Abstract
Background
Several cardiovascular pathologies cause heart failure. Heart failure with reduced ejection fraction (HFrEF) is deteriorated by neurohormonal activation, so neurohormonal antagonists are recommended in HFrEF patients. They improve morbidity, mortality, and quality of life and reduce hospital admissions. Heart failure treatment guidelines recommend achieving target doses of those drugs. However, many clinicians prescribe suboptimal doses for the fear of inducing hypotension. The aim of this systematic review and meta-analysis is to understand whether it is still beneficial to uptitrate the doses of those drugs even if the patient is at the risk of developing hypotension.
Methods
The primary outcome is symptomatic or asymptomatic hypotension in patients on neurohormonal antagonist drugs for HFrEF. Secondary outcomes are blood pressure reduction, New Yok Heart Association functional class deterioration, non-fatal cardiovascular events, cardiovascular mortality, all-cause mortality, heart failure hospitalizations, and adverse events. Randomized controlled trials involving adults with HFrEF will be included. Comprehensive literature search will be done in MEDLINE, Scopus, Web of Science, WHO Global Index Medicus, and the Cochrane Central Register of Controlled Trials. MEDLINE will be searched first using controlled vocabulary and free text terms and then adapted to other databases. Linear and nonlinear dose-response meta-analyses will be conducted. Publication bias and statistical heterogeneity will be tested by Egger’s regression and Cochran’s Q tests, respectively. Sensitivity, subgroup, and meta-regression analyses will be performed. Grading of Recommendations Assessment, Development and Evaluation approach will be used to judge the quality of evidence.
Discussion
This systematic review and meta-analysis will provide information about the risk of hypotension in patients on neurohormonal antagonist drugs for HFrEF. The results will be published in a peer-reviewed journal. The implications for further research will be discussed.
Systematic review registration
PROSPERO CRD42019140307
Similar content being viewed by others
Background
Heart failure (HF) is a progressive, complex clinical syndrome resulting from an abnormality of cardiac structure or function due to myocardial, pericardial, endocardial, valvular, or arrhythmic causes. It leads to reduced cardiac output and/or high filling pressures with exertion or at rest [1]. It is manifested by dyspnea and fatigue leading to exercise intolerance and fluid retention leading to pulmonary congestion and/or peripheral edema [2].
HF is a global health problem affecting an estimated 40 million people worldwide with an incidence of 1–4/1000 person-years [3, 4]. Even though the rates of first hospitalization for HF declined, HF is still one of the leading causes of hospitalization [5]. In 2012, the economic burden of HF was estimated to be around $108 billion per annum, with approximately 60% ($65 billion) being direct costs and the remaining 40% ($43 billion) being indirect costs [6]. HF affects health-related quality of life adversely and dramatically leading to depression, even in their partners [7].
HF is classified based on either the severity of symptoms (New York Heart Association (NYHA) functional classes I–IV) or the level of disease progression (stages A to D of American College of Cardiology Foundation/American Heart Association) [8, 9]. However, for practical purposes, left ventricular ejection fraction (LVEF) is used to distinguish HF into three groups: HF with preserved ejection fraction (HFpEF) with LVEF ≥ 50%, HF with midrange ejection fraction (HFmrEF) with LVEF 40–49%, and HF with reduced ejection fraction (HFrEF) with LVEF < 40% [10].
The goal of HFrEF management, including pharmacological and device therapies, is to reduce morbidity and mortality, improve quality of life, and reduce hospital admissions [11]. Optimal patient outcomes in HFrEF are achieved through guideline-directed medical therapy (GDMT) which addresses pathophysiologic responses in myocardial dysfunction [9]. The mainstay of pharmacological treatment for HFrEF is neurohormonal blockade with the aim to limit disease progression, improve symptoms and quality of life, and reduce mortality [12]. The neurohormonal antagonist drugs used for the treatment of patients with HFrEF include well-established drugs like angiotensin-converting enzyme inhibitors (ACEi) [angiotensin receptor blockers (ARB) if an ACEi is not tolerated], beta blockers (BB), mineralocorticoid receptor antagonists (MRA), and the more recent angiotensin receptor neprilysin inhibitor (ARNI) [13,14,15]. Other disease-modifying drugs that have shown benefit in HFrEF include hydralazine and isosorbide dinitrate combination, If-channel blocker, and dapagliflozin [16,17,18]. All the HF clinical practice guidelines recommend treating patients with HFrEF with recommended or maximum tolerated doses of these drugs [9, 19,20,21,22,23]. It has been shown that combination therapy with these drugs improves outcomes than monotherapy [24].
However, it has been found that many patients are not receiving the target doses of these drugs [25,26,27]. In addition to the beneficial long-term effects on cardiac function, these drugs also have blood pressure-lowering effect [28]. Hypotension is one of the reasons why clinicians do not uptitrate these drugs to their recommended doses [29]. It is a challenging problem in the management of HFrEF. Thus it is very important for clinicians to understand up to what minimum blood pressure levels they can safely uptitrate the guideline-directed medical therapy drugs to maximum doses without increasing morbidity and/or mortality due to hypotension in patients with HFrEF [30]. This systematic review and meta-analysis will attempt to delineate that sweet spot in the management of patients with HFrEF.
Objective
The objective of this systematic review and meta-analysis is to examine the relationship between neurohormonal antagonist drugs given for the treatment of HFrEF and hypotension. To this end, this systematic review and meta-analysis will specifically address the following three questions:
-
1.
What is the risk of hypotension (blood pressure lower than 90/60 mmHg or mean arterial pressure less than 65 mmHg or presence of specific symptoms such as dizziness, near syncope, and fatigue associated with drop in blood pressure from typical level for a particular patient) in patients on different neurohormonal antagonist drugs given for the treatment of HFrEF?
-
2.
What are the linear and nonlinear dose-response relationships between the neurohormonal antagonist drugs and hypotension?
-
3.
What are the adverse outcomes of treatment with neurohormonal antagonist drugs in patients with HFrEF?
Methods/design
This protocol has been developed as per the Preferred Reporting Items for Systematic review and Meta-Analysis Protocols (PRISMA-P) 2015 guidelines (Additional file 1) [31].
Eligibility criteria
Study designs
Only randomized controlled trials will be included. Non-randomized controlled trials, controlled before and after studies, prospective and retrospective cohort studies, case-control studies, nested case-control studies, cross-sectional studies, case series, and case reports will be excluded. Non-research articles such as commentaries, letters, and editorials will also be excluded.
Participants
Only those studies examining adult (18 years and older) human population diagnosed with HFrEF will be included. The definition of HFrEF is left ventricular ejection fraction < 40%, as per the latest clinical practice guidelines [9, 19, 21,22,23, 32].
We will include only those studies with participants who were ambulatory with symptomatic heart failure and (1) were randomised to neurohormonal antagonist drugs or placebo (or other inactive substance) or (2) randomised to different doses of same neurohormonal antagonist drugs in the intervention and control arms or (3) different classes of neurohormonal antagonist drugs in the intervention and control arms.
We will exclude those studies in which the comparator was not clearly defined and which were done on people with acute heart failure, hospitalized acute heart failure patients, people with reduced ejection fraction during myocardial infarction, and people with asymptomatic reduced ejection fraction.
Interventions
The interventions of interest are neurohormonal antagonist drugs indicated for the pharmacological treatment of HFrEF as recommended by the clinical practice guidelines [9, 19, 21,22,23, 32]. These include angiotensin-converting enzyme inhibitors (captopril, enalapril, fosinopril, lisinopril, perindopril, quinapril, ramipril, trandolapril), angiotensin receptor blockers (candesartan, losartan, valsartan), mineralocorticoid receptor antagonists (eplerenone, spironolactone), beta blockers (bisoprolol, carvedilol, carvedilol continuous release, metoprolol succinate continuous/extended release, nebivolol), and angiotensin receptor neprilysin inhibitor (sacubitril/valsartan).
Comparators
The controls will be the group of people who were given a placebo (or other inactive substance) or another dose of same neurohormonal antagonist drug as in the intervention arm or another class of neurohormonal antagonist drug different from the intervention arm.
Outcomes
The primary outcome is symptomatic or asymptomatic hypotension. Asymptomatic hypotension is defined as blood pressure lower than 90/60 mmHg or mean arterial pressure less than 65 mmHg. Symptomatic hypotension is defined as presence of specific symptoms such as dizziness, near syncope, and fatigue associated with drop in blood pressure from typical level for a particular patient.
The secondary outcomes are blood pressure reduction, NYHA functional class deterioration, non-fatal cardiovascular events, cardiovascular mortality, all-cause mortality, heart failure hospitalizations, and adverse events.
For binary outcomes, we will take the number of participants who experienced or not experienced the outcomes in both the intervention and control groups. For continuous outcomes, we will take the number of participants in each of the two arms and the mean and standard deviation of the outcomes. For time-to-event data, we will use the observed and expected values and their variances. We will then calculate the individual study estimates. However, we will extract the estimates of effect directly from individual studies in the case of cluster randomized controlled trials, crossover trials, analyses were adjusted for variables used in stratified randomization or minimization, analysis of covariance was used to adjust for baseline measures of outcome and when time-to-event data is not summarized for each intervention group.
Timing
Studies selected for inclusion will not be based on the length of follow-up for outcomes.
Setting
There will be no restrictions by type of setting.
Language
Only articles reported in English language will be included. If it is feasible to translate articles published in languages other than English using an online or computer-installed machine translation software tool, then other language articles will also be included.
Information sources
MEDLINE (via both Ovid and PubMed), Scopus, Web of Science, WHO Global Index Medicus, and the Cochrane Central Register of Controlled Trials will be searched.
The electronic bibliographic database search will be supplemented by searching for study records through the ISRCTN registry (http://www.isrctn.com/), WHO International Clinical Trials Registry Platform (http://apps.who.int/trialsearch/Default.aspx), UK Clinical Trials Gateway (https://www.ukctg.nihr.ac.uk/), ClinicalTrials.gov (https://clinicaltrials.gov/ct2/home), EU Clinical Trials Register (https://www.clinicaltrialsregister.eu/ctr-search/search), OpenTrials (https://explorer.opentrials.net/), and metaRegister of Controlled Trials (http://www.isrctn.com/page/mrct).
Grey literature will also be searched through OpenGrey (http://opengrey.org/), MedNar (https://mednar.com/mednar/desktop/en/search.html), Google Advanced Search, and Google Scholar.
Search strategy
The literature search strategies will be developed using a combination of controlled vocabularies (“exploded” where appropriate) with a wide range of free text terms related to HF and the different classes of neurohormonal antagonist drugs used for the treatment of HFrEF. The specific search strategies will be created by a review team member. The MEDLINE strategy will be developed first by this team member with input from the review team (Additional file 2). After the MEDLINE strategy is finalized, it will be adapted to the syntax and controlled vocabularies (subject headings) of the other databases.
No date limits will be imposed on the search, but the search will be limited to clinical trials, controlled clinical trials, meta-analyses, pragmatic clinical trials, and randomized controlled trials in human subjects only.
To ensure literature saturation, the reference lists of included studies will be scanned for any relevant studies. Forward citation searching will also be used to identify newly published studies.
The literature search will be updated toward the end of the review, in order to capture any additional studies published since the original literature search.
Selection process
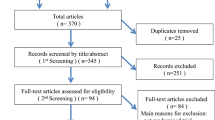
Screening questionnaire for level 1 (title and abstract) and data extraction form for level 2 (full-text articles) will be developed based on the inclusion criteria and will be tested. The two reviewers will independently screen all the titles and abstracts yielded by the literature search against the inclusion criteria. Full-text articles will be obtained for all the titles and abstracts that appear to meet the inclusion criteria and also where there is any uncertainty about eligibility. The two reviewers will then independently screen the full-text articles and decide whether those full-text articles meet the inclusion criteria. Additional information will be sought from study authors, where necessary, to resolve questions about eligibility. Disagreements between the two reviewers will be resolved through discussion between them and, if the disagreements are not resolved through discussion, then through arbitration by a third member of the review team. The reasons for excluding the studies will be recorded. Neither of the two reviewers will be blind to the journal titles or to the study authors or institutions.
Data management
The abstracts from the literature search, and then the selected full-text articles, will be uploaded to Rayyan web application (https://rayyan.qcri.org/welcome) that facilitates collaboration among the two reviewers during the study selection process [33].
Data collection
Using the standardized data extraction form, the two reviewers will extract data independently from each study. To ensure consistency across the two reviewers, calibration exercises of data extraction form will be conducted before starting the review. Data extracted will include demographic information, methodology, participant and intervention details, and all patient-important outcomes.
Data items
The following data will be extracted: study information (title, author, publication year, journal name, author contact details, study funding source, possible conflicts of interest), study characteristics (name of the study, study design, country, setting, inclusion/exclusion criteria, methods of recruitment, duration of follow-up), participant characteristics (sample size, age, gender, race/ethnicity, co-morbidities, other relevant sociodemographics), interventions/comparators and outcomes, statistical methods used for the analysis, risk estimates and 95% confidence intervals, and covariates that were matched or adjusted for in the analysis.
Risk of bias
To facilitate the assessment of possible risk of bias in each included study, the revised Cochrane Risk-of-Bias tool for randomized trials (RoB 2) will be used to collect information about: randomization process, deviations from intended interventions, missing outcome data, measurement of the outcome, and selection of the reported result [34]. For each domain in the RoB 2 tool, the procedures undertaken for each study will be described. A judgment as to the possible risk of bias in each of the five domains will be made from the extracted information, rated as “low risk of bias,” “some concerns,” and “high risk of bias.”
If sufficient details are not reported in a study, the risk of bias will be judged as “unclear” and then the original study investigators will be contacted for more information.
These judgements will be made independently by the two reviewers based on the criteria for judging the risk of bias. Disagreements between the two reviewers will be resolved first by discussion between them and, if not resolved, then by consulting a third member of the team for arbitration.
Graphic representations of potential bias will be computed within and across studies using the latest major version of Review Manager, which is RevMan 5.3 [35]. Each item in the risk of bias assessment will be considered independently without an attempt to collate and assign an overall score.
Data synthesis
All statistical analyses will be conducted with “dosresmeta” and “metafor” packages in the “R” software (The R Foundation for Statistical Computing, Vienna, Austria).
The odds ratios and hazard ratios referring to new-onset incident cases of hypotension will be deemed as equivalent to risk ratios (RRs). When neurohormonal antagonist drug dose is illustrated by ranges of intake, the midpoint of the range will be used. When the highest category is open-ended, it will be assumed that the width of the upper category is the same as the adjacent category. When the lowest category is open-ended, the lower boundary will be set to zero.
Two meta-analytical approaches will be undertaken.
Generalized least squares (GLS) will be used to calculate study-specific coefficients across categories of neurohormonal antagonist drug intake accounting for the correlation within each set of RRs. Nonlinear dose-response analysis will be modeled using restricted cubic splines with 3 knots at fixed percentiles (25%, 50%, and 75%) of the distribution. Coefficients estimated within each study will be combined by performing random effects meta-analysis. DerSimonian and Laird’s method will be used for linear dose-response meta-analysis. In nonlinear dose-response meta-analysis, the multivariate extension of the method of moments will be used to estimate the RRs. Whether the two regression coefficients are simultaneously equal to zero will be tested, and a p value for nonlinearity will be calculated by testing whether the coefficient of the second spline is equal to zero.
A summary statistic for each study will be calculated, to describe the observed intervention effect (risk ratio if the data are dichotomous and mean difference if the data are continuous). Then a summary (pooled) intervention effect estimate will be calculated as a weighted average of the intervention effects estimated in the individual studies. Both adjusted and unadjusted effect estimates will be included but will be synthesized separately.
A sensitivity analysis will be conducted by excluding one study at a time (leave-one-out), based on study design and quality of evidence, to determine the stability and robustness of the results.
Subgroup analyses by sex, type of neurohormonal antagonist drug, etc. will be performed to test for potential confounders. To further investigate whether other unmeasured potential confounders should be included in the interpretation of the results, the distribution of potential confounders across categories of neurohormonal antagonist drug dose will be investigated. For this purpose, a separate two-stage bivariate meta-analysis for each confounder variable will be performed to determine its association with neurohormonal antagonist drug intake. First, linear regression coefficients (slope and intercept) between neurohormonal antagonist drug intake and the potential confounders will be estimated. Second, GLS will be used to synthesize these intercepts and slope coefficients, accounting for the corresponding variance-covariance matrices.
To determine the significance of the proposed confounders on the association of neurohormonal antagonist drug dose and risk of hypotension, a meta-regression analysis will be conducted. Specifically, the joint slope coefficient of the association will be used as the moderator in the meta-regression analysis.
Publication bias will be assessed using Egger’s regression test, and statistical heterogeneity will be tested by using Cochran’s Q test (statistical significance is defined as a p value less than 0.10) and quantified through the multivariate generalization of the I2 statistic (no, low, medium, and high heterogeneity are defined by I2 values < 25%, 25–50%, 50–75%, and 75%, respectively).
The quality of evidence for all outcomes will be judged using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) approach [36]. The quality of evidence will be assessed across the domains of risk of bias, consistency, directness, precision, and publication bias. Additional domains may be considered where appropriate. Quality will be adjudicated as high (further research is very unlikely to change our confidence in the estimate of effect), moderate (further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate), low (further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate), or very low (very uncertain about the estimate of effect).
Discussion
HFrEF is the final pathway of several different cardiovascular diseases. It poses a major challenge to clinicians in terms of treatment, and a burden to patients and their families in terms of morbidity, mortality, and costs. Even though all the HF clinical guidelines recommend treating patients with HFrEF with target doses of neurohormonal antagonist drugs, it is rarely achieved in routine clinical practice [27, 37]. The fear of inducing hypotension in patients with HFrEF is a major reason for clinicians not to uptitrate those drugs and for patients being reluctant to take increased doses of those drugs.
As per one of the largest surveys across 136 cardiology centers in 12 European countries, the target doses of neurohormonal antagonist drugs are achieved only in about one-third to one-fourth of patients with HF, with the achieved target doses being as low as 16% in case of some drugs [38]. The 1-year follow-up of a prospective, observational registry from 211 cardiology centers in 21 European and/or Mediterranean countries has shown that with the increasing use of neurohormonal antagonists the survival of patients with HF has improved [39]. However, it is interesting to note that the mean baseline systolic blood pressure (SBP) (± standard deviation) of patients with HFrEF in this registry was 121.6 ± 20.0 mmHg with only 34.4% of them with an SBP ≤ 110 mmHg and only 3.9% with peripheral hypoperfusion [40].
This systematic review and meta-analysis will address this major clinical issue in the management of patients with HFrEF by trying to identify the maximum doses of neurohormonal antagonist drugs at which patients develop hypotension. The results of this study will also help us understand the consequences of hypotension in patients with HFrEF. We are not aware of any published or ongoing systematic review and/or meta-analysis addressing the same clinical problem. We expect that the results will help clinicians to uptitrate the neurohormonal antagonist drugs in patients with HFrEF safely unto the maximum doses without inducing hypotension in them. The patients with HFrEF will also be able to make informed decisions about their treatment.
There are several strengths and limitations to our planned methodology. This systematic review and meta-analysis is designed according to the PRISMA guidelines [41, 42]. We want to include only controlled trials, so we may miss some useful information from observation studies. We intentionally developed a very comprehensive search strategy without any limits so as not miss any published literature. However, we will not be able to search all the bibliographic databases because of lack of access to some of them. As we want to include various neurohormonal antagonist drugs used for HFrEF, we expect some potential heterogeneity but we plan to use random effects model approach and do subgroup analyses.
Availability of data and materials
Not applicable.
Abbreviations
- ACEi:
-
Angiotensin-converting enzyme inhibitor
- ARB:
-
Angiotensin receptor blocker
- ARNI:
-
Angiotensin receptor neprilysin inhibitor
- BB:
-
Beta blocker
- GDMT:
-
Guideline-directed medical therapy
- GLS:
-
Generalized least squares
- GRADE:
-
Grading of Recommendations Assessment, Development, and Evaluation
- HF:
-
Heart failure
- HFmrEF:
-
Heart failure with midrange ejection fraction
- HFpEF:
-
Heart failure with preserved ejection fraction
- HFrEF:
-
Heart failure with reduced ejection fraction
- ISRCTN:
-
International Standard Randomised Controlled Trials Number
- LVEF:
-
Left ventricular ejection fraction
- MRA:
-
Mineralocorticoid receptor antagonist
- PRISMA-P:
-
Preferred Reporting Items for Systematic review and Meta-Analysis Protocols
- PROSPERO:
-
International prospective register of systematic reviews
- RoB 2:
-
Revised Cochrane Risk-of-Bias tool for randomized trials
- RR:
-
Risk ratio
- SBP:
-
Systolic blood pressure
References
Hassenfuss GMJ. Pathophysiology of heart failure. In: ZD MJL, Libby P, Bonow RO, Braunwald E, editors. Braunwald’s heart disease: a textbook of cardiovascular medicine. Philadelphia: Saunders Elsevier; 2015.
Januzzi JLMD. Clinical assessment of heart failure. In: Mann JLZD, Libby P, Bonow RO, Braunwald E, editors. Braunwald’s heart disease: a textbook of cardiovascular medicine. Philadelphia: Saunders Elsevier; 2015.
Disease GBD, Injury I, Prevalence C. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1545–602.
Orso F, Fabbri G, Maggioni AP. Epidemiology of heart failure. Handb Exp Pharmacol. 2017;243:15–33.
Jhund PS, Macintyre K, Simpson CR, Lewsey JD, Stewart S, Redpath A, et al. Long-term trends in first hospitalization for heart failure and subsequent survival between 1986 and 2003: a population study of 5.1 million people. Circulation. 2009;119(4):515–23.
Cook C, Cole G, Asaria P, Jabbour R, Francis DP. The annual global economic burden of heart failure. Int J Cardiol. 2014;171(3):368–76.
Jaarsma T, Johansson P, Agren S, Stromberg A. Quality of life and symptoms of depression in advanced heart failure patients and their partners. Curr Opin Support Palliat Care. 2010;4(4):233–7.
Chacko KA. AHA medical/scientific statement: 1994 revisions to classification of functional capacity and objective assessment of patients with diseases of the heart. Circulation. 1995;92(7):2003–5.
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;62(16):e147–239.
Nussbaumerova B, Rosolova H. Diagnosis of heart failure: the new classification of heart failure. Vnitr Lek. 2018;64(9):847–51.
Gedela M, Khan M, Jonsson O. Heart failure. S D Med. 2015;68(9):403–5 7-9.
Heart Failure Society of A, Lindenfeld J, Albert NM, Boehmer JP, Collins SP, Ezekowitz JA, et al. HFSA 2010 Comprehensive Heart Failure Practice Guideline. J Card Fail. 2010;16(6):e1–194.
Biglane JB, Becnel MF, Ventura HO, Krim SR. Pharmacologic therapy for heart failure with reduced ejection fraction: closing the gap between clinical guidelines and practice. Prog Cardiovasc Dis. 2017;60(2):187–97.
Paul S, Page RL 2nd. Foundations of pharmacotherapy for heart failure with reduced ejection fraction: evidence meets practice, Part I. J Cardiovasc Nurs. 2016;31(2):101–13.
McIlvennan CK, Page RL 2nd. Foundations of pharmacotherapy for heart failure with reduced ejection fraction: evidence meets practice, Part II. J Cardiovasc Nurs. 2016;31(6):545–54.
Nyolczas N, Dekany M, Muk B, Szabo B. Combination of hydralazine and isosorbide-dinitrate in the treatment of patients with heart failure with reduced ejection fraction. Adv Exp Med Biol. 2018;1067:31–45.
Swedberg K, Komajda M, Bohm M, Borer JS, Ford I, Dubost-Brama A, et al. Ivabradine and outcomes in chronic heart failure (SHIFT): a randomised placebo-controlled study. Lancet. 2010;376(9744):875–85.
McMurray JJV, Solomon SD, Inzucchi SE, Kober L, Kosiborod MN, Martinez FA, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med. 2019.
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 2016;18(8):891–975.
Group NCHFGW, Atherton JJ, Sindone A, De Pasquale CG, Driscoll A, MacDonald PS, et al. National Heart Foundation of Australia and Cardiac Society of Australia and New Zealand: guidelines for the prevention, detection, and management of heart failure in Australia 2018. Heart Lung Circ. 2018;27(10):1123–208.
Ezekowitz JA, O'Meara E, McDonald MA, Abrams H, Chan M, Ducharme A, et al. 2017 comprehensive update of the Canadian Cardiovascular Society Guidelines for the management of heart failure. Can J Cardiol. 2017;33(11):1342–433.
Chronic heart failure in adults: diagnosis and management 2018 13-08-2019: 38 p.. Available from: https://www.nice.org.uk/guidance/ng106.
Management of chronic heart failure: a national clinical guideline 2016 13-08-2019:[82 p.]. Available from: http://www.sign.ac.uk.
Levy WC, Mozaffarian D, Linker DT, Sutradhar SC, Anker SD, Cropp AB, et al. The Seattle Heart Failure Model: prediction of survival in heart failure. Circulation. 2006;113(11):1424–33.
Komajda M, Anker SD, Cowie MR, Filippatos GS, Mengelle B, Ponikowski P, et al. Physicians’ adherence to guideline-recommended medications in heart failure with reduced ejection fraction: data from the QUALIFY global survey. Eur J Heart Fail. 2016;18(5):514–22.
Swennen MH, Rutten FH, Kalkman CJ, van der Graaf Y, Sachs AP, van der Heijden GJ. Do general practitioners follow treatment recommendations from guidelines in their decisions on heart failure management? A cross-sectional study. BMJ Open. 2013;3(9):e002982.
Ouwerkerk W, Voors AA, Anker SD, Cleland JG, Dickstein K, Filippatos G, et al. Determinants and clinical outcome of uptitration of ACE-inhibitors and beta-blockers in patients with heart failure: a prospective European study. Eur Heart J. 2017;38(24):1883–90.
Rifkin DE, Kiernan M, Sarnak MJ. Hitting the mark: blood pressure targets and agents in those with prevalent cardiovascular disease and heart failure. Adv Chronic Kidney Dis. 2015;22(2):140–4.
Parwani P, Ryan J. Heart failure patients with low blood pressure: how should we manage neurohormonal blocking drugs? Circ Heart Fail. 2012;5(6):819.
Packer M. Heart failure’s dark secret: does anyone really care about optimal medical therapy? Circulation. 2016;134(9):629–31.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1.
AlHabeeb W, Al-Ayoubi F, AlGhalayini K, Al Ghofaili F, Al Hebaishi Y, Al-Jazairi A, et al. Saudi Heart Association (SHA) guidelines for the management of heart failure. J Saudi Heart Assoc. 2019;31(4):204–53.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210.
Sterne JACSJ, Page MJ, Elbers RG, Blencowe NS, Boutron I, Cates CJ, Cheng H-Y, Corbett MS, Eldridge SM, Hernán MA, Hopewell S, Hróbjartsson A, Junqueira DR, Jüni P, Kirkham JJ, Lasserson T, Li T, McAleenan A, Reeves BC, Shepperd S, Shrier I, Stewart LA, Tilling K, White IR, Whiting PF, Higgins JPT. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. in press.
Review Manager (RevMan). 5.3 ed. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration; 2014.
Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64(4):383–94.
Greene SJ, Butler J, Albert NM, DeVore AD, Sharma PP, Duffy CI, et al. Medical therapy for heart failure with reduced ejection fraction: the CHAMP-HF registry. J Am Coll Cardiol. 2018;72(4):351–66.
Maggioni AP, Dahlstrom U, Filippatos G, Chioncel O, Leiro MC, Drozdz J, et al. EURObservational Research Programme: the Heart Failure Pilot Survey (ESC-HF Pilot). Eur J Heart Fail. 2010;12(10):1076–84.
Crespo-Leiro MG, Anker SD, Maggioni AP, Coats AJ, Filippatos G, Ruschitzka F, et al. European Society of Cardiology Heart Failure Long-Term Registry (ESC-HF-LT): 1-year follow-up outcomes and differences across regions. Eur J Heart Fail. 2016;18(6):613–25.
Chioncel O, Lainscak M, Seferovic PM, Anker SD, Crespo-Leiro MG, Harjola VP, et al. Epidemiology and one-year outcomes in patients with chronic heart failure and preserved, mid-range and reduced ejection fraction: an analysis of the ESC Heart Failure Long-Term Registry. Eur J Heart Fail. 2017;19(12):1574–85.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700.
Acknowledgements
Not applicable.
Funding
This systematic review and meta-analysis is not funded and also is not in receipt of any nonfinancial sources of support. RKG is currently supported by a Marie Sklodowska-Curie Actions Early Career Research Fellowship (EU H2020 Grant agreement ID 754432). SS is currently supported by a Marie Sklodowska-Curie Actions Early Career Research Fellowship (EU H2020 Grant agreement ID 754432).
Author information
Authors and Affiliations
Contributions
The study protocol was conceived by RKG and KAK, with inputs from PMS, JJ, SS, and AA. RKG registered the protocol with PROSPERO. RKG and KAK controlled the decision to publish the protocol. RKG wrote the first draft of the manuscript. All the authors provided inputs to the manuscript. All the authors read and approved the final manuscript. RKG accepts full responsibility for the final manuscript. RKG and KAK are the guarantors of the systematic review and meta-analysis.
Authors’ information
RKG is a PhD (doctoral) student and a research assistant. PMS is a research assistant. JJ is a lecturer. SS is a PhD (doctoral) student and a research assistant. AA is a medical student. KAK is a cardiologist and a professor.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
RKG is a shareholder in three Indian multinational pharmaceutical companies (Ajanta Pharma Limited, Divi’s Laboratories Limited, and NATCO Pharma Limited).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1.
PRISMA-P checklist.
Additional file 2.
MEDLINE (PubMed) search strategy.
Additional file 3.
Draft data extraction form.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Guggilla, R.K., Sowa, P.M., Jamiolkowski, J. et al. Effects of neurohormonal antagonists on blood pressure in patients with heart failure with reduced ejection fraction (HFrEF): a systematic review protocol. Syst Rev 9, 194 (2020). https://doi.org/10.1186/s13643-020-01452-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13643-020-01452-0