Abstract
Background
To evaluate the short-term efficacy of intravitreal injections of aflibercept (IVA) to treat retinal angiomatous proliferation (RAP) and identify factors related to functional outcomes.
Methods
This retrospective case series consisted of 19 eyes in 19 patients with RAP. All 19 eyes received 3 monthly consecutive IVA. The primary outcome measures were best-corrected visual acuity (BCVA) and central retinal thickness (CRT) after the last IVA.
Results
Of the 19 treated eyes, 8 (42%) were pre-treated with 1 dose of bevacizumab one month prior to the initiation of treatment with aflibercept. BCVA was significantly improved and CRT was significantly reduced after 3 consecutive IVAs (P = 0.014 and P = 0.0002, respectively). Stabilization or improvement in BCVA was observed in 17 eyes (90%) treated with IVA. Eyes with baseline fibrovascular pigment epithelial detachment (PED) showed no significant gain in BCVA, and fibrovascular PED was negatively correlated with final BCVA (Spearman’s correlation coefficient = − 0.481, P = 0.037). The mean follow-up was 3.5 ± 0.5 months.
Conclusions
In this short-term study, three consecutive IVAs showed efficacy for improving vision and reducing retinal edema in RAP patients. Eyes with fibrovascular PED showed poorer responses, and the presence of fibrovascular PED at baseline was negatively correlated with visual outcomes.
Similar content being viewed by others
Background
Retinal angiomatous proliferation (RAP) is recognized as a variant of neovascular age-related macular degeneration (nAMD) that displays a tendency to develop into a bilateral disease and has been associated with a guarded visual prognosis [1,2,3]. Cases of RAP comprise 15.1% of newly diagnosed cases of nAMD in Caucasians [4] and was identified in 4.5–7.5% of all Japanese nAMD patients [5, 6].
Before the introduction of anti-vascular endothelial growth factor (anti-VEGF) agents, treatments for RAP included conventional laser photocoagulation [7], surgical ablation [8, 9], transpupillary thermotherapy [10], photodynamic therapy (PDT) with verteporfin (Visudyne; Novartis Pharma AG, Basel, Switzerland) [11, 12], or combined intravitreal injections of triamcinolone acetonide with PDT [13]. These have each been studied and found to provide a limited response or have a high complication rate.
Intravitreal injections of anti-VEGF agents, such as bevacizumab (Avastin®, Genentech, South San Francisco, California, USA) and ranibizumab (Lucentis®; Genentech, South San Francisco, California, USA), have shown promising results for the treatment of RAP [14,15,16]. Intravitreal injections of aflibercept (IVA) (Eylea®; Bayer HealthCare, Berlin, Germany) have also been demonstrated to be effective for treating Type 1 and Type 2 nAMD [17]. However, to our knowledge, only a few studies have focused on responses to aflibercept in RAP patients [18,19,20]. The aim of this study was to determine the short-term efficacy of IVA as a treatment for RAP.
Materials and methods
This was a retrospective case review of 19 eyes in 19 Taiwanese patients who presented with RAP between November 2013 and February 2016 in Chung-Gang Memorial Hospital, Taoyuan, Taiwan. The study was conducted according to the principles of the Declaration of Helsinki. The ethics committee of Chung-Gang Memorial Hospital approved this study. All patients were followed in a single center for at least 1 month after 3 monthly IVAs.
The diagnostic criteria for RAP lesions were based on clinical and angiographic findings [21], including 1) age of 55 years old or older; 2) nAMD with characteristics of intraretinal lesions when observed on optical coherence tomography (OCT), including associated intraretinal edema with or without sub-retinal pigment epithelium (RPE) fluid; 3) focal hyperfluourescent lesions and late leakage on fluorescein angiography (FA) at the site of an intraretinal lesion; and 4) a corresponding “hot spot” on indocyanine green angiography (ICGA). Other associated features more often observed in RAP [22, 23] were also analysed, including intraretinal hemorrhage (IRH) on fundus photography and near-infrared (IR) reflectance imaging, late leakage from the “hot spot” on ICGA late frames, identification of associated retinal feeding arterioles and draining venules on FA/ICGA, intraretinal cysts (IRC) and RPE interruption (PEI) along the PED on OCT, and the presence of reticular pseudodrusen (RPD) on OCT and IR imaging. All the clinical images were reviewed by a junior and a senior Ophthalmologist (HC and CL).
Patients with a defined RAP lesion who were treated with 3 consecutive monthly IVAs were included in the study. Patients with the following conditions were excluded: 1) a concurrent macular disease, such as diabetic maculopathy, retinal vascular occlusion, or macular telangiectasia; 2) any other condition that might affect a visual prognosis, such as uncontrolled glaucoma, degenerative myopia, trauma, uveitis, or previous vitreoretinal surgery; and 3) prior treatment with photodynamic therapy.
While the National Health Insurance Administration in Taiwan (NHI) covers the expense for 3 IVAs in nAMD patients, it takes a few weeks to obtain approval for these treatments. Therefore, to prevent further visual decline in patients, 8 eyes (42%, designated as the pre-treatment group) received 1 dose of intravitreal injection of bevacizumab (IVB) at the time of the RAP diagnosis and before IVA use was approved. This group of patients was required to pay for the cost of the IVB. One month later, after the NHI had approved the IVA application, each of these patients received three consecutive monthly IVAs. The remainder of the eyes (11 eyes, 58%, designated as the naïve group) were treatment-naïve and received three consecutive monthly IVAs after approval from the NHI.
The treatments were injected into the vitreous cavity 3.5 or 4.0 mm posterior to the corneal limbus using a 30-gauge needle after topical anaesthesia was applied, depending on the status of lens. The injection doses were 2 mg /0.05 ml for IVA and 1.25 mg/0.05 ml for IVB.
In every case, the baseline condition (at month 0) was examined before the first IVA treatment was performed. In the pre-treatment group, the baseline condition was examined 1 month after the IVB injection and before the first IVA treatment. The post-treatment condition of the eye was examined 1 month after the final injection of IVA (at month 3). All patients underwent a standardised examination including slit-lamp biomicroscopy, color and red-free fundus photography (TRC-50EX; Topcon, or Nonmyd α-DIII; KOWA, Tokyo, Japan), IR reflectance imaging and FA/ICGA (Heidelberg Retina Angiograph HRA2; Heidelberg Engineering, Dossenheim, Germany). OCT examinations were performed using spectral-domain OCT (SD-OCT) in a Spectralis HRA-OCT system (Heidelberg Engineering, Dossenheim, Germany). BCVA was measured using a standard decimal Landolt C visual acuity chart and converted to the logarithm of the minimum angle of resolution (LogMAR) equivalent for analysis. The CRT was defined as the distance from the RPE to the inner limiting membrane of the fovea center and measured using SD-OCT imaging and the software included with the machine.
The primary outcome measures were BCVA and CRT, which were determined using SD-OCT. The secondary outcome measures were the presence/absence of PED and subretinal fluid (SRF) on the SD-OCT after treatment was completed. The data are expressed as the mean ± standard deviation (SD).
Statistical analyses were performed using the Wilcoxon Signed-Rank Test to evaluate changes in BCVA and CRT. Bivariate relationships were examined using Pearson’s correlation analysis. The level of significance was defined as P < 0.05.
Results
A total of 19 eyes in 19 patients (9 men and 10 women) were included (Table 1). All of the patients received 3 monthly IVA treatments. A subgroup of 8 patients (8 eyes, 42%) was pre-treated with 1 dose of IVB at 1 month before the initiation of the 3 monthly IVA treatments. The mean age of the patients was 68.2 ± 8.0 years old (mean ± SD, range, 57–82 years old). At baseline, 5 eyes (26.3%) had no PED, and 14 eyes (73.7%) had PED. 6 eyes (31.6%) had no SRF, and 13 eyes (68.4%) had SRF. All patients were followed up at least until 1 month after the last IVA treatment (Fig. 1).
Intravitreal aflibercept treatment for RAP. Case 3: A 59-year-old female with a stage IIb RAP lesion. a-f Pre-treatment exams. g-l Post-treatment exams performed one month after 3 monthly IVAs. a Red-free fundus photograph showing a circumscribed area of PED with a focal area of retinal hemorrhage at the center. b Early phase ICGA demonstrating a neovascularised lesion in a macula with retino-retinal vessel anastomosis. c Late-phase FA showing dye leaking and pooling in the macula. d Late-phase ICGA revealing a “hot spot” corresponding to a neovascularised macular lesion. e, k The orientation of SD-OCT. f SD-OCT image taken before treatment showing a PED, subretinal fluid accumulation, and an overlying intraretinal lesion corresponding to the “hot spot” in late-phase ICGA. g Resolution of the circumscribed PED and the retinal hemorrhage. h The neovascularised lesion in the macula regressed. i,j Decreased dye leakage was observed in the macula, and the “hot spot” was no longer present. l Resolution of the PED and subretinal fluid. Some RPE bumps were still present
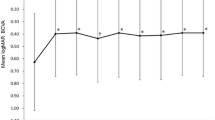
Baseline BCVA was LogMAR 1.23 ± 0.56 (range, 0.30–2.00) and significantly improved to LogMAR 0.87 ± 0.41 (range 0.30–1.70) (P = 0.014) after treatment (Table 2). The mean change in BCVA was LogMAR 0.36 ± 0.56 (range, −0.48-1.70). The BCVA improved by 3 LogMAR lines or more in 9 eyes (47.4%), remained stable in 8 eyes (42.1%), and was worse by 3 lines or more in 2 eyes (10.5%) (Fig. 2).
Graph showing the distribution of mean changes in best-corrected visual acuity (BCVA) from baseline after treatment with aflibercept. In the whole series, BCVA improved in 47.4%, remained stable in 42.1%, and decreased in 10.5% of the eyes. In the naïve subgroup, BCVA improved in 54.5%, remained stable in 36.4%, and decreased in 9.1% of the eyes. In the pre-treatment subgroup, BCVA improved in 37.5%, remained stable in 50.0%, and decreased in 12.5% of the eyes
The baseline CRT mean ± SD was 404.0 ± 131.7 μm (range, 225–699 μm). CRT was significantly lower, at 306.1 ± 112.0 μm (range 193–637 μm) (P = 0.0002), after treatment (Table 2). The mean change in CRT was 97.9 ± 67.3 μm (range, 0–222.0 μm). When the mean change in CRT was compared to the mean baseline CRT (mean CRT change / mean baseline CRT), the mean percentage change in CRT was 23.1 ± 14.6% (range 0%–49.6%).
A subgroup analysis was performed to compare the naïve group and the pre-treatment group (Table 2). In the naïve group, the baseline mean ± SD BCVA was LogMAR 1.32 ± 0.58, and this value significantly improved to LogMAR 0.92 ± 0.47 (P = 0.047). In the same group, the baseline mean ± SD CRT was 436.6 ± 96.6 μm, and this value significantly decreased to 298.6 ± 87.3 μm (P = 0.003). In the pre-treatment group, the baseline mean ± SD BCVA was LogMAR 1.09 ± 0.54, and this value improved to LogMAR 0.78 ± 0.33, but the difference was not significant (P = 0.173). The baseline mean ± SD CRT was 359.1 ± 165.2 μm, and this value significantly decreased to 316.5 ± 145.4 μm (P = 0.018).
In the naïve group, the BCVA improved by 3 lines or more in 6 eyes (54.5%), remained stable in 4 eyes (36.4%), and decreased by 3 lines or more in 1 eye (9.1%) (Fig. 2). In the pre-treatment group, the BCVA improved by 3 lines or more in 3 eyes (37.5%), remained stable in 4 eyes (50.0%), and decreased by 3 lines or more in 1 eye (12.5%).
Overall, 14 eyes had baseline PED, 6 eyes had serous PED, and 8 eyes had fibrovascular PED. After treatment, PED had resolved in 5 eyes (35.7%). In the 6 eyes with baseline serous PED, PED resolved with only some RPE bump remained in 5 eyes (83.3%), and persistent PED was noted in 1 eye (13.7%). Fibrovascular PED persisted after IVA in all 8 of the eyes with baseline fibrovascular PED. No eyes without initial PED developed PED after treatment or during the follow-up period. A further subgroup analysis showed that patients with baseline fibrovascular PED had a poorer response to aflibercept and achieved no significant gain in BCVA (P = 0.446). The presence of fibrovascular PED at baseline was also negatively correlated with BCVA at the end of the follow-up period (Spearman’s correlation coefficient = − 0.481, P = 0.037).
SRF was present at baseline in 13 eyes (68.4%). After treatment with aflibercept, SRF had diminished completely in 12 (92.3%) of the 13 eyes with baseline SRF. No eyes without initial SRF developed SRF after treatment or during the follow-up period.
No ocular complications, including elevated intraocular pressure, ocular infection, drug-related intraocular inflammation, vitreous hemorrhage, or retinal detachment, were noted in any of the patients during the follow-up period. There were also no significant systemic side effects.
Discussion
In this retrospective study, we show that IVA significantly achieved functional and anatomical improvements in RAP patients over a short-term follow-up period. Visual acuity improved in 47.4% of the eyes and stabilized in 42.1% of the eyes. CRT significantly decreased after IVA, SRF diminished in 92.3% of affected eyes, and PED resolved in 35.7% of affected eyes.
The best treatment option for RAP patients remains unclear. Few relevant studies are available, and their results are difficult to compare because of their small sample sizes and difference in their study designs. PDT monotherapy with verteporfin provides some improvements in visual response but has a high chance of causing RPE tears, especially in patients with larger RAP lesions [11, 12, 24]. Intravitreal injections of bevacizumab or ranibizumab have been investigated and found to be effective for improving or maintaining BCVA [14, 25,26,27]. A head-to-head comparison between intravitreal injections of ranibizumab (IVR) and IVB was conducted, and the results showed that these two anti-VEGF agents were equally effective in improving or maintaining visual acuity in RAP patients [28]. In addition, after IVR, the rate of developing RPE tears was lower than those treated with PDT monotherapy [29], but the rate of geographic atrophy was higher than in patients with typical nAMD [30].
Aflibercept had been demonstrated to be as effective as ranibizumab in treating nAMD, and required fewer injections [17]. IVA was also associated with a higher incidence of drying the macula than IVR in patients with choroidal vascular hyperpermeability [31], and associated with a higher reduction rate of PED in nAMD patients [19]. In nAMD eyes that showed a poor response to IVR, switching to IVA achieved functional and anatomical improvements [32, 33].
However, study focused on the effect of treating RAP patients with aflibercept is scarce, with small case numbers and limited information on outcomes [19, 20]. Recently, Matsumoto et al. [18] reported the one-year results of treat-and-extend regimen of IVA on treating RAP. In their series, BCVA significantly improved and CRT significant decreased since post-IVA month one and persisted up to one year. However, the responses of PED were not described.
In the current study, 73.7% of the eyes had PED at baseline, and the mean baseline BCVA was relatively poor (Snellen chart equivalent of 20/340). Both the anatomical and functional responses to IVA were favorable, and the post-treatment mean BCVA significantly improved to 20/148, while the mean CRT was reduced from 404.0 μm to 306.1 μm. These results imply that aflibercept effectively dried the retina and improved vision even in patients with advanced RAP lesions and poor visual acuity. Nevertheless, the current study outcomes represent only short-term results, and RAP lesions are notorious for their high recurrence rate. Hence, a study including a longer observation period is needed to more accurately determine the long-term effects of IVA.
The reason that BCVA did not significantly improve in the pre-treatment subgroup is unclear. The fact that the rate of fibrovascular PED was initially higher (50%) in the pre-treatment group than in the in the naïve group (36%) could have contributed to the poorer responses that were observed in the pre-treatment group. The fact that baseline BCVA was better in the pre-treatment group may also have left less room for improvement: BCVA tended to be maintained (50.0%) in the pre-treatment group and improved (54.5%) in the naïve group. In both groups, only 1 eye had a BCVA that worsened by more than 3 lines.
PED, and especially fibrovascular PED, was a more difficult condition to manage. In previous reports on nAMD, PED has been associated with a poorer prognosis in patients treated with anti-VEGF agents [34, 35]. One recent report concluded that in patients with nAMD, fibrovascular PED had a lower probability of resolving than serous PED [36]. In the current series, the only 2 cases in which BCVA worsened by >3 lines (case 10 and 12) had baseline fibrovascular PED that persisted after IVA, and this prevented them from showing improved BCVA. The only 2 cases that had a thicker CRT after IVA (case 16 and 17) also had baseline fibrovascular PED, but their BCVA remained stable after treatment. Tsaousis et al. [37] reported 2 eyes in which CRT decreased while BCVA failed to improve. In our series, 4 eyes displayed reduced CRT but worsened BCVA. All 4 of these eyes had initial PED.
The above findings suggest that patients with PED lesions are at risk of having PED progression and altered RPE function. Both of these effects could impede visual outcomes despite the retina-drying effect of aflibercept. Although aflibercept has been reported to have better efficacy in resolving PED in nAMD patients than ranibizumab [36, 38, 39], the appropriate treatment for patients with RAP that has advanced beyond stage IIb remains to be determined in future studies.
Limitations of this study include its retrospective design and short-term follow-up period. Nearly half of the included patients were pre-treated with IVB, and this may have altered the conditions in the pre-treatment group. Although the period of clinical activity of bevacizumab has been reported to be as long as 100 days [40], and although a 6 weekly evaluation/treatment interval was proposed [41], most current study protocols use a series 3 monthly loading injections of bevacizumab to achieve an initial clinical response [42]. In our study, IVB dried the serous PED in 1 eye and improved mean CRT from 428 ± 165.2 μm (before IVB, referred to as month −1) to 359.1 ± 165.2 μm (at 1 month after IVB, referred to as month 0). However, this change was not significant (P = 0.263). It was only after IVA that the mean CRT in the pre-treatment group significantly improved. These improvements might be partially related to the effect of bevacizumab, but aflibercept appears to play a major role. The small sample size of the cohort may also have compromised data analysis. A study including a control group or that evaluates a matched comparison between different anti-VEGF agents is needed to clarify this issue. A longer follow-up period is also critically needed to evaluate the incidence of late complications, including geographic atrophy and RPE tears, and to determine the closure rate of vessel anastomosis.
Conclusion
Our study shows that IVA was efficacious in treating RAP patients over a short-term follow-up period. Ninety percent of the eyes showed improved or stable BCVA at the end of follow-up. Patients with baseline PED, especially fibrovascular PED, were more difficult to manage. Further studies are needed to determine the long-term efficacy of IVA in RAP patients in different stages of the disease.
Change history
15 August 2017
An erratum to this article has been published.
Abbreviations
- anti-VEGF:
-
anti-vascular endothelial growth factor
- BCVA:
-
best-corrected visual acuity
- CRT:
-
central retinal thickness
- F/D:
-
feeding/draining vessels
- FA:
-
fluorescein angiography
- ICGA:
-
indocyanine green angiography
- IR :
-
near-infrared
- IRC :
-
intraretinal cysts
- IRH:
-
intraretinal hemorrhage
- IVA:
-
intravitreal injections of aflibercept
- IVB:
-
intravitreal injection of bevacizumab
- IVR:
-
intravitreal injections of ranibizumab
- LogMAR:
-
logarithm of minimum angle of resolution
- nAMD:
-
neovascular age-related macular degeneration
- NHI:
-
National Health Insurance Administration in Taiwan
- OCT:
-
optical coherence tomography
- PDT:
-
photodynamic therapy
- PED:
-
pigment epithelial detachment
- PEI:
-
RPE interruption
- RAP:
-
retinal angiomatous proliferation
- RPD :
-
reticular pseudodrusen
- RPE:
-
retinal pigment epithelium
- SD:
-
standard deviation
- SD-OCT:
-
spectral-domain OCT
- SRF:
-
subretinal fluid
References
Yannuzzi LA, Negrao S, Iida T, Carvalho C, Rodriguez-Coleman H, Slakter J, Freund KB, Sorenson J, Orlock D, Borodoker N. Retinal angiomatous proliferation in age-related macular degeneration. Retina (Philadelphia, Pa). 2001;21(5):416–34.
Viola F, Massacesi A, Orzalesi N, Ratiglia R, Staurenghi G. Retinal angiomatous proliferation: natural history and progression of visual loss. Retina (Philadelphia, Pa). 2009;29(6):732–9.
Sawa M, Ueno C, Gomi F, Nishida K. Incidence and characteristics of neovascularization in fellow eyes of Japanese patients with unilateral retinal angiomatous proliferation. Retina (Philadelphia, Pa). 2014;347(4):761–7.
Cohen SY, Creuzot-Garcher C, Darmon J, Desmettre T, Korobelnik JF, Levrat F, et al. Types of choroidal neovascularisation in newly diagnosed exudative age-related macular degeneration. Br J Ophthalmol. 2007;91(9):1173–6.
Maruko I, Iida T, Saito M, Nagayama D, Saito K. Clinical characteristics of exudative age-related macular degeneration in Japanese patients. Am J Ophthalmol. 2007;144(1):15–22.
Sakurada Y, Yoneyama S, Sugiyama A, Tanabe N, Kikushima W, Mabuchi F, et al. Prevalence and genetic characteristics of geographic atrophy among elderly Japanese with age-related macular degeneration. PLoS One. 2016;11(2):e0149978.
Johnson TM, Glaser BM. Focal laser ablation of retinal angiomatous proliferation. Retina (Philadelphia, Pa). 2006;26(7):765–72.
Sakimoto S, Gomi F, Sakaguchi H, Tano Y. Recurrent retinal angiomatous proliferation after surgical ablation. Am J Ophthalmol. 2005;139(5):917–8.
Shiragami C, Iida T, Nagayama D, Baba T, Shiraga F. Recurrence after surgical ablation for retinal angiomatous proliferation. Retina (Philadelphia, Pa). 2007;27(2):198–203.
Kuroiwa S, Arai J, Gaun S, Iida T, Yoshimura N. Rapidly progressive scar formation after transpupillary thermotherapy in retinal angiomatous proliferation. Retina (Philadelphia, Pa). 2003;23(3):417–20.
Boscia F, Furino C, Sborgia L, Reibaldi M, Sborgia C. Photodynamic therapy for retinal angiomatous proliferations and pigment epithelium detachment. Am J Ophthalmol. 2004;138(6):1077–9.
Silva RM, Cachulo ML, Figueira J, de Abreu JR, Cunha-Vaz JG. Chorioretinal anastomosis and photodynamic therapy: a two-year follow-up study. Graefe's Arch Clin Exper Ophthalmol. 2007;245(8):1131–9.
Saito M, Shiragami C, Shiraga F, Kano M, Iida T. Comparison of intravitreal triamcinolone acetonide with photodynamic therapy and intravitreal bevacizumab with photodynamic therapy for retinal angiomatous proliferation. Am J Ophthalmol. 2010;149(3):472–481.e471.
Gharbiya M, Parisi F, Cruciani F, Bozzoni-Pantaleoni F, Pranno F, Abdolrahimzadeh S. Intravitreal anti-vascular endothelial growth factor for retinal angiomatous proliferation in treatment-naive eyes: long-term functional and anatomical results using a modified PrONTO-style regimen. Retina (Philadelphia, Pa). 2014;34(2):298–305.
Hemeida TS, Keane PA, Dustin L, Sadda SR, Fawzi AA. Long-term visual and anatomical outcomes following anti-VEGF monotherapy for retinal angiomatous proliferation. Br J Ophthalmol. 2010;94(6):701–5.
Gharbiya M, Allievi F, Recupero V, Martini D, Mazzeo L, Gabrieli CB. Intravitreal bevacizumab as primary treatment for retinal angiomatous proliferation: twelve-month results. Retina (Philadelphia, Pa). 2009;29(6):740–9.
Schmidt-Erfurth U, Kaiser PK, Korobelnik JF, Brown DM, Chong V, Nguyen QD, et al. Intravitreal aflibercept injection for neovascular age-related macular degeneration: ninety-six-week results of the VIEW studies. Ophthalmology. 2014;121(1):193–201.
Matsumoto H, Sato T, Morimoto M, Mukai R, Takahashi M, Hiroe T, Ehara K, Takayama M, Mimura K, Kishi S. Treat-and-extend regimen with aflibercept for retinal angiomatous proliferation. Retina (Philadelphia, Pa). 2016;36(12):2282–9.
Dirani A, Ambresin A, Marchionno L, Decugis D, Mantel I. Factors Influencing the Treatment Response of Pigment Epithelium Detachment in Age-Related Macular Degeneration. Am J Ophthalmol. 2015;160(4):732–738.e732.
Oishi A, Tsujikawa A, Yamashiro K, Ooto S, Tamura H, Nakanishi H, Ueda-Arakawa N, Miyake M, Akagi-Kurashige Y, Hata M, et al. One-year result of aflibercept treatment on age-related macular degeneration and predictive factors for visual outcome. Am J ophthalmol. 2015;159(5):853–860.e851.
Nagiel A, Sarraf D, Sadda SR, Spaide RF, Jung JJ, Bhavsar KV, Ameri H, Querques G, Freund KB. Type 3 neovascularization: evolution, association with pigment epithelial detachment, and treatment response as revealed by spectral domain optical coherence tomography. Retina (Philadelphia, Pa). 2015;35(4):638–47.
Ravera V, Bottoni F, Giani A, Cigada M, Staurenghi G. Retinal angiomatous proliferation diagnosis: a multiimaging approach. Retina (Philadelphia, Pa). 2016;36(12):2274–81.
Tsai AS, Cheung N, Gan AT, Jaffe GJ, Sivaprasad S, Wong TY, et al. Retinal angiomatous proliferation. Survey of ophthalmology. 2017.
Boscia F, Parodi MB, Furino C, Reibaldi M, Sborgia C. Photodynamic therapy with verteporfin for retinal angiomatous proliferation. Graefe's Arch Clin Exper Ophthalmol. 2006;244(10):1224–32.
Inoue M, Arakawa A, Yamane S, Kadonosono K. Long-term results of intravitreal ranibizumab for the treatment of retinal angiomatous proliferation and utility of an advanced RPE analysis performed using spectral-domain optical coherence tomography. Br J Ophthalmol. 2014;98(7):956–60.
Rouvas AA, Chatziralli IP, Theodossiadis PG, Moschos MM, Kotsolis AI, Ladas ID. Long-term results of intravitreal ranibizumab, intravitreal ranibizumab with photodynamic therapy, and intravitreal triamcinolone with photodynamic therapy for the treatment of retinal angiomatous proliferation. Retina (Philadelphia, Pa). 2012;32(6):1181–9.
Cho HJ, Lee TG, Han SY, Kim HS, Kim JH, Han JI, Lew YJ, Kim JW. Long-term visual outcome and prognostic factors of Intravitreal anti-vascular endothelial growth factor treatment for retinal angiomatous proliferation. Graefe's Arch Clin Exper Ophthalmol. 2016;254(1):23–30.
Parodi MB, Iacono P, Menchini F, Sheth S, Polini G, Pittino R, et al. Intravitreal bevacizumab versus ranibizumab for the treatment of retinal angiomatous proliferation. Acta Ophthalmol. 2013;91(3):267–73.
Cho HJ, Kim HS, Yoo SG, Han JI, Lew YJ, Cho SW, Lee TG, Kim JW. Retinal Pigment Epithelial Tear After Intravitreal Ranibizumab Treatment for Retinal Angiomatous Proliferation. Am J Ophthalmol. 2015;160(5):1000–1005.e1002.
Cho HJ, Yoo SG, Kim HS, Kim JH, Kim CG, Lee TG, Kim JW. Risk factors for geographic atrophy after intravitreal ranibizumab injections for retinal angiomatous proliferation. Am J Ophthalmol. 2015;159(2):285–292.e281.
Hata M, Oishi A, Tsujikawa A, Yamashiro K, Miyake M, Ooto S, et al. Efficacy of intravitreal injection of aflibercept in neovascular age-related macular degeneration with or without choroidal vascular hyperpermeability. Invest Ophthalmol Vis Sci. 2014;55(12):7874–80.
Chang AA, Li H, Broadhead GK, Hong T, Schlub TE, Wijeyakumar W, et al. Intravitreal aflibercept for treatment-resistant neovascular age-related macular degeneration. Ophthalmology. 2014;121(1):188–92.
Wykoff CC, Brown DM, Maldonado ME, Croft DE. Aflibercept treatment for patients with exudative age-related macular degeneration who were incomplete responders to multiple ranibizumab injections (TURF trial). Br J Ophthalmol. 2014;98(7):951–5.
Simader C, Ritter M, Bolz M, Deak GG, Mayr-Sponer U, Golbaz I, et al. Morphologic parameters relevant for visual outcome during anti-angiogenic therapy of neovascular age-related macular degeneration. Ophthalmology. 2014;121(6):1237–45.
Schmidt-Erfurth U, Waldstein SM, Deak GG, Kundi M, Simader C. Pigment epithelial detachment followed by retinal cystoid degeneration leads to vision loss in treatment of neovascular age-related macular degeneration. Ophthalmology. 2015;122(4):822–32.
Cho HJ, Kim KM, Kim HS, Lee DW, Kim CG, Kim JW. Response of pigment epithelial detachment to anti-vascular endothelial growth factor treatment in age-related macular degeneration. Am J Ophthalmol. 2016;166:112–9.
Tsaousis KT, Konidaris VE, Banerjee S, Empeslidis T. Intravitreal aflibercept treatment of retinal angiomatous proliferation: a pilot study and short-term efficacy. Graefe's archive for clinical and experimental ophthalmology = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie. 2015;253(4):663–5.
Broadhead GK, Hong T, Zhu M, Li H, Schlub TE, Wijeyakumar W, Chang AA. Response of pigment epithelial detachments to intravitreal aflibercept among patients with treatment-resistant neovascular age-related macular degeneration. Retina (Philadelphia, Pa). 2015;35(5):975–81.
Patel KH, Chow CC, Rathod R, Mieler WF, Lim JI, Ulanski LJ, 2nd, Leiderman YI, Arun V, Chau FY. Rapid response of retinal pigment epithelial detachments to intravitreal aflibercept in neovascular age-related macular degeneration refractory to bevacizumab and ranibizumab. Eye (London, England). 2013;27(5):663–7; quiz 668.
Shah AR, Del Priore LV. Duration of action of intravitreal ranibizumab and bevacizumab in exudative AMD eyes based on macular volume measurements. Br J Ophthalmol. 2009;93(8):1027–32.
Tufail A, Patel PJ, Egan C, Hykin P, da Cruz L, Gregor Z, Dowler J, Majid MA, Bailey C, Mohamed Q, et al. Bevacizumab for neovascular age related macular degeneration (ABC Trial): multicentre randomised double masked study. BMJ (Clinical research ed). 2010;340:c2459.
Moja L, Lucenteforte E, Kwag KH, Bertele V, Campomori A, Chakravarthy U, D'Amico R, Dickersin K, Kodjikian L, Lindsley K, et al. Systemic safety of bevacizumab versus ranibizumab for neovascular age-related macular degeneration. Cochrane Database Syst Rev. 2014(9):Cd011230.
Acknowledgements
Not applicable.
Funding
There were no funding sources for this study.
Availability of data and materials
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request. (E-mail: chichun.lai@gmail.com)
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Contributions
HC drafted the manuscript. CL provided the idea of the study and carried out all the exams. CL and KC reviewed the images of the study participants. CL, WW, LC, and NW revised the manuscript and reviewed the article. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
All procedures involving human participants were performed in accordance with the ethical standards of the ethics committee of Chung-Gang Memorial Hospital (study reference number: 102-0780A) and adhered to the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent for publication
Written informed consents were obtained from the patients for publication of any information contained within the manuscript itself. The copies of the written consent are available for review by the Editor of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
The original version of this article has been revised to correct table 1.
An erratum to this article is available at https://doi.org/10.1186/s12886-017-0531-2.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Chou, HD., Wu, WC., Wang, NK. et al. Short-term efficacy of intravitreal Aflibercept injections for retinal angiomatous proliferation. BMC Ophthalmol 17, 104 (2017). https://doi.org/10.1186/s12886-017-0497-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-017-0497-0