine predictive risk factors, causality, and biomarkers that enable monitoring and response to treatment. In addition, there is a need for more prospective and interventional studies in this area in CF.
Finally, clinicians should appreciate the findings of fungal species and should keep in mind that these fungi might cause a significant infection in pwCF that needs to be treated in an appropriate way. In response to rising concerns about antifungal restistances, very potent drugs with fosmanogepix, ibrexafungerp, olorofim, opelconazole, and rezafungin [126] are in the pipeline. A promising drug in CF seems to be olorofim, an orotamide, which in the future will play a central role in the treatment of multi-resistant mold infections, including azole-resistant aspergillosis, L. prolificans, and endemic mycoses.
References
King JA, Nichols AL, Bentley S, Carr SB, Davies JC. An update on CFTR modulators as new therapies for cystic fibrosis. Pediatr Drugs. 2022;24(4):321–33. https://doi.org/10.1007/s40272-022-00509-y. [cited 2022 Nov 5].
Middleton PG, Mall MA, Dřevínek P, Lands LC, McKone EF, Polineni D, et al. VX17-445-102 Study Group. Elexacaftor-Tezacaftor-Ivacaftor for cystic fibrosis with a single Phe508del Allele. N Engl J Med. 2019;381(19):1809–19. https://doi.org/10.1056/NEJMoa1908639.
Ridley K, Condren M. Elexacaftor-Tezacaftor-Ivacaftor: the first triple-combination cystic fibrosis transmembrane conductance regulator modulating therapy. J Pediatr Pharmacol Ther. 2020;25(3):192–7. https://doi.org/10.5863/1551-6776-25.3.192.
Pihet M, Carrere J, Cimon B, Chabasse D, Delhaes L, Symoens F, et al. Occurrence and relevance of filamentous fungi in respiratory secretions of patients with cystic fibrosis--a review. Med Mycol. 2009;47(4):387–97. https://doi.org/10.1080/13693780802609604.
Düesberg U, Wosniok J, Naehrlich L, Eschenhagen P, Schwarz C. Risk factors for respiratory Aspergillus fumigatus in German Cystic Fibrosis patients and impact on lung function. Sci Rep. 2020;10(1):18999. https://doi.org/10.1038/s41598-020-75886-w.
Schwarz C, Bouchara J-P, Buzina W, Chrenkova V, Dmeńska H, de la Pedrosa EGG, et al. Organization of patient management and fungal epidemiology in cystic fibrosis. Mycopathologia [Internet]. 2018;183(1):7–19. https://doi.org/10.1007/s11046-017-0205-x.
Singh A, Ralhan A, Schwarz C, Hartl D, Hector A. Fungal pathogens in CF airways: leave or treat? Mycopathologia [Internet]. 2018;183(1):119–37. https://doi.org/10.1007/s11046-017-0184-y.
Bouchara J-P, Symoens F, Schwarz C, Chaturvedi V. Fungal respiratory infections in cystic fibrosis (CF): recent progress and future research agenda. Mycopathologia [Internet]. 2018;183(1):1–5. https://doi.org/10.1007/s11046-017-0241-6.
Schwarz C, Vandeputte P, Rougeron A, Giraud S, Dugé De Bernonville T, Duvaux L, et al. Developing collaborative works for faster progress on fungal respiratory infections in cystic fibrosis. Med Mycol. 2018;56(suppl_1):S42-59. https://academic.oup.com/mmy/article/56/suppl_1/S42/4925969.
Chotirmall SH, McElvaney NG. Fungi in the cystic fibrosis lung: bystanders or pathogens? Int J Biochem Cell Biol [Internet]. 2014;52:161–73.
Ramirez-Garcia A, Pellon A, Rementeria A, Buldain I, Barreto-Bergter E, Rollin-Pinheiro R, et al. Scedosporium and Lomentospora: an updated overview of underrated opportunists. Medical Mycology. 2018;56:S102-25.
Bouchara J-P, Hsieh HY, Croquefer S, Barton R, Marchais V, Pihet M, et al. Development of an oligonucleotide array for direct detection of fungi in sputum samples from patients with cystic fibrosis. J Clin Microbiol [Internet]. 2009;47(1):142–52. http://jcm.asm.org/cgi/doi/10.1128/JCM.01668-08.
Middleton PG, Chen SCA, Meyer W. Fungal infections and treatment in cystic fibrosis. Curr Opin Pulm Med [Internet]. 2013;19(6):670–5. http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00063198-201311000-00013.
Schwarz C, Brandt C, Antweiler E, Krannich A, Staab D, Schmitt-Grohé S, et al. Prospective multicenter German study on pulmonary colonization with Scedosporium /Lomentospora species in cystic fibrosis: epidemiology and new association factors. Chotirmall SH, editor. PLoS One. 2017;12(2):e0171485. https://dx.plos.org/10.1371/journal.pone.0171485.
Schwarz C, Brandt C, Whitaker P, Sutharsan S, Skopnik H, Gartner S, et al. Invasive pulmonary fungal infections in cystic fibrosis. Mycopathologia [Internet]. 2018Feb 1;183(1):33–43. https://doi.org/10.1007/s11046-017-0199-4.
Schwarz C, Brandt C, Melichar V, Runge C, Heuer E, Sahly H, et al. Combined antifungal therapy is superior to monotherapy in pulmonary scedosporiosis in cystic fibrosis. J Cyst Fibros. 2019;18(2):227–32.
Roehmel JF, Tintelnot K, Bernhardt A, Seibold M, Staab D, Schwarz C. Arxula adeninivorans causing invasive pulmonary mycosis and fungaemia in cystic fibrosis. Lancet. 2015;385(9976):1476.
Zalar P, Novak M, de Hoog GS, Gunde-Cimerman N. Dishwashers – a man-made ecological niche accommodating human opportunistic fungal pathogens. Fungal Biol [Internet]. 2011;115(10):997–1007. https://linkinghub.elsevier.com/retrieve/pii/S1878614611000729.
Kusenbach G, Skopnik H, Haase G, Friedrichs F, Döhmen H. Exophiala dermatitidis pneumonia in cystic fibrosis. Eur J Pediatr [Internet]. 1992May;151(5):344–6. https://doi.org/10.1007/BF02113255.
Haase G, Skopnik H, Kusenbach G. Exophiala dermatitidis infection in cystic fibrosis. Lancet. 1990;336(8708):188–9. https://doi.org/10.1016/0140-6736(90)91721-l.
Hickey PW, Sutton DA, Fothergill AW, Rinaldi MG, Wickes BL, Schmidt HJ, et al. Trichosporon mycotoxinivorans, a novel respiratory pathogen in patients with cystic fibrosis. J Clin Microbiol. 2009;47(10):3091–7. https://doi.org/10.1128/JCM.00460-09.
Hirschi S, Letscher-Bru V, Pottecher J, Lannes B, Jeung MY, Degot T, et al. Disseminated Trichosporon mycotoxinivorans, Aspergillus fumigatus, and Scedosporium apiospermum coinfection after lung and liver transplantation in a cystic fibrosis patient. J Clin Microbiol [Internet]. 2012;50(12):4168–70. http://jcm.asm.org/cgi/doi/10.1128/JCM.01928-12.
Jubin V, Ranque S, Stremler Le bel N, Sarles J, Dubus J-C. Risk factors for Aspergillus colonization and allergic bronchopulmonary aspergillosis in children with cystic fibrosis. Pediatr Pulmonol [Internet]. 2010;45(8):764–71. http://doi.wiley.com/10.1002/ppul.21240.
Eschenhagen P, Grehn C, Schwarz C. Prospective evaluation of Aspergillus fumigatus-Specific IgG in patients with cystic fibrosis. Front Cell Infect Microbiol. 2021;10:602836. https://doi.org/10.3389/fcimb.2020.602836.
Geller DE, Kaplowitz H, Light MJ, Colin AA. Allergic bronchopulmonary aspergillosis in cystic fibrosis. Chest [Internet]. 1999;116(3):639–46. https://linkinghub.elsevier.com/retrieve/pii/S0012369216352795.
Baxter CG, Dunn G, Jones AM, Webb K, Gore R, Richardson MD, et al. Novel immunologic classification of aspergillosis in adult cystic fibrosis. J Allergy Clin Immunol [Internet]. 2013Sep;132(3):560-566.e10. https://linkinghub.elsevier.com/retrieve/pii/S0091674913005988.
Brandt C, Roehmel J, Rickerts V, Melichar V, Niemann N, Schwarz C. Aspergillus bronchitis in patients with cystic fibrosis. Mycopathologia. 2018;183(1):61–9.
Albon D, Zhang L, Patrie J, Jones M, Li ZG, Noonan E, et al. Association between Cystic Fibrosis exacerbations, lung function, T2 inflammation and microbiological colonization. Allergy Asthma Clin Immunol. 2023;19(1):15. https://doi.org/10.1186/s13223-023-00760-z.
https://www.ecfs.eu/projects/ecfs-patient-registry/annual-reports.
Hong G, Desai S, Moss RB, Eschenhagen P, Quon BS, Schwarz C. Clinician variability in the diagnosis and treatment of Aspergillus fumigatus-related conditions in cystic fibrosis: an international survey. J Cyst Fibros. 2022;21(1):136–42.
Shoseyov D, Brownlee KG, Conway SP, Kerem E. Aspergillus bronchitis in cystic fibrosis. Chest. 2006;130(1):222–6.
King J, Brunel SF, Warris A. Aspergillus infections in cystic fibrosis. J Infect. 2016;72 Suppl:S50–5. https://doi.org/10.1016/j.jinf.2016.04.022.
Ryan PJ, Stableforth DE, Muhdi KM, Reynolds J. Treatment of pulmonary aspergilloma in cystic fibrosis by percutaneous instillation of amphotericin B VIA indwelling catheter. Thorax. 1995;50(7):809–10.
Maguire CP, Hayes JP, Hayes M, FitzGerald MX, Masterson J. Three cases of pulmonary aspergilloma in adult patients with cystic fibrosis. Thorax. 1995;50(7):805–6.
Logan M, McLoughlin R, Gibney RG, Griscom NT. Aspergilloma complicating cystic fibrosis. AJR Am J Roentgenol [Internet]. 1993;161(3):674–5. Available from: https://pubmed.ncbi.nlm.nih.gov/8352126/.
Cohen-Cymberknoh M. Fungal infection and ABPA in CF. Paediatr Respir Rev [Internet]. 2013;14:S34-5. https://linkinghub.elsevier.com/retrieve/pii/S1526054213700307.
Schwarz C, Hartl D, Eickmeier O, Hector A, Benden C, Durieu I, et al. Progress in definition, prevention and treatment of fungal infections in cystic fibrosis. Mycopathologia [Internet]. 2018;183(1):21–32. https://doi.org/10.1007/s11046-017-0182-0.
Scheffold A, Schwarz C, Bacher P. Fungus-specific CD4 T cells as specific sensors for identification of pulmonary fungal infections. Mycopathologia. 2018;183(1):213–26.
Bacher P, Steinbach A, Kniemeyer O, Hamprecht A, Assenmacher M, Vehreschild MJGT, et al. Fungus-specific CD4 + T cells for rapid identification of invasive pulmonary mold infection. Am J Respir Crit Care Med [Internet]. 2015;191(3):348–52. http://www.atsjournals.org/doi/abs/10.1164/rccm.201407-1235LE.
Borman AM, Palmer MD, Delhaes L, Carrère J, Favennec L, Ranque S, et al. Lack of standardization in the procedures for mycological examination of sputum samples from CF patients: a possible cause for variations in the prevalence of filamentous fungi. Med Mycol. 2010;48(Suppl 1):S88–97. https://doi.org/10.3109/13693786.2010.511287.
Pashley CH, Fairs A, Morley JP, Tailor S, Agbetile J, Bafadhel M, et al. Routine processing procedures for isolating filamentous fungi from respiratory sputum samples may underestimate fungal prevalence. Med Mycol. 2012;50(4):433–8. https://doi.org/10.3109/13693786.2011.615762.
Rey MM, Hong G. Growing mold together–moving beyond standard cultures in assessing fungi in the CF airway. J Cyst Fibros. 2021;20(2):191–2.
Hong G, Miller HB, Allgood S, Lee R, Lechtzin N, Zhang SX. Use of selective fungal culture media increases rates of detection of fungi in the respiratory tract of cystic fibrosis patients. J Clin Microbiol. 2017;55(4):1122–30.
Thronicke A, Heger N, Antweiler E, Krannich A, Roehmel J, Brandt C, et al. Allergic bronchopulmonary aspergillosis is associated with pet ownership in cystic fibrosis. Pediatr Allergy Immunol. 2016;27(6):597–603.
Grehn C, Eschenhagen P, Temming S, Düesberg U, Neumann K, Schwarz C. Urban life as risk factor for aspergillosis. Front Cell Infect Microbiol. 2020;10:601834. https://doi.org/10.3389/fcimb.2020.601834.
Grehn C, Eschenhagen P, Temming S, Düesberg U, Neumann K, Schwarz C. Frequent pet contact as risk factor for allergic bronchopulmonary aspergillosis in cystic fibrosis. Front Cell Infect Microbiol. 2021;10:601821. https://doi.org/10.3389/fcimb.2020.601821.
Reece E, McClean S, Greally P, Renwick J. The prevalence of Aspergillus fumigatus in early cystic fibrosis disease is underestimated by culture-based diagnostic methods. J Microbiol Methods. 2019;164:105683. https://doi.org/10.1016/j.mimet.2019.105683.
Boyle M, Moore JE, Whitehouse JL, Bilton D, Downey DG. The diagnosis and management of respiratory tract fungal infection in cystic fibrosis: a UK survey of current practice. Med Mycol. 2019;57(2):155–60. https://doi.org/10.1093/mmy/myy014.
Sedlacek L, Graf B, Schwarz C, Albert F, Peter S, Würstl B, et al. Prevalence of Scedosporium species and Lomentospora prolificans in patients with cystic fibrosis in a multicenter trial by use of a selective medium. J Cyst Fibros [Internet]. 2015;14(2):237–41. https://linkinghub.elsevier.com/retrieve/pii/S1569199314003117.
Tintelnot K, Just-Nübling G, Horré R, Graf B, Sobottka I, Seibold M, et al. A review of German Scedosporium prolificans cases from 1993 to 2007. Med Mycol [Internet]. 2009;47(4):351–8. https://academic.oup.com/mmy/article-lookup/doi/10.1080/13693780802627440.
Chen SCA, Meyer W, Pashley CH. Challenges in laboratory detection of fungal pathogens in the airways of cystic fibrosis patients. Mycopathologia. 2018;183(1):89–100.
Coron N, Pihet M, Fréalle E, Lemeille Y, Pinel C, Pelloux H, et al. Toward the standardization of mycological examination of sputum samples in cystic fibrosis: results from a French multicenter prospective study. Mycopathologia [Internet]. 2018;183(1):101–17. https://doi.org/10.1007/s11046-017-0173-1.
Delhaes L, Touati K, Faure-Cognet O, Cornet M, Botterel F, Dannaoui E, et al. Prevalence, geographic risk factor, and development of a standardized protocol for fungal isolation in cystic fibrosis: results from the international prospective study "MFIP". J Cyst Fibros. 2019;18(2):212–20. https://doi.org/10.1016/j.jcf.2018.10.001.
Engel TGP, Tehupeiory-Kooreman M, Melchers WJG, Reijers MH, Merkus P, Verweij PE. Evaluation of a new culture protocol for enhancing fungal detection rates in respiratory samples of cystic fibrosis patients. J Fungi (Basel). 2020;6(2):82. https://doi.org/10.3390/jof6020082.
Devoto TB, Alava KSH, Pola SJ, Pereda R, Rubeglio E, Finquelievich JL, et al. Molecular epidemiology of Aspergillus species and other moulds in respiratory samples from Argentinean patients with cystic fibrosis. Med Mycol [Internet]. 2020;58(7):867–73. https://academic.oup.com/mmy/article/58/7/867/5698398.
Nagano Y, Millar BC, Goldsmith CE, Walker JM, Elborn JS, Rendall J, et al. Development of selective media for the isolation of yeasts and filamentous fungi from the sputum of adult patients with cystic fibrosis (CF). J Cyst Fibros. 2008;7(6):566–72.
Hedayati MT, Tavakoli M, Maleki M, Heidari S, Mortezaee V, Gheisari M, et al. Fungal epidemiology in cystic fibrosis patients with a special focus on Scedosporium species complex. Microb Pathog. 2019;129:168–75. https://doi.org/10.1016/j.micpath.2019.02.009.
Raclavsky V, Novotny R. Burkholderia cepacia selective agar can be useful for recovery of Exophiala dermatitidis from sputum samples of cystic fibrosis patients. J Cyst Fibros. 2016;15(2):e19. https://doi.org/10.1016/j.jcf.2015.12.021.
Boyle M, Moore JE, Whitehouse JL, Bilton D, Downey DG. Laboratory diagnosis and characterization of fungal disease in patients with cystic fibrosis (CF): a survey of current UK practice in a cohort of clinical microbiology laboratories. Mycopathologia. 2018;183(4):723–9. https://doi.org/10.1007/s11046-018-0251-z.
Hong G, White M, Lechtzin N, West NE, Avery R, Miller H, et al. Fatal disseminated Rasamsonia infection in cystic fibrosis post-lung transplantation. J Cyst Fibros [Internet]. 2017;16(2):e3-7. https://linkinghub.elsevier.com/retrieve/pii/S1569199317300127.
Giraud S, Favennec L, Bougnoux ME, Bouchara JP. Rasamsonia argillacea species complex: taxonomy, pathogenesis and clinical relevance. Future Microbiol. 2013;8(8):967–78.
Giraud S, Pihet M, Razafimandimby B, Carrère J, Degand N, Mely L, et al. Geosmithia argillacea: an emerging pathogen in patients with cystic fibrosis. J Clin Microbiol. 2010;48(7):2381–6. https://doi.org/10.1128/JCM.00047-10.
Nagano Y, Elborn JS, Millar BC, Walker JM, Goldsmith CE, Rendall J, et al. Comparison of techniques to examine the diversity of fungi in adult patients with cystic fibrosis. Med Mycol. 2010;48(1):166–76.e1. https://doi.org/10.3109/13693780903127506.
Balashov SV, Gardiner R, Park S, Perlin DS. Rapid, high-throughput, multiplex, real-time PCR for identification of mutations in the cyp51A gene of Aspergillus fumigatus that confer resistance to itraconazole. J Clin Microbiol [Internet]. 2005;43(1):214–22. https://jcm.asm.org/content/43/1/214.
Hahn A, Sanyal A, Perez GF, Colberg-Poley AM, Campos J, Rose MC, et al. Different next generation sequencing platforms produce different microbial profiles and diversity in cystic fibrosis sputum. J Microbiol Methods. 2016;1(130):95–9.
Kondori N, Lindblad A, Welinder-Olsson C, Wennerås C, Gilljam M. Development of IgG antibodies to Exophiala dermatitidis is associated with inflammatory responses in patients with cystic fibrosis. J Cyst Fibros. 2014;13(4):391–9. https://doi.org/10.1016/j.jcf.2013.12.007.
Martin-Souto L, Buldain I, Areitio M, Aparicio-Fernandez L, Antoran A, Bouchara JP, et al. ELISA test for the serological detection of Scedosporium/Lomentospora in cystic fibrosis patients. Front Cell Infect Microbiol. 2020;10:602089. https://doi.org/10.3389/fcimb.2020.602089.
Martin-Souto L, Antoran A, Areitio M, Aparicio-Fernandez L, Martín-Gómez MT, Fernandez R, et al. Dot immunobinding assay for the rapid serodetection of Scedosporium/Lomentospora in cystic fibrosis patients. J Fungi (Basel). 2023;9(2):158. https://doi.org/10.3390/jof9020158.
Vandeputte P, Dugé de Bernonville T, Le Govic Y, Le Gal S, Nevez G, Papon N, et al. Comparative transcriptome analysis unveils the adaptative mechanisms of Scedosporium apiospermum to the microenvironment encountered in the lungs of patients with cystic fibrosis. Comput Struct Biotechnol J. 2020;18:3468–83. https://doi.org/10.1016/j.csbj.2020.10.034
Mello TP, Oliveira SSC, Branquinha MH, Santos ALS. Decoding the antifungal resistance mechanisms in biofilms of emerging, ubiquitous and multidrug-resistant species belonging to the Scedosporium/Lomentospora genera. Med Mycol. 2022;60(6):myac036. https://doi.org/10.1093/mmy/myac036.
Mello TP, Lackner M, Branquinha MH, Santos ALS. Impact of biofilm formation and azoles' susceptibility in Scedosporium/Lomentospora species using an in vitro model that mimics the cystic fibrosis patients' airway environment. J Cyst Fibros. 2021;20(2):303–9. https://doi.org/10.1016/j.jcf.2020.12.001.
Prigitano A, Esposto MC, Biffi A, De Lorenzis G, Favuzzi V, Koncan R, et al. Triazole resistance in Aspergillus fumigatus isolates from patients with cystic fibrosis in Italy. J Cyst Fibros [Internet]. 2017;16(1):64–9. https://linkinghub.elsevier.com/retrieve/pii/S1569199316305513.
Seufert R, Sedlacek L, Kahl B, Hogardt M, Hamprecht A, Haase G, et al. Prevalence and characterization of azole-resistant Aspergillus fumigatus in patients with cystic fibrosis: a prospective multicentre study in Germany. J Antimicrob Chemother. 2018;73(8):2047–53. https://doi.org/10.1093/jac/dky147.
Abdolrasouli A, Scourfield A, Rhodes J, Shah A, Elborn JS, Fisher MC, et al. High prevalence of triazole resistance in clinical Aspergillus fumigatus isolates in a specialist cardiothoracic centre. Int J Antimicrob Agents [Internet]. 2018;52(5):637–42. https://linkinghub.elsevier.com/retrieve/pii/S0924857918302309.
Lavergne RA, Morio F, Danner-Boucher I, Horeau-Langlard D, David V, Hagen F, et al. One year prospective survey of azole resistance in Aspergillus fumigatus at a French cystic fibrosis reference centre: prevalence and mechanisms of resistance. J Antimicrob Chemother [Internet]. 2019;74(7):1884–9. https://academic.oup.com/jac/article/74/7/1884/5481886.
Risum M, Hare RK, Gertsen JB, Kristensen L, Johansen HK, Helweg-Larsen J, et al. Azole-Resistant Aspergillus fumigatus among danish cystic fibrosis patients: increasing prevalence and dominance of TR34/L98H. Front Microbiol. 2020;11:1850. https://doi.org/10.3389/fmicb.2020.01850.
Fischer J, Van Koningsbruggen-Rietschel S, Rietschel E, Vehreschild MJGT, Wisplinghoff H, Krönke M, et al. Prevalence and molecular characterization of azole resistance in Aspergillus spp. isolates from German cystic fibrosis patients. J Antimicrob Chemother. 2014;69(6):1533–6.
Schwarz C, Brandt C, Melichar V, Runge C, Heuer E, Sahly H, et al. Combined antifungal therapy is superior to monotherapy in pulmonary scedosporiosis in cystic fibrosis. J Cyst Fibros [Internet]. 2019;18(2):227–32. https://linkinghub.elsevier.com/retrieve/pii/S156919931830794X.
Schwarz C, Eschenhagen P, Bouchara JP. Emerging fungal threats in cystic fibrosis. Mycopathologia. 2021;186(5):639–53. https://doi.org/10.1007/s11046-021-00574-w.
Marchiori E, Zanetti G, Hochhegger B, Irion KL, Carvalho ACP, Godoy MCB. Reversed halo sign on computed tomography: state-of-the-art review. Lung [Internet]. 2012;190(4):389–94. https://doi.org/10.1007/s00408-012-9392-x.
Hussien A, Lin CT. CT findings of fungal pneumonia with emphasis on aspergillosis. Emerg Radiol [Internet]. 2018;25(6):685–9. https://doi.org/10.1007/s10140-018-1621-z.
Bacher P, Scheffold A. Flow-cytometric analysis of rare antigen-specific T cells. Cytom Part A [Internet]. 2013;83A(8):692–701. http://doi.wiley.com/10.1002/cyto.a.22317.
Bacher P, Schink C, Teutschbein J, Kniemeyer O, Assenmacher M, Brakhage AA, et al. Antigen-reactive T cell enrichment for direct, high-resolution analysis of the human naive and memory Th cell repertoire. J Immunol [Internet]. 2013;190(8):3967–76. http://www.jimmunol.org/lookup/doi/10.4049/jimmunol.1202221.
Jenks JD, Prattes J, Frank J, Spiess B, Mehta SR, Boch T, et al. Performance of the bronchoalveolar lavage fluid aspergillus galactomannan lateral flow assay with cube reader for diagnosis of invasive pulmonary aspergillosis: a multicenter cohort study. Clin Infect Dis. 2021;73(7):e1737–44. https://doi.org/10.1093/cid/ciaa1281.
Hoenigl M, Egger M, Boyer J, Schulz E, Prattes J, Jenks JD. Serum lateral flow assay with digital reader for the diagnosis of invasive pulmonary aspergillosis: a two-centre mixed cohort study. Mycoses. 2021;64(10):1197–202.
Egger M, Penziner S, Dichtl K, Gornicec M, Kriegl L, Krause R, et al. Performance of the euroimmun aspergillus antigen ELISA for the diagnosis of invasive pulmonary aspergillosis in bronchoalveolar lavage fluid. J Clin Microbiol. 2022;60(4):e0021522. https://doi.org/10.1128/jcm.00215-22.
Mina S, Staerck C, Marot A, Godon C, Calenda A, Bouchara JP, et al. Scedosporium boydii CatA1 and SODC recombinant proteins, new tools for serodiagnosis of Scedosporium infection of patients with cystic fibrosis. Diagn Microbiol Infect Dis. 2017;89(4):282–7. https://doi.org/10.1016/j.diagmicrobio.2017.08.013.
Emerson J, Rosenfeld M, McNamara S, Ramsey B, Gibson RL. Pseudomonas aeruginosa and other predictors of mortality and morbidity in young children with cystic fibrosis. Pediatr Pulmonol [Internet]. 2002;34(2):91–100. http://doi.wiley.com/10.1002/ppul.10127.
Hector A, Kirn T, Ralhan A, Graepler-Mainka U, Berenbrinker S, Riethmueller J, et al. Microbial colonization and lung function in adolescents with cystic fibrosis. J Cyst Fibros [Internet]. 2016;15(3):340–9. https://linkinghub.elsevier.com/retrieve/pii/S1569199316000114.
Mousset S, Buchheidt D, Heinz W, Ruhnke M, Cornely OA, Egerer G, et al. Treatment of invasive fungal infections in cancer patients-updated recommendations of the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Oncology (DGHO). Ann Hematol. 2014;93(1):13–32. https://doi.org/10.1007/s00277-013-1867-1.
Navarro J, Rainisio M, Harms HK, Hodson ME, Koch C, Mastella G, et al. Factors associated with poor pulmonary function: cross-sectional analysis of data from the ERCF. European Epidemiologic Registry of Cystic Fibrosis. Eur Respir J. 2001;18(2):298–305. https://doi.org/10.1183/09031936.01.00068901.
Ruhnke M, Cornely OA, Schmidt-Hieber M, Alakel N, Boell B, Buchheidt D, et al. Treatment of invasive fungal diseases in cancer patients-Revised 2019 Recommendations of the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Oncology (DGHO). Mycoses. 2020;63(7):653–82. https://doi.org/10.1111/myc.13082.
Pellon A, Ramirez-Garcia A, Buldain I, Antoran A, Martin-Souto L, Rementeria A, et al. Pathobiology of Lomentospora prolificans: could this species serve as a model of primary antifungal resistance? Int J Antimicrob Agents. 2018;51(1):10–15. https://doi.org/10.1016/j.ijantimicag.2017.06.009.
Hamprecht A, Morio F, Bader O, Le Pape P, Steinmann J, Dannaoui E. Azole resistance in aspergillus fumigatus in patients with cystic fibrosis: a matter of concern? Mycopathologia. 2018;183(1):151–60. https://doi.org/10.1007/s11046-017-0162-4.
Bentley S, Davies JC, Carr SB, Balfour-Lynn IM. Combination antifungal therapy for Scedosporium species in cystic fibrosis. Pediatr Pulmonol. 2020;55(8):1993–5. https://doi.org/10.1002/ppul.24789.
Cuenca-Estrella M, Alastruey-Izquierdo A, Alcazar-Fuoli L, Bernal-Martinez L, Gomez-Lopez A, Buitrago MJ, et al. In vitro activities of 35 double combinations of antifungal agents against Scedosporium apiospermum and Scedosporium prolificans. Antimicrob Agents Chemother [Internet]. 2008;52(3):1136–9. http://aac.asm.org/cgi/doi/10.1128/AAC.01160-07.
Matos T, de Hoog GS, de Boer AG, de Crom I, Haase G. High prevalence of the neurotrope Exophiala dermatitidis and related oligotrophic black yeasts in sauna facilities. Mycoses. 2002;45(9-10):373–7. https://doi.org/10.1046/j.1439-0507.2002.00779.x.
Kirchhoff L, Olsowski M, Zilmans K, Dittmer S, Haase G, Sedlacek L, et al. Biofilm formation of the black yeast-like fungus Exophiala dermatitidis and its susceptibility to antiinfective agents. Sci Rep. 2017;7:42886. https://doi.org/10.1038/srep42886.
Sudhadham M, Prakitsin S, Sivichai S, Chaiyarat R, Dorrestein GM, Menken SB, et al. The neurotropic black yeast Exophiala dermatitidis has a possible origin in the tropical rain forest. Stud Mycol. 2008;61:145–55. https://doi.org/10.3114/sim.2008.61.15.
Kirchhoff L, Olsowski M, Rath PM, Steinmann J. Exophiala dermatitidis: key issues of an opportunistic fungal pathogen. Virulence. 2019;10(1):984–8. https://doi.org/10.1080/21505594.2019.1596504.
Shah AV, McColley SA, Weil D, Zheng X. Trichosporon mycotoxinivorans infection in patients with cystic fibrosis. J Clin Microbiol. 2014;52(6):2242–4. https://doi.org/10.1128/JCM.03309-13.
Kröner C, Kappler M, Grimmelt AC, Laniado G, Würstl B, Griese M. The basidiomycetous yeast Trichosporon may cause severe lung exacerbation in cystic fibrosis patients - clinical analysis of Trichosporon positive patients in a Munich cohort. BMC Pulm Med. 2013;13:61. https://doi.org/10.1186/1471-2466-13-61.
Yang YL, Liu YW, Chen HT, Tsai MS, Chu WL, Lo HJ. Genotype analysis based on intergenic spacer 1 sequences of Trichosporon asahii collected in Taiwan. Med Mycol. 2013;51(8):880–3.
Agarwal R, Chakrabarti A, Shah A, Gupta D, Meis JF, Guleria R, et al. ABPA complicating asthma ISHAM working group. Allergic bronchopulmonary aspergillosis: review of literature and proposal of new diagnostic and classification criteria. Clin Exp Allergy. 2013;43(8):850–73. https://doi.org/10.1111/cea.12141.
Colombo AL, Padovan AC, Chaves GM. Current knowledge of Trichosporon spp. and Trichosporonosis. Clin Microbiol Rev. 2011;24(4):682–700. https://doi.org/10.1128/CMR.00003-11.
Chotirmall SH. Candida albicans in cystic fibrosis: “opening statements presented, let the trial begin.” Pediatr Pulmonol [Internet]. 2016;51(5):445–6. http://doi.wiley.com/10.1002/ppul.23315.
Hector A, Kirn T, Ralhan A, Graepler-Mainka U, Berenbrinker S, Riethmueller J, et al. Microbial colonization and lung function in adolescents with cystic fibrosis. J Cyst Fibros [Internet]. 2016;15(3):340–9. https://linkinghub.elsevier.com/retrieve/pii/S1569199316000114.
Slavin M, van Hal S, Sorrell TC, Lee A, Marriott DJ, Daveson K, et al. Invasive infections due to filamentous fungi other than Aspergillus: epidemiology and determinants of mortality. Clin Microbiol Infect [Internet]. 2015;21(5):490.e1-490.e10. https://doi.org/10.1016/j.cmi.2014.12.021.
Miraldi F, Anile M, Ruberto F, Tritapepe L, Puglese F, Quattrucci S, et al. Scedosporium apiospermum atrial mycetomas after lung transplantation for cystic fibrosis. Transpl Infect Dis [Internet]. 2012Apr;14(2):188–91. https://doi.org/10.1111/j.1399-3062.2011.00679.x.
Shah SS, Karnak D, Budev M, Avery RK, Mehta AC. Endobronchial Pseudallescheria boydii in lung transplant patient with cystic fibrosis. J Bronchol [Internet]. 2007;14(1):48–50. https://insights.ovid.com/crossref?an=00128594-200701000-00014.
Luijk B, Ekkelenkamp MB, De Jong PA, Kwakkel-van Erp JM, Grutters JC, van Kessel DA, et al. Effective prolonged therapy with voriconazole in a lung transplant recipient with spondylodiscitis induced by Scedosporium apiospermum. Case Rep Infect Dis [Internet]. 2011;2011:1–4. http://www.hindawi.com/journals/criid/2011/460313/.
Vagefi MR, Kim ET, Alvarado RG, Duncan JL, Howes EL, Crawford JB. Bilateral endogenous Scedosporium prolificans endophthalmitis after lung transplantation. Am J Ophthalmol [Internet]. 2005;139(2):370–3. https://linkinghub.elsevier.com/retrieve/pii/S0002939404009559.
Williams C, Ranjendran R, Ramage G. Pathogenesis of fungal infections in cystic fibrosis. Curr Fungal Infect Rep [Internet]. 2016;10(4):163–9. https://doi.org/10.1007/s12281-016-0268-z.
Kosmidis C, Denning DW. The clinical spectrum of pulmonary aspergillosis. Thorax [Internet]. 2015;70:270–7. http://thorax.bmj.com/.
Stevens DA, Moss RB, Kurup VP, Knutsen AP, Greenberger P, Judson MA, et al. Allergic bronchopulmonary aspergillosis in cystic fibrosis—state of the art: Cystic Fibrosis Foundation Consensus Conference. Clin Infect Dis [Internet]. 2003;37(s3):S225-64. https://academic.oup.com/cid/article-lookup/doi/10.1086/376525.
Meis JF, Chowdhary A, Rhodes JL, Fisher MC, Verweij PE. Clinical implications of globally emerging azole resistance in Aspergillus fumigatus. Biological Sciences: Philosophical Transactions of the Royal Society B; 2016.
Perlin DS, Rautemaa-Richardson R, Alastruey-Izquierdo A. The global problem of antifungal resistance: prevalence, mechanisms, and management. Lancet Infect Dis. 2017;17(12):e383–92. https://doi.org/10.1016/S1473-3099(17)30316-X.
Mourad A, Perfect JR. Tolerability profile of the current antifungal armoury. J Antimicrob Chemother. 2018;73(suppl_1):i26–i32. https://doi.org/10.1093/jac/dkx446.
Rivosecchi RM, Samanta P, Demehin M, Nguyen MH. Pharmacokinetics of azole antifungals in cystic fibrosis. Mycopathologia. 2018;183(1):139–50. https://doi.org/10.1007/s11046-017-0189-6.
Van Daele R, Spriet I, Wauters J, Maertens J, Mercier T, Van Hecke S, et al. Antifungal drugs: what brings the future? Med Mycol. 2019;57(Supplement_3):S328–43. https://doi.org/10.1093/mmy/myz012.
Tsai A, Wu SP, Haseltine E, Kumar S, Moskowitz SM, Panorchan P, et al. Physiologically based pharmacokinetic modeling of CFTR modulation in people with cystic fibrosis transitioning from mono or dual regimens to Triple-Combination Elexacaftor/Tezacaftor/Ivacaftor. Pulm Ther. 2020;6(2):275–86. https://doi.org/10.1007/s41030-020-00124-7.
Eschenhagen P, Schwarz C. Therapie der Mukoviszidose – neue Medikamente geben Hoffnung [Therapy of cystic fibrosis - new drugs give hope]. Dtsch Med Wochenschr. 2020;145(20):1486–9. German. https://doi.org/10.1055/a-1140-3937.
Gauthier J, Derome N. Evenness-richness scatter plots: a visual and insightful representation of shannon entropy measurements for ecological community analysis. mSphere. 2021;6(2):e01019–20. https://doi.org/10.1128/mSphere.01019-20.
Lozupone CA, Knight R. Species divergence and the measurement of microbial diversity. FEMS Microbiol Rev. 2008;32(4):557–78. https://doi.org/10.1111/j.1574-6976.2008.00111.x.
O'Connor JB, Wagner BD, Harris JK, Frank DN, Clabots DE, Laguna TA. Detection and identification of fungi in the lower airway of children with and without cystic fibrosis. Front Microbiol. 2023;14:1119703. https://doi.org/10.3389/fmicb.2023.1119703.
Hoenigl M, Sprute R, Egger M, Arastehfar A, Cornely OA, Krause R, et al. The antifungal pipeline: fosmanogepix, ibrexafungerp, olorofim, opelconazole, and rezafungin. Drugs. 2021;81(15):1703–29. https://doi.org/10.1007/s40265-021-01611-0.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Schwarz, C., Mainz, J.G., Romanowska, E. et al. Respiratory Fungal Infections in Cystic Fibrosis: Diagnostic and Therapeutic Challenges. Curr Fungal Infect Rep 17, 202–213 (2023). https://doi.org/10.1007/s12281-023-00467-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12281-023-00467-z