Abstract
Background
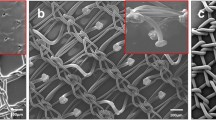
Mesh fixation in hernia repair is currently based on penetrating sutures or anchors, with proven early and late complications such as pain, adhesions, erosions, and anchor migration. In an attempt to reduce these complications, a bio-adhesive-based self-fixation system was developed. The purpose of this study was to assess the performance and safety of this novel self-adhesive mesh (LifeMesh™) by comparing it with standard tack fixation.
Methods
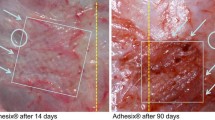
A full-thickness abdominal wall defect was created bilaterally in 24 pigs. The defects were measured 14 days later, and laparoscopic intraperitoneal onlay mesh (IPOM) repairs were performed. In each animal, both LifeMesh and a titanium tack-fixed control, either uncoated polypropylene mesh (PP) or composite mesh (Symbotex™), were used. After 28 and 90 days, we performed macroscopic evaluation and analyzed the fixation strength, shrinkage, adhesion scores, and histopathology in all samples.
Results
Measurements at both time points revealed that LifeMesh had fully conformed to the abdominal wall, and that its fixation strength was superior to that of the tack-fixated Symbotex and comparable to that of the tack-fixated PP. Shrinkage in all groups was similar. Adhesion scores with LifeMesh were lower than with PP and comparable with Symbotex at both time points. Histology demonstrated similar tissue responses in LifeMesh and Symbotex. Lack of necrosis, mineralization, or exuberant inflammatory reaction in all three groups pointed to their good progressive integration of the mesh to the abdominal wall. By 28 days the bio-adhesive layer in LifeMesh was substantially degraded, allowing a gradual tissue ingrowth that became the main fixation mode of this mesh to the abdominal wall.
Conclusions
The excellent incorporation of LifeMesh to the abdominal wall and its superior fixation strength, together with its low adhesion score, suggest that LifeMesh may become a preferred alternative for abdominal wall repair.






Similar content being viewed by others
References
Kingsnorth A (2004) Treating inguinal hernias. BMJ. https://doi.org/10.1136/bmj.328.7431.59
Baylón K, Rodríguez-Camarillo P, Elías-Zúñiga A, Díaz-Elizondo JA, Gilkerson R, Lozano K (2017) Past, present and future of surgical meshes: a review. Membranes (Basel) 7(3):47
Beldi G, Wagner M, Bruegger LE, Kurmann A, Candinas D (2011) Mesh shrinkage and pain in laparoscopic ventral hernia repair: a randomized clinical trial comparing suture versus tack mesh fixation. Surg Endosc. https://doi.org/10.1007/s00464-010-1246-0
Bageacu S, Blanc P, Breton C, Gonzales M, Porcheron J, Chabert M, Balique JG (2002) Laparoscopic repair of incisional hernia: a retrospective study of 159 patients. Surg Endosc Other Interv Tech. https://doi.org/10.1007/s00464-001-0018-2
Reynvoet E, Berrevoet F (2014) Pros and cons of tacking in laparoscopic hernia repair. Surg Technol Int 25(136):40
Karahasanoglu T, Onur E, Baca B, Hamzaoglu I, Pekmezci S, Boler DE, Kilic N, Altug T (2004) Spiral tacks may contribute to intra-abdominal adhesion formation. Surg Today. https://doi.org/10.1007/s00595-004-2831-4
Gungor B, Malazgirt Z, Topgül K, Gök A, Bilgin M, Yürüker S (2010) Comparative Evaluation of Adhesions to Intraperitoneally Placed Fixation Materials: a Laparoscopic Study in Rats. Indian J Surg. 72(6):475–480. https://doi.org/10.1007/s12262-010-0168-3
Haltmeier T, Groebli Y (2013) Small bowel lesion due to spiral tacks after laparoscopic intraperitoneal onlay mesh repair for incisional hernia. Int J Surg Case Rep. https://doi.org/10.1016/j.ijscr.2012.12.005
Peach G, Tan LC (2008) Small bowel obstruction and perforation due to a displaced spiral tacker: a rare complication of laparoscopic inguinal hernia repair. Hernia 12(3):303–305. https://doi.org/10.1007/s10029-007-0289-1
Fitzgerald HL, Orenstein SB, Novitsky YW (2010) Small bowel obstruction owing to displaced spiral tack after laparoscopic TAPP inguinal hernia repair. Surg Laparosc Endosc Percutaneous Tech 20(3):e132–e135. https://doi.org/10.1097/sle.0b013e3181dfbc05
Kenton K, FitzGerald MP, Brubaker L (2002) Multiple foreign body erosions after laparoscopic colposuspension with mesh. Am J Obstet Gynecol. https://doi.org/10.1067/mob.2002.124288
Wirsching A, Vonlanthen R, Lehmann K (2014) Gallbladder perforation by absorbable spiral tacker. Ann R Coll Surg Engl 3:150. https://doi.org/10.1308/003588414x13946184902280
Malmstrøm ML, Thorlacius-Ussing O (2010) Cardiac tamponade as a rare complication in laparoscopic incisional hernia repair. Hernia 14:421–422. https://doi.org/10.1007/s10029-009-0557-3
Golash V (2008) Large gut fistula due to a protruding spiral tacker after laparoscopic repair of a ventral hernia. Oman Med J 23(1):50
Ladurner R, Mussack T (2004) Small bowel perforation due to protruding spiral tackers: a rare complication in laparoscopic incisional hernia repair. Surg Endosc. https://doi.org/10.1007/s00464-003-4276-z
Paz YE, Vazquez J, Bessler M (2011) Cardiac tamponade as a complication of laparoscopic hiatal hernia repair: case report and literature review. Catheter Cardiovasc Interv 3:150. https://doi.org/10.1002/ccd.23178
Baltazar G, Coakley K, Badiwala A, Chendrasekhar A (2013) Ventral hernia mesh tack causes liver hemorrhage. Hernia 3:150. https://doi.org/10.1007/s10029-012-1001-7
Feliu X, Claveria R, Besora P, Luque D, Vinas X (2011) A calcified foreign body in the bladder due to: an unusual complication after laparoscopic incisional hernia repair. Surg Laparosc Endosc Percutan Tech. https://doi.org/10.1097/sle.0b013e31820660fc
Lantis JC, Schwaitzberg SD (1999) Tack Entrapment of the Ilioinguinal Nerve during Laparoscopic Hernia Repair. J Laparoendosc Adv Surg Tech. https://doi.org/10.1089/lap.1999.9.285
Chevallier JM, Wind P, Lassau JP (1996) Damage to the inguino-femoral nerves in the treatment of hernias. An anatomical hazard of traditional and laparoscopic techniques. Ann Chir 50(9):767–775
Reinpold W, Schroeder AD, Schroeder M, Berger C, Rohr M, Wehrenberg U (2015) Retroperitoneal anatomy of the iliohypogastric, ilioinguinal, genitofemoral, and lateral femoral cutaneous nerve: consequences for prevention and treatment of chronic inguinodynia. Hernia. https://doi.org/10.1007/s10029-015-1396-z
Stark E, Oestreich K, Wendl K, Rumstadt B, Hagmüller E (1999) Nerve irritation after laparoscopic hernia repair. Surg Endosc. https://doi.org/10.1007/s004649901124
Hiremath BV, Rajasridhar B, Pipara G (2012) Tack sinus: a new complication of laparoscopic ventral hernia repair. World J Laparosc Surg. https://doi.org/10.5005/jp-journals-10007-1159
Reynvoet E, Berrevoet F, De Somer F, Vercauteren G, Vanoverbeke I, Chiers K, Troisi R (2012) Tensile strength testing for resorbable mesh fixation systems in laparoscopic ventral hernia repair. Surg Endosc Other Interv Tech 3:150. https://doi.org/10.1007/s00464-012-2224-5
Poobalan AS, Bruce J, Smith WC, King PM, Krukowski ZH, Chambers WA (2003) A review of chronic pain after inguinal herniorrhaphy. Clin J Pain 19(1):48–54. https://doi.org/10.1097/00002508-200301000-00006
Gillian GK, Geis WP, Grover G (2002) Laparoscopic incisional and ventral hernia repair (LIVH): an evolving outpatient technique. JSLS 6(4):315
Antoniou SA, Köhler G, Antoniou GA, Muysoms FE, Pointner R, Granderath FA (2016) Meta-analysis of randomized trials comparing nonpenetrating vs mechanical mesh fixation in laparoscopic inguinal hernia repair. Am J Surg 211(1):239–249. https://doi.org/10.1016/j.amjsurg.2015.06.008
Harslof SS, Wara P, Friis-Andersen H (2014) Fixation devices in laparoscopic ventral hernia repair: a review. Surg Technol Int 24:203–213
Labori KJ, Trondsen E, Buanes T, Hauge T (2009) Endoscopic sealing of pancreatic fistulas: four case reports and review of the literature. Scand J Gastroenterol 3:150. https://doi.org/10.3109/00365520903362610
Lindsey I, Smilgin-Humphreys MM, Cunningham C, Mortensen NJM, George BD (2002) A randomized, controlled trial of fibrin glue vs. conventional treatment for anal fistula. Dis Colon Rectum. https://doi.org/10.1097/01.dcr.0000034622.59957.55
Pascual G, Sotomayor S, Rodríguez M, Pérez-Köhler B, Kühnhardt A, Fernández-Gutiérrez M, San Román J, Bellón JM (2016) Cytotoxicity of cyanoacrylate-based tissue adhesives and short-term preclinical in vivo biocompatibility in abdominal hernia repair. PLoS ONE 11:e0157920. https://doi.org/10.1371/journal.pone.0157920
Samson D, Marshall D (1986) Carcinogenic potential of isobutyl-2-cyanoacrylate. J Neurosurg 65(4):571–572. https://doi.org/10.3171/jns.1986.65.4.0571a
Fortelny RH, Petter-Puchner AH, Walder N, Mittermayr R, Öhlinger W, Heinze A, Redl H (2007) Cyanoacrylate tissue sealant impairs tissue integration of macroporous mesh in experimental hernia repair. Surg Endosc Other Interv Tech 21:1781–1785. https://doi.org/10.1007/s00464-007-9243-7
Sanders DL, Waydia S (2014) A systematic review of randomised control trials assessing mesh fixation in open inguinal hernia repair. Hernia 30:150. https://doi.org/10.1007/s10029-013-1093-8
Fernández Lobato R, García Septiem J, Ortega Deballon P, Marín Lucas FJ, Ruíz De Adana JC, Limones Esteban M (2001) Tissucol application in dermolipectomy and incisional hernia repair. Int Surg 86(4):240–245
Chevrel JP, Rath AM, Chevrel P (1997) The use of fibrin glues in the surgical treatment of incisional hernias. Hernia. https://doi.org/10.1007/bf02426381
Campanelli G, Pascual MH, Hoeferlin A, Rosenberg J, Champault G, Kingsnorth A, Miserez M (2012) Randomized, controlled, blinded trial of tisseel/tissucol for mesh fixation in patients undergoing lichtenstein technique for primary inguinal hernia repair: results of the TIMELI trial. Ann Surg. https://doi.org/10.1097/sla.0b013e31824b32bf
Bracale U, Rovani M, Picardo A, Merola G, Pignata G, Sodo M, Di Salvo E, Ratto EL, Noceti A, Melillo P, Pecchia L (2014) Beneficial effects of fibrin glue (Quixil) versus Lichtenstein conventional technique in inguinal hernia repair: a randomized clinical trial. Hernia. https://doi.org/10.1007/s10029-012-1020-4
Liu H, Zheng X, Gu Y, Guo S (2015) A meta-analysis examining the use of fibrin glue mesh fixation versus suture mesh fixation in open inguinal hernia repair. Dig Surg 31(6):444–451. https://doi.org/10.1159/000370249
Schreinemacher MHF, van Barneveld KWY, Peeters E, Miserez M, Gijbels MJJ, Greve JWM, Bouvy ND (2014) Adhesions to sutures, tackers, and glue for intraperitoneal mesh fixation: an experimental study. Hernia 18:865–872. https://doi.org/10.1007/s10029-013-1192-6
Schug-Pass C, Lippert H, Köckerling F (2009) Fixation of mesh to the peritoneum using a fibrin glue: Investigations with a biomechanical model and an experimental laparoscopic porcine model. Surg Endosc Other Interv Tech. https://doi.org/10.1007/s00464-009-0509-0
Jenkins ED, Melman L, Desai S, Brown SR, Frisella MM, Deeken CR, Matthews BD (2011) Evaluation of intraperitoneal placement of absorbable and nonabsorbable barrier coated mesh secured with fibrin sealant in a New Zealand white rabbit model. Surg Endosc Other Interv Tech 25(2):604–612. https://doi.org/10.1007/s00464-010-1230-8
Shahan CP, Stoikes NN, Roan E, Tatum J, Webb DL, Voeller GR (2017) Short-term strength of non-penetrating mesh fixation: LifeMesh???, Tisseel???, and ProGrip??? Surg Endosc Other Interv Tech 31:1350–1353. https://doi.org/10.1007/s00464-016-5119-z
Shahan CP, Stoikes NN, Roan E, Tatum J, Webb DLVG (2018) Biomechanical and histologic evaluation of LifeMesh™: biomechanical and histologic evaluation of LifeMesh™: a novel self-fixating mesh adhesive. Am Surg 84:520–525
Sahoo S, Baker AR, Haskins IN, Krpata DM, Rosen MJ, Derwin KA (2017) Development of a critical-sized ventral hernia model in the pig. J Surg Res 210:115–123. https://doi.org/10.1016/j.jss.2016.10.026
Cobb WS, Burns JM, Kercher KW, Matthews BD, James Norton H, Todd Heniford B (2005) Normal intraabdominal pressure in healthy adults. J Surg Res 129:231–235. https://doi.org/10.1016/j.jss.2005.06.015
Gudmundsson FF, Viste A, Gislason H, Svanes K (2002) Comparison of different methods for measuring intra-abdominal pressure. Intensive Care Med. https://doi.org/10.1007/s00134-001-1187-0
Baptista ML, Bonsack ME, Felemovicius I, Delaney JP (2000) Abdominal adhesions to prosthetic mesh evaluated by laparoscopy and electron microscopy. J Am Coll Surg. https://doi.org/10.1016/s1072-7515(99)00277-x
Surgical Membrane Study Group (1992) Prophylaxis of pelvic sidewall adhesions with Gore-Tex surgical membrane: *a multicenter clinical investigation. Fertil Steril 57:921–923. https://doi.org/10.1016/s0015-0282(16)54981-4
Tagaya N, Mikami H, Aoki H, Kubota K (2004) Long-term complications of laparoscopic ventral and incisional hernia repair. Surg Laparosc Endosc Percutan Tech. https://doi.org/10.1097/00129689-200402000-00002
Eubanks S, Newman L 3rd, Goehring L, Lucas GW, Adams CP, Mason E, Duncan T (1993) Meralgia paresthetica: a complication of laparoscopic herniorrhaphy. Surg Laparosc Endosc 3(5):381–385
Phillips EH, Arregui M, Carroll BJ, Corbitt J, Crafton WB, Fallas MJ, Filipi C, Fitzgibbons RJ, Franklin MJ, McKernan B, Olsen D, Ortega A, Payne JH, Peters J, Rodriguez R, Rosette P, Schultz L, Seid A, Sewell R, Smoot R, Toy F, Waddell R, Watson S (1995) Incidence of complications following laparoscopic hernioplasty. Surg Endosc. https://doi.org/10.1007/bf00187878
Toosie K, Gallego K, Stabile BE, Schaber B, French S, De Virgilio C (2000) Fibrin glue reduces intra-abdominal adhesions to synthetic mesh in a rat ventral hernia model. Am Surg 66(1):41
Petter-Puchner AH, Fortelny R, Mittermayr R, Öhlinger W, Redl H (2005) Fibrin sealing versus stapling of hernia meshes in an onlay model in the rat. Hernia. https://doi.org/10.1007/s10029-005-0009-7
Garcia-Vallejo L, Couto-Gonzalez I, Concheiro-Coello P, Brea-Garcia B, Taboada-Suarez A (2014) Cyanoacrylate surgical glue for mesh fixation in laparoscopic total extraperitoneal hernia repair. Surg Laparosc Endosc Percutaneous Tech. https://doi.org/10.1097/sle.0b013e3182a2f008
Jourdan IC, Bailey ME (1998) Initial experience with the use of n-butyl 2-cyanoacrylate glue for the fixation of polypropylene mesh in laparoscopic hernia repair. Surg Laparosc Endosc Percutaneous Tech. https://doi.org/10.1097/00019509-199808000-00011
Topart P, Vandenbroucke F, Lozac’h P (2005) Tisseel vs tack staples as mesh fixation in totally extraperitoneal laparoscopic repair of groin hernias: a retrospective analysis. Surg Endosc Other Interv Tech. https://doi.org/10.1007/s00464-004-8812-2
Novik B, Hagedorn S, Mörk UB, Dahlin K, Skullman S, Dalenbäck J (2006) Fibrin glue for securing the mesh in laparoscopic totally extraperitoneal inguinal hernia repair: a study with a 40-month prospective follow-up period. Surg Endosc Other Interv Tech. https://doi.org/10.1007/s00464-005-0391-3
Lovisetto F, Zonta S, Rota E, Mazzilli M, Bardone M, Bottero L, Faillace G, Longoni M (2007) Use of human fibrin glue (Tissucol) versus staples for mesh fixation in laparoscopic transabdominal preperitoneal hernioplasty: a prospective, randomized study. Ann Surg. https://doi.org/10.1097/01.sla.0000245832.59478.c6
Canonico S, Santoriello A, Campitiello F, Fattopace A, Della Corte A, Sordelli I, Benevento R (2005) Mesh fixation with human fibrin glue (Tissucol) in open tension-free inguinal hernia repair: a preliminary report. Hernia. https://doi.org/10.1007/s10029-005-0020-z
Jenkins ED, Melman L, Frisella MM, Deeken CR, Matthews BD (2010) Evaluation of acute fixation strength of absorbable and nonabsorbable barrier coated mesh secured with fibrin sealant. Hernia 14:505–509. https://doi.org/10.1007/s10029-010-0670-3
Shahan CP, Stoikes NN, Roan E, Tatum J, Webb DL, Voeller GR (2017) Short-term strength of non-penetrating mesh fixation: Lifemesh™, Tisseel™, and ProGrip™. Surg Endosc Other Interv Tech. https://doi.org/10.1007/s00464-016-5119-z
Eriksen JR, Bisgaard T, Assaadzadeh S, Jorgensen LN, Rosenberg J (2013) Fibrin sealant for mesh fixation in laparoscopic umbilical hernia repair: 1-year results of a randomized controlled double-blinded study. Hernia 17:511–514. https://doi.org/10.1007/s10029-013-1101-z
Schug-Pass C, Lippert H, Köckerling F (2010) Mesh fixation with fibrin glue (Tissucol/Tisseel??) in hernia repair dependent on the mesh structure—is there an optimum fibrin-mesh combination?—investigations on a biomechanical model. Langenbeck’s Arch Surg 395:569–574. https://doi.org/10.1007/s00423-009-0466-z
Leggat PA, Smith DR, Kedjarune U (2007) Surgical applications of cyanoacrylate adhesives: a review of toxicity. ANZ J Surg 77(4):209–213
Leggat PA, Kedjarune U, Smith DR (2004) Toxicity of cyanoacrylate adhesives and their occupational impacts for dental staff. Ind Health. https://doi.org/10.2486/indhealth.42.207
Dinsmore RC, Calton WC, Harvey SB, Blaney MW (2000) Prevention of adhesions to polypropylene mesh in a traumatized bowel model. J Am Coll Surg. https://doi.org/10.1016/s1072-7515(00)00337-9
Eriksen JR, Gögenur I, Rosenberg J (2007) Choice of mesh for laparoscopic ventral hernia repair. Hernia 11(6):481–492
Junge K, Binnebösel M, Rosch R, Jansen M, Kämmer D, Otto J, Schumpelick V, Klinge U (2009) Adhesion formation of a polyvinylidenfluoride/polypropylene mesh for intra-abdominal placement in a rodent animal model. Surg Endosc Other Interv Tech 23:327–333. https://doi.org/10.1007/s00464-008-9923-y
Divilio LT (2005) Surgical adhesion development and prevention. Int Surg 90(3 Suppl):S6
DiZerega GS, Campeau JD (2001) Peritoneal repair and post-surgical adhesion formation. Hum Reprod Update. https://doi.org/10.1093/humupd/7.6.547
Nohuz E, Alaboud M, Darcha C, Alloui A, Aublet-Cuvelier B, Jacquetin B (2014) Effectiveness of Hyalobarrier and Seprafilm to prevent polypropylene mesh shrinkage: a macroscopic and histological experimental study. Int Urogynecol J Pelvic Floor Dysfunct. https://doi.org/10.1007/s00192-014-2357-2
Jonas J (2009) The problem of mesh shrinkage in laparoscopic incisional hernia repair. Zentralbl Chir. https://doi.org/10.1055/s-0028-1098779
Acknowledgments
The study was funded by LifeBond Ltd., Caesarea, Israel.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
The study was funded by LifeBond LTD, Caesarea, Israel. Dr. Ben Yehuda Amir is a medical advisor to LifeBond and reports personal fees from LifeBond, during the conduct of the study. Dr. Szold Amir is a medical advisor to LifeBond and reports personal fees from LifeBond, during the conduct of the study. Dr. Nyska Abraham has no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ben Yehuda, A., Nyska, A. & Szold, A. Mesh fixation using novel bio-adhesive coating compared to tack fixation for IPOM hernia repair: in vivo evaluation in a porcine model. Surg Endosc 33, 2364–2375 (2019). https://doi.org/10.1007/s00464-019-06806-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-06806-x