Abstract
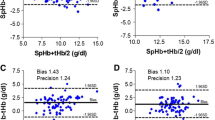
The evolution of non-invasive hemoglobin measuring technology would save time and improve transfusion practice. The validity of pulse co-oximetry hemoglobin (SpHb) measurement in the perioperative setting was previously evaluated; however, the accuracy of SpHb in different volume statuses as well as in different perfusion states was not well investigated. The aim of this work is to evaluate the accuracy and trending of SpHb in comparison to laboratory hemoglobin (Lab-Hb) during acute bleeding and after resuscitation. Seventy patients scheduled for major orthopedic procedures with anticipated major blood loss were included. Radical-7 device was used for continuous assessment of SpHb, volume status [via pleth variability index (PVI)] and perfusion status [via perfusion index (PI)]. Lab-Hb and SpHb were measured at three time-points, a baseline reading, after major bleeding, and after resuscitation. Samples were divided into fluid-responsive and fluid non-responsive samples, and were also divided into high-PI and low-PI samples. Accuracy of SpHb was determined using Bland–Altman analysis. Trending of SpHb was evaluated using polar plot analysis. We obtained 210 time-matched readings. Fluid non-responsive samples were 106 (50.5%) whereas fluid responsive samples were 104 (49.5%). Excellent correlation was reported between Lab-Hb and SpHb (r = 0.938). Excellent accuracy with moderate levels of agreement was also reported between both measures among all samples, fluid non-responsive samples, fluid-responsive samples, high-PI samples, and low-PI samples [Mean bias (limits of agreement): 0.01 (− 1.33 and 1.34) g/dL, − 0.08 (− 1.27 and 1.11) g/dL, 0.09 (− 1.36 and 1.54) g/dL, 0.01 (− 1.34 to 1.31) g/dL, and 0.04 (− 1.31 to 1.39) g/dL respectively]. Polar plot analysis showed good trending ability for SpHb as a follow up monitor. In conclusion, SpHb showed excellent correlation with Lab-Hb in fluid responders, fluid non-responders, low-PI, and high PI states. Despite a favorable mean bias of 0.01 g/dL for SpHb, the relatively wide levels of agreement (− 1.3 to 1.3 g/dL) might limit its accuracy. SpHb showed good performance as a trend monitor.





Similar content being viewed by others
References
Zwart A, van Assendelft OW, Bull BS, England JM, Lewis SM, Zijlstra WG. Recommendations for reference method for haemoglobinometry in human blood (ICSH standard 1995) and specifications for international haemiglobinocyanide standard. J Clin Pathol. 1996;49:271–4.
Rasmy I, Mohamed H, Nabil N, Abdalah S, Hasanin A, Eladawy A, et al. Evaluation of perfusion index as a predictor of vasopressor requirement in patients with severe sepsis. Shock. 2015;44:554–9.
Hasanin A, Mohamed SAR, El-adawy A. Evaluation of perfusion index as a tool for pain assessment in critically ill patients. J Clin Monit Comput. 2016;31(5):961–65.
Kim S-H, Lilot M, Murphy LS-L, Sidhu KS, Yu Z, Rinehart J, et al. Accuracy of continuous noninvasive hemoglobin monitoring: a systematic review and meta-analysis. Anesth Analg. 2014;119:332–46.
Gamal M, Abdelhamid B, Zakaria D, Dayem OA El, Rady A, Fawzy M, et al. Evaluation of non-invasive hemoglobin monitoring in trauma patients with low hemoglobin levels. Shock. 2017;49(2):150–3.
Hasanin A. Fluid responsiveness in acute circulatory failure. J Intensive Care. 2015;3:50.
Hasanin A, Mukhtar A, Nassar H. Perfusion indices revisited. J Intensive Care. 2017;5:24.
Hellstern P, Haubelt H. Indications for plasma in massive transfusion. Thromb Res. 2002;107:S19–22.
Critchley LA, Yang XX, Lee A. Assessment of trending ability of cardiac output monitors by polar plot methodology. J Cardiothorac Vasc Anesth. 2011;25:536–46.
Kozek-Langenecker SA, Ahmed AB, Afshari A, Albaladejo P, Aldecoa C, Barauskas G, et al. Management of severe perioperative bleeding. Eur J Anaesthesiol. 2017;34:332–95.
Moore LJ, Wade CE, Vincent L, Podbielski J, Camp E, Junco D del, et al. Evaluation of noninvasive hemoglobin measurements in trauma patients. Am J Surg. 2013;206:1041–7.
Galvagno SM, Hu P, Yang S, Gao C, Hanna D, Shackelford S, et al. Accuracy of continuous noninvasive hemoglobin monitoring for the prediction of blood transfusions in trauma patients. J Clin Monit Comput. 2015;29:815–21.
Awada WN, Mohmoued MF, Radwan TM, Hussien GZ, Elkady HW. Continuous and noninvasive hemoglobin monitoring reduces red blood cell transfusion during neurosurgery: a prospective cohort study. J Clin Monit Comput. 2015;29:733–40.
Marques NR, Kramer GC, Voigt RB, Salter MG, Kinsky MP. Trending, accuracy, and precision of noninvasive hemoglobin monitoring during human hemorrhage and fixed crystalloid bolus. Shock. 2015;44:45–9.
Dewhirst E, Naguib A, Winch P, Rice J, Galantowicz M, McConnell P, et al. Accuracy of noninvasive and continuous hemoglobin measurement by pulse co-oximetry during preoperative phlebotomy. J Intensive Care Med. 2014;29:238–42.
Isosu T, Obara S, Hosono A, Ohashi S, Nakano Y, Imaizumi T, et al. Validation of continuous and noninvasive hemoglobin monitoring by pulse co-oximetry in Japanese surgical patients. J Clin Monit Comput. 2013;27:55–60.
Wittenmeier E, Bellosevich S, Mauff S, Schmidtmann I, Eli M, Pestel G, et al. Comparison of the gold standard of hemoglobin measurement with the clinical standard (BGA) and noninvasive hemoglobin measurement (SpHb) in small children: a prospective diagnostic observational study. Pediatr Anesth. 2015;25:1046–53.
Miller RD, Ward TA, McCulloch CE, Cohen NH. A comparison of lidocaine and bupivacaine digital nerve blocks on noninvasive continuous hemoglobin monitoring in a randomized trial in volunteers. Anesth Analg. 2014;118:766–71.
Abdelnasser A, Abdelhamid B, Elsonbaty A, Hasanin A. AR. Predicting successful supraclavicular brachial plexus block using pulse oximeter perfusion index. ]. 2017:119(2):276–80.
Lima AP, Beelen P, Bakker J. Use of a peripheral perfusion index derived from the pulse oximetry signal as a noninvasive indicator of perfusion. Crit Care Med. 2002;30:1210–3.
Høiseth L, Hisdal J, Hoff IE, Hagen OA, Landsverk SA, Kirkebøen KA. Tissue oxygen saturation and finger perfusion index in central hypovolemia: influence of pain. Crit Care Med. 2015;43:747–56.
Shamir M, Eidelman LA, Floman Y, Kaplan L, Pizov R. Pulse oximetry plethysmographic waveform during changes in blood volume. ]. 1999;82:178–81.
Sandroni C, Cavallaro F, Marano C, Falcone C, De Santis P, Antonelli M. Accuracy of plethysmographic indices as predictors of fluid responsiveness in mechanically ventilated adults: a systematic review and meta-analysis. Intensive Care Med. 2012;38:1429–37.
Feissel M, Teboul JL, Merlani P, Badie J, Faller JP, Bendjelid K. Plethysmographic dynamic indices predict fluid responsiveness in septic ventilated patients. Intensive Care Med. 2007;33:993–9.
Acknowledgements
We would like to thank Dr. Ahmed Mukhtar, professor of anesthesia and Dr. Menna Alshaarawy, resident of anesthesia for their help in this study.
Funding
Funding was provided by Cairo University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest with this work.
Rights and permissions
About this article
Cite this article
Adel, A., Awada, W., Abdelhamid, B. et al. Accuracy and trending of non-invasive hemoglobin measurement during different volume and perfusion statuses. J Clin Monit Comput 32, 1025–1031 (2018). https://doi.org/10.1007/s10877-018-0101-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-018-0101-z