Abstract
One of the ways in which modern radiology is manifesting itself in higher education and research is through the increasing importance of scientific mobility. This article seeks to provide an overview and a prospective of radiology fellows in their last year of training about the current trends and policy tools for promoting mobility among young radiologists, especially inside the European Union. Nowadays, the need to promote international cooperation is even greater to ensure that the best evidence-based medical practices become a common background of a next cross-border generation of radiologists. Organisations such as the European Society of Radiology (ESR) and the Radiological Society of North America (RSNA) are called upon to play as guarantors of the training of young radiologists building know-how and world-class excellence. Today, it is not just being certified radiologist that matters, the place where the training was done plays an important role in enhancing chances when applying for a high-level job or fellowship. The article argues that the mobility of radiology trainees is an indispensable prerequisite to face new challenges, including the application of artificial intelligence to medical imaging, which will require a large multicentre collaboration.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Key Points
• ESR and RSNA have a central role for young radiologists supporting international training opportunities, enhancing scientific mobility and promoting cooperation between centres of different countries.
• Evidence-based medicine requires multicentre collaboration to identify a best practice, standardise it and share it. Mobility helps to uniform techniques and terminology in different countries, which are crucial to develop widely shared guidelines.
• Investing in trainees’ mobility means promoting collaboration among centres/systems that cannot remain isolated, which is a risk in the current era of nationalisms.
• The cultural-knowledge and the networks developed during mobility can be used by the trainees to advance in their career.
Introduction
In this paper, I present my point of view about the role of trainee’s mobility in their curriculum, analysing firstly the advantages and, in the last part of the paper, the disadvantages of this opportunity. The rationale of promoting international collaboration is to ensure that the best evidence-based medical practices become a common background of a next cross-border generation of radiologists. Particularly, new challenges such as application of artificial intelligence (AI) in medical imaging will require large international cooperation to standardise the techniques and to uniform the methods of research. Organisations such as the European Society of Radiology (ESR) and the Radiological Society of North America (RSNA) already offer international training opportunities and support mobility to advance radiology education. The hope is that these efforts will be pursued over time and even increased, together with governments and scientific institutions, to play as the guarantor of an international training for residents and young radiologists. While other educational hubs and interesting dynamics are emerging in several countries, a worldwide analysis of scientific mobility is beyond the aims of this article which, since it is inspired by my personal experience, mainly focuses on the European Union (EU) and the USA contexts.
The present and the future of scientific mobility for young radiologists
Both in the EU and in the USA, international scientific mobility significantly increased over the past decade, including for medical students, academic faculty members, and medical degreed trainees [1]. While US universities are leading the international higher education market and enrolling unprecedented numbers of foreign students, the EU has consistently emphasised its intention to become one of the most competitive “knowledge economy” in the world [2]. Recently, the EU issued recommendations for promoting mobility in a broader view of the European area based on greater employment opportunities, lower poverty levels and on the free movement of people and ideas [3]. Accordingly, the EU adopted in early 2014 a guideline that facilitated the mobility of researchers across various European academic centres [2].
Although Europe has a current surplus of talent (the unemployed youth), it will face widespread expertise shortages, as the European Commission estimates that a net increase of even one million researchers is needed over this decade [4, 5]. Therefore, a paradox seems to play out: while the EU has many talented and skilled researchers, they account for a significantly lower share of the labour force than is the case in the USA [6].
Currently, the UK and Netherlands, followed by Sweden, Belgium, and Austria, are the European countries with the largest surpluses of scientific researchers, while almost all other countries demonstrate a deficit, with the largest for Italy, followed by Germany, Spain, and France, which have a lot of nationals who moved elsewhere thanks to the European grants [5, 6]. The main reasons for losing highly skilled researchers is the lack of research funds and better economic conditions or career opportunities abroad [6]. The paucity of available grants affects the radiology research too: both in the EU and USA, much of the research and the education in radiology continues to be done with voluntary time and materials [7]. Moreover, many hospital departments operate with a budget deficit that is being addressed by increasing the clinical productivity of their medical staff, which erodes the already limited time for research and educational purposes [7].
Therefore, the traditional European model of the university and research hospitals, with its overly disciplinary fragmentation, is being challenged. Today, given advances in communication technology, a core group of networked researchers may go a long way towards helping a country with modest scientific resources achieve the analogue world-class excellence of the richest countries, in a broader win-win situation [8]. However, these new avenues will require strong leadership, revised governance structures and enhanced institutional autonomy. International organisations such as the ESR and RSNA can play an important role to involve local centres into global science projects. With the help of these societies, a radiology trainee can easily take advantage of the international training opportunities that are currently offered by public or private grants, enhancing the scientific mobility and the cooperation among research centres of different countries.
This kind of scientific mobility could be co-funded by departments through the clinical income trainees generate by spending a percentage of their time practicing clinical radiology. Possibly, such mobility programs would result in a critical mass of radiology education investigators that could substantially impact the support allocated for such research within the field of radiology [7].
Mobility shows the need for standardisation of radiological education
Referring to my personal education experience, mobility took a central role in my training. After 2 years training in several research hospital in Milan (Italy), I visited Ghent (Belgium) for a fellowship co-founded by the EU’s grant “Erasmus + Programme” [9] as a first step of an educational journey which led me to Bethesda (MD, USA) for a research fellow and to Chicago (IL, USA), thanks to the RSNA’s project “Introduction to Research for International Young Academics” (IRIYA) [10]. Finally, the European School of Radiology (ESOR) [11] supported me for a scholarship in London (UK).
During this experience, I realised how guidelines and their application vary from one country to another (e.g. breast cancer screening programs, use of standardised report systems, indications to imaging examinations, performance of image-guided interventional procedures) [12,13,14,15,16] in the daily clinical practice. It was somehow surprising that there can be so much variation when these are supposedly based on the principles of evidence-based medicine.
In health care sciences, solutions to complex problems require collaboration and common approaches to identify a best practice, standardise it, and then share it to improve the care for patients [17].
The first step to reach a consistent radiological practice is to standardise the techniques [13, 18]. For instance, the size of a mass in organs can be compared best if the comparison MRI/CT/US scans are performed with precisely the same imaging protocol [17]. Similarly, an appropriate segmentation of an index lesion in the training process of an AI system requires the most uniform images possible [19,20,21].
The second step is to reduce variations in terminology (namely, in reports). A common and international imaging lexicon, for instance through structured reports, can provide a uniform method to share the information, which is important for an improved communication between radiologists of different centres, between radiologists and clinicians and, at last but not least, between radiologists and patients too [13, 18, 22, 23].
The American College of Radiology (ACR) proposed the Reporting and Data Systems (RADS) to provide a standardised framework for reporting on imaging findings and assessing the probability of disease [24]. However, with few exceptions (e.g. the PI-RADS [25], for prostate cancer, and the O-RADS, for ovarian and adnexal cancer [26], which were established in collaboration with European societies), these projects were developed by US scientific societies only.
Indeed, although the EU should be proud of its research talent, researchers are poorly equipped to translate their potentials into international guidelines to reach standardised radiological practice [6, 27]. Accordingly, there is a further need for European cooperation for gathering and distillation of information. Then, the radiology community will identify and prioritise research project and, through shared approaches and standardised methods, will collaborate to ensure that a broad range of topics can be addressed across the EU and USA [28].
Communication and scientific mobility as the assets in the new era of patient-centred radiology
A cultural change is required to the new generation of radiologists who will fully adopt the patients, rather than the images, as the central reason for their job. Recently, radiologists have been characterised as “doctor-to-doctor” consultants who are distanced from patients [29]. Young radiologists must change the perception that they are merely consultants and become more active participants in patient care by embracing greater patient interaction, as their predecessors probably did before technology took over the human aspect of their job. Indeed, the more our technological capabilities evolve, the harder it becomes to deliver personalised care, especially if we, as doctors, separate ourselves from the patients who make our work meaningful.
The shift away from direct patient-provider engagement has diminished the perception of the central role radiology plays in patient care (with implications for funding and research), as shown in a survey among 694 RSNA members [30]: 89% of participants agreed that promoting awareness of radiology’s role in patients’ overall healthcare is important for how they practice. However, 73% reported that time or workload frequently prevented them from communicating directly with patients and only 31% noted their practices regularly promote awareness of radiology’s role in patients’ overall healthcare.
Beyond the implications for student interest in radiology and staff morale, a lack of communication is a serious loss for patients. An analysis of the ESR [31] showed a robust association between direct radiologist-to-patient interaction and a higher level of clinical effectiveness that feeds into a comprehensive diagnosis.
A patient-centred model in which radiologists are reintegrated into direct patient care and imaging processes are reorganised around patients’ needs is now demanded [29]. Scientific societies must provide international recommendations to improve communication as a fundamental aspect of the job of radiologists, who should openly interact with patients and primary care physicians to provide a comprehensive diagnostic and advisory service. Trust is the foundation of the doctor–patient relationship, and the patients do not necessarily just trust a radiological report based only on the results of an AI’s algorithm [32].
This patient-centred approach may need a greater personal effort by young radiologists, who have not (probably) received the appropriate training in this regard, but the potential benefits include higher quality of patient care and safety.
This is a topical need, in an era in which AI will change the professional status of radiologists, and it will make crucial the collaboration among researchers worldwide. Collaboration between different centres will be critical as machine learning algorithms require a huge amount of data (namely radiological images) to be trained [33, 34], and the lack of well-annotated big datasets for training these algorithms is a key obstacle to a large introduction of AI-systems in radiology [35,36,37,38].
Alongside the irreversible increase in imaging data and the possibility to identify findings and patterns detectable and not detectable by humans [39], radiology is now moving from a subjective perceptual skill (currently limited by subjectivity) to a more objective science supported by sophisticated AI systems [40, 41]. Therefore, AI has the potential to replace at least part of the routine detection, characterisation and quantification tasks currently performed by radiologists [16, 36, 42, 43], and the new generation of radiologists can use this time to communicate with patients, to participate in multidisciplinary teams, to design multicentre studies, to develop international guidelines and finally to reach high standard of radiology practice without worrying about the high number of examinations to be reported [21, 44].
Radiology does not treat images, but patients and its teaching has long been recognised as more than a process that imparts formal technical knowledges: the radiologist’s duties also include communication of diagnosis, consideration of patient’s values and preferences, medical judgment, quality assurance, teaching, policy-making, interventional procedures and many more tasks that, so far, cannot be performed by computer programs alone [21].
In this scenario, mobility is still important for both personal development and employability of the future radiologists, because it fosters respect for diversity and a capacity to deal with other cultures, which is basic to a high-quality doctor–patient relationship, it encourages communication through linguistic pluralism and it increases cooperation between higher education institutions.
ESR and RSNA have already sought to improve access to a global collaboration and education through meritocratic means and widening participation strategies, supporting scientific mobility and promoting universally recognised certification systems such as European Diploma in Radiology (EDiR) [45]. Indeed, as trainees’ mobility is becoming increasingly important, the EDiR can certify a standard of radiological knowledge deemed appropriate for independent practice in general radiology.
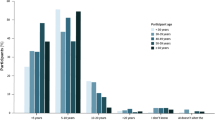
From a survey conducted by ESR in 2018 among 1045 radiologists (78% of them being trainees) [46], a conspicuous lack of trainees’ confidence in their own professional skills emerged [47]. This uncertainty can be overcome by using international training curriculum, which offers the guarantee of standardisation in acquired knowledge [46]. Although EDiR does not replace any national board certificate, a successful examination EDiR is an added value to the trainees’ curriculum vitae. In literature, it was suggested that the trainees’ curriculum must change with the health care system and international societal expectations [7, 48]: EDiR meets these needs and it represents a significant step towards transnational harmonisation of radiological standards throughout Europe.
The role of scientific mobility in the current social context and market labour
Policies supporting scientific mobility may have significant implications for the state and future of education, especially considering the current widespread rise of nationalist sentiments and the probable implications of the recent UK referendum for leaving EU [49].
In this uncertain and fast-changing context [50], AI does not necessarily represent a positive innovation: the future digitisation and automation of work threaten to make parts of workforce obsolete in the current labour market that is already facing a situation with high unemployment rate, especially among the youth (7,9% of the labour force in EU28 in 2018, 16% for the under 25) [51]. At the same time, several vacancies in scientific and medical areas, including 800,000 researchers, remain unfulfilled [6].
While the governments play as the guarantor for the rights of every citizen to have a job, in the narrower field of radiology, the guarantor role of the young radiologists should be taken up by cosmopolite academic institutions, research hospitals and societies such as the ECR or RSNA, which already have a critical role in the education of future radiologists. In the current era of globalised medicine, investing in trainees’ mobility means to promote collaboration among different health care systems that should not remain isolated in national borders.
In 2015, a study [3] showed that programmes for mobility supported by the EU promote direct perception of a European identity of end-users, indicating the existence of supranational identity and awareness opportunities within the EU. Scientific mobility prepares participants for performing in a global society and, at the same time, society may also benefit from workers with greater international competences [1,2,3, 6].
A full consideration of the potential policy implications of scientific mobility should require a careful consideration of the social context, and it is beyond the aim of this article. However, the internationalisation of the trainees’ curriculum though scientific mobility may serve as an opportunity even for the least developed higher education and research systems, and it can improve the personal ability to integrate both culturally and organisationally with colleagues with different background and nationality [8].
The hidden face of the scientific mobility
Although scientific mobility may represent an investment for wider educational and better labour market perspectives, this might not necessarily always the case. Even when a stay abroad is transferred and internationally recognised, such as with EDiR, employers and colleagues may not always be aware of the value of foreign degrees and experiences, thus treating mobile radiologists as newcomers [52]. Furthermore, by going abroad, the trainees may weaken their local networks which can influence their access to new positions. Finally, employers may favour individuals who are familiar with how things are done over people who worked for some time abroad [1]. This is the hidden face of scientific mobility, and perhaps it has become more actual in the current era of divisive nationalisms [2].
In conclusion, although there are some disadvantages in dealing with scientific mobility, the European-level competitiveness is positively on the rise, and a positive impact on the quality of research can be expected on the basis of the advantages of trainees’ mobility, i.e. the above-average performance of a migrant scientist, as evidenced in the USA [6].
This is the way for young radiologists like me to build our future.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Abbreviations
- ACR:
-
American College of Radiology
- AI:
-
Artificial intelligence
- EDiR:
-
European Diploma in Radiology
- ESR:
-
European Society of Radiology
- EU:
-
European Union
- MD:
-
Maryland
- RADS:
-
Reporting and Data Systems
- RSNA:
-
Radiological Society of North America
References
Bilecen B, Van Mol C (2017) Introduction: international academic mobility and inequalities. J Ethn Migr Stud 43:1241–1255
Kim T (2017) Academic mobility, transnational identity capital, and stratification under conditions of academic capitalism. High Educ 1:1–17
Jacobone V, Moro G (2015) Evaluating the impact of the Erasmus programme: skills and European identity. Assessment & Evaluation in Higher Education 40:309–328
European Commission (2019) Science, Research and Innovation Performance of the EU 2018.
European Commission (2013) DG Research and Innovation. Researchers’ Report 2013. Final Report,
Van der Wende M (2015) International academic mobility: towards a concentration of the minds in. Eur Rev 23:S70–S88
Collins J (2006) Medical education research: challenges and opportunities. Radiology 240:639–647
Jacob M, Meek VL (2013) Scientific mobility and international research networks: trends and policy tools for promoting research excellence and capacity building. Stud High Educ 38:331–344
European Commission (2019) Erasmus +. Available via http://ec.europa.eu/programmes/erasmus-plus/node_en. Accessed 19 Febr 2019. 2019
Radiological Society of North America (RSNA) (2019) Introduction to Research for International Young Academics. Available via https://www.rsna.org/en/education/workshops/introduction-research-international-young-academics
European School of Radiology (ESOR) (2019) ESOR Visiting Scholarship Programme Europe. Available via http://www.esor.org/cms/website.php?id=/en/programmes/visiting_scholarship_programmes/scholarships_in_europe.htm. Accessed 19 Feb 2019.
Shapiro S, Coleman EA, Broeders M et al (1998) Breast cancer screening programmes in 22 countries: current policies, administration and guidelines. International Breast Cancer Screening Network (IBSN) and the European Network of Pilot Projects for Breast Cancer Screening. Int J Epidemiol 27:735–742
Larson DB, Towbin AJ, Pryor RM, Donnelly LF (2013) Improving consistency in radiology reporting through the use of department-wide standardized structured reporting. Radiology 267:240–250
Leong S, Keeling AN, Lee MJ (2009) A survey of interventional radiology awareness among final-year medical students in a European country. Cardiovasc Intervent Radiol 32:623–629
Hamoen EHJ, de Rooij M, Witjes JA, Barentsz JO, Rovers MM (2015) Use of the prostate imaging reporting and data system (PI-RADS) for prostate cancer detection with multiparametric magnetic resonance imaging: a diagnostic meta-analysis. Eur Urol 67:1112–1121
Pesapane F, Volonte C, Codari M, Sardanelli F (2018) Artificial intelligence as a medical device in radiology: ethical and regulatory issues in Europe and the United States. Insights Imaging. https://doi.org/10.1007/s13244-018-0645-y
Swensen SJ, Johnson CD (2005) Radiologic quality and safety: mapping value into radiology. J Am Coll Radiol 2:992–1000
Schwartz LH, Panicek DM, Berk AR, Li Y, Hricak H (2011) Improving communication of diagnostic radiology findings through structured reporting. Radiology 260:174–181
Pereira S, Pinto A, Alves V, Silva CA (2016) Brain tumor segmentation using convolutional neural networks in MRI Images. IEEE Trans Med Imaging 35:1240–1251
Moeskops P, Viergever MA, Mendrik AM, de Vries LS, Benders MJ, Isgum I (2016) Automatic segmentation of MR brain images with a convolutional neural network. IEEE Trans Med Imaging 35:1252–1261
Pesapane F, Codari M, Sardanelli F (2018) Artificial intelligence in medical imaging: threat or opportunity? Radiologists again at the forefront of innovation in medicine. Eur Radiol Exp 2:35
Langlotz CP, Caldwell SA (2002) The completeness of existing lexicons for representing radiology report information. J Digit Imaging 15(Suppl 1):201–205
Reiner BI, Knight N, Siegel EL (2007) Radiology reporting, past, present, and future: the radiologist's perspective. J Am Coll Radiol 4:313–319
American College of Radiology (ACR) (2019) ACR Reporting and Data Systems (RADS) available via https://www.acr.org/Clinical-Resources/Reporting-and-Data-Systems
American College of Radiology (ACR) (2019) Prostate Imaging Reporting and Data System (PI-RADS). Available via https://www.acr.org/Clinical-Resources/Reporting-and-Data-Systems/PI-RADS
American College of Radiology (ACR) (2019) Ovarian-adnexal reporting & data system (O-RADS). Available via https://www.acr.org/Clinical-Resources/Reporting-and-Data-Systems/O-Rads
Kahn CE Jr, Heilbrun ME, Applegate KE (2013) From guidelines to practice: how reporting templates promote the use of radiology practice guidelines. Journal of the American College of Radiology 10:268–273
Sardanelli F, Hunink MG, Gilbert FJ, Di Leo G, Krestin GP (2010) Evidence-based radiology: why and how? Eur Radiol 20:1–15
Itri JN (2015) Patient-centered Radiology. Radiographics 35:1835–1846
Kemp JL, Mahoney MC, Mathews VP, Wintermark M, Yee J, Brown SD (2017) Patient-centered radiology: where are we, where do we want to be, and how do we get there? Radiology 285:601–608
European Society of Radiology (2009) The future role of radiology in healthcare. Insights Imaging 1:2–11
Mohan C SM (2018) Artificial intelligence in radiology—are we treating the image or the patient? Indian J Radiol Imaging 28:137–139
Thrall JH, Li X, Li Q et al (2018) Artificial intelligence and machine learning in radiology: opportunities, challenges, pitfalls, and criteria for success. Journal of the American College of Radiology 15:504–508
Yi PH, Hui FK, Ting DSW (2018) Artificial intelligence and radiology: collaboration is key. Journal of the American College of Radiology. https://doi.org/10.1016/j.jacr.2017.12.037
Miller DD, Brown EW (2018) Artificial intelligence in medical practice: the question to the answer? Am J Med 131:129–133
Krittanawong C (2018) The rise of artificial intelligence and the uncertain future for physicians. Eur J Intern Med 48:e13–e14
Lee JG, Jun S, Cho YW et al (2017) Deep learning in medical imaging: general overview. Korean J Radiol 18:570–584
Kruskal JB, Berkowitz S, Geis JR, Kim W, Nagy P, Dreyer K (2017) Big data and machine learning-strategies for driving this bus: a summary of the 2016 Intersociety Summer Conference. Journal of the American College of Radiology 14:811–817
Gillies RJ, Kinahan PE, Hricak H (2016) Radiomics: images are more than pictures, they are data. Radiology 278:563–577
Jha S, Topol EJ (2016) Adapting to artificial intelligence: radiologists and pathologists as information specialists. JAMA 316:2353–2354
Sardanelli F, Di Leo G (2009) Planning, Performing, and Writing a Radiologic Study. In: Sardanelli F, Di Leo G (eds) Biostatistics for Radiologists. Springer-Verlag, Milan, pp XXII, 231. https://doi.org/10.1007/978-88-470-1133-5.
Lakhani P, Prater AB, Hutson RK et al (2018) Machine learning in radiology: applications beyond image interpretation. Journal of the American College of Radiology 15:350–359
King BF Jr (2017) Guest editorial: discovery and artificial intelligence. AJR Am J Roentgenol 209:1189–1190
Recht M, Bryan RN (2017) Artificial intelligence: threat or boon to radiologists? Journal of the American College of Radiology 14:1476–1480
European Board of Radiology (EBR) (2018) The European Diploma in Radiology (EDiR): investing in the future of the new generations of radiologists. Insights Imaging 9:905–909
European Society of Radiology (ESR) (2018) Radiology trainees forum survey report on workplace satisfaction, ESR education, mobility and stress level. Insights Imaging 9:755–759
Nyhsen CM, Lawson C, Higginson J (2011) Radiology teaching for junior doctors: their expectations, preferences and suggestions for improvement. Insights Imaging 2:261–266
Chew FS (1990) Standardization of the curriculum for resident education in diagnostic radiology. Invest Radiol 25:1258–1260
Hanson K, O'Dwyer E (2018) Patriotism and nationalism, left and right: a Q-methodology study of American National Identity. Political Psychol. https://doi.org/10.1111/pops.12561
Eger MA, Valdez S (2018) From radical right to neo-nationalist. Eur Political Sci 1:1–21
Eurostat (2019) Unemployment rates, seasonally adjusted, December 2018,
Weiß A (2016) Understanding physicians’ professional knowledge and practice in research on skilled migration. Ethn Health 21:397–409
Acknowledgements
I am grateful to the Director of my Postgraduation School in Radiodiagnostic Prof. Francesco Sardanelli (Università degli Studi di Milano, IRCCS Policlinico San Donato, Milan, Italy), who contributed towards this article with valuable comments, for his capable support to the scientific mobility during my radiology training.
I am thankful to Prof. Gianpaolo Carrafiello (Università degli Studi di Milano, ASST Santi Paolo e Carlo, Milan, Italy) and to Dr. Enrico Cassano (IEO European Institute of Oncology, Milan, Italy) for their encouragement to develop an international collaboration among worldwide research institutes.
I express my deep gratitude to Prof. Geert Villeirs (Ghent University Hospital, Ghent, Belgium), Dr. Bradford J. Wood (Clinical Center, National Institutes of Health, Bethesda, MD, USA), Prof. Paul Sidhu (King's College Hospital, London, UK) and Prof. Dow-Mu Koh (The Institute of Cancer Research, Royal Marsden Hospital, Sutton, UK), the mentors during my mobility periods, for welcoming me and including me in the activity of their radiology departments, for their inspirations and useful critiques of my clinical and research work.
Funding
The author states that this work has not received any funding.
Author information
Authors and Affiliations
Contributions
FP is the only author of this article. He designed the work, acquired, analysed and interpreted the data and drafted the manuscript. Therefore, he approved the submitted version and agreed both to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work are appropriately investigated, resolved, and the resolution documented in the literature.
Authors’ information
Filippo Pesapane is a senior resident radiologist in his fifth year of the Postgraduation School in Radiodiagnostic of the University of Milan in Italy.
He graduated in medicine with first-class honours in 2013 and worked in Italy at a number of Milan University Hospitals (ASST Santi Paolo e Carlo, IRCCS Policlinico San Donato, IEO European Institute of Oncology), in Belgium at University Hospital of Gent, in the USA at NIH National Institute of Health in Bethesda (MD) and in the UK at King's College Hospital in London and at Royal Marsden Hospital in Sutton.
In 2019, he got the first place as “Radiology Rising Star” in EuroMinnies awards.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Institutional Review Board approval or Informed Consent was not required because the research does not involve human populations or animals, but it is a narrative and educational review about training in radiology.
Consent for publication
The author of the manuscript has read and agreed to its content and are accountable for all aspects of the accuracy and integrity of the manuscript in accordance with ICMJE criteria.
That the article is original, has not already been published in a journal, and is not currently under consideration by another journal.
Other Consent of publications was not required because the research does not involve human populations or animals.
Competing interests
The author of this manuscript declares that he has no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Pesapane, F. How scientific mobility can help current and future radiology research: a radiology trainee’s perspective. Insights Imaging 10, 85 (2019). https://doi.org/10.1186/s13244-019-0773-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13244-019-0773-z