Abstract
Background
Meningoencephalocele is a skull defect that includes herniation of the cerebrospinal fluid and the brain tissue, and of meninges through it.
Case presentation
We report the anaesthetic management in a case of a 14-day-old neonate with a huge occipital meningoencephalocele referred for surgical excision and repair. The major anaesthetic challenges encountered in the management of occipital meningoencephalocele were to maintain adequate positioning of the neonate on the operation theatre table during induction and securing the airway thereafter.
Conclusions
The anaesthetic management of an occipital meningoencephalocele poses challenges for an anaesthesiologist in terms of positioning, difficulty encountered in securing airway particularly in the lateral position, blood loss and perioperative care; thus, attention should always be paid for proper positioning and perfect handling of airways along with replacement of blood loss intraoperatively.
Similar content being viewed by others
Background
The term encephalocele represents the herniation of cranial contents through a defect in the skull. If herniation of only cerebrospinal fluid and meninges exists, it is termed as meningocele. The herniation of the cerebrospinal fluid and meninges, along with the brain tissue, is termed as meningoencephalocele (Cote and Miller 2010). In Southeast Asia, the incidence of meningoencephalocele is one in 5000 live births (Creighton et al. 1974). The anaesthetic management of the airway may be challenging in neonates and young infants with large neck mass such as a huge occipital meningoencephalocele. Occipital meningoencephalocele poses challenges to an anaesthesiologist because of inadequate extension of the neck and inability to lay down the neonate in the supine position on the table, which makes the optimal position for intubation difficult.
Case presentation
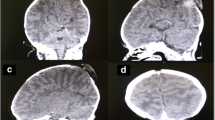
A 14-day-old male neonate weighing 1.8 kg presented with a huge cystic swelling on the posterior aspect of the neck and was scheduled for emergency surgical excision and repair. The size of the swelling was 20 × 18 cm. It was cystic, non-tender, and protruding from the occipital bone. The transillumination test was negative, and the skin over the swelling was red and oedematous, but there was no local rise of temperature. The swelling was almost twice the size of the neonate’s head. As the swelling was huge, and in view of impending rupture, it was decided by the neurosurgeon to operate upon the neonate. The neonate was not irritable, and his cry was normal. Preanaesthetic evaluation was thoroughly carried out. Radiography of the chest, spine and skull was carried out to locate the swelling and to determine its size; in addition, ultrasonography of the swelling was performed. A large cystic mass lesion was detected along with a defect in the occipital bone and herniation of the brain tissues in cyst. Multiple internal septations were also detected (Fig. 1). Cardiovascular, respiratory and neurological examinations were normal. There were no other associated congenital abnormalities. The results of laboratory evaluations were within normal limits. The neonate was laid laterally on the operation theatre table with a shoulder pack under the shoulder girdle. The swelling was also supported on a soft doughnut roll on the left side. Non-invasive blood pressure, ECG, pulse oximetry and skin temperature probes were attached for monitoring, and two intravenous lines of 24 G were secured. The neonate was premedicated with glycopyrrolate 0.01 mg and tramadol 4 mg given intravenously and then induced with sevoflurane 6% with 100% oxygen in the lateral posture. After confirming adequate mask ventilation, muscle relaxation was achieved with succinylcholine 2 mg/kg iv, and then, the neonate was intubated successfully with a 2.5-mm uncuffed endotracheal tube on first attempt using a stylet in the lateral position. The endotracheal tube position was confirmed, and after proper tube fixation, the baby was drapped and the surgeon decided to operate in the lateral position only. Anaesthesia was maintained with O2 to N2O (50:50), sevoflurane 1–2% and atracurium (0.5 mg/kg) iv bolus. Intraoperative blood loss was ∼ 100 ml, replaced with 100 ml of blood, and 40 ml of isolate-P was given intraoperatively. After completion of the surgery and return of spontaneous respiratory efforts, the neonate was given reversal glycopyrrolate 0.02 mg and neostigmine 0.1 mg iv and extubated after adequate return of muscle power. After extubation, the baby was oxygenated with 100% oxygen for 3 min. Cry was normal, and respiration was spontaneous and adequate; SpO2 was 97% on air, and the pulse rate was 120/min postoperatively. The baby was monitored by an anaesthesiologist for the next 24 h. Oxygen saturation was maintained on air with spontaneous breathing.
Discussion
Occipital meningoencephalocele represents hernial protrusion of meninges and the brain tissue in a sac through a bony defect in the occipital bone (Fig. 2). Approximately 75% of the encephaloceles are located in the occipital region. The commonly associated congenital defects are club foot, hydrocephalus, extrophy of bladder, prolapsed uterus, Klippel–Feil syndrome and congenital cardiac anomalies, and these children may also have a varying degree of sensory and motor deficit (Creighton et al. 1974). The major anaesthetic challenges associated in the management of occipital meningoencephalocele are adequate positioning of the neonate on the operation theatre table and securing the airway (Fig. 3) (Creighton et al. 1974; Stephen et al. 1986; Singh 1980). Improper positioning and inadequate extension of neck in the supine position can make endotracheal intubation of neonate difficult or impossible. There may be a likelihood of rupture of sac in the supine position. The airway management of these patients is very crucial for an anaesthesiologist at this stage. Most commonly, the lateral position for intubation is preferred, although anaesthesia may also be induced in the supine position depending upon the size of the sac. The sac is protected by elevating it using a doughnut-shaped support. Awake tracheal intubation in the lateral position can also be tried to avoid undue pressure on the sac (Singh et al. 2007; Cevik et al. 2012; Singh et al. 2012; Dey et al. 2007). The other alternative approach is to place the child in the supine position on a platform of rolled up blankets with an assistant temporarily supporting the head or placing the child’s head beyond the edge of the table with an assistant supporting it (Singh et al. 2012; Mowafi et al. 2000; Goel et al. 2010). We did mask ventilation in the lateral position after inducing with sevoflurane (Fig. 4), and after achieving adequate mask ventilation, succinylcholine was given and the neonate was intubated in the lateral position with sac supported on a doughnut roll on the left side. The intraoperative muscle relaxation was maintained with intravenous atracurium boluses. Usually, succinylcholine does not have a hyperkalemic response due to associated upper and lower motor neuron dysfunction in these neonates (Stephen et al. 1986). These neonates, however, may have an abnormal ventilatory response to hypoxia and hypercarbia due to limited reserve. Anaesthetic management of these children requires careful attention to positioning, airway management with careful securing of endotracheal tube to avoid accidental extubation, monitoring of the body temperature to prevent hypothermia, estimation of blood and fluid loss intraoperatively and adequate replacement according to loss (Fig. 5) (Singh et al. 2007; Cevik et al. 2012; Goel et al. 2010). The precautions for latex allergy should be taken in these children who are exposed first to anaesthetic procedure as it may lead to intraoperative bronchospasm and cardiovascular collapse.
Conclusions
So, in conclusion, the perioperative management of a case of occipital meningoencephalocele may pose challenges both for an anaesthesiologist and a neurosurgeon. In our case, a neonate with a huge occipital meningoencephalocele, the problems encountered were essentially because of its large size, positioning during induction and intubation and blood loss during resection of large amount of redundant skin. Thus, added attention should be paid to look for other congenital abnormalities along with proper positioning, perfect handling of airways and replacement of blood loss intraoperatively.
References
Cevik B, Orskiran A, Yelmaz M, Ekti Y (2012) Anaesthetic management of a new born with giant occipital meningoencephalocele. Case report. Int J Case Rep Images 3:10–12
Cote CJ, Miller RD (2010) Miller’s anaesthesia, 7th ed., chapter: 82. Pediatric anesthesia, Churchill Livingstone, p 2589
Creighton RE, Relton JES, Meridy HW (1974) Anaesthesia for occipital encephalocele. Can Anaesth Soc J 21:403–406
Dey N, Gomber KK, Khanna AK, Khandelwal P (2007) Anaesthetic management in neonates with occipital encephalocele: adjustment and modifications. Paediatr Anaesth 17:1119–1120
Goel V, Dogra N, Khandelwal M, Chaudhri RS (2010) Management of neonatal giant occipital encephalocele: anaesthetic challenge. Indian J Anaesth 54:477–478
Mowafi HA, Sheikh BY, Al-Ghamdi AA (2000) Positioning for anaesthetic induction of neonates with encephalocele. Internet J Anesthesiol 5(3):1–3
Singh CV (1980) Anaesthetic management of meningocele and meningomyelocele. J Indian Med Assoc 75:130–132
Singh K, Garasia M, Ambardekar M, Thota R, Dewoolkar LV, Mehta K (2007) Giant occipital meningoencephalocele: anaesthetic implications. Internet J Anesthesiol 13:2
Singh N, Rao PB, Ambesh SP, Gupta D (2012) Anaesthetic management of a giant encephalocele: size does matter. Paed Neurosurg 48:249–252
Stephen F, Dierdorf McNiece WL, Rao CC (1986) Failure of succinylcholine to alter plasma potassium in children with myelomeningocele. Anesthesiology 64:272–273
Consent form
The consent form is attached separately (signed by parent–mother) for the reproduction of images of child as a purpose of publication in a journal.
Availability of data and materials
The data is extracted from the medical records file of the patient through medical record department of our hospital and the materials are being used which were available in our set up with valid reasons.
Author information
Authors and Affiliations
Contributions
KJ and SKS have reviewed the available literature and participated in the data acquisition and analysis. SKS prepared the primary manuscript. SKS, KJ, NJ, and VP reviewed and edited final manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Although this is not a study, the permission for sending a case report was taken from the local institutional ethical committee after obtaining a valid consent from the patient’s mother.
Consent for publication
Written permission/consent for reproduction of images of the patient for the purpose of publication in an educational medical journal was obtained from the parents (mother) of the patient.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Jain, K., Sethi, S.K., Jain, N. et al. Anaesthetic management of a huge occipital meningoencephalocele in a 14 days old neonate. Ain-Shams J Anesthesiol 10, 13 (2018). https://doi.org/10.1186/s42077-018-0005-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42077-018-0005-7