Abstract
Background
Antigen-presenting cells (APC)/T/NK cells are key immune cells that play crucial roles in fighting against malignancies including lung adenocarcinoma (LUAD). In this study, we aimed to identify an APC/T/NK cells-related gene signature (ATNKGS) and potential immune cell-related genes (IRGs) to realize risk stratification, prognosis, and immunotherapeutic response prediction for LUAD patients.
Methods
Based on the univariate Cox regression and the LASSO Cox regression results of 196 APC/T/NK cells-related genes collected from three pathways in the KEGG database, we determined the final genes and established the ATNKGS-related risk model. The single-cell RNA sequencing data were applied for key IRGs identification and investigate their value in immunotherapeutic response prediction. Several GEO datasets and an external immunotherapy cohort from Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, were applied for validation.
Results
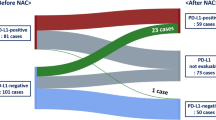
In this study, nine independent public datasets including 1108 patients were enrolled. An ATNKGS containing 16 genes for predicting overall survival of LUAD patients was constructed with robust prognostic capability. The ATNKGS high risk group was related to significantly worse OS outcomes than those in the low-risk group, which were verified in TCGA and four GEO datatsets. A nomogram combining the ATNKGS risk score with clinical TNM stage achieved the optimal prediction performance. The single-cell RNA sequencing analysis revealed CTSL as an IRG of macrophage and monocyte. Moreover, though CTSL was an indicator for poor prognosis of LUAD patients, CTSL high expression group was associated with higher ESTIMATEScore, immune checkpoints expression, and lower TIDE score. Several immunotherapeutic cohorts have confirmed the response-predicting significance of CTSL in patients receiving immune checkpoint inhibitor (ICI) treatment.
Conclusions
Our study provided an insight into the significant role of APC/T/NK cells-related genes in survival risk stratification and CTSL in response prediction of immunotherapy in patients with LUAD.








Similar content being viewed by others
Data availability
The datasets used in the current study are available from the corresponding author upon reasonable request.
Abbreviations
- APC:
-
Antigen-presenting cells
- ATNKGS:
-
APC/T/NK cells-related gene signature
- AUC:
-
Area under the curve
- CTLA4:
-
Cytotoxic T-lymphocyte-associated antigen 4
- CI:
-
Confidence interval
- CR:
-
Complete response
- ESTIMATE:
-
Estimation of stromal and immune cells in malignant tumors using expression data
- FFPE:
-
Formalin-fixed paraffin-embedded
- GOBP:
-
Gene ontology biological process
- HR:
-
Hazard ratio
- ICI:
-
Immune checkpoint inhibitor
- IRG:
-
Immune-related gene
- KEGG:
-
Kyoko encyclopedia of genes and genomes
- LASSO:
-
Least absolute shrinkage and selection operator
- LUAD:
-
Lung adenocarcinoma
- MATH:
-
Mutant-allele tumor heterogeneity
- MPS:
-
Mononuclear phagocyte system
- NSCLC:
-
Non-small cell lung cancer
- OS:
-
Overall survival
- PD:
-
Progressive disease
- PD-1:
-
Programmed cell death protein 1
- PD-L1:
-
Programmed cell death-ligand 1
- PFS:
-
Progression-free survival
- PR:
-
Partial response
- ROC:
-
Receiver operating characteristic
- scRNA:
-
Single-cell RNA
- SD:
-
Stable disease
- TIDE:
-
Tumor immune dysfunction and exclusion
- TME:
-
Tumor microenvironment
References
Sung H, Ferlay J, Siegel RL et al (2021) Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin 71(3):209–249. https://doi.org/10.3322/caac.21660
Thai AA, Solomon BJ, Sequist LV et al (2021) Lung cancer. Lancet 398(10299):535–554. https://doi.org/10.1016/s0140-6736(21)00312-3
Zeng H, Chen W, Zheng R et al (2018) Changing cancer survival in China during 2003–15: a pooled analysis of 17 population-based cancer registries. Lancet Glob Health 6(5):e555–e567. https://doi.org/10.1016/s2214-109x(18)30127-x
Ding Y, Wang Y, Hu Q (2022) Recent advances in overcoming barriers to cell-based delivery systems for cancer immunotherapy. Exploration 2(3):20210106. https://doi.org/10.1002/EXP.20210106
Huang L, Tang L, Dai L et al (2022) The prognostic significance of tumor spread through air space in stage I lung adenocarcinoma. Thorac Cancer 13(7):997–1005. https://doi.org/10.1111/1759-7714.14348
Ettinger DS, Wood DE, Aisner DL et al. (2022) Non-Small Cell Lung Cancer, Version 3.2022, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 20(5):497–530
Zhong Z, Zhi LZ (2021) Chinese Association for Clinical Oncologists MOBoCIE, Promotion Association for Medical Healthcare. [Clinical practice guideline for stage IV primary lung cancer in China(2021 version)]. 43(1):39–59
Niu M, Yi M, Li N et al (2021) Predictive biomarkers of anti-PD-1/PD-L1 therapy in NSCLC. Exp Hematol Oncol 10(1):18. https://doi.org/10.1186/s40164-021-00211-8
Hinshaw DC, Shevde LA (2019) The tumor microenvironment innately modulates cancer progression. Cancer Res 79(18):4557–4566. https://doi.org/10.1158/0008-5472.Can-18-3962
Mao X, Xu J, Wang W et al (2021) Crosstalk between cancer-associated fibroblasts and immune cells in the tumor microenvironment: new findings and future perspectives. Mol Cancer 20(1):131. https://doi.org/10.1186/s12943-021-01428-1
Huang L, Jiang S, Shi Y (2022) Prognostic significance of baseline neutrophil-lymphocyte ratio in patients with non-small-cell lung cancer: a pooled analysis of open phase III clinical trial data. Future Oncol 18(14):1679–1689. https://doi.org/10.2217/fon-2021-1304
Lee MY, Jeon JW, Sievers C et al. (2020) Antigen processing and presentation in cancer immunotherapy. J Immunother Cancer 8(2). https://doi.org/10.1136/jitc-2020-001111
Roche PA, Furuta K (2015) The ins and outs of MHC class II-mediated antigen processing and presentation. Nat Rev Immunol 15(4):203–216. https://doi.org/10.1038/nri3818
Jakubzick CV, Randolph GJ, Henson PM (2017) Monocyte differentiation and antigen-presenting functions. Nat Rev Immunol 17(6):349–362. https://doi.org/10.1038/nri.2017.28
Hume DA, Irvine KM, Pridans C (2019) The mononuclear phagocyte system: the relationship between monocytes and macrophages. Trends Immunol 40(2):98–112. https://doi.org/10.1016/j.it.2018.11.007
Germic N, Frangez Z, Yousefi S et al (2019) Regulation of the innate immune system by autophagy: monocytes, macrophages, dendritic cells and antigen presentation. Cell Death Differ 26(4):715–727. https://doi.org/10.1038/s41418-019-0297-6
Jhunjhunwala S, Hammer C, Delamarre L (2021) Antigen presentation in cancer: insights into tumour immunogenicity and immune evasion. Nat Rev Cancer 21(5):298–312. https://doi.org/10.1038/s41568-021-00339-z
Waldman AD, Fritz JM, Lenardo MJ (2020) A guide to cancer immunotherapy: from T cell basic science to clinical practice. Nat Rev Immunol 20(11):651–668. https://doi.org/10.1038/s41577-020-0306-5
He J, Xiong X, Yang H et al (2022) Defined tumor antigen-specific T cells potentiate personalized TCR-T cell therapy and prediction of immunotherapy response. Cell Res 32(6):530–542. https://doi.org/10.1038/s41422-022-00627-9
Sivori S, Pende D, Quatrini L, et al. (2021) NK cells and ILCs in tumor immunotherapy. Mol Aspects Med 80:100870. https://doi.org/10.1016/j.mam.2020.100870
Zeng Y, Lv X, Du J (2021) Natural killer cell‑based immunotherapy for lung cancer: Challenges and perspectives (Review). Oncol Rep 46(5). https://doi.org/10.3892/or.2021.8183
Huang L, Jiang S, Shi Y (2020) Tyrosine kinase inhibitors for solid tumors in the past 20 years (2001–2020). J Hematol Oncol 13(1):143. https://doi.org/10.1186/s13045-020-00977-0
Reck M, Remon J, Hellmann MD (2022) First-line immunotherapy for non-small-cell lung cancer. J Clin Oncol 40(6):586–597. https://doi.org/10.1200/jco.21.01497
Marusyk A, Almendro V, Polyak K (2012) Intra-tumour heterogeneity: a looking glass for cancer? Nat Rev Cancer 12(5):323–334. https://doi.org/10.1038/nrc3261
Esensten JH, Helou YA, Chopra G et al (2016) CD28 costimulation: from mechanism to therapy. Immunity 44(5):973–988. https://doi.org/10.1016/j.immuni.2016.04.020
Acharya N, Sabatos-Peyton C, Anderson AC (2020) Tim-3 finds its place in the cancer immunotherapy landscape. J Immunother Cancer 8(1). https://doi.org/10.1136/jitc-2020-000911
Das M, Zhu C, Kuchroo VK (2017) Tim-3 and its role in regulating anti-tumor immunity. Immunol Rev 276(1):97–111. https://doi.org/10.1111/imr.12520
Stratmann JA, Sebastian M (2019) Polo-like kinase 1 inhibition in NSCLC: mechanism of action and emerging predictive biomarkers. Lung Cancer (Auckl) 10:67–80. https://doi.org/10.2147/lctt.S177618
Sebastian M, Reck M, Waller CF et al (2010) The efficacy and safety of BI 2536, a novel Plk-1 inhibitor, in patients with stage IIIB/IV non-small cell lung cancer who had relapsed after, or failed, chemotherapy: results from an open-label, randomized phase II clinical trial. J Thorac Oncol 5(7):1060–1067. https://doi.org/10.1097/JTO.0b013e3181d95dd4
Caiola E, Iezzi A, Tomanelli M et al (2020) LKB1 deficiency renders NSCLC cells sensitive to ERK inhibitors. J Thorac Oncol 15(3):360–370. https://doi.org/10.1016/j.jtho.2019.10.009
Moschos SJ, Sullivan RJ, Hwu WJ, et al (2018) Development of MK-8353, an orally administered ERK1/2 inhibitor, in patients with advanced solid tumors. JCI Insight 3(4). https://doi.org/10.1172/jci.insight.92352
Valero C, Lee M, Hoen D et al (2021) The association between tumor mutational burden and prognosis is dependent on treatment context. Nat Genet 53(1):11–15. https://doi.org/10.1038/s41588-020-00752-4
Chifman J, Pullikuth A, Chou JW et al (2016) Conservation of immune gene signatures in solid tumors and prognostic implications. BMC Cancer 16(1):911. https://doi.org/10.1186/s12885-016-2948-z
Schoenfeld AJ, Bandlamudi C, Lavery JA et al (2020) The genomic landscape of SMARCA4 alterations and associations with outcomes in patients with lung cancer. Clin Cancer Res 26(21):5701–5708. https://doi.org/10.1158/1078-0432.Ccr-20-1825
Altan-Bonnet G, Mukherjee R (2019) Cytokine-mediated communication: a quantitative appraisal of immune complexity. Nat Rev Immunol 19(4):205–217. https://doi.org/10.1038/s41577-019-0131-x
Ozga AJ, Chow MT, Luster AD (2021) Chemokines and the immune response to cancer. Immunity 54(5):859–874. https://doi.org/10.1016/j.immuni.2021.01.012
Kolev M, Markiewski MM (2018) Targeting complement-mediated immunoregulation for cancer immunotherapy. Semin Immunol 37:85–97. https://doi.org/10.1016/j.smim.2018.02.003
Li YY, Fang J, Ao GZ (2017) Cathepsin B and L inhibitors: a patent review (2010 - present). Expert Opin Ther Pat 27(6):643–656. https://doi.org/10.1080/13543776.2017.1272572
Zhao MM, Yang WL, Yang FY et al (2021) Cathepsin L plays a key role in SARS-CoV-2 infection in humans and humanized mice and is a promising target for new drug development. Signal Transduct Target Ther 6(1):134. https://doi.org/10.1038/s41392-021-00558-8
Gocheva V, Zeng W, Ke D et al (2006) Distinct roles for cysteine cathepsin genes in multistage tumorigenesis. Genes Dev 20(5):543–556. https://doi.org/10.1101/gad.1407406
Zhang L, Wei C, Li D et al (2022) COVID-19 receptor and malignant cancers: association of CTSL expression with susceptibility to SARS-CoV-2. Int J Biol Sci 18(6):2362–2371. https://doi.org/10.7150/ijbs.70172
Sudhan DR, Siemann DW (2015) Cathepsin L targeting in cancer treatment. Pharmacol Ther 155:105–116. https://doi.org/10.1016/j.pharmthera.2015.08.007
Han ML, Zhao YF, Tan CH et al (2016) Cathepsin L upregulation-induced EMT phenotype is associated with the acquisition of cisplatin or paclitaxel resistance in A549 cells. Acta Pharmacol Sin 37(12):1606–1622. https://doi.org/10.1038/aps.2016.93
Dana D, Pathak SK (2020) A review of small molecule inhibitors and functional probes of human Cathepsin L. Molecules 25(3). https://doi.org/10.3390/molecules25030698
Acknowledgements
We thank the data donors and research groups of TCGA-LUAD, GSE11969, GSE31210, GSE37745, GSE50081, GSE126044, GSE135222, and GSE117570. We thank the public TCGA, GEO, and KEGG databases, as well as UCSC Xena website, thank the patients in Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College who provided samples in this study. We also would like to thank Wu et al.’s article (https://doi.org/10.1038/s41388-021-01853-y) and He et al.’s article (https://doi.org/10.1093/bib/bbac291) as Figures 2 and 3 in this study referred to the typesetting format of their articles.
Funding
This work was funded by China National Major Project for New Drug Innovation (2017ZX09304015) and Major Project of Medical Oncology Key Foundation of Cancer Hospital Chinese Academy of Medical Sciences (CICAMS-MOMP2022006).
Author information
Authors and Affiliations
Contributions
YKS and XHH contributed to supervision, conceptualization, funding acquisition, project administration, and writing—review and editing. LLH helped in data curation, visualization, writing—original draft, and writing—review and editing. NL helped in data curation, visualization, and writing—review and editing; TJX contributed to visualization and writing—review and editing. Le Tang contributed to writing—review and editing. All authors contributed to manuscript revision and final approval.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that there are no conflicts of interest.
Ethical statement
The study was conducted according to the guidelines of the Declaration of Helsinki, was approved by the institutional ethical committee of Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College (19–019/1804), and informed consent was obtained from all patients.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Huang, L., Lou, N., Xie, T. et al. Identification of an antigen-presenting cells/T/NK cells-related gene signature to predict prognosis and CTSL to predict immunotherapeutic response for lung adenocarcinoma: an integrated analysis of bulk and single-cell RNA sequencing. Cancer Immunol Immunother 72, 3259–3277 (2023). https://doi.org/10.1007/s00262-023-03485-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00262-023-03485-5