Abstract
The mechanisms involved in the induction of allergic sensitization by pollen are not fully understood. Within the last few decades, findings from epidemiological and experimental studies support the notion that allergic sensitization is not only dependent on the genetics of the host and environmental factors, but also on intrinsic features of the allergenic source itself. In this review, we summarize the current concepts and newest advances in research focusing on the initial mechanisms inducing pollen sensitization. Pollen allergens are embedded in a complex and heterogeneous matrix composed of a myriad of bioactive molecules that are co-delivered during the allergic sensitization. Surprisingly, several purified allergens were shown to lack inherent sensitizing potential. Thus, growing evidence supports an essential role of pollen-derived components co-delivered with the allergens in the initiation of allergic sensitization. The pollen matrix, which is composed by intrinsic molecules (e.g. proteins, metabolites, lipids, carbohydrates) and extrinsic compounds (e.g. viruses, particles from air pollutants, pollen-linked microbiome), provide a specific context for the allergen and has been proposed as a determinant of Th2 polarization. In addition, the involvement of various pattern recognition receptors (PRRs), secreted alarmins, innate immune cells, and the dependency of DCs in driving pollen-induced Th2 inflammatory processes suggest that allergic sensitization to pollen most likely results from particular combinations of pollen-specific signals rather than from a common determinant of allergenicity. The exact identification and characterization of such pollen-derived Th2-polarizing molecules should provide mechanistic insights into Th2 polarization and pave the way for novel preventive and therapeutic strategies against pollen allergies.
Similar content being viewed by others
Background
Worldwide, the sensitisation rate to pollen allergens is around 40% and over 400 million people suffer from allergic rhinitis symptoms caused by pollinosis [1,2,3,4]. Wind plays a key role in the induction of pollen sensitization enabling the direct contact of pollen with the human immune system at sites such as the upper respiratory tract, the ocular and oral mucosal surfaces, where the humid milieu facilitates the release of soluble allergens and other co-delivered bioactive compounds from the pollen matrix. Among wind-pollinated plants, the four plant families Oleaceae, Poaceae, Asteraceae and Betulaceae represent the main sources of allergenic pollen in Europe [5, 6]. Up to now, 987 different allergens have been officially described, of which 195 are registered as plant-derived airborne allergens (https://www.allergen.org, 1st April 2020). Besides triggering seasonal rhinoconjunctivitis symptoms, a clinical condition also known as “hay fever”, pollen can also cause asthma, skin inflammation, and even food allergies due to structural homology of food antigens to some pollen allergens [7,8,9,10,11,12,13,14]. The rising numbers of pollen-affected individuals, the variety of symptoms and the impact on the patients´ quality of life are making pollen allergies a vast and serious socio-economic burden of Western civilization [15]. In this respect, it is of utmost importance to understand the underlying mechanisms of sensitization to pollen allergens in order to develop innovative therapeutic strategies to efficiently tackle pollinosis. The scope of this review is to summarize the current concepts and newest advances in research focusing on pollen sensitization.
Current concepts of allergic sensitization
Exposure to environmental proteins does not normally trigger an immune response due to their non-pathogenic nature, yet allergic sensitization to pollen molecules is a global health problem. Allergies are thus considered type 1 (IgE-mediated) hypersensitivity reactions to innocuous environmental antigens that is characterized by an imbalanced immune response [16, 17].
IgE-mediated allergic immune response
In type 1 hypersensitivity reactions, antigen-presenting cells (APCs), mainly dendritic cells (DCs), control the differentiation of naïve T helper cells into effector T cells, such as Th1 or Th2 cells, depending on the nature and source of the antigen [17, 18]. Upon initial allergen encounter, Th2 polarization, a hallmark of allergic sensitization, is triggered by interleukin 4 (IL-4) signalling and characterized by the secretion of Th2-associated cytokines (IL-4, IL-5 and IL-13) [19]. While IL-4 has a key role in the initiation of sensitization, IL-5 and IL-13 are relevant in later stages of the sensitization process as well as the effector phase. IL-5 is mainly involved in airway eosinophilia and hyperresponsiveness, whereas IL-13 mainly contributes to the maintenance of allergic disease by recruiting and activating various effector cells to the site of allergic inflammation [20, 21]. Upon activation by Th2 cytokines, B cells undergo class-switching to produce antigen-specific immunoglobulin E (IgE) antibodies, which prime mast cells and basophils by binding to its high affinity receptor FcεRI. Allergic sensitization is defined by the presence of allergen-specific IgE. Upon re-exposure, allergen-IgE cross-linking causes cell degranulation and release of inflammatory mediators within minutes, leading to the recruitment of other immune cells, and, consequently, triggering the onset of allergic symptoms [22]. Besides its role in allergic diseases, type 2 immunity is also associated with homeostasis and protective immune responses such as wound healing, clearance of parasitic infections and venom resistance [23,24,25,26,27,28,29,30,31,32,33,34,35].
Factors contributing to allergic sensitization
Allergy is generally considered a multifactorial disease, but the individual factors and their respective contribution to sensitization are not yet fully defined. The prevalence of allergic diseases has been associated with a westernized lifestyle—the so-called hygiene hypothesis—but also with environmental and genetic factors. Linkage analysis studies have already revealed allergy-relevant loci, while genome-wide association studies hold the promise for new and reproducible genetic associations with allergic diseases [36]. However, given the multifactorial nature and heterogeneous manifestation of allergic phenotypes, the integration of genetic predisposition data into a coherent picture remains challenging.
The hygiene hypothesis by Strachan, which has been redefined and updated over the years with the continuous emergence of new data, presently postulates that several variables associated with a westernized lifestyle, such as diminished exposure to microbes, environmental changes, medication, diet, parasitic infections and others, influence the susceptibility of the immune system to allergic diseases [37,38,39,40]. For instance, in contrast to life in urbanized cities and poor nutrition, growing up near farms and fibre-rich nutrition were classed as beneficial factors leading to immune tolerance [41]. While it is well known that environmental stimuli are directly linked to epigenetic modifications, the field has been understudied in regard to allergic diseases [42]. In summary, experimental and epidemiological findings within the last few decades support the view that the allergic sensitization process is not solely dependent on the genetics of the host and environmental factors, but also on intrinsic features of the allergenic source itself. In addition, epigenetic mechanisms might contribute to the initiation of sensitization and maintenance of allergic diseases [43].
Initiation of sensitization by allergenic pollen
The activation of the innate immune system
Besides the known adaptive immunity components involved in allergic sensitization, a superordinate role can be allocated to the epithelium itself since it represents the primary contact site of the human body encountering the pollen. Whether sensitization to pollen-derived allergens occurs at the oral mucosa, the olfactory or corneal epithelium is still a matter of debate; the skin has also been proposed as a sensitization route for allergenic pollen [44,45,46]. Upon encounter, the pollen hydrates and releases a hydrophilic cocktail consisting of allergenic and non-allergenic proteins and various other bioactive molecules, including lipid mediators, inducing an inflammatory milieu favouring Th2 polarization [47,48,49,50,51].
Epithelial cells and APCs, are endowed with a series of specialized pattern recognition receptors (PRRs), such as Toll-like receptors (TLRs) and protease activated receptors (PARs), which are required to provide first defence mechanisms in order to keep pathogens under surveillance. The vast majority of allergenic tree, grass and weed pollen, including white birch (Betula verrucosa), rye grass (Lolium perenne) and short ragweed (Ambrosia artemisiifolia), contain proteolytic enzymes able to disrupt epithelial cells [52,53,54,55]. Most identified proteins thereof belong to the family of cysteine, serine and aspartic proteases, and are responsible for the disruption of tight junctions enabling the transportation of allergens across the epithelium. The occurring damage of epithelial cells was observed to be irreversible, but can be blocked by protease-specific inhibitors [56]. However, the question emerges as to what extent these proteases originate from pollen itself (intrinsic origin) or are derived from pollen-inhabiting microorganisms (extrinsic origin) [52]. Purified pollen allergens that are per se non-proteases, such as Ole e 1 and Bet v 1, were also observed to interact with the epithelial barrier [46, 57, 58]. Interestingly, interaction of Japanese cedar (Cryptomeria japonica) Cry j 1 and epithelial cells led to the activation of PAR2 and stimulation with Japanese hop (Humulus japonicus) increased the PAR2 expression levels on human airway epithelial cells [59, 60]. Direct effects observed for pollen-derived proteases on PAR activation are, however, still lacking but seem to be dependent on the protease class and its abundance within the respective pollen source [55].
Upon stimulation with pollen extracts, epithelial cells release a number of pro-inflammatory cytokines, including IL-1, IL-6, IL-8 and TNFα [55]. Additionally, the secretion of pro-allergic alarmins (e.g. thymic stromal lymphopoietin, (TSLP); IL-33; IL-25) favours a Th2-biased immune response and promotes allergic sensitization.
The levels of TSLP are increased in the nasal secretion of patients suffering from allergic rhinitis, but there is no evidence directly correlating TSLP expression and pollen allergen-specific IgE levels, suggesting a more general role of TSLP in the initiation and maintenance of a type 2 inflammatory response [61,62,63]. In fact, TSLP has been considered a key cytokine driving Th2 polarization through (i) the activation of DCs and macrophages to express OX40 ligand (OX40L), which in turn binds OX40 on naïve CD4+ T cells, and (ii) direct induction of IL4+ and IL-13+ CD4+ T cells [64,65,66]. The pollen-induced secretion of TSLP and the associated type 2 inflammation were observed to be dependent on TLR4 and myeloid differentiation primary response 88 (MyD88), and probably linked to oxidative stress [60, 66,67,68]. In this respect, stimulation of epithelial cells with pollen extracts from short ragweed, birch, timothy grass and mountain cedar caused elevation in the levels of reactive oxygen species (ROS) [60, 69,70,71]. Thus, the contribution of oxidative stress to the allergic sensitization is likely mediated by ROS, which up-regulates the expression of PAR2 in epithelial cells, as well as the secretion of TSLP and IL-8 [60, 70]. The latter is a neutrophil chemotactic factor responsible for the recruitment of neutrophils in allergic airway inflammation. Although pollen were observed to induce both TLR4-dependent and independent ROS production, Hosoki et al. showed that short ragweed pollen only induced neutrophil recruitment in a TLR4-dependent manner, which in turn facilitated allergic sensitization [67, 69, 71].
As described for TSLP, a TLR4-/MyD88-dependency has also been observed for pollen-induced IL-33-mediated Th2 responses [67, 72]. IL-33 binds and up-regulates its receptor, ST2, expressed on DCs and CD4+ T cells, thus triggering Th2 polarization and the expression of the associated cytokines IL-5 and IL-13 [73,74,75,76]. TLSP receptor and ST2 double-knockout mice showed a complete ablation of the Th2 response, with decreased Th2-related eosinophilia and specific IgE production, when compared to wild type animals [76]. These observations support the notion that both TLSP and IL-33 cytokines are key players in allergic sensitization to pollen. On the other hand, aluminium hydroxide per se, which is frequently used as adjuvant in most in vivo models of pollen sensitization, facilitates the release of IL-33, making it difficult to assess the individual contribution of IL-33 to allergic sensitization [77].
Another cytokine implicated in the allergic sensitization is IL-25, which has the potential to initiate and activate type 2 innate lymphoid cells (ILC2) and Th2 cells [78]. Increased concentrations of IL-25 were observed in nasal secretion and supernatants from patients allergic to Japanese cedar pollen [79]. However, in a direct comparison with IL-33, IL-25 is less efficient in mediating pollen-induced airway hyperreactivity [80, 81].
In general, the involvement of TLR4 signalling and its ligands, such as the endotoxin lipopolysaccharide (LPS), in the initiation of allergic sensitization is still controversially debated. Although low doses of LPS were shown to be associated with the induction of Th2 cells [82, 83], it is unclear whether TLR4 exerts a more general role in the maintenance of inflammatory responses or is essential in initiating Th2 polarization. Whereas TLR4-deficiency abrogated the ability of birch pollen to activate DCs, stimulation of TLR4-deficient DCs with pollen extracts from Japanese cedar, Japanese cypress, short ragweed or Kentucky bluegrass (Poa pratensis) caused up-regulation of maturation markers and induced cytokine secretion similarly to those observed in wild type cells. In vivo, only endotoxin-contaminated mugwort pollen (Artemisia vulgaris) was able to induce allergic sensitization [84, 85]. In line with these observations, it has been shown that co-administration of TLR4 and TLR2 agonists resulted in a general suppression of the allergic response due to shifting of the immune balance toward Th1 [86, 87]. Taken together, these findings suggest that for some, but not for all pollen sources, activation of DCs, a necessary signal for T cell polarization, occurs in a TLR4-independent manner. In contrast, Dittrich et al. demonstrated that innate immune signals are dispensable for the initiation of an inflammatory allergic response to allergens since IL-4, the key cytokine driving Th2 polarization, can bypass TLR4- and MyD88-depedent signalling pathways [88]. Despite the controversies, up-regulation of extracellular TLR2 and TLR4 as well as intracellular TLR3 were detected in the nasal mucosa of allergic rhinitis patients upon allergen challenge [89]. As yet, studies investigating other types of TLRs in the context of allergic sensitization are scarce.
Origin and essentiality of IL-4
In allergic sensitization, DCs are activated either directly by the allergenic source or indirectly via epithelial cell-secreted alarmins. In turn, activated DCs instruct Th2 polarization by providing three important signals to naïve T cells: (i) antigen-derived peptides presented via MHC-II, (ii) expression of co-stimulatory molecules and (iii) the secretion of pro-inflammatory cytokines and chemokines [90]. Activated DCs associated with Th2 priming show an activation of the transcription factors interferon regulatory factor 4 (IRF4) and GATA-3 [91, 92]. DCs also up-regulate the expression of specific Th2-associated surface markers, including OX40L and the notch ligands jagged-1 and -2 [91,92,93,94,95]. Furthermore, activated DCs secrete CCL17, CCL22 and CXCL13 chemokines and express CXCR5 and CCR7 chemokine receptors, which enable them to migrate to the lymph nodes where they prime naïve T cells to become antigen-specific Th2 cells [93, 96,97,98,99].
Apart from the extraordinary role of DCs linking innate to adaptive immunity, the source for the initial IL-4, which is required for efficient Th2 priming, remains elusive. Although basophils, mast cells and NKT cells were shown to produce IL-4, their role remains controversial, particularly in the context of pollen sensitization [100,101,102,103]. Once generated, Th2 cells themselves represent the most important source of IL-4. This raises the question of whether IL-4 is strictly required for the initiation of Th2 polarization. IL-33 and IL-25, for instance, are able to mount a STAT6/GATA-3/IL-4-independent Th2 response via the activation of ILC2s and the accompanied secretion of IL-13 [78, 104,105,106,107]. Similarly, TSLP induced Th2 polarization in the absence of IL-4 via the involvement of NF-κB and STAT5 [106]. However, the role of STAT5, IRF4, and NKT cells in the context of pollen sensitization is unclear and requires in-depth investigations.
In summary, the mechanisms involved in the induction of allergic sensitization by pollen are not fully understood. In fact, it seems that different allergenic pollen sources interact with distinct innate receptors and signalling pathways. The involvement of various PRRs, secreted alarmins, and innate immune cells, and the dependency of DCs in driving pollen-induced Th2 inflammatory processes suggest that allergic sensitization to pollen most likely results from particular combinations of pollen-specific signals rather than from a common determinant of allergenicity. An overview of the initiation process of allergic sensitization is presented in Fig. 1 and Table 1.
Pollen-induced activation of the innate immune system and Th2 polarization. The initiation of allergic sensitization is a complex network of diverse immune cells, such as DCs, ILC2s and neutrophils. Upon encounter with the epithelium the pollen hydrates and releases its content including allergens and various other bioactive molecules (1). At the epithelium (2), this immunogenic cocktail causes the disruption of the epithelial membrane, activates PRRs such as TLR4 and PAR2, triggers the release of alarmins (TSLP, IL-25 and IL-33), and induces oxidative stress and secretion of IL-8 and other pro-inflammatory cytokines (IL-1, IL-6 and TNFα). In turn, DCs are activated (upregulation of surface markers including OX40L and notch ligands), migrate to the lymph nodes (expression of CXCR5), where they present processed antigens via MHC-II to naïve T cells (3). Th2 polarization occurs either STAT6/GATA-3/IL-4-dependent (4A) or -independent via the NF-κB/STAT5 pathway and the contribution of ILC2s (4B). The origin of initial IL-4 for Th2 polarization is still a matter of discussion; proposed candidate are basophils and NKT cells. Once a Th2 immune response has been initiated, a class-switch of B cells to antigen-specific IgE-producing plasma cells occurs resulting in the sensitization of susceptible individuals to pollen allergens (5). CCL17, CCL22 chemokine (C–C motif) ligand 17 and 22, CCR7 C–C chemokine receptor type 7, CD80, CD86 and CD40 cluster of differentiation 80, 86 and 40, CXCL-13 C-X-C motif chemokine 13, CXCR5 C-X-C chemokine receptor type 5, DCs dendritic cells, GATA-3 GATA binding protein 3, IL- Interleukin, ILC2 type 2 innate lymphoid cells, IRF4 interferon regulatory factor 4, NF-κB nuclear factor 'kappa-light-chain-enhancer' of activated B cells, NKT natural killer T, OX40L OX40 ligand, PARs protease activated receptors, PRRs pattern recognition receptors, ROS reactive oxygen species, ST2 IL-33 receptor, STAT5, STAT6 signal transducer and activator of transcription 5 and 6, Th T helper cells, TLR4 toll-like receptor 4, TNFα Tumor necrosis factor alpha, TSLP thymic stromal lymphopoietin
The concept of the pollen matrix in allergic sensitization
The question “why only some environmental proteins cause aberrant Th2-mediated allergic sensitization and others not” has attracted much attention of researchers. Pollen allergens share specific physicochemical properties, such as hydrophilicity, posttranslational modifications and structural stability that favour the bioavailability and facilitate the antigen uptake by APCs [108,109,110]. Only a few pollen allergens, including Cyn d 1, Cup a 1 and Amb a 11, exhibit an intrinsic adjuvant activity [75, 111, 112]. Glycan structures on Cyn d 1 from Bermuda grass pollen, for instance, mimic a molecular pattern that binds C-type lectin receptors, PRRs recognizing complex glycan structures [111]. The cysteine protease Amb a 11 from ragweed pollen was shown to initiate a type 2 inflammation via protease-mediated disruption of airway epithelia [112]. Despite the aforementioned characteristics, no generally applicable concept has been put forward to explain the molecular basis of allergenicity, i.e. the capacity of certain molecules to induce type 2 inflammation and specific IgE antibodies [113]. Despite the lack of common characteristics, allergens are still viewed as the main drivers of the allergic immune response since they trigger the typical reactions of the effector phase of sensitization. Nevertheless, growing evidence supports the essential role of pollen-derived components co-delivered with the allergens in the initiation of allergic sensitization [114].
The immunomodulatory potential of the pollen matrix
Several studies suggested that the allergenic potential of pollen proteins depends on the context of their respective sources. In vitro, purified recombinant Bet v 1 (rBet v 1) could not induce DC maturation compared to a complete aqueous birch pollen extract (BPE). In vivo, BPE, but not rBet v 1, was able to induce Th2 polarization and no differences were observed upon depletion of natural Bet v 1 from BPE [94]. These findings strongly support the view that pure Bet v 1 is a poor immunogen regarding the activation of DCs and the polarization of Th2 cells. We also showed recently that compared to the complete Timothy grass pollen extract, recombinant Phl p 5 (rPhl p 5) was unable to induce IL4-producing Th cells in a short adjuvant-free Th2 polarization in vivo model [115]. Contrasting results have been reported for Amb a 1, the major ragweed pollen allergen. One study showed that the complete ragweed pollen extract, but not purified natural Amb a 1, was able to induce a Th2-biased immune response in mice [116]. On the other hand, Wolf et al. reported that purified natural Amb a 1 isoforms were able to induce high IgE titres in mice even in the absence of Alum as adjuvant [117]. It should be mentioned that different immunization routes (i.e. intranasal instillation and subcutaneous injections) were employed in these Amb a 1 studies. In summary, several purified allergens were shown to lack inherent sensitizing potential. However, the respective pollen contexts (e.g. aqueous pollen extracts) empower them with their full allergenic potential. According to this hypothesis, sensitization to a given allergen might result from a pre-primed Th2 micromilieu initiated by pollen-derived non-allergenic adjuvant components, a phenomenon described as collateral Th2-priming [118, 119]. Yet, the reason for the high sensitization rates to major allergens such as Bet v 1 remains unclear. It is possible that the amounts and stability of proteins are important requirements for a pollen protein to become a major allergen. In this respect, Bet v 1 is the most abundant protein (10–30% of total proteins) in BPE [94] and its thermal- and proteolytic- stability shown to be modulated by intrinsic pollen compounds [120]. In keeping with this view, allergens would then serve as secondary Th2 targets, i.e. target for IgE antibodies, thus determining the antigenic specificity of the allergic inflammatory response.
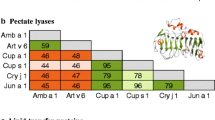
Composition of pollen matrix: intrinsic and extrinsic compounds
Pollen allergens are embedded in a complex and heterogeneous matrix composed of a myriad of bioactive molecules that are co-delivered during the allergic sensitization. The pollen matrix can be divided into two compartments, an intrinsic part consisting of compounds inherent to the pollen, such as proteins, metabolites, lipids, carbohydrates, and an extrinsic fraction, including viruses, aerosols and particles from air pollutants and a pollen-linked microbiome [52, 114, 121,122,123,124,125,126]. Together these compounds provide a specific context for the allergen, designated as the pollen matrix and proposed as a determinant of allergenicity and Th2 sensitization (Fig. 2).
The composition of the pollen matrix influencing the sensitizing potential of allergenic pollen sources. The intrinsic part consists of compounds inherent to the pollen and the extrinsic fraction, includes a prominent microbiome retaining diverse bacterial strains, viruses and fungi. Major immune stimulators can be proteins including allergens with intrinsic adjuvant activities, non-allergenic proteases, but also lipids and metabolites such as PALMS, adenosine and flavonoids. Additionally, climate and exposure to air pollutants shape the composition of the pollen matrix. Details on the immunomodulatory activities of pollen matrix-derived components as well as on the modulation of the matrix composition can be found in Tables 2 and 3. PALMs, pollen-associated lipid mediators; CO2, carbon dioxide; NO2, nitrogen oxides
Intrinsic compartment
Pollen grains are rich in lipids displaying immunomodulatory effects and contributing to the pathogenesis of pollen allergies [121]. Cypress pollen-derived phospholipids were shown to be presented by MHC-related molecules on DCs to T cells via CD1, an interaction causing T cell proliferation and secretion of IFN-γ and IL-4 in cypress-sensitized individuals, but not in healthy controls [122, 127, 128]. Contribution of invariant natural killer T (iNKT) cells in mediating the effects of pollen lipids was also described for olive and birch pollen in humans and in murine in vitro models, respectively [50, 127].
Several studies described the immunostimulatory activity of non-protein low-molecular weight compounds prepared from pollen extracts. These fractions enriched in various metabolites were able to activate innate immunity signalling and preferentially induced a Th2-biased response (Table 2) [49, 121, 129, 130].
Pollen-associated lipid mediators (PALMs), classified into leukotriene-like molecules and phytoprostanes, are eicosanoid-like molecules involved in plant stress responses. PALMs have been identified in aqueous extracts of various pollen sources were shown to attract innate immune cells and to inhibit Th1-differentiation by DCs [131]. Timothy grass- and birch pollen-derived PALMS were shown to attract and activate human neutrophils and eosinophils [132,133,134]. Upon LPS-stimulation of human DCs, pollen-derived phytoprostane E1 (PPE1) inhibited IL-12p70 production via blocking of NF‐κB and activation of PPAR‐γ, hence suppressing the Th1 response [51, 135, 136]. Further, the protein-free low-molecular weight fraction of ragweed pollen was reported to enhance IgE production by Th2-primed B cells, an effect probably attributable to PPE1 [137]. Gilles et al. demonstrated that the low-molecular weight fraction of aqueous pollen extracts induced the expression of Th2-associated notch ligands on DCs [95]. PPE1 was also shown to bind with high affinity to Bet v 1 and to inhibit endolysosomal cathepsin proteases, thus interfering with the antigen-processing machinery in APCs and modulating antigen presentation to T cells [120].
Adenosine has been identified in pollen as a metabolite and immunomodulator with dual properties. Adenosine from BPE was shown to inhibit the production of IL-12p70 by DCs via cAMP signalling. In allogenic co-cultures, BPE-treated DCs from non-atopic donors induced the priming of regulatory T cells. This effect, mediated by pollen-derived adenosine, was less efficient when the DCs in the co-cultures were derived from atopic donors [129]. In vivo, intranasal instillation of adenosine-depleted ragweed pollen extract led to a rapid secretion of Th2-associated cytokines. However, adenosine-depleted pollen extract failed to induce the full allergic lung phenotype when administered to mice that had already been sensitized to ragweed pollen beforehand, showing divergent effects of adenosine: protective during sensitization and pro-inflammatory during challenge. Adenosine-depleted ragweed pollen extract also lost the ability to induce neutrophil and eosinophil migration towards supernatants of bronchial epithelial cells in vitro. Alone, pollen-derived adenosine lacked this ability, suggesting a general effect as cofactor [116]. Functional alteration of bronchial epithelial barriers (ionic permeability and cytokine secretion) was attributed to Timothy grass pollen-derived adenosine and to the flavonoid isorhamnetin. The latter also instructed activated epithelial cells to secrete IL-8, similarly to the complete pollen extract [138]. However, the significance of adenosine in allergic sensitization has been questioned by Mueller et al. who quantified adenosine levels in various pollen extracts and concluded that the measured amounts too low to exert a physiological effect [139]. The discrepancy of these results might be explained by environmental factors influencing the adenosine content in pollen.
Pollen contain non-allergenic proteases, either intrinsic to the pollen or extrinsic derived from its microbiome. Proteases in allergenic sources have also been associated with the pathogenesis of inflammatory allergic diseases [52, 114, 140,141,142]. Pollen-derived proteases can degrade tight junctions and disrupt the airway epithelial barrier, thus facilitate antigen uptake by APCs [143, 144]. The critical role of pollen proteases has been documented in a murine model of asthma in which addition of exogenous proteases to inhaled ovalbumin was necessary to initiate type 2 allergic lung inflammation, whereas the antigen administered alone had no such effect [145].
Extrinsic compartment
Pollutants in ambient air, such as irritant gases and diesel exhaust particles, ozone, carbon dioxide and nitrogen oxides, do not only affect humans but also plants and their pollen in various ways (Table 3) [125, 146]. Pollutants can influence the composition of the pollen microbiota, induce chemical modifications in allergens, act as adjuvant, damage the epithelial barrier, activate immune cells, and in this way trigger inflammation and promote Th2 polarization [124, 147, 148].
In this regard, a correlation between exposure to atmospheric pollutants and the content of allergens as well as of immunostimulatory compounds in pollen was reported [149,150,151]. Pollen collected from plants growing near roads with heavy traffic and exposed to intense air pollution contained higher levels of PALMs, suggesting a stronger immunostimulatory activity than pollen collected in rural meadow areas [152, 153]. Another study demonstrated a positive association between ambient ozone levels and Bet v 1 sensitization of susceptible individuals [151]. In contrast, the content of PALMs with structural and functional homology to mammalian prostaglandin E2 (PGE2) was negatively correlated with ozone concentrations. These observations suggest that areas with low ozone levels and high concentration of PGE2-like PALMs might facilitate sensitization by promoting Th2 responses, whereas areas with high ozone levels and high allergen concentration might be more prone to induce allergic symptoms in already sensitized individuals. A positive correlation was recently observed between air pollutants and the microbial diversity of birch and Timothy grass pollen, which was further associated with the content of allergen and PALMs.
Although the bacterial species involved in the immunomodulatory effects discussed above have not been identified yet [48], the effect of the microbiota inhabiting pollen deserves further investigation. Its composition is variable and specific for each pollen species [48, 154]. Besides intrinsic pollen-derived lipids, microbial lipids constitute a source of immunomodulators and enhancers of the sensitization process [121]. LPS deriving from gram-negative bacteria has been frequently discussed in the context of allergic sensitization [82, 84, 155, 156]. The presence of endotoxin derived from Pseudomonas and Pantoea in mugwort pollen extracts was suggested to be a critical factor for the development of airway allergic inflammation in vivo. In contrast, other studies demonstrated that although LPS acts as a strong adjuvant, it does not account for the full sensitizing activity of birch and ragweed pollen extracts [94, 157].
Gram-positive bacteria could also contribute to the extrinsic adjuvant activity of pollen. Supernatants of homogenized Bacillus cereus and B. subtilis found in high amounts in Timothy grass pollen was able to induce maturation of DCs derived from grass pollen-allergic donors. A co-culture of autologous CD4+ T cells with DCs pulsed with grass pollen extract plus supernatants of homogenized bacteria enhanced T cell proliferation, as well as secretion of type-2 and -17 cytokines, compared to DCs pulsed with grass pollen alone, thus, contributing to Th2- and Th17-mediated inflammation [126].
The influence of plant viral infection on the sensitizing potential of pollen remains largely unknown. A small pilot study compared the size of skin wheals after skin-prick tests with Cocksfoot streak potyvirus (CSV)-infected and non-infected Cocksfoot grass pollen extracts [123]. The observed differences suggested that allergic individuals might be more prone to react to virus-infected pollen, which could have implications in allergy diagnosis and treatment.
The concept of allergen-specific immunotherapy (AIT) in the treatment of pollen allergies
AIT is the only available curative approach of allergic diseases addressing the underlying molecular and cellular mechanisms of the disease. It hereby relies on a constant exposure to allergenic extracts (e.g. pollen extracts) making patients tolerant toward the allergen responsible for the occurrence of symptoms [158]. This induction of immune tolerance is facilitated by the immunosuppressive function (direct interaction or release of anti-inflammatory cytokines) of regulatory T and B cells as well as by tolerogenic DCs [158, 159]. However, the latter two have hardly been investigated in context of pollen AIT yet. In the treatment of pollen allergy, AIT is currently performed with pollen extracts that are applied either subcutaneously (SCIT) or sublingually (SLIT). Both treatment options result in an efficient relief of symptoms, although head-to-head SCIT versus SLIT comparative studies are still lacking. At present, the aforementioned treatment choice mostly depends on the patient´s personal preference [160].
There is a clear difference between the United States and European countries regarding the standardization of allergen extracts as well as the usage of adjuvants (e.g. aluminium hydroxide, alum adsorption). In contrast to the US, where adjuvant-adsorbed pollen extracts are rarely used, the majority of European countries implemented SCIT products adsorbed to alum in their daily routine [161]. Adjuvants are required to facilitate an adaptive immune response. An additional beneficial effect by alum adsorption of antigens is the “depot effect”, resulting in a slow localized release of the antigens at the sites of administration and, thus, preventing systemic side effects such as anaphylaxis [162]. However, as reported herein, pollen extracts possess their own immunomodulatory efficacy making an adjuvant-free application equally possible. Although the evaluation of recombinant wild-type allergens in clinical trials is scarce, it is apparent they are less effective compared to complete pollen extracts implying the presence of adjuvant signals induce tolerance-favouring mechanisms [163].
A major drawback of current AIT products is the standardization methods of pollen extracts among pharmaceutical companies and batch-to-batch variability. Most extract-based AIT vaccines are standardized toward the concentration of disease-dominating allergen(s), while missing out on the complex nature of extracts [161]. Facing these struggles, it is almost impossible to draw accurate conclusions about the immunoreactivity of pollen extracts regarding the induction of immunotolerance as also reflected by the large variance of responders and non-responders to the treatment, and poor treatment compliance [164]. Other treatment-associated disadvantages are, the limitation in sufficient biomarkers predicting treatment efficacy, a long treatment duration and treatment-induced side effects such as de novo sensitizations to other/minor allergens [165, 166]. In order to overcome these conceptual obstacles it is of utmost importance to point out the necessity of improving current AIT procedures and to provide a sufficient AIT alternative not only able to expedite a more efficient induction of immunotolerance but also a perpetual one.
In light of the present review, and since TLSP, IL-33, and to some extent also IL-25 seem to play important roles in the maintenance of Th2 responses, the concomitantly targeting of alarmins or respective signalling pathways may represent an attractive alternative/addition to current AIT protocols [74, 76, 81]. In addition, the characterization of tolerance-inducing pollen compounds could provide further therapeutic tools to ameliorate AIT efficacy.
Conclusion
Pollen sensitization results from complex interactions between pollen-derived adjuvants co-delivered with allergens and the innate immune network. These pollen-derived adjuvants are thought to contribute to the generation of a pro-inflammatory microenvironment at exposure sites that primes DCs to favour Th2 polarization in the draining lymph nodes. Due to a multitude of immunological effects reported for various pollen sources upon interaction with the host cells, it seems reasonable to suggest that initiation of sensitization by various pollen occurs via distinct molecular mechanisms, probably also involving pollen species-specific immune adjuvants. The identity of these pollen-derived factors triggering the initial signals for Th2 polarization remains largely unknown. Thus, their identification and evaluation of their role in the initiation of allergic sensitization should to be addressed in future studies. Such findings will provide mechanistic insights into Th2 polarization in allergic sensitization, and pave the way for novel preventive and therapeutic strategies for an efficient management of pollen allergies.
Availability of data and materials
Not applicable.
Abbreviations
- AIT:
-
Allergen-specific immunotherapy
- Alum:
-
Aluminium hydroxide
- APCs:
-
Antigen-presenting cells
- BPE:
-
Birch pollen extract
- cAMP:
-
Cyclic adenosine monophosphate
- CCL17, CCL22:
-
Chemokine (C–C motif) ligand 17 and 22
- CCR7:
-
C–C chemokine receptor type 7
- CD80:
-
CD86 and CD40, cluster of differentiation 80, 86 and 40
- CSV:
-
Cocksfoot streak potyvirus
- CXCL-13:
-
C-X-C motif chemokine 13
- CXCR5:
-
C-X-C chemokine receptor type 5
- DCs:
-
Dendritic cells
- Fas:
-
CD95, APO-1
- GATA-3:
-
GATA binding protein 3
- Ig:
-
Immunoglobulin
- IL-:
-
Interleukin
- ILC2:
-
Type 2 innate lymphoid cells
- iNKT:
-
Invariant natural killer T
- IRF4:
-
Interferon regulatory factor 4
- LPS:
-
Lipopolysaccharide
- MHC-II:
-
Major histocompatibility complex class II
- MyD88:
-
Myeloid differentiation primary response 88
- NF-κB:
-
Nuclear factor 'kappa-light-chain-enhancer' of activated B cells
- OX40L:
-
OX40 ligand
- PALMs:
-
Pollen-associated lipid mediators
- PARs:
-
Protease activated receptors
- PPE1:
-
Phytoprostane E1
- PR-10:
-
Pathogenesis-related proteins class 10
- PRRs:
-
Pattern recognition receptors
- PPAR‐γ:
-
Peroxisome proliferator-activated receptor gamma
- ROS:
-
Reactive oxygen species
- ST2:
-
IL-33 receptor
- STAT5, STAT6:
-
Signal transducer and activator of transcription 5 and 6
- Th:
-
T helper
- TLR:
-
Toll-like receptor
- TNFα:
-
Tumor necrosis factor alpha
- TSLP:
-
Thymic stromal lymphopoietin
References
Lake IR, Jones NR, Agnew M, Goodess CM, Giorgi F, Hamaoui-Laguel L, et al. Climate change and future pollen allergy in Europe. Environ Health Perspect. 2017;125(3):385–91. https://doi.org/10.1289/ehp173.
Stemeseder T, Klinglmayr E, Moser S, Lueftenegger L, Lang R, Himly M, et al. Cross-sectional study on allergic sensitization of Austrian adolescents using molecule-based IgE profiling. Allergy. 2017;72(5):754–63. https://doi.org/10.1111/all.13071.
Hasnain SM, Al-Frayh AR, Subiza JL, Fernández-Caldas E, Casanovas M, Geith T, et al. Sensitization to indigenous pollen and molds and other outdoor and indoor allergens in allergic patients from saudi arabia, United arab emirates, and Sudan. World Allergy Organ J. 2012;5(6):59–655. https://doi.org/10.1097/WOX.0b013e31825a73cd.
Ogershok PR, Warner DJ, Hogan MB, Wilson NW. Prevalence of pollen sensitization in younger children who have asthma. Allergy Asthma Proc. 2007;28(6):654–8. https://doi.org/10.2500/aap.2007.28.3055.
Smith M, Jager S, Berger U, Sikoparija B, Hallsdottir M, Sauliene I, et al. Geographic and temporal variations in pollen exposure across Europe. Allergy. 2014;69(7):913–23. https://doi.org/10.1111/all.12419.
Garcia-Mozo H. Poaceae pollen as the leading aeroallergen worldwide: a review. Allergy. 2017;72(12):1849–58. https://doi.org/10.1111/all.13210.
Biedermann T, Winther L, Till SJ, Panzner P, Knulst A, Valovirta E. Birch pollen allergy in Europe. Allergy. 2019;74(7):1237–48. https://doi.org/10.1111/all.13758.
Zetterstrom O, Fagerberg E, Wide L. An investigation of pollen extracts from different deciduous trees in patients with springtime allergy in Sweden. Acta Allergol. 1972;27(1):15–211. https://doi.org/10.1111/j.1398-9995.1972.tb01638.x.
Niederberger V, Pauli G, Gronlund H, Froschl R, Rumpold H, Kraft D, et al. Recombinant birch pollen allergens (rBet v 1 and rBet v 2) contain most of the IgE epitopes present in birch, alder, hornbeam, hazel, and oak pollen: a quantitative IgE inhibition study with sera from different populations. J Allergy Clin Immunol. 1998;102(4 Pt 1):579–91. https://doi.org/10.1016/s0091-6749(98)70273-8.
Ipsen H, Bowadt H, Janniche H, Nuchel Petersen B, Munch EP, Wihl JA, et al. Immunochemical characterization of reference alder (Alnus glutinosa) and hazel (Corylus avellana) pollen extracts and the partial immunochemical identity between the major allergens of alder, birch and hazel pollens. Allergy. 1985;40(7):510–8. https://doi.org/10.1111/j.1398-9995.1985.tb00259.x.
Ipsen H, Hansen OC. The NH2-terminal amino acid sequence of the immunochemically partial identical major allergens of Alder (Alnus glutinosa) Aln g I, birch (Betula verrucosa) Bet v I, hornbeam (Carpinus betulus) Car b I and oak (Quercus alba) Que a I pollens. Mol Immunol. 1991;28(11):1279–88. https://doi.org/10.1016/0161-5890(91)90015-c.
Heath MD, Collis J, Batten T, Hutchings JW, Swan N, Skinner MA. Molecular, proteomic and immunological parameters of allergens provide inclusion criteria for new candidates within established grass and tree homologous groups. World Allergy Organ J. 2015;8(1):21. https://doi.org/10.1186/s40413-015-0069-9.
Wuthrich B, Straumann F. Pollen cross-reactivity can we establish a link between the in vitro results and the clinical situation? Allergy. 1997;52(12):1187–93. https://doi.org/10.1111/j.1398-9995.1997.tb02522.x.
Hirschwehr R, Jager S, Horak F, Ferreira F, Valenta R, Ebner C, et al. Allergens from birch pollen and pollen of the European chestnut share common epitopes. Clin Exp Allergy. 1993;23(9):755–61. https://doi.org/10.1111/j.1365-2222.1993.tb00363.x.
Zuberbier T, Lotvall J, Simoens S, Subramanian SV, Church MK. Economic burden of inadequate management of allergic diseases in the European Union: a GA(2) LEN review. Allergy. 2014;69(10):1275–9. https://doi.org/10.1111/all.12470.
Calzada D, Cremades-Jimeno L, Pedro MA, Baos S, Rial M, Sastre J, et al. Therapeutic potential of peptides from Ole e 1 in olive-pollen allergy. Sci Rep. 2019;9(1):15942. https://doi.org/10.1038/s41598-019-52286-3.
Descotes J, Choquet-Kastylevsky G. Gell and Coombs's classification: is it still valid? Toxicology. 2001;158(1–2):43–9. https://doi.org/10.1016/s0300-483x(00)00400-5.
Kim B, Kim TH. Fundamental role of dendritic cells in inducing Th2 responses. Korean J Intern Med. 2018;33(3):483–9. https://doi.org/10.3904/kjim.2016.227.
Kumar S, Jeong Y, Ashraf MU, Bae YS. Dendritic cell-mediated Th2 immunity and immune disorders. Int J Mol Sci. 2019;20(9):2159. https://doi.org/10.3390/ijms20092159.
Blümchen K, Kallinich T, Hamelmann E. Interleukin-5: a novel target for asthma therapy. Expert Opin Biol Ther. 2001;1(3):433–53. https://doi.org/10.1517/14712598.1.3.433.
Seyfizadeh N, Seyfizadeh N, Gharibi T, Babaloo Z. Interleukin-13 as an important cytokine: a review on its roles in some human diseases. Acta Microbiol Immunol Hung. 2015;62(4):341–78. https://doi.org/10.1556/030.62.2015.4.2.
Soyer OU, Akdis M, Ring J, Behrendt H, Crameri R, Lauener R, et al. Mechanisms of peripheral tolerance to allergens. Allergy. 2013;68(2):161–70. https://doi.org/10.1111/all.12085.
Sitcharungsi R, Sirivichayakul C. Allergic diseases and helminth infections. Pathog Glob Health. 2013;107(3):110–5. https://doi.org/10.1179/2047773213y.0000000080.
Schwartz C, Turqueti-Neves A, Hartmann S, Yu P, Nimmerjahn F, Voehringer D. Basophil-mediated protection against gastrointestinal helminths requires IgE-induced cytokine secretion. Proc Natl Acad Sci USA. 2014;111(48):E5169–E51775177. https://doi.org/10.1073/pnas.1412663111.
Chen F, Liu Z, Wu W, Rozo C, Bowdridge S, Millman A, et al. An essential role for TH2-type responses in limiting acute tissue damage during experimental helminth infection. Nat Med. 2012;18(2):260–6. https://doi.org/10.1038/nm.2628.
Monticelli LA, Sonnenberg GF, Abt MC, Alenghat T, Ziegler CG, Doering TA, et al. Innate lymphoid cells promote lung-tissue homeostasis after infection with influenza virus. Nat Immunol. 2011;12(11):1045–54. https://doi.org/10.1031/ni.2131.
Herbert DR, Orekov T, Roloson A, Ilies M, Perkins C, O'Brien W, et al. Arginase I suppresses IL-12/IL-23p40-driven intestinal inflammation during acute schistosomiasis. J Immunol. 2010;184(11):6438–46. https://doi.org/10.4049/jimmunol.0902009.
Pesce JT, Ramalingam TR, Mentink-Kane MM, Wilson MS, El Kasmi KC, Smith AM, et al. Arginase-1-expressing macrophages suppress Th2 cytokine-driven inflammation and fibrosis. PLoS Pathog. 2009;5(4):e1000371. https://doi.org/10.1371/journal.ppat.1000371.
Nguyen JK, Austin E, Huang A, Mamalis A, Jagdeo J. The IL-4/IL-13 axis in skin fibrosis and scarring: mechanistic concepts and therapeutic targets. Arch Dermatol Res. 2020;312(2):81–92. https://doi.org/10.1007/s00403-019-01972-3.
Jackson JA, Friberg IM, Little S, Bradley JE. Review series on helminths, immune modulation and the hygiene hypothesis: immunity against helminths and immunological phenomena in modern human populations: coevolutionary legacies? Immunology. 2009;126(1):18–27. https://doi.org/10.1111/j.1365-2567.2008.03010.x.
Díaz A, Allen JE. Mapping immune response profiles: the emerging scenario from helminth immunology. Eur J Immunol. 2007;37(12):3319–26. https://doi.org/10.1002/eji.200737765.
Loke Pn, Gallagher I, Nair MG, Zang X, Brombacher F, Mohrs M, et al. Alternative activation is an innate response to injury that requires CD4+ T cells to be sustained during chronic infection. J Immunol. 2007;179(6):3926–36. https://doi.org/10.4049/jimmunol.179.6.3926.
Galli SJ, Starkl P, Marichal T, Tsai M. Mast cells and IgE in defense against venoms: Possible "good side" of allergy? Allergol Int. 2016;65(1):3–15. https://doi.org/10.1016/j.alit.2015.09.002.
Marichal T, Starkl P, Reber LL, Kalesnikoff J, Oettgen HC, Tsai M, et al. A beneficial role for immunoglobulin E in host defense against honeybee venom. Immunity. 2013;39(5):963–75. https://doi.org/10.1016/j.immuni.2013.10.005.
Tsai M, Starkl P, Marichal T, Galli SJ. Testing the 'toxin hypothesis of allergy': mast cells, IgE, and innate and acquired immune responses to venoms. Curr Opin Immunol. 2015;36:80–7. https://doi.org/10.1016/j.coi.2015.07.001.
Doull IJ, Lawrence S, Watson M, Begishvili T, Beasley RW, Lampe F, et al. Allelic association of gene markers on chromosomes 5q and 11q with atopy and bronchial hyperresponsiveness. Am J Respir Crit Care Med. 1996;153(4 Pt 1):1280–4. https://doi.org/10.1164/ajrccm.153.4.8616554.
Strachan DP. Hay fever, hygiene, and household size. BMJ. 1989;299(6710):1259–60. https://doi.org/10.1136/bmj.299.6710.1259.
Fishbein AB, Fuleihan RL. The hygiene hypothesis revisited: does exposure to infectious agents protect us from allergy? Curr Opin Pediatr. 2012;24(1):98–102. https://doi.org/10.1097/MOP.0b013e32834ee57c.
Lambrecht BN, Hammad H. The immunology of the allergy epidemic and the hygiene hypothesis. Nat Immunol. 2017;18(10):1076–83. https://doi.org/10.1038/ni.3829.
Liu AH. Revisiting the hygiene hypothesis for allergy and asthma. J Allergy Clin Immunol. 2015;136(4):860–5. https://doi.org/10.1016/j.jaci.2015.08.012.
Sbihi H, Boutin RC, Cutler C, Suen M, Finlay BB, Turvey SE. Thinking bigger: how early-life environmental exposures shape the gut microbiome and influence the development of asthma and allergic disease. Allergy. 2019;74(11):2103–15. https://doi.org/10.1111/all.13812.
Potaczek DP, Harb H, Michel S, Alhamwe BA, Renz H, Tost J. Epigenetics and allergy: from basic mechanisms to clinical applications. Epigenomics. 2017;9(4):539–71. https://doi.org/10.2217/epi-2016-0162.
Gilles S, Akdis C, Lauener R, Schmid-Grendelmeier P, Bieber T, Schäppi G, et al. The role of environmental factors in allergy: A critical reappraisal. Exp Dermatol. 2018;27(11):1193–200. https://doi.org/10.1111/exd.13769.
Knaysi G, Smith AR, Wilson JM, Wisniewski JA. The skin as a route of allergen exposure: part II. Allergens and role of the microbiome and environmental exposures. Curr Allergy Asthma Rep. 2017;17(1):7. https://doi.org/10.1007/s11882-017-0675-4.
Serhane H, Amro L, Sajiai H, Alaoui YA. Prevalence of skin sensitization to pollen of date palm in Marrakesh, morocco. J Allergy (Cairo). 2017;2017:6425869. https://doi.org/10.1155/2017/6425869.
Mattila P, Joenvaara S, Renkonen J, Toppila-Salmi S, Renkonen R. Allergy as an epithelial barrier disease. Clin Transl Allergy. 2011;1(1):5. https://doi.org/10.1186/2045-7022-1-5.
Bacher P, Heinrich F, Stervbo U, Nienen M, Vahldieck M, Iwert C, et al. Regulatory T cell specificity directs tolerance versus allergy against aeroantigens in humans. Cell. 2016;167(4):1067–78.e16. https://doi.org/10.1016/j.cell.2016.09.050.
Obersteiner A, Gilles S, Frank U, Beck I, Haring F, Ernst D, et al. Pollen-associated microbiome correlates with pollution parameters and the allergenicity of pollen. PLoS ONE. 2016;11(2):e0149545. https://doi.org/10.1371/journal.pone.0149545.
Gilles-Stein S, Beck I, Chaker A, Bas M, McIntyre M, Cifuentes L, et al. Pollen derived low molecular compounds enhance the human allergen specific immune response in vivo. Clin Exp Allergy. 2016;46(10):1355–65. https://doi.org/10.1111/cea.12739.
Gonzalez Roldan N, Engel R, Dupow S, Jakob K, Koops F, Orinska Z, et al. Lipid mediators from timothy grass pollen contribute to the effector phase of allergy and prime dendritic cells for glycolipid presentation. Front Immunol. 2019;10:974. https://doi.org/10.3389/fimmu.2019.00974.
Gilles S, Mariani V, Bryce M, Mueller MJ, Ring J, Jakob T, et al. Pollen-derived E1-phytoprostanes signal via PPAR-gamma and NF-kappaB-dependent mechanisms. J Immunol. 2009;182(11):6653–8. https://doi.org/10.4049/jimmunol.0802613.
McKenna OE, Posselt G, Briza P, Lackner P, Schmitt AO, Gadermaier G, et al. Multi-approach analysis for the identification of proteases within birch pollen. Int J Mol Sci. 2017;18(7):1433. https://doi.org/10.3390/ijms18071433.
Raftery MJ, Saldanha RG, Geczy CL, Kumar RK. Mass spectrometric analysis of electrophoretically separated allergens and proteases in grass pollen diffusates. Respir Res. 2003;4:10. https://doi.org/10.1186/1465-9921-4-10.
Mabalirajan U. Possible involvement of protease-mediated neutrophil recruitment and epithelial barrier disruption in ragweed pollen sensitization. Am J Respir Cell Mol Biol. 2017;56(2):271–2. https://doi.org/10.1165/rcmb.2016-0148LE.
Hosoki K, Brasier AR, Kurosky A, Boldogh I, Sur S. Reply: protease plays a role in ragweed pollen-induced neutrophil recruitment and epithelial barrier disruption. Am J Respir Cell Mol Biol. 2017;56(2):272–3. https://doi.org/10.1165/rcmb.2016-0281LE.
Van Cleemput J, Poelaert KCK, Laval K, Impens F, Van den Broeck W, Gevaert K, et al. Pollens destroy respiratory epithelial cell anchors and drive alphaherpesvirus infection. Sci Rep. 2019;9(1):4787. https://doi.org/10.1038/s41598-019-41305-y.
Renkonen J, Mattila P, Lehti S, Makinen J, Sormunen R, Tervo T, et al. Birch pollen allergen Bet v 1 binds to and is transported through conjunctival epithelium in allergic patients. Allergy. 2009;64(6):868–75. https://doi.org/10.1111/j.1398-9995.2008.01919.x.
Lopez-Rodriguez JC, Solis-Fernandez G, Barderas R, Villalba M, Batanero E. Effects of Ole e 1 on Human Bronchial Epithelial Cells Cultured at the Air-Liquid Interface. J Investig Allergol Clin Immunol. 2018;28(3):186–9. https://doi.org/10.18176/jiaci.0227.
Kumamoto J, Tsutsumi M, Goto M, Nagayama M, Denda M. Japanese Cedar (Cryptomeria japonica) pollen allergen induces elevation of intracellular calcium in human keratinocytes and impairs epidermal barrier function of human skin ex vivo. Arch Dermatol Res. 2016;308(1):49–544. https://doi.org/10.1007/s00403-015-1602-y.
Lee SI, le Pham D, Shin YS, Suh DH, Park HS. Environmental changes could enhance the biological effect of Hop J pollens on human airway epithelial cells. J Allergy Clin Immunol. 2014;134(2):470–2. https://doi.org/10.1016/j.jaci.2014.01.034.
Tyurin YA, Lissovskaya SA, Fassahov RS, Mustafin IG, Shamsutdinov AF, Shilova MA, et al. Cytokine profile of patients with allergic rhinitis caused by pollen, mite, and microbial allergen sensitization. J Immunol Res. 2017;2017:3054217. https://doi.org/10.1155/2017/3054217.
Zhu DD, Zhu XW, Jiang XD, Dong Z. Thymic stromal lymphopoietin expression is increased in nasal epithelial cells of patients with mugwort pollen sensitive-seasonal allergic rhinitis. Chin Med J (Engl). 2009;122(19):2303–7.
Salter BM, Oliveria JP, Nusca G, Smith SG, Tworek D, Mitchell PD, et al. IL-25 and IL-33 induce Type 2 inflammation in basophils from subjects with allergic asthma. Respir Res. 2016;17:5. https://doi.org/10.1186/s12931-016-0321-z.
Ochiai S, Jagot F, Kyle RL, Hyde E, White RF, Prout M, et al. Thymic stromal lymphopoietin drives the development of IL-13(+) Th2 cells. Proc Natl Acad Sci U S A. 2018;115(5):1033–8. https://doi.org/10.1073/pnas.1714348115.
Deng R, Chen X, Zhang Y, Bian F, Gao N, Hu J, et al. Short ragweed pollen promotes M2 macrophage polarization via TSLP/TSLPR/OX40L signaling in allergic inflammation. Mucosal Immunol. 2019;12(5):1141–9. https://doi.org/10.1038/s41385-019-0187-8.
Li DQ, Zhang L, Pflugfelder SC, De Paiva CS, Zhang X, Zhao G, et al. Short ragweed pollen triggers allergic inflammation through Toll-like receptor 4-dependent thymic stromal lymphopoietin/OX40 ligand/OX40 signaling pathways. J Allergy Clin Immunol. 2011;128(6):1318–25.e2. https://doi.org/10.1016/j.jaci.2011.06.041.
Hosoki K, Aguilera-Aguirre L, Brasier AR, Kurosky A, Boldogh I, Sur S. Facilitation of allergic sensitization and allergic airway inflammation by pollen-induced innate neutrophil recruitment. Am J Respir Cell Mol Biol. 2016;54(1):81–90. https://doi.org/10.1165/rcmb.2015-0044OC.
Chen X, Deng R, Chi W, Hua X, Lu F, Bian F, et al. IL-27 signaling deficiency develops Th17-enhanced Th2-dominant inflammation in murine allergic conjunctivitis model. Allergy. 2019;74(5):910–21. https://doi.org/10.1111/all.13691.
Shalaby KH, Allard-Coutu A, O'Sullivan MJ, Nakada E, Qureshi ST, Day BJ, et al. Inhaled birch pollen extract induces airway hyperresponsiveness via oxidative stress but independently of pollen-intrinsic NADPH oxidase activity, or the TLR4-TRIF pathway. J Immunol. 2013;191(2):922–33. https://doi.org/10.4049/jimmunol.1103644.
Yadav UC, Ramana KV, Srivastava SK. Aldose reductase inhibition suppresses airway inflammation. Chem Biol Interact. 2011;191(1–3):339–45. https://doi.org/10.1016/j.cbi.2011.02.014.
Hosoki K, Redding D, Itazawa T, Chakraborty A, Tapryal N, Qian S, et al. Innate mechanism of pollen- and cat dander-induced oxidative stress and DNA damage in the airways. J Allergy Clin Immunol. 2017;140(5):1436–9.e5. https://doi.org/10.1016/j.jaci.2017.04.044.
Li J, Zhang L, Chen X, Chen D, Hua X, Bian F, et al. Pollen/TLR4 innate immunity signaling initiates IL-33/ST2/Th2 pathways in allergic inflammation. Sci Rep. 2016;6:36150. https://doi.org/10.1038/srep36150.
Gluck J, Rymarczyk B, Jura-Szoltys E, Rogala B. Serum levels of interleukin 33 and its receptor ST2 in patients treated with subcutaneous allergen immunotherapy in intermittent allergic rhinitis. Cent Eur J Immunol. 2019;44(2):214–7. https://doi.org/10.5114/ceji.2019.87075.
Matsuba-Kitamura S, Yoshimoto T, Yasuda K, Futatsugi-Yumikura S, Taki Y, Muto T, et al. Contribution of IL-33 to induction and augmentation of experimental allergic conjunctivitis. Int Immunol. 2010;22(6):479–89. https://doi.org/10.1093/intimm/dxq035.
Gabriele L, Schiavoni G, Mattei F, Sanchez M, Sestili P, Butteroni C, et al. Novel allergic asthma model demonstrates ST2-dependent dendritic cell targeting by cypress pollen. J Allergy Clin Immunol. 2013;132(3):686–95.e7. https://doi.org/10.1016/j.jaci.2013.02.037.
Akasaki S, Matsushita K, Kato Y, Fukuoka A, Iwasaki N, Nakahira M, et al. Murine allergic rhinitis and nasal Th2 activation are mediated via TSLP- and IL-33-signaling pathways. Int Immunol. 2016;28(2):65–766. https://doi.org/10.1093/intimm/dxv055.
Rose WA 2nd, Okragly AJ, Patel CN, Benschop RJ. IL-33 released by alum is responsible for early cytokine production and has adjuvant properties. Sci Rep. 2015;5:13146. https://doi.org/10.1038/srep13146.
Mjösberg JM, Trifari S, Crellin NK, Peters CP, van Drunen CM, Piet B, et al. Human IL-25- and IL-33-responsive type 2 innate lymphoid cells are defined by expression of CRTH2 and CD161. Nat Immunol. 2011;12(11):1055–62. https://doi.org/10.1038/ni.2104.
Kouzaki H, Kikuoka H, Matsumoto K, Kato T, Tojima I, Shimizu S, et al. A mechanism of interleukin-25 production from airway epithelial cells induced by Japanese cedar pollen. Clin Immunol. 2018;193:46–51. https://doi.org/10.1016/j.clim.2018.01.009.
Hong HY, Chen FH, Sun YQ, Hu XT, Wei Y, Fan YP, et al. Local IL-25 contributes to Th2-biased inflammatory profiles in nasal polyps. Allergy. 2018;73(2):459–69. https://doi.org/10.1111/all.13267.
Barlow JL, Peel S, Fox J, Panova V, Hardman CS, Camelo A, et al. IL-33 is more potent than IL-25 in provoking IL-13-producing nuocytes (type 2 innate lymphoid cells) and airway contraction. J Allergy Clin Immunol. 2013;132(4):933–41. https://doi.org/10.1016/j.jaci.2013.05.012.
Eisenbarth SC, Piggott DA, Huleatt JW, Visintin I, Herrick CA, Bottomly K. Lipopolysaccharide-enhanced, toll-like receptor 4-dependent T helper cell type 2 responses to inhaled antigen. J Exp Med. 2002;196(12):1645–51. https://doi.org/10.1084/jem.20021340.
Kumar S, Adhikari A. Dose-dependent immunomodulating effects of endotoxin in allergic airway inflammation. Innate Immun. 2017;23(3):249–57. https://doi.org/10.1177/1753425917690443.
Oteros J, Bartusel E, Alessandrini F, Nunez A, Moreno DA, Behrendt H, et al. Artemisia pollen is the main vector for airborne endotoxin. J Allergy Clin Immunol. 2019;143(1):369–77.e5. https://doi.org/10.1016/j.jaci.2018.05.040.
Kamijo S, Takai T, Kuhara T, Tokura T, Ushio H, Ota M, et al. Cupressaceae pollen grains modulate dendritic cell response and exhibit IgE-inducing adjuvant activity in vivo. J Immunol. 2009;183(10):6087–94. https://doi.org/10.4049/jimmunol.0901039.
Chung SH, Choi SH, Cho KJ, Joo CK. Toll-like receptor 4 signalling attenuates experimental allergic conjunctivitis. Clin Exp Immunol. 2011;164(2):275–81. https://doi.org/10.1111/j.1365-2249.2011.04368.x.
Velasco G, Campo M, Manrique OJ, Bellou A, He H, Arestides RS, et al. Toll-like receptor 4 or 2 agonists decrease allergic inflammation. Am J Respir Cell Mol Biol. 2005;32(3):218–24. https://doi.org/10.1165/rcmb.2003-0435OC.
Dittrich AM, Chen HC, Xu L, Ranney P, Connolly S, Yarovinsky TO, et al. A new mechanism for inhalational priming: IL-4 bypasses innate immune signals. J Immunol. 2008;181(10):7307–15. https://doi.org/10.4049/jimmunol.181.10.7307.
Fransson M, Adner M, Erjefalt J, Jansson L, Uddman R, Cardell LO. Up-regulation of Toll-like receptors 2, 3 and 4 in allergic rhinitis. Respir Res. 2005;6:100. https://doi.org/10.1186/1465-9921-6-100.
Yang D, Han Z, Oppenheim JJ. Alarmins and immunity. Immunol Rev. 2017;280(1):41–56. https://doi.org/10.1111/imr.12577.
Gueguen C, Bouley J, Moussu H, Luce S, Duchateau M, Chamot-Rooke J, et al. Changes in markers associated with dendritic cells driving the differentiation of either TH2 cells or regulatory T cells correlate with clinical benefit during allergen immunotherapy. J Allergy Clin Immunol. 2016;137(2):545–58. https://doi.org/10.1016/j.jaci.2015.09.015.
Walker JA, McKenzie ANJ. TH2 cell development and function. Nat Rev Immunol. 2018;18(2):121–33. https://doi.org/10.1038/nri.2017.118.
Han M, Hu R, Ma J, Zhang B, Chen C, Li H, et al. Fas signaling in dendritic cells mediates Th2 polarization in HDM-induced allergic pulmonary inflammation. Front Immunol. 2018;9:3045. https://doi.org/10.3389/fimmu.2018.03045.
Aglas L, Gilles S, Bauer R, Huber S, Araujo GR, Mueller G, et al. Context matters: TH2 polarization resulting from pollen composition and not from protein-intrinsic allergenicity. J Allergy Clin Immunol. 2018;142(3):984–7.e6. https://doi.org/10.1016/j.jaci.2018.05.004.
Gilles S, Beck I, Lange S, Ring J, Behrendt H, Traidl-Hoffmann C. Non-allergenic factors from pollen modulate T helper cell instructing notch ligands on dendritic cells. World Allergy Organ J. 2015;8(1):2. https://doi.org/10.1186/s40413-014-0054-8.
Leon B, Ballesteros-Tato A, Browning JL, Dunn R, Randall TD, Lund FE. Regulation of T(H)2 development by CXCR5+ dendritic cells and lymphotoxin-expressing B cells. Nat Immunol. 2012;13(7):681–90. https://doi.org/10.1038/ni.2309.
Kikuchi K, Yanagawa Y, Onoé K. CCR7 Ligand-enhanced phagocytosis of various antigens in mature dendritic cells—time course and antigen distribution different from phagocytosis in immature dendritic cells. Microbiol Immunol. 2005;49(6):535–44. https://doi.org/10.1111/j.1348-0421.2005.tb03759.x.
Kucharczyk A, Jahnz-Rózyk K, Targowski T, Grabowska-Krawiec P, Owczarek W, Kucharczyk P. Evaluation of CCL22 AND CCL17 Concentrations In Patients Sensitized To Grass Pollen Grains During Specific Immunotherapy. Int Rev. 2010;16(3–4):63–70.
Batsalova T, Kostova Z, Moten D, Teneva I, Dzhambazov B. Serum levels of certain CC and CXC chemokines in birch pollen allergic individuals out of the pollen season. Adv Biol. Earth Sci. 2017;2(1):23–33.
Zhong W, Su W, Zhang Y, Liu Q, Wu J, Di C, et al. Basophils as a primary inducer of the T helper type 2 immunity in ovalbumin-induced allergic airway inflammation. Immunology. 2014;142(2):202–15. https://doi.org/10.1111/imm.12240.
Okamoto Y, Horiguchi S, Yamamoto H, Yonekura S, Hanazawa T. Present situation of cedar pollinosis in Japan and its immune responses. Allergol Int. 2009;58(2):155–62. https://doi.org/10.2332/allergolint.08-RAI-0074.
Abos Gracia B, Lopez Relano J, Revilla A, Castro L, Villalba M, Martin Adrados B, et al. Human invariant natural killer T cells respond to antigen-presenting cells exposed to lipids from olea europaea pollen. Int Arch Allergy Immunol. 2017;173(1):12–22. https://doi.org/10.1159/000467394.
Mukai K, Tsai M, Saito H, Galli SJ. Mast cells as sources of cytokines, chemokines, and growth factors. Immunol Rev. 2018;282(1):121–50. https://doi.org/10.1111/imr.12634.
Halim TY, Steer CA, Matha L, Gold MJ, Martinez-Gonzalez I, McNagny KM, et al. Group 2 innate lymphoid cells are critical for the initiation of adaptive T helper 2 cell-mediated allergic lung inflammation. Immunity. 2014;40(3):425–35. https://doi.org/10.1016/j.immuni.2014.01.011.
Hurrell BP, Shafiei Jahani P, Akbari O. Social networking of group two innate lymphoid cells in allergy and asthma. Front Immunol. 2018;9:2694. https://doi.org/10.3389/fimmu.2018.02694.
Hussaarts L, Yazdanbakhsh M, Guigas B. Priming dendritic cells for th2 polarization: lessons learned from helminths and implications for metabolic disorders. Front Immunol. 2014;5:499. https://doi.org/10.3389/fimmu.2014.00499.
Pasha MA, Patel G, Hopp R, Yang Q. Role of innate lymphoid cells in allergic diseases. Allergy Asthma Proc. 2019;40(3):138–45. https://doi.org/10.2500/aap.2019.40.4217.
Traidl-Hoffmann C, Jakob T, Behrendt H. Determinants of allergenicity. J Allergy Clin Immunol. 2009;123(3):558–66. https://doi.org/10.1016/j.jaci.2008.12.003.
Scheurer S, Toda M, Vieths S. What makes an allergen? Clin Exp Allergy. 2015;45(7):1150–61. https://doi.org/10.1111/cea.12571.
Deifl S, Bohle B. Factors influencing the allergenicity and adjuvanticity of allergens. Immunotherapy. 2011;3(7):881–93. https://doi.org/10.2217/imt.11.69.
Hsu SC, Chen CH, Tsai SH, Kawasaki H, Hung CH, Chu YT, et al. Functional interaction of common allergens and a C-type lectin receptor, dendritic cell-specific ICAM3-grabbing non-integrin (DC-SIGN), on human dendritic cells. J Biol Chem. 2010;285(11):7903–10. https://doi.org/10.1074/jbc.M109.058370.
Groeme R, Airouche S, Kopecny D, Jaekel J, Savko M, Berjont N, et al. Structural and functional characterization of the major allergen Amb a 11 from short ragweed pollen. J Biol Chem. 2016;291(25):13076–87. https://doi.org/10.1074/jbc.M115.702001.
Radauer C, Bublin M, Wagner S, Mari A, Breiteneder H. Allergens are distributed into few protein families and possess a restricted number of biochemical functions. J Allergy Clin Immunol. 2008;121(4):847–52.e7. https://doi.org/10.1016/j.jaci.2008.01.025.
Gilles S, Behrendt H, Ring J, Traidl-Hoffmann C. The pollen enigma: modulation of the allergic immune response by non-allergenic, pollen-derived compounds. Curr Pharm Des. 2012;18(16):2314–9. https://doi.org/10.2174/138161212800166040.
Araujo GR, Aglas L, Vaz ER, Machado Y, Huber S, Himly M, et al. TGFbeta1 mimetic peptide modulates immune response to grass pollen allergens in mice. Allergy. 2019. https://doi.org/10.1111/all.14108.
Wimmer M, Alessandrini F, Gilles S, Frank U, Oeder S, Hauser M, et al. Pollen-derived adenosine is a necessary cofactor for ragweed allergy. Allergy. 2015;70(8):944–54. https://doi.org/10.1111/all.12642.
Wolf M, Twaroch TE, Huber S, Reithofer M, Steiner M, Aglas L, et al. Amb a 1 isoforms: unequal siblings with distinct immunological features. Allergy. 2017;72(12):1874–82. https://doi.org/10.1111/all.13196.
Eisenbarth SC, Zhadkevich A, Ranney P, Herrick CA, Bottomly K. IL-4-dependent Th2 collateral priming to inhaled antigens independent of toll-like receptor 4 and myeloid differentiation factor 88. J Immunol. 2004;172(7):4527–34. https://doi.org/10.4049/jimmunol.172.7.4527.
Cadot P, Meyts I, Vanoirbeek JA, Vanaudenaerde B, Bullens DM, Ceuppens JL. Sensitization to inhaled ryegrass pollen by collateral priming in a murine model of allergic respiratory disease. Int Arch Allergy Immunol. 2010;152(3):233–42. https://doi.org/10.1159/000283031.
Soh WT, Aglas L, Mueller GA, Gilles S, Weiss R, Scheiblhofer S, et al. Multiple roles of Bet v 1 ligands in allergen stabilization and modulation of endosomal protease activity. Allergy. 2019;74(12):2382–93. https://doi.org/10.1111/all.13948.
Bublin M, Eiwegger T, Breiteneder H. Do lipids influence the allergic sensitization process? J Allergy Clin Immunol. 2014;134(3):521–9. https://doi.org/10.1016/j.jaci.2014.04.015.
Bashir ME, Lui JH, Palnivelu R, Naclerio RM, Preuss D. Pollen lipidomics: lipid profiling exposes a notable diversity in 22 allergenic pollen and potential biomarkers of the allergic immune response. PLoS ONE. 2013;8(2):e57566. https://doi.org/10.1371/journal.pone.0057566.
Pallett DW, Soh E, Edwards ML, Bodey K, Lau LC, Cooper JI, et al. Proof of concept pilot study: prevalence of grass virus infection and the potential for effects on the allergenic potency of pollen. Environ Health. 2009;8(Suppl 1):S10. https://doi.org/10.1186/1476-069x-8-s1-s10.
Reinmuth-Selzle K, Kampf CJ, Lucas K, Lang-Yona N, Frohlich-Nowoisky J, Shiraiwa M, et al. Air pollution and climate change effects on allergies in the anthropocene: abundance, interaction, and modification of allergens and adjuvants. Environ Sci Technol. 2017;51(8):4119–411. https://doi.org/10.1021/acs.est.6b04908.
Senechal H, Visez N, Charpin D, Shahali Y, Peltre G, Biolley JP, et al. A review of the effects of major atmospheric pollutants on pollen grains, pollen content, and allergenicity. Sci World J. 2015;2015:940243. https://doi.org/10.1155/2015/940243.
Heydenreich B, Bellinghausen I, Konig B, Becker WM, Grabbe S, Petersen A, et al. Gram-positive bacteria on grass pollen exhibit adjuvant activity inducing inflammatory T cell responses. Clin Exp Allergy. 2012;42(1):76–84. https://doi.org/10.1111/j.1365-2222.2011.03888.x.
Abos-Gracia B, del Moral MG, Lopez-Relano J, Viana-Huete V, Castro L, Villalba M, et al. Olea europaea pollen lipids activate invariant natural killer T cells by upregulating CD1d expression on dendritic cells. J Allergy Clin Immunol. 2013;131(5):1393–9.e5. https://doi.org/10.1016/j.jaci.2012.11.014.
Agea E, Russano A, Bistoni O, Mannucci R, Nicoletti I, Corazzi L, et al. Human CD1-restricted T cell recognition of lipids from pollens. J Exp Med. 2005;202(2):295–308. https://doi.org/10.1084/jem.20050773.
Gilles S, Fekete A, Zhang X, Beck I, Blume C, Ring J, et al. Pollen metabolome analysis reveals adenosine as a major regulator of dendritic cell-primed T(H) cell responses. J Allergy Clin Immunol. 2011;127(2):454–461.e9. https://doi.org/10.1016/j.jaci.2010.12.1082.
Gilles S, Mariani V, Bryce M, Mueller MJ, Ring J, Behrendt H, et al. Pollen allergens do not come alone: pollen associated lipid mediators (PALMS) shift the human immune systems towards a T(H)2-dominated response. Allergy Asthma Clin Immunol. 2009;5(1):3. https://doi.org/10.1186/1710-1492-5-3.
Gunawan H, Takai T, Kamijo S, Wang XL, Ikeda S, Okumura K, et al. Characterization of proteases, proteins, and eicosanoid-like substances in soluble extracts from allergenic pollen grains. Int Arch Allergy Immunol. 2008;147(4):276–88. https://doi.org/10.1159/000144035.
Behrendt H, Kasche A, Traidl C, Plötz S, Huss-Marp J, Risse U, et al. Pollen grains contain and release not only allergens, but also eicosanoid-like substances with neutrophil chemotactic activity: a new step in the initiation of allergie sensitization? In: Ring J, Behrendt H, editors. New Trends in Allergy. Berlin: Springer; 2002. p. 3–8.
Plotz SG, Traidl-Hoffmann C, Feussner I, Kasche A, Feser A, Ring J, et al. Chemotaxis and activation of human peripheral blood eosinophils induced by pollen-associated lipid mediators. J Allergy Clin Immunol. 2004;113(6):1152–60. https://doi.org/10.1016/j.jaci.2004.03.011.
Traidl-Hoffmann C, Kasche A, Jakob T, Huger M, Plotz S, Feussner I, et al. Lipid mediators from pollen act as chemoattractants and activators of polymorphonuclear granulocytes. J Allergy Clin Immunol. 2002;109(5):831–8. https://doi.org/10.1067/mai.2002.124655.
Traidl-Hoffmann C, Mariani V, Hochrein H, Karg K, Wagner H, Ring J, et al. Pollen-associated phytoprostanes inhibit dendritic cell interleukin-12 production and augment T helper type 2 cell polarization. J Exp Med. 2005;201(4):627–36. https://doi.org/10.1084/jem.20041065.
Gilles S, Jacoby D, Blume C, Mueller MJ, Jakob T, Behrendt H, et al. Pollen-derived low-molecular weight factors inhibit 6-sulfo LacNAc+ dendritic cells' capacity to induce T-helper type 1 responses. Clin Exp Allergy. 2010;40(2):269–78. https://doi.org/10.1111/j.1365-2222.2009.03369.x.
Oeder S, Alessandrini F, Wirz OF, Braun A, Wimmer M, Frank U, et al. Pollen-derived nonallergenic substances enhance Th2-induced IgE production in B cells. Allergy. 2015;70(11):1450–60. https://doi.org/10.1111/all.12707.
Blume C, Swindle EJ, Gilles S, Traidl-Hoffmann C, Davies DE. Low molecular weight components of pollen alter bronchial epithelial barrier functions. Tissue Barriers. 2015;3(3):e1062316. https://doi.org/10.1080/15476286.2015.1062316.
Mueller GA, Thompson PM, DeRose EF, O'Connell TM, London RE. A metabolomic, geographic, and seasonal analysis of the contribution of pollen-derived adenosine to allergic sensitization. Metabolomics. 2016. https://doi.org/10.1007/s11306-016-1130-6.
Gunawan H, Takai T, Ikeda S, Okumura K, Ogawa H. Protease activity of allergenic pollen of cedar, cypress, juniper, birch and ragweed. Allergol Int. 2008;57(1):83–91. https://doi.org/10.2332/allergolint.O-07-507.
Matsumura Y. Role of allergen source-derived proteases in sensitization via airway epithelial cells. J Allergy (Cairo). 2012;2012:903659. https://doi.org/10.1155/2012/903659.
Reed CE, Kita H. The role of protease activation of inflammation in allergic respiratory diseases. J Allergy Clin Immunol. 2004;114(5):997–1008. https://doi.org/10.1016/j.jaci.2004.07.060.
Runswick S, Mitchell T, Davies P, Robinson C, Garrod DR. Pollen proteolytic enzymes degrade tight junctions. Respirology. 2007;12(6):834–42. https://doi.org/10.1111/j.1440-1843.2007.01175.x.
Vinhas R, Cortes L, Cardoso I, Mendes VM, Manadas B, Todo-Bom A, et al. Pollen proteases compromise the airway epithelial barrier through degradation of transmembrane adhesion proteins and lung bioactive peptides. Allergy. 2011;66(8):1088–98. https://doi.org/10.1111/j.1398-9995.2011.02598.x.
Kheradmand F, Kiss A, Xu J, Lee SH, Kolattukudy PE, Corry DB. A protease-activated pathway underlying Th cell type 2 activation and allergic lung disease. J Immunol. 2002;169(10):5904–11. https://doi.org/10.4049/jimmunol.169.10.5904.
Barnes CS. Impact of climate change on pollen and respiratory disease. Curr Allergy Asthma Rep. 2018;18(11):59. https://doi.org/10.1007/s11882-018-0813-7.
Darbah JN, Kubiske ME, Nelson N, Oksanen E, Vaapavuori E, Karnosky DF. Impacts of elevated atmospheric CO2 and O3 on paper birch (Betula papyrifera): reproductive fitness. ScientificWorldJournal. 2007;7(Suppl 1):240–6. https://doi.org/10.1100/tsw.2007.42.
Sedghy F, Sankian M, Moghadam M, Ghasemi Z, Mahmoudi M, Varasteh AR. Impact of traffic-related air pollution on the expression of Platanus orientalis pollen allergens. Int J Biometeorol. 2017;61(1):1–9. https://doi.org/10.1007/s00484-016-1186-z.
Eckl-Dorna J, Klein B, Reichenauer TG, Niederberger V, Valenta R. Exposure of rye (Secale cereale) cultivars to elevated ozone levels increases the allergen content in pollen. J Allergy Clin Immunol. 2010;126(6):1315–7. https://doi.org/10.1016/j.jaci.2010.06.012.
Kanter U, Heller W, Durner J, Winkler JB, Engel M, Behrendt H, et al. Molecular and immunological characterization of ragweed (Ambrosia artemisiifolia L.) pollen after exposure of the plants to elevated ozone over a whole growing season. PLoS ONE. 2013;8(4):e61518. https://doi.org/10.1371/journal.pone.0061518.
Beck I, Jochner S, Gilles S, McIntyre M, Buters JT, Schmidt-Weber C, et al. High environmental ozone levels lead to enhanced allergenicity of birch pollen. PLoS ONE. 2013;8(11):e80147. https://doi.org/10.1371/journal.pone.0080147.
Behrendt H, Becker WM. Localization, release and bioavailability of pollen allergens: the influence of environmental factors. Curr Opin Immunol. 2001;13(6):709–15. https://doi.org/10.1016/s0952-7915(01)00283-7.
Behrendt H, Kasche A, von Ebner Eschenbach C, Risse U, Huss-Marp J, Ring J. Secretion of proinflammatory eicosanoid-like substances precedes allergen release from pollen grains in the initiation of allergic sensitization. Int Arch Allergy Immunol. 2001;124(1–3):121–5. https://doi.org/10.1159/000053688.
Zasloff M. Pollen has a microbiome: implications for plant reproduction, insect pollination and human allergies. Environ Microbiol. 2017;19(1):1–2. https://doi.org/10.1111/1462-2920.13661.
Spiewak R, Skorska C, Prazmo Z, Dutkiewicz J. Bacterial endotoxin associated with pollen as a potential factor aggravating pollinosis. Ann Agric Environ Med. 1996;3(1):57–9.
Zhu Z, Oh SY, Zheng T, Kim YK. Immunomodulating effects of endotoxin in mouse models of allergic asthma. Clin Exp Allergy. 2010;40(4):536–46. https://doi.org/10.1111/j.1365-2222.2010.03477.x.
Hosoki K, Boldogh I, Aguilera-Aguirre L, Sun Q, Itazawa T, Hazra T, et al. Myeloid differentiation protein 2 facilitates pollen- and cat dander-induced innate and allergic airway inflammation. J Allergy Clin Immunol. 2016;137(5):1506–13.e2. https://doi.org/10.1016/j.jaci.2015.09.036.
Głobińska A, Boonpiyathad T, Satitsuksanoa P, Kleuskens M, van de Veen W, Sokolowska M, et al. Mechanisms of allergen-specific immunotherapy: Diverse mechanisms of immune tolerance to allergens. Ann Allergy Asthma Immunol. 2018;121(3):306–12. https://doi.org/10.1016/j.anai.2018.06.026.
Domogalla MP, Rostan PV, Raker VK, Steinbrink K. Tolerance through education: how tolerogenic dendritic cells shape immunity. Front Immunol. 2017;8:1764. https://doi.org/10.3389/fimmu.2017.01764.
Durham SR, Penagos M. Sublingual or subcutaneous immunotherapy for allergic rhinitis? J Allergy Clin Immunol. 2016;137(2):339–49.e10. https://doi.org/10.1016/j.jaci.2015.12.1298.
Mahler V, Esch RE, Kleine-Tebbe J, Lavery WJ, Plunkett G, Vieths S, et al. Understanding differences in allergen immunotherapy products and practices in North America and Europe. J Allergy Clin Immunol. 2019;143(3):813–28. https://doi.org/10.1016/j.jaci.2019.01.024.
Ghimire TR. The mechanisms of action of vaccines containing aluminum adjuvants: an in vitro vs in vivo paradigm. Springerplus. 2015;4:181. https://doi.org/10.1186/s40064-015-0972-0.
Grönlund H, Gafvelin G. Recombinant Bet v 1 vaccine for treatment of allergy to birch pollen. Hum Vaccin. 2010;6(12):970–7. https://doi.org/10.4161/hv.6.12.13348.
Wang W, Yin J. Is it worthy to take full-course immunotherapy for allergic rhinitis? About efficacy biomarker of allergen immunotherapy. Scand J Immunol. 2020;91(1):e12817. https://doi.org/10.1111/sji.12817.
Sindher SB, Long A, Acharya S, Sampath V, Nadeau KC. The use of biomarkers to predict aero-allergen and food immunotherapy responses. Clin Rev Allergy Immunol. 2018;55(2):190–204. https://doi.org/10.1007/s12016-018-8678-z.
Sohn MH. Efficacy and safety of subcutaneous allergen immunotherapy for allergic rhinitis. Allergy Asthma Immunol Res. 2018;10(1):1–3. https://doi.org/10.4168/aair.2018.10.1.1.
Acknowledgements
The authors thank Prof. Dr. Nicola Hüsing (Department of Chemistry and Physics of Materials, University of Salzburg) for providing the scanning electron microscope images of Timothy grass, birch and short ragweed pollen used for the creation of the figures of this manuscript.
Funding
The work of the authors has been supported by the Austrian Science Funds (Projects P32189 and P27589), by the University of Salzburg priority program “Allergy-Cancer-BioNano Research Centre”, by the doctoral program “Immunity in Cancer and Allergy—ICA” funded by the Austrian Science Fund (FWF W1213) and by the Doctoral School Program “Biomolecules” of the University of Salzburg.
Author information
Authors and Affiliations
Contributions
LA, LP and AB created the figures and tables. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
FF reports personal fees from HAL Allergy, from the Swiss Institute of Allergy and Asthma Research (SIAF), from AllergenOnline, all outside the submitted work. All other authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Pointner, L., Bethanis, A., Thaler, M. et al. Initiating pollen sensitization – complex source, complex mechanisms. Clin Transl Allergy 10, 36 (2020). https://doi.org/10.1186/s13601-020-00341-y
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13601-020-00341-y