Abstract
Background
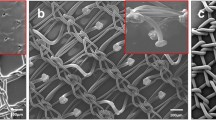
Atraumatic fixation is a key element of modern hernia repair. Two different concepts of self-adhering meshes were directly compared in this study. Adhesix® (AH) is coated with polyethylene glycol (PEG) and polyvinylpyrrolidone (PVP), whereas Parietene Progrip® (PP) relies on the mechanical principle of micro grips made of polylactic acid (PLA). These meshes are the main competitors in the field.
Methods
AH and PP were tested in Sprague–Dawley rats at 14 and 90 days. Four groups were operated (n = 8 animals per group). Two meshes were implanted per animal in an operation model of onlay hernia repair. Dislocation, tissue integration and foreign-body reaction were evaluated.
Results
AH dislocated significantly more frequently (every second mesh) at both time points of observation than PP. Tissue integration was good with PP and could not be reliably assessed in AH due to frequent dislocation. Histologic examination revealed only a mild foreign body reaction in all groups.
Conclusions
In our hands, PP (mechanical grip fixation) was superior to hydrogel fixation with PEG and PVP in AH in an onlay model. The reason for dislocation of AH requires further clarification as well as the impact of long-term degradation of the PLA grips.






Similar content being viewed by others
References
Petter-Puchner A, Fortelny R, Mittermayr R, Ohlinger W, Redl H (2005) Fibrin sealing vs. stapling of hernia meshes in an onlay model in the rat. Hernia 9:322–329
Gruber-Blum S, Petter-Puchner AH, Mika K, Brand J, Redl H, Ohlinger W, Benesch T, Fortelny RH (2010) A comparison of a bovine albumin/glutaraldehyde glue versus fibrin sealant for hernia mesh fixation in experimental onlay and IPOM repair in rats. Surg Endosc 24:3086–3094
Fortelny RH, Petter-Puchner AH, Ferguson J, Gruber-Blum S, Brand J, Mika K, Redl H (2011) A comparative biomechanical evaluation of hernia mesh fixation by fibrin sealant. J Surg Res 171:576–581
Schwab R, Schumacher O, Junge K, Binnebosel M, Klinge U, Becker HP, Schumpelick V (2008) Biomechanical analyses of mesh fixation in TAPP and TEP hernia repair. Surg Endosc 22:731–738
Kingsnorth AN, Shahid MK, Valliattu AJ, Hadden RA, Porter CS (2008) Open onlay mesh repair for major abdominal wall hernias with selective use of components separation and fibrin sealant. World J Surg 32:26–30
Baer A, Sauer T, Bohnert N, Gortezki PE, Lammers BJ (2009) Less pain intensity after Liechtenstein-repair by using biolgue for mesh fixation. www surgicaltechnology com0-STI-XVIII-Articles/243-Bar-Galley02 pdf
Kim-Fuchs C, Angst E, Vorburger S, Helbling C, Candinas D, Schlumpf R (2012) Prospective randomized trial comparing sutured with sutureless mesh fixation for Lichtenstein hernia repair: long-term results. Hernia 16:21–27
Schopf S, von AT, von AM, Schardey H (2011) Chronic pain after laparoscopic transabdominal preperitoneal hernia repair: a randomized comparison of light and extralight titanized polypropylene mesh. World J Surg 35:302–310
Fortelny RH, Schwab R, Glaser KS, Puchner KU, May C, Konig F, Redl H, Petter-Puchner AH (2008) The assessment of quality of life in a trial on lightweight mesh fixation with fibrin sealant in transabdominal preperitoneal hernia repair. Hernia 12:499–505
Furst W, Banerjee A (2005) Release of glutaraldehyde from an albumin-glutaraldehyde tissue adhesive causes significant in vitro and in vivo toxicity. Ann Thorac Surg 79:1522–1528
Fortelny RH, Petter-Puchner AH, Walder N, Mittermayr R, Ohlinger W, Heinze A, Redl H (2007) Cyanoacrylate tissue sealant impairs tissue integration of macroporous mesh in experimental hernia repair. Surg Endosc 21:1781–1785
Jourdan IC, Bailey ME (1998) Initial experience with the use of N-butyl 2-cyanoacrylate glue for the fixation of polypropylene mesh in laparoscopic hernia repair. Surg Laparosc Endosc 8:291–293
Shirai T, Shimota H, Chida K, Sano S, Takeuchi Y, Yasueda H (2005) Anaphylaxis to aprotinin in fibrin sealant. Intern Med 44:1088–1089
Fortelny RH, Petter-Puchner AH, May C, Jaksch W, Benesch T, Khakpour Z, Redl H, Glaser KS (2011) The impact of atraumatic fibrin sealant vs. staple mesh fixation in TAPP hernia repair on chronic pain and quality of life: results of a randomized controlled study. Surg Endosc 26:249–254
Champault G, Polliand C, Dufour F, Ziol M, Behr L (2009) A “self adhering” prosthesis for hernia repair: experimental study. Hernia 13:49–52
Petter-Puchner AH, Fortelny RH, Mittermayr R, Walder N, Ohlinger W, Redl H (2006) Adverse effects of porcine small intestine submucosa implants in experimental ventral hernia repair. Surg Endosc 20:942–946
Johansson M, Gunnarsson U, Strigard K (2011) Different techniques for mesh application give the same abdominal muscle strength. Hernia 15:65–68
Hollinsky C, Kolbe T, Walter I, Joachim A, Sandberg S, Koch T, Rulicke T (2009) Comparison of a new self-gripping mesh with other fixation methods for laparoscopic hernia repair in a rat model. J Am Coll Surg 208:1107–1114
Jenkins ED, Lerdsirisopon S, Costello KP, Melman L, Greco SC, Frisella MM, Matthews BD, Deeken CR (2011) Laparoscopic fixation of biologic mesh at the hiatus with fibrin or polyethylene glycol sealant in a porcine model. Surg Endosc 25:3405–3413
Ferland R, Campbell PK (2009) Pre-clinical evaluation of a next-generation spray adhesion barrier for multiple site adhesion protection. Surg Technol Int 18:137–143
Champault G, Torcivia A, Paolino L, Chaddad W, Lacaine F, Barrat C (2011) A self-adhering mesh for inguinal hernia repair: preliminary results of a prospective, multicenter study. Hernia 15:635–641
Greca FH, Souza-Filho ZA, Giovanini A, Rubin MR, Kuenzer RF, Reese FB, Araujo LM (2008) The influence of porosity on the integration histology of two polypropylene meshes for the treatment of abdominal wall defects in dogs. Hernia 12:45–49
Schumpelick V, Klinge U, Junge K, Stumpf M (2004) Incisional abdominal hernia: the open mesh repair. Langenbecks Arch Surg 389:1–5
Kapischke M, Schulze H, Caliebe A (2010) Self-fixating mesh for the Lichtenstein procedure–a prestudy. Langenbecks Arch Surg 395:317–322
Bruna EM, Cantos PM, Artigues Sanchez De RE (2010) Use of adhesive mesh in hernioplasty compared to the conventional technique. Results of a randomised prospective study. Cir Esp 88:253–258
Kosai N, Sutton PA, Evans J, Varghese J (2011) Laparoscopic preperitoneal mesh repair using a novel self-adhesive mesh. J Minim Access Surg 7:192–194
Birk D, Hess S, Garcia-Pardo C (2013) Low recurrence rate and low chronic pain associated with inguinal hernia repair by laparoscopic placement of Parietex ProGrip™ mesh: clinical outcomes of 220 hernias with mean follow-up at 23 months. Hernia 17(3):313–320
Lambrecht J (2011) Overlap-coefficient for the relationship between mesh size and defect size in laparoscopic ventral hernia surgery. Hernia 15:473–474
Pielacinski K, Dabrowski W, Szczepanik AB, Misiak A (2011) Self-fixating Progrip implant used in the laparoscopic totally extraperitoneal technique for inguinal hernia repair. Pol Merkur Lekarski 31:345–347
Conflict of interest
HR. is a consultant to Baxter Innovations, Austria. S. G-B, N. R., J. B., C. K., R. F. and A. P-P. have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gruber-Blum, S., Riepl, N., Brand, J. et al. A comparison of Progrip® and Adhesix® self-adhering hernia meshes in an onlay model in the rat. Hernia 18, 761–769 (2014). https://doi.org/10.1007/s10029-014-1258-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-014-1258-0