Abstract
Background
Gastrointestinal complications, predominantly anastomotic leak (AL), are the most frequent source of severe morbidity after cytoreductive surgery (CRS).
Objective
The aim of this study was to present the technical standards for colorectal anastomoses developed and systematically applied to all patients undergoing CRS in a high-volume tertiary center, and the associated AL rates.
Methods
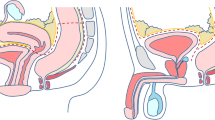
This was a descriptive study reporting the technical characteristics of a standardized protocol for three types of colorectal anastomoses (colorectal, ileorectal, and ileocolic) in CRS with heated intraperitoneal chemotherapy (HIPEC), and a retrospective analysis of prospectively collected data on anastomotic outcomes. All patients (1172) undergoing CRS with HIPEC from September 2006 to September 2020 were included. The anastomotic complications were classified according to the International Study Group of Rectal Cancer Surgery (ISGRCS) classification.
Results
Overall, 1172 patients underwent 1300 procedures and 1359 gastrointestinal anastomoses. An ileocolic anastomosis was performed in 408 patients, colorectal anastomosis in 469 patients, and ileorectal anastomosis in 16 patients, none with diverting ileostomy; 345 other gastrointestinal reconstructions and 82 urinary reconstructions were performed in these patients. The AL rate was 1% (4/408) for the ileocolic anastomosis, 0.85% (4/469) for the colorectal anastomosis, and 0% (0/16) for the ileorectal anastomosis. One patient died postoperatively due to AL.
Conclusions
Systematic application of standardized techniques adapted to ensure optimal tissue healing (stapled anastomoses avoiding overlap, accurate staple deployment, and hand-sewn reinforcement) are associated with a very high level of anastomotic safety in a large cohort of patients undergoing CRS and HIPEC.





Similar content being viewed by others
References
Moghdamyeghaneh Z, Hanna MH, Alizadeh RF, et al. Contemporary management of anastomotic leak after colon surgery: assessing the need for reoperation. Am J Surg. 2016;211:1005–13.
Takahashi H, Haraguchi N, Nishimura J, et al. The severity of anastomotic leakage may negatively impact the long term prognosis of colorectal cancer. Anticancer Res. 2018;38:533–9.
Bruce J, Krukowski ZH, Al-Khairy G, et al. Systematic review of the definition and measurement of anastomotic leak after gastrointestinal surgery. Br J Surg. 2001;88:1157–68.
Rahbari NN, Weitz J, Hohenberger W, et al. Definition and grading of anastomotic leakage following anterior resection of the rectum: a proposal by the International Study Group of Rectal Cancer. Surgery. 2010;147:339–51.
Turrentine FE, Denlinger CE, Simpson VB, et al. Morbidity, mortality, cost, and survival estimates of gastrointestinal anastomotic leaks. J Am Coll Surg. 2015;220(2):195–206.
McDermott FD, Heeney A, Kelly ME, et al. Systematic review of preoperative, intraoperative and postoperative risk factors for colorectal anastomotic leaks. BJS. 2015;102:462–79.
Golda T, Lazzara C, Martin CZ, et al. Risk factors for ileocolic anastomosis dehiscence; a cohort study. Am J Surg. 2020;220(1):170–7.
Ali Chaouch M, Kellil T, Jeddi C, et al. How to prevent anastomotic leak in colorectal surgery? A systematic review. Ann Coloproctol. 2020;36(4):213–22.
Jacquet P, Stephens AD, Averbach AM, et al. Analysis of morbidity and mortality in 60 patients with peritoneal carcinomatosis treated by cytoreductive surgery and heated intraoperative intraperitoneal chemotherapy. Cancer. 1996;77(12):2622–9.
Glehen O, Osinsky D, Cotte E, et al. Intraperitoneal chemohyperthermia using a closed abdominal procedure and cytoreductive surgery for the treatment of peritoneal carcinomatosis: morbidity and mortality analysis of 216 consecutive procedures. Ann Surg Oncol. 2003;10:863–9.
Kusamura S, Younan R, Baratti D, et al. Cytoreductive surgery followed by intraperitoneal hyperthermic perfusion: analysis of morbidity and mortality in 209 peritoneal surface malignancies treated with closed abdomen technique. Cancer. 2006;106:1144–53.
Foster JM, Sleightholm R, Patel A, et al. Morbidity and mortality rates following cytoreductive surgery combined with hyperthermic intraperitoneal chemotherapy compared with other high-risk surgical oncology procedures. JAMA Netw Open. 2019;2(1):e186847.
Sugarbaker PH, Alderman R, Edwards G, et al. Prospective morbidity and mortality assessment of cytoreductive surgery plus perioperative intraperitoneal chemotherapy to treat peritoneal dissemination of appendiceal mucinous malignancy. Ann Surg Oncol. 2006;13(5):635–44.
Kelly KJ, Cajas L, Baumgartner JM, et al. Factors associated with 60-day readmission following cytoreduction and hyperthermic intraperitoneal chemotherapy. Ann Surg Oncol. 2018;25(1):91–7.
Doud AN, Levine EA, Fino NF, et al. Stoma creation and reversal after cytoreductive surgery with hyperthermic intraperitoneal chemotherapy. Ann Surg Oncol. 2016;23(2):503–10.
Frye J, Bokey EL, Chapuis PH, et al. Anastomotic leakage after resection of colorectal cancer generates prodigious use of hospital resources. Colorectal Dis. 2009;11:917–20.
Nesbakken A, Nygaard K, Lunde OC. Outcome and late functional results after anastomotic leakage following mesorectal excision for rectal cancer. Br J Surg. 2001;88:400–4.
Konishi T, Watanabe T, Kishimoto J, et al. Risk factors for anastomotic leakage after surgery for colorectal cancer: results of prospective surveillance. J Am Coll Surg. 2006;202(3):439–44.
Mäkelä JT, Kiviniemi H, Laitinen S, et al. Risk factors for anastomotic leakage after left-sided colorectal resection with rectal anastomosis. Dis Colon Rectum. 2003;46:653–60.
Frasson M, Flor-Lorente B, Ramos Rodriguez JL, et al. Risk factors for anastomotic leak after colon resection for cancer. Multivariate analysis and nomogram from a multicentric, prospective, national study with 3193 patients. ANACO Study Group. Ann Surg. 2015;262:321–30.
Pommergaard HC, Gessler B, Burcharth J, et al. Preoperative risk factors for anastomotic leakage after resection for colorectal cancer: a systematic review and meta-analysis. Colorectal Dis. 2014;16:662–71.
Kawada K, Sakai Y. Preoperative, intraoperative and postoperative risk factors for anastomotic leakage after laparoscopic low anterior resection with double stapling technique anastomosis. World J Gastroenterol. 2016;22:5718–27.
Frasson M, Granero-Castro P, Ramos Rodriguez JL, et al. Risk factors for anastomotic leak and postoperative morbidity and mortality after elective colectomy for cancer: results from a prospective, multicentric study of 1102 patients. Int J Colorectal Dis. 2016;31(1):105–14.
van Rooijen SJ, Huisman D, Stuijvenberg M, et al. Intraoperative modifiable risk factors of colorectal anastomotic leakage: why surgeons and anesthesiologists should act together. Int J Surg. 2016;36:183–200.
Choy PYG, Bissett IP, Docherty JG. Stapled versus handsewn methods for ileocolic anastomoses. Cochrane Database Syst Rev. 2011;9:CD004320.
Docherty JG, McGregor JR, Akyol AM, et al. Scotland and Highland Anastomosis Study Group. Comparison of manually constructed and stapled anastomoses in colorectal surgery. Ann Surg. 1995;221(2):176–84.
Eto K, Urashima M, Kosuge M, et al. Standarization of surgical procedures to reduce risk of anastomotic leakage, reoperation, and surgical site infection in colorectal cancer surgery: a retrospective cohort study of 1189 patients. Int J Colorectal Dis. 2018;33(6):755–62. https://doi.org/10.1007/s00384-018-3037-3.
Archampong D, Borowski D, Wille-Jørgensen P, et al. Workload and surgeon’s specialty for outcome after colorectal cancer surgery. Cochrane Database Syst Rev. 2012;3:CD005391.
Foppa C, Ng SC, Montorsi M, et al. Anastomotic leak in colorectal cancer patients: new insights and perspectives. Eur J Surg Oncol. 2020;46(6):943–54.
Vignali A, Fazio VW, Lavery IC, et al. Factors associated with the occurrence of leaks in stapled rectal anastomoses: a review of 1014 patients. J Am Coll Surg. 1997;185:105–13.
Barrios P, Ramos I, Escayola C et al. Implementación y desarrollo de un Programa de Tratamiento de la Carcinomatosis Peritoneal en Cataluña (España). Indicaciones y resultados de la Técnica de Sugarbaker. Available at: http://www.gencat.cat/salut/depsan/units/aatrm/pdf/carcinoma peritoneo sugarbaker aatrmo9.pdf.
Sugarbaker PH. Peritonectomy procedures. Ann Surg. 1995;221(1):29–42.
Barrios P, Ramos I, Crusellas O, et al. Colorectal anastomosis during cytoreductive radical surgery in patients with peritoneal surface malignancies. Validation of a new technique (without stoma) to prevent anastomosis leakage in more than 1000 procedures. Clin Transl Oncol. 2021. https://doi.org/10.1007/s12094-020-02511-7.
Sugarbaker PH. Avoiding diverting ileostomy in patients requiring complete pelvic peritonectomy. Ann Surg Oncol. 2016;23(5):1481–5.
Baron E, Gushchin V, King MC, et al. Pelvic anastomosis without protective ileostomy is safe in patients treated with cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. Ann Surg Oncol. 2020;27(13):4931–40.
Karam C, Lord S, Gett R, Meagher AP. Circumferentially oversewn inverted stapled anastomosis. ANZ J Surg. 2018;88:E232–6.
Bakker IS, Grossmann I, Henneman D, et al. Risk factors for anastomotic leakage and leak-related mortality after colonic cancer surgery in a nationwide audit. BJS. 2014;101:424–32.
Castellví J, Perez Calvo J, Centeno A, et al. Mechanical reinforced terminolateral ileo-transverse anastomosis: an option after right hemicolectomy – a 452 patients study. Surg Technol Int. 2018;33:sti33/1024.
Montedori A, Cirocchi R, Farinella E, Sciannameo F, Abraha I. Covering ileo- or colostomy in anterior resection for rectal carcinoma. Cochrane Database Syst Rev. 2010;5:CD006878.
Breitenbuch P, Piso P, Schlitt H, et al. Safety of rectum anastomosis after cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. J Surg Oncol. 2018;118:1–6.
Brandl A, Raue W, Aigner F, et al. Safety of extraperitoneal rectal resection and ileo- or colorectal anastomosis without loop ileostomy in patients with peritoneal metastases treated with CRS and HIPEC. Colorectal Dis. 2018;20(3):61–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Pedro Barrios, Isabel Ramos, Oriol Crusellas, Domenico Sabia, Sergio Mompart, and Lana Bijelic declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Barrios, P., Ramos, I., Crusellas, O. et al. Safe Anastomoses without Ostomies in Cytoreductive Surgery with Heated Intraperitoneal Chemotherapy: Technical Considerations and Modifications. Ann Surg Oncol 28, 7784–7792 (2021). https://doi.org/10.1245/s10434-021-09842-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-021-09842-x