Abstract
Background
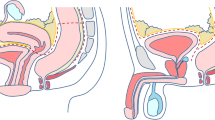
The role of fecal diversion with pelvic anastomosis during cytoreductive surgery (CRS) with hyperthermic intraperitoneal chemotherapy (HIPEC) is not well defined.
Methods
A retrospective review of patients who underwent CRS and HIPEC between 2009 and 2016 was performed to identify those with a pelvic anastomosis (colorectal, ileorectal, or coloanal anastomosis).
Results
The study identified 73 patients who underwent CRS and HIPEC at three different institutions between July 2009 and June of 2016. Of these patients, 32 (44%) underwent a primary anastomosis with a diverting ileostomy, whereas 41 (56%) underwent a primary anastomosis without fecal diversion. The anastomotic leak rate for the no-diversion group was 22% compared with 0% for the group with a diverting ileostomy (p < 0.01). The 90-day mortality rate for the no-diversion group was 7.1%. The hospital stay was 14.1 ± 8.0 days in the diversion group compared with 17.9 ± 12.5 days in the no-diversion group (p = 0.12). Of those patients with a diverting ileostomy, 68% (n = 22) had their bowel continuity restored, 18% of which required a laparotomy for reversal. Postoperative complications occurred for 50% of those who required a laparotomy and for 44% of those who did not require a laparotomy (p = 0.84).
Conclusion
Diverting ileostomies in patients with a pelvic anastomosis undergoing CRS and HIPEC are associated with a significantly reduced anastomotic leak rate. Reversal of the diverting ileostomy in this patient population required a laparotomy in 18% of the cases and had an associated morbidity rate of 50%.
Similar content being viewed by others
References
Paun BC, Cassie S, Maclean AR, Dixon E, Buie WD. Postoperative complications following surgery for rectal cancer. Ann Surg. 2010;251:807–18. doi:10.1097/SLA.0b013e3181dae4ed.
Vignali A, Fazio VW, Lavery IC, et al. Factors associated with the occurrence of leaks in stapled rectal anastomoses: a review of 1014 patients. ACS. 1997;185:105–13. doi:10.1016/S1072-7515(97)00018-5.
Akiyoshi T, Ueno M, Fukunaga Y, et al. Incidence of and risk factors for anastomotic leakage after laparoscopic anterior resection with intracorporeal rectal transection and double-stapling technique anastomosis for rectal cancer. Am J Surg. 2011;202:259–64. doi:10.1016/j.amjsurg.2010.11.014.
Laparoscopic Colorectal Surgery Study Group (LCSSG), Köckerling F, Rose J, et al. Laparoscopic colorectal anastomosis: risk of postoperative leakage. Surg Endosc. 2014;13:639–44. doi:10.1007/s004649901064.
Karanjia ND, Corder AP, Bearn P, Heald RJ. Leakage from stapled low anastomosis after total mesorectal excision for carcinoma of the rectum. Br J Surg. 1994;81:1224–6. doi:10.1002/bjs.1800810850.
Trencheva K, Morrissey KP, Wells M, et al. Identifying important predictors for anastomotic leak after colon and rectal resection. Ann Surg. 2013;257:108–13. doi:10.1097/SLA.0b013e318262a6cd.
Jung SH, Yu CS, Choi PW, et al. Risk factors and oncologic impact of anastomotic leakage after rectal cancer surgery. Dis Colon Rectum. 2008;51:902–8. doi:10.1007/s10350-008-9272-x.
Rullier E, Laurent C, Garrelon JL, Michel P, Saric J, Parneix M. Risk factors for anastomotic leakage after resection of rectal cancer. Br J Surg. 1998;85:355–8. doi:10.1046/j.1365-2168.1998.00615.x.
Mäkelä JT, Kiviniemi H, Laitinen S. Risk factors for anastomotic leakage after left-sided colorectal resection with rectal anastomosis. Dis Colon Rectum. 2003;46:653–60. doi:10.1007/s10350-004-6627-9.
Sauer R, Becker H, Hohenberger W, et al. Preoperative versus postoperative chemoradiotherapy for rectal cancer. N Engl J Med. 2004;351:10. doi:10.1056/NEJMoa040694.
Kapiteijn E, Marijnen CAM, Nagtegaal ID, et al. Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer. N Engl J Med. 2001;345:638–46. doi:10.1056/NEJMoa010580.
Mealy K, Burke P, Hyland J. Anterior resection without a defunctioning colostomy: questions of safety. Br J Surg. 1992;79:305–7. doi:10.1002/bjs.1800790406.
Younan R, Kusamura S, Baratti D, et al. Bowel complications in 203 cases of peritoneal surface malignancies treated with peritonectomy and closed-technique intraperitoneal hyperthermic perfusion. Ann Surg Oncol. 2005;12:910–18. doi:10.1245/ASO.2005.11.030.
Jacquet P, Stephens AD, Averbach AM, et al. Analysis of morbidity and mortality in 60 patients with peritoneal carcinomatosis treated by cytoreductive surgery and heated intraoperative intraperitoneal chemotherapy. Cancer. 1996;77:2622–9. doi:10.1002/(SICI)1097-0142(19960615)77:12<2622::AID-CNCR28>3.0.CO;2-T.
Chua TC, Yan TD, Saxena A, Morris DL. Should the treatment of peritoneal carcinomatosis by cytoreductive surgery and hyperthermic intraperitoneal chemotherapy still be regarded as a highly morbid procedure? Ann Surg. 2009;249:900–7. doi:10.1097/SLA.0b013e3181a45d86.
de Cuba EMV, Verwaal VJ, de Hingh IHJT, et al. Morbidity associated with colostomy reversal after cytoreductive surgery and HIPEC. Ann Surg Oncol. 2013;21:883–90. doi:10.1245/s10434-013-3370-2.
Wong NY, Eu KW. A defunctioning ileostomy does not prevent clinical anastomotic leak after a low anterior resection: a prospective, comparative study. Dis Colon Rectum. 2005;48:2076–9. doi:10.1007/s10350-005-0146-1.
Matthiessen P, Hallböök O, Rutegård J, Simert G, Sjödahl R. Defunctioning stoma reduces symptomatic anastomotic leakage after low anterior resection of the rectum for cancer: a randomized multicenter trial. Ann Surg. 2008;247:719–20. doi:10.1097/SLA.0b013e31816a74b5.
Beck-Kaltenbach N, Voigt K, Rumstadt B. Renal impairment caused by temporary loop ileostomy. Int J Colorectal Dis. 2011;26:623–6. doi:10.1007/s00384-010-1086-3.
Kann BR. Early stomal complications. Clin Colon Rectal Surg. 2008;21:23–30. doi:10.1055/s-2008-1055318.
Robertson I, Leung E, Hughes D, et al. Prospective analysis of stoma-related complications. Colorectal Dis. 2005;7:279–85. doi:10.1111/j.1463-1318.2005.00785.x.
Chude GG, Rayate NV, Patris V, et al. Defunctioning loop ileostomy with low anterior resection for distal rectal cancer: should we make an ileostomy as a routine procedure? A prospective randomized study. Hepatogastroenterology. 2008;55:1562–7.
Mark K, Uranitsch S, Pedross F, et al. Colon/rectum diverting ileostomy versus no diversion after low anterior resection for rectal cancer: a prospective, randomized, multicenter trial. Surgery. 2016;159:1129–39. doi:10.1016/j.surg.2015.11.006
Seo S-I, Yu CS, Kim GS, et al. The role of diverting stoma after an ultra-low anterior resection for rectal cancer. Ann Coloproctol. 2013;29:66. doi:10.3393/ac.2013.29.2.66.
Hanna MH, Vinci A, Pigazzi A. Diverting ileostomy in colorectal surgery: when is it necessary? Langenbecks Arch Surg. 2015;400:145–52. doi:10.1007/s00423-015-1275-1.
Luglio G, Pendlimari R, Holubar SD, Cima RR, Nelson H. Loop ileostomy reversal after colon and rectal surgery: a single institutional 5-year experience in 944 patients. Arch Surg. 2011;146:1191–6. doi:10.1001/archsurg.2011.234.
Doud AN, Levine EA, Fino NF, Stewart JH, Shen P, Votanopoulos KI. Stoma creation and reversal after cytoreductive surgery with hyperthermic intraperitoneal chemotherapy. Ann Surg Oncol. 2016;23:503–10. doi:10.1245/s10434-015-4674-1.
Sugarbaker PH. Avoiding diverting ileostomy in patients requiring complete pelvic peritonectomy. Ann Surg Oncol. 2015;23:1481–5. doi:10.1245/s10434-015-4961-x.
Shiomi A, Ito M, Maeda K, et al. Effects of a diverting stoma on symptomatic anastomotic leakage after low anterior resection for rectal cancer: a propensity score matching analysis of 1014 consecutive patients. ACS. 2015;220:186–94. doi:10.1016/j.jamcollsurg.2014.10.017.
Schnüriger B, Inaba K, Wu T, Eberle BM, Belzberg H, Demetriades D. Crystalloids after primary colon resection and anastomosis at initial trauma laparotomy: excessive volumes are associated with anastomotic leakage. J Trauma Injury Infect Crit Care. 2011;70:603–10. doi:10.1097/TA.0b013e3182092abb.
Boesen AK, Maeda Y, Madsen MR. Perioperative fluid infusion and its influence on anastomotic leakage after rectal cancer surgery: implications for prevention strategies. Colorectal Dis. 2013:15:e522. doi:10.1111/codi.12321
Waterland P, Goonetilleke K, Naumann DN, Sutcliff M, Soliman F. Defunctioning ileostomy reversal rates and reasons for delayed reversal: does delay impact on complications of ileostomy reversal? A study of 170 defunctioning ileostomies. J Clin Med Res. 2015;7:685–9. doi:10.14740/jocmr2150w.
Junginger T, Gönner U, Trinh TT, Lollert A, Oberholzer K, Berres M. Permanent stoma after low anterior resection for rectal cancer. Dis Colon Rectum. 2010;53:1632–9. doi:10.1007/DCR.0b013e3181ed0aae.
Çubukçu A, Alponat A, Gönüllü NN. Mitomycin-C prevents reformation of intra-abdominal adhesions after adhesiolysis. Surgery. 2002;131:81–4. doi:10.1067/msy.2002.118316.
Çubukçu A, Alponat A, Gönüllü NN, Özkan S, Erçin C. An experimental study evaluating the effect of mitomycin C on the prevention of postoperative intraabdominal adhesions. J Surg Res. 2001;96:163–6. doi:10.1006/jsre.2000.6059.
Liu Y, Li H, Shu X, Gray S, Prestwich G. Crosslinked hyaluronan hydrogels containing mitomycin C reduce postoperative abdominal adhesions. Fertil Steril. 2005;83:1275–83. doi:10.1016/j.fertnstert.2004.09.038.
Chung J. Mitomycin C for the prevention of adhesion formation after endoscopic sinus surgery: a randomized, controlled study. Otolaryngol Head Neck Surg. 2002;126:468–74. doi:10.1067/mhn.2002.124705.
Orhan A, Görmüş N, Toy H, Görmüş IS, Çağlayan O, Tanyeli Ö. Prevention of retrosternal pericardial adhesions after cardiac surgery with mitomycin C. Heart Lung Circulation. 2014;23:357–62. doi:10.1016/j.hlc.2013.10.080.
Jacquet P, Sugarbaker PH. Abdominal adhesions causing intestinal obstruction following cytoreductive surgery and early postoperative intraperitoneal chemotherapy. Acta Chir Austriaca. 1995;27:92–5.
Markman M, Cleary S, Howell SB. Complications of extensive adhesion formation after intraperitoneal chemotherapy. Surg Gynecol Obstet. 1986;162(5):445–8.
Blouhos K, Pramateftakis M-G, Tsachalis T, et al. The integrity of colonic anastomoses following the intraperitoneal administration of oxaliplatin. Int J Colorectal Dis. 2010;25:835–41. doi:10.1007/s00384-010-0912-y.
Conflict of interest
There are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
The original version of this article was revised: Sarath Sujatha-Bhaskar’s family name was misspelled.
An erratum to this article is available at http://dx.doi.org/10.1245/s10434-017-5893-4.
Rights and permissions
About this article
Cite this article
Whealon, M.D., Gahagan, J.V., Sujatha-Bhaskar, S. et al. Is Fecal Diversion Needed in Pelvic Anastomoses During Hyperthermic Intraperitoneal Chemotherapy (HIPEC)?. Ann Surg Oncol 24, 2122–2128 (2017). https://doi.org/10.1245/s10434-017-5853-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-017-5853-z