Abstract
Background/Objectives
In patients with severe aortic stenosis (AS), frailty is a clinically relevant measure of increased vulnerability that should be included in the preoperative risk assessment. Bioelectrical impedance analysis (BIA) derived phase angle (PA) reflects cell membrane integrity and function. Few studies are available on the relative contribution of adiposity distribution on frailty, and about the influences of frailty and visceral obesity in PA value. Therefore, we aimed to evaluate associations among frailty, visceral fat depots and PA in patients with symptomatic severe AS.
Methods
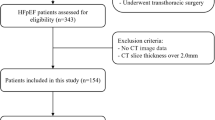
In a cohort of patients with symptomatic severe AS and preserved ejection fraction, we examined the associations between frailty, visceral fat depots and bioelectrical impedance analysis (BIA) derived phase angle (PA); and between visceral fat and PA. Frailty was defined according the Fried et al. scale criteria and the body fat distribution was determined by multidetector computed tomography and by BIA.
Results
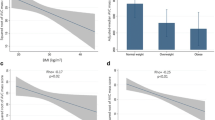
Of the fifty-five included patients, 26 were frail (47%). Adjusting for age and gender, frailty was associated with indexed epicardial adipose tissue volume (EATVi) (the odds of frailty increased 4.1-fold per additional 100 cm3/m2 of EAT [95% confidence interval (CI) of 1.03 to 16.40, p=0.04] and with PA (OR of 0.50, 95% CI, 0.26 to 0.97, p=0.04), but not with body mass index (BMI), waist circumference (WC), indexed total, visceral and subcutaneous abdominal fat areas (TAFAi, VAFAi and SAFAi) nor with indexed mediastinal adipose tissue volume (MATVi). In an age and gender adjusted linear model, PA was inversely correlated with EATVi (β=-0.008, 95% CI, -0.016 to -0.001, p=0.03), but not with BMI, WC, nor with MATVi, VAFAi, SAFAi and TAFAi.
Conclusions
In patients with symptomatic severe AS, EATVi is associated with frailty, independently of age and gender, but not with MAFVi or VAFAi. Moreover, frailty and EATVi are associated with impaired cell membrane integrity and function assessed by PA.







Similar content being viewed by others
References
O’Brien SM, Shahian DM, Filardo G, Ferraris VA, Haan CK, Rich JB, et al. The Society of Thoracic Surgeons 2008 cardiac surgery risk models: part 2—isolated valve surgery. The Annals of Thoracic Surgery. 2009;88(1 Suppl):S23–42.
Nashef SA, Roques F, Sharples LD, Nilsson J, Smith C, Goldstone AR, et al. EuroSCORE II. European Journal of Cardio-thoracic Surgery: official journal of the European Association for Cardio-thoracic Surgery. 2012;41(4):734–44; discussion 44-5.
Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, 3rd, Guyton RA, et al. 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: executive summary: a report of the American College of Cardiology/ American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(23):2440–92.
Ferrucci L, Cavazzini C, Corsi A, Bartali B, Russo CR, Lauretani F, et al. Biomarkers of frailty in older persons. Journal of Endocrinological Investigation. 2002;25(10 Suppl):10–5.
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. The Journals of Gerontology Series A, Biological Sciences and Medical Sciences. 2001;56(3):M146–56.
Woods NF, LaCroix AZ, Gray SL, Aragaki A, Cochrane BB, Brunner RL, et al. Frailty: emergence and consequences in women aged 65 and older in the Women’s Health Initiative Observational Study. Journal of the American Geriatrics Society. 2005;53(8):1321–30.
Aarts S, Patel KV, Garcia ME, Van Den Akker M, Verhey FRJ, Metsemakers JFM, et al. Co-presence of multimorbidity and disability with frailty: An examination of heterogeneity in the frail older population. J Frailty Aging. 2015;4(3):131–8.
Vellas B. Implementing Frailty Screening, Assessment, and Sustained Intervention: The experience of the Gerontopole. The Journal of Nutrition, Health & Aging. 2015;19(6):673–80.
Santos-Eggimann B, Cuenoud P, Spagnoli J, Junod J. Prevalence of frailty in middleaged and older community-dwelling Europeans living in 10 countries. The Journals of Gerontology Series A, Biological Sciences and Medical Sciences. 2009;64(6):675–81.
Green P, Woglom AE, Genereux P, Daneault B, Paradis JM, Schnell S, et al. The impact of frailty status on survival after transcatheter aortic valve replacement in older adults with severe aortic stenosis: a single-center experience. JACC Cardiovascular Interventions. 2012;5(9):974–81.
Ewe SH, Ajmone Marsan N, Pepi M, Delgado V, Tamborini G, Muratori M, et al. Impact of left ventricular systolic function on clinical and echocardiographic outcomes following transcatheter aortic valve implantation for severe aortic stenosis. American Heart Journal. 2010;160(6):1113–20.
Kalyani RR, Varadhan R, Weiss CO, Fried LP, Cappola AR. Frailty status and altered glucose-insulin dynamics. The Journals of Gerontology Series A, Biological Sciences and Medical Sciences. 2012;67(12):1300–6.
Kyle UG, Bosaeus I, De Lorenzo AD, Deurenberg P, Elia M, Gomez JM, et al. Bioelectrical impedance analysis—part I: review of principles and methods. Clinical Nutrition (Edinburgh, Scotland). 2004;23(5):1226–43.
Selberg O, Selberg D. Norms and correlates of bioimpedance phase angle in healthy human subjects, hospitalized patients, and patients with liver cirrhosis. European Journal of Applied Physiology. 2002;86(6):509–16.
Bosy-Westphal A, Danielzik S, Dorhofer RP, Later W, Wiese S, Muller MJ. Phase angle from bioelectrical impedance analysis: population reference values by age, sex, and body mass index. JPEN Journal of Parenteral and enteral Nutrition. 2006;30(4):309–16.
Lukaski HCaS, M. G. Phase angle as a prognostic indicator in cancer. Procedings of the AAAI. 2011;1:37–41.
Gupta D, Lammersfeld CA, Burrows JL, Dahlk SL, Vashi PG, Grutsch JF, et al. Bioelectrical impedance phase angle in clinical practice: implications for prognosis in advanced colorectal cancer. The American Journal of Clinical Nutrition. 2004;80(6):1634–8.
Mushnick R, Fein PA, Mittman N, Goel N, Chattopadhyay J, Avram MM. Relationship of bioelectrical impedance parameters to nutrition and survival in peritoneal dialysis patients. Kidney International Supplement. 2003(87):S53-6.
Gupta D, Lis CG, Dahlk SL, Vashi PG, Grutsch JF, Lammersfeld CA. Bioelectrical impedance phase angle as a prognostic indicator in advanced pancreatic cancer. The British Journal of Nutrition. 2004;92(6):957–62.
Lang RM BM, Devereux RB, et al. Recommendations for chamber quantification. European Journal of Echocardiography: the journal of the Working Group on Echocardiography of the European Society of Cardiology. 2006;7:79–108.
Fess. E. Grip strength. In: Casanova J, editor. Clinical assessment recommendations. 2nd ed. Chicago: American Society of Hand Therapists; 1992. p. p. 41–5.
Stewart A, Marfell-Jones, M., Olds, T., and de Ridder, H. International standards for anthropometric assessment. ISAK: Lower Hutt, New Zealand. 2011.
Kyle UG, Genton L, Karsegard L, Slosman DO, Pichard C. Single prediction equation for bioelectrical impedance analysis in adults aged 20—94 years. Nutrition. 2001;17(3):248–53.
Lukaski HC, Johnson PE, Bolonchuk WW, Lykken GI. Assessment of fat-free mass using bioelectrical impedance measurements of the human body. The American Journal of Clinical Nutrition. 1985;41(4):810–7.
Du Bois D, Du Bois EF. A formula to estimate the approximate surface area if height and weight be known. 1916. Nutrition. 1989;5(5):303–11; discussion 12-3.
Borkan GA, Gerzof SG, Robbins AH, Hults DE, Silbert CK, Silbert JE. Assessment of abdominal fat content by computed tomography. The American Journal of Clinical Nutrition. 1982;36(1):172–7.
Yoshizumi T, Nakamura T, Yamane M, Islam AH, Menju M, Yamasaki K, et al. Abdominal fat: standardized technique for measurement at CT. Radiology. 1999;211(1):283–6.
Ashwell M, Cole TJ, Dixon AK. Obesity: new insight into the anthropometric classification of fat distribution shown by computed tomography. British Medical Journal (Clinical research ed). 1985;290(6483):1692–4.
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, et al. Recommendations for chamber quantification. Eur J Echocardiogr. 2006;7(2):79–108.
Rosenhek R, Binder T, Porenta G, Lang I, Christ G, Schemper M, et al. Predictors of outcome in severe, asymptomatic aortic stenosis. The New England journal of medicine. 2000;343(9):611–7.
Shah K, Hilton TN, Myers L, Pinto JF, Luque AE, Hall WJ. A new frailty syndrome: central obesity and frailty in older adults with the human immunodeficiency virus. Journal of the American Geriatrics Society. 2012;60(3):545–9.
Blaum CS, Xue QL, Michelon E, Semba RD, Fried LP. The association between obesity and the frailty syndrome in older women: the Women’s Health and Aging Studies. Journal of the American Geriatrics Society. 2005;53(6):927–34.
Hubbard RE, Lang IA, Llewellyn DJ, Rockwood K. Frailty, body mass index, and abdominal obesity in older people. The Journals of Gerontology Series A, Biological Sciences and Medical Sciences. 2010;65(4):377–81.
Romero-Corral A, Somers VK, Sierra-Johnson J, Thomas RJ, Collazo-Clavell ML, Korinek J, et al. Accuracy of body mass index in diagnosing obesity in the adult general population. International Journal of Obesity (2005). 2008;32(6):959–66.
Sampaio LR, Simoes EJ, Assis AM, Ramos LR. Validity and reliability of the sagittal abdominal diameter as a predictor of visceral abdominal fat. Arquivos brasileiros de endocrinologia e metabologia. 2007;51(6):980–6.
Illouz F, Roulier V, Rod A, Gallois Y, Pelle CP, Aube C, et al. Distribution of adipose tissue: quantification and relationship with hepatic steatosis and vascular profiles of type 2 diabetic patients with metabolic syndrome. Diabetes & Metabolism. 2008;34(1):68–74.
Despres JP, Lemieux I. Abdominal obesity and metabolic syndrome. Nature. 2006;444(7121):881–7.
Iacobellis G, Corradi D, Sharma AM. Epicardial adipose tissue: anatomic, biomolecular and clinical relationships with the heart. Nature Clinical Practice Cardiovascular Medicine. 2005;2(10):536–43.
Ormseth MJ, Lipson A, Alexopoulos N, Hartlage GR, Oeser AM, Bian A, et al. Association of epicardial adipose tissue with cardiometabolic risk and metabolic syndrome in patients with rheumatoid arthritis. Arthritis Care & Research. 2013;65(9):1410–5.
Sam S, Haffner S, Davidson MH, D’Agostino RB, Sr., Feinstein S, Kondos G, et al. Relationship of abdominal visceral and subcutaneous adipose tissue with lipoprotein particle number and size in type 2 diabetes. Diabetes. 2008;57(8):2022–7.
Xu Y, Cheng X, Hong K, Huang C, Wan L. How to interpret epicardial adipose tissue as a cause of coronary artery disease: a meta-analysis. Coronary Artery Disease. 2012;23(4):227–33.
Erdogan T, Cetin M, Kocaman SA, Durakoglugil ME, Ergul E, Ugurlu Y, et al. Epicardial adipose tissue is independently associated with increased left ventricular mass in untreated hypertensive patients: an observational study. Anadolu kardiyoloji dergisi: AKD = the Anatolian Journal of Cardiology. 2013;13(4):320–7.
Capoulade R, Larose E, Mathieu P, Clavel MA, Dahou A, Arsenault M, et al. Visceral adiposity and left ventricular mass and function in patients with aortic stenosis: the PROGRESSA study. The Canadian Journal of Cardiology. 2014;30(9):1080–7.
Cetin M, Kocaman SA, Durakoglugil ME, Erdogan T, Ergul E, Dogan S, et al. Effect of epicardial adipose tissue on diastolic functions and left atrial dimension in untreated hypertensive patients with normal systolic function. Journal of Cardiology. 2013;61(5):359–64.
Fontes-Carvalho R, Fontes-Oliveira M, Sampaio F, Mancio J, Bettencourt N, Teixeira M, et al. Influence of epicardial and visceral fat on left ventricular diastolic and systolic functions in patients after myocardial infarction. The American Journal of Cardiology. 2014;114(11):1663–9.
Mazurek T, Zhang L, Zalewski A, Mannion JD, Diehl JT, Arafat H, et al. Human epicardial adipose tissue is a source of inflammatory mediators. Circulation. 2003;108(20):2460–6.
Baker AR, Silva NF, Quinn DW, Harte AL, Pagano D, Bonser RS, et al. Human epicardial adipose tissue expresses a pathogenic profile of adipocytokines in patients with cardiovascular disease. Cardiovascular Diabetology. 2006;5:1.
Marchington JM, Pond CM. Site-specific properties of pericardial and epicardial adipose tissue: the effects of insulin and high-fat feeding on lipogenesis and the incorporation of fatty acids in vitro. International Journal of Obesity. 1990;14(12):1013–22.
Bettencourt N, Toschke AM, Leite D, Rocha J, Carvalho M, Sampaio F, et al. Epicardial adipose tissue is an independent predictor of coronary atherosclerotic burden. International Journal of Cardiology. 2012;158(1):26–32.
Oikawa M, Owada T, Yamauchi H, Misaka T. Epicardial adipose tissue reflects the presence of coronary artery disease: comparison with abdominal visceral adipose tissue. BioMed Research International. 2015;2015:483982.
Lin J, Lopez EF, Jin Y, Van Remmen H, Bauch T, Han HC, et al. Age-related cardiac muscle sarcopenia: Combining experimental and mathematical modeling to identify mechanisms. Experimental Gerontology. 2008;43(4):296–306.
Beyer I, Mets T, Bautmans I. Chronic low-grade inflammation and agerelated sarcopenia. Current Opinion in Clinical Nutrition and Metabolic Care. 2012;15(1):12–22.
Wilhelm-Leen ER, Hall YN, Horwitz RI, Chertow GM. Phase angle, frailty and mortality in older adults. Journal of General Internal Medicine. 2014;29(1):147–54.
Visser M, van Venrooij LM, Wanders DC, de Vos R, Wisselink W, van Leeuwen PA, et al. The bioelectrical impedance phase angle as an indicator of undernutrition and adverse clinical outcome in cardiac surgical patients. Clinical Nutrition (Edinburgh, Scotland). 2012;31(6):981–6.
Doesch C, Suselbeck T, Leweling H, Fluechter S, Haghi D, Schoenberg SO, et al. Bioimpedance analysis parameters and epicardial adipose tissue assessed by cardiac magnetic resonance imaging in patients with heart failure. Obesity (Silver Spring, Md). 2010;18(12):2326–32.
Doesch C, Haghi D, Suselbeck T, Schoenberg SO, Borggrefe M, Papavassiliu T. Impact of functional, morphological and clinical parameters on epicardial adipose tissue in patients with coronary artery disease. Circulation Journal: official journal of the Japanese Circulation Society. 2012;76(10):2426–34.
Author information
Authors and Affiliations
Corresponding author
Additional information
Both authors contributed equally for this work.
Rights and permissions
About this article
Cite this article
Pinheiro, M., Mancio, J., Conceição, G. et al. Frailty syndrome: Visceral adipose tissue and frailty in patients with symptomatic severe aortic stenosis. J Nutr Health Aging 21, 120–128 (2017). https://doi.org/10.1007/s12603-016-0795-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-016-0795-x