Abstract
Purpose
Recent data suggest that individual morphologic factors should be respected to restore preoperative patellofemoral alignment and thus reduce the likelihood of anterior knee pain. The goal of this study was to investigate the effect of excessive femoral torsion (FT) on clinical outcome of TKA.
Methods
Patients who underwent TKA and complete preoperative radiographic evaluation including a long-leg radiograph and CT scan were included. 51 patients showed increased FT of > 20° and were matched for age/sex to 51 controls (FT < 20°). Thirteen patients were lost to follow-up. Thirty-eight matched pairs were compared after a 2 year follow-up clinically (Kujala and patellofemoral score for TKA) and radiographically (FT, frontal leg axis, TT-TG, patellar thickness, patellar tilt, and lateral displacement of patella). Functional alignment of TKA was performed (hybrid-technique). All patellae were denervated but no patella was resurfaced.
Results
There was no significant difference between clinical scores two years after surgery between patients with normal and excessive FT (n.s.). Kujala score was 64.3 ± 16.7 versus 64.8 ± 14.4 (n.s.), and patellofemoral score for TKA was 74.3 ± 21 versus 78.5 ± 20.7 (n.s.) for increased FT group and control group, respectively. There was no correlation between preoperative FT and clinical scores. Other radiographic parameters were similar between both groups. No correlations between clinical outcomes and preoperative/postoperative frontal leg axis or total leg axis correction were found (n.s.).
Conclusion
If the leg axis deformity is corrected to a roughly neutral alignment during cemented TKA, including patellar denervation, then excessive FT was not associated with patellofemoral pain or instability.
Level of evidence.
Prospective comparative study, level II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With up to 10%, anterior knee pain is the most common reason for unsatisfying outcomes following total knee arthroplasty (TKA), and leads the ranking of reasons for TKA revision surgery [2, 34, 43]. According to literature, including national registry data, 25–30% of all TKA revisions are performed because of patellar problems [27, 28, 40].
Patellofemoral maltracking can occur in both resurfaced and non-resurfaced patellae [29]. An important technical consideration to avoid patellofemoral maltracking includes appropriate rotational component alignment [30]. In addition, recent data suggest that individual morphologic factors should be respected to restore preoperative patellofemoral alignment and thus reduce the likelihood of anterior knee pain [14, 15]. In addition to coronal malalignment, however, there is another factor that has not yet been considered in current research. In parallel with the complexity of bony malalignment in patients with patellofemoral instability, increased femoral torsion (FT) might be another risk factor for anterior knee pain following TKA. It was shown that excessive FT negatively affects the outcome after surgical treatment of patients with patellofemoral instability [10]. Accordingly, osteotomies to correct axial and frontal plane malalignment have recently become popular [4, 7, 9, 11]. Furthermore, femoral rotational deformity was elaborated to affect patellar tracking and increase joint stress, resulting in accelerated femoropatellar joint degeneration [8, 26].
The purpose of this study was therefore to investigate whether excessive preoperative FT is associated with patellofemoral pain or instability following TKA. The hypothesis was that preoperative FT has no relevant influence on clinical outcomes of TKA patients. A second hypothesis was that as long as the frontal leg axis is aligned to roughly neutral, postoperative coronal alignment will not affect outcome either.
Materials and methods
Study population
All patients who received a primary total knee replacement (Medacta MyKnee GMK, Medacta International, Castel San Pietro, CH) at our institution as of 2019 were potential candidates for the study. Exclusion criteria were trauma (including patella fractures or dislocations), previous tumors, previous surgical knee procedures, chronic patellar dislocation, or malformation (or malunion after a fracture) of the affected limb. Complete preoperative radiographic (long-leg standing view, lateral and anteroposterior radiograph, axial view of the patella) work-up needed to be available too. For preoperative CT-based planning of patient-specific instrumented knee replacement, a computed tomography (CT) of the affected lower extremity was acquired using a specially developed protocol to scan the regions of interest (i.e. proximal femur, knee centre with distal femur and proximal tibia, ankle joint centre with distal tibia, distal fibula and talus).
Fifty-one patients of 210 showed increased FT of > 20° and were matched for age and sex to 51 controls (FT < 20°). Five study group patients (FT > 20°) refused to participate and 8 patients were lost to follow-up. Therefore, at final follow-up, two years after total knee replacement, the study population consisted of 38 matched pairs.
Surgical technique
In all cases, patient-specific cutting blocks were used. Femoral and tibial cuts were performed to place implants perpendicular to the mechanical axis of the bone. However, deviations of bone cuts (and femoral component rotation) were made using PSI to ensure optimal gap balancing in some cases. No ligament balancing was performed in any case. Moreover, no effort was made to compensate for increased FT. The surgeon was not aware of the patient’s preoperative FT (FT was blinded). The femoral component was externally rotated with the sole goal of creating a rectangular and symmetric flexion gap. On average, external rotation was 2.5° (range 0–5°) from the posterior condylar axis. All patellae were denervated but no patella was resurfaced. All components were cemented.
Clinical assessment
All 76 patients completed the final follow-up after two years. Kujala score and the patellofemoral scoring system for TKA were acquired preoperatively and two years after surgery [1, 24]. Patients reported outcome measurements independent of any medical staff. Postoperative clinical examination for objective scores was performed by one of the authors, and consisted of the following parameters: presence of patellofemoral crepitus (none, mild, moderate, severe), patellar tenderness (absent or present), presence of a J-sign, and quadriceps strength (M0-M5).
Radiographic assessment
Parameters of interest were: FT, frontal mechanical leg axis, patellar thickness, patellar lateralization, patellar tilt, and tibial tuberosity-trochlear groove (TT-TG) distance.
Radiographs and CT of all included patients were analyzed on a picture archiving and communicating system (PACS) workstation by two independent observers (two orthopedic consultants). Parameters measured as Interclass Correlation Coefficients (ICCs) were calculated to determine the interobserver and intraobserver reproducibility, and are given in the methods section.
CT slice thickness was 2 mm for the proximal femur, 1 mm for the knee and 2 mm for the ankle joint, with increments of 1 mm, 0.5 mm, and 1 mm, respectively. All images were acquired using a clinical 40-slice or 64-slice CT scanner with image reformations using a bone kernel. CT examinations were performed with patients in supine position, with symmetric pelvis and straightened parallel legs.
Measurements (accuracy per pixel: 0.1 mm and 0.1°) were performed in a standardized technique as described in detail below. Regarding clinical relevance, outcome variables are given by one decimal.
Femoral torsion
CT-based measurement of femoral torsion was performed according to the method described by Murphy et al. [31]. Sutter et al. compared mean values and standard deviation of asymptomatic volunteers to patients with femoroacetabular impingement [39]. FT in the control group was 13° ± 10. Based on available data, the cut-off for increased femoral antetorsion was set to 20°. Inter and intrareader ICC for femoral torsion were 0.95 and 0.96 [5, 22, 42, 44].
Frontal mechanical leg axis
On long-leg standing radiographs taken preoperatively and one year after surgery, frontal leg axis was measured as the angle between the mechanical femoral and mechanical tibial axis, according to Strecker et al. [38]. Positive values indicate varus alignment and negative values indicate valgus. Inter and intrareader ICC for the measurement of frontal leg axis were 0.94 and 0.95.
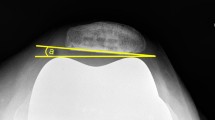
Thickness, lateral displacement and tilt of the patella
The patellar thickness was measured from the anterior surface of the patella to the median ridge at the proximo-distal center of the median ridge, according to Iranpour et al. [21]. Lateral patella displacement was measured according to Zhang et al. (negative values indicating medial displacement) [45]. The patellar tilt was defined as the angle between a line across the posterior condyles and a line at the maximal patellar width, as previously described in various studies [23]. All parameters were measured on preoperative CT. Interreader ICC was 0.94, 0.84 and 0.83 for thickness, lateral displacement and tilt, respectively. Intrareader ICC was 0.95, 0.87 and 0.90, respectively.
Tibial tuberosity—trochlear groove distance
TT-TG measurement was performed on CT scans using the same methodology as described by Dejour [3]. Inter and intrareader ICC for the measurement of TT-TG were both 0.84 and 0.91, respectively.
Statistical analysis
An a priori power analysis (α = 0.05, power level β = 0.90) revealed a minimum sample size of n = 40 (20 per group) to detect a minimum decrease of 5.41 points (minimal clinically important difference) in total HSS score with an increased FT, assuming a mean total HSS score of 95.1 points for satisfied patients after TKA according to Fan et al. [6]. The power analysis was conducted using G*Power (version 3.1; Franz Faull, Universität Kiel).
Descriptive statistics used frequencies and percentages to present the data. All parameters were tested using the Kolmogorov–Smirnov test for normality. When the criteria for normality were met, a 2-tailed paired t test was used. Otherwise, the Wilcoxon signed-rank test was applied. Chi-square test was used for non-parametric data. Spearman/Pearson correlation was used to identify a potential relationship between increased FT and clinical scores. A logistic regression analysis was used for odds ratio between clinical parameters, FT and postoperative coronal leg alignment. The level of significance level was set at a < 0.05. All the statistical analyses were performed using SPSS, version 22 software (SPSS Inc., Chicago, IL).
Ethical aspects.
This prospective age and sex matched case–control study was approved by the Institutional Review Board and the local ethical committee (Zurich Cantonal Ethics Commission, KEK 2019–01749). It was conducted entirely at the authors’ institution. Informed consent was obtained of all patients.
Results
No patient had preoperative patellar instability, and there was no pre or postoperative J-sign. There was no statistically significant difference between clinical scores two years after surgery between patients with normal and excessive FT (Table 1). Kujala score was 64.3 ± 16.7 versus 64.8 ± 14.4 (n.s.), and the patellofemoral score for TKA was 74.3 ± 21 versus 78.5 ± 20.7 (n.s.) for increased FT group and control group, respectively.
There was no correlation between preoperative FT and clinical scores (Table 2) two years after surgery. In the control group, FT was corrected downward more intraoperatively by external rotation of the femoral component (mean 2.8 ± 0.9° versus 2.2 ± 1.7° external rotation), not resulting in any change regarding correlation to clinical scores (Table 3).
All other radiographic parameters were similar between both groups (Table 1), except TT-TG distance which is due to its correlation to FT. Subjects from the control group showed 3.6° more varus preoperatively (n.s.). After surgery, frontal leg axis was more neutrally aligned (difference 1.6°). No correlations of clinical outcomes and preoperative/postoperative frontal leg axis or total leg axis correction were found (all n.s.) (Table 2 and 3). Logistic regression analysis found no lower clinical scores in patients with a postoperative valgus (n.s.) (data not shown).
Discussion
The most important finding of this study is that excessive preoperative FT is not associated with patellofemoral pain or instability following TKA.
Previous reports advocated for restoration of individual patellofemoral tracking with the aim of decreasing the risk of anterior knee pain [14, 15]. As the role of excessive FT in TKA has not yet been explored in literature, the main goal of this prospective study was to answer the question whether excessive FT should be corrected in TKA, as it is increasingly performed in patients with patellofemoral instability [4, 7, 9, 11, 18, 19]. However, no correlation between FT and scores which are specific for the patellofemoral complaints could be found. Moreover, results were independent of the extent to which FT was compensated by means of external rotation of the femur component to balance the gaps.
Other morphologic factors influence patellofemoral tracking such as coronal leg alignment and TT-TG [20]. To date, the most current philosophy is to align the prosthesis guided by individual constitutional phenotype to restore normal knee kinematics and function. Kinematic alignment, as proposed by Howell in 2006, places no restrictions on the patient’s anatomy and post-operative correction [13, 16, 17, 25]. There are, however, reports that postoperative valgus alignment should be avoided [36]. Only in patients with preoperative non-varus alignment, Slevin et al. found a significant correlation between neutral limb alignment and higher clinical scores [36]. Nevertheless, no influence of overall leg alignment on postoperative outcome could be shown in other studies [35]. This is consistent with the here presented data, as no correlation to patellofemoral scores was found despite a significant amount of postoperative valgus knees. Nonetheless, it was demonstrated that femoral valgus alignment negatively affects patellofemoral tracking in that the patella showed increased bone tracer uptake with femoral valgus [37]. Arguably, this effect might be only subclinical if valgus does not exceed 5°—or symptoms are prevented by intraoperative patellar denervation with electrocautery [12, 41].
This study has several limitations. First, preoperative patellofemoral grade of osteoarthritis was not assessed and compared between groups. It would have been interesting to examine the condition of the patellofemoral cartilage intraoperatively to determine the extent to which this affects anterior knee pain. A preoperative MRI was available for 15 patients in the increased FT group and 12 controls only. However, although the results were certainly underpowered, there was no difference between the lateral or medial retropatellar cartilage condition according to the ICRS classification (n.s.). This is in accordance to a recent published paper that found no association between clinical outcomes and visual grading of patellar cartilage degeneration after TKA without patella resurfacing [32]. Furthermore, no postoperative CT scan was available to assess postoperative TT-TG distance, patellar tilt or displacement, which could have confounded the scores. TT-TG distance, for example, is expected to significantly decrease independently of preoperative mechanical leg axis [46]. Further study is however warranted to evaluate alteration of TT-TG distance as a potential cause for postoperative patellofemoral maltracking and pain. This would have gone beyond the scope of this study. Furthermore, it must be added that knowledge and surgical technique of TKA have improved substantially over the past years. Accordingly, the rate of outliers in terms of component placement and postoperative frontal axis deformity has become low, which makes thorough research on this topic somewhat difficult [33]. Finally, standard deviations of clinical scores were higher in this study cohort than those used for the a priori power analysis, implying that this study may still be underpowered. However, given the nearly identical results, no difference is expected in a larger patient cohort.
Conclusion
If the leg axis deformity is corrected to a roughly (± 5°) neutral alignment during cemented TKA, including patellar denervation, then excessive FT was not associated with patellofemoral pain or instability.
References
Baldini A, Anderson JA, Zampetti P, Pavlov H, Sculco TP (2006) A new patellofemoral scoring system for total knee arthroplasty. Clin Orthop Relat Res 452:150–154
Bozic KJ, Kurtz SM, Lau E, Ong K, Chiu V, Vail TP et al (2010) The epidemiology of revision total knee arthroplasty in the United States. Clin Orthop Relat Res 468:45–51
Dejour D, Saggin P (2010) The sulcus deepening trochleoplasty-the Lyon’s procedure. Int Orthop 34:311–316
Dickschas J, Harrer J, Pfefferkorn R, Strecker W (2012) Operative treatment of patellofemoral maltracking with torsional osteotomy. Arch Orthop Trauma Surg 132:289–298
Fabricant PD, Fields KG, Taylor SA, Magennis E, Bedi A, Kelly BT (2015) The effect of femoral and acetabular version on clinical outcomes after arthroscopic femoroacetabular impingement surgery. J Bone Joint Surg Am 97:537–543
Fan XY, Ma JH, Wu X, Xu X, Shi L, Li T et al (2021) How much improvement can satisfy patients? Exploring patients’ satisfaction 3 years after total knee arthroplasty. J Orthop Surg Res 16:389
Flury A, Aregger F, Rahm S, Hoch A, Zingg PO (2022) Subtrochanteric osteotomy in the management of femoral maltorsion results in anteroposterior malcorrection of the greater trochanter: computed simulations of 3D surface models of 100 cadavers. Hip Int. https://doi.org/10.1177/1120700021107104611207000211071046
Flury A, Hoch A, Andronic O, Fritz B, Imhoff FB, Fucentese SF (2021) Increased femoral antetorsion correlates with higher degrees of lateral retropatellar cartilage degeneration, further accentuated in genu valgum. Knee Surg Sports Traumatol Arthrosc 29:1760–1768
Flury A, Hoch A, Hodel S, Imhoff FB, Fucentese SF, Zingg PO (2022) No relevant mechanical leg axis deviation in the frontal and sagittal planes is to be expected after subtrochanteric or supracondylar femoral rotational or derotational osteotomy. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-021-06843-x
Franciozi CE, Ambra LF, Albertoni LJ, Debieux P, Rezende FC, Oliveira MA et al (2017) Increased femoral anteversion influence over surgically treated recurrent patellar instability patients. Arthroscopy 33:633–640
Frings J, Krause M, Akoto R, Wohlmuth P, Frosch KH (2018) Combined distal femoral osteotomy (DFO) in genu valgum leads to reliable patellar stabilization and an improvement in knee function. Knee Surg Sports Traumatol Arthrosc 26:3572–3581
Goicoechea N, Hinarejos P, Torres-Claramunt R, Leal-Blanquet J, Sanchez-Soler J, Monllau JC (2021) Patellar denervation does not reduce post-operative anterior knee pain after primary total knee arthroplasty with patellar resurfacing. Knee Surg Sports Traumatol Arthrosc 29:3346–3351
Gu Y, Roth JD, Howell SM, Hull ML (2014) How frequently do four methods for mechanically aligning a total knee arthroplasty cause collateral ligament imbalance and change alignment from normal in white patients? AAOS exhibit selection. J Bone Joint Surg Am 96:e101
Hochreiter B, Hirschmann MT, Amsler F, Behrend H (2019) Highly variable tibial tubercle-trochlear groove distance (TT-TG) in osteoarthritic knees should be considered when performing TKA. Knee Surg Sports Traumatol Arthrosc 27:1403–1409
Hochreiter B, Moser LB, Hess S, Hirschmann MT, Amsler F, Behrend H (2021) Osteoarthritic knees have a highly variable patellofemoral alignment: a systematic review. Knee Surg Sports Traumatol Arthrosc 29:483–490
Howell SM, Howell SJ, Kuznik KT, Cohen J, Hull ML (2013) Does a kinematically aligned total knee arthroplasty restore function without failure regardless of alignment category? Clin Orthop Relat Res 471:1000–1007
Howell SM, Shelton TJ, Hull ML (2018) Implant survival and function ten years after kinematically aligned total knee arthroplasty. J Arthroplasty 33:3678–3684
Imhoff FB, Beitzel K, Zakko P, Obopilwe E, Voss A, Scheiderer B et al (2018) Derotational osteotomy of the distal femur for the treatment of patellofemoral instability simultaneously leads to the correction of frontal alignment: a laboratory cadaveric study. Orthop J Sports Med 6:2325967118775664
Imhoff FB, Cotic M, Liska F, Dyrna FGE, Beitzel K, Imhoff AB et al (2019) Derotational osteotomy at the distal femur is effective to treat patients with patellar instability. Knee Surg Sports Traumatol Arthrosc 27:652–658
Imhoff FB, Funke V, Muench LN, Sauter A, Englmaier M, Woertler K et al (2020) The complexity of bony malalignment in patellofemoral disorders: femoral and tibial torsion, trochlear dysplasia, TT-TG distance, and frontal mechanical axis correlate with each other. Knee Surg Sports Traumatol Arthrosc 28:897–904
Iranpour F, Merican AM, Amis AA, Cobb JP (2008) The width:thickness ratio of the patella: an aid in knee arthroplasty. Clin Orthop Relat Res 466:1198–1203
Ito K, Minka MA 2nd, Leunig M, Werlen S, Ganz R (2001) Femoroacetabular impingement and the cam-effect. A MRI-based quantitative anatomical study of the femoral head-neck offset. J Bone Joint Surg Br 83:171–176
Jibri Z, Jamieson P, Rakhra KS, Sampaio ML, Dervin G (2019) Patellar maltracking: an update on the diagnosis and treatment strategies. Insights Imaging 10:65
Kujala UM, Jaakkola LH, Koskinen SK, Taimela S, Hurme M, Nelimarkka O (1993) Scoring of patellofemoral disorders. Arthrosc J Arthrosc Relat Surg 9:159–163
Lee YS, Howell SM, Won YY, Lee OS, Lee SH, Vahedi H et al (2017) Kinematic alignment is a possible alternative to mechanical alignment in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 25:3467–3479
Macri EM, Felson DT, Ziegler ML, Cooke TDV, Guermazi A, Roemer FW et al (2019) The association of frontal plane alignment to MRI-defined worsening of patellofemoral osteoarthritis: the MOST study. Osteoarthr Cartil 27:459–467
Martin Beck CB, Bernard Christen, Vilijam Zdravkovic (2021) Swiss National Hip & Knee Joint Registry - Report 2021 - Annual Report of the SIRIS Registry, Hip & Knee, 2012 – 2020
Martin Beck CB, Bernhard Christen, Vilijam Zdravkovic (2020) Swiss National Hip & Knee Joint Registry - Report 2020 - Annual Report of the SIRIS Registry, Hip & Knee, 2012 – 2019
Matz J, Lanting BA, Howard JL (2019) Understanding the patellofemoral joint in total knee arthroplasty. Can J Surg 62:57–65
Merican AM, Ghosh KM, Iranpour F, Deehan DJ, Amis AA (2011) The effect of femoral component rotation on the kinematics of the tibiofemoral and patellofemoral joints after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 19:1479–1487
Murphy SB, Simon SR, Kijewski PK, Wilkinson RH, Griscom NT (1987) Femoral anteversion. JBJS 69:1169–1176
Park HJ, Chang MJ, Kim TW, Chang CB, Kang KS, Kang SB (2021) Subchondral bone condition and intraoperative grading of cartilage degeneration underneath patella unrelated to the clinical outcome after TKA with unresurfaced patella. J Knee Surg. https://doi.org/10.1055/s-0041-1723980
Rahm S, Camenzind RS, Hingsammer A, Lenz C, Bauer DE, Farshad M et al (2017) Postoperative alignment of TKA in patients with severe preoperative varus or valgus deformity: is there a difference between surgical techniques? BMC Musculoskelet Disord 18:272
Sharkey PF, Lichstein PM, Shen C, Tokarski AT, Parvizi J (2014) Why are total knee arthroplasties failing today–has anything changed after 10 years? J Arthroplasty 29:1774–1778
Slevin O, Amsler F, Hirschmann MT (2017) No correlation between coronal alignment of total knee arthroplasty and clinical outcomes: a prospective clinical study using 3D-CT. Knee Surg Sports Traumatol Arthrosc 25:3892–3900
Slevin O, Hirschmann A, Schiapparelli FF, Amsler F, Huegli RW, Hirschmann MT (2018) Neutral alignment leads to higher knee society scores after total knee arthroplasty in preoperatively non-varus patients: a prospective clinical study using 3D-CT. Knee Surg Sports Traumatol Arthrosc 26:1602–1609
Slevin O, Schmid FA, Schiapparelli FF, Rasch H, Amsler F, Hirschmann MT (2017) Coronal femoral TKA position significantly influences in vivo patellar loading in unresurfaced patellae after primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 25:3605–3610
Strecker W (2006) Planning analysis of knee-adjacent deformities. I. Frontal plane deformities Oper Orthop Traumatol 18:259–272
Sutter R, Dietrich TJ, Zingg PO, Pfirrmann CW (2012) Femoral antetorsion: comparing asymptomatic volunteers and patients with femoroacetabular impingement. Radiology 263:475–483
Thiele K, Perka C, Matziolis G, Mayr HO, Sostheim M, Hube R (2015) Current failure mechanisms after knee arthroplasty have changed: polyethylene wear is less common in revision surgery. J Bone Joint Surg Am 97:715–720
Thiengwittayaporn S, Tangtrakul P, Hongku N, Tunyasuwanakul R (2021) Patellar denervation reduces postoperative anterior knee pain after patellar resurfacing total knee arthroplasty: a randomized controlled trial. J Arthroplasty 36:1295–1301
Toogood PA, Skalak A, Cooperman DR (2009) Proximal femoral anatomy in the normal human population. Clin Orthop Relat Res 467:876–885
van Jonbergen HP, Reuver JM, Mutsaerts EL, Poolman RW (2014) Determinants of anterior knee pain following total knee replacement: a systematic review. Knee Surg Sports Traumatol Arthrosc 22:478–499
Wells J, Nepple JJ, Crook K, Ross JR, Bedi A, Schoenecker P et al (2017) Femoral morphology in the dysplastic hip: three-dimensional characterizations with CT. Clin Orthop Relat Res 475:1045–1054
Zhang LK, Wang XM, Niu YZ, Liu HX, Wang F (2016) Relationship between patellar tracking and the “Screw-home” mechanism of tibiofemoral joint. Orthop Surg 8:490–495
Zimmermann SM, Scherrer Y, Zaleski M, Jentzsch T, Fucentese SF (2022) Decrease of tibial tuberosity trochlear groove distance following mechanically aligned total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-022-06952-1
Funding
Open access funding provided by University of Zurich. The authors received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Contributions
FA and HA: researched literature and conceived the study. FA, HA, NK and FSF: protocol development and gaining ethical approval. HA, NK and GC: patient recruitment. FA, SH and GC: radiological assessment. FA, SH, VL and ZS: data analysis. FA wrote the first draft of the manuscript. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Ethical approval
Ethical approval for this study was obtained from Zurich Cantonal Ethics Comission: KEK 2019-01749.
Informed consent
Written informed consent was obtained from all subjects before the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Flury, A., Hoch, A., Cirigliano, G. et al. Excessive femoral torsion is not associated with patellofemoral pain or instability if TKA is functionally aligned and the patella denervated. Knee Surg Sports Traumatol Arthrosc 31, 3665–3671 (2023). https://doi.org/10.1007/s00167-022-07162-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-022-07162-5