Abstract
Background
During surgery, proper fluid resuscitation and hemostatic control is critical. Pleth variability index (PVI) is advocated as a reliable way of optimizing intraoperative fluid resuscitation. PVI is a measure of dynamic change in perfusion index during a complete respiratory cycle. Non-invasive monitoring of total hemoglobin could provide a reliable means to determine need for transfusion. We analyzed the impact of insufflation and obesity on non-invasive measurements of hemoglobin and PVI in laparoscopic procedures to validate reliability of fluid responsiveness and hemoglobin levels.
Methods
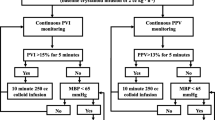
A non-invasive hemoglobin and PVI monitoring device was prospectively analyzed in patients undergoing abdominal operations. Patients were stratified by open and laparoscopic approach and obesity (body mass index (BMI) ≥35). PVI and hemoglobin values were assessed before, during, and after insufflation and compared to control patients undergoing open surgery.
Results
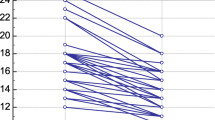
Sixty-three patients were enrolled (mean age 42 years; 71 % male; mean BMI 36) with 24 patients laparoscopic non-obese (LNO), 20 laparoscopic obese (LO), and 19 undergoing open operations. There was no significant blood loss. Hemoglobin did not change significantly before or after insufflation. There was false elevation of PVI with insufflation and more pronounced in obese patients.
Conclusions
Insufflation or obesity was not associated with significant variations in hemoglobin. Non-invasive monitoring of hemoglobin is useful in laparoscopic procedures in obese and non-obese patients. PVI values should be used cautiously during laparoscopic procedures, particularly in obese patients.

Similar content being viewed by others
References
Marik PE, Cavallazzi R, Vasu T, et al. Dynamic changes in arterial waveform derived variables and fluid responsiveness in mechanically ventilated patients: a systematic review of the literature. Crit Care Med. 2009;37(9):2642–7.
Rivers E, Nguyen B, Havstad S, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345(19):1368–77.
Teboul JL, Monnet X. Detecting volume responsiveness and unresponsiveness in intensive care unit patients: two different problems, only one solution. Crit Care. 2009;13(4):175.
Shah MR, Hasselblad V, Stevenson LW, et al. Impact of the pulmonary artery catheter in critically ill patients: meta-analysis of randomized clinical trials. JAMA. 2005;294(13):1664–70.
Hadian M, Pinsky MR. Evidence-based review of the use of the pulmonary artery catheter: impact data and complications. Crit Care. 2006;10 Suppl 3:S8.
Marik PE, Baram M, Vahid B. Does central venous pressure predict fluid responsiveness? A systematic review of the literature and the tale of seven mares. Chest. 2008;134(1):172–8.
Jefferson P, Ball DR. Central venous access in morbidly obese patients. Anesth Analg. 2002;95(3):782.
Trick WE, Miranda J, Evans AT, et al. Prospective cohort study of central venous catheters among internal medicine ward patients. Am J Infect Control. 2006;34(10):636–41.
Brusasco C, Corradi F, Zattoni PL, et al. Ultrasound-guided central venous cannulation in bariatric patients. Obes Surg. 2009;19(10):1365–70.
Cotter G, Moshkovitz Y, Kaluski E, et al. Accurate, noninvasive continuous monitoring of cardiac output by whole-body electrical bioimpedance. Chest. 2004;125(4):1431–40.
Bodo M, Settle T, Royal J, et al. Multimodal noninvasive monitoring of soft tissue wound healing. J Clin Monit Comput. 2013;27(6):677–88.
Muller JC, Kennard JW, Browne JS, et al. Hemodynamic monitoring in the intensive care unit. Nutr Clin Pract. 2012;27(3):340–51.
Lipcsey M, Woinarski NC, Bellomo R. Near infrared spectroscopy (NIRS) of the thenar eminence in anesthesia and intensive care. Ann Intensive Care. 2012;2(1):11.
Mohan VK, Chanderlekha, Kashyap L. Cardiac output monitoring based on thoracic electrical bioimpedance. J Postgrad Med. 2002;48(4):329–30.
Cannesson M, Desebbe O, Rosamel P, et al. Pleth variability index to monitor the respiratory variations in the pulse oximeter plethysmographic waveform amplitude and predict fluid responsiveness in the operating theatre. Br J Anaesth. 2008;101(2):200–6.
Feissel M, Teboul JL, Merlani P, et al. Plethysmographic dynamic indices predict fluid responsiveness in septic ventilated patients. Intensive Care Med. 2007;33(6):993–9.
Loupec T, Nanadoumgar H, Frasca D, et al. Pleth variability index predicts fluid responsiveness in critically ill patients. Crit Care Med. 2011;39(2):294–9.
Causey MW, Miller S, Foster A, et al. Validation of noninvasive hemoglobin measurements using the masimo radical-7 SpHb station. Am J Surg. 2011;201(5):592–8.
Henny CP, Hofland J. Laparoscopic surgery: pitfalls due to anesthesia, positioning, and pneumoperitoneum. Surg Endosc. 2005;19(9):1163–71.
Jafari MD, Jafari F, Young MT, et al. Volume and outcome relationship in bariatric surgery in the laparoscopic era. Surg Endosc. 2013;27(12):4539–46.
Nguyen NT, Nguyen B, Gebhart A, et al. Changes in the makeup of bariatric surgery: a national increase in use of laparoscopic sleeve gastrectomy. J Am Coll Surg. 2013;216(2):252–7.
Brandt S, Regueira T, Bracht H, et al. Effect of fluid resuscitation on mortality and organ function in experimental sepsis models. Crit Care. 2009;13(6):R186.
Verdant C, De Backer D. How monitoring of the microcirculation may help us at the bedside. Curr Opin Crit Care. 2005;11(3):240–4.
Lv L, Shao YF, Zhou YB. The enhanced recovery after surgery (ERAS) pathway for patients undergoing colorectal surgery: an update of meta-analysis of randomized controlled trials. Int J Colorectal Dis. 2012;27(12):1549–54.
Hoiseth LO, Hoff IE, Myre K, et al. Dynamic variables of fluid responsiveness during pneumoperitoneum and laparoscopic surgery. Acta Anaesthesiol Scand. 2012;56(6):777–86.
Holodinsky JK, Roberts DJ, Ball CG, et al. Risk factors for intra-abdominal hypertension and abdominal compartment syndrome among adult intensive care unit patients: a systematic review and meta-analysis. Crit Care. 2013;17(5):R249.
Robinson BR, Cotton BA, Pritts TA, et al. Application of the Berlin definition in PROMMTT patients: the impact of resuscitation on the incidence of hypoxemia. J Trauma Acute Care Surg. 2013;75(1 Suppl 1):S61–7.
Kulemann B, Timme S, Seifert G, et al. Intraoperative crystalloid overload leads to substantial inflammatory infiltration of intestinal anastomoses—a histomorphological analysis. Surgery. 2013;154(3):596–603.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of Interest
The authors have no conflict of interests to declare. The views expressed are those of the author(s) and do not reflect the official policy of the Department of the Army, the Department of Defense or the US Government.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
DeBarros, M., Causey, M.W., Chesley, P. et al. Reliability of Continuous Non-Invasive Assessment of Hemoglobin and Fluid Responsiveness: Impact of Obesity and Abdominal Insufflation Pressures. OBES SURG 25, 1142–1148 (2015). https://doi.org/10.1007/s11695-014-1505-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-014-1505-6