Abstract
Purpose of the Review
Preserved ejection fraction heart failure and obesity frequently coexist. Whether obesity plays a consistent role in the pathogenesis of preserved ejection fraction heart failure is unclear. Accumulation of visceral adiposity underlies the pathogenic aftermaths of obesity. However, visceral adiposity imaging is assessed by computed tomography or magnetic resonance and thus not routinely available. In contrast, epicardial adiposity thickness is assessed by echocardiography and thus routinely available. We review the rationale for assessing epicardial adiposity thickness in patients with preserved ejection fraction heart failure and elevated body mass index.
Recent Findings
Body mass index correlates poorly with visceral, and epicardial adiposity. Visceral and epicardial adiposity enlarges as preserved ejection fraction heart failure progresses. Epicardial adiposity may hasten the progression of coronary artery disease and impairs left ventricular sub-endocardial perfusion and diastolic function.
Summary
Epicardial adiposity thickness may help monitor the therapeutic response in patients with preserved ejection failure heart failure and elevated body mass index.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Introduction
Besides prevention of water and salt retention, the pharmacologic treatment of preserved ejection heart failure (HFpEF) focuses on common metabolic and cardiovascular comorbidities such as hypertension (HT), type 2 diabetes (T2D), and arterial stiffening [1]. However, obesity and associated conditions play an increasing role in the development and progression of HFpEF [2]. Obesity contributes to the development and progression of HFpEF through accumulation of visceral and epicardial adipose tissue (VAT, EAT) that promotes low-grade systemic inflammation and adipokine dysregulation [3, 4]. Thus, imaging VAT or EAT may be helpful when assessing the response to therapy in patients with HFpEF and obesity.
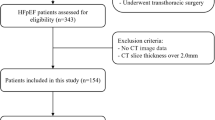
Magnetic resonance (MR) and computed tomography (CT) imaging allow direct and accurate measurement of VAT and EAT mass [5, 6]. As both imaging modalities are expensive, with CT exposing subjects to ionizing radiation and MRI being unpractical in severe obesity, VAT and EAT volumes are not readily obtained in clinical practice. Although two-dimensional (2D) echocardiography is an unreliable imaging modality for measurement of EAT volume, it reliably determines EAT thickness, a useful estimate of EAT in clinical settings [7, 8].
We review the development, characteristics, and clinical implications of VAT and EAT in the syndrome of HFpEF and advocate routine determination of EAT thickness in the management of patients with HFpEF.
Visceral Adipose Tissue
The amount of VAT is typically measured as the area of omental and mesenteric adipose tissue (AT) on a single abdominal cross-sectional slice by MR or CT at 5–6 cm above the L4-L5 disc [9]. Alternatively, the amount of VAT may be measured in 3 abdominal cross-sectional slices at L2-L3, L3-L4, and L4-L5 intervertebral spaces and average values derived from the 3 slices [10].
In response to excess intake of nutrients, lipids are stored as triglycerides (TGs) in the subcutaneous (SC) adipose tissue (SAT) surrounding the flanks, hips, buttocks, and thighs to mold the “pear shape” pattern of obesity [3, 11, 12]. When nutrient intake continues to exceed energy expenditure, the SC adipocytes become tenfold larger than in the basal state and SAT undergoes considerable accumulation [13]. When SAT reaches its maximum capacity for TG storage, visceral adipocytes start accumulating TG in the omental and mesenteric adipose depots followed by non-neuronal organs (liver, skin, vasculature, kidney, ovaries, adrenal glands, skeletal muscle, and heart) [13,14,15,16]. Regional specific differences among AT depots exist in pre-adipocyte proliferation, apoptosis, and differentiation capacity [11].
Visceral adiposity increases the risk of cardiovascular disease independent of total body adiposity [17]. Adipocyte lineages in the VAT and EAT originate from the visceral mesothelium that lines the internal organs [16]. Accumulation of VAT reflects the inability of SAT to act as a metabolic sink and to protect organs from toxic metabolites such as fatty acyl-coAs, diacylglycerides, and ceramides [3, 18, 19]. However, in turn, VAT accumulation fails to prevent storage of lipids in the liver, heart, pancreas, and skeletal muscle although it may delay it [20]. As obesity steadily progresses, reduced functional activity lowers energy expenditure thereby widening the caloric intake-energy expenditure gap and heightening the lipid storage burden [21]. Further, visceral adipocytes have a restrained capacity for lipid storage owing to a limited increase in size and a potential for hyperplasia [13]. Although visceral adipocytes do not enlarge as much as SC adipocytes, VAT accumulation triggers a stronger inflammatory compared to SAT and results in extensive visceral adipocyte necrosis and fibrosis [15, 16]. Specific adaptive AT responses to accumulation are important determinants of AT health and systemic metabolic homeostasis. Obesity-induced alterations in AT metabolism, extracellular matrix formation, immune system function, and inflammation regulate metabolic function in several organs. Differences in these factors likely contribute to heterogeneity in metabolic health in obesity [15].
Epicardial Adipose Tissue
Lying between the myocardium and visceral pericardium, EAT covers most of the right ventricle (RV) and part the left ventricle (LV) with an EAT-myocardium ratio of 0.48 for the RV and 0.15 for the LV [22] (Fig. 1). Epicardial AT surrounds large coronary arteries, and their branches as EAT occupies atrial-ventricular and interventricular grooves [23]. The thickness of healthy EAT ranges from 5 to 7 mm over the RV free wall and from 10 to 14 mm in atrial-ventricular and interventricular grooves [24]. The amount of EAT correlates weakly with body mass index (BMI) [25]. Although age, waist circumference, ethnicity, and myocardial hypertrophy are independent determinants of EAT, one unfrequently adjusts EAT thickness [26]. Both EAT and VAT originate from the splanchnopleuric mesoderm with EAT being vascularized by the coronary artery network [27].
The contiguity of adipocytes and stromal vascular fraction (resident inflammatory cells plus lymphocytes [CD3+], macrophages [CD68+], and mast cells) to coronary arteries underlies the vascular effects of EAT [28, 29••, 30]. Accumulation of EAT in the left atrioventricular groove has a strong association with coronary atheromatous plaques while excessive VAT contributes to the development of the metabolic syndrome [31]. Further, accumulation of EAT and VAT was associated with coronary atheromatous plaques in 174 patients with suspected coronary artery disease (CAD) with only EAT predicting the presence of coronary calcifications [32]. In 45 patients with CAD, EAT volume indexed to body surface area was greater around functionally significant coronary stenosis (mean fractional flow reserve [FFR] of 0.74) than around non-significant stenosis (mean FFR of 0.89) 0.34 vs 0.27 ml/m2, p = 0.045 [33]. Yu et al. corroborated the association between EAT volume and hemodynamically significant CAD in 164 patients [34].
Local expression of chemokine monocyte chemotactic protein [MCP]-1, interleukin [IL]-1β, IL-6, and tumor necrosis factor [TNF]-α RNA and protein is greater in EAT than in SAT from patients with critical CAD [28]. Heightened EAT inflammation may foster the development of coronary artery lesions. Alternatively, atherosclerosis-induced inflammation may propagate to contiguous AT [35, 36]. Nevertheless, the plasma concentration of circulating inflammatory cytokines does not reflect the degree of EAT inflammation [28]. Secretion of adiponectin, an anti-inflammatory adipokine, is 40% lower in patients with than in patients without CAD [17]. Dysregulated levels of novel adipokines and pro-inflammatory cells in EAT compared to VAT underlie the strong contribution of EAT to the pathogenesis of CAD [37]. Catecholamine-stimulated synthesis and release is greater in EAT than in other AT depots [17]. Last, protein content is greater and glucose oxidation capacity is lower in EAT than in VAT [17].
Epicardial AT expression of TNF-α is greater in patients with than in patients without non-calcified coronary plaques and is independent from coronary calcium score and clinical status [38]. Enhanced AT expression of TNF-α and increased vascular expression of endogenous endothelin (ET)-1 and ET receptor A (ETA) contribute to imbalance of the endothelin [ET]-1/nitric oxide [NO] system by impairing tonic NO release [39]. Adiponectin gene expression and thus concentration decreases significantly in epicardial adipocytes as coronary artery atherosclerosis progresses [40]. Epicardial AT expansion is inversely related to perfusion of LV sub-endocardial layers and LV global longitudinal strain in patients with CAD; sub-endocardial layer perfusion and LV strain are directly related [41]. Analysis of macrophage polarization markers reveals increased low-grade inflammation in EAT biopsies from patients with CAD [42]. Epicardial AT inflammation and neo-angiogenesis correlate with the presence of non-calcified plaques and coronary calcifications in patients with and without obstructive CAD [38]. The contribution of EAT to the progression of coronary atherosclerosis is well recognized [43, 44]. However, the usefulness of EAT attenuation for risk stratification and prediction of major acute cardiac events remains controversial in patients with CAD [45,46,47].
In patients with non-atherosclerotic vascular disease, AT surrounding arteries may release mediators that regulate vascular smooth muscle cell proliferation, matrix degradation, and neo-revascularization [48]. Release of cytokines, free fatty acids, exosomes carrying protein, lipids, ribonucleic acids (RNAs), and miRNAs from EAT to vascular smooth muscle and endothelial cells through the coronary arterial wall vasa vasorum may underlie local inflammation and coronary microvascular dysfunction [29••]. The interaction between perivascular adipose tissue (PVAT) and obesity sheds light on the impact of EAT on the coronary vasculature. In lean subjects, PVAT attenuates the vascular responsiveness to phenylephrine, angiotensin II, and ET-1 by releasing adipocyte- or perivascular-derived relaxing factors [49]. In patients with obesity, PVAT does not exert the anti-contractile effect to phenylephrine, angiotensin II, and ET-1 that PVAT exerts in lean patients [50]. The obesity triad of hypoxia, local inflammation, and oxidative stress upregulates pro-inflammatory cytokine expression in PVAT and downregulates that of adiponectin and anti-inflammatory cytokines thereby counteracting the anti-contractile effect of PVAT in lean subjects [49]. Associated with myocardial hypertrophy and capillary rarefaction, obesity causes local hypoxia that leads to fibrosis and necrosis of cardiomyocytes.
The volume of EAT by CT correlates inversely with myocardial blood flow reserve (MFR) estimated by rubidium-82 (82Rb) positron emission tomography in patients with normal myocardial perfusion imaging and no coronary artery calcifications [51]. Patients with increased EAT volume and no obstructive CAD display reduced global LV longitudinal strain (GLS) and normal global LV circumferential and radial strain [52]. Selective LV sub-endocardial layer dysfunction, as evidenced by a decrease in LV GLS, argues against myocardial fat infiltration as the cause of LV GLS decrease. Increased EAT volume may reduce MFR, thereby decreasing sub-endocardial layer perfusion and LV GLS [53]. Hence, impaired LV sub-endocardial perfusion mediates LV diastolic dysfunction in women with obesity, HFpEF, and no CAD [54]. Independent of general measures of adiposity, increased EAT thickness correlated with coronary microvascular function in 399 elderly patients [55]. Myocardial and hepatic TG contents were measured by proton magnetic resonance spectroscopy (1H-MRS), and LV function VAT volume and EAT area were measured by MR imaging in 75 non-diabetic subjects with hepatic steatosis [56]. Hepatic TG content was low in 26 subjects, moderate in 24, and high in the remaining 25 subjects. Subjects with high and moderate hepatic TG content had 2–threefold higher myocardial TG content than those with low TG hepatic content. Hepatic TG content and VAT were inversely related to LV diastolic function. In contrast, myocardial TG content was unrelated to LV diastolic function. Thus, myocardial lipotoxicity may not contribute to LV diastolic dysfunction in patients with increased VAT and EAT.
Epicardial Adipose Tissue and Preserved Ejection Fraction Heart Failure
The thickness of EAT over the RV in parasternal long- and short-axis echocardiographic views indexed to body surface area predicted incident HFpEF over a mean follow-up of 4.3 years in 379 patients with CAD and no overt HF [57]. The predictive value of EAT was independent of age, BMI, and sex. However, patients, who developed HFpEF, had presumably latent HFpEF as they were receiving more loop diuretics and renin–angiotensin–aldosterone inhibitors at enrollment in the study than patients who did not develop HFpEF were receiving [57]. Patients with HFpEF, elevated BMI, and increased EAT thickness display higher LV eccentricity index and lower peak functional capacity than their counterparts with normal EAT thickness [58]. Similarly, HFpEF patients with increased EAT thickness and BMI > 30 kg/m2 have a lower peak oxygen uptake after adjustment for pulmonary vascular resistance and BMI than patients with BMI < 30 kg/m2 and normal EAT thickness [59]. Increased EAT thickness closely correlates with arterial stiffness in HFpEF patients [60]. The mechanisms that link EAT to increased arterial stiffness remain poorly understood. The volume of EAT by MRI predicted a composite clinical outcome of all-cause mortality and first HF hospitalizations over a median follow up of 2 years in 105 patients with mid-range and preserved ejection heart failure whose BMI averaged 30 kg/m2 [8]. The predictive value of EAT was independent of BMI, age, sex, HF severity, and several comorbidities. Systemic HT was the most prevalent comorbidity; it affected 80% of patients whose mean systolic blood pressure was 140 mmHg at baseline despite treatment. As expected, 52% of patients with high EAT volume had CAD compared to 23% in patients with low EAT volume. Last, VAT was not measured and thus not entered as covariate in the multivariable Cox proportional hazard regression models.
Epicardial Versus Visceral Adipose Tissue in Preserved Ejection Fraction Heart Failure
The majority of cardiometabolic studies that assess EAT volume/thickness reports a consistent relationship between EAT and clinical outcomes [61,62,63,64]. However, cardiometabolic studies that conjointly assess the amount of VAT and cardiac AT assert that VAT mass is the overwhelming pathogenic factor in obesity except for an association between ectopic cardiac AT and coronary artery calcification or atrial fibrillation [18, 19, 26, 65].
The relative impact of AT distribution (epicardial versus visceral) on LV diastolic function may depend on the amount of VAT [66••]. Accumulation of EAT contributes to LV diastolic dysfunction in patients with low VAT mass and does not contribute to LV diastolic dysfunction in patients with high VAT mass [66••]. Both VAT and EAT contribute to LV diastolic dysfunction in patients with recent myocardial infarction (MI) [67]. However, the association between VAT and LV diastolic dysfunction is much stronger than the association between total adiposity and LV diastolic dysfunction in patients with recent MI [67]. Last, only VAT accumulation correlates with sub-clinical LV diastolic dysfunction in patients with end-stage renal disease on peritoneal dialysis [68].
Epicardial Adipose Tissue Thickness as an Endpoint in Clinical Trials
A composite of cardiovascular mortality and HF hospitalization is the prevailing primary endpoint in HF therapeutic trials. However, the incidence of cardiovascular mortality is relatively low in patients with HFpEF. Cardiovascular mortality was 8.9% over 35 months in the placebo arm of the sacubitril/valsartan HFpEF trial [69]. Non-cardiac comorbidities are highly prevalent in patients with HFpEF [70, 71]. Patients with HFpEF are as likely to be hospitalized for decompensated HFpEF as they are for worsening of non-cardiac comorbidities [72]. The incidence of HF hospitalizations was only 14.6% over 39 months in the placebo arm of the spironolactone HFpEF trial [73]. Further, HFpEF patients with high BMI are at increased risk of non-HF hospitalizations due to obesity-related comorbidities like cellulitis, deep vein thrombosis, gastrointestinal-esophageal reflux disease, or respiratory illness [74].
A randomized, placebo-controlled trial recently reported that 52 weeks with 2.4 mg of semaglutide, a glucagon-like peptide 1 receptor agonist (GLP1-RA), significantly improved HF-related symptoms and physical limitations in patients with HFpEF and a median BMI of 37.2 kg/m2 [75]. Kansas City Cardiomyopathy Clinical Questionnaire clinical summary score (KCCQ-CSS) and 6-min walk distance increased as C-reactive protein (CRP) level decreased in patients randomized to semaglutide. Whether the improvement in KCCQ-CSS and 6-min walk distance resulted from improvement(s) in obesity-related cardiac/peripheral disturbances or from a -13.3% loss body weight is unclear [75]. Semaglutide reduced CRP levels by 44, 39, and 48% in the Semaglutide Treatment Effect in People with Obesity (STEP) 1, 2 and 3 trials, and caloric reduction-induced weight loss increased peak oxygen uptake by 1.8 ml/min/kg in patients with HFpEF [76, 77]. Inclusion of epicardial adiposity as an endpoint in obesity therapeutic trials may help uncover how anti-obesity medication or procedures benefit elevated BMI patients with HFpEF besides a straight weight loss [22, 78,79,80].
In summary, visceral adipose tissue plays a larger role in the development and progression of LV diastolic dysfunction than epicardial adipose tissue although the latter may have a local impact on the coronary circulation and thereby on LV diastolic function. However, assessment of visceral adipose tissue mass requires CT or MR and thus is not routinely available in patients with HFpEF. In contrast, 2D echocardiography, which provides a reliable estimate of epicardial adipose tissue thickness, is routinely available in patients with HFpEF. Differentiating a healthy from an unhealthy metabolic status is challenging in patients with HFpEF and obesity as HT, T2D, and dyslipidemia are shared comorbidities [81]. Increased epicardial adipose tissue thickness points to a pathogenic role of obesity in patients with HFpEF and elevated BMI. Increased epicardial adipose tissue thickness signals the need to add anti-obesity medications or procedures to standard HFpEF therapy.
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Lam CSP, Voors AA, de Boer RA, Solomon SD, van Veldhuisen DJ. Heart failure with preserved ejection fraction: from mechanisms to therapies. Eur Heart J. 2018;39(30):2780–92. https://doi.org/10.1093/eurheartj/ehy301.
Borlaug BA, Jensen MD, Kitzman DW, Lam CSP, Obokata M, Rider OJ. Obesity and heart failure with preserved ejection fraction: new insights and pathophysiological targets. Cardiovasc Res. 2023;118(18):3434–50. https://doi.org/10.1093/cvr/cvac120.
Stefan N. Causes, consequences, and treatment of metabolically unhealthy fat distribution. Lancet Diabetes Endocrinol. 2020;8(7):616–27. https://doi.org/10.1016/S2213-8587(20)30110-8.
Neeland IJ, Ross R, Despres JP, Matsuzawa Y, Yamashita S, Shai I, et al. Visceral and ectopic fat, atherosclerosis, and cardiometabolic disease: a position statement. Lancet Diabetes Endocrinol. 2019;7(9):715–25. https://doi.org/10.1016/S2213-8587(19)30084-1.
Neeland IJ, Hughes C, Ayers CR, Malloy CR, Jin ES. Effects of visceral adiposity on glycerol pathways in gluconeogenesis. Metabolism. 2017;67:80–9. https://doi.org/10.1016/j.metabol.2016.11.008.
Pou KM, Massaro JM, Hoffmann U, Vasan RS, Maurovich-Horvat P, Larson MG, et al. Visceral and subcutaneous adipose tissue volumes are cross-sectionally related to markers of inflammation and oxidative stress: the framingham heart study. Circulation. 2007;116(11):1234–41. https://doi.org/10.1161/CIRCULATIONAHA.107.710509.
van Woerden G, van Veldhuisen DJ, Westenbrink BD, de Boer RA, Rienstra M, Gorter TM. Connecting epicardial adipose tissue and heart failure with preserved ejection fraction: mechanisms, management and modern perspectives. Eur J Heart Fail. 2022;24(12):2238–50. https://doi.org/10.1002/ejhf.2741.
van Woerden G, van Veldhuisen DJ, Manintveld OC, van Empel VPM, Willems TP, de Boer RA, et al. Epicardial adipose tissue and outcome in heart failure with mid-range and preserved ejection fraction. Circ Heart Fail. 2022;15(3):e009238. https://doi.org/10.1161/CIRCHEARTFAILURE.121.009238.
Seimon RV, Wild-Taylor AL, Keating SE, McClintock S, Harper C, Gibson AA, et al. Effect of weight loss via severe vs moderate energy restriction on lean mass and body composition among postmenopausal women with obesity: the TEMPO diet randomized clinical trial. JAMA Netw Open. 2019;2(10):e1913733. https://doi.org/10.1001/jamanetworkopen.2019.13733.
Covassin N, Sert-Kuniyoshi FH, Singh P, Romero-Corral A, Davison DE, Lopez-Jimenez F, et al. Experimental weight gain increases ambulatory blood pressure in healthy subjects: implications of visceral fat accumulation. Mayo Clin Proc. 2018;93(5):618–26. https://doi.org/10.1016/j.mayocp.2017.12.012.
Vishvanath L, Gupta RK. Contribution of adipogenesis to healthy adipose tissue expansion in obesity. J Clin Invest. 2019;129(10):4022–31. https://doi.org/10.1172/JCI129191.Thepaperunderlinestheimportanceofsubcutaneouswhiteadiposetissueexpansioninmaintenanceofmetabolicallyhealthyobesity.
Rana MN, Neeland IJ. Adipose tissue inflammation and cardiovascular disease: an update. Curr Diab Rep. 2022;22(1):27–37. https://doi.org/10.1007/s11892-021-01446-9.
Ghaben AL, Scherer PE. Adipogenesis and metabolic health. Nat Rev Mol Cell Biol. 2019;20(4):242–58. https://doi.org/10.1038/s41580-018-0093-z.
Despres JP. Body fat distribution and risk of cardiovascular disease: an update. Circulation. 2012;126(10):1301–13. https://doi.org/10.1161/CIRCULATIONAHA.111.067264.
Klein S, Gastaldelli A, Yki-Jarvinen H, Scherer PE. Why does obesity cause diabetes? Cell Metab. 2022;34(1):11–20. https://doi.org/10.1016/j.cmet.2021.12.012.
Kahn CR, Wang G, Lee KY. Altered adipose tissue and adipocyte function in the pathogenesis of metabolic syndrome. J Clin Invest. 2019;129(10):3990–4000. https://doi.org/10.1172/JCI129187.
Gruzdeva O, Borodkina D, Uchasova E, Dyleva Y, Barbarash O. Localization of fat depots and cardiovascular risk. Lipids Health Dis. 2018;17(1):218. https://doi.org/10.1186/s12944-018-0856-8.
Chartrand DJ, Murphy-Despres A, Almeras N, Lemieux I, Larose E, Despres JP. Overweight, obesity, and CVD risk: a focus on visceral/ectopic fat. Curr Atheroscler Rep. 2022;24(4):185–95. https://doi.org/10.1007/s11883-022-00996-x.
Britton KA, Massaro JM, Murabito JM, Kreger BE, Hoffmann U, Fox CS. Body fat distribution, incident cardiovascular disease, cancer, and all-cause mortality. J Am Coll Cardiol. 2013;62(10):921–5. https://doi.org/10.1016/j.jacc.2013.06.027.
Despres JP, Lemieux I, Bergeron J, Pibarot P, Mathieu P, Larose E, et al. Abdominal obesity and the metabolic syndrome: contribution to global cardiometabolic risk. Arterioscler Thromb Vasc Biol. 2008;28(6):1039–49. https://doi.org/10.1161/ATVBAHA.107.159228.
Stencel J, Alai HR, Dhore-Patil A, Urina-Jassir D, Le Jemtel TH. Obesity, preserved ejection fraction heart failure, and left ventricular remodeling. J Clin Med. 2023. https://doi.org/10.3390/jcm12093341.
Cheladze P, Martuszewski A, Poreba R, Gac P. The importance of the assessment of epicardial adipose tissue in scientific research. J Clin Med. 2022. https://doi.org/10.3390/jcm11195621.
Bergman RN, Kim SP, Catalano KJ, Hsu IR, Chiu JD, Kabir M, et al. Why visceral fat is bad: mechanisms of the metabolic syndrome. Obesity (Silver Spring). 2006;14(Suppl 1):16S–S19. https://doi.org/10.1038/oby.2006.277.
Iacobellis G, Willens HJ. Echocardiographic epicardial fat: a review of research and clinical applications. J Am Soc Echocardiogr. 2009;22(12):1311–9; quiz 417–8. https://doi.org/10.1016/j.echo.2009.10.013.
Peczkowski KK, Mashali MA, Saad NS, Hare A, Campbell CM, Whitson BA, et al. Quantification of cardiac adipose tissue in failing and nonfailing human myocardium. J Am Heart Assoc. 2022;11(13):e025405. https://doi.org/10.1161/JAHA.121.025405.
Le Jemtel TH, Samson R, Ayinapudi K, Singh T, Oparil S. Epicardial adipose tissue and cardiovascular disease. Curr Hypertens Rep. 2019;21(5):36. https://doi.org/10.1007/s11906-019-0939-6.
Antonopoulos AS, Antoniades C. The role of epicardial adipose tissue in cardiac biology: classic concepts and emerging roles. J Physiol. 2017;595(12):3907–17. https://doi.org/10.1113/JP273049.
Mazurek T, Zhang L, Zalewski A, Mannion JD, Diehl JT, Arafat H, et al. Human epicardial adipose tissue is a source of inflammatory mediators. Circulation. 2003;108(20):2460–6. https://doi.org/10.1161/01.CIR.0000099542.57313.C5.
•• Ansaldo AM, Montecucco F, Sahebkar A, Dallegri F, Carbone F. Epicardial adipose tissue and cardiovascular diseases. Int J Cardiol. 2019;278:254–60. https://doi.org/10.1016/j.ijcard.2018.09.089. The paper focuses on the cross talk between epicardial adipose tissue and coronary atherosclerosis as well as the relationship between dysfunctional epicardial adipose tissue and impair cardiac structure and function.
Turkmen K, Ozer H, Kusztal M. The relationship of epicardial adipose tissue and cardiovascular disease in chronic kidney disease and hemodialysis patients. J Clin Med. 2022;11(5):1308. https://doi.org/10.3390/jcm11051308.
Wu FZ, Wu CC, Kuo PL, Wu MT. Differential impacts of cardiac and abdominal ectopic fat deposits on cardiometabolic risk stratification. BMC Cardiovasc Disord. 2016;16:20. https://doi.org/10.1186/s12872-016-0195-5.
Oikawa M, Owada T, Yamauchi H, Misaka T, Machii H, Yamaki T, et al. Epicardial adipose tissue reflects the presence of coronary artery disease: comparison with abdominal visceral adipose tissue. Biomed Res Int. 2015;2015:483982. https://doi.org/10.1155/2015/483982.
Du Y, Yang L, Liu Y, Yang B, Lv S, Hu C, et al. Relation between quantity and quality of peri-coronary epicardial adipose tissue and its underlying hemodynamically significant coronary stenosis. BMC Cardiovasc Disord. 2020;20(1):226. https://doi.org/10.1186/s12872-020-01499-w.
Yu W, Chen Y, Zhang F, Liu B, Wang J, Shao X, et al. Association of epicardial adipose tissue volume with increased risk of hemodynamically significant coronary artery disease. Quant Imaging Med Surg. 2023;13(4):2582–93. https://doi.org/10.21037/qims-22-709.
Ngo DT, Gokce N. Epicardial adipose tissue: a benign consequence of obesity? Circ Cardiovasc Imaging. 2015. https://doi.org/10.1161/CIRCIMAGING.115.003156.
Ahmadieh S, Kim HW, Weintraub NL. Potential role of perivascular adipose tissue in modulating atherosclerosis. Clin Sci (Lond). 2020;134(1):3–13. https://doi.org/10.1042/CS20190577.
Fan W, Si Y, Xing E, Feng Z, Ding Z, Liu Y, et al. Human epicardial adipose tissue inflammation correlates with coronary artery disease. Cytokine. 2023;162:156119. https://doi.org/10.1016/j.cyto.2022.156119.
Kitagawa T, Yamamoto H, Hattori T, Sentani K, Takahashi S, Senoo A, et al. Tumor necrosis factor-alpha gene expression in epicardial adipose tissue is related to coronary atherosclerosis assessed by computed tomography. J Atheroscler Thromb. 2018;25(3):269–80. https://doi.org/10.5551/jat.41178.
Virdis A, Duranti E, Rossi C, Dell’Agnello U, Santini E, Anselmino M, et al. Tumour necrosis factor-alpha participates on the endothelin-1/nitric oxide imbalance in small arteries from obese patients: role of perivascular adipose tissue. Eur Heart J. 2015;36(13):784–94. https://doi.org/10.1093/eurheartj/ehu072.
Gruzdeva OV, Belik EV, Dyleva YA, Borodkina DA, Sinitsky MY, Naumov DY, et al. Expression of adipocytokines in heart fat depots depending on the degree of coronary artery atherosclerosis in patients with coronary artery disease. PLoS ONE. 2021;16(3):e0248716. https://doi.org/10.1371/journal.pone.0248716.
Zhu J, Xie Z, Huang H, Li W, Zhuo K, Bai Z, Huang R. Association of epicardial adipose tissue with left ventricular strain and MR myocardial perfusion in patients with known coronary artery disease. J Magn Reson Imaging. 2023. https://doi.org/10.1002/jmri.28619.
Papotti B, Opstad TB, Akra S, Tonnessen T, Braathen B, Hansen CH, et al. Macrophage polarization markers in subcutaneous, pericardial, and epicardial adipose tissue are altered in patients with coronary heart disease. Front Cardiovasc Med. 2023;10:1055069. https://doi.org/10.3389/fcvm.2023.1055069.
Nerlekar N, Brown AJ, Muthalaly RG, Talman A, Hettige T, Cameron JD, Wong DTL. Association of epicardial adipose tissue and high-risk plaque characteristics: a systematic review and meta-analysis. J Am Heart Assoc. 2017. https://doi.org/10.1161/JAHA.117.006379.
Muthalaly RG, Nerlekar N, Wong DT, Cameron JD, Seneviratne SK, Ko BS. Epicardial adipose tissue and myocardial ischemia assessed by computed tomography perfusion imaging and invasive fractional flow reserve. J Cardiovasc Comput Tomogr. 2017;11(1):46–53. https://doi.org/10.1016/j.jcct.2016.12.007.
Wen D, Ren Z, Xue R, An R, Xu J, Li J, Zheng M. Lack of incremental prognostic value of pericoronary adipose tissue computed tomography attenuation beyond coronary artery disease reporting and data system for major adverse cardiovascular events in patients with acute chest pain. Circ Cardiovasc Imaging. 2023;16(7):536–44. https://doi.org/10.1161/CIRCIMAGING.122.015120.
Lin A, Nerlekar N, Yuvaraj J, Fernandes K, Jiang C, Nicholls SJ, Dey D, Wong DTL. Pericoronary adipose tissue computed tomography attenuation distinguishes different stages of coronary artery disease: a cross-sectional study. Eur Heart J Cardiovasc Imaging. 2021;22(3):298–306. https://doi.org/10.1093/ehjci/jeaa224.
Napoli G, Pergola V, Basile P, De Feo D, Bertrandino F, Baggiano A, Mushtaq S, Fusini L, Fazzari F, Carrabba N, Rabbat MG, Motta R, Ciccone MM, Pontone G, Guaricci AI. Epicardial and pericoronary adipose tissue, coronary inflammation, and acute coronary syndromes. J Clin Med. 2023;12(23):7212. https://doi.org/10.3390/jcm12237212.PMID:38068263;PMCID:PMC10707039.
Horimatsu T, Kim HW, Weintraub NL. The role of perivascular adipose tissue in non-atherosclerotic vascular disease. Front Physiol. 2017;8:969. https://doi.org/10.3389/fphys.2017.00969.
Xia N, Li H. The role of perivascular adipose tissue in obesity-induced vascular dysfunction. Br J Pharmacol. 2017;174(20):3425–42. https://doi.org/10.1111/bph.13650.
Greenstein AS, Khavandi K, Withers SB, Sonoyama K, Clancy O, Jeziorska M, et al. Local inflammation and hypoxia abolish the protective anticontractile properties of perivascular fat in obese patients. Circulation. 2009;119(12):1661–70. https://doi.org/10.1161/CIRCULATIONAHA.108.82118.
Nappi C, Ponsiglione A, Acampa W, Gaudieri V, Zampella E, Assante R, et al. Relationship between epicardial adipose tissue and coronary vascular function in patients with suspected coronary artery disease and normal myocardial perfusion imaging. Eur Heart J Cardiovasc Imaging. 2019;20(12):1379–87. https://doi.org/10.1093/ehjci/jez182.
Maimaituxun G, Kusunose K, Yamada H, Fukuda D, Yagi S, Torii Y, et al. Deleterious effects of epicardial adipose tissue volume on global longitudinal strain in patients with preserved left ventricular ejection fraction. Front Cardiovasc Med. 2020;7: 607825. https://doi.org/10.3389/fcvm.2020.607825.
Rabkin SW. Is reduction in coronary blood flow the mechanism by which epicardial fat produces left ventricular diastolic dysfunction? Can J Cardiol. 2017;33(11):1459–61. https://doi.org/10.1016/j.cjca.2017.08.013.
Markley R, Del Buono MG, Mihalick V, Pandelidis A, Trankle C, Jordan JH, et al. Abnormal left ventricular subendocardial perfusion and diastolic function in women with obesity and heart failure and preserved ejection fraction. Int J Cardiovasc Imaging. 2023;39(4):811–9. https://doi.org/10.1007/s10554-022-02782-x.
Mahmoud I, Dykun I, Karner L, Hendricks S, Totzeck M, Al-Rashid F, et al. Epicardial adipose tissue differentiates in patients with and without coronary microvascular dysfunction. Int J Obes (Lond). 2021;45(9):2058–63. https://doi.org/10.1038/s41366-021-00875-6.
Graner M, Nyman K, Siren R, Pentikainen MO, Lundbom J, Hakkarainen A, et al. Ectopic fat depots and left ventricular function in nondiabetic men with nonalcoholic fatty liver disease. Circ Cardiovasc Imaging. 2015. https://doi.org/10.1161/CIRCIMAGING.114.001979.
Mahabadi AA, Anapliotis V, Dykun I, Hendricks S, Al-Rashid F, Ludike P, et al. Epicardial fat and incident heart failure with preserved ejection fraction in patients with coronary artery disease. Int J Cardiol. 2022;357:140–5. https://doi.org/10.1016/j.ijcard.2022.04.009.
Koepp KE, Obokata M, Reddy YNV, Olson TP, Borlaug BA. Hemodynamic and functional impact of epicardial adipose tissue in heart failure with preserved ejection fraction. JACC Heart Fail. 2020;8(8):657–66. https://doi.org/10.1016/j.jchf.2020.04.016.
Gorter TM, van Woerden G, Rienstra M, Dickinson MG, Hummel YM, Voors AA, et al. Epicardial adipose tissue and invasive hemodynamics in heart failure with preserved ejection fraction. JACC Heart Fail. 2020;8(8):667–76. https://doi.org/10.1016/j.jchf.2020.06.003.
Liu Z, Hu W, Zhang H, Tao H, Lei P, Liu J, et al. EAT thickness as a predominant feature for evaluating arterial stiffness in patients with heart failure with preserved ejection fraction. Diabetes Metab Syndr Obes. 2022;15:1217–26. https://doi.org/10.2147/DMSO.S356001.
Krishnan A, Sharma H, Yuan D, Trollope AF, Chilton L. The role of epicardial adipose tissue in the development of atrial fibrillation, coronary artery disease and chronic heart failure in the context of obesity and type 2 diabetes mellitus: a narrative review. J Cardiovasc Dev Dis. 2022. https://doi.org/10.3390/jcdd9070217.
Venkateshvaran A, Faxen UL, Hage C, Michaelsson E, Svedlund S, Saraste A, et al. Association of epicardial adipose tissue with proteomics, coronary flow reserve, cardiac structure and function, and quality of life in heart failure with preserved ejection fraction: insights from the PROMIS-HFpEF study. Eur J Heart Fail. 2022;24(12):2251–60. https://doi.org/10.1002/ejhf.2709.
Christensen RH, Hansen CS, von Scholten BJ, Jensen MT, Pedersen BK, Schnohr P, et al. Epicardial and pericardial adipose tissues are associated with reduced diastolic and systolic function in type 2 diabetes. Diabetes Obes Metab. 2019;21(8):2006–11. https://doi.org/10.1111/dom.13758.
Song Y, Song F, Wu C, Hong Y-X, Li G. The roles of epicardial adipose tissue in heart failure. Heart Fail Rev. 2022;27(1):369–77. https://doi.org/10.1007/s10741-020-09997-x.
Rosito GA, Massaro JM, Hoffmann U, Ruberg FL, Mahabadi AA, Vasan RS, et al. Pericardial fat, visceral abdominal fat, cardiovascular disease risk factors, and vascular calcification in a community-based sample: the Framingham Heart Study. Circulation. 2008;117(5):605–13. https://doi.org/10.1161/CIRCULATIONAHA.107.743062.
•• Takahari K, Utsunomiya H, Itakura K, Yamamoto H, Nakano Y. Impact of the distribution of epicardial and visceral adipose tissue on left ventricular diastolic function. Heart Vessels. 2022;37(2):250–61. https://doi.org/10.1007/s00380-021-01904-0. A rare study where the investigators assess conjointly the effects of epicardial adipose tissue and visceral adipose tissue on left ventricular diastolic function. The effect of epicardial adipose tissue depends on the amount of visceral adipose tissue.
Fontes-Carvalho R, Fontes-Oliveira M, Sampaio F, Mancio J, Bettencourt N, Teixeira M, et al. Influence of epicardial and visceral fat on left ventricular diastolic and systolic functions in patients after myocardial infarction. Am J Cardiol. 2014;114(11):1663–9. https://doi.org/10.1016/j.amjcard.2014.08.037.
Wu CK, Huang YT, Lin HH, Yang CY, Lien YC, Lee JK, et al. Dissecting the mechanisms of left ventricular diastolic dysfunction and inflammation in peritoneal dialysis patients. PLoS ONE. 2013;8(5):e62722. https://doi.org/10.1371/journal.pone.0062722.
Solomon SD, McMurray JJV, Anand IS, Ge J, Lam CSP, Maggioni AP, et al. Angiotensin-neprilysin inhibition in heart failure with preserved ejection fraction. N Engl J Med. 2019;381(17):1609–20. https://doi.org/10.1056/NEJMoa1908655.
Hogg K, Swedberg K, McMurray J. Heart failure with preserved left ventricular systolic function; epidemiology, clinical characteristics, and prognosis. J Am Coll Cardiol. 2004;43(3):317–27. https://doi.org/10.1016/j.jacc.2003.07.046.
Edelmann F, Stahrenberg R, Gelbrich G, Durstewitz K, Angermann CE, Dungen HD, et al. Contribution of comorbidities to functional impairment is higher in heart failure with preserved than with reduced ejection fraction. Clin Res Cardiol. 2011;100(9):755–64. https://doi.org/10.1007/s00392-011-0305-4.
Ather S, Chan W, Bozkurt B, Aguilar D, Ramasubbu K, Zachariah AA, et al. Impact of noncardiac comorbidities on morbidity and mortality in a predominantly male population with heart failure and preserved versus reduced ejection fraction. J Am Coll Cardiol. 2012;59(11):998–1005. https://doi.org/10.1016/j.jacc.2011.11.040.
Pitt B, Pfeffer MA, Assmann SF, Boineau R, Anand IS, Claggett B, et al. Spironolactone for heart failure with preserved ejection fraction. N Engl J Med. 2014;370(15):1383–92. https://doi.org/10.1056/nejmoa1313731.
Heymsfield SB, Wadden TA. Mechanisms, pathophysiology, and management of obesity. N Engl J Med. 2017;376(3):254–66. https://doi.org/10.1056/nejmra1514009.
Kosiborod MN, Abildstrom SZ, Borlaug BA, Butler J, Rasmussen S, Davies M, et al. Semaglutide in patients with heart failure with preserved ejection fraction and obesity. N Engl J Med. 2023. https://doi.org/10.1056/NEJMoa2306963.
Verma S, Bhatta M, Davies M, Deanfield JE, Garvey WT, Jensen C, et al. Effects of once-weekly semaglutide 2.4 mg on C-reactive protein in adults with overweight or obesity (STEP 1, 2, and 3): exploratory analyses of three randomised, double-blind, placebo-controlled, phase 3 trials. eClinicalMedicine. 2023;55:101737. https://doi.org/10.1016/j.eclinm.2022.101737.
Kitzman DW, Brubaker P, Morgan T, Haykowsky M, Hundley G, Kraus WE, et al. Effect of caloric restriction or aerobic exercise training on peak oxygen consumption and quality of life in obese older patients with heart failure with preserved ejection fraction. JAMA. 2016;315(1):36. https://doi.org/10.1001/jama.2015.17346.
Salvatore T, Galiero R, Caturano A, Vetrano E, Rinaldi L, Coviello F, et al. Dysregulated epicardial adipose tissue as a risk factor and potential therapeutic target of heart failure with preserved ejection fraction in diabetes. Biomolecules. 2022;12(2):176. https://doi.org/10.3390/biom12020176.
Myasoedova VA, Parisi V, Moschetta D, Valerio V, Conte M, Massaiu I, et al. Efficacy of cardiometabolic drugs in reduction of epicardial adipose tissue: a systematic review and meta-analysis. Cardiovasc Diabetol. 2023. https://doi.org/10.1186/s12933-023-01738-2.
Christensen RH, Wedell-Neergaard A-S, Lehrskov LL, Legaard GE, Dorph E, Larsen MK, et al. Effect of aerobic and resistance exercise on cardiac adipose tissues. JAMA Cardiology. 2019;4(8):778. https://doi.org/10.1001/jamacardio.2019.2074.
Bluher M. Metabolically healthy obesity. Endocr Rev. 2020. https://doi.org/10.1210/endrev/bnaa004.
Acknowledgements
Current Hypertension Reports is grateful to Dr. John Hall, for his review of this manuscript.
Author information
Authors and Affiliations
Contributions
Conceptualization of idea: T.L.J., Literature search: T.L.J, A.D.P, D.U.J. Draft manuscript: A.D.P, D.U.J, R.S, Review and editing: D.U.J, R.S, T.L.J, S.O, Critical revision: T.L.J, S.O. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interests
The authors did not receive support from any organization for the submitted work. Financial interests: All authors declare they have no financial interests. Non-financial interests: Dr. Suzanne Oparil was the editor-in-chief of Current of Hypertension Reports.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dhore-Patil, A., Urina-Jassir, D., Samson, R. et al. Epicardial Adipose Tissue Thickness and Preserved Ejection Fraction Heart Failure. Curr Hypertens Rep 26, 381–388 (2024). https://doi.org/10.1007/s11906-024-01302-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11906-024-01302-7