Abstract
Near infrared spectroscopy of the thenar eminence (NIRSth) is a noninvasive bedside method for assessing tissue oxygenation. The NIRS probe emits light with several wavelengths in the 700- to 850-nm interval and measures the reflected light mainly from a predefined depth. Complex physical models then allow the measurement of the relative concentrations of oxy and deoxyhemoglobin, and thus tissue saturation (StO2), as well as an approximation of the tissue hemoglobin, given as tissue hemoglobin index.
Here we review of current knowledge of the application of NIRSth in anesthesia and intensive care.
We performed an analytical and descriptive review of the literature using the terms “near-infrared spectroscopy” combined with “anesthesia,” “anesthesiology,” “intensive care,” “critical care,” “sepsis,” “bleeding,” “hemorrhage,” “surgery,” and “trauma” with particular focus on all NIRS studies involving measurement at the thenar eminence.
We found that NIRSth has been applied as clinical research tool to perform both static and dynamic assessment of StO2. Specifically, a vascular occlusion test (VOT) with a pressure cuff can be used to provide a dynamic assessment of the tissue oxygenation response to ischemia. StO2 changes during such induced ischemia-reperfusion yield information on oxygen consumption and microvasculatory reactivity. Some evidence suggests that StO2 during VOT can detect fluid responsiveness during surgery. In hypovolemic shock, StO2 can help to predict outcome, but not in septic shock. In contrast, NIRS parameters during VOT increase the diagnostic and prognostic accuracy in both hypovolemic and septic shock. Minimal data are available on static or dynamic StO2 used to guide therapy.
Although the available data are promising, further studies are necessary before NIRSth can become part of routine clinical practice.
Similar content being viewed by others
Introduction
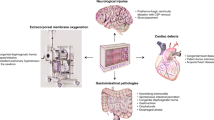
Oxygen delivery (DO2) and consumption (VO2) often are disturbed in critically ill patients [1]. Such disturbance may lead to pathological changes in tissue oxygenation. Thus, monitoring of tissue oxygenation appears desirable. Invasive monitoring of systemic DO2 and VO2 has been used in intensive care medicine for decades [2]. In contrast, no method for assessing tissue oxygenation has yet gained widespread clinical use. This is unfortunate, because tissue oxygenation may reflect changes in the microcirculation, a similarly important target for therapy during major surgery and in the critically ill. Disturbances in microcirculation are common and well documented in hemorrhage and critical illness [3, 4], and they logically relate to tissue oxygenation. Thus, monitoring of tissue oxygenation may provide useful information not only about the state of tissue oxygenation itself but probably about the state of the microcirculation. A potentially useful method to monitor tissue oxygenation may be offered by near infrared spectroscopy (NIRS)-based technology.
Although the concept of NIRS has already been available during the second half of the 20th century, its main initial application was for chemical analysis [5, 6]. Since the end of the 1970s [7], numerous studies have been published about this method [8, 9]. NIRS offers real-time noninvasive monitoring of oxy and deoxyhemoglobin in tissues within a few centimeters from the skin (Figure 1). Furthermore, so-called dynamic values, i.e., values registered during short occlusion of the vascular supply of the area under assessment can be measured. These dynamic values might give additional data on local VO2 and probably the condition of the blood flow of the microcirculation [10]. Some NIRS variables also correlate with invasively monitored central circulatory variables [11]. More recently, due to device development, availability, and marketing, clinical research dealing with the utility of NIRS has focused on the specific methodology of NIRS of the thenar eminence (NIRSth).
Clinical application of NIRSth remains a relatively new method in a field where no “gold standards” exist. Thus, clinicians considering the use of NIRSth need to understand the principles and evidence behind it and appreciate the many areas of uncertainty that surround its application. In this review, we assess several of these aspects and suggest studies to address areas of controversy.
The principle of clinical NIRS is to noninvasively measure the attenuation of light by hemoglobin, where the emitted light is in a wavelength range longer than visible light [12, 13]. NIRS utilizes a narrower spectrum of wavelengths than pulse oximetry, which penetrate deeper into the tissue [14]. Furthermore, whilst NIRS characterizes the total tissue oxy and deoxyhemoglobin in a quantitative and qualitative fashion [13], generating information on oxygen supply and demand, pulse oximetry monitors only hemoglobin in the arterial (pulsatile) part of the local circulation [15].
The near infrared (NIR) light spectrum ranges from 700 nm to 1000 nm. For clinical applications of NIRS, wavelengths approximately 700 to 850 nm are used. The interval stretches on either side of the isobestic point of hemoglobin, i.e., a given wavelength where absorption of light for oxy and deoxyhemoglobin is identical. This wavelength interval maximizes the difference between oxy and deoxyhemoglobin and minimizes the influence of other chromophores, such as myoglobin, cytochrome oxidase, melanin, and bilirubin, on the measurements [16]. Fortunately, the impact of myoglobin on NIRS for measuring tissue oxygenation is minimal [17, 18] and melanin, due to its superficial localization, is not a major issue in this regard. Increased conjugated bilirubin levels do influence measurements by dampening the signal. However, trends can still be followed even with jaundice [19].
Physical background
NIRS technology is based on sophisticated physical models, which are greatly simplified in the description below. The attenuation of light in a sample or tissue is proportional to the pathlength of the light and the absorption coefficient of the chromophore according to the physical principles referred to in the Lambert-Beer law [20]. The absorption coefficient of a compound, in the former equation, is a product of the concentration of the compound and the specific extinction coefficient of the compound. Thus, if attenuation of NIR spectrum light is measured and if all other components of the equation described above are known, the concentration of the chromophore, e.g., oxyhemoglobin can be measured. Unfortunately, because the pathlength of light varies due to reflection and interference in a complex milieu of different tissues, absolute concentrations are difficult to estimate. However, the pathlength of light is more or less constant and the extinction coefficients of the common chromophores are known physical quantities. Thus, changes in attenuation of light will be directly proportional to relative changes in concentration of the chromophore. Absolute changes in concentration can be approximated by creating mathematical algorithms for light pathlength in a tissue.
Because the absorption coefficient is direct proportional to concentrations of a chromophore in a tissue studied and extinction coefficient of the compound is constant, estimating the absorption coefficient yields approximations of the absolute chromophore concentration. This is possible through advanced modeling of the behavior of NIR light in tissues and the technical possibility of measuring at several NIR wavelengths [21]. Yet, given the large number of assumptions and approximations in the theoretical basis of NIRS, one may consider trends in different NIRS parameters as more robust than discrete values.
Technical considerations
The NIRS probes in current use measure reflected light. Thus, the NIR light source is placed beside the light sensor. The distance between the light source and sensor determine the distance from where the main part of the reflected light is measured. The technical limit of the monitored depth is the energy of light that does not damage tissues [21]. The main determinants of signal are small vessels of the microcirculation [22].
The brain [23], kidney [24], lower extremity [25], brachioradialis muscle [26], and thenar eminence [27] are all possible sites for bedside NIRS monitoring. The advantage of the thenar eminence compared with other sites, in terms of minimizing variability, is the relatively thin fat tissue over the muscle. Additionally, fibrous strands in its subcutaneous tissue limit the extent of edema formation providing the best possible setting for muscle tissue saturation (StO2) measurement even in obese and critically ill patients [28]. Due to anatomical conditions, both the brachioradial muscle and the muscles of the thenar eminence can be easily subjected to the vascular obstruction test (see below).
Derived parameters – the vascular occlusion test
Assessing the ratio of oxy and deoxyhemoglobin in the monitored tissue gives continuous StO2. Because absolute hemoglobin content also can be estimated, total tissue hemoglobin and its absolute changes are expressed as tissue hemoglobin index (THI), which can be obtained with this method. THI is, however, not total tissue hemoglobin but its approximation, based on the signal strength of hemoglobin in the monitored area. Low StO2 and THI are common findings in hypovolemic shock states.
By occluding the arterial [16] or the venous [29] blood flow to the thenar eminence, NIRS can assess dynamic changes that reflect VO2 and postischemic reperfusion and hyperemia. This, vascular occlusion test (VOT), is of special interest in septic shock [30, 31] or during anesthesia [32] where the static variables may not be affected despite disturbed circulation.
Arterial and venous vascular occlusion is achieved by a pneumatic cuff on the arm inflated to pressures well above the systolic arterial pressure, aiming to induce ischemia in the thenar muscles and changes in StO2 (Figures 2a,b). Considerable duration of obstruction is required to obtain a reperfusion response that differentiates healthy volunteers from resuscitated septic shock patients [33]. However, the optimal way of performing VOT is a matter of debate. Both the intensity and/or duration of the VOT are a matter of controversy; some authors advocate a time-targeted VOT [34, 35], and others advocate occlusion to a StO2-targeted VOT [33, 36]. The argument for time-targeted VOT is that maximal ischemic vascular response is reached within a few minutes of VOT [37] and that long vascular occlusion times could lead to inability to complete VOT procedure due to subject discomfort [38]. On the other hand, argument for StO2-targeted VOT, i.e., aiming for StO2 of 40%, is that a standardized level of ischemia is achieved, thus interindividual variations in response to VOT giving varying level of ischemia can be minimized.
The rate of desaturation in the thenar muscles (Rdes; % × sec-1) after vascular obstruction can be used to estimate VO2 in the thenar muscles. The product of the absolute value of Rdes and mean THI value quantifies the amount of desaturated hemoglobin [16]. The latter can be converted to thenar VO2 using the hemoglobin-oxygen binding constant [39].
In addition, after cuff deflation there is a swift restoration of blood flow that can be described in terms of the derivate of the StO2 upslope (Rres; % × sec-1). During this reactive hyperemia, the StO2 increases over baseline levels, indicating postischemic vasodilatation and capillary recruitment. The integral of the post reoxygenation StO2 curve over baseline quantifies reactive hyperemia.
The VOT derived variables add to the robustness of NIRS measurements. In a small study, Rdes, Rres, and reactive hyperemia were all lower in septic shock patients than in healthy controls [31]. Moreover, Rres had an inverse relationship to sequential organ failure assessment (SOFA) and predicted mortality. Finally, a coefficient of variation of less than 10% has been reported for Rres [33].
Venous occlusion is performed by inflating a pneumatic cuff above venous pressure on the arm [29]. In this setting, NIRS shows increased THI due to vascular congestion and eventually decreasing StO2. The venous occlusion method also can be used to estimate local VO2. Some have reported varying reproducibility of VO2 measurements with venous occlusion [40].
NIRS during the perioperative period
Although there is an extensive literature on NIRS used before [41], during [42–45] or after surgery [46, 47], relatively little has been published on NIRSth during the perioperative period. However, in a recent publication Rres, measured in patients undergoing major abdominal surgery patients, was decreased in fluid responsive patients [32]. In the same study, fluid responsiveness was detected by invasive methods, such as pulse pressure variation.
Data are conflicting on the ability of NIRSth to detect blood loss, an area of central interest in anesthesia. In awake volunteers, a 500-ml blood loss at blood donation did not lead to changes in NIRS variables [27]. On the other hand, hemodynamically significant hypovolemia, in awake volunteers, did decrease StO2 and THI [48]. A possible explanation could be that tissue hemoglobin and oxygenation at the thenar eminence are not affected by blood loss within the capacity of the compensatory mechanisms of hypovolemia.
In patients after cardiac surgery, StO2 and THI did not correlate with global circulatory parameters, but changes in body-finger temperature correlated with changes in StO2 [49]. However, StO2 during the perioperative period in cardiac surgery is lower in patients who develop certain postoperative complications [50] than those who do not [51]. StO2 at the thenar eminence does not predict mortality in cardiac surgery [51] or surgical-site infections in colon surgery [52].
Intensive care applications
In a general intensive care population with most patients in resuscitated shock, StO2 and Rres appear related to capillary refill time and central to peripheral temperature gradient, but not to the etiology of shock [53]. In a mixed group of patients with increased blood lactate levels observed during 8 hours of resuscitation [54], half had low StO2 (<70%) on admission. There was no difference in systemic circulatory variables between patients with low or normal StO2, but SOFA scores and acute physiology and chronic health evaluation II scores were higher in patients with decreased StO2. However, blood transfusion substantially increasing blood hemoglobin did not increase StO2 in a mixed group of stable patients [55] and the correlation between blood hemoglobin and tissue hemoglobin index may be limited [31, 55]. In patients with hypovolemic or septic patients, more homogenous observations have been described.
NIRS in hypovolemic shock
The rationale for monitoring peripheral tissue as the thenar eminence in hypovolemic shock is centralization of circulation to vital organs leading to decreased blood flow in muscles [56]. In acute hemorrhage, activation of the sympathetic nervous system [57] should decrease thenar muscles blood flow, with increased oxygen extraction and decreased tissue hemoglobin content. In this setting, NIRSth may thus act as a sensor of the vascular response to hypovolemia. In trauma patients with severe shock, StO2 is lower in than in milder grades of shock or in normal individuals [58], although patients with shock can present with StO2 values as in controls [38].
In a study of severe postpartum hemorrhage, the StO2 range overlapped during and after hemorrhage, but StO2 increased after control of bleeding [59]. The lowest StO2 in the trauma bay has been shown to be as good as the lowest systolic blood pressure at identifying severe shock as defined by experienced clinicians [58]. Furthermore, StO2 within 1 hour of admission is lower in trauma patients who develop multiorgan dysfunction (MODS) or die, and a strongest predictor of MODS or death than other diagnostic modalities [60, 61]. Low StO2 within 1 hour of admission was as sensitive as a high base deficit in identifying patients who developed MODS or died, although specificity for both was low [62]. Finally, low StO2 within 1 hour of admission identifies trauma patients who will require blood transfusion within the next 24 hours [63].
The discriminatory power of dynamic NIRS parameters, however, is of greater interest. Rres was lower in trauma patients compared with controls with little overlap [38]. Moreover, low Rres predicted increased troponin I levels in postpartum bleeding [59]. Thus, in hypovolemia, low static StO2 predict adverse outcome but dynamic NIRS parameters seem to be more promising.
NIRS in sepsis
In septic shock, although hypovolemia can be a finding [64], there is a substantial microcirculatory disturbance with closed capillaries, arteriovenous shunting, and decreased flow [65]. As a result of these phenomena, oxygen content in the vessels of the microcirculation could be normal, making clinical interpretation of NIRS data complex. These pathophysiologic changes may be not necessarily mirrored by low StO2, but rather by low Rres and impaired postischemic hyperemic response.
Several studies report a difference in StO2 between healthy subjects and patients with severe sepsis or septic shock [16, 30, 34, 66, 67], whereas others do not [31, 68, 69]. Although variation in population characteristics could partly explain these results, in all studies StO2 values overlap between septic shock patients and healthy volunteers. This is not surprising because, in sepsis, StO2 in sepsis can be at the higher end of the normal spectrum or markedly low [65]. Dynamic NIRS parameters, however, improve the power of the method to distinguish pathologic tissue oxygenation from normal. The Rdes of the thenar muscles is slower in septic shock patients, indicating a lower rate of tissue VO2 [16, 31, 68, 69]. Furthermore, Rdes varies with the severity of systemic infections [69]. Similarly, Rres appears lower in septic patients compared with healthy controls [16, 30, 31, 34, 70] and decreases with increasing disease severity [30, 31]. Rres ranges overlap minimally [30, 68, 70] or not at all [34] when comparing healthy controls and septic patients, and Rres improves as septic shock resolves [34]. Finally postischemic hyperemia is decreased in septic patients compared with healthy controls [30, 31]. Thus, NIRSth could be a method for bedside assessment of the microcirculation [71].
Monitoring global hemodynamics with NIRSth also has attracted interest. In sepsis, treatment based on venous saturation in the superior vena cava (ScvO2) [64] or the pulmonary artery (SvO2) [72] is used, because these are markers of global DO2 and VO2 balance [73]. Noninvasively obtained surrogates of ScvO2 or SvO2 would be valuable. In this regard, StO2 correlates to ScvO2 [74] and SvO2 [67] in patients with severe sepsis or septic shock; however, correlation coefficients are relatively low. The accuracy of estimating SvO2 could be substantially improved by calculating the “NIRS-derived SvO2” [67]. In severe sepsis and severe heart failure, StO2, however, did not estimate SvO2 [75]. Still, data suggest that patients with severe sepsis or septic shock and low StO2 also have low ScvO2, suggesting hypodynamic circulation [74].
Variables related to DO2 may correlate with NIRS parameters. Rres correlates with cardiac output and to a lesser extent with blood lactate levels in septic patients [34], whereas StO2 does not correlate with lactate or base deficit [67]. A low StO2 predicts a very low DO2 in early sepsis with high sensitivity and specificity [76]; however, moderately low DO2 does not correlate with StO2. Neither was change in Rres correlated to change in cardiac output in septic patients. Finally, StO2 did not correlate with the severity of illness [67], but a StO2 <78% in resuscitated patients predicted mortality [77]. Low Rres correlates with organ failure [31] and Rres is lower in nonsurvivors than survivors [34].
Recently, it has been reported that increasing blood pressure with noradrenalin infusion from 65 mmHg to 85 mmHg in resuscitated sepsis patients normalized Rres [78]. These patients, although seemingly resuscitated according to the Surviving Sepsis Campaign guidelines, could improve the thenar perfusion by achieving higher mean arterial pressure [79]. These data could suggest that NIRS can identify patients who benefit from treatment beyond the traditional goals, thus the usefulness of NIRS as a bedside tool to optimize tissue oxygenation [71]. Thus, in resuscitated, septic patients, dynamic NIRS of the thenar eminence provides information on microcirculation and trends could be used to guide treatment.
NIRS in miscellaneous conditions
In patients with chronic heart failure, thenar StO2, Rdes, and Rres are low [80]. NIRSth parameters in these patients improved after 6 hours of dobutamine or levosimendan infusion [80], or 3 months of regular exercise training [81]. Patients with cirrhosis demonstrated a supranormal hyperemic response after vascular occlusion test [82], which increases with increasing severity of liver disease [82].
NIRS-derived and central hemodynamic parameters
The performance of NIRSth in estimating global circulatory parameters is highly dependent on the coupling between the circulation of the hand and the central circulation. Static NIRS parameters, such as StO2, should, in theory, be related to centrally measured circulatory parameters. However, this relationship has not been demonstrated in general in critically ill patients [54] or after cardiac surgery [49]. Although, global venous saturations have been described to correlate to StO2 in sepsis, this relationship is weak [67, 74, 83]. In sepsis, correlation between StO2 and SvO2 can be improved with correction equations [67]. Only substantial deviations from normal DO2 levels are detected reliably by StO2 in sepsis [76]. In these patients, Rres correlates with cardiac index and blood lactate levels [34].
Low StO2 also predicts MODS in a mixed population of critically ill patients [54], in trauma patients [60–62], and in postcardiac surgery patients [51]. In sepsis, dynamic NIRS variables, such as Rdes [69] and Rres [31, 34], have been associated with organ failure.
Limitations
NIRSth monitors peripheral muscle as a marker of perfusion elsewhere. The theoretical concern is whether the small volume of distal muscle can be a good indicator of the state of the tissue oxygenation in the rest of the body and the vital organs. For example, local factors, such as obstruction to flow by atherosclerosis, an arterial catheter, or thrombosis after previous arterial catheterization, could affect measurement. Although a brief report suggests that catheterization of the radial artery in adult, elective, surgical patients does not affect StO2 [84], this may not be the case in critically ill patients with circulatory failure.
StO2 is not the same as tissue blood flow in the tissue or even oxygen supply. StO2 is affected by local VO2, which could be affected by states that alter muscle metabolism, such as muscle relaxants. The balance between the metabolic state of the muscle and other vital organs may vary between individuals and intraindividually during the course of disease, affecting the global relevance of some of the NIRS variables. Also tissues overlaying the thenar muscles can influence measurements [85]. Very dark skin with high melanin content or thick, edematous, or injured connective tissues and low hemoglobin levels also could pose problems with NIRS measurements [86].
There are many studies on NIRS in the perioperative period and critical illness where many different sites are monitored. Moreover, the methodology of NIRS is not standardized [87, 88]. Several probes are available on the market, different occlusion protocols are used, and different parts of downslope and the upslope StO2 curves at vascular occlusion are used in calculations. Furthermore, studies are conducted on patients in different phases of disease, which may represent different pathophysiologic situations. Hence, comparing results can be difficult (Table 1).
Static NIRS variables are influenced by the temperature of the hands compared with core temperature [53] and could be a reason for the overlap between patients with normal and abnormal peripheral circulation. In anesthesia with volatile anaesthetics, vasodilatation is a common feature [89] and monitoring StO2 would be expected to be less affected by peripheral vascular tone.
The question of whether organ failure in sepsis is mostly dependent on disturbed mitochondrial oxygen metabolism [90–92], or on limited DO2 [93, 94], is a matter of debate. NIRS does not assess mitochondrial oxygen metabolism in sepsis, although decreased tissue VO2, Rdes, could imply mitochondrial dysfunction. However, decreased tissue VO2 also could depend on shunting of delivered oxygen [65]. This phenomenon is not measured by NIRS either. However, with all of its limitations, NIRSth is a noninvasive method that, given that supporting data will be available, could become part of anesthetic and intensive care monitoring in a manner similar to pulse oximetry.
Conclusions NIRSth eminence estimates StO2 in peripheral muscles. In hypovolemia, such StO2 is decreased and relates to severity of disease and outcome. Hence, StO2 measurements could aid with the clinical management of these patients. In unresuscitated or inadequately resuscitated septic shock, Rdes and Rres are decreased, indicating disturbed tissue oxygen metabolism and microvascular reserve. The pathologic findings in these dynamic NIRS parameters could be of value in resuscitated sepsis where macrocirculatory failure has been corrected and during anesthesia to monitor adequacy of peripheral perfusion and fluid status. Despite its limitations, NIRSth takes monitoring from global to local level. The existing literature on NIRSth is mainly focused on validation of this technique. Future studies that implement NIRSth into treatment algorithms in anesthesia and intensive care would be valuable to define the place for this monitoring modality in daily management of critically ill patients.
References
Seymour CW, Kahn JM, Cooke CR, Watkins TR, Heckbert SR, Rea TD: Prediction of critical illness during out-of-hospital emergency care. JAMA 2010, 304: 747–754. 10.1001/jama.2010.1140
Forrester JS, Ganz W, Diamond G, McHugh T, Chonette DW, Swan HJ: Thermodilution cardiac output determination with a single flow-directed catheter. Am Heart J 1972, 83: 306–311. 10.1016/0002-8703(72)90429-2
Hungerer S, Nolte D, Botzlar A, Messmer K: Effects of Diaspirin Crosslinked Hemoglobin (DCLHb) on microcirculation and local tissue pO2of striated skin muscle following resuscitation from hemorrhagic shock. Artif Cell Blood Substit Biotechnol 2006, 34: 455–471. 10.1080/10731190600769008
Trzeciak S, Dellinger RP, Parrillo JE, Guglielmi M, Bajaj J, Abate NL, Arnold RC, Colilla S, Zanotti S, Hollenberg SM, et al.: Early microcirculatory perfusion derangements in patients with severe sepsis and septic shock: relationship to hemodynamics, oxygen transport, and survival. Ann Emerg Med 2007, 49: 88–98. 98 e81–82 10.1016/j.annemergmed.2006.08.021
Borchman D, Yappert MC, Herrell P: Structural characterization of human lens membrane lipid by infrared spectroscopy. Invest Ophthalmol Vis Sci 1991, 32: 2404–2416.
Metsala M, Schmidt FM, Skytta M, Vaittinen O, Halonen L: Acetylene in breath: background levels and real-time elimination kinetics after smoking. J Breath Res 2010, 4: 046003. 10.1088/1752-7155/4/4/046003
Jobsis FF: Noninvasive, infrared monitoring of cerebral and myocardial oxygen sufficiency and circulatory parameters. Science 1977, 198: 1264–1267. 10.1126/science.929199
Taillefer MC, Denault AY: Cerebral near-infrared spectroscopy in adult heart surgery: systematic review of its clinical efficacy. Can J Anaesth 2005, 52: 79–87. 10.1007/BF03018586
Santora RJ, Moore FA: Monitoring trauma and intensive care unit resuscitation with tissue hemoglobin oxygen saturation. Crit Care 2009,13(Suppl 5):S10. 10.1186/cc8008
Bartels SA, Bezemer R, Milstein DM, Radder M, Lima A, Cherpanath TG, Heger M, Karemaker JM, Ince C: The microcirculatory response to compensated hypovolemia in a lower body negative pressure model. Microvasc Res 2011, 82: 374–380. 10.1016/j.mvr.2011.07.010
Mozina H, Podbregar M: Near-infrared spectroscopy during stagnant ischemia estimates central venous oxygen saturation and mixed venous oxygen saturation discrepancy in patients with severe left heart failure and additional sepsis/septic shock. Crit Care 2010, 14: R42. 10.1186/cc8929
Wariar R, Gaffke JN, Haller RG, Bertocci LA: A modular NIRS system for clinical measurement of impaired skeletal muscle oxygenation. J Appl Physiol 2000, 88: 315–325.
Wahr JA, Tremper KK, Samra S, Delpy DT: Near-infrared spectroscopy: theory and applications. J Cardiothorac Vasc Anesth 1996, 10: 406–418. 10.1016/S1053-0770(96)80107-8
McMorrow RC, Mythen MG: Pulse oximetry. Curr Opin Crit Care 2006, 12: 269–271.
Sinex JE: Pulse oximetry: principles and limitations. Am J Emerg Med 1999, 17: 59–67. 10.1016/S0735-6757(99)90019-0
Skarda DE, Mulier KE, Myers DE, Taylor JH, Beilman GJ: Dynamic near-infrared spectroscopy measurements in patients with severe sepsis. Shock 2007, 27: 348–353. 10.1097/01.shk.0000239779.25775.e4
Seiyama A, Hazeki O, Tamura M: Noninvasive quantitative analysis of blood oxygenation in rat skeletal muscle. J Biochem 1988, 103: 419–424.
Mancini DM, Bolinger L, Li H, Kendrick K, Chance B, Wilson JR: Validation of near-infrared spectroscopy in humans. J Appl Physiol 1994, 77: 2740–2747.
Madsen PL, Skak C, Rasmussen A, Secher NH: Interference of cerebral near-infrared oximetry in patients with icterus. Anesth Analg 2000, 90: 489–493.
Uludag K, Kohl M, Steinbrink J, Obrig H, Villringer A: Cross talk in the Lambert-Beer calculation for near-infrared wavelengths estimated by Monte Carlo simulations. J Biomed Opt 2002, 7: 51–59. 10.1117/1.1427048
Murkin JM, Arango M: Near-infrared spectroscopy as an index of brain and tissue oxygenation. Br J Anaesth 2009,103(Suppl 1):i3-i13.
Creteur J: Muscle StO2 in critically ill patients. Curr Opin Crit Care 2008, 14: 361–366. 10.1097/MCC.0b013e3282fad4e1
Wolf M, Ferrari M, Quaresima V: Progress of near-infrared spectroscopy and topography for brain and muscle clinical applications. J Biomed Opt 2007, 12: 062104. 10.1117/1.2804899
Owens GE, King K, Gurney JG, Charpie JR: Low renal oximetry correlates with acute kidney injury after infant cardiac surgery. Pediatr Cardiol 2011, 32: 183–188. 10.1007/s00246-010-9839-x
Shuler MS, Reisman WM, Kinsey TL, Whitesides TE Jr, Hammerberg EM, Davila MG, Moore TJ: Correlation between muscle oxygenation and compartment pressures in acute compartment syndrome of the leg. J Bone Joint Surg Am 2010, 92: 863–870. 10.2106/JBJS.I.00816
Rodriguez A, Lisboa T, Martin-Loeches I, Diaz E, Trefler S, Restrepo MI, Rello J: Mortality and Regional Oxygen Saturation Index in Septic Shock Patients: A Pilot Study. J Trauma 2011, 70: 1145–1152. 10.1097/TA.0b013e318216f72c
Jeger V, Jakob SM, Fontana S, Wolf M, Zimmermann H, Exadaktylos AK: 500 ml of blood loss does not decrease non-invasive tissue oxygen saturation (StO2) as measured by near infrared spectroscopy - A hypothesis generating pilot study in healthy adult women. J Trauma Manag Outcomes 2010, 4: 5. 10.1186/1752-2897-4-5
Poeze M: Tissue-oxygenation assessment using near-infrared spectroscopy during severe sepsis: confounding effects of tissue edema on StO2 values. Intensive Care Med 2006, 32: 788–789. 10.1007/s00134-006-0121-x
Girardis M, Rinaldi L, Busani S, Flore I, Mauro S, Pasetto A: Muscle perfusion and oxygen consumption by near-infrared spectroscopy in septic-shock and non-septic-shock patients. Intensive Care Med 2003, 29: 1173–1176. 10.1007/s00134-003-1805-0
Creteur J, Carollo T, Soldati G, Buchele G, De Backer D, Vincent JL: The prognostic value of muscle StO2 in septic patients. Intensive Care Med 2007, 33: 1549–1556. 10.1007/s00134-007-0739-3
Doerschug KC, Delsing AS, Schmidt GA, Haynes WG: Impairments in microvascular reactivity are related to organ failure in human sepsis. Am J Physiol Heart Circ Physiol 2007, 293: H1065-H1071. 10.1152/ajpheart.01237.2006
Futier E, Christophe S, Robin E, Petit A, Pereira B, Desbordes J, Bazin JE, Vallet B: Use of near-infrared spectroscopy during a vascular occlusion test to assess the microcirculatory response during fluid challenge. Crit Care 2011, 15: R214. 10.1186/cc10449
Mayeur C, Campard S, Richard C, Teboul JL: Comparison of four different vascular occlusion tests for assessing reactive hyperemia using near-infrared spectroscopy. Crit Care Med 2011, 39: 695–701. 10.1097/CCM.0b013e318206d256
Payen D, Luengo C, Heyer L, Resche-Rigon M, Kerever S, Damoisel C, Losser MR: Is thenar tissue hemoglobin oxygen saturation in septic shock related to macrohemodynamic variables and outcome? Crit Care 2009,13(Suppl 5):S6. 10.1186/cc8004
Damoisel C, Payen D: Vascular occlusion tests: Do we need another definition? Crit Care Med 2011, 39: 2587–2588.
Mayeur C, Teboul JL: Vascular occlusion tests: Do we need another definition? Crit Care Med 2011, 39: 2588–2589. 10.1097/CCM.0b013e3182326456
Farnebo S, Thorfinn J, Henricson J, Tesselaar E: Hyperaemic changes in forearm skin perfusion and RBC concentration after increasing occlusion times. Microvasc Res 2010, 80: 412–416. 10.1016/j.mvr.2010.07.008
Gomez H, Torres A, Polanco P, Kim HK, Zenker S, Puyana JC, Pinsky MR: Use of non-invasive NIRS during a vascular occlusion test to assess dynamic tissue O2saturation response. Intensive Care Med 2008, 34: 1600–1607. 10.1007/s00134-008-1145-1
McGee WT, Mailloux P, Jodka P, Thomas J: The pulmonary artery catheter in critical care. Semin Dial 2006, 19: 480–491. 10.1111/j.1525-139X.2006.00210.x
Van Beekvelt MC, Colier WN, Wevers RA, Van Engelen BG: Performance of near-infrared spectroscopy in measuring local O2consumption and blood flow in skeletal muscle. J Appl Physiol 2001, 90: 511–519.
Bundgaard-Nielsen M, Ruhnau B, Secher NH, Kehlet H: Flow-related techniques for preoperative goal-directed fluid optimization. Br J Anaesth 2007, 98: 38–44.
Sako H, Hadama T, Miyamoto S, Anai H, Wada T, Iwata E, Hamamoto H, Tanaka H, Urushino K, Shuto T: Effect of prostaglandin E1 on ischemia-reperfusion injury during abdominal aortic aneurysm surgery. Surg Today 2006, 36: 140–146. 10.1007/s00595-005-3116-2
Schoen J, Husemann L, Tiemeyer C, Lueloh A, Sedemund-Adib B, Berger KU, Hueppe M, Heringlake M: Cognitive function after sevoflurane- vs propofol-based anaesthesia for on-pump cardiac surgery: a randomized controlled trial. Br J Anaesth 2011, 106: 840–850. 10.1093/bja/aer091
Kwak HJ, Lee D, Lee YW, Yu GY, Shinn HK, Kim JY: The intermittent sequential compression device on the lower extremities attenuates the decrease in regional cerebral oxygen saturation during sitting position under sevoflurane anesthesia. J Neurosurg Anesthesiol 2011, 23: 1–5. 10.1097/ANA.0b013e3181e97a5e
Hirano Y, Omura K, Tatsuzawa Y, Shimizu J, Kawaura Y, Watanabe G: Tissue oxygen saturation during colorectal surgery measured by near-infrared spectroscopy: pilot study to predict anastomotic complications. World J Surg 2006, 30: 457–461. 10.1007/s00268-005-0271-y
Mutoh T, Ishikawa T, Suzuki A, Yasui N: Continuous cardiac output and near-infrared spectroscopy monitoring to assist in management of symptomatic cerebral vasospasm after subarachnoid hemorrhage. Neurocrit Care 2010, 13: 331–338. 10.1007/s12028-010-9383-9
Kahraman S, Kayali H, Atabey C, Acar F, Gocmen S: The accuracy of near-infrared spectroscopy in detection of subdural and epidural hematomas. J Trauma 2006, 61: 1480–1483. 10.1097/01.ta.0000197616.10279.48
Bartels SA, Bezemer R, de Vries FJ, Milstein DM, Lima A, Cherpanath TG, van den Meiracker AH, van Bommel J, Heger M, Karemaker JM, Ince C: Multi-site and multi-depth near-infrared spectroscopy in a model of simulated (central) hypovolemia: lower body negative pressure. Intensive Care Med 2011, 37: 671–677. 10.1007/s00134-010-2128-6
Uilkema RJ, Groeneveld AB: Correlates of thenar near-infrared spectroscopy-derived tissue O2 saturation after cardiac surgery. Interact Cardiovasc Thorac Surg 2007, 6: 265–269. 10.1510/icvts.2006.149658
Bennett-Guerrero E, Welsby I, Dunn TJ, Young LR, Wahl TA, Diers TL, Phillips-Bute BG, Newman MF, Mythen MG: The use of a postoperative morbidity survey to evaluate patients with prolonged hospitalization after routine, moderate-risk, elective surgery. Anesth Analg 1999, 89: 514–519.
Sanders J, Toor IS, Yurik TM, Keogh BE, Mythen M, Montgomery HE: Tissue oxygen saturation and outcome after cardiac surgery. Am J Crit Care 2011, 20: 138–145. 10.4037/ajcc2011739
Govinda R, Kasuya Y, Bala E, Mahboobi R, Devarajan J, Sessler DI, Akca O: Early postoperative subcutaneous tissue oxygen predicts surgical site infection. Anesth Analg 2010, 111: 946–952.
Lima A, van Bommel J, Sikorska K, van Genderen M, Klijn E, Lesaffre E, Ince C, Bakker J: The relation of near-infrared spectroscopy with changes in peripheral circulation in critically ill patients. Crit Care Med 2011, 39: 1649–1654. 10.1097/CCM.0b013e3182186675
Lima A, van Bommel J, Jansen TC, Ince C, Bakker J: Low tissue oxygen saturation at the end of early goal-directed therapy is associated with worse outcome in critically ill patients. Crit Care 2009,13(Suppl 5):S13. 10.1186/cc8011
Creteur J, Neves AP, Vincent JL: Near-infrared spectroscopy technique to evaluate the effects of red blood cell transfusion on tissue oxygenation. Crit Care 2009,13(Suppl 5):S11. 10.1186/cc8009
McKinley BA, Parmley CL, Butler BD: Skeletal muscle PO2, PCO2, and pH in hemorrhage, shock, and resuscitation in dogs. J Trauma 1998, 44: 119–127. 10.1097/00005373-199801000-00015
Bonanno FG: Physiopathology of shock. J Emerg Trauma Shock 2011, 4: 222–232. 10.4103/0974-2700.82210
Crookes BA, Cohn SM, Bloch S, Amortegui J, Manning R, Li P, Proctor MS, Hallal A, Blackbourne LH, Benjamin R, et al.: Can near-infrared spectroscopy identify the severity of shock in trauma patients? J Trauma 2005, 58: 806–813. discussion 813–806 10.1097/01.TA.0000158269.68409.1C
Heyer L, Mebazaa A, Gayat E, Resche-Rigon M, Rabuel C, Rezlan E, Lukascewicz AC, Madadaki C, Pirracchio R, Schurando P, et al.: Cardiac troponin and skeletal muscle oxygenation in severe post-partum haemorrhage. Crit Care 2009,13(Suppl 5):S8. 10.1186/cc8006
Beilman GJ, Blondet JJ, Nelson TR, Nathens AB, Moore FA, Rhee P, Puyana JC, Moore EE, Cohn SM: Early hypothermia in severely injured trauma patients is a significant risk factor for multiple organ dysfunction syndrome but not mortality. Ann Surg 2009, 249: 845–850. 10.1097/SLA.0b013e3181a41f6f
Moore FA, Nelson T, McKinley BA, Moore EE, Nathens AB, Rhee P, Puyana JC, Beilman GJ, Cohn SM: Massive transfusion in trauma patients: tissue hemoglobin oxygen saturation predicts poor outcome. J Trauma 2008, 64: 1010–1023. 10.1097/TA.0b013e31816a2417
Cohn SM, Nathens AB, Moore FA, Rhee P, Puyana JC, Moore EE, Beilman GJ: Tissue oxygen saturation predicts the development of organ dysfunction during traumatic shock resuscitation. J Trauma 2007, 62: 44–54. discussion 54–45 10.1097/TA.0b013e31802eb817
Smith J, Bricker S, Putnam B: Tissue oxygen saturation predicts the need for early blood transfusion in trauma patients. Am Surg 2008, 74: 1006–1011.
Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M: Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 2001, 345: 1368–1377. 10.1056/NEJMoa010307
De Backer D, Ospina-Tascon G, Salgado D, Favory R, Creteur J, Vincent JL: Monitoring the microcirculation in the critically ill patient: current methods and future approaches. Intensive Care Med 2010, 36: 1813–1825. 10.1007/s00134-010-2005-3
De Backer D, Ospina-Tascon G, Salgado D, Favory R, Creteur J, Vincent JL: Monitoring the microcirculation in the critically ill patient: current methods and future approaches. Intensive Care Med 2010, 36: 1813–1825. 10.1007/s00134-010-2005-3
Mulier KE, Skarda DE, Taylor JH, Myers DE, McGraw MK, Gallea BL, Beilman GJ: Near-infrared spectroscopy in patients with severe sepsis: correlation with invasive hemodynamic measurements. Surg Infect (Larchmt) 2008, 9: 515–519. 10.1089/sur.2007.091
Nanas S, Gerovasili V, Renieris P, Angelopoulos E, Poriazi M, Kritikos K, Siafaka A, Baraboutis I, Zervakis D, Markaki V, et al.: Non-invasive assessment of the microcirculation in critically ill patients. Anaesth Intensive Care 2009, 37: 733–739.
Pareznik R, Knezevic R, Voga G, Podbregar M: Changes in muscle tissue oxygenation during stagnant ischemia in septic patients. Intensive Care Med 2006, 32: 87–92. 10.1007/s00134-005-2841-8
Georger JF, Hamzaoui O, Chaari A, Maizel J, Richard C, Teboul JL: Restoring arterial pressure with norepinephrine improves muscle tissue oxygenation assessed by near-infrared spectroscopy in severely hypotensive septic patients. Intensive Care Med 2010, 36: 1882–1889. 10.1007/s00134-010-2013-3
Silva S, Teboul JL: Defining the adequate arterial pressure target during septic shock: not a 'micro' issue but the microcirculation can help. Crit Care 2011, 15: 1004. 10.1186/cc10486
Velissaris D, Pierrakos C, Scolletta S, De Backer D, Vincent JL: High mixed venous oxygen saturation levels do not exclude fluid responsiveness in critically ill septic patients. Crit Care 2011, 15: R177.
Baele PL, McMichan JC, Marsh HM, Sill JC, Southorn PA: Continuous monitoring of mixed venous oxygen saturation in critically ill patients. Anesth Analg 1982, 61: 513–517.
Mesquida J, Masip J, Gili G, Artigas A, Baigorri F: Thenar oxygen saturation measured by near infrared spectroscopy as a noninvasive predictor of low central venous oxygen saturation in septic patients. Intensive Care Med 2009, 35: 1106–1109. 10.1007/s00134-009-1410-y
Podbregar M, Mozina H: Skeletal muscle oxygen saturation does not estimate mixed venous oxygen saturation in patients with severe left heart failure and additional severe sepsis or septic shock. Crit Care 2007, 11: R6. 10.1186/cc5153
Mesquida J, Gruartmoner G, Martinez ML, Masip J, Sabatier C, Espinal C, Artigas A, Baigorri F: Thenar oxygen saturation and invasive oxygen delivery measurements in critically ill patients in early septic shock. Shock 2011, 35: 456–459. 10.1097/SHK.0b013e3182094ab9
Leone M, Blidi S, Antonini F, Meyssignac B, Bordon S, Garcin F, Charvet A, Blasco V, Albanese J, Martin C: Oxygen tissue saturation is lower in nonsurvivors than in survivors after early resuscitation of septic shock. Anesthesiology 2009, 111: 366–371. 10.1097/ALN.0b013e3181aae72d
Thooft A, Favory R, Salgado DR, Taccone FS, Donadello K, De Backer D, Creteur J, Vincent JL: Effects of changes in arterial pressure on organ perfusion during septic shock. Crit Care 2011, 15: R222. 10.1186/cc10462
Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R, Reinhart K, Angus DC, Brun-Buisson C, Beale R, et al.: Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med 2008, 36: 296–327. 10.1097/01.CCM.0000298158.12101.41
Nanas S, Gerovasili V, Dimopoulos S, Pierrakos C, Kourtidou S, Kaldara E, Sarafoglou S, Venetsanakos J, Roussos C, Nanas J, Anastasiou-Nana M: Inotropic agents improve the peripheral microcirculation of patients with end-stage chronic heart failure. J Card Fail 2008, 14: 400–406. 10.1016/j.cardfail.2008.02.001
Gerovasili V, Drakos S, Kravari M, Malliaras K, Karatzanos E, Dimopoulos S, Tasoulis A, Anastasiou-Nana M, Roussos C, Nanas S: Physical exercise improves the peripheral microcirculation of patients with chronic heart failure. J Cardiopulm Rehabil Prev 2009, 29: 385–391.
Thomson SJ, Cowan ML, Forton DM, Clark SJ, Musa S, Grounds M, Rahman TM: A study of muscle tissue oxygenation and peripheral microcirculatory dysfunction in cirrhosis using near infrared spectroscopy. Liver Int 2010, 30: 463–471. 10.1111/j.1478-3231.2009.02157.x
Napoli AM, Machan JT, Forcada A, Corl K, Gardiner F: Tissue oxygenation does not predict central venous oxygenation in emergency department patients with severe sepsis and septic shock. Acad Emerg Med 2010, 17: 349–352.
Lopez PP, Jonas RB, Muir MT, Cohn SM: The impact of radial artery catheterization on thenar muscle tissue oxygen monitoring. J Trauma 2009, 67: 895.
van Beekvelt MC, Borghuis MS, van Engelen BG, Wevers RA, Colier WN: Adipose tissue thickness affects in vivo quantitative near-IR spectroscopy in human skeletal muscle. Clin Sci (Lond) 2001, 101: 21–28. 10.1042/CS20000247
Kurth CD, Thayer WS: A multiwavelength frequency-domain near-infrared cerebral oximeter. Phys Med Biol 1999, 44: 727–740. 10.1088/0031-9155/44/3/015
Bezemer R, Lima A, Myers D, Klijn E, Heger M, Goedhart PT, Bakker J, Ince C: Assessment of tissue oxygen saturation during a vascular occlusion test using near-infrared spectroscopy: the role of probe spacing and measurement site studied in healthy volunteers. Crit Care 2009,13(Suppl 5):S4. 10.1186/cc8002
Gomez H, Mesquida J, Simon P, Kim HK, Puyana JC, Ince C, Pinsky MR: Characterization of tissue oxygen saturation and the vascular occlusion test: influence of measurement sites, probe sizes and deflation thresholds. Crit Care 2009,13(Suppl 5):S3. 10.1186/cc8001
Dahlgren G, Ohqvist G, Brodin LA, Fischerstrom A, Settergren G: Isoflurane and intravenous anesthesia used for induction before coronary artery bypass grafting. Acta Anaesthesiol Scand 1989, 33: 99–104. 10.1111/j.1399-6576.1989.tb02869.x
Harrois A, Huet O, Duranteau J: Alterations of mitochondrial function in sepsis and critical illness. Curr Opin Anaesthesiol 2009, 22: 143–149. 10.1097/ACO.0b013e328328d1cc
Fink MP: Cytopathic hypoxia. Is oxygen use impaired in sepsis as a result of an acquired intrinsic derangement in cellular respiration? Crit Care Clin 2002, 18: 165–175. 10.1016/S0749-0704(03)00071-X
Brealey D, Singer M: Mitochondrial dysfunction in sepsis. Curr Infect Dis Rep 2003, 5: 365–371. 10.1007/s11908-003-0015-9
Ince C: The microcirculation is the motor of sepsis. Crit Care 2005,9(Suppl 4):S13-S19. 10.1186/cc3753
Trzeciak S, Dellinger RP, Parrillo JE, Guglielmi M, Bajaj J, Abate NL, Arnold RC, Colilla S, Zanotti S, Hollenberg SM: Early microcirculatory perfusion derangements in patients with severe sepsis and septic shock: relationship to hemodynamics, oxygen transport, and survival. Ann Emerg Med 2007, 49: 88–98. 98 e81–82 10.1016/j.annemergmed.2006.08.021
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors contributions
All authors conceived the manuscript. Both ML and NCZW reviewed the literature. ML wrote the first draft. RB reviewed and refined the first draft. Further drafts were completed by ML, RB and NCZW. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Lipcsey, M., Woinarski, N.C. & Bellomo, R. Near infrared spectroscopy (NIRS) of the thenar eminence in anesthesia and intensive care. Ann. Intensive Care 2, 11 (2012). https://doi.org/10.1186/2110-5820-2-11
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/2110-5820-2-11