Abstract
Background
CHEK2 is involved in the DNA damage repair response Fanconi anemia (FA)-BRCA pathway. An increased risk for breast and other cancers has been documented in individuals who carry a single pathogenic CHEK2 variant. As for other genes involved in cancer predisposition, different types of pathogenic variants have been observed, including single nucleotide variations, short insertions/deletions, large genomic rearrangements and splicing variants. Splicing variants occurring in the splicing acceptor or donor site result in alternative mature mRNA produced and can cause intron retention, exon skipping, or creation of alternative 3′ and 5′ splice site. Thus, the pathogenicity of this type of alterations should always be explored experimentally and their effect in the mRNA and consequently the protein produced, should be defined. The aim of this study was the delineation of the effect of a splicing variant in the CHEK2 gene.
Case presentation
A healthy 28-year-old woman with a family history of breast and ovarian cancer was referred for genetic testing. The variant c.793-1G > A (rs730881687) was identified by Next Generation Sequencing (NGS) using a solution-based capture method, targeting 33 cancer predisposition genes (SeqCap EZ Probe library, Roche NimbleGen). Experimental analysis in patient-derived leukocytes using RT-PCR of mRNA followed by cDNA sequencing revealed the deletion of one base from the alternative transcript created (r.793del). This resulted in a frameshift leading to premature termination codon within exon 7 (p.(Asp265Thrfs*10)).
Conclusions
This finding suggests that the CHEK2 splicing variant c.793-1G > A is a deleterious variant. Our case shows that RNA analysis is a valuable tool for uncharacterized splice site variants in individuals referred for testing and facilitates their personalized management.
Similar content being viewed by others
Background
Germline CHEK2 pathogenic variants have been associated with breast, prostate, colorectal, gastric, thyroid, bladder and kidney cancer [1]. CHEK2 pathogenic variants such as the c.1100delC variant [2] are associated with breast cancer and have been characterized. In addition, other CHEK2 variants, such as c.470 T > C, p.(Ile157Thr) and c.1283C > T, p.(Ser428Phe), are characterized as of low penetrance for breast cancer [3].
Nowadays, Next Generation Sequencing (NGS) technology has allowed multi-gene panel analysis which is used in clinical practice for the identification of individuals with an inherited predisposition to cancer. Usually, the majority of genes analyzed in such panels is included in guidelines and have clinical management [4].
The type of pathogenic variants identified using NGS methodology include single nucleotide variations (SNV), short insertions/deletions (Ins/Del), large genomic rearrangements (LGR) and splicing variants. All these alterations usually occur in tumor suppressor genes and are related to increased risk of cancer development. The classification of the variants identified in a five-tier classification system is done using the American College of Medical Genetics and Genomics (ACMG) Laboratory Quality Assurance Committee guidelines [5]. According to this system a variant can be classified as pathogenic, likely pathogenic, variant of uncertain significance, likely benign and benign. The assignment of a variant in the pathogenic class requires the presence of both experimental and in silico analysis that provide multi-level evidence for a major impact of the alteration in the protein’s function.
Splicing variants occurring in the splicing acceptor or donor site result in alternative mature mRNA production [6] and can cause intron retention, exon skipping, or creation of alternative 3′ and 5′ splice site, resulting in the production of a disrupted or non-functional protein. The detection of such variants provides strong evidence of pathogenicity based on the ACMG guidelines, but their effect can be also investigated by in silico analysis that should be confirmed either at the mRNA or the protein level.
In our case, we report the functional characterization of a CHEK2 variant located in intron 6. The variant c.793-1G > A alters the wild type acceptor site and activates a cryptic acceptor site one nucleotide base downstream, creating a new transcript with a premature translation stop codon 10 amino acid residues later. This is expected to lead in an absent or disrupted protein product.
Case presentation
Patient
A 28-year-old healthy woman, with a family history of breast and ovarian cancer, was referred to our laboratory for multigene testing. Our proband was informed about the significance of molecular testing, provided information about her personal and family history and signed an informed consent form prior to molecular genetic testing and permission for the anonymous use of her data for research purposes and/or scientific publications.
Gene testing
Genomic DNA was extracted from peripheral blood leukocytes using MagCore® Genomic DNA Whole Blood Kit (RBC Bioscience) according to the manufacturer’s instructions.
The analysis of genes involved in hereditary cancer predisposition was performed using a solution-based capture approach. Targeted NGS was performed with a panel of 33 genes (Roche NimbleGen SeqCap EZ Choice) [APC (NM_000038.5), ATM (NM_000051.3), BARD1 (NM_000465.2), BMPR1A (NM_004329.2), BRCA1 (NM_007294.2), BRCA2 (NM_000059.3), BRIP1 (NM_032043.2), CDH1 (NM_004360.4), CDK4 (NM_000075.3), CDKN2A (NM_000077.4), CHEK1 (NM_001114121.2), CHEK2 (NM_007194.3), EPCAM (NM_002354.2), MEN1 (NM_000244.3), MLH1 (NM_000249.3), MRE11 (NM_005591.3), MSH2 (NM_000251.2), MSH6 (NM_000179.2), MUTYH (NM_001128425.1), NBN (NM_002485.4), NF1 (NM_000267.3), PALB2 (NM_024675.3), PMS2 (NM_000535.5), PTEN (NM_000314.4), RAD50 (NM_005732.3), RAD51B (NM_133509.3), RAD51C (NM_058216.2), RAD51D (NM_002878.3), RET (NM_020975.4), SMAD4 (NM_005359.5), STK11 (NM_000455.4), TP53 (NM_000546.5), VHL (NM_000551.3)]. The sample preparation was performed according to the manufacturer’s instructions in the SeqCap EZ Choice Library User’s Guide (Roche NimbleGen). Sequencing was carried out using the Miseq Illumina NGS technology and sequence changes were identified and interpreted in the context of a single clinically relevant transcript using the commercially available software suite SeqNext (JSI medical systems GmbH, Germany).
Variant classification and bioinformatics analysis
The clinical significance of variants was further examined using standards and guidelines for the interpretation of sequence variants recommended by the ACMG Laboratory Quality Assurance Committee and the Association for Molecular Pathology (AMP) [5]. The impact of missense substitutions on protein function or structure was analyzed using computational (in silico) predictive algorithms combined with the ensemble mutational impact score of MetaSVM [7]. The effect on splicing was computationally examined using Human Splicing Finder [8].
RNA analysis
Total RNA was extracted from peripheral blood lymphocytes using Trizol (Invitrogen, Paisley, UK) following standard protocol. cDNA was synthesized using SuperScript™ VILO™ cDNA Synthesis Kit (Thermo Fisher Scientific) as described by the supplier. The resulting cDNA was amplified with the CHEK2 specific primers CHEK2X5F_RNA:5′-ACATCATGTCAAAAACTCTTGGAA-3′ and CHEK2X8-9R_RNA: 5′-CCCCTTCCATCAATTCCAAAACAA-3′ and the PCR-products were purified using NucleoFast® 96 PCR Clean-up kit (Macherey-Nagel GmbH and Co., Düren, Germany). The purified PCR product were used for each sequencing reaction, which was performed using the BigDye® Terminator v1.1 Cycle Sequencing kit (Applied Biosystems, Foster City, CA, USA) and Sequencing reaction products were purified prior to electrophoresis using the Montage™ SEQ96 Sequencing Reaction kit (EMD Millipore Corp., Billerica, MA, USA) and sequenced using an Applied Biosystems 3130 Genetic Analyzer (Applied Biosystems).
Results
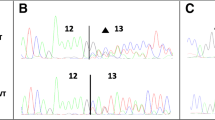
The proband was referred to genetic counseling, since her mother was diagnosed with breast and ovarian cancer at a young age (Fig. 1). Our analysis using NGS technology identified the variant c.793-1G > A (rs730881687) in the CHEK2 gene, in heterozygosity. This alteration was a replacement of the last nucleotide base in intron 6 of the CHEK2 gene. This finding was confirmed by Sanger Sequencing using the following forward and reverse primers (5′-TCAGGCAGCCTTGAGTCAAC-3′ and 5′- CAGCTAAATGACAGCTAGGC-3′ respectively) as described previously [9] (Fig. 2a). This particular location is strictly conserved in human and splice donor and acceptor site variants typically lead to loss of protein function [10]. Furthermore, loss-of-function variants in CHEK2 are known to be pathogenic [11]. No other pathogenic/likely pathogenic variants were identified in the remaining 32 genes that were analyzed.
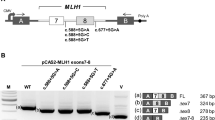
a Sequencing analysis of genomic DNA from the proband carrying the c.793-1G > A variant in the CHEK2 gene. b Binding sites of the primers on the cDNA of CHEK2 c RT-PCR electrophoresis products on 3% agarose gel. Lane 1: proband’s sample with the splicing variant, Lane 2: normal sample, Lane 3: negative control, Lane 4: 1000 bp DNA ladder (New England Biolabs). d Sequencing analysis of the proband’s cDNA showing the frameshift of the variant and the generation of a premature translation stop signal (TAG) 10 amino acid residues later (bottom panel) compared to the sequencing analysis of a wild type sample (top panel)
In silico analysis predicted that this change is disrupting the wild type acceptor site and is activating an intronic cryptic splice acceptor 1 bp downstream, creating a frameshift. The prediction was confirmed by RNA analysis, (Fig. 2b, c, d) showing that the c.793-1G > A variant affects splicing by creating an alternative splice site 1 bp downstream (r.793del) which results in a frameshift effect and the generation of a premature translation stop signal 10 amino acid residues later and is predicted to result in a truncated protein (p.(Asp265Thrfs*10)).
Discussion and conclusions
The variant c.793-1G > A identified in the proband tested has been previously reported in an individual affected with breast cancer [4] and in individuals who underwent genetic tests for hereditary cancer risk [12]. The variant database ClinVar contains entries for this variant (rs730881687) where it is listed as likely pathogenic and pathogenic (https://www.ncbi.nlm.nih.gov/clinvar/variation/182430/) without any available experimental evidence reported. Our clinical interpretation (pathogenic) for this variant along with the above experimental information has now been submitted to ClinVar (SUB5321389).
To our knowledge, this study provides the first experimental characterization of the CHEK2 c.793-1G > A variant, elucidating its impact on splicing.
The proband could receive clinical management based on the NCCN guidelines suggested for CHEK2 pathogenic variant carriers, such as annual mammogram with consideration of tomosynthesis and breast MRI with contrast at age 40 y.o. [13]. The main limitation of this study was the absence of genetic material from the proband’s mother who had breast and ovarian cancer diagnosis and died at the age of 56. Moreover, testing of the proband’s father was not possible although was requested by our lab.
In conclusion RNA analysis confirmed the disrupting impact of the splice site variant c.793-1G > A in the CHEK2 mRNA, leading to the definite classification of this variant as pathogenic. We propose that RNA classification should always be conducted wherever an uncharacterized splice site variant is identified in individuals referred for genetic testing.
Availability of data and materials
All data generated or analyzed during this study are included in this published article. The clinical interpretation of the genomic variant along with the experimental information has been submitted to ClinVar (SUB5321389).
Abbreviations
- ACMG:
-
American College of Medical Genetics and Genomics
- AMP:
-
Association for Molecular Pathology
- FA:
-
Fancomi Anemia
- NCCN:
-
National Comprehensive Cancer Network
- NGS:
-
Next Generation Sequencing
- RT-PCR:
-
Reverse-Transcription Polymerase Chain Reaction
References
Cybulski C, Górski B, Huzarski T, et al. CHEK2 is a multiorgan cancer susceptibility gene. Am J Hum Genet. 2004;75:1131–5.
CHEK2 Breast Cancer Case-Control Consortium. CHEK2*1100delC and susceptibility to breast cancer: a collaborative analysis involving 10,860 breast cancer cases and 9,065 controls from 10 studies. Am J Hum Genet. 2004;74:1175–82.
Cybulski C, Wokołorczyk D, Jakubowska A, et al. Risk of breast cancer in women with a CHEK2 mutation with and without a family history of breast cancer. J Clin Oncol. 2011;29:3747–52.
Susswein LR, Marshall ML, Nusbaum R, et al. Pathogenic and likely pathogenic variant prevalence among the first 10,000 patients referred for next-generation cancer panel testing. Genet Med. 2016;18:823–32.
Richards S, Aziz N, Bale S, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17:405–24.
Anna A, Monika G. Splicing mutations in human genetic disorders: examples, detection, and confirmation. J Appl Genet. 2018;59:253–68.
Dong C, Wei P, Jian X, et al. Comparison and integration of deleteriousness prediction methods for nonsynonymous SNVs in whole exome sequencing studies. Hum Mol Genet. 2015;24:2125–37.
Desmet FO, Hamroun D, Lalande M, et al. Human splicing finder: an online bioinformatics tool to predict splicing signals. Nucleic Acids Res. 2009;37:e67.
Dufault MR, Betz B, Wappenschmidt B, et al. Limited relevance of the CHEK2 gene in hereditary breast cancer. Int J Cancer. 2004;110:320–5.
Baralle D, Baralle M. Splicing in action: assessing disease causing sequence changes. J Med Genet. 2005;42:737–48.
Bąk A, Janiszewska H, Junkiert-Czarnecka A, et al. A risk of breast cancer in women - carriers of constitutional CHEK2 gene mutations, originating from the north - Central Poland. Hered Cancer Clin Pract. 2014;12:10.
Leedom TP, LaDuca H, McFarland R, et al. Breast cancer risk is similar for CHEK2 founder and non-founder mutation carriers. Cancer Genet. 2016;209:403–7.
The National Comprehensive Cancer Network. Genetic/Familiar High-Risk Assessment: Breast and Ovarian (Version 2.2019). Accessed 27 Aug 2018.
Acknowledgements
Not applicable
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
KA, EP and GNT drafted the manuscript. KA and EP designed the study and the sequencing experiments, and coordinated the study. KA, GP and SK carried out the DNA extraction, sequencing and RNA analysis and contributed to the analysis and interpretation of the variant data. GNT performed the bioinformatics analysis. MAK provided the proband material, demographic data, family history and management. GN conceived of the study, and participated in its design and coordination. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The proband provided a signed informed consent form prior to molecular genetic testing.
Consent for publication
The proband provided a signed informed consent form prior to molecular genetic testing for the permission of the anonymous use of her data for research purposes and/or scientific publications.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Agiannitopoulos, K., Papadopoulou, E., Tsaousis, G.N. et al. Characterization of the c.793-1G > A splicing variant in CHEK2 gene as pathogenic: a case report. BMC Med Genet 20, 131 (2019). https://doi.org/10.1186/s12881-019-0862-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12881-019-0862-3