Abstract
The prevalence of obesity has reached pandemic proportions, and now approximately 25% of adults in Westernized countries have obesity. Recognized as a major health concern, obesity is associated with multiple comorbidities, particularly cardiometabolic disorders. In this Review, we present obesity as an evolutionarily novel condition, summarize the epidemiological evidence on its detrimental cardiometabolic consequences and discuss the major mechanisms involved in the association between obesity and the risk of cardiometabolic diseases. We also examine the role of potential moderators of this association, with evidence for and against the so-called ‘metabolically healthy obesity phenotype’, the ‘fatness but fitness’ paradox or the ‘obesity paradox’. Although maintenance of optimal cardiometabolic status should be a primary goal in individuals with obesity, losing body weight and, particularly, excess visceral adiposity seems to be necessary to minimize the risk of cardiometabolic diseases.
Key points
-
Obesity has reached pandemic proportions, which in turn has led to an increase in the risk of concomitant cardiometabolic conditions.
-
Obesity is an evolutionary mismatch between our ancient, genetically determined physiology and the modern diet and lifestyle; not only did we not evolve to have obesity but we never evolved to cope with its numerous associated maladaptations, such as massive adipocyte hypertrophy to accommodate excess fat.
-
Obesity is associated with both excess quantity and dysfunction of white adipose tissue, particularly visceral adipose depots.
-
‘Metabolically healthy obesity’ often reflects a transitionary stage to an unhealthy phenotype.
-
Sustained body weight control in individuals with obesity improves their cardiometabolic risk status.



Similar content being viewed by others
References
NCD Risk Factor Collaboration Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19.2 million participants. Lancet 387, 1377–1396 (2016).
GBD 2015 Obesity Collaborators. Health effects of overweight and obesity in 195 countries over 25 years. N. Engl. J. Med. 377, 13–27 (2017).
Hales, C. M., Carroll, M. D., Fryar, C. D. & Ogden, C. L. NCHS Data Brief No. 360: Prevalence of obesity and severe obesity among adults: United States, 2017–2018 https://www.cdc.gov/nchs/data/databriefs/db360-h.pdf (2020).
World Health Organization. WHO European Regional Obesity Report 2022. https://apps.who.int/iris/bitstream/handle/10665/353747/9789289057738-eng.pdf (2022).
Templin, T. et al. The overweight and obesity transition from the wealthy to the poor in low- and middle-income countries: a survey of household data from 103 countries. PLoS Med. 16, e1002968 (2019).
Dai, H. et al. The global burden of disease attributable to high body mass index in 195 countries and territories, 1990-2017: an analysis of the Global Burden of Disease study. PLoS Med. 17, e1003198 (2020).
Global BMI Mortality Collaboration. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet 388, 776–786 (2016).
Santos-Lozano, A. et al. Implications of obesity in exceptional longevity. Ann. Transl. Med. 4, 416 (2016).
Kivimaki, M. et al. Body-mass index and risk of obesity-related complex multimorbidity: an observational multicohort study. Lancet Diabetes Endocrinol. 10, 253–263 (2022).
Powell-Wiley, T. M. et al. Obesity and cardiovascular disease: a scientific statement from the American Heart Association. Circulation 143, e984–e1010 (2021).
Kivimaki, M. et al. Overweight, obesity, and risk of cardiometabolic multimorbidity: pooled analysis of individual-level data for 120 813 adults from 16 cohort studies from the USA and Europe. Lancet Public Health 2, e277–e285 (2017).
Kim, M. S. et al. Association between adiposity and cardiovascular outcomes: an umbrella review and meta-analysis of observational and Mendelian randomization studies. Eur. Heart J. 42, 3388–3403 (2021).
Tomiyama, A. J. et al. How and why weight stigma drives the obesity ‘epidemic’ and harms health. BMC Med. 16, 123 (2018).
Puhl, R. & Suh, Y. Health consequences of weight stigma: implications for obesity prevention and treatment. Curr. Obes. Rep. 4, 182–190 (2015).
Phelan, S. M. et al. Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obes. Rev. 16, 319–326 (2015).
Ford, N. D., Patel, S. A. & Narayan, K. M. Obesity in low- and middle-income countries: burden, drivers, and emerging challenges. Annu. Rev. Public Health 38, 145–164 (2017).
Song, X. et al. Obesity attenuates gender differences in cardiovascular mortality. Cardiovasc. Diabetol. 13, 144 (2014).
Mongraw-Chaffin, M. L., Peters, S. A. E., Huxley, R. R. & Woodward, M. The sex-specific association between BMI and coronary heart disease: a systematic review and meta-analysis of 95 cohorts with 1·2 million participants. Lancet Diabetes Endocrinol. 3, 437–449 (2015).
Kammerlander, A. A. et al. Sex differences in the associations of visceral adipose tissue and cardiometabolic and cardiovascular disease risk: the framingham heart study. J. Am. Heart Assoc. 10, e019968 (2021).
National Research Council. Body Composition in Animals and Man (eds Breidenstein Reid, B. C., Hansard, S. L., Stenaker, H. H. & Zobrisky, S. E.) 45e70 (National Research Council of National Academy of Sciences, 1968).
Speakman, J. R. Evolutionary perspectives on the obesity epidemic: adaptive, maladaptive, and neutral viewpoints. Annu. Rev. Nutr. 33, 289–317 (2013).
Kaplan, H., Hill, K., Lancaster, J. & Hurtado, A. M. A theory of human life history evolution: diet, intelligence, and longevity. Evolut. Anthropol. 9, 156–185 (2000).
van Raaij, J. M., Schonk, C. M., Vermaat-Miedema, S. H., Peek, M. E. & Hautvast, J. G. Energy cost of lactation, and energy balances of well-nourished Dutch lactating women: reappraisal of the extra energy requirements of lactation. Am. J. Clin. Nutr. 53, 612–619 (1991).
Raichlen, D. A. & Lieberman, D. E. The evolution of human step counts and its association with the risk of chronic disease. Curr. Biol. 32, R1206–R1214 (2022).
Eaton, S. B., Konner, M. & Shostak, M. Stone agers in the fast lane: chronic degenerative diseases in evolutionary perspective. Am. J. Med. 84, 739–749 (1988).
Raichlen, D. A. et al. Physical activity patterns and biomarkers of cardiovascular disease risk in hunter-gatherers. Am. J. Hum. Biol. 29, 22919 (2017).
Truswell, A. S. & Hansen, J.D.L. in Kalahari Hunter-Gatherers (ed. Lee, R.B. & DeVore, I.) 166–194 (1976).
Pontzer, H., Wood, B. M. & Raichlen, D. A. Hunter-gatherers as models in public health. Obes. Rev. 19, 24–35 (2018).
Johnson, R. J., Lanaspa, M. A. & Fox, J. W. Upper paleolithic figurines showing women with obesity may represent survival symbols of climatic change. Obesity 29, 11–15 (2021).
Walker, R. et al. Growth rates and life histories in twenty-two small-scale societies. Am. J. Hum. Biol. 18, 295–311 (2006).
Gurven, M., Jaeggi, A. V., Kaplan, H. & Cummings, D. Physical activity and modernization among Bolivian Amerindians. PLoS ONE 8, e55679 (2013).
Lindeberg, S., Nilsson-Ehle, P., Terent, A., Vessby, B. & Schersten, B. Cardiovascular risk factors in a Melanesian population apparently free from stroke and ischaemic heart disease: the Kitava study. J. Intern. Med. 236, 331–340 (1994).
Carvalho, J. J. et al. Blood pressure in four remote populations in the INTERSALT study. Hypertension 14, 238–246 (1989).
Little, M. A., Galvin, K. & Mugambi, M. Cross-sectional growth of nomadic Turkana pastoralists. Hum. Biol. 55, 811–830 (1983).
Mbalilaki, J. A. et al. Daily energy expenditure and cardiovascular risk in Masai, rural and urban Bantu Tanzanians. Br. J. Sports Med. 44, 121–126 (2010).
Kaplan, H. et al. Coronary atherosclerosis in indigenous South American Tsimane: a cross-sectional cohort study. Lancet 389, 1730–1739 (2017).
Carrera-Bastos, P. et al. C-reactive protein in traditional melanesians on Kitava. BMC Cardiovasc. Disord. 20, 524 (2020).
Floud, R., Fogel, R. W., Harris, B. & Hong, S. K. The Changing Body: Health, Nutrition, and Human Development in the Western World since 1700 (Cambridge Univ. Press, 2011).
Lieberman, D. E. The Story of the Human Body: Evolution, Health and Disease (Pantheon, 2013).
Cypess, A. M. Reassessing human adipose tissue. N. Engl. J. Med. 386, 768–779 (2022).
Becher, T. et al. Brown adipose tissue is associated with cardiometabolic health. Nat. Med. 27, 58–65 (2021).
Nabasenja, C., Barry, K., Nelson, T., Chandler, A. & Hewis, J. Imaging individuals with obesity. J. Med. Imaging Radiat. Sci. 53, 291–304 (2022).
Neeland, I. J., Yokoo, T., Leinhard, O. D. & Lavie, C. J. 21st century advances in multimodality imaging of obesity for care of the cardiovascular patient. JACC Cardiovasc. Imaging 14, 482–494 (2021).
Fox, C. S. et al. Abdominal visceral and subcutaneous adipose tissue compartments: association with metabolic risk factors in the Framingham Heart Study. Circulation 116, 39–48 (2007).
Neeland, I. J. et al. Body fat distribution and incident cardiovascular disease in obese adults. J. Am. Coll. Cardiol. 65, 2150–2151 (2015).
Neeland, I. J. et al. Associations of visceral and abdominal subcutaneous adipose tissue with markers of cardiac and metabolic risk in obese adults. Obesity 21, E439–E447 (2013).
Shah, R. V. et al. Visceral adiposity and the risk of metabolic syndrome across body mass index: the MESA Study. JACC Cardiovasc. Imaging 7, 1221–1235 (2014).
Liu, J. et al. Impact of abdominal visceral and subcutaneous adipose tissue on cardiometabolic risk factors: the Jackson Heart Study. J. Clin. Endocrinol. Metab. 95, 5419–5426 (2010).
Linge, J. et al. Body composition profiling in the UK Biobank imaging study. Obesity 26, 1785–1795 (2018).
Lee, J. J., Pedley, A., Hoffmann, U., Massaro, J. M. & Fox, C. S. Association of changes in abdominal fat quantity and quality with incident cardiovascular disease risk factors. J. Am. Coll. Cardiol. 68, 1509–1521 (2016).
Neeland, I. J., Grundy, S. M., Li, X., Adams-Huet, B. & Vega, G. L. Comparison of visceral fat mass measurement by dual-X-ray absorptiometry and magnetic resonance imaging in a multiethnic cohort: the Dallas Heart Study. Nutr. Diabetes 6, e221 (2016).
Kaul, S. et al. Dual-energy X-ray absorptiometry for quantification of visceral fat. Obesity 20, 1313–1318 (2012).
Borga, M. et al. Advanced body composition assessment: from body mass index to body composition profiling. J. Investig. Med. 66, 1–9 (2018).
Schlecht, I. et al. Reproducibility and validity of ultrasound for the measurement of visceral and subcutaneous adipose tissues. Metabolism 63, 1512–1519 (2014).
Cypess, A. M. et al. Identification and importance of brown adipose tissue in adult humans. N. Engl. J. Med. 360, 1509–1517 (2009).
Chen, K. Y. et al. Brown adipose reporting criteria in imaging studies (BARCIST 1.0): recommendations for standardized FDG-PET/CT experiments in humans. Cell Metab. 24, 210–222 (2016).
Kulterer, O. C. et al. Brown adipose tissue prevalence is lower in obesity but its metabolic activity is intact. Front. Endocrinol. 13, 858417 (2022).
Ruiz, J. R. et al. Role of human brown fat in obesity, metabolism and cardiovascular disease: strategies to turn up the heat. Prog. Cardiovasc. Dis. 61, 232–245 (2018).
Sun, L. et al. Brown adipose tissue: multimodality evaluation by PET, MRI, infrared thermography, and whole-body calorimetry (TACTICAL-II). Obesity 27, 1434–1442 (2019).
Nirengi, S. et al. An optimal condition for the evaluation of human brown adipose tissue by infrared thermography. PLoS ONE 14, e0220574 (2019).
Ang, Q. Y. et al. A new method of infrared thermography for quantification of brown adipose tissue activation in healthy adults (TACTICAL): a randomized trial. J. Physiol. Sci. 67, 395–406 (2017).
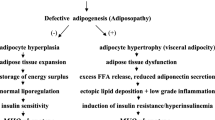
Gustafson, B., Hedjazifar, S., Gogg, S., Hammarstedt, A. & Smith, U. Insulin resistance and impaired adipogenesis. Trends Endocrinol. Metab. 26, 193–200 (2015).
Laforest, S., Labrecque, J., Michaud, A., Cianflone, K. & Tchernof, A. Adipocyte size as a determinant of metabolic disease and adipose tissue dysfunction. Crit. Rev. Clin. Lab. Sci. 52, 301–313 (2015).
Ryden, M., Andersson, D. P., Bergstrom, I. B. & Arner, P. Adipose tissue and metabolic alterations: regional differences in fat cell size and number matter, but differently: a cross-sectional study. J. Clin. Endocrinol. Metab. 99, E1870–E1876 (2014).
Hoffstedt, J. et al. Regional impact of adipose tissue morphology on the metabolic profile in morbid obesity. Diabetologia 53, 2496–2503 (2010).
McLaughlin, T. et al. Enhanced proportion of small adipose cells in insulin-resistant vs insulin-sensitive obese individuals implicates impaired adipogenesis. Diabetologia 50, 1707–1715 (2007).
Kim, J. Y. et al. Obesity-associated improvements in metabolic profile through expansion of adipose tissue. J. Clin. Invest. 117, 2621–2637 (2007).
Abreu-Vieira, G. et al. Cidea improves the metabolic profile through expansion of adipose tissue. Nat. Commun. 6, 7433 (2015).
Ahmadian, M. et al. PPARgamma signaling and metabolism: the good, the bad and the future. Nat. Med. 19, 557–566 (2013).
Hammarstedt, A. et al. WISP2 regulates preadipocyte commitment and PPARgamma activation by BMP4. Proc. Natl Acad. Sci. USA 110, 2563–2568 (2013).
Gustafson, B., Hammarstedt, A., Hedjazifar, S. & Smith, U. Restricted adipogenesis in hypertrophic obesity: the role of WISP2, WNT, and BMP4. Diabetes 62, 2997–3004 (2013).
Majithia, A. R. et al. Rare variants in PPARG with decreased activity in adipocyte differentiation are associated with increased risk of type 2 diabetes. Proc. Natl Acad. Sci. USA 111, 13127–13132 (2014).
Mozaffarian, D., Hao, T., Rimm, E. B., Willett, W. C. & Hu, F. B. Changes in diet and lifestyle and long-term weight gain in women and men. N. Engl. J. Med. 364, 2392–2404 (2011).
Virtue, S. & Vidal-Puig, A. Adipose tissue expandability, lipotoxicity and the metabolic syndrome—an allostatic perspective. Biochim. Biophys. Acta 1801, 338–349 (2010).
Shungin, D. et al. New genetic loci link adipose and insulin biology to body fat distribution. Nature 518, 187–196 (2015).
De Fano, M. et al. Adipose tissue plasticity in response to pathophysiological cues: a connecting link between obesity and its associated comorbidities. Int. J. Mol. Sci. 23, 5511 (2022).
Sethi, J. K. Activatin’ human adipose progenitors in obesity. Diabetes 59, 2354–2357 (2010).
Porter, S. A. et al. Abdominal subcutaneous adipose tissue: a protective fat depot? Diabetes Care 32, 1068–1075 (2009).
Neeland, I. J. et al. Visceral and ectopic fat, atherosclerosis, and cardiometabolic disease: a position statement. Lancet Diabetes Endocrinol. 7, 715–725 (2019).
Corvera, S., Solivan-Rivera, J. & Yang Loureiro, Z. Angiogenesis in adipose tissue and obesity. Angiogenesis 25, 439–453 (2022).
Hammarstedt, A., Gogg, S., Hedjazifar, S., Nerstedt, A. & Smith, U. Impaired adipogenesis and dysfunctional adipose tissue in human hypertrophic obesity. Physiol. Rev. 98, 1911–1941 (2018).
Imbeault, P. et al. Relationship of visceral adipose tissue to metabolic risk factors for coronary heart disease: is there a contribution of subcutaneous fat cell hypertrophy? Metabolism 48, 355–362 (1999).
Cotillard, A. et al. Adipocyte size threshold matters: link with risk of type 2 diabetes and improved insulin resistance after gastric bypass. J. Clin. Endocrinol. Metab. 99, E1466–E1470 (2014).
Landgraf, K. et al. Evidence of early alterations in adipose tissue biology and function and its association with obesity-related inflammation and insulin resistance in children. Diabetes 64, 1249–1261 (2015).
Arner, E. et al. Adipocyte turnover: relevance to human adipose tissue morphology. Diabetes 59, 105–109 (2010).
Suarez-Cuenca, J. A. et al. Enlarged adipocytes from subcutaneous vs. visceral adipose tissue differentially contribute to metabolic dysfunction and atherogenic risk of patients with obesity. Sci. Rep. 11, 1831 (2021).
Henninger, A. M., Eliasson, B., Jenndahl, L. E. & Hammarstedt, A. Adipocyte hypertrophy, inflammation and fibrosis characterize subcutaneous adipose tissue of healthy, non-obese subjects predisposed to type 2 diabetes. PLoS ONE 9, e105262 (2014).
Rosenquist, K. J. et al. Visceral and subcutaneous fat quality and cardiometabolic risk. JACC Cardiovasc. Imaging 6, 762–771 (2013).
Gealekman, O. et al. Depot-specific differences and insufficient subcutaneous adipose tissue angiogenesis in human obesity. Circulation 123, 186–194 (2011).
Paavonsalo, S., Hariharan, S., Lackman, M. H. & Karaman, S. Capillary rarefaction in obesity and metabolic diseases-organ-specificity and possible mechanisms. Cells 9, 2683 (2020).
Spencer, M. et al. Adipose tissue extracellular matrix and vascular abnormalities in obesity and insulin resistance. J. Clin. Endocrinol. Metab. 96, E1990–E1998 (2011).
Pasarica, M. et al. Reduced adipose tissue oxygenation in human obesity: evidence for rarefaction, macrophage chemotaxis, and inflammation without an angiogenic response. Diabetes 58, 718–725 (2009).
Belligoli, A. et al. Characterization of subcutaneous and omental adipose tissue in patients with obesity and with different degrees of glucose impairment. Sci. Rep. 9, 11333 (2019).
Cao, Y. Angiogenesis and vascular functions in modulation of obesity, adipose metabolism, and insulin sensitivity. Cell Metab. 18, 478–489 (2013).
Goossens, G. H. et al. Increased adipose tissue oxygen tension in obese compared with lean men is accompanied by insulin resistance, impaired adipose tissue capillarization, and inflammation. Circulation 124, 67–76 (2011).
Zhang, M., Hu, T., Zhang, S. & Zhou, L. Associations of different adipose tissue depots with insulin resistance: a systematic review and meta-analysis of observational studies. Sci. Rep. 5, 18495 (2015).
Neeland, I. J. et al. Dysfunctional adiposity and the risk of prediabetes and type 2 diabetes in obese adults. JAMA 308, 1150–1159 (2012).
Nicklas, B. J. et al. Visceral adipose tissue cutoffs associated with metabolic risk factors for coronary heart disease in women. Diabetes Care 26, 1413–1420 (2003).
Cifarelli, V. et al. Decreased adipose tissue oxygenation associates with insulin resistance in individuals with obesity. J. Clin. Invest. 130, 6688–6699 (2020).
Chait, A. & den Hartigh, L. J. Adipose tissue distribution, inflammation and its metabolic consequences, including diabetes and cardiovascular disease. Front. Cardiovasc. Med. 7, 22 (2020).
Halberg, N. et al. Hypoxia-inducible factor 1alpha induces fibrosis and insulin resistance in white adipose tissue. Mol. Cell Biol. 29, 4467–4483 (2009).
Vasamsetti, S. B., Natarajan, N., Sadaf, S., Florentin, J. & Dutta, P. Regulation of cardiovascular health and disease by visceral adipose tissue-derived metabolic hormones. J. Physiol. https://doi.org/10.1113/JP282728 (2022).
Furman, D. et al. Chronic inflammation in the etiology of disease across the life span. Nat. Med. 25, 1822–1832 (2019).
Park, H. S., Park, J. Y. & Yu, R. Relationship of obesity and visceral adiposity with serum concentrations of CRP, TNF-alpha and IL-6. Diabetes Res. Clin. Pract. 69, 29–35 (2005).
Valenzuela, P. L. et al. Lifestyle interventions for the prevention and treatment of hypertension. Nat. Rev. Cardiol. 18, 251–275 (2021).
Hall, J. E., do Carmo, J. M., da Silva, A. A., Wang, Z. & Hall, M. E. Obesity, kidney dysfunction and hypertension: mechanistic links. Nat. Rev. Nephrol. 15, 367–385 (2019).
Chandra, A. et al. The relationship of body mass and fat distribution with incident hypertension: observations from the Dallas Heart Study. J. Am. Coll. Cardiol. 64, 997–1002 (2014).
Mirzababaei, A., Mozaffari, H., Shab-Bidar, S., Milajerdi, A. & Djafarian, K. Risk of hypertension among different metabolic phenotypes: a systematic review and meta-analysis of prospective cohort studies. J. Hum. Hypertens. 33, 365–377 (2019).
Grassi, G. et al. Sympathetic neural overdrive in the obese and overweight state. Hypertension 74, 349–358 (2019).
Kalil, G. Z. & Haynes, W. G. Sympathetic nervous system in obesity-related hypertension: mechanisms and clinical implications. Hypertens. Res. 35, 4–16 (2012).
Raheem, J. et al. Visceral adiposity is associated with metabolic profiles predictive of type 2 diabetes and myocardial infarction. Commun. Med. 2, 81 (2022).
Parikh, N. I. et al. Visceral and subcutaneous adiposity and brachial artery vasodilator function. Obesity 17, 2054–2059 (2009).
Fuster, J. J., Ouchi, N., Gokce, N. & Walsh, K. Obesity-induced changes in adipose tissue microenvironment and their impact on cardiovascular disease. Circ. Res. 118, 1786–1807 (2016).
Matacchione, G. et al. Senescent macrophages in the human adipose tissue as a source of inflammaging. Geroscience 44, 1941–1960 (2022).
Antonopoulos, A. S. & Antoniades, C. The role of epicardial adipose tissue in cardiac biology: classic concepts and emerging roles. J. Physiol. 595, 3907–3917 (2017).
Nabati, M. et al. Epicardial adipose tissue and its association with cardiovascular risk factors and mitral annular calcium deposits. Ultrasound 27, 217–224 (2019).
Scarano Pereira, J. P. et al. Epicardial adipose tissue, obesity, and the occurrence of atrial fibrillation: an overview of pathophysiology and treatment methods. Expert. Rev. Cardiovasc. Ther. 20, 307–322 (2022).
Packer, M. Disease-treatment interactions in the management of patients with obesity and diabetes who have atrial fibrillation: the potential mediating influence of epicardial adipose tissue. Cardiovasc. Diabetol. 18, 121 (2019).
Wang, T. J. et al. Obesity and the risk of new-onset atrial fibrillation. JAMA 292, 2471–2477 (2004).
Packer, M. The epicardial adipose inflammatory triad: coronary atherosclerosis, atrial fibrillation, and heart failure with a preserved ejection fraction. Eur. J. Heart Fail. 20, 1567–1569 (2018).
Sinha, S. K. et al. Epicardial adipose tissue thickness and its association with the presence and severity of coronary artery disease in clinical setting: a cross-sectional observational study. J. Clin. Med. Res. 8, 410–419 (2016).
McKenney-Drake, M. L. et al. Epicardial adipose tissue removal potentiates outward remodeling and arrests coronary atherogenesis. Ann. Thorac. Surg. 103, 1622–1630 (2017).
Packer, M. Epicardial adipose tissue may mediate deleterious effects of obesity and inflammation on the myocardium. J. Am. Coll. Cardiol. 71, 2360–2372 (2018).
Ardissino, M. et al. Pericardial adiposity is independently linked to adverse cardiovascular phenotypes: a CMR study of 42 598 UK Biobank participants. Eur. Heart J. Cardiovasc. Imaging 23, 1471–1481 (2022).
Hachiya, R., Tanaka, M., Itoh, M. & Suganami, T. Molecular mechanism of crosstalk between immune and metabolic systems in metabolic syndrome. Inflamm. Regen. 42, 13 (2022).
Ito, A. et al. Role of CC chemokine receptor 2 in bone marrow cells in the recruitment of macrophages into obese adipose tissue. J. Biol. Chem. 283, 35715–35723 (2008).
Weisberg, S. P. et al. CCR2 modulates inflammatory and metabolic effects of high-fat feeding. J. Clin. Invest. 116, 115–124 (2006).
Kamei, N. et al. Overexpression of monocyte chemoattractant protein-1 in adipose tissues causes macrophage recruitment and insulin resistance. J. Biol. Chem. 281, 26602–26614 (2006).
Kanda, H. et al. MCP-1 contributes to macrophage infiltration into adipose tissue, insulin resistance, and hepatic steatosis in obesity. J. Clin. Invest. 116, 1494–1505 (2006).
Lancaster, G. I. et al. Evidence that TLR4 is not a receptor for saturated fatty acids but mediates lipid-induced inflammation by reprogramming macrophage metabolism. Cell Metab. 27, 1096–1110.e5 (2018).
Suganami, T. et al. Attenuation of obesity-induced adipose tissue inflammation in C3H/HeJ mice carrying a Toll-like receptor 4 mutation. Biochem. Biophys. Res. Commun. 354, 45–49 (2007).
Iwasaki, Y. et al. Activating transcription factor 4 links metabolic stress to interleukin-6 expression in macrophages. Diabetes 63, 152–161 (2014).
Swanson, K. V., Deng, M. & Ting, J. P. The NLRP3 inflammasome: molecular activation and regulation to therapeutics. Nat. Rev. Immunol. 19, 477–489 (2019).
Vandanmagsar, B. et al. The NLRP3 inflammasome instigates obesity-induced inflammation and insulin resistance. Nat. Med. 17, 179–188 (2011).
Xu, H. et al. Chronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistance. J. Clin. Invest. 112, 1821–1830 (2003).
Plomgaard, P. et al. Tumor necrosis factor-alpha induces skeletal muscle insulin resistance in healthy human subjects via inhibition of Akt substrate 160 phosphorylation. Diabetes 54, 2939–2945 (2005).
Efthymiou, V. & Patti, M. E. It is not just fat: dissecting the heterogeneity of adipose tissue function. Curr. Diab. Rep. 22, 177–187 (2022).
Lenz, M., Arts, I. C. W., Peeters, R. L. M., de Kok, T. M. & Ertaylan, G. Adipose tissue in health and disease through the lens of its building blocks. Sci. Rep. 10, 10433 (2020).
Vijay, J. et al. Single-cell analysis of human adipose tissue identifies depot and disease specific cell types. Nat. Metab. 2, 97–109 (2020).
Bruno, M. E. C. et al. Accumulation of gammadelta T cells in visceral fat with aging promotes chronic inflammation. Geroscience 44, 1761–1778 (2022).
Fruhbeck, G. et al. Increased levels of interleukin-36 in obesity and type 2 diabetes fuel adipose tissue inflammation by inducing its own expression and release by adipocytes and macrophages. Front. Immunol. 13, 832185 (2022).
Li, G. et al. Transcriptome of visceral adipose tissue identifies an inflammation-related ceRNA network that regulates obesity. Mol. Cell Biochem. 477, 1095–1106 (2022).
Murano, I. et al. Dead adipocytes, detected as crown-like structures, are prevalent in visceral fat depots of genetically obese mice. J. Lipid Res. 49, 1562–1568 (2008).
Cinti, S. et al. Adipocyte death defines macrophage localization and function in adipose tissue of obese mice and humans. J. Lipid Res. 46, 2347–2355 (2005).
Olona, A. et al. Adipoclast: a multinucleated fat-eating macrophage. BMC Biol. 19, 246 (2021).
Malavazos, A. E. et al. The density of crown-like structures in epicardial adipose tissue could play a role in cardiovascular diseases. Eat. Weight Disord. 27, 2905–2910 (2022).
Ichioka, M. et al. Increased expression of macrophage-inducible C-type lectin in adipose tissue of obese mice and humans. Diabetes 60, 819–826 (2011).
Tanaka, M. et al. Macrophage-inducible C-type lectin underlies obesity-induced adipose tissue fibrosis. Nat. Commun. 5, 4982 (2014).
Henningsen, J. B. & Scheele, C. Brown adipose tissue: a metabolic regulator in a hypothalamic cross talk? Annu. Rev. Physiol. 83, 279–301 (2021).
Carobbio, S., Guenantin, A. C., Samuelson, I., Bahri, M. & Vidal-Puig, A. Brown and beige fat: from molecules to physiology and pathophysiology. Biochim. Biophys. Acta Mol. Cell Biol. Lipids 1864, 37–50 (2019).
Carpentier, A. C., Blondin, D. P., Haman, F. & Richard, D. Brown adipose tissue – a translational perspective. Endocr. Rev. https://doi.org/10.1210/endrev/bnac015 (2022).
Bartelt, A. et al. Thermogenic adipocytes promote HDL turnover and reverse cholesterol transport. Nat. Commun. 8, 15010 (2017).
Shimizu, I. et al. Vascular rarefaction mediates whitening of brown fat in obesity. J. Clin. Invest. 124, 2099–2112 (2014).
Herz, C. T. et al. Active brown adipose tissue is associated with a healthier metabolic phenotype in obesity. Diabetes https://doi.org/10.2337/db21-0475 (2021).
Wibmer, A. G. et al. Brown adipose tissue is associated with healthier body fat distribution and metabolic benefits independent of regional adiposity. Cell Rep. Med. 2, 100332 (2021).
Carpentier, A. C. et al. Brown adipose tissue energy metabolism in humans. Front. Endocrinol. 9, 447 (2018).
Berbée, J. F. et al. Brown fat activation reduces hypercholesterolaemia and protects from atherosclerosis development. Nat. Commun. 6, 6356 (2015).
Zhang, Q. et al. Differences in the metabolic status of healthy adults with and without active brown adipose tissue. Wien. Klin. Wochenschr. 125, 687–695 (2013).
Matsushita, M. et al. Impact of brown adipose tissue on body fatness and glucose metabolism in healthy humans. Int. J. Obes. 38, 812–817 (2014).
Global Burden of Metabolic Risk Factors for Chronic Diseases, C. Metabolic mediators of the effects of body-mass index, overweight, and obesity on coronary heart disease and stroke: a pooled analysis of 97 prospective cohorts with 1.8 million participants. Lancet 383, 970–983 (2014).
Lu, Y., Hajifathalian, K., Rimm, E. B., Ezzati, M. & Danaei, G. Mediators of the effect of body mass index on coronary heart disease: decomposing direct and indirect effects. Epidemiology 26, 153–162 (2015).
Bakhtiyari, M. et al. Contribution of obesity and cardiometabolic risk factors in developing cardiovascular disease: a population-based cohort study. Sci. Rep. 12, 1544 (2022).
Blüher, M. Metabolically healthy obesity. Endocr. Rev. 41, bnaa004 (2020).
Smith, G. I., Mittendorfer, B. & Klein, S. Metabolically healthy obesity: facts and fantasies. J. Clin. Invest. 129, 3978–3989 (2019).
Ortega, F. B., Lavie, C. J. & Blair, S. N. Obesity and cardiovascular disease. Circ. Res. 118, 1752–1770 (2016).
Ortega, F. B. et al. Role of physical activity and fitness in the characterization and prognosis of the metabolically healthy obesity phenotype: a systematic review and meta-analysis. Prog. Cardiovasc. Dis. 61, 190–205 (2018).
Martinez-Gomez, D. et al. Physical activity and risk of metabolic phenotypes of obesity: a prospective taiwanese cohort study in more than 200,000 adults. Mayo Clin. Proc. 94, 2209–2219 (2019).
Barrea, L. et al. Metabolically healthy obesity (MHO) vs. metabolically unhealthy obesity (MUO) phenotypes in PCOS: association with endocrine-metabolic profile, adherence to the mediterranean diet, and body composition. Nutrients 13, 3925 (2021).
Tanisawa, K. et al. Association between dietary patterns and different metabolic phenotypes in Japanese adults: WASEDA’S health study. Front. Nutr. 9, 779967 (2022).
Slagter, S. N. et al. Dietary patterns and physical activity in the metabolically (un)healthy obese: the Dutch Lifelines cohort study. Nutr. J. 17, 18 (2018).
Zhang, N., Chen, Y., Guo, X., Sun, G. & Sun, Y. The prevalence and predictors of metabolically healthy obesity in obese rural population of China: a cross-sectional study. Psychol. Health Med. 22, 303–309 (2017).
Farabi, S. S., Smith, G. I., Schweitzer, G. G., Stein, R. I. & Klein, S. Do lifestyle factors and quality of life differ in people with metabolically healthy and unhealthy obesity? Int. J. Obes. 46, 1778–1785 (2022).
Kanagasabai, T., Dhanoa, R., Kuk, J. L. & Ardern, C. I. Association between sleep habits and metabolically healthy obesity in adults: a cross-sectional study. J. Obes. 2017, 5272984 (2017).
Ankita, A., Mehta, B., Dutt, N., Nayak, P. & Sharma, P. Poor sleep and the metabolic derangements associated with obesity in adult males. J. Fam. Med. Prim. Care 11, 2026–2031 (2022).
Brochu, M. et al. What are the physical characteristics associated with a normal metabolic profile despite a high level of obesity in postmenopausal women? J. Clin. Endocrinol. Metab. 86, 1020–1025 (2001).
Kim, L. J. et al. Associations of visceral and liver fat with the metabolic syndrome across the spectrum of obesity: the AGES-Reykjavik study. Obesity 19, 1265–1271 (2011).
Hwang, Y. C. et al. Visceral abdominal fat accumulation predicts the conversion of metabolically healthy obese subjects to an unhealthy phenotype. Int. J. Obes. 39, 1365–1370 (2015).
Kang, Y. M. et al. Visceral adiposity index predicts the conversion of metabolically healthy obesity to an unhealthy phenotype. PLoS ONE 12, e0179635 (2017).
Fabbrini, E. et al. Intrahepatic fat, not visceral fat, is linked with metabolic complications of obesity. Proc. Natl Acad. Sci. USA 106, 15430–15435 (2009).
Esser, N. et al. Obesity phenotype is related to NLRP3 inflammasome activity and immunological profile of visceral adipose tissue. Diabetologia 56, 2487–2497 (2013).
Karelis, A. D. et al. The metabolically healthy but obese individual presents a favorable inflammation profile. J. Clin. Endocrinol. Metab. 90, 4145–4150 (2005).
Phillips, C. M. & Perry, I. J. Does inflammation determine metabolic health status in obese and nonobese adults? J. Clin. Endocrinol. Metab. 98, E1610–E1619 (2013).
Eckel, N., Meidtner, K., Kalle-Uhlmann, T., Stefan, N. & Schulze, M. B. Metabolically healthy obesity and cardiovascular events: a systematic review and meta-analysis. Eur. J. Prev. Cardiol. 23, 956–966 (2016).
Caleyachetty, R. et al. Metabolically healthy obese and incident cardiovascular disease events among 3.5 million men and women. J. Am. Coll. Cardiol. 70, 1429–1437 (2017).
Lassale, C. et al. Separate and combined associations of obesity and metabolic health with coronary heart disease: a pan-European case-cohort analysis. Eur. Heart J. 39, 397–406 (2018).
Eckel, N. et al. Transition from metabolic healthy to unhealthy phenotypes and association with cardiovascular disease risk across BMI categories in 90 257 women (the Nurses’ Health Study): 30 year follow-up from a prospective cohort study. Lancet Diabetes Endocrinol. 6, 714–724 (2018).
Lin, L. et al. Transition of metabolic phenotypes and risk of subclinical atherosclerosis according to BMI: a prospective study. Diabetologia 63, 1312–1323 (2020).
Abiri, B., Koohi, F., Ebadinejad, A., Valizadeh, M. & Hosseinpanah, F. Transition from metabolically healthy to unhealthy overweight/obesity and risk of cardiovascular disease incidence: a systematic review and meta-analysis. Nutr. Metab. Cardiovasc. Dis. 32, 2041–2051 (2022).
Hosseinpanah, F. et al. The association between transition from metabolically healthy obesity to metabolic syndrome, and incidence of cardiovascular disease: Tehran lipid and glucose study. PLoS ONE 15, e0239164 (2020).
Mongraw-Chaffin, M. et al. Metabolically healthy obesity, transition to metabolic syndrome, and cardiovascular risk. J. Am. Coll. Cardiol. 71, 1857–1865 (2018).
Ortega, F. B., Ruiz, J. R., Labayen, I., Lavie, C. J. & Blair, S. N. The fat but fit paradox: what we know and don’t know about it. Br. J. Sports Med. 52, 151–153 (2018).
Lee, C. D., Blair, S. N. & Jackson, A. S. Cardiorespiratory fitness, body composition, and all-cause and cardiovascular disease mortality in men. Am. J. Clin. Nutr. 69, 373–380 (1999).
Tarp, J. et al. Fitness, fatness, and mortality in men and women from the UK Biobank: prospective cohort study. J. Am. Heart Assoc. 10, e019605 (2021).
McAuley, P. A., Kokkinos, P. F., Oliveira, R. B., Emerson, B. T. & Myers, J. N. Obesity paradox and cardiorespiratory fitness in 12,417 male veterans aged 40 to 70 years. Mayo Clin. Proc. 85, 115–121 (2010).
Goel, K. et al. Combined effect of cardiorespiratory fitness and adiposity on mortality in patients with coronary artery disease. Am. Heart J. 161, 590–597 (2011).
Hemmingsson, E., Vaisanen, D., Andersson, G., Wallin, P. & Ekblom-Bak, E. Combinations of BMI and cardiorespiratory fitness categories: trends between 1995 and 2020 and associations with CVD incidence and mortality and all-cause mortality in 471 216 adults. Eur. J. Prev. Cardiol. 29, 959–967 (2022).
Barry, V. W., Caputo, J. L. & Kang, M. The joint association of fitness and fatness on cardiovascular disease mortality: a meta-analysis. Prog. Cardiovasc. Dis. 61, 136–141 (2018).
Koolhaas, C. M. et al. Impact of physical activity on the association of overweight and obesity with cardiovascular disease: the Rotterdam study. Eur. J. Prev. Cardiol. 24, 934–941 (2017).
Zhang, X., Cash, R. E., Bower, J. K., Focht, B. C. & Paskett, E. D. Physical activity and risk of cardiovascular disease by weight status among U.S adults. PLoS ONE 15, e0232893 (2020).
Valenzuela, P. L. et al. Joint association of physical activity and body mass index with cardiovascular risk: a nationwide population-based cross-sectional study. Eur. J. Prev. Cardiol. 29, e50–e52 (2022).
Li, T. Y. et al. Obesity as compared with physical activity in predicting risk of coronary heart disease in women. Circulation 113, 499–506 (2006).
Carlsson, A. C. et al. Physical activity, obesity and risk of cardiovascular disease in middle-aged men during a median of 30 years of follow-up. Eur. J. Prev. Cardiol. 23, 359–365 (2016).
Lavie, C. J., De Schutter, A. & Milani, R. V. Healthy obese versus unhealthy lean: the obesity paradox. Nat. Rev. Endocrinol. 11, 55–62 (2015).
Elagizi, A. et al. An overview and update on obesity and the obesity paradox in cardiovascular diseases. Prog. Cardiovasc. Dis. 61, 142–150 (2018).
Sharma, A. et al. Meta-analysis of the relation of body mass index to all-cause and cardiovascular mortality and hospitalization in patients with chronic heart failure. Am. J. Cardiol. 115, 1428–1434 (2015).
Niedziela, J. et al. The obesity paradox in acute coronary syndrome: a meta-analysis. Eur. J. Epidemiol. 29, 801–812 (2014).
Nitsche, L. J. et al. Exploring the impact of the obesity paradox on lung cancer and other malignancies. Cancers 14, 1440 (2022).
Li, S. et al. Systematic review of prognostic roles of body mass index for patients undergoing lung cancer surgery: does the ‘obesity paradox’ really exist? Eur. J. Cardiothorac. Surg. 51, 817–828 (2017).
Cortellini, A. et al. A multicenter study of body mass index in cancer patients treated with anti-PD-1/PD-L1 immune checkpoint inhibitors: when overweight becomes favorable. J. Immunother. Cancer 7, 57 (2019).
McQuade, J. L. et al. Association of body-mass index and outcomes in patients with metastatic melanoma treated with targeted therapy, immunotherapy, or chemotherapy: a retrospective, multicohort analysis. Lancet Oncol. 19, 310–322 (2018).
Shah, R. et al. Body mass index and mortality in acutely decompensated heart failure across the world: a global obesity paradox. J. Am. Coll. Cardiol. 63, 778–785 (2014).
Wang, Z. J. et al. Association of body mass index with mortality and cardiovascular events for patients with coronary artery disease: a systematic review and meta-analysis. Heart 101, 1631–1638 (2015).
Iliodromiti, S. et al. The impact of confounding on the associations of different adiposity measures with the incidence of cardiovascular disease: a cohort study of 296 535 adults of white European descent. Eur. Heart J. 39, 1514–1520 (2018).
Kokkinos, P. et al. Cardiorespiratory fitness and the paradoxical BMI-mortality risk association in male veterans. Mayo Clin. Proc. 89, 754–762 (2014).
Donini, L. M., Pinto, A., Giusti, A. M., Lenzi, A. & Poggiogalle, E. Obesity or BMI paradox? beneath the tip of the iceberg. Front. Nutr. 7, 53 (2020).
The Lancet Diabetes Endocrinology. The obesity-cancer link: of increasing concern. Lancet Diabetes Endocrinol. 8, 175 (2020).
Feletto, E. et al. An ecological study of obesity-related cancer incidence trends in Australia from 1983 to 2017. Lancet Reg. Health West. Pac. 29, 100575 (2022).
Ringel, A. E. et al. Obesity shapes metabolism in the tumor microenvironment to suppress anti-tumor immunity. Cell 183, 1848–1866.e26 (2020).
Wang, Z. et al. Paradoxical effects of obesity on T cell function during tumor progression and PD-1 checkpoint blockade. Nat. Med. 25, 141–151 (2019).
Sanchez, A. et al. Transcriptomic signatures related to the obesity paradox in patients with clear cell renal cell carcinoma: a cohort study. Lancet Oncol. 21, 283–293 (2020).
Lee, D. H. & Giovannucci, E. L. The obesity paradox in cancer: epidemiologic insights and perspectives. Curr. Nutr. Rep. 8, 175–181 (2019).
Strulov Shachar, S. & Williams, G. R. The obesity paradox in cancer-moving beyond BMI. Cancer Epidemiol. Biomark. Prev. 26, 13–16 (2017).
Straub, L. G. & Scherer, P. E. Metabolic messengers: adiponectin. Nat. Metab. 1, 334–339 (2019).
Arita, Y. et al. Paradoxical decrease of an adipose-specific protein, adiponectin, in obesity. Biochem. Biophys. Res. Commun. 257, 79–83 (1999).
van Andel, M., Heijboer, A. C. & Drent, M. L. Adiponectin and its isoforms in pathophysiology. Adv. Clin. Chem. 85, 115–147 (2018).
Maeda, N., Funahashi, T., Matsuzawa, Y. & Shimomura, I. Adiponectin, a unique adipocyte-derived factor beyond hormones. Atherosclerosis 292, 1–9 (2020).
Woodward, L., Akoumianakis, I. & Antoniades, C. Unravelling the adiponectin paradox: novel roles of adiponectin in the regulation of cardiovascular disease. Br. J. Pharmacol. 174, 4007–4020 (2017).
Spranger, J. et al. Adiponectin and protection against type 2 diabetes mellitus. Lancet 361, 226–2288 (2003).
Wang, Y. et al. Plasma adiponectin levels and type 2 diabetes risk: a nested case-control study in a Chinese population and an updated meta-analysis. Sci. Rep. 8, 406 (2018).
Koenig, W., Khuseyinova, N., Baumert, J., Meisinger, C. & Löwel, H. Serum concentrations of adiponectin and risk of type 2 diabetes mellitus and coronary heart disease in apparently healthy middle-aged men: results from the 18-year follow-up of a large cohort from southern Germany. J. Am. Coll. Cardiol. 48, 1369–1377 (2006).
Frystyk, J. et al. Serum adiponectin is a predictor of coronary heart disease: a population-based 10-year follow-up study in elderly men. J. Clin. Endocrinol. Metab. 92, 571–576 (2007).
Pischon, T. et al. Plasma adiponectin levels and risk of myocardial infarction in men. JAMA 291, 1730–1737 (2004).
Persson, J. et al. Low plasma adiponectin concentration is associated with myocardial infarction in young individuals. J. Intern. Med. 268, 194–205 (2010).
Kazumi, T., Kawaguchi, A., Hirano, T. & Yoshino, G. Serum adiponectin is associated with high-density lipoprotein cholesterol, triglycerides, and low-density lipoprotein particle size in young healthy men. Metabolism 53, 589–593 (2004).
Saarikoski, L. A. et al. Adiponectin is related with carotid artery intima-media thickness and brachial flow-mediated dilatation in young adults—the Cardiovascular Risk in Young Finns Study. Ann. Med. 42, 603–611 (2010).
Sattar, N. et al. Adiponectin and coronary heart disease: a prospective study and meta-analysis. Circulation 114, 623–629 (2006).
Sook Lee, E. et al. Association between adiponectin levels and coronary heart disease and mortality: a systematic review and meta-analysis. Int. J. Epidemiol. 42, 1029–1039 (2013).
Arregui, M. et al. Adiponectin and risk of stroke: prospective study and meta-analysis. Stroke 45, 10–17 (2014).
Wu, Z., Cheng, Y., Aung, L. H. & Li, B. Association between adiponectin concentrations and cardiovascular disease in diabetic patients: a systematic review and meta-analysis. PLoS ONE 8, e78485 (2013).
Scarale, M. G., Fontana, A., Trischitta, V., Copetti, M. & Menzaghi, C. Circulating adiponectin levels are paradoxically associated with mortality rate. A systematic review and meta-analysis. J. Clin. Endocrinol. Metab. 104, 1357–1368 (2018).
Menzaghi, C. & Trischitta, V. The adiponectin paradox for all-cause and cardiovascular mortality. Diabetes 67, 12–22 (2018).
Menzaghi, C. et al. Circulating adiponectin and cardiovascular mortality in patients with type 2 diabetes mellitus: evidence of sexual dimorphism. Cardiovasc. Diabetol. 13, 130 (2014).
Kollerits, B. et al. Gender-specific association of adiponectin as a predictor of progression of chronic kidney disease: the mild to moderate kidney disease study. Kidney Int. 71, 1279–1286 (2007).
Wang, Y., Ma, X. L. & Lau, W. B. Cardiovascular adiponectin resistance: the critical role of adiponectin receptor modification. Trends Endocrinol. Metab. 28, 519–530 (2017).
Kim-Mitsuyama, S. et al. Total adiponectin is associated with incident cardiovascular and renal events in treated hypertensive patients: subanalysis of the ATTEMPT-CVD randomized trial. Sci. Rep. 9, 16589 (2019).
Bruce, C. R., Mertz, V. A., Heigenhauser, G. J. & Dyck, D. J. The stimulatory effect of globular adiponectin on insulin-stimulated glucose uptake and fatty acid oxidation is impaired in skeletal muscle from obese subjects. Diabetes 54, 3154–3160 (2005).
Chen, M. B. et al. Impaired activation of AMP-kinase and fatty acid oxidation by globular adiponectin in cultured human skeletal muscle of obese type 2 diabetics. J. Clin. Endocrinol. Metab. 90, 3665–36672 (2005).
Tsuchida, A. et al. Insulin/Foxo1 pathway regulates expression levels of adiponectin receptors and adiponectin sensitivity. J. Biol. Chem. 279, 30817–30822 (2004).
Zhao, S., Kusminski, C. M. & Scherer, P. E. Adiponectin, leptin and cardiovascular disorders. Circ. Res. 128, 136–149 (2021).
Yang, W., Kelly, T. & He, J. Genetic epidemiology of obesity. Epidemiol. Rev. 29, 49–61 (2007).
Locke, A. E. et al. Genetic studies of body mass index yield new insights for obesity biology. Nature 518, 197–206 (2015).
Silventoinen, K. et al. Differences in genetic and environmental variation in adult BMI by sex, age, time period, and region: an individual-based pooled analysis of 40 twin cohorts. Am. J. Clin. Nutr. 106, 457–466 (2017).
Elks, C. E. et al. Variability in the heritability of body mass index: a systematic review and meta-regression. Front. Endocrinol. 3, 29 (2012).
Johnson, W. D., Brashear, M. M., Gupta, A. K., Rood, J. C. & Ryan, D. H. Incremental weight loss improves cardiometabolic risk in extremely obese adults. Am. J. Med. 124, 931–938 (2011).
Bailey-Davis, L. et al. Impact of sustained weight loss on cardiometabolic outcomes. Am. J. Cardiol. 162, 66–72 (2022).
Wing, R. R. et al. Association of weight loss maintenance and weight regain on 4-year changes in CVD risk factors: the action for health in diabetes (Look AHEAD) clinical trial. Diabetes Care 39, 1345–1355 (2016).
Magkos, F. et al. Effects of moderate and subsequent progressive weight loss on metabolic function and adipose tissue biology in humans with obesity. Cell Metab. 23, 591–601 (2016).
Chen, C., Ye, Y., Zhang, Y., Pan, X. F. & Pan, A. Weight change across adulthood in relation to all cause and cause specific mortality: prospective cohort study. BMJ 367, l5584 (2019).
Adams, K. F. et al. Body mass and weight change in adults in relation to mortality risk. Am. J. Epidemiol. 179, 135–144 (2014).
Iwamoto, S. J., Abushamat, L. A., Zaman, A., Millard, A. J. & Cornier, M. A. Obesity management in cardiometabolic disease: state of the art. Curr. Atheroscler. Rep. 23, 59 (2021).
Franz, M. J. et al. Weight-loss outcomes: a systematic review and meta-analysis of weight-loss clinical trials with a minimum 1-year follow-up. J. Am. Diet. Assoc. 107, 1755–1767 (2007).
Hall, K. D. et al. Quantification of the effect of energy imbalance on bodyweight. Lancet 378, 826–837 (2011).
Polidori, D., Sanghvi, A., Seeley, R. J. & Hall, K. D. How strongly does appetite counter weight loss? Quantification of the feedback control of human energy intake. Obesity 24, 2289–2295 (2016).
Berger, S. E., Huggins, G. S., McCaffery, J. M., Jacques, P. F. & Lichtenstein, A. H. Change in cardiometabolic risk factors associated with magnitude of weight regain 3 years after a 1-year intensive lifestyle intervention in type 2 diabetes mellitus: the look AHEAD trial. J. Am. Heart Assoc. 8, e010951 (2019).
Anderson, J. W., Konz, E. C., Frederich, R. C. & Wood, C. L. Long-term weight-loss maintenance: a meta-analysis of US studies. Am. J. Clin. Nutr. 74, 579–584 (2001).
Ge, L. et al. Comparison of dietary macronutrient patterns of 14 popular named dietary programmes for weight and cardiovascular risk factor reduction in adults: systematic review and network meta-analysis of randomised trials. BMJ 369, m696 (2020).
Thorogood, A. et al. Isolated aerobic exercise and weight loss: a systematic review and meta-analysis of randomized controlled trials. Am. J. Med. 124, 747–755 (2011).
Verheggen, R. J. et al. A systematic review and meta-analysis on the effects of exercise training versus hypocaloric diet: distinct effects on body weight and visceral adipose tissue. Obes. Rev. 17, 664–690 (2016).
Chang, Y. H., Yang, H. Y. & Shun, S. C. Effect of exercise intervention dosage on reducing visceral adipose tissue: a systematic review and network meta-analysis of randomized controlled trials. Int. J. Obes. 45, 982–997 (2021).
Swift, D. L., Johannsen, N. M., Lavie, C. J., Earnest, C. P. & Church, T. S. The role of exercise and physical activity in weight loss and maintenance. Prog. Cardiovasc. Dis. 56, 441–447 (2014).
Johns, D. J., Hartmann-Boyce, J., Jebb, S. A. & Aveyard, P., Behavioural Weight Management Review Group. Diet or exercise interventions vs combined behavioral weight management programs: a systematic review and meta-analysis of direct comparisons. J. Acad. Nutr. Diet. 114, 1557–1568 (2014).
Fiuza-Luces, C. et al. Exercise benefits in cardiovascular disease: beyond attenuation of traditional risk factors. Nat. Rev. Cardiol. 15, 731–743 (2018).
Dombrowski, S. U., Knittle, K., Avenell, A., Araújo-Soares, V. & Sniehotta, F. F. Long term maintenance of weight loss with non-surgical interventions in obese adults: systematic review and meta-analyses of randomised controlled trials. BMJ 348, g2646 (2014).
Khera, R. et al. Association of pharmacological treatments for obesity with weight loss and adverse events: a systematic review and meta-analysis. JAMA 315, 2424–2434 (2016).
Salari, N. et al. The best drug supplement for obesity treatment: a systematic review and network meta-analysis. Diabetol. Metab. Syndr. 13, 110 (2021).
Jastreboff, A. M. et al. Tirzepatide once weekly for the treatment of obesity. N. Engl. J. Med. 387, 205–216 (2022).
Rao, S. et al. Effect of exercise and pharmacological interventions on visceral adiposity: a systematic review and meta-analysis of long-term randomized controlled trials. Mayo Clin. Proc. 94, 211–224 (2019).
Lundgren, J. R. et al. Healthy weight loss maintenance with exercise, liraglutide, or both combined. N. Engl. J. Med. 384, 1719–1730 (2021).
Ricci, C. et al. Long-term effects of bariatric surgery on type II diabetes, hypertension and hyperlipidemia: a meta-analysis and meta-regression study with 5-year follow-up. Obes. Surg. 25, 397–405 (2015).
Wu, F. Z. et al. Differential effects of bariatric surgery versus exercise on excessive visceral fat deposits. Medicine 95, e2616 (2016).
Ren, Z. Q., Lu, G. D., Zhang, T. Z. & Xu, Q. Effect of physical exercise on weight loss and physical function following bariatric surgery: a meta-analysis of randomised controlled trials. BMJ Open 8, e023208 (2018).
Mohammadian Khonsari, N. et al. Normal weight obesity and cardiometabolic risk factors: a systematic review and meta-analysis. Front. Endocrinol. 13, 857930 (2022).
Gomez-Ambrosi, J. et al. Body mass index classification misses subjects with increased cardiometabolic risk factors related to elevated adiposity. Int. J. Obes. 36, 286–294 (2012).
Romero-Corral, A. et al. Normal weight obesity: a risk factor for cardiometabolic dysregulation and cardiovascular mortality. Eur. Heart J. 31, 737–746 (2010).
Batsis, J. A. et al. Normal weight obesity and mortality in United States subjects >/=60 years of age (from the Third National Health and Nutrition Examination Survey). Am. J. Cardiol. 112, 1592–1598 (2013).
Rakhmat, I. I. et al. Cardiometabolic risk factors in adults with normal weight obesity: a systematic review and meta-analysis. Clin. Obes. 12, e12523 (2022).
Gagnon, E. et al. Mendelian randomization prioritizes abdominal adiposity as an independent causal factor for liver fat accumulation and cardiometabolic diseases. Commun. Med. 2, 130 (2022).
Zhang, C., Rexrode, K. M., van Dam, R. M., Li, T. Y. & Hu, F. B. Abdominal obesity and the risk of all-cause, cardiovascular, and cancer mortality: sixteen years of follow-up in US women. Circulation 117, 1658–1667 (2008).
Cerhan, J. R. et al. A pooled analysis of waist circumference and mortality in 650,000 adults. Mayo Clin. Proc. 89, 335–345 (2014).
Reis, J. P. et al. Comparison of overall obesity and body fat distribution in predicting risk of mortality. Obesity 17, 1232–1239 (2009).
Sahakyan, K. R. et al. Normal-weight central obesity: implications for total and cardiovascular mortality. Ann. Intern. Med. 163, 827–835 (2015).
Coutinho, T. et al. Combining body mass index with measures of central obesity in the assessment of mortality in subjects with coronary disease: role of “normal weight central obesity”. J. Am. Coll. Cardiol. 61, 553–560 (2013).
Konieczna, J. et al. Body adiposity indicators and cardiometabolic risk: cross-sectional analysis in participants from the PREDIMED-Plus trial. Clin. Nutr. 38, 1883–1891 (2019).
Ross, R. et al. Waist circumference as a vital sign in clinical practice: a Consensus Statement from the IAS and ICCR Working Group on Visceral Obesity. Nat. Rev. Endocrinol. 16, 177–189 (2020).
Ibrahim, M. M. Subcutaneous and visceral adipose tissue: structural and functional differences. Obes. Rev. 11, 11–18 (2010).
Spalding, K. L. et al. Dynamics of fat cell turnover in humans. Nature 453, 783–787 (2008).
Wang, Q. A., Tao, C., Gupta, R. K. & Scherer, P. E. Tracking adipogenesis during white adipose tissue development, expansion and regeneration. Nat. Med. 19, 1338–1344 (2013).
Gustafson, B. & Smith, U. The WNT inhibitor Dickkopf 1 and bone morphogenetic protein 4 rescue adipogenesis in hypertrophic obesity in humans. Diabetes 61, 1217–1224 (2012).
Driskell, R. R., Jahoda, C. A., Chuong, C. M., Watt, F. M. & Horsley, V. Defining dermal adipose tissue. Exp. Dermatol. 23, 629–631 (2014).
Zhang, Z. et al. Dermal adipose tissue has high plasticity and undergoes reversible dedifferentiation in mice. J. Clin. Invest. 129, 5327–5342 (2019).
Kasza, I., Hernando, D., Roldán-Alzate, A., Alexander, C. M. & Reeder, S. B. Thermogenic profiling using magnetic resonance imaging of dermal and other adipose tissues. JCI Insight 1, e87146 (2016).
Plikus, M. V. et al. Regeneration of fat cells from myofibroblasts during wound healing. Science 355, 748–752 (2017).
Rivera-Gonzalez, G., Shook, B. & Horsley, V. Adipocytes in skin health and disease. Cold Spring Harb. Perspect. Med. 4, a015271 (2014).
Kruglikov, I. L., Zhang, Z. & Scherer, P. E. The role of immature and mature adipocytes in hair cycling. Trends Endocrinol. Metab. 30, 93–105 (2019).
Schmidt, B. A. & Horsley, V. Intradermal adipocytes mediate fibroblast recruitment during skin wound healing. Development 140, 1517–1527 (2013).
Hwang, I. & Kim, J. B. Two faces of white adipose tissue with heterogeneous adipogenic progenitors. Diabetes Metab. J. 43, 752–762 (2019).
Ledoux, S. et al. Traditional anthropometric parameters still predict metabolic disorders in women with severe obesity. Obesity 18, 1026–1032 (2010).
O’Connell, J. et al. The relationship of omental and subcutaneous adipocyte size to metabolic disease in severe obesity. PLoS ONE 5, e9997 (2010).
Arner, P. et al. Variations in the size of the major omentum are primarily determined by fat cell number. J. Clin. Endocrinol. Metab. 98, E897–E901 (2013).
Jeffery, E., Church, C. D., Holtrup, B., Colman, L. & Rodeheffer, M. S. Rapid depot-specific activation of adipocyte precursor cells at the onset of obesity. Nat. Cell Biol. 17, 376–385 (2015).
Corvera, S. Cellular heterogeneity in adipose tissues. Annu. Rev. Physiol. 83, 257–278 (2021).
Whitehead, A. et al. Brown and beige adipose tissue regulate systemic metabolism through a metabolite interorgan signaling axis. Nat. Commun. 12, 1905 (2021).
Yang, F. T. & Stanford, K. I. Batokines: mediators of inter-tissue communication (a mini-review). Curr. Obes. Rep. 11, 1–9 (2022).
AlZaim, I. & Kalucka, J. Batokine neuregulin 4 promotes atherosclerotic resolution. Nat. Metab. 4, 1440–1441 (2022).
Acknowledgements
The authors are grateful to K. McCreath for his editorial assistance with the manuscript before initial submission. Research by A.L. is funded by the Wereld Kanker Onderzoek Fonds (WKOF), as part of the World Cancer Research Fund International grant programme and the Spanish Ministry of Science and Innovation (Fondo de Investigaciones Sanitarias (FIS)) and Fondos FEDER (grant number PI18/00139). Research by P.L.V. is supported by a Sara Borrell postdoctoral contract granted by Instituto de Salud Carlos III (CD21/00138).
Author information
Authors and Affiliations
Contributions
P.L.V., P.C.-B., D.E.L. and A.L. wrote the manuscript. All the authors researched data for the article, contributed to discussion of content and reviewed and/or edited the article before submission.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Cardiology thanks Charalambos Antoniades and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Glossary
- Adipocytokine
-
From the Greek adipo (fat), cytos (cell) and kinos (movement); also termed ‘adipokine’. Cytokine secreted by adipose tissue.
- Adipogenesis
-
Formation of new adipocytes from precursor cells.
- Aerobic exercise
-
Also known as endurance exercise. Exercise that is performed for more than a few minutes and preferentially involves aerobic metabolism for energy production (for example, brisk walking, bicycling or swimming).
- Bariatric surgery
-
Also known as weight-loss surgery. Various surgical procedures (such as gastric bypass) performed on people with obesity that alters levels of digestive hormones responsible for hunger and satiety.
- Cardiorespiratory fitness
-
The capacity of the circulatory and respiratory systems to supply oxygen to skeletal muscle mitochondria for production of the energy needed during physical activity, usually determined by treadmill or cycle-ergometer testing until exhaustion.
- Damage‐associated molecular patterns
-
(DAMPs). Molecules that act as endogenous danger signals; they are released into the extracellular space in response to cell damage and promote inflammatory responses by binding to pattern recognition receptors.
- Dual-energy X-ray absorptiometry
-
(DXA or DEXA). A method of measuring fat and lean (muscle and bone) mass based on the different attenuation coefficients to X-rays of soft tissue and bone.
- Glycated haemoglobin
-
Also known as haemoglobin A1c (HbA1c). A form of haemoglobin that is produced when glucose reacts with the amino group on a haemoglobin molecule, thereby reflecting the presence of hyperglycaemia, which is often indicative of diabetes mellitus.
- Heart failure with preserved ejection fraction
-
A type of heart failure that occurs when the muscle in the left ventricle stiffens and has a lower relaxation capacity. Patients have signs and symptoms of heart failure despite having a normal, or near-normal, left ventricular ejection fraction (≥50%).
- Hyperplasia
-
An increase in the number of cells in an organ or tissue (by recruitment and differentiation of new precursor cells) that seem normal under a microscope (as opposed to dysplasia) and result in an increase in organ or tissue size.
- Hypertrophy
-
An increase in the size of cells in an organ or tissue as a result of elevated synthesis of structural components (not of cellular swelling) that can result in an increase in organ or tissue size.
- Integrated stress response
-
An evolutionarily conserved intracellular signalling network that helps the cell, tissue and organism to adapt to a variable environment and maintain health.
- Lipoapoptosis
-
Ectopic lipid overload can interfere with cell functions and induce apoptosis, thereby contributing to gradual organ failure.
- Lipodystrophy syndromes
-
Heterogeneous group of diseases characterized by the selective absence of adipose tissue, where the primary defect is the loss of functional adipocytes, leading to lipotoxicity, severe dyslipidaemia or insulin resistance.
- Lipotoxicity
-
When the storage capacity of the white adipose tissue is exceeded, ectopic fat storage occurs in several organs (skeletal muscle, liver, heart and pancreas), leading to cellular dysfunction in these organs.
- Long-chain saturated fatty acids
-
(LCSFAs). Fatty acids with aliphatic tails with >12 carbon atoms (for example, palmitate and stearate), resulting from the hydrolysis of neutral lipids (such as triacylglycerols stored in adipocytes). LCSFAs are also found abundantly in dairy fat, tallow, lard and palm oil.
- Mediterranean diet
-
A diet abundant in fruits, vegetables, legumes, whole grains, olives, nuts and seeds, and containing extra-virgin olive oil, associated with frequent consumption of fish, moderate consumption of dairy products and red wine, and low consumption of red meat and isolated sugars.
- Metabolic syndrome
-
A clustering of three or more of the following five medical conditions: abdominal obesity (as determined by waist circumference), high blood pressure, hyperglycaemia, hypertriglyceridaemia and low serum HDL-cholesterol level.
- Neutral lipids
-
Based on their chemical characteristics, lipids can be classified into neutral (for example, triacylglycerols) and polar (such as phospholipids and glycolipids) lipids; neutral lipids are used as major energy sources and polar lipids as cell membrane components.
- NLRP3 inflammasome
-
Cytosolic multiprotein oligomer involved in the innate immune response, responsible for the activation of pro-inflammatory responses.
- Obesity class
-
Class 1 is defined as BMI of 30 to <35 kg/m2, class 2 as BMI 35 to <40 kg/m2 and class 3 as BMI ≥40 kg/m2.
- Omentum
-
The layers of peritoneum (the serous membrane forming the lining of the abdominal cavity) that surround abdominal organs: the greater omentum is a large apron-like fold of visceral peritoneum that hangs down from the stomach, whereas the lower omentum hangs down from the liver.
- Pattern recognition receptor
-
A type of receptor that recognizes damage-associated molecular patterns, as well as molecular structures produced by microbial pathogens.
- Physical activity
-
Any bodily movement produced by skeletal muscles that requires energy expenditure (for example, walking). The WHO recommends that adults engage in regular (150–300 min per week) moderate or vigorous aerobic physical activities (such as brisk walking).
- Physical exercise
-
Also termed ‘exercise training’ or simply ‘exercise’. A subset of physical activity that is planned, structured and repetitive and has a final or an intermediate objective of improving or maintaining fitness or health outcomes.
- Sarcopenia
-
Derived from the Greek ‘sarx’ (flesh) and ‘penia’ (loss). The age-induced (or sometimes disease-induced) loss of muscle mass and function.
- Senescence-associated secretory phenotype
-
Phenotype associated with senescent cells, which secrete high levels of pro-inflammatory cytokines, chemokines and other molecules.
- Severe obesity
-
Also known as obesity class 3; BMI ≥40 kg/m2. The term ‘morbid obesity’ was also formerly used to define a BMI of ≥40 kg/m2 (or BMI ≥35 kg/m2 when accompanied by obesity-related conditions).
- Systemic, low-grade, chronic inflammation
-
A sterile chronic inflammation characterized by the activation of immune components that are often distinct from those engaged in acute immune responses, potentially causing major alterations in all tissues and organs as well as in normal cellular physiology and increasing the risk of various non-communicable diseases across the lifespan of the individual.
- γδ T cells
-
A small subset of T lymphocytes that express heterodimeric T cell receptors (TCRs) composed of γ and δ chains, as opposed to the classical CD4+ T helper cells or CD8+ cytotoxic T cells, which express αβ TCRs.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Valenzuela, P.L., Carrera-Bastos, P., Castillo-García, A. et al. Obesity and the risk of cardiometabolic diseases. Nat Rev Cardiol 20, 475–494 (2023). https://doi.org/10.1038/s41569-023-00847-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41569-023-00847-5
- Springer Nature Limited
This article is cited by
-
ASGR1 deficiency diverts lipids toward adipose tissue but results in liver damage during obesity
Cardiovascular Diabetology (2024)
-
Revisiting an old relationship: the causal associations of the ApoB/ApoA1 ratio with cardiometabolic diseases and relative risk factors—a mendelian randomization analysis
Cardiovascular Diabetology (2024)
-
White adipocyte dysfunction and obesity-associated pathologies in humans
Nature Reviews Molecular Cell Biology (2024)
-
Gut microbiota in overweight and obesity: crosstalk with adipose tissue
Nature Reviews Gastroenterology & Hepatology (2024)
-
Incidence of Post-operative Gastro-esophageal Reflux Disorder in Patients Undergoing Laparoscopic Sleeve Gastrectomy: A Systematic Review and Meta-analysis
Obesity Surgery (2024)