Abstract
The literature for evidence of autoimmunity in multiple sclerosis (MS) is analysed critically. In contrast to the accepted theory, the human counterpart of the animal model experimental autoimmune demyelinating disease, experimental allergic encephalomyelitis (EAE), is not MS but a different demyelinating disorder, i.e. acute disseminated encephalomyelitis and acute haemorrhagic leucoencephalitis. Extrapolation of EAE research to MS has been guided largely by faith and a blind acceptance rather than sound, scientific rationale. No specific or sensitive immunological test exists that is diagnostic of MS despite the extensive application of modern technology. Immunosuppression has failed to have any consistent effect on prognosis or disease progression. The available data on MS immunotherapy are conflicting, at times contradictory and are based on findings in animals with EAE. They show predominantly a 30% effect in relapsing/remitting MS which suggests powerful placebo effect. Critical analysis of the epidemiological data shows no association with any specific autoimmune diseases, but does suggest that geographic factors and age at development posit an early onset possibly dependent on environmental influences. Certain neurological diseases are, however, found in association with MS, namely hypertrophic peripheral neuropathy, neurofibromatosis-1, cerebral glioma, glioblastoma multiforme and certain familial forms of narcolepsy. These share a common genetic influence possibly from genes on chromosome 17 affecting cell proliferation. A significant number of these disorders are of neural crest origin, the classical example being abnormalities of the Schwann cell. These and other data allow us to propose that MS is a developmental neural crest disorder, i.e. a cristopathy, implicating glial cell dysfunction with diffuse blood–brain barrier breakdown. The data on transcription factor SOX10 mutations in animals may explain these bizarre clinical associations with MS and the phenotypic variability of such alterations (Cossais et al. 2010). Research directed to the area of neural crest associations is likely to be rewarding.
Similar content being viewed by others
“If a man is offered a fact which goes against his instincts, he will scrutinize it closely, and unless the evidence is overwhelming, he will refuse to believe it. If, on the other hand, he is offered something which affords a reason for acting in accordance to his instincts, he will accept it even on the slightest evidence. The origin of myths is explained in this way.”
Bertrand Russell (Roads to Freedom, 1970, p. 116, Routledge)
Introduction
The cause of MS is unknown as is the exact pathogenesis of the disorder (Noseworthy 1999). This point needs to be stressed as there is a common, recurring statement in a vast proportion of the literature on MS that it is of autoimmune aetiology. Multiple sclerosis (MS) is clinically a heterogeneous condition and to date still defies both clinical and exact definition (Steiner and Wirguin 2000). Sadly, these factors may be responsible for the minimal progress that has been made towards understanding its aetiology and pathogenesis or in developing a rational mode of therapy. At present, two main theories are proffered as to its causation, namely that it may be due to a viral infection, or to a viral infection which initiates autoimmune mechanisms. No firm reproducible evidence exists to support either of these contentions. Epidemiological data suggest that exposure during development and childhood to some environmental agent may be the initiating event, but this need not be infectious.
Certainly, the occurrence of MS is greater in first, second and third degree relatives of MS patients than in matched control populations, which suggests genetic input. Similarly, the concordance rate is greater in monozygotic as opposed to dizygotic twins. Evidence thus points to it being, therefore, a polygenic disorder (Bell and Lathrop 1996). Some studies have claimed to have found an MS susceptibility locus in the class II region of the major histocompatibility complex (MHC) (Haines et al. 1998). Another point used in support of the autoimmune hypothesis, but it should be realised that many genes also in this region have nothing to do with the immune system. The increased recurrence risk within families clearly indicates a role for genetic factors. A number of genes may influence susceptibility to the development of MS and subsequent course of the disease. Extensive searches across chromosomal candidate regions and whole genome screens have so far yielded few convincing candidates. In common with most other complex traits, no major susceptibility gene has been identified, although several regions of potential linkage have been associated with MS, including the chromosomal regions 1p, 6p, 10p, 17q and 19q (Kalman and Lublin 1999). Indeed, genome, epigenome and RNA sequences of monozygotic twins discordant for MS, while supporting our hypothesis, does not in itself unravel the genetic mystery (Baranzini et al. 2010).
As the cause of MS remains unknown, it is important to explore the possible mechanisms of disease pathogenicity that may provide clues to identifying susceptibility loci. Epidemiological studies have identified other diseases associated with MS, namely malignant glioma, neurofibromatosis and hypertrophic peripheral neuropathy. The mechanisms of these diseases are independent. It is intriguing that the gene for neurofibromatosis, a disease characterised by increased incidence of glioma, has been located on chromosome 17q (von Deimling et al. 1995), a region which has been previously associated with MS (Johnson et al. 2000; Compston and Coles 2002), glioblastoma multiforme and Charcot-Marie-Tooth peripheral neuropathy (Wrabetz et al. 2001). Indeed, these associated neurological disorders are neural crest disorders, i.e. neurocristopathies. A recent study tracking the expression of transcription factors (neural crest cell markers) in the neural crest in vivo, in human embryos, presents findings some of which concern those disorders of the peripheral nervous system which we have found to be strongly associated with MS. Such new data lends support to our hypothesis that MS is a developmental neural crest disorder (Betters et al. 2010).
For the past century the major lines of research in MS have focused on an immunopathological aetiology. This has enormous implications, not only for the future and direction of research, but also in directing treatment. Despite many attempts at immunosuppression, no convincing evidence has been put forward that such therapy has any significant effect on the clinical course of the disease (Holfield and Wiendl 2002). Whilst there are some claims for the possible modest efficacy of β-interferon, many caveats surround this conclusion (Steiner and Wirguin 2000; Rice et al. 2002), and it should be realised that even the mechanism of how β-interferon may work is not understood, although it may have some healing effect on the blood–brain barrier (Stone et al. 1995). β-interferon is certainly not a cure, nor does it induce great symptomatic improvement whilst immunosuppressive therapy has many serious side effects and complications, including fatality. The consequence of continuing to accept an autoimmune hypothesis may therefore have a very serious, negative outcome in relation to therapy.
Relationship between MS and EAE
The idea that certain neurological diseases have an ‘allergic’ basis was advanced in 1927 by Glanzmann (1927), as an explanation for the encephalomyelitis that complicates certain viral infections, such as chickenpox, smallpox and post-vaccination. Soon after the introduction of the vaccine for rabies by Pasteur in 1876, it was noted that several patients developed paralysis and other neurological dysfunction after receiving the vaccine. Critical observers also noted that often the offending dog that had bitten them was later found not to be rabid. Remlinger in 1928 analysed the clinical details of 1,164,264 patients treated with the Pasteur vaccine and found 529 cases with such neurological complications (Remlinger 1928). Attention was directed later as to the possible cause of such neurological complications and at the potential for disease induction by materials in the vaccine other than the virus.
Animals would not tolerate immunisation with brain material and often developed convulsions, paralysis and weight loss (Aujeszky 1900). Early workers studied possible allergic reactions in the brains of animals, and these studies coupled with the finding that whole brain extracts could induce an encephalitis, gave an enormous impetus to this research. The brains of patients with such ‘neuroparalytic accidents’ were found histologically to differ from those dying of rabies (Bassoe and Grinker 1930). Schwentker and Rivers (1934) showed that the poorly antigenic homologous brain inoculum used to try to induce encephalitis could be rendered more antigenic by autolysis or infection; the antigenicity of brain tissue paralleled its myelin content (Schwentker and Rivers 1934). Encephalomyelitis was capable of being induced in monkeys by repeated injections of aqueous or alcohol/ether extracts of brain (Rivers and Schwentker 1935), with the disease appearing after months of repeated injections. After the discovery of Freund’s adjuvant, EAE could be produced by a single immunisation in guinea pigs, rabbits and monkeys (Kabat et al. 1946; Freund et al. 1947).
Comparative neuropathological studies of EAE drew attention to histological similarities between this experimental model and post-rabies encephalomyelitis of man (Adams 1959; Levine 1971). It is our contention that the extension of this comparison to include the prototype primary human demyelinating disease, MS, is one of the major pitfalls in MS research. Experimental allergic encephalomyelitis is totally different clinically, immunologically and histologically from MS although it does have similarities with other human diseases categorised as demyelinating.
ADEM, AHLE and EAE
Acute disseminated encephalomyelitis and its hyperacute form, acute necrotising haemorrhagic leucoencephalopathy (variously known as acute haemorrhagic leucoencephalitis (AHLE) are inflammatory diseases of the human CNS which occur following rabies vaccinations, other vaccinations, immunisations and after viral infections (Behan and Currie 1978); acute disseminated encephalomyelitis may also occur as a complication of endotoxic shock and after severe burns (Behan and Currie 1978; Graham et al. 1979) or where there is damage to cerebral endothelial cells (Graham et al. 1979). Acute disseminated encephalomyelitis and AHLE are part of the spectrum of the same disorder (Russell 1955). These diseases are often classified as primary demyelinating diseases, but in reality they are vasculopathies of the CNS, in which only a tiny area of myelin loss occurs adjacent to the affected vessels and rarely exceeds 1–2 mm in diameter. Acute disseminated encephalomyelitis is similar to EAE and differs entirely in all aspects from MS (Levine 1971; Behan et al. 1972). Comparison of AHLE and ADEM to EAE in monkeys shows that an exact analogy exists between hyperacute EAE and AHLE in monkeys and between ‘ordinary’ EAE and ADEM, in all clinical, pathological and immunological aspects (Behan et al. 1972, 1973; Behan and Currie 1978). Abundant immunological and other evidence shows that the lesion in ADEM and AHLE in humans is at the brain/endothelial cell interface and that any demyelination which occurs is a secondary bystander reaction. These conditions should not be called primary demyelinating diseases since they are severe inflammatory disorders with little or no resemblance to the prototype primary demyelinating disease of humans, MS (Levine 1971; Behan et al. 1972). Acute haemorrhagic leucoencephalitis and ADEM occur in conditions that are known to be pure endothelialopathies (Graham et al. 1979).
Similarities between EAE and MS
Clinically, EAE runs a monophasic course usually with a dramatic onset of weakness, hind leg paralysis and incontinence of urine in lower animals but often optic neuritis, cerebellar signs and paralysis in non-human primates (Behan et al. 1973; Behan and Currie 1978). The disorder clearly involves T lymphocytes, but the histological appearance varies enormously between animal species, and its clinical and histological expression depends on such factors as the type of animal and the route and method of immunisation. Monkeys injected with a small quantity of purified myelin-basic protein in complete Freund’s adjuvant usually develop a mild monophasic clinical illness in whom histologically perivenous mononuclear cell infiltrates are found in the white matter, similar to those found in acute disseminated encephalomeylitis (ADEM) in humans (Levine 1971). Repeated injections using the same procedure but with the addition of pertussis bacilli in the adjuvant or with whole white matter as antigen will result in an entirely different clinical and histological outcome. These animals will have multiple abnormal cerebral foci, which are frankly haemorrhagic with severe oedema, fibrinoid necrosis of blood vessels within the lesion and a cellular component varying from mononuclear lymphocyte CD4+ cell infiltrates to that of intense polymorphonuclear neutrophil exudates with extravasation of fibrin and serum (Raine 1994). In our experience of inducing hyperacute EAE in baboons and monkeys, the condition is identical to acute haemorrhagic leucoencephalitis (AHLE) in humans.
Hyperacute EAE, i.e. the disease that occurs when EAE is induced by routine methods in cats, dogs and monkeys, bears no clinical or histological resemblance to MS. This form of EAE in animals is clinically identical to AHLE in humans. In EAE in monkeys and AHLE in humans, such intense cerebral oedema occurs that gross morphological displacement of brain structures often occurs and an increase in water content of up to 20% (Levine 1971). If the brain of normal animals is traumatised, it may develop a cellular infiltrate that is composed of macrophages and T lymphocytes (Popovich et al. 1996). Concomitant with this perivenous inflammation is breakdown of the blood–brain barrier (Paterson 1987). The exact mechanism why this occurs is unknown, but may be related to inflammatory mediators released from macrophages and other invading mononuclear cells. Similarly, animals with traumatic damage to the CNS will also show increased cerebral vascular endothelial permeability (Noble and Wrathall 1989; Aihara et al. 1994). The breakdown of the blood–brain barrier is the one feature that EAE and post-traumatic lesions of the CNS have in common with AHLE, ADEM and, indeed, MS.
Dissimilarities between EAE and MS
The lesions in EAE are different to those in MS where the characteristic feature is the well-defined edge clearly, differentiating it from that of ADEM and hence EAE. The inflammatory cerebral lymphocytic infiltrates that occur in most cases of MS are usually weak, scant, lack aggressiveness (Dawson 1916; Lumsden 1955; Adams 1977) and, as pointed out by Lumsden, cannot be compared to those of ADEM (Lumsden 1955). Mild inflammatory haematogenous infiltrates and oedema which are not consistent pathological findings in MS have been deemed by Lumsden (1955) not to be essential morphological criteria for the diagnosis. He drew attention to the self-propagative character of the MS lesion which showed variable discontinuous sleeves of demyelination surrounding blood vessels which he regards as the essential distinction between the more regular and uniform perivenular lesions of ADEM and EAE (Lumsden 1955).
Extensive studies have been made of the experimental allergic encephalomyelitis animal model since all parameters can be examined and controlled. The precise mechanisms of how lymphocytes traffic in the brain in EAE have been elucidated as has been the role of adhesion molecules and other subcellular elements in controlling and directing cerebral lymphocyte traffic (Raine 1994). This supposes that the traffic of lymphocytes in the brains of mice is similar to that of lymphocytes (when they do occur) in the brains of patients with MS. Gulcher et al. (1994) argued in examining these data ‘This comment reflects the leap of faith that often characterises the literature on neuroimmunology of multiple sclerosis’. Raine (1994) accepted that it was impossible to know the dynamic movements over time of cells within the parenchyma of the brain in MS and assumed that such cellular traffic in the animal model, i.e. EAE, was similar to MS.
Further criticisms can be made for accepting that several of the immunological reactions which occur in animals with EAE and in patients with MS are similar. One of us demonstrated many years ago that, using in vitro techniques, one could detect circulating sensitised lymphocytes in non-human primates immunised to develop EAE, and showed that sensitisation occurred to myelin antigens (Behan et al. 1972, 1973). Detailed and repeated identical experiments on patients with MS failed to show a singular case in which clear-cut sensitisation to myelin antigens could be detected (Behan et al. 1968; Johnson et al. 1986). However, sensitisation was demonstrated in patients with ADEM and in patients with AHLE (Behan et al. 1968). These results have been confirmed in different laboratories (Johnson et al. 1986), but there has not yet been any confirmed report that such sensitisation occurs truly and specifically in patients with MS as compared to controls and to patients with other neurological diseases.
A large number of potential MS therapies have been envisaged from experiments in animals with EAE. These include vaccination with specific encephalogenic T cells or peptide fragments derived from similar cells, antibodies against the T-cell receptor, modification of the MHC molecule, anticytokine treatments and the intravenous, intranasal or oral administration of different encephalogenic peptides and proteins. The list is far from complete, but it should be stressed that the application of these potential therapeutic techniques to man has been consummately associated with failure (Holfield and Wiendl 2002).
MS as a possible autoimmune disease
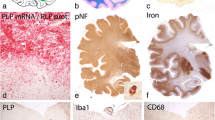
Histological findings
Multiple sclerosis is one of the most common neurological disorders and certainly the most common human demyelinating disease. It was first described by Carswell from Scotland and Cruveilhier from France in the 1830s, but still its exact pathogenesis is unknown. The classical lesion of MS is the plaque, an area in which there is relative preservation of axons, loss of myelin and digestion of the myelin by macrophages and microglia. Over time the lesion shows pronounced astrocytic gliosis, and the final product is a gliotic scar. The plaque is centred round a blood vessel, and there may or may not be a mild inflammatory infiltrate of lymphocytes. The vessel involved is usually a small vein, but may be a small artery.
Still no general agreement exists on what precisely happens in the development of this MS plaque. Earlier students such as Lumsden (1970) found that the myelin disintegrated in the absence of any infiltrating cells. Dawson (1916), however, noted initial pallor of the myelin with an increase of lipid-containing macrophages. Most scholars are certain that in some cases there are absolutely no inflammatory cells initially, while even in the developed plaque these are predominantly described as minimal (Adams 1977). Electron microscopic analysis has shown that myelin breakdown is concomitant with the arrival of the infiltrating macrophages and not the lymphocytes, which arrive much later. Indeed, early ultrastructural studies showed changes in the myelin and in the oligodendrocytes but without any infiltrating cells being present. The initial hypercellularity in the plaque is due to the presence of astrocytes and infiltrating microglia. Lumsden (1970) pointed out that gliofibrillogenesis begins simultaneously with demyelination. The histological features of MS are readily distinguished from other conditions by lack of petechial haemorrhages, accumulated haemosiderin and that of conspicuous oedema. It is often stated that the lesions of MS localise in a random fashion but on more careful analysis there is a distinct symmetry when small plaques and all demyelinating activity are taken into account. Lesions of MS usually tend to occur in the cervical cord before involving the cerebral hemispheres. Indeed, the symmetrical distribution of plaques was regarded by Lumsden (1970) as one of the most striking statistical findings in that disorder. Further studies confirm this finding.
Plaques grow slowly, and it has been estimated from statistical studies of patients with long-standing MS that the rate of growth of a plaque is between 2 and 4 mm a year. The demyelinating process, however, can be more rapid or more severe. It is of extreme interest that Lumsden (1970) further argues “The basis for this predilection of the multiple sclerosis process for the optic pathways and cord is still, in the writer’s view, the major riddle in the pathology of the disease”. As postulated by Oppenheimer (1978), these two areas are constantly being traumatised; we move our eyes conjugately in all directions each day, and we move our neck laterally and in a flexion/extension arc constantly (whether we have cervical spondylosis which would exaggerate the effects of such movements). These could predispose to disruption of the blood–brain barrier locally. Brain and Wilkinson (1957) noted that cervical spondylosis may be associated with MS, and they suggested that “The effect of cervical spondylosis upon the spinal cord may be to make it more susceptible to the lesion of multiple sclerosis at that level”. This association of MS and cervical spondylosis has been confirmed by Burgerman et al. (1992) and Chaudhuri and David (2009).
Plaques in the spinal cord are usually longer than those occurring elsewhere. Symmetry of plaque formation is often seen particularly with bilateral involvement of the fifth nerve entry zone in the pons. In the classic early plaque, special histological stains show preservation of axons with myelin being the primary target. Accompanying the damage to myelin is gliofibrillogenesis with the development of grossly hypertrophied astrocytes. Myelin is broken down into “myelin balls”, i.e. droplets of fat, crystallised lipids and granules. The simultaneous vigorous astrocytic response to the breakdown of myelin is possibly the earliest pathological observable abnormality (Dawson 1916). Microglia are not involved until there is myelin breakdown, whereas reactive astrocytes almost appear simultaneously as myelin breakdown. Microglia are activated as a normal secondary event and would be so activated if damage to the myelin were to occur in another way. The remarkable response of astrocytes in MS has been commented on by many authors (Dawson 1916; Lumsden 1970; Arstila et al. 1973). Other than the response that one finds in prion disease, the astrocytic response in MS is exceptional. Charcot himself commented on the simultaneous gliofibrillae with the astrocyte swelling. Such changes in astrocytes suggest a relationship to the mechanism for development of a glioma.
The pathological features associated with the initiation and development of acute lesions remain controversial. Lumsden (1970) was of the view that demyelination occurred first and, simultaneously, there was astrogliofibrillogenesis and then involvement of microglia and haematogenous cells, and subsequently the later invasion by lymphocytes (Lumsden 1970). Dawson (1916) held similar views. He also, in reviewing the earlier literature, found many examples and cases in which on histological examination there was no inflammation whatsoever. Serious scholars of the classical histological lesions of MS have noted scant or even absent ‘inflammatory’ cellular reactions (Seitelberger 1960; Graham et al. 1979). Seitelberger (1960) stated that the demyelination of the acute plaque occurred “in the absence of mononuclear immune cells”. Indeed, as exemplified by several investigators, Guseo and Gellinger (1975) found in a detailed study of 19 cases of MS with a short clinical course (the mean of less than 1 year) that a significant number of these patients had no perivascular infiltrate in the CNS. The absence of lymphocyte cuffing in patients with acute MS is not the exception and is said to occur in one-third of all cases (Adams 1977). Lymphocytes are a normal occurrence in the perivascular spaces. Similar infiltrates, in fact exceeding that found in MS, may occur in a wide variety of pathological conditions including trauma, infarcts, tumour and following infections. Most investigators who have looked for lymphocytes in contact with the myelin sheaths and oligodendroglia found that “the number of lymphocytes that leave the perivascular compartment and enter the parenchyma is very small, both in absolute numbers and relative to the number of macrophages present” (Sluga 1969; Prineas 1975; Tanaka et al. 1975; Prineas et al. 1984; Prineas 1985).
There are multiple reports of detailed and sophisticated immunological analysis of the inflammatory cells that are found in the brains of patients with MS. Clearly, it is imperative to compare their type and composition with that found in non-specific conditions with no primary immunological pathogenesis. Similar cells are found in a large number of other conditions including adrenoleucodystrophy (McGuinness and Smith 1999), a disorder of inborn metabolism, and in neurodegenerative disorders such as amyotrophic lateral sclerosis (Engelhardt et al. 1993). Similar infiltrates are found up to 40 years later in the spinal cord of those with poliomyelitis (Pezeshkpour and Dalakas 1988).
Dawson (1916) was of the opinion that the myelin sheath was first to be affected, and simultaneously changes in the neuroglia occurred. There was then alteration in the permeability of the blood vessels. “The first cellular increase is secondary to the reabsorptive processes and infiltration of fat granule cells: this is followed by a proliferation in all the cell elements of the adventitae and, at a later stage, by a modified infiltration of lymphocyte-like cells and a few plasma cells” (Dawson 1916). Since the cause of MS is unknown, the significance of the mere finding of a scant haematogenous cellular infiltrate is likewise unknown. As stated, histologists have remarked on the mildness of this infiltrate, and Adams et al. (1985) were of the view that it was too modest to constitute “a florid autoimmune reaction”.
The finding of inflammatory cells in parts of the brain in patients with MS that contain no myelin such as the retina (Lightman et al. 1987) and also the finding of cellular infiltrates away from the plaques (Adams 1989) further raises doubt as to whether such cells have a primary pathological function. Since the earliest lesion in MS is not known, examination of the brains of patients who have had the illness for some time makes it impossible to give a precise age to the inflammatory or demyelinating lesions found. There is still little knowledge as to the precise pathological processes and timing of events that occur in the genesis of the MS plaque. One-third of all MS plaques may not contain cellular infiltrates, and such infiltrates when they are found are often scant, lack aggressiveness and indeed may occur in parts of the brain which contain no myelin. Reliance on the presence of these inflammatory cells as the prime pathological process in the disease therefore seems to be totally unfounded. The persistently aggressive nature of the illness classically seen in primary progressive MS but even in the relapsing/remitting type brings the disorder more in line with a neurodegenerative disease than with acquired inflammatory disorder. Indeed Confavreaux et al. (2000) showed that patients with MS had a progressive course that was not significantly influenced in its progression by relapses and remissions. This finding may help to cement what is in our opinion a false separation of primary progressive MS from the other types. Our contention is that there is only one type of the disease with different rates of clinical progression. In our opinion too, the pathological lesions are identical in both conditions and whilst it is suggested that there may be more inflammatory infiltrates in the secondary progressive disorder, this may be readily explained by the rate of tissue destruction (Revesz et al. 1994). Furthermore, the finding of minor differences in the presence of oligoclonal bands in primary progressive as opposed to the remaining types does not detract from this opinion (Revesz et al. 1994). The presence of oligoclonal bands is non-specific and relates to breakdown of the blood–brain barrier allowing lymphocytes to produce immunoglobulins within the parenchyma of the brain.
Detailed studies in looking at axonal loss in MS also support our view that MS is a neurodegenerative disease (Ganter et al. 1999). Generalised axonal loss correlates well with clinical deterioration compared with “any other measure of structural central nervous system (CNS) change investigated” (Isaac et al. 1998). We will comment later on magnetic resonance spectroscopy studies on total N-acetylaspartate in the central nervous system white matter, but here again there is good correlation with functional impairment.
Immunological findings in MS
The present hypothesis of the pathogenesis of MS is that it is an autoimmune inflammatory condition triggered by an unknown infectious agent; the basis of the hypothesis is that T cells, specifically sensitised to an unknown antigen, invade the nervous system and cause immunological damage to myelin. A voluminous literature has grown up documenting the innumerable minimal changes found in the peripheral blood and cerebrospinal fluid of patients with MS. No one specific abnormality has ever been found and confirmed.
Attention should be given to the fact that many of these claimed findings are said to occur during the active phase of the disease, i.e. as the patient exhibits new symptoms. However, similar comparative studies are done during the quiescent phase when for every new symptom that a patient may develop, there may be at least ten silent demyelinating episodes occurring in the brain, which are visible only on a magnetic resonance imaging (MRI) scan. Differentiating activity of the disease merely by documenting exacerbations or new symptoms is clearly open to misinterpretation (Truyen et al. 1991; Isaac et al. 1998).
T-cell abnormalities
In an endeavour to support a possible immunopathological basis for MS, researchers have turned to the blood and cerebrospinal fluid to identify any specific immunological abnormalities that correlate with the disease. In animals with EAE, it is possible to demonstrate sensitisation of T cells against components of myelin. Indeed, this phenomenon is also positive in humans with ADEM and AHLE, but has never been confirmed to occur in patients with MS. There are no definitive findings on conventional immunological techniques that polyclonal specific T-cell immune responses against myelin occur in patients with MS.
Using the advanced method of cloning different subsets of T lymphocytes, it has been claimed that specific clones of T lymphocytes sensitised to myelin-basic protein are more frequent in patients with MS than in controls. These experiments were repeated, however, and found wanting (Brinkman et al. 1982; Burns et al. 1983). Further studies failed to show that there were increased numbers of specific sensitised clones of T lymphocytes to myelin antigens in patients with MS (Burns et al. 1983; Richert et al. 1983; Hafler et al. 1985; Tournier-Lasserve et al. 1988). Notwithstanding these failures, the protagonists have put forward the idea that the T-receptor gene might be different in T-lymphocyte clones from MS patients as compared to the T-cell receptor gene usage of similar clones in patients without MS. This hypothesis also has been found wanting (Ben-Nun et al. 1991). Other claims regarding the T lymphocyte and sensitisation to myelin or myelin-specific peptides have been made, but have not stood the test of time (Martin et al. 1993).
A wide variety of other immunological abnormalities have been claimed to occur in MS, but are non-specific. Among these is the claim that during relapses patients have a decreased suppressor cell function (Antel et al. 1979) and that these cells show a normal function when the patient is asymptomatic and increased activity during remissions. Again the poor correlation between exacerbations, new symptoms and active demyelination should be noted. This again has been shown to be a non-specific phenomenon since suppressor cell function can vary with a number of abnormalities of the brain, including trauma and brain tumours (Thomas et al. 1975; Quattrocchi et al. 1990). Indeed, studies of the CD8 suppressor cells in MS demonstrated that they produced normal cell-mediated lysis of alloantigens and that immunoglobulin secretion might be increased (Antel et al. 1986).
A variety of other abnormalities involving T-cell subsets and cell-mediated immunity have been described in MS. These have never been consistently confirmed nor proved to play a primary role in pathogenesis; similar abnormalities have been found in patients with other neurological diseases (Rohowsky-Kochan et al. 1990). Serial analysis of T-cell activation markers and detailed analysis of cytokines failed to show any reproducible abnormality (Freedman et al. 1992). No firm evidence of an abnormality of T-cell lymphocyte immunity, or of specific sensitisation to myelin antigens or other neural antigens was confirmed (Behan et al. 1968; Johnson et al. 1986). Clearly, the many claims for humoral abnormalities have neither stood the test of time nor have the many studies on immunoglobulin abnormalities found in the cerebrospinal fluid.
Attempts at therapy based on experiments in rodents with EAE have so far failed. For example, it has been shown that rats given myelin antigens orally may fail on immunisation with encephalitogenic proteins to develop EAE: oral tolerisation has therefore been induced in rats. In a huge trial in humans, oral tolerisation to myelin antigens in patients with MS was attempted; no beneficial effect was observed. These experiments were perhaps a further cautionary tale in accepting the theory of autoimmunity in MS (Quinn 2001).
Association with autoimmune diseases
In the early 1960s, Simpson (1960) proposed a theory of autoimmune aetiology for myasthenia gravis. Interestingly, this theory was developed predominantly from studying patients with the disease and their first- and second-degree relatives: a demonstrably increased association of other autoimmune diseases was found in all three. For example, he found that 16 of 440 patients with myasthenia gravis had concurrently rheumatoid arthritis. His observations have been amply confirmed in several studies. No such association with autoimmune diseases and correlations with histocompatibility antigens and other markers were found in MS (Behan and Haniffah 1994). This is borne out by the scant reports of single case occurrences of MS suggesting that there is no true association (Aita et al. 1974; Shakir et al. 1983). Other workers who were keen to highlight such an association have suggested an association with diabetes mellitus (Warren and Warren 1982); yet, studies looking specifically at this association failed to show the increased incidence of autoimmune disease and patients with MS, particularly diabetes (Alter et al. 1970). Broadley et al. (2000), by the most convoluted arguments, were unable to show any increase in autoimmune diseases in patients with MS when compared with index controls or population data; however, they concluded that autoimmune disease was more common in first-degree relatives of patients with MS, a finding they commented on that was consistent with previous larger groups looking especially at this relationship: “The finding of an increased familial rate of autoimmune disease without a corresponding increase in patients with multiple sclerosis seems counterintuitive” (Broadley et al. 2000). Further epidemiological studies failed to confirm an increased diagnosis of autoimmune diseases in families with MS (Langer-Gould et al. 2010).
Lumsden (1955) in a careful post-mortem study of a very large number of patients with MS was unable to show any evidence or stigmata of autoimmune disease. Broadley et al. (2000) found the highest association in first-degree relatives with thyroid disease, but this is a difficult and misleading condition to use as a prime example of an autoimmune disease. Thyroid disease is extremely common, may be occult and it is difficult to determine its exact incidence. Indeed, a very detailed study from France showed an overall decrease of autoimmune disease in first-degree relatives of patients with MS, whilst reporting a high prevalence of Graves’ disease (Heinzlef et al. 1999). Clearly, no association of autoimmune disease with MS occurs, and the absence of any increased incidence in such disorders in the probands leave us in no doubt that no true association exists.
Effect of immunosuppressive/immunomodulation in MS
The importance of the autoimmune hypothesis is well displayed in treatment trials with various and powerful immunosuppressive drugs. The use of these drugs adds another pitfall in the treatment of the condition. The diagnosis of MS depends on a number of different criteria combining clinical and paraclinical factors (McDonald et al. 2001); the criteria which were newly introduced are helpful, but still may permit a wrong diagnosis. Even if a correct diagnosis is made, patients still form a heterogeneous study group. MRI studies have shown that for each clinical symptom there may be ten silent lesions in the brain. MS is a complex disease, and the natural history of this disorder is not fully appreciated; the mechanisms underlining variable clinical expression are not known, but modern observations suggest that the disease is invariably progressive with a different rate of progression per patient (Amato et al. 1999; Confavreux et al. 2000). In a carefully conducted study Confavreux et al. (2000) showed that relapses in essence do not significantly influence the progression of the irreversible disability. Other modern observers have noted that “The failure of a remission to be complete may be more important than the frequency or severity of antecedent relapses in increasing neurological impairment, and in the transition to a secondary progressive phase” (Amato et al. 1999). Notwithstanding this, it should also be noted that the majority of patients with MS usually have a rather benign course; even after 10 years, 75% of their patients had less than ten lesions on MRI scan of the brain and an extended disability status scale of less than three (O’Riordan et al. 1998). It can thus be readily seen that there are many difficulties in evaluating patients on a clinical trial.
Clinical trials there are, however, in abundance: a rise from 50 such papers in 1965 to more than 300 by the year 2000. This has been described by some as reflecting “the sense of excitement in the field of MS therapeutics” (Holfield and Wiendl 2002), but is regarded by us as a sad reflection on the gullibility of researchers in accepting an unproven hypothesis. The authors commented on this sense of excitement philosophically enough to coin the truism: “The road to success is paved with failures” (Holfield and Wiendl 2002). The enormous number of trials based on putative immunosuppression and immunoregulatory mechanisms have singularly failed to show a cure or convey major benefit to MS patients in addition to subjecting them to an increased morbidity and mortality. Immunosuppression studies using the most powerful drugs have been applied to patients with MS.
Some of the trials used (See Holfield and Wiendl 2002) were:
-
1.
Immunosuppression: Linomide, Deoxyspergualine, Cladribine.
-
2.
Cytokine modulators: Lenercept, Infliximab, TGF-β 2 (transforming growth factor β2) IL-10 (Interleukin-10).
-
3.
Inducers of remyelination: IVIg (Gamimune N).
-
4.
Antigen-derived therapies: Oral myelin (Myloral: Al-100), APL (altered peptide ligand: CGP77117; NBI5788). DR2:MBP82-102 (AG284).
-
5.
T-cell-receptor directed therapies: T-cell vaccination, T-cell receptor peptide vaccination.
-
6.
Interferons: (IFNβ-1a and IFNβ-1b).
-
7.
Glatiramer acetate (Copolymer-1).
Claims for the powerful immunosuppressor cyclophosphamide led to the widespread use of this drug in MS in Europe and the US (The Multiple Sclerosis Study Group 1990). The initial studies were not double-blinded, but double-blind, placebo-controlled studies failed to show any improvement (Likosky et al. 1991; The Canadian Cooperative Multiple Sclerosis Study Group 1991). Similar results were found with cyclosporine (Hauser et al. 1993) and with azathioprine (Yudkin et al. 1991).
Brain and total lymphoid irradiation and plasma exchange have also been tried. The collected reports of these and other immune-mediated therapies aimed at ‘Modifying the course of multiple sclerosis’ make for sad reading since a review of the vast number of different trials show no definite benefit (Compston 1998). The dramatic failure of trying to induce oral tolerisation to myelin-basic protein in humans with MS has even been the subject of a best-selling book (Quinn 2001).
β-interferon and glatiramer acetate in MS
The two leading immunomodulating drugs for which beneficial claims have been made are glatiramer acetate and INF-β interferon (Holfield and Wiendl 2002; Dhib-Jalbut 2002; Calabresi 2002). In a recent editorial, data on glatiramer acetate were said to provide reassuring information on its beneficial effects in MS (Holfield and Wiendl 2002): such data as exist suggest that both β-interferon and glatiramer acetate be looked at with extreme caution before total acceptance. Glatiramer acetate “is thought to act by inducing a population of regulatory (Th-2 type) T-cells that migrate to inflammatory sites in the central nervous system (CNS), where they are activated by cross-reacting myelin antigens to exert their beneficial ‘bystander effect’” (Holfield and Wiendl 2002). This process may take several months to develop. Such an explanation defies belief and lies more in the realm of science fiction.
In a study looking at the mechanisms of action of interferons and glatiramer acetate, we note that “Over the past decade multiple sclerosis patients have benefited enormously from therapeutic research efforts” (Dhib-Jalbut 2002). Sadly we cannot readily accept this statement from our own clinical experience or from the data provided. Others have questioned the efficacy of such trials (Steiner and Wirguin 2000). Their study comparing patients from the same country and from an identical population found that the placebo patients in the copolymer-1 versus placebo group, fared better than patients receiving β-interferon. Steiner and Wirguin drew attention to the fact that “Comparison between studies with even slightly different end-points is extremely difficult”. Of importance is the caveat of Steiner and Wirguin that “All three studies report a very similar reduction (around 30%) in the relapse rate”. They highlight that “The almost identical results of clinical trials using different agents, and their inability to go beyond the 33% line, raise the possibility that the entire observed benefit is only a placebo effect, and that the significant deviation from the true placebo might be the outcome of partial unblinding of patients by the side-effects” (Steiner and Wirguin 2000). Similar results were found by Calabresi (2002) where improvement with β-interferon 1a was precisely 33%.
In a review of the possible benefits of interferon in relapsing-remitting MS, The Cochrane Review drew attention to 208 articles of which only seven met all the selection criteria and formed the subject of their conclusions (Rice et al. 2002). The variable quality of the trials, the inadequate methodology, the very high proportion and incomplete description of drop-outs, and the failure to adhere to the strict original intentions of the trial detract seriously from any claims that were made (Rice et al. 2002). These trials should be considered as single rather than double-blind. They drew attention to the fact that if interferon-treated patients who had been removed from the study were deemed to have worsened, the significance of the reported effects was therefore lost. The efficacy of interferon on both exacerbations and on progression of the disease was modest after 1–2 years (Rice et al. 2002).
The precise action of interferon-β is unknown, but an important effect is that it reduces the permeability of the blood–brain barrier, a mechanism that may explain its modest benefit rather than immunomodulation (Stone et al. 1995). It is said to rapidly block the blood–brain barrier leakage, within 2 weeks, as seen by gadolinium-enhancement scans (Stone et al. 1995). Glatiramer acetate also has an effect on the blood–brain barrier but less dramatic resolution of gadolinium-enhanced MRI activity. In a recent issue of Neurology devoted to Practical issues in the management of multiple sclerosis, a number of investigators look at the action and the clinical results of treatment by glatiramer acetate and interferons. They all begin with a statement that MS is an immunologically mediated disease and all are influenced by the comparison they make with EAE. Dr. Dhib-Jalbut writes of the amplification of immunoreactivity “in the central nervous system where T-cells are further activated by antigens presented on microglia resulting in the secretion of pro-inflammatory cytokines and chemokines that attract and retain inflammatory cells in the CNS” (Dhib-Jalbut 2002). We have discussed in this paper the fact that there is no convincing evidence for any of these statements, indeed no antigen has ever been identified that is specific for MS. Dr. Dhib-Jalbut further goes on to state that the mechanisms of action in MS of β-interferon is by reducing T-cell activation, inhibiting interferon-gamma effects, induction of immune deviation and inhibition of the blood–brain barrier. We would humbly suggest that the data, which are founded on wide speculations, attempting to explain these putative mechanisms would need to be further evaluated, strengthened and confirmed before being accepted.
Glatiramer acetate (Copolymer-1) is a synthetic molecule made of four amino acids glutamine, lysine alanine and tyrosine. The same acids are found in myelin-basic protein and because myelin-basic protein has been suspected, but never proved to be, the antigenic component involved in MS, a giant intellectual jump occurs in assuming that glatiramer acetate, through its action involving immune attack on myelin-basic protein, allows one to use it in the treatment of MS. Again, the original work on evaluating copolymer activity was that it blocked the induction of EAE in animals. Glatiramer acetate has been stated to bind to human leucocyte antigen (HLA) class II (DR) molecules as a result of this possible interaction based on data from its use in animals with EAE, and it is said to inhibit myelin-reactive T-cells by inducing anergy in such cells and bringing about anti-inflammatory TH2 cells which have “bystander suppression in the CNS” along with “neuroprotection” (Dhib-Jalbut 2002).
In the same issue of Neurology, Calabresi (2002) describes the disease-modifying therapies available for relapsing-remitting MS. He reported the result of a 2-year study of placebo versus β-interferon-1a. He found the beneficial effect, a reduced exacerbation rate of 34%, whilst in a further study, β-interferon-1a (Avonex), he was able to demonstrate a beneficial effect of 32% (Calabresi 2002). This finding was replicated in yet another study that compared placebo with interferon-beta-1a (Rebif) (Calabresi 2002). Examining the effects of β-interferon-1b, β-interferon-1a (Avonex) and Copolymer-1, Steiner and Wirguin (2000) noted that “The Copolymer-1 placebo patients fared better even than the interferon treated group” despite the fact that both studies were performed in the same country with patients from an identical population pool. An analysis of these three studies showed that they all had effect, but the effect was all around 30% reduction of the relapse rate. These studies have a similar effect on those recently quoted in the US for both glatiramer acetate and β-interferon (Dhib-Jalbut 2002; Calabresi 2002).
In 1955, Beecher (1955) published his important paper on The powerful placebo, where he showed a placebo effect of 30%. In a trial of transfer factor in patients with MS one of us was struck by the extraordinary placebo phenomenon that was also observed in patients with MS treated by different techniques (Behan et al. 1976; Behan 1980). We would therefore agree with the recent critiques on reporting clinical trials (Mayor 2002; Clarke et al. 2002).
Recent immunological findings implicating B cells
Now that the T-cell epoch is over; B cells are the latest focus of attention. There is an extensive literature on B cells, autoantibodies, serum factors and plasma cells in MS, and the general consensus is that they have no direct pathological role since they are found in equal numbers both in patients and in controls (Tourtellotte and Tumani 1997; Esiri and Gay 1997). B cells are seldom found within the demyelinating MS lesion (plaque) or non-plaque parenchyma and are usually present in perivascular spaces in acute plaques. There is no specific or pathogenic antibody in MS and B cells make up only a very small proportion of the lymphocytes in most perivascular infiltrates around plaques although occasional infiltrates may contain up to 40% of B cells (Tourtellotte and Tumani 1997). Previous attempts of B-cell depletion with anti-lymphocyte globulin and total lymphoid irradiation in MS were unsuccessful. In a recently reported trial of rituximab, a chimeric mouse-human monoclonal antibody against CD20, which is specific to B cells, patients had fewer relapses and enhancing MRI lesions (Hauser et al. 2008). The chronology of clinical and MRI changes on rituximab was non-specific and appeared to be anti-inflammatory rather than due to a specific effect on soluble antibodies or B-cell lysis (Hauser et al. 2008). Similar rapid non-specific effects have been reported in Alzheimer’s disease (Griffin 2008; Tobinick and Gross 2008). Rituximab does not target mature plasma cells, so it was unlikely that a reduction of pathological antibodies could explain the rapidity of treatment effect, and like natalizumab, it carries a risk of progressive multifocal leucoencephalopathy (PML). Cases of PML have been reported after treatment with other monoclonal antibodies, such as rituximab, natalizumab and efalizumab (Carson et al. 2009).
Previous studies have shown that the use of anti-lymphocytic globulin and total lymphoid irradiation in patients with MS is futile. It is difficult therefore to understand that depletion of B cell (CD20) helps clinically since acute demyelination can evolve without B cells, and one-third of lesions in patients with MS show no cells whatsoever (Seitelberger 1960; Guseo and Jellinger 1975; Adams 1977). There is no disease-specific antibody in MS unlike other autoimmune diseases in which rituximab is effective. Furthermore, in previous trials of MS, a huge gap has been found between the treatment effect and assessment of changes on MRI on relapse rates. This gap is bridged as in the rituximab trial by statistical extrapolation rather than by longitudinal follow up data. There is a growing doubt among MS scholars concerning the mild inflammatory changes, since studies have shown that these lesions are mild, scant, and most unlikely to be involved in aggressive autoimmune reactions (Adams 1977).
The two other monoclonal antibodies still in development are alemtuzumab (Campath-1H) is a human monoclonal antibody targeting CD52 which is expressed by T and B lymphocytes, monocytes and eosinophils, and induces a profound leucopoenia rapidly (Johnston and Conly 2006). Alemtuzumab was the third monoclonal antibody following natalizumab and rituximab which was tested in relapsing-remitting MS (Moreau et al. 1994). Experience with alemtuzumab, a humanised monoclonal antibody against CD52 receptors on lymphocytes and monocytes, suggested that it was not effective for preventing progression of disability in secondary progressive MS (Moreau et al. 1994). However, in a recent new trial targeting patients with relatively early relapsing-remitting MS, with low disability (range 0–3.5), in a physician-blinded randomised clinical trial, alemtuzumab was more effective in reducing relapse rates than subcutaneous beta interferon 1a; however, there was no advantage of using the higher dose (24 mg), and the statistical reduction of the risk of sustained disability was superior for the lower dose (12 mg) in alemtuzumab-treated patients. Post-treatment median EDSS score and the range of scores of patients were not available in the published data, and the only analysis was for mean EDSS score which improved by a clinically meaningless fraction of 0.39 from the baseline score of 1.9, i.e. there was effectively no change in the clinical measure of disability in the treated group (EDSS score within the 1.5–2.0 range before and after treatment) which would be consistent with the previous experience of the drug in secondary progressive MS. Comparison of efficacy of alemtuzumab against interferon beta-1a was also open to criticism because of the high rate of treatment discontinuation (41%) in patients who were well aware of the assigned treatment. Moreover, treated patients had higher incidence of systemic autoimmune diseases—a quarter developed autoimmune thyroid disease, and there was a case fatality due to autoimmune thrombocytopenic purpura; treated patients also had persistent leucopoenia and higher risk of infection (one patient had Listeria meningitis). The increased risk of autoimmune disease due to alemtuzumab begs the question as to why it should be specifically more effective against the presumed autoimmune pathogenesis of MS, but not other autoimmune disease (Coles et al. 2008).
There was no therapeutic benefit of alemtuzumab in secondary progressive MS despite MRI improvement and profound and persistent lymphopenia. In an ongoing study of relapsing-remitting MS patients, alemtuzumab reduced relapse rates comparable to those achieved with natalizumab; however, relapse rate reduction in patients treated with beta-interferon in this trial was significantly higher (60%) than what is experienced in clinical practice. In addition, treatment with alemtuzumab has serious risks due to an acute, post-infusion cytokine-release syndrome and long-term risk of developing antibody-mediated autoimmune diseases (Coles et al. 2008). Daclizumab is directed against CD25 and blocks the alpha-chain of interleukin-2 receptor (Bielekova et al. 2004). Despite a significant reduction in MRI lesions in patients receiving high dose daclizumab, reduction of relapse rate was similar to both high-and low-dose groups and comparable to those achieved with beta interferon.
The beneficial claims of the two original immunomodulating drugs namely β-interferon and glatiramer acetate have had relatively little impact on the burden of MS disability Behan et al. 2002; Calabresi 2002). Neither treatment is effective in progressive MS and do not hold out any great claims when compared with placebo. As stated above, in a review of the possible benefits of interferon in relapsing-remitting MS, The Cochrane Review drew attention to 208 articles of which only seven met all the selection criteria and formed the subject of their conclusions (Rice et al. 2002). It is also interesting that in most clinical trials with beta interferon, its clinical effect on relapse rate reduction is approximately one-third, which would be the effect of a powerful placebo. Any minor benefits from beta interferon are probably brought about by vascular capillary changes which have been shown to occur in endothelial cells in vitro experiments (Stone et al. 1995). Our own experience shows that placebo effect is strong in patients with MS, and we are not convinced of any other therapeutic benefit. How many patients would be willing to take a drug for their MS if told:
-
that the drug had very serious side effects including death;
-
that it needed to be taken for an indefinite period;
-
and that benefit would not be measured clinically, but would require in-depth sophisticated statistical analysis to document if the benefit should occur, pointing out that in all trials of these drugs there is no evidence for total arrest or cure in a single patient?
Newer treatments based on immunomodulation/immunosuppression
Multiple sclerosis is probably the best example of the commercialisation of clinical research for the benefit of all except the patients. There is no treatment that has stood the test of time in preventing disability progression over the long term, and no effective treatment exists for those with secondary and primary progressive MS. However, the “MS market” is estimated to be worth almost US $8 billion in 2008, with a growth rate of 10.6% year-on-year (CNS Drug Discoveries, accessed 01 May 2009). Besides β-interferon and glatiramer acetate, there will be 12 new disease-modifying inmmunosuppressive treatments, four monoclonal antibodies and three potential vaccines as candidates (see Table 1) none of which would be tested head-to-head against each other or will have long-term efficacy and safety data before seeking marketing approval.
How will these developments help a patient with relapsing-remitting MS? Are we going to “try out” each one of them in turn as and when the patient prefers, or as and when the MS groups promote these drugs, or according to the order in which they arrive on the market? Worldwide, there are nearly 40,000 patients who are now receiving natalizumab at an estimated annual cost of US $25,000 per patient without any long-term evidence that the treatment necessarily works to prevent disability progression, giving a strange sense of déjà vu of the early years with beta interferon (CNS Drug Discoveries, accessed 01 May 2009).
Lessons from therapeutic experiences in MS
In therapeutics, response to targeted interventions is often regarded as an indirect evidence of disease mechanism. Unfortunately therapeutic response in MS clinical trials does not measure up to what could be considered as an effective treatment (Holfield and Wiendl 2002). MRI-based outcome measures consistently overestimate treatment benefit, and few clinical trials have reported sustained benefit in disability progression beyond 3 years. Annualised relapse rate, one of the primary clinical outcomes in clinical trials, is an inappropriate measure because relapse rate is not a continuous variable that can be averaged as a fraction. Furthermore, improvements in MRI scans are seen with non-immunological treatments such as fluoxetine, tetracycline or statins (Puri et al. 2001; Metz et al. 2004; Ifergan et al. 2006). There is no evidence that monoclonal antibodies are any more effective than anti-inflammatory effects of high-dose steroids, and it is known that cytokines can have a non-specific mode of action that is poorly understood. Experience of immunosuppressive therapy in MS has, likewise, shown little, if any, benefit (Holfield and Wiendl 2002).
Treatment trials based on EAE, the putative animal model for MS, have been therapeutic failures and the claimed immunological breakthroughs reported in the leading medical journals, often with laudatory editorials, have not been subsequently confirmed (Behan et al. 2002; Kirk et al. 2003).
Phenomena which militate against the hypothesis that MS is an autoimmune disease
MS in infants
It is difficult, if not impossible, to induce EAE in neonatal animals (Umehara et al. 1990); immunisation is only successful after a certain age. This is very important since the age at which animals become susceptible to develop EAE corresponds in humans to about the age of 2 years. This phenomenon of relative resistance to disease is also seen in the histology of ADEM in infants who until the age of 2 years develop an encephalopathy rather than an encephalomyelitis after the appropriate inciting event which is characterised by the lack of infiltration of mononuclear cells (Oppenheimer 1969).
If sensitised lymphocytes invading the brain are thought to be involved in the pathogenesis of MS, one might therefore not expect to find MS occurring below the age of 2 years. Indeed, there have been several reports of MS occurring in infants (Brandt et al. 1981; Taylor and Cuendet 1986; Shaw and Alvord 1987; Guilhoto et al. 1995).
MS and HIV infection
If MS is an autoimmune disease, a particularly informative setting for studying this would be in patients who have MS and who are concomitantly infected with HIV infection, a situation which is known to induce a severe state of immune deficiency. Berger et al. (1989) reported seven such patients, six of whom developed an immunodeficient state after HIV infection but who continued to have relapsing/remitting MS. Some of these patients had brain biopsies whilst another died and a full autopsy was performed; there was no doubt about the diagnosis. These data would argue strongly against any autoimmune aetiology, i.e. T cell-mediated autoimmune pathogenesis.
Effect of radiation on MS
When recipient rats involved in passive cellular transfer of EAE were previously irradiated, they were found to have more virulent disease than non-radiated animals. Total body irradiation of these recipient animals did something to them that allowed the passively transferred sensitised cells to induce a more rapid and severe encephalitis (Peterson et al. 1993). In other experiments irradiation of the donor rat, however, reduced the severity of EAE, but specific focal spinal cord irradiation enhanced its development (Oldendorf and Cornford 1997). These data are consistent with the known facts that irradiation damages the blood–brain barrier. Damage to the blood–brain barrier certainly enhances EAE. Indeed, in passive cellular transfer experiments, focal damage to one area of the brain 3 days before transfer will render the animals exquisitely sensitive to develop EAE, and they will develop it first within hours in the area of increased blood–brain barrier breakdown (Levine and Hoenig 1968).
Acute radiation therapy, particularly at tumouricidal doses may disrupt the blood–brain barrier and even cause an encephalopathy (Peterson et al. 1993). Patients with MS who are irradiated would be expected to do badly since disruption of their blood–brain barrier would promote further demyelination. Cerebral demyelinating lesions of MS may appear as single or multiple contrast-enhancing lesions on MRI scans, and be mistaken clinically and radiologically for primary or metastatic brain tumours. Peterson et al. (1993) reported five such patients who received radiation therapy. Four of the patients received radiation in full tumouricidal doses and had extremely poor clinical outcomes. Magnetic resonance imaging scans of patients who have deteriorated after radiation show new lesions which have been verified pathologically as demyelinating. At autopsy in these cases there was profound demyelination (Peterson et al. 1993). Aarli et al. reported a case of a man with MS who had a glioblastoma multiforme and was treated with radiation. He died 2 months later, and the autopsy showed no infiltrating tumour but diffuse demyelinating disease of the white matter (Oldendorf and Cornford 1997).
Twenty patients with MS received craniospinal radiotherapy, and their cerebrospinal fluid IgG level was measured (Tourtellotte et al. 1980). Five patients had a transient decline in IgG synthesis which lasted 3–6 weeks; ten had totally inconsistent responses whilst the remaining five that were given radiation as well as ACTH and prednisolone showed a decline in their IgG synthesis rate. What is important to note is that none of these patients were found to have any improvement clinically (Tourtellotte et al. 1980).
Total lymphoid irradiation to induce immune suppression (Zimmerman and Netsky 1950) was also tried in MS: no clinical benefit ensued but a number of deaths occurred; these most likely being secondary to immune suppression (Cook et al. 1986, 1987, 1989; Devereux et al. 1988), with an increase in the severity of the disease and the development of infections. The worsening of their demyelinating disease would appear to be the effect of radiation on blood vessels enhancing vascular permeability (Peterson et al. 1993).
MS associated with other disorders
Epidemiological studies in certain diseases have shown that there is an increased incidence of related disorders in the probands and first-degree and second-degree relatives of such patients. Studies applying similar methods to patients with MS have shown that certain diseases other than autoimmune diseases are associated with MS. Classically, these are malignant glioma, including glioblastoma multiforme, neurofibromatosis Type I and hypertrophic peripheral neuropathy.
Glioma
A compelling series of reports of malignant astrocytomas associated with MS have been published (Scherer 1938; Munch-Peterson 1949; Zimmerman and Netsky 1950; Russell and Rubinstein 1977; Matthews 1962; Brihaye et al. 1963; Barnard and Jellinek 1967; Aubert et al. 1968; Boyazis et al. 1968; Mathews and Moosy 1972; Reagan and Frieman 1973; Currie and Urich 1974; Lynch 1974; Kalimo et al. 1979; Lahl 1980; Ho and Wolfe 1981; Malmgren et al. 1984; Vieregge et al. 1984; Nahser et al. 1986; Barnard and Geddes 1987; Oldendorf and Cornford 1997; Shankar et al. 1989; Perilongo et al. 1999; Costa et al. 2000). Other tumours reported in association with MS have included ependymomas, meningiomas, oligodendrogliomas, and odd non-gliomatous tumours, but these are very rare and likely to be pure coincidental occurrences.
Multiple sclerosis always occurs first, and the tumour generally tends to occur in patients with long-standing disease. In some instances, the tumour appears to arise from the adjacent edge of an MS plaque, but in the great majority it arises from foci far removed from the demyelinating lesions. It is interesting that there is a very high incidence of multicentric origin (Reagan and Frieman 1973). In a proportion of MS cases with associated tumours it is impossible to determine whether the tumour is multifocal or not; this is a function of the extent to which the brain is sampled (Russell and Rubinstein 1977). A frequency of 8.75% of multicentricity for all gliomas has been found as compared to 50% when the glioma occurs with MS (Reagan and Frieman 1973).
The number of reported cases almost certainly does not reflect the true incidence of this association. We have personally seen in our institute a further case of MS, Charcot-Marie-Tooth disease and astrocytoma, and two further cases of the association with malignant astrocytoma. Neurological symptoms occurring in someone with a long-standing disease such as MS are likely to be overlooked and attributed to the original disease. Furthermore, patients with MS who die, rarely come to a post-mortem examination. This is important since in the reported cases of this unique association, several were found at post-mortem examination (i.e. the association had in fact been occult).
This association highlights the role of astrocytes in both disorders. It is extraordinary that mitotic figures very rarely, if ever, occur in areas of astrocytic hyperplasia since astrocytes may divide by another mechanism which has been referred to as “amitosis” (Adams and Sidman 1968a, b). Indeed astrocytes may, like melanoma and other cells, divide under certain conditions by subdivision (Okun and Edelstein 1967). Glioblastomas, astrocytomas, ependymomas and oligodendrogliomas are all derived from the same progenitor glial cell.
The development of gliomas in patients with MS almost certainly does not occur by chance and is not coincidental. Most astrocytomas are sporadic with no known cause, some, however, are associated with inherited genetic disorders, e.g. neurofibromatosis Type I. This is an autosomal dominant disorder with an incidence of one in 3,000 associated with the development of tumours such as neurofibrosarcoma and optic glioma (Ferner et al. 1995). This condition is also associated with the development of MS so that some intriguing molecular biological deficit appears to link glioma, MS and neurofibromatosis (Ferner et al. 1995; Alfonso et al. 1996; Masson and Colombani 1997). That common histogenesis is involved in this association is further supported in the finding of patients with MS, and glioma and Charcot-Marie-Tooth disease (Mathews and Moosy 1972). Furthermore, in patients with both gliomas and MS there are often multicentric origins of the neoplasm which, being a rare occurrence by itself, may suggest a common pathogenesis.
Since oligodendroglia are the predominant cells involved in demyelination, one might have expected such cells to proliferate in putative disorders, including neoplasms, associated with MS. Instead, the vast majority of neoplasms are either glioblastomas or astrocytomas (Appendix) involving different cells. Similarly, there is no evidence in most cases of a continuous transformation of the reactive glial cells of an MS plaque to an adjacent tumour; thus, the neoplastic transformation from reactive glial cells of the MS plaque is unlikely to be the mechanism. Some authors have, however, claimed that the neoplastic transformation of astrocytes has occurred from the activated cells within the MS plaque (Malmgren et al. 1984). Malmgren et al. (1984) commented on their case in which neoplastic astrocytes were found within the MS plaque suggesting that the neoplastic change had arisen de novo within the plaque.
Ho and Wolfe (1981) in their study of 20 cases found six astrocytomas that were multiple, which is a far greater number than is usually described as occurring in patients with glioma alone. Currie and Urich (1974) stressed that the high frequency of multiple sites of origin when glioma occurs with MS exceeded even “the exceptionally high estimate of 20% which (see Scherer 1940) gave as the frequency of multiple tumours in all cases of glioma”. This point is reinforced by Reagan and Freiman (1973), who refer to the very high incidence—up to 50%—of multifocal lesions in patients who have a glioma and MS.
Hypertrophic peripheral neuropathies
Clinical, electrophysiological, morphological and pathological studies have shown abnormalities in the peripheral nervous system in patients with MS (Schoene et al. 1977; Rosenberg and Bourdette 1983; Ro et al. 1983; Rubin et al. 1987; Thomas et al. 1987; Quan et al. 2005; Quan and Kleinschmidt-DeMasters 2005a, b). Pollock et al. (1977) found peripheral nerve abnormalities in 80% or more with reduction in myelin thickness. One difference was that the demyelinated and re-myelinated segments of the peripheral nerve did not extend laterally outside the spinal cord as occurred in MS plaques. There was no correlation with clinical findings. Earlier workers considered that these peripheral lesions were associated with malnutrition and avitaminosis (Hasson et al. 1958). Others have attributed them to an autoimmune mechanism; in some cases molecular genetic testing revealed myelin-protein gene duplication, characteristics of Type Ia Charcot-Marie-Tooth disease (Almsaddi et al. 1998). Interestingly, the molecular abnormalities in Charcot-Marie-Tooth neuropathy are found in intrinsic Schwann cell proteins and not in the axons (Griffin and Sheikh 1999). Charcot-Marie-Tooth neuropathy has been found in association with MS in several studies (Frasson et al. 1997; Rajabally and Abbott 2005; Isoardo et al. 2005a, b; Parman et al. 2007).
Other neuropathies have also been found in association with MS (Lassmann et al. 1981; Tachi et al. 1985; Mills and Murray 1986; Poser 1987; Acar et al. 2004; Kwon et al. 2008; Sharma et al. 2008).
The data showing involvement of the peripheral nerve system in patients with MS are overwhelming and includes altered supernormality in MS peripheral nerve (Eisen et al. 1982), reduced myelin thickness of internodes (Pollock et al. 1977), ultrastructural abnormalities in Schwann cells (Argyrakis 1980), gross onion bulb neuropathy (Schoene et al. 1977; Rosenberg and Bourdette 1983; Ro et al. 1983), normal regional curare test (Eisen et al. 1978), abnormal single fibre EMG (Weir et al. 1979), prolonged refractoriness of sensory nerves (Hopf and Eysholdt 1978) and abnormal slowing of motor conduction as evidenced by collision technique (Hopf 1963). In a classic case of severe onion bulb neuropathy associated with MS (Schoene et al. 1977), both of these diseases began simultaneously: whatever caused MS was likely to be involved in the initiation of onion bulb neuropathy (Schoene et al. 1977).
It would be reasonable to consider a promoting factor that caused proliferation both of Schwann cells and glia since the rise in the CSF protein early in the course of the disease suggests root involvement at the time of developing MS. Schwann cells and glia must therefore share a common receptor. The unique finding, in this case, of Schwann cells within the plaque in the spinal cord is very remarkable. Some workers have reported that peripheral myelin, i.e. the product of Schwann cells, can occur in MS plaques (Feigen 1969; Feigen and Ogata 1971). These earlier workers suggested that there must be pleuripotential stem cells within the cord so that the plaque contains in these unique cases multiplying glia and Schwann cells that arise from the pleuripotential cells. The rapid proliferation, in some way, perhaps by diverting normal metabolism may cause demyelination. For such an event to occur the milieu in the spinal cord must contain such a proliferating factor(s). Whether this comes from the cord itself or from the blood is unknown. Neuregulin and the erb B receptors are likely candidates (Cannella et al. 1999).
Neurofibromatosis
We were intrigued to find a young pregnant woman who presented with classical neurofibromatosis Type I and a progressive paraparesis. Investigations revealed the paraparesis to be secondary to a spinal cord MS plaque with multiple lesions throughout the white matter of the CNS. Two other cases referred to us suggested this might be more than coincidence, and a review of the literature showed neurofibromatosis, and MS had previously been reported to occur together (Huson et al. 1988; Ferner et al. 1993; 1995; Hinks et al. 1995; Alfonso et al. 1996; Masson and Colombani 1997; Johnson et al. 2000; Pál et al. 2001; Perini and Gallo 2001; Feuillet et al. 2004). We have subsequently identified several families in which MS and schwannomas occurred concurrently.
Neurofibromatosis is an autosomal dominant condition with a wide intrafamilial variability in clinical manifestations. About 50% of all cases represent new mutations. There is association with glial nodules in the brain and spinal cord and an increased incidence of glioma. The NF1 gene consists of 350 kb of genomic DNA and encodes for a protein of 2,818 amino acids, i.e. neurofibromin which is expressed in many different tissues. Its precise role is unknown, but it does act as a GTPase-activating protein in the same pathway of signal transduction as RAS (von Deimling et al. 1995), and it may act as a tumour suppressor in controlling the proliferation and differentiation of cells. Indeed, for normal embryological development to occur the spatial and temporal expression of the NF1 gene is crucial (von Deimling et al. 1995). The gene is located on chromosome 17q11.2 (Ratner and Daston 2001). These genes are enclosed in an intron of this gene including oligodendrocyte myelin glycoprotein. This membrane glycoprotein appears in the human brain around the time of myelination (von Deimling et al. 1995). The finding of an increased association of NF1 with glioma (Ratner and Daston 2001) and MS (Alfonso et al. 1996; Masson and Colombani 1997) suggests that this may reflect a shared pathogenesis. The finding of the gene for NF1 on chromosome 17q11.2 is of particular interest and importance (von Deimling et al. 1995).
MS, a metabolically determined neurodegenerative disorder?
Evidence from neuroimaging
Since the earlier work of Charcot, Dejerine, Marie and Dawson, neuronal loss in MS has been recognised, and more recently, confirmed by MRI, ultrastructural and magnetic resonance spectroscopy (MRS) studies. Neuronal loss in MS is an essential part of the disease since demyelination alone does not adequately explain the functional impairment and long-term disability (Matthew et al. 1998). It is also important to stress that there is significant heterogeneity in the pathological pattern of MS demyelination and myelin loss in MS is likely to be the final pathway of multiple pathogenic mechanisms (Lucchinetti et al. 1998).
Data from MRS clearly point to early metabolic changes in evolving MS lesions. Based on new magnetic resonance technology, it is now clear that metabolic changes appear first, often weeks before (e.g. 3 months in one study) the appearance of gadolinium (Gd)-enhancement in MS (Narayana et al. 1998). Total brain (rather than regional) N-acetyl aspartate (NAA), a marker of functional neuronal mass, correlates well with relapses (Gonen et al. 2000). Reduction of total brain NAA is an excellent predictor of focal relapses in MS, suggesting that relapses (and their biological marker, demyelination) are related to global reduction of brain metabolic function (reduced NAA) reversible in some cases (Matthew et al. 1998). Since white matter has a limited metabolic repertoire, compromised areas of white matter will retain water and swell. Increased water content in the metabolically compromised white matter will appear as increased signal in the T2-weighted images in MRI. Focal breakdown of blood–brain barrier (lesion enhancement) probably occurs in response to the metabolic changes, allowing macrophages to be drawn into the lesion. These cells will phagocytose the swollen myelin, representing the initial “inflammatory” infiltrate well documented in Dawson’s (1916) original observations. That global metabolic compromise is an integral component of developing MS lesions as indicated by the fact that grey matter lesions are always present, notably in the basal ganglia and at the grey-white junctional areas of the cortex (Gonen et al. 2000). This is distinct from primary oligodendroglial disease, as seen in progressive multifocal leucoencephalopathy (PML) that spares grey matter and (unlike MS), involves the subcortical “U” fibres. Unlike conventional MRI, magnetic resonance spectroscopy studies in MS have shown very significant axonal damage, even in the normal appearing white matter (NAWM) (Fu et al. 1998; Evangelou et al. 2000) early in the disease (Narayana et al. 1998). Magnetic resonance spectroscopy measures of NAA correlate with clinical changes in MS disability. Correlation has been found between the NAA cerebellar levels and the number of lesions (Davie et al. 1995). N-acetyl aspartate measures of corpus callosum in MS showed a progressive decline in the NAA resonance in a serial study (Arnold et al. 1994). This is also true for the spinal cord where reduced NAA levels correlated with reduced axonal areas in the spinal cord cross-sections in an autopsy study (Bjartmar et al. 2001). In contrast, post-mortem tissue sampling by using MRI has confirmed low specificity of T2-weighted imaging. Using in vivo quantitative MR studies, T1-weighted images were found to be more relevant than T2-weighted images in identifying lesions that cause disability. T1 hypointensity (“black holes”) on the other hand, strongly correlated with axonal loss (van Waesberghe et al. 1999).
Metabolic changes were observed well before the appearance of magnetic resonance lesions—in serial MR studies that included proton MR spectroscopic imaging (MRSI), contrast-enhanced MRI imaging and volumetric lesion studies of 25 patients with mild to moderate clinical deficits over a period of 2 years (Narayana et al. 1998). Regional metabolite changes were both dynamic and reversible. In four patients, strong lipid peaks in the absence of Gd-enhancement and magnetic resonance-defined lesions were observed, clearly indicating that demyelination can occur independent of “inflammatory” changes. It should be remembered that, when examined at autopsy, one-third of all plaques contain no inflammatory infiltrates (Adams 1989). While focal reductions in NAA levels did not always imply axonal loss, reduction in whole brain NAA was a putative marker of the MS disease burden (Narayana et al. 1998). As compared to healthy controls, reduction in whole brain NAA in this study was found to be greater in older than younger patients consistent with the clinical experience that older MS patients usually have worse outcomes. The age-dependent decrease of whole brain NAA in MRS suggests that progressive neuronal cell loss is a cardinal feature of the disease, very similar to other neurodegenerative diseases. The similarity of cerebellar MRS changes in MS patients with cerebellar symptoms and autosomal dominant cerebellar ataxia attest to this view (Davie et al. 1995).
Direct pathological studies of the NAWM have revealed axonal loss, and the degree of volume loss was greater than one would anticipate from MS demyelinating lesions alone (Evangelou et al. 2000). Recently, it was shown with T1-weighted magnetic resonance follow-up studies that the degree of “inflammatory activity” is a poor predictor of not only T1 but also T2-lesion load at long-term follow-up, indicating that the T2-lesion load is not an accurate measure of the MS pathology (van Waderveen et al. 1999). Consistent with the previous observations, the authors of the latter study found that the baseline T1-lesion load was the single most important factor in the subsequent increases in hypointense T1 lesion load. Taken together, these findings clearly confirm that the so-called inflammatory-demyelinating indices in conventional MRI (abnormal increased signals in T2-weighted MRI and Gd-enhancement) do not predict long-term MS disability and are poor outcome measures for treatment trials designed to prevent progression to disability. It also appears that long-term MS disability is largely predetermined by the axonal loss already present at the symptom onset, a feature characteristic of neurometabolic and degenerative diseases. Imaging and pathological studies in chronic demyelinated cervical spinal cord plaques clearly indicate that slow axonal degeneration rather than acute changes is responsible for chronic disability in MS. A predominance of widespread NAWM changes over focal lesions appears to be the hallmark of primary progressive MS (Matthew et al. 1998). These observations support the conclusions of a recent MS epidemiological study proposing a biological dissociation between relapse rate and progressive functional disability as being characteristic of the natural history in MS (Confavreux et al. 2000).
Relationship of glial proliferation and metabolic changes to MRI abnormalities
Diffusion of water molecules in relation to the directional organisation of the myelinated white matter can be measured by diffusion tensor MRI. In this form of neuroimaging, magnitude and translational motion of the water molecules (‘anisotropy’) with respect to the white matter fibre tracts can be defined. Myelin and cell membranes provide natural barriers to diffusion across the white matter fibres (Beaulieu and Allen 1994). As a result, the water molecules can diffuse only along these fibres. Therefore, a high degree of anisotropy is expected in normal myelinated white matter fibres, and this has been confirmed in histologic and imaging studies (Beaulieu and Allen 1994; Pierpaoli et al. 1996; Hajnal et al. 1999; Werring et al. 1999). On the other hand, decreases in diffusion anisotropy have been shown to occur in diseases that affect myelin or axonal integrity, such as MS, neurodegenerative diseases, cerebral ischaemia and leucodystrophies (Hajnal et al. 1999; Sorensen et al. 1999; Tivesky et al. 1999; Werring et al. 1999; Guo et al. 2001).
In MS, reduction in the fractional anisotropy in diffusion tensor MRI precedes any other change in the conventional MRI. This applies to patients with clinically definite MS and normal T2-weighted magnetic resonance scans (Fillipi et al. 1999), and patients with clinically isolated syndromes suggestive of MS (Iannucci et al. 2000). The anisotropy measurements also correlate well with evidence from histologic and MRS studies (Guo et al. 2002). It is thus clear that the disease process in MS extends well beyond the borders of the plaque identified in the T2-weighted images. There is a progressive gradient in the decline of anisotropy observed in MS from the NAWM to the peri-plaque and intra-plaque white matter with the latter showing the most extensive changes. A progressive decrease of magnetisation transfer ratio is also seen to extend from the remote NAWM towards the plaque (Guo et al. 2002). In contrast, the white matter abnormalities in ADEM do not extend beyond the focal areas of injury, and the magnetisation transfer ratios of the uninvolved brain and spinal cord in ADEM is practically identical to the values observed in the healthy control subjects (Inglese et al. 2002). The anisotropic changes in the normal appearing brain tissue is always present in all clinical phenotypes of MS irrespective of their presentations (Fillipi et al. 1999; Iannucci et al. 2000; Tortorella et al. 2000).
The basis of the anisotropic gradient that extends from the NAWM to the fully formed MS plaque in MS is important in the understanding of its pathogenesis. Irrespective of the clinical phenotype, two consistent abnormalities are revealed in the MS brain by the newer imaging technologies. First, there is reduced brain metabolism, and second, the water diffusibility is reduced along the white matter fibre tract, and the plaque is centred round the area where the anisotropy is lowest. Such findings are unique to MS, being absent in ADEM, Devic’s neuromyelitis and in patients with other systemic immunological diseases associated with multiple T2-weighted signal abnormalities in the MRI (Rovaris et al. 2000). Changes in MRS and diffusion tensor imaging appear to occur before other magnetic resonance changes and correlate with functional impairment in MS (Guo et al. 2002). Results of a follow-up study showed that 80% of the newly formed MS lesions are hypointense on unenhanced T1-weighted scans associated with the highest anisotropy changes (van Waesberghe et al. 1998). However, more than half (44%) of these new lesions returned to isointensity spontaneously during the course of the follow-up (van Waesberghe et al. 1998). This spontaneous reversibility is very characteristic of metabolic disease. Data from the MRS and diffusion tensor imaging do, therefore, suggest that MS is a neurodegenerative disease in which the rate of myelin loss is metabolically determined. In this paradigm, plaque formation is a subacute process that follows a failure of metabolic reversibility and characteristically occurs in an area farthest from the NAWM. This is comparable to the zonal architecture proposed in the functional anatomy of the hepatic lobule where the metabolic changes tend to be maximum towards the periphery of the lobule.
It may not be out of place to consider possible explanations for reduced anisotropy in MS. As already noted, anisotropic changes in the MS brain are extensive, being abnormal in virtually all white matter regions and always extending well beyond the focal areas of myelin loss (Guo et al. 2002). In the developing brain, increased permeability and anisotropic diffusion across myelin have been shown to occur before the onset of myelination. Premyelination anisotropy may be due to a number of changes, including an increase in the fibre diameter and axonal membrane changes (Huppi et al. 2001). This may explain why demyelination may occur in infancy or in the structural disorders of axons and myelin (leucodystrophies). It has also been postulated that as a result of change in energy metabolism, oligodendrocytes may fail to meet the required energy demand in mitochondrial encephalopathies, thus leading to demyelination. However, anisotropy may also be reduced by glial proliferation (Majoie et al. 2002). Because glial cells are fairly amorphous and glial proliferation is not a structurally organised process, anisotropy will be reduced in areas where glial proliferation occurs (Fillipi et al. 2001). It is our contention that the reduced anisotropy in the MS brain is a direct function of glial proliferation, and consequent metabolic changes in the myelin leads to plaque formation by way of increased permeability. It is the generalised glial proliferation in MS that accounts for the globally reduced anisotropy; the metabolic changes contribute to the formation of plaque in the areas of maximum compromise.
A final comment has to be made about the so-called “inflammatory” magnetic resonance lesions. The conventional MRI data (T2-weighted and Gd-enhancement) in MS merely show that some MR plaques are swollen (oedematous) with a breakdown of the blood–brain barrier. These changes would certainly be expected if myelin and cell membrane permeabilities are altered. However, to suggest that these magnetic resonance changes in the MS plaques reflect specific T cell-mediated autoimmune inflammatory process has not yet been substantiated. As previously stated, at least one-third of MS plaques in pathological studies show no evidence of inflammatory infiltrate, and the mononuclear infiltrate in the other plaques is either mild or inconsistent. Comparable infiltrates are encountered, as described, in diseased brain due to stroke, tumour or indeed, even in Alzheimer’s or motor neurone disease. Logic therefore dictates that cellular infiltrates are unlikely to be responsible for oedema in the MS plaques or focal breakdown in the blood–brain barrier. This is certainly supported by the data from the magnetisation transfer and diffusion tensor MRI in MS.
Pregnancy and MS
The effect of pregnancy on MS provides an important clue to the nature of this yet unknown factor stimulating glial proliferation and reducing myelin metabolism. Pregnancy has an apparent stabilising effect on the clinical course of MS. Indeed, Confavreux has commented that the effect of pregnancy on MS is better than the treatment effects of β-interferon or glatiramer acetate (Confraveux 2002). However, the 3-month, post-partum period shows an increasing relapse rate. The effect of pregnancy on MS contrasts sharply with systemic lupus erythematosus (SLE), a classical autoimmune disease, where a flare-up of disease is common during pregnancy.
Comparative epidemiology of MS and neurodegenerative diseases
In this review, we have shown that MS is not an autoimmune disease due to its intrinsic clinical, immunological, radiological and histological differences with ADEM and its experimental animal model, EAE. In our opinion, MS has the characteristics of a metabolically determined neurodegenerative disorder with strong genetic influence. There is now evidence from epidemiological studies that other neurodegenerative diseases (Parkinson’s disease and motor neurone disease), once thought to be evenly spread and occur at a uniform rate throughout the world, to be influenced by geographic factors similar to MS (Betemps and Buncher 1993). This analogy can be extended further in that we, and others, have shown that MS may be precipitated, but not caused, by specific trauma to the CNS (Poser 2000; Chaudhuri and Behan 2001). Trauma has also been implicated in the precipitation of both Parkinson’s disease and of motor neurone disease (Jankovic 1994; Cardoso and Jankovic 1995). Of great interest is the finding that electrical injuries were found to be statistically significant in a prospective study of physical trauma and MS (Sibley et al. 1991), and both motor neurone disease (Kurtzke and Beebe 1980; Kelly and Shapiro 2001) and Parkinson’s disease (Morris et al. 1998) have been described as occurring following electrical injuries.
Further data indicating that MS is a progressive neurodegenerative disorder is found in a recent study looking at clinical analysis of 250 families in which a cohort of 262 pairs of co-affected siblings were studied (Chataway et al. 2001). The authors of this report found that once the disease was established, concordance was more related to the ultimate clinical course than to the number of attacks or presentation and the end result of disability and handicap scores was similar (Chataway et al. 2001).
The proposition that MS is a prototype autoimmune disease is weak and open to question: MS is not a model of EAE or indeed, of any autoimmune disease. Its histology compares more favourably with other forms of demyelination known to be metabolic in aetiology, such as leucoencephalopathies due to mitochondrial encephalopathy, central pontine myelinolysis and Marchiafava-Bignami disease. Many scholars of MS in the past have argued strongly that the disease is toxic/metabolic in origin (Wolfgram 1979). The suggested association of a HLA in MS is neither strong nor persuasive. Such data for a claimed association with DR2 would argue against any link with diabetes since DR2 protects against this disorder. Whatever immunologic finding that has been claimed to be specific for MS is soon found wanting. There is never a shortage of candidates such as the heat-shock protein of β crystalline that is found in brains with other neurological diseases as well as normals (van Noort et al. 1995). It genuinely is time to seek a paradigm shift in the pathogenesis of MS and look anew at the known facts.
Conclusion
Multiple sclerosis remains a disease of unknown aetiology. In the recent years, most researchers have uncritically accepted the hypothesis that it is an autoimmune disorder. An in-depth review of the literature failed to support this concept, and the immunological claims for this disease are tenuous and fragile. There is no one specific immunological abnormality found in MS that does not occur in patients with other diseases or in normal controls. The acceptance of EAE as a model for MS is an unfortunate error that has its basis on faith rather than science. Whilst EAE is a good example of an experimental organ-specific autoimmune disorder in animals, it however cannot be accepted as a model for MS for a wide variety of reasons. This is particularly important in relation to the development of MS pharmacotherapy. We have analysed the literature on immune-modifying therapy in MS, and it is clear that none of these agents can qualify as a candidate therapy under scrutiny.
A clear association of MS exists with other glial disorders of proliferation and differentiation. Based on comparative neuropathology and neuroimaging data, it is proposed that the initial lesion in MS is one of astrocytic proliferation and plaque formation and is a consequence of metabolic abnormality affecting myelin permeability. We believe that these pathogenic changes in MS are influenced by a combination of genetic and environmental factors. One of the genes most likely to be involved in MS pathogenesis may be located on chromosome 17. The gene expression in MS is influenced by external factors, and whilst such factors have not been identified with certainty, one of these is likely to be the influence of sunlight, perhaps mediated through vitamin D metabolism (McGrath 2001).
Abbreviations
- ADEM:
-
Acute disseminated encephalomyelitis
- AHLE:
-
Acute haemorrhagic leucoencephalomyelitis
- CNS:
-
Central nervous system
- EAE:
-
Experimental allergic encephalomyelitis
- HLA:
-
Histocompatibility antigen (human leucocyte antigen)
- MS:
-
Multiple sclerosis
- MHC:
-
Major histocompatibility complex
- MRI:
-
Magnetic resonance imaging
- MRS:
-
Magnetic resonance spectroscopy
- MRSI:
-
Proton magnetic resonance spectroscopic imaging
- NAA:
-
N-acetyl aspartate
- NAWM:
-
Normal appearing white matter
- PNS:
-
Peripheral nervous system
- RNA:
-
Ribonucleic acid
References
Aarli JJ, Mork SJ, Myrseth E et al (1989) Glioblastoma associated with multiple sclerosis: coincidence of induction? Eur Neurol 29:312–316
Acar MA, Birch MK, Abbott R, Rosenthal AR (1993) Chronic granulomatous anterior uveitis associated with multiple sclerosis. Graefes Arch Clin Exp Opthalmol 231:166–168
Acar G, Tanriover G, Demir N, Kayisli UA, Sati GL, Yaba A, Idiman E, Demir R (2004) Ultrastructural and immunohistochemical similarities of two distinct entities; multiple sclerosis and hereditary motor sensory neuropathy. Acta Histochem 106(5):363–371
Adams RD (1959) A comparison of the morphology of the human demyelinating diseases and experimental “allergic encephalomyelitis”. In: Kies MW, Alvord EC (eds) “Allergic” encephalomyelitis, chap 5. Charles C Thomas, Washington, DC, pp 183–209
Adams CWM (1977) Pathology of multiple sclerosis: progression of the lesion. Br Med Bull 3:15–20
Adams CWM (1989) Histology and cellular features of multiple sclerosis. In: A colour atlas of multiple sclerosis and other myelin disorders. Wolfe Medical Pubs Ltd, London, pp 130–139
Adams RD, Sidman RL (1968) The glial cells and their pathological reactions. In: Introduction to neuropathology. McGraw-Hill, New York, p 33
Adams RD, Sidman RL (1968) Introduction to neuropathology. McGraw-Hill, New York, p 34
Adams CWM, Poston RN, Buk SJ et al (1985) Inflammatory vasculitis in multiple sclerosis. J Neurol Sci 69:269–283
Aihara N, Tanno H, Hall JJ et al (1994) Immunocytochemical localisation of immunoglobulins in the rat brain: relationship to the blood-brain barrier. J Comp Neurol 342:481–496
Aita FJ, Snyder HD, Reichl W (1974) Myasthenia gravis and multiple sclerosis: an unusual combination of diseases. Neurology 24:72–75
Alfonso S, Roquer J, Pou A (1996) Multiple sclerosis and neurofibromatosis 1. Neurologia 11(6):233–235 (in Spanish)
Almsaddi M, Bertorini TE, Seltzer WK (1998) Demyelinating neuropathy in a patient with multiple sclerosis and genotypical HMSN-1. Neuromusc Dis 8:87–89
Alter M, Sawyer GT, Latham K (1970) The frequency of diabetes mellitus in families of patients with multiple sclerosis. Neurology 20:619–621
Amato MP, Ponziani G, Bartolozzi ML et al (1999) A prospective study on the natural history of multiple sclerosis: clues to the conduct and interpretation of clinical trials. J Neurol Sci 168:96–106
Antel JP, Arnason BGW, Medof ME (1979) Suppressor cell function in multiple sclerosis; correlation with clinical disease activity. Ann Neurol 5:338–349
Antel JP, Nicholas MK, Bania MB et al (1986) Comparison of T8+ cell-mediated suppressor and cytotoxic functions in multiple sclerosis. J Neuroimmunol 12:215–224
Argyrakis A (1980) Ultrastructural changes in peripheral nerves in multiple sclerosis and subacute sclerosing panencephalitis. In: Bauer HJ, Poser S, Ritter G (eds) Progress in multiple sclerosis research. Springer, Berlin, pp 360–364
Arnold DL, Reiss GT, Matthews PM et al (1994) Use of proton magnetic resonance spectroscopy for monitoring disease progression in multiple sclerosis. Ann Neurol 36:76–82
Arstila AU, Riekkinen PJ, Rinne UK et al (1973) Studies of the pathogenesis of multiple sclerosis. Participation of lysosomes in demyelination in the CNS white matter. Europ Neurol 9:1–21
Aubert L, Arroyo H, Dumas B et al (1968) Un can d’association entre sclerose en plaques et glioblastome cerebral. Rev Neurol 119:374–376
Aujeszky A (1900) Ueber Immunisirung gegen Wut mit normaler Nervensubstanz. Centralbl Bakt Jena 27:5–10
Baker D, Rosenwasser OA, O’Neil JK et al (1995) Genetic analysis of experimental allergic encephalomyelitis in mice. J Immunol 155:4046–4051
Baranzini SE, Mudge J, van Velkinburgh JC et al (2010) Genome, epigenome and RNA sequences of monozygotic twins discordant for multiple sclerosis. Nature 464(7293):1351–1356
Barnard RO, Geddes JF (1987) The incidence of multifocal cerebral gliomas. Cancer 60:1519–1531
Barnard RO, Jellinek EH (1967) Multiple sclerosis with amyotrophy complicated by oligodendroglioma. J Neurol Sci 5:441–455
Bartt RE (2006) Multiple sclerosis, natalizumab therapy, and progressive multifocal leukoencephalopathy. Curr Opin Neurol 19:341–349
Bassoe P, Grinker RR (1930) Human rabies and rabies vaccine encephalomyelitis: a clinicopathological study. Arch Neurol Psychiatry 23:1138–1160
Beaulieu C, Allen PS (1994) Determinants of anisotropic water diffusion in nerves. Magn Reson Med 31:394–400
Beecher HK (1955) The powerful placebo. JAMA 159:1602–1606
Behan PO (1980) Dorsal column stimulation in multiple sclerosis. BMJ 2:1287–1288
Behan PO, Currie S (1978) Acute disseminated encephalomyelitis. In: Clinical neuroimmunology, chap 4. Saunders, London, pp 49–61
Behan PO, Haniffah BAG (1994) The genetics of myasthenia gravis. In: Lisak RP (ed) Handbook of myasthenia gravis and myasthenic syndromes. Marcel Dekker Inc, pp 165–191
Behan PO, Geshwind N, Lamarche JB et al (1968) Delayed hypersensitivity to encephalitogenic protein in disseminated encephalitis. Lancet ii:1009–1012
Behan PO, Behan WMH, Feldman RG et al (1972) Cell-mediated hypersensitivity to neural antigens. Arch Neurol 27:145–152
Behan PO, Kies MW, Lisak RP et al (1973) Immunologic mechanisms in experimental encephalomyelitis in non-human primates. Arch Neurol 29:4–9
Behan PO, Melville ID, Durward WF et al (1976) Transfer-factor therapy in multiple sclerosis. Lancet i:988–990
Behan PO, Chaudhuri A, Roep BO (2002) The pathogenesis of multiple sclerosis revisited. J R Coll Physicians Edinb 32:244–265
Bell J, Lathrop G (1996) Multiple loci for multiple sclerosis. Nat Genet 13:377–378
Ben-Nun A, Liblau RS, Cohen L et al (1991) Restricted T-cell receptor gene usage by myelin basic protein-specific T-cell clones in multiple sclerosis. Predominant genes vary in individuals. Proc Natl Acad Sci USA 88:2466–2470
Berger JR, Sheremata WA, Resnick L et al (1989) Multiple sclerosis-like illness occurring with human immunodeficiency virus infection. Neurology 39:324–329
Betemps EJ, Buncher CR (1993) Birthplace as a risk factor in motor neurone disease and Parkinson’s disease. Int J Epidemiol 22(5):898–904
Betters E, Liu Y, Kjaeldgaard A, Sundström E, García-Castro MI (2010) Analysis of early human neural crest development. Dev Biol 344(2):578–592
Bielekova B, Richert N, Howard T, Blevins G, Markovic-Plese S, McCartin J, Frank JA, Würfel J, Ohayon J, Waldmann TA, McFarland HF, Martin R (2004) Humanized anti-CD25 (daclizumab) inhibits disease activity in multiple sclerosis patients failing to respond to interferon β. Proc Natl Acad Sci USA 101:8705–8708
Bjartmar C, Kinkel RP, Kidd G et al (2001) Axonal loss in normal-appearing white matter in a patient with acute MS. Neurology 57:1248–1252
Boyazis RM, Martin L, Bouteille M et al (1968) Images histochimiques et ultrastructurales dans un cas de sclerose en plaques associee a un spongioblastome. Riv Pat Nerv Ment 88:1–20
Brain W, Wilkinson M (1957) The association of cervical spondylosis and disseminated sclerosis. Brain 80:456–478
Brandt S, Gyldensted C, Offner H et al (1981) Multiple sclerosis with onset in a two-year old boy. Neuropaediatrics 12(1):75–82
Breger BC, Leopold IH (1966) The incidence of uveitis in multiple sclerosis. Am J Opthalmol 62:540–545
Brihaye J, Perier O, Stenuit J (1963) Multiple sclerosis associated with a cerebral glioma. J Neuropath Exp Neurol 22:128–137
Brinkman CJJ, Nillesen WM, Hommes OR et al (1982) Cell-mediated immunity in multiple sclerosis as determined by sensitivity of different lymphocyte populations to various brain tissue antigens. Ann Neurol 11:450–455
Broadley SA, Deans J, Sawcer SJ et al (2000) Autoimmune disease in first-degree relatives of patients with multiple sclerosis. A UK survey. Brain 123:1102–1111
Burgerman R, Rigaminto E, Randle JM et al (1992) The association of cervical spondylosis and multiple sclerosis. Surg Neurol 38:265–270
Burns J, Rosenweig A, Zweiman B et al (1983) Isolation of myelin basic protein-reactive T-cell lines from normal human blood. Cell Immunol 81:435–440
Calabresi PA (2002) Considerations in the treatment of relapsing-remitting multiple sclerosis. Neurology 58(Suppl 4):S10–S22
Cannella B, Pitt D, Marchionni M et al (1999) Neuregulin and erbB receptor expression in normal and diseased human white matter. J Neuroimmunol 100(1–2):233–242
Cardoso F, Jankovic J (1995) Peripherally induced tremor and parkinsonism. Arch Neurol 52:263–270
Carson KR, Focosi D, Major EO et al (2009) Monoclonal antibody-associated progressive multifocal leucoencephalopathy in patients treated with rituximab, natalizumab, and efalizumab: a review from the Research on Adverse Drug Events and Reports (RADAR) project. Lancet Oncol 10:816–824
Chataway J, Mander A, Robertson N et al (2001) Multiple sclerosis in sibling pairs: an analysis of 250 families. J Neurol Neurosurg Psychiatry 71:757–761
Chaudhuri A, Behan PO (2001) Acute cervical hyperextension-hyperflexion injury may precipitate and/or exacerbate symptomatic multiple sclerosis. Eur J Neurol 8:659–664
Chaudhuri A, Behan PO (2004) Multiple sclerosis is not an autoimmune disease. Arch Neurol 61:1610–1612
Chaudhuri A, David K (2009) Behan Po. Cervical cord demyelination due to physical trauma. J Neurol Sci 285(S1):S155–S339
Clarke M, Alderson P, Chalmers I (2002) Discussion sections in reports of controlled trials published in general medical journals. JAMA 287:2799–2801
Cohen JA, Lisak RP (1987) Acute disseminated encephalomyelitis. In: Aarli JA, Behan WMH, Behan PO (eds) Clinical neuroimmunology, vol 15. Blackwell, Oxford, pp 192–213
Coles A, Compston DA et al (2008) (The CAMMS223 Trial Investigators) alemtuzumab vs. interferon beta-1a in early multiple sclerosis. N Engl J Med 359:1786–1801
Compston A (1998) Treatment and management of multiple sclerosis. In: Compston A, Ebers G, Lassmann H et al (eds) McApline’s multiple sclerosis. Churchill Livingstone, Edinburgh, pp 437–498
Compston A, Coles A (2002) Multiple sclerosis. Lancet 359:1221–1231
Confavreux C, Vukusic S, Moreau T et al (2000) Relapses and progression of disability in multiple sclerosis. N Eng J Med 343:1430–1438
Confraveux C (2002) Relapses, progression, inflammation and neurodegeneration in multiple sclerosis: a changing view. Adv Clin Neurosci Rehabil 2(1):7–9
Cook SD, Devereux C, Troiano R et al (1986) Effect of total lymphoid irradiation in chronic progressive multiple sclerosis. Lancet 1:1405–1409
Cook SD, Devereux C, Troiano R et al (1987) Total lymphoid irradiation in multiple sclerosis: blood lymphocytes and clinical course. Ann Neurol 22:634–638
Cook SD, Troiano R, Zito G et al (1989) Deaths after total lymphoid irradiation for multiple sclerosis. Lancet 2:277–278
Cook SD, Devereux C, Triano R et al (1995) Combination total lymphoid irradiation and low dose corticosteroid therapy for progressive multiple sclerosis. Acta Neurol Scand 91:22–27
Cossais F, Wahlbuhl M, Kriesch J, Wegner M (2010) SOX10 structure-function analysis in the chicken neural tube reveals important insights into its role in human neurocristopathies. Hum Mol Genet 19(12):2409–2420
Costa MF, Novis SAP, Filho PN et al (2000) Esclerose Multipla, Ependimoma Medular E Meningioma Intracraniano. Arq Neuropsiquiatr 58(4):1133–1137
Currie S, Urich H (1974) Concurrence of multiple sclerosis and glioma. J Neurol Neurosurg Psychiatry 37:598–605
Davie CA, Barker GJ, Webb S et al (1995) Persistent functional deficit in multiple sclerosis and autosomal dominant cerebellar ataxia is associated with axon loss. Brain 118:1583–1592
Dawson J (1916) The histology of disseminated sclerosis. Trans R Soc Edinb 50:517–540
De Caso R (2000) Esclerose Multipla, ependimoma medular e meningioma intracraniano. Arq Neuropsiquiatr 58:1133–1137
Devereux CK, Vidaver R, Hafstein MP et al (1988) Total lymphoid irradiation for multiple sclerosis. Int J Radiat Oncol Biol Phys 14:197–203
Dhib-Jalbut S (2002) Mechanisms of action of interferons and glatiramer acetate in multiple sclerosis. Neurology 58(Suppl 4):S3–S9
Edwards LJ, Constantinescu CS (2004) A prospective study of conditions associated with multiple sclerosis in a cohort of 658 consecutive outpatients attending a multiple sclerosis clinic. Mult Scler 10:575–581
Eisen A, Yufe R, Trop D et al (1978) Reduced neuromuscular transmission safety factor in multiple sclerosis. Neurology 28:498–602
Eisen A, Paty D, Hoirch M (1982) Altered supernormality in multiple sclerosis peripheral nerve. Muscle Nerve 5:411–414
Engelhardt JI, Tajti J, Appel SH (1993) Lymphocytic infiltrates in the spinal cord in amyotrophic lateral sclerosis. Arch Neurol 50:30–36
Esiri MM, Gay D (1997) The immunocytochemistry of multiple sclerosis plaques. In: Raine CS, McFarland HF, Tourtellotte WW (eds) Multiple sclerosis: clinical and pathogenic basis. Chapman & Hall, London, pp 173–186
Espicom Business Intelligence Ltd (2008) CNS drug discoveries: multiple sclerosis chapter. Espicom Business Intelligence Ltd., p 128. http://www.researchandmarkets.com/product/c33228/cns_drug_discoveries_multiple_sclerosis_chap. Accessed 01 May 2009
Evangelou N, Esiri MM, Smith S et al (2000) Quantitative pathological evidence for axonal loss in normal appearing white matter in multiple sclerosis. Ann Neurol 47:391–395
Feigen I (1969) Mesenchymal tissues of the nervous system, the indigenous origin of brain macrophages in hypoxic states and in multiple sclerosis. J Neuropathol Exp Neurol 28:6–23
Feigen I, Ogata J (1971) Schwann cells and peripheral myelin within human central nervous tissues: the mesenchymal character of Schwann cells. J Neuropathol Exp Neurol 30:603–612
Ferner RE, Chaudhuri R, Bingham J et al (1993) MRI in neurofibromatosis 1. The nature and evolution of increased intensity T2 weighted lesions and their relationship to intellectual impairment. J Neurol Neurosurg Psychiatry 56:492–495
Ferner RE, Hughes RAC, Johnson MR (1995) Neurofibromatosis1 and multiple sclerosis. J Neurol Neurosurg Psychiatry 58:582–585
Feuillet L, Boudinet H, Casseron W, Uzenot D, Pelletier J, Ali Cherif A (2004) Multiple sclerosis associated with neurofibromatosis type I. Rev Neurol 160(4 Pt 1):447–451 (in French)
Fillipi M, Rocca MA, Minicucci L et al (1999) Magnetization transfer imaging of patients with definite MS and negative conventional MRI. Neurology 52:845–848
Fillipi M, Cercignani M, Inglese M et al (2001) Diffusion tensor magnetic resonance imaging in multiple sclerosis. Neurology 56:304–311
Frasson E, Polo A, Di Summa A, Fabrizi GM, Taioli F, Fiaschi A, Rizzuto N, Moretto G (1997) Multiple sclerosis associated with duplicated CMT1A: a report of two cases. J Neurol Neurosurg Psychiatry 63(3):413–414
Freedman MS, Muth KL, Trotter JL et al (1992) Prospective serial analysis of interleukin-2 receptor in relapsing-remitting multiple sclerosis. Neurology 42:1596–1601
Freund J, Stern ER, Pisani TM (1947) Isoallergic encephalomyelitis and radiculitis in guinea pigs after one injection of brain and mycobacteria in water-in-oil emulsion. J Immunol 57:179–194
Fritz RB, Skeen MJ, Jen-Chou CH et al (1985) Major histocompatibility complex-linked control of the murine immune response to myelin basic protein. J Immunol 134:2328–2332
Fu L, Matthews PM, De Stefano N et al (1998) Imaging axonal damage in the normal appearing white matter in multiple sclerosis. Brain 121:103–113
Ganter P, Prince C, Esiri MM (1999) Spinal cord axonal loss in multiple sclerosis: a post-mortem study. Neuropathol Appl Neurobiol 25:459–467
Gibbs E, Tremlett H, Ball N, Hasimoto S (2008) Malignant melanoma in a multiple sclerosis patient with persistent neutralising antibodies to interferon-beta. Eur J Neurol 15:e4
Glanzmann E (1927) Die Nervosen Komplicationen der Varizellen der Variola und Vakzine. Schweiz Med Wochenschr 57:145–154
Gonen O, Catalaa I, Babb JS et al (2000) Total brain N-acetylaspartate: a new measure of disease load in multiple sclerosis. Neurology 54:15–19
Graham DI, Behan PO, More IAR (1979) Brain damage complicating septic shock. J Neurol Neurosurg Psychiatry 42:19–28
Greve B, Simonenko R, Illes Z, Peterfalvi A, Hamdi N, Mycko MP, Selmaj KW, Rozsa C, Rajczy K, Bauer P, Berger K, Weissert R (2008) Multiple sclerosis and the CTLA4 autoimmunity polymorphism CT60: no association in patients from Germany, Hungary and Poland. Mult Scler 14:153–158
Griffin WST (2008) Perispinal etanercept: potential as an Alzheimer therapeutic. J Neuroinflammation 5:3
Griffin JW, Sheikh K (1999) Schwann cell-axon interactions in Charcot-Marie-Tooth disease. Ann N Y Acad Sci 883:77–90
Guilhoto LMRR, Osorio CAM, Machado LB (1995) Paediatric multiple sclerosis report of 14 cases. Brain Dev 17:9–12
Gulcher JR, Vartanian T, Stefansson K (1994) Is multiple sclerosis an autoimmune disease? Clin Neurosci 2:246–252
Guo AC, Petrella JR, Kurtzberg J et al (2001) Evaluation of white matter anisotropy in Krabbe disease using diffusion tensor MR imaging; initial experience. Radiology 218:809–815
Guo AC, MacFall JR, Provenzale JM (2002) Multiple sclerosis: diffusion tensor MR imaging for evaluation of normal appearing white matter. Radiology 222:729–736
Guseo A, Jellinger K (1975) The significance of perivascular infiltrations in multiple sclerosis. J Neurol 211:51–60
Hafler DA (2004) Multiple sclerosis. J Clin Invest 113:788–794
Hafler DA, Buchsbaum M, Johnson D et al (1985) Phenotypic and functional analysis of T-cells cloned directly from the blood and cerebrospinal fluid of patients with multiple sclerosis. Ann Neurol 18:451–458
Haines J et al (1998) Linkage of the MHC to familial multiple sclerosis suggests genetic heterogeneity. Hum Mol Genet 7:1229–1234
Hajnal JV, Dornan M, Hall AS et al (1999) Clinical use of diffusion-tensor imaging for diseases causing neuronal and axonal damage. Am J Neuroradiol 20:1044–1048
Hasson J, Terry RD, Zimmerman M (1958) Peripheral neuropathy in multiple sclerosis. Neurology 8(7):503–510
Hauser SL, Dawson DM, Lehrich JR et al (1993) Intensive immunosuppression in progressive multiple sclerosis: a randomised, three-arm study of high-dose intravenous cyclophosphamide, plasma exchange, and ACTH. N Eng J Med 308:173–180
Hauser SL, Waubant E, Arnold DL, Vollmer T, Antel J, Fox RJ, Bar-Or A, Panzara M, Sarkar N, Agarwal S, Langer-Gould A, Smith CH (2008) B-cell depletion with rituximab in relapsing-remitting multiple sclerosis. N Engl J Med 358:676–688
Heinzlef O, Alamowitch S, Sazdovitch S et al (1999) Autoimmune disease in families of French patients with multiple sclerosis. Acta Neurol Scand 100:1–5
Hinks LJ, Price SE, Mason CR, Thompson RJ (1995) Single strand conformation analysis of two genes contained within the first intron of the neurofibromatosis type I gene in patients with multiple sclerosis. Neuropathol Appl Neurobiol 21(3):201–207
Ho KL, Wolfe DE (1981) Concurrence of multiple sclerosis and primary intracranial neoplasms. Cancer 47:2913–2919
Holfield R, Wiendl H (2002) The ups and downs of multiple sclerosis therapeutics. Ann Neurol 49(3):281–284
Hopf HC (1963) Electromyographic study on so-called mononeuritis. Arch Neurol 9:307–312
Hopf HC, Eysholdt M (1978) Impaired refractory periods of peripheral sensory nerves in multiple sclerosis. Ann Neurol 4:499–501
Huppi PS, Murphy B, Maier SE et al (2001) Microstructural brain development after perinatal cerebral white matter injury assessed by diffusion tensor magnetic resonance imaging. Paediatrics 107:455–460
Huson SM, Harper PS, Compston DAS (1988) Von Recklinghausen neurofibromatosis. A clinical and population study in south-east Wales. Brain 111:1355–1381
Iannucci G, Tortorella C, Rovaris M et al (2000) Prognostic value of MR and magnetization transfer imaging findings in patients with clinically isolated syndromes suggestive of multiple sclerosis at presentation. Am J Neuroradiol 21:1034–1038
Ifergan I, Wosik K, Cayrol R, Kébir H, Auger C, Bernard M, Bouthillier A, Moumdjian R, Duquette P, Prat A (2006) Statins reduce human blood-brain barrier permeability and restrict leukocyte migration: relevance to multiple sclerosis. Ann Neurol 60(1):45–55
Inglese M, Salvi F, Iannucci G et al (2002) Magnetization transfer and diffusion tensor MR imaging of acute disseminated encephalomyelitis. Am J Neuroradiol 23:267–272
Isaac C, Li DKB, Genton M et al (1998) Multiple sclerosis: a serial study using MRI in relapsing patients. Neurology 38:1511–1515
Isoardo G, Di Vito N, Nobile M, Benetton G, Fassio F (2005a) X-linked Charcot-Marie-Tooth disease and progressive-relapsing central demyelinating disease. Neurology 65(10):1672–1673
Isoardo G, Fassio F, Nobile M, DiVito (2005) Charcot-Marie-Tooth disease Type 1X and progressive relapsing multiple sclerosis. A case report. 2005 meeting of the Peripheral Nerve Society July 9–13, 2005. J Peripher Nerv Syst (Suppl 10):36
Jankovic J (1994) Post-traumatic movement disorders: central and peripheral mechanisms. Neurology 44:2006–2014
Jessen KR, Mirsky R (1983) Astrocyte-like glia in the peripheral nervous system: an immunohistochemical study of enteric glia. J Neurosci 3:2206–2218
Johnson DA, Hafler DA, Fallis RJ et al (1986) Cell-mediated immunity to myelin-associated glycoprotein, proteo-lipid protein, and myelin basic protein in multiple sclerosis. J Neuroimmunol 13:99–108
Johnson MR, Ferner RE, Bobrow M, Hughes RA (2000) Detailed analysis of the oligodendrocyte myelin glycoprotein gene in four patients with neurofibromatosis 1 and primary progressive multiple sclerosis. J Neurol Neurosurg Psychiatry 68(5):643–646
Johnston BL, Conly JM (2006) Alemtuzumab and natalizumab: the monoclonal antibody story continues. Can J Infect Dis Med Microbiol 17:327–329
Kabat EA, Solf A, Bezer AE (1946) Rapid production of acute disseminated encephalomyelitis in rhesus monkeys by injection of brain tissue with adjuvants. Science 104:362–363
Kalimo H, Frey H, Raine CS et al (1979) Late-onset malignant astrocytoma in a case of multiple sclerosis. Acta Neuropathol 46:231–234
Kalman B, Leist TP (2003) A mitochondrial component of neurodegeneration in multiple sclerosis. Neuromolecular Med 3:147–157
Kalman B, Lublin FD (1999) The genetics of multiple sclerosis. A review. Biomed Pharmacother 53(8):358–370
Kelly PJ, Shapiro BE (2001) Amyotrophic lateral sclerosis and other motor neurone disorders. In: Bachelor T, Gudkowicz MR (eds) Principles of neuroepidemiology. Butterworth, Boston, pp 265–287
Kirk J, Plumb J, Meenakshi M, McQuaid S (2003) Tight junctional abnormality in multiple sclerosis white matter affects all calibres of vessel and is associated with blood-brain barrier leakage and active demyelination. J Pathol 201:319–327
Kurtzke JF, Beebe GW (1980) Epidemiology of amyotrophic lateral sclerosis: 1. A case-control comparison based on ALS deaths. Neurology 30:453–462
Kwon JY, Kim JY, Jeong JH, Park KD (2008) Multiple sclerosis and peripheral multifocal demyelinating neuropathies occurring in a same patient. J Clin Neurol 4(1):51–57
Lahl R (1980) Combination of multiple sclerosis and cerebral glioblastoma. Eur Neurol 19:192–197
Lamarche JB, Behan PO, Segarra JM et al (1972) Recurrent acute necrotising haemorrhagic encephalopathy. Acta Neuropathol 22:79–87
Langer-Gould A, Albers KB, Van Den Eeden SK, Nelson LM (2010) Autoimmune diseases prior to the diagnosis of multiple-sclerosis: a population-based case-control study. Mult Scler 16(7):855–861
Lassmann H, Buidka H, Schnaberth G (1981) Inflammatory demyelinating polyradiculitis in a patient with multiple sclerosis. Arch Neurol 38:99–102
Levine S (1971) Relationship of experimental allergic encephalomyelitis to human disease. In: Rowland LP (ed) Immunological disorders of the nervous system. Williams & Wilkins, Baltimore
Levine S, Hoenig EM (1968) Induced localisation of allergic adrenalitis and encephalomyelitis at sites of thermal injury. J Immunol 100(6):1310–1318
Lightman S, McDonald WI, Bird AC et al (1987) Retinal venous sheathing in optic neuritis. Its significance for the pathogenesis of multiple sclerosis. Brain 110:405–414
Likosky WH, Fireman B, Elmore R et al (1991) Intense immunosuppression in chronic progressive multiple sclerosis: the Kaiser study. J Neurol Neurosurg Psychiatry 54:1055–1060
Lucchinetti CF, Brueck W, Rodriguez M et al (1998) Multiple sclerosis: lessons from neuropathology. Semin Neurol 18:337–345
Lumsden CE (1955) Pathology of multiple sclerosis and allied demyelinating diseases. In: McAlpine D, Compston ND, Lumsden CE (eds) Multiple sclerosis. Livingstone, Edinburgh, pp 208–293
Lumsden C (1970) The neuropathology of multiple sclerosis. In: Vinken PJ, Bruyn GW (eds) Handbook of clinical neurology. Vol. 9. Multiple sclerosis and other demyelinating diseases. North Holland, Amsterdam, pp 217–309
Lynch PG (1974) Multiple sclerosis and malignant gliomas. BMJ 3:577
Majoie CB, Akkerman EM, Blank C et al (2002) Mitochondrial encephalomyopathy: comparison of conventional MR imaging with diffusion-weighted and diffusion tensor imaging: case report. Am J Neuroradiol 23:13–16
Malmgren RM, Detels R, Verity MA (1984) Co-occurrence of multiple sclerosis and glioma—case report and neuropathologic and epidemiologic review. Clin Neuropathol 3(1):1–9
Martin R, McFarland HF (1997) Immunology of multiple sclerosis and experimental allergic encephalomyelitis. In: Raine CS, McFarland HF, Tourtellotte WW (eds) Multiple sclerosis. Chapman & Hall, London, pp 221–239
Martin R, Voskuhl R, Flerlage M et al (1993) Myelin basic protein-specific T-cell responses in identical twins discordant or concordant for multiple sclerosis. Ann Neurol 34:524–535
Masson C, Colombani JM (1997) Neurofibromatosis 1 and multiple sclerosis. Apropos of a case. Rev Neurol 153(11):684–686 (in French)
Mathews T, Moosy J (1972) Mixed glioma, multiple sclerosis & Charcot-Marie-Tooth disease. Arch Neurol 27:263–268
Matthew PM, De Stefano N, Narayanan S et al (1998) Putting magnetic resonance spectroscopy studies in context: axonal damage and disability in multiple sclerosis. Semin Neurol 18:327–336
Matthews WB (1962) Epilepsy and disseminated sclerosis. Q J Med 31:141–155
Mayor S (2002) Researchers claim clinical trials are reported with misleading statistics. BMJ 324:1353
McDonald WI et al (2001) Recommended diagnostic criteria for multiple sclerosis: Guidelines from the International Panel on the diagnosis of multiple sclerosis. Ann Neurol 50:121–127
McGrath J (2001) Does ‘imprinting’ with low prenatal vitamin D contribute to the risk of various adult disorders? Med Hypotheses 56(3):367–371
McGuinness MC, Smith KD (1999) Cerebral inflammation in X-linked adrenoleukodystrophy (review). Arch Immunol Ther Exp 47(5):281–187
McNair Scott TF (1967) Post-infectious and vaccinial encephalitis. In: Sweeney FJ Jr (Ed) Medical clinics of North America, vol 51, chap 14. W.B. Saunders, Philadelphia, pp 701–717
Metz LM, Zhang Y, Yeung M, Patry DG, Bell RB, Stoian CA, Yong VW, Patten SB, Duquette P, Antel JP, Mitchell JR (2004) Minocycline reduces gadolinium-enhancing magnetic resonance imaging lesions in multiple sclerosis. Ann Neurol 55:756
Mills KR, Murray NM (1986) Neurophysiological evaluation of associated demyelinating peripheral neuropathy and multiple sclerosis: a case report. J Neurol Neurosurg Psychiatry 49:320–323
Mittler RS, Foell J, McCausland M, Strahotin S, Niu L, Bapat A, Hewes LB (2004) Anti-CD137 antibodies in the treatment of autoimmune disease and cancer. Immunol Res 29:197–208
Moreau T, Thorpe J, Miller D et al (1994) Preliminary evidence from magnetic resonance imaging for reduction in disease activity after lymphocyte depletion in multiple sclerosis. Lancet 344:298–301; erratum 486
Morris HW, Moriabadi NF, Lees AJ et al (1998) Parkinsonism following electrical injury to the hand. Mov Disord 13(3):600–602
Mullen JT, Vartainan TK, Atkins MB (2008) Melanoma complicating treatment with natalizumab for multiple sclerosis. N Eng J Med 358:647–648
Munch-Peterson CJ (1949) Case of disseminated sclerosis and glioma of the brain in the same patient. Acta Psychiat Neurol Scand 24:599–605
Nahser HC, Vieregge P, Nau HE et al (1986) Coincidence of multiple sclerosis and glioma. Surg Neurol 26:45–51
Narayana PA, Doyle TJ, Lai D et al (1998) Serial proton magnetic resonance spectroscopy imaging, contrast enhanced magnetic resonance imaging and quantitative lesion volumetry in multiple sclerosis. Ann Neurol 43:56–71
Noble LJ, Wrathall JR (1989) Distribution and time course of protein extravasation in the rat spinal cord after contusive injury. Brain Res 482:57–66
Noseworthy JH (1999) Progress in determining the causes and treatment of multiple sclerosis. Nature 399:A40–A47
O’Riordan JI, Thompson AJ, Kingsley DP et al (1998) The prognostic value of brain MRI in clinically isolated syndromes of the CNS: a 10-year follow-up. Brain 121:495–503
Okun MR, Bowman T (1999) Mitotic and amitotic cell replication in malignant melanoma: the role of subdivisional cell replication. Speculations Sci Technol 21:321–328
Okun MR, Edelstein LM (1967) Cell reproduction by subdivision? Lancet 1:1056–1057
Oldendorf WH, Cornford EM (1997) A comparison of total body and local spinal cord irradiation in experimental allergic encephalomyelitis. J Neuropathol Exp Neurol 36:50–61
Oppenheimer DR (1969) Acute encephalopathy in children. In: Whitty CWM, Hughes JT, MacCallum FO (eds) Virus diseases and the nervous system. Blackwell, Oxford
Oppenheimer DR (1978) The cervical spine in multiple sclerosis. Neuropathol Appl Neuobiol 4:151–162
Pál E, Gömöri EE, Gáti I (2001) Neurofibromatosis and glioblastoma in a case of multiple sclerosis. Eur J Neurol 8(6):717–718
Palo J, Duchesne J, Wikstrom J (1977) Malignant disease among patients with multiple sclerosis. J Neurol 216:217–222
Parman Y, Ciftci F, Poyraz M, Halefoglu AM, Oge AE, Eraksoy M, Saruhan-Direskeneli G, Deymeer F, Battaloglu E (2007) X-linked Charcot-Marie-Tooth disease and multiple sclerosis. J Neurol 254((7):953–955
Paterson PY (1987) Neuroimmunology: an overview and personal perspective. In: Aarli JA, Behan WMH, Behan PO (eds) Clinical neuroimmunology. Blackwell, Oxford, pp 3–25
Perilongo G, Moras P, Carollo C et al (1999) Spontaneous partial regression of low-grade glioma in children with neurofibromatosis-1: a real possibility. J Child Neurol 14:352–356
Perini P, Gallo P (2001) The range of multiple sclerosis associated with neurofibromatosis type 1. J Neurol Neurosurg Psychiatry 71(5):679–681
Peterson K, Rosenblum MK, Powers JM et al (1993) Effect of brain irradiation on demyelinating lesions. Neurology 43:2105–2112
Pezeshkpour GH, Dalakas MC (1988) Long-term changes in the spinal cords of patients with old poliomyelitis. Arch Neurol 45:505–508
Pierpaoli C, Jezzard P, Basser PJ et al (1996) Diffusion tensor MR imaging of the human brain. Radiology 201:637–648
Pollock M, Calder C, Allpress S (1977) Peripheral nerve abnormality in multiple sclerosis. Ann Neurol 2:41–48
Popovich PG, Stokes BT, Whitacre CC (1996) Concept of autoimmunity following spinal cord injury: possible roles for T lymphocytes in the traumatised central nervous system. J Neurosci Res 45:349–363
Poser CM (1987) The peripheral nervous system in multiple sclerosis. A review and pathogenetic hypothesis. J Neurol Sci 79((1-2)):83–90
Poser CM (2000) Trauma to the central nervous system may result in formation or enlargement of multiple sclerosis plaques. Arch Neurol 57:1074–1076
Prineas J (1975) Pathology of the early lesion in multiple sclerosis. Hum Pathol 6:531–554
Prineas JW (1985) The neuropathology of multiple sclerosis. In: Koetsier JC (ed) Handbook of clinical neurology, vol 47. Elsevier, Amsterdam, pp 213–257
Prineas JW, Kwon EE, Sternberger NH et al (1984) The distribution of myelin-associated glycoprotein and myelin basic protein in actively demyelinating multiple sclerosis lesions. J Neuroimmunol 6:251–264
Puri BK, Bydder GM, Chaudhuri KR, Al Saffar BY, Curati WL, White SJ, Mitchell L, Hajnal JV, Horrobin DF (2001) MRI changes in multiple sclerosis following treatment with iofepramine and l-phenylalanine. Neuroreport 12:1821–1824
Purmann J, Arendt G, Cleveland S, Borchard F, Fürst W, Gemsa R, Bertrams J, Hengels KJ (1992) Association of Crohn’s disease and multiple sclerosis. Is there a common background? J Clin Gastroenterol 14:43–46
Quan D, Kleinschmidt-DeMasters BK (2005) A 71-year-old male with 4 decades of symptoms referable to both central and peripheral nervous system. Brain Pathol 15(4):369–370, 373
Quan D, Kleinschmidt-DeMasters BK (2005b) Case of the month: May 2005. Chronic inflammatory demyelinating polyradiculoneuropathy (CIDP) with onion bulb formation in hypertrophic nerves and coexistent multiple sclerosis (MS). Brain Pathol 15(4):369–370
Quan D, Pelak VS, Tanabe J, Durairaj V, Kleinschmidt-DeMasters BK (2005) Symptomatic spinal and cranial hypertrophic neuropathy in multiple sclerosis. Muscle Nerve 6:772–779
Quattrocchi KB, Frank EH, Miller CE et al (1990) Suppression of cellular immune activity following severe head injury. J Neurotrauma 7(2):77–87
Quinn S (2001) Human trials. Scientists, investors and patients in the quest for a cure. Perseus Publishing, Cambridge
Raine CS (1994) The Dale E. McFarlin memorial lecture: the immunology of the multiple sclerosis lesion. Ann Neurol 36:S61–S72
Rajabally YA, Abbott RJ (2005) Charcot-Marie-Tooth disease due to the Thr124Met mutation in the myelin protein zero gene associated with multiple sclerosis. J Peripher Nerv Syst 10(4):388–389
Ransohoff RM (2007) Natalizumab for multiple sclerosis. N Engl J Med 356:2622–2629
Ratner N, Daston MM (2001) Genetic and cellular mechanisms of Schwann cell tumour formation: neurofibromatosis type 1 and neurofibromatosis type 2. In: Jessen KR, Richardson WD (eds) Glial cell development, 2nd edn. Oxford University Press, Oxford, pp 355–378
Reagan TJ, Frieman IS (1973) Multiple cerebral gliomas in multiple sclerosis. J Neurol Neurosurg Psychiatry 36:523–528
Remlinger P (1928) Les paralysies du traitement antirabique. Ann Inst Pasteur Lille 42(Suppl 71)
Revesz T, Kidd D, Thompson AJ et al (1994) Comparison of the pathology of primary and secondary progression of multiple sclerosis. Brain 117:759–765
Rice GPA, Incorvaia B, Munari L et al (2002) Interferon in relapsing-remitting multiple sclerosis (Cochrane review). In: The Cochrane library 1. Update Software, Oxford
Richert JR, McFarlin DE, Rose JW et al (1983) Expansion of antigen-specific T-cells from cerebrospinal fluid of patients with multiple sclerosis. J Neuroimmunol 5:317–324
Rivers TM, Schwentker FF (1935) Encephalomyelitis accompanied by myelin destruction experimentally produced in monkeys. J Exp Med 61:689–702
Ro YI, Alexander CB, Oh SJ (1983) Multiple sclerosis and hypertrophic demyelinating peripheral neuropathy. Muscle Nerve 6:312–316
Rohowsky-Kochan C, Eiman D, Troiano R et al (1990) Decreased suppressor-inducer T lymphocytes in multiple sclerosis and other neurological diseases. J Neuroimmunol 28:161–166
Rosenberg NL, Bourdette D (1983) Hypertrophic neuropathy and multiple sclerosis. Neurology 33:1361–1364
Rovaris M, Viti B, Ciboddo G et al (2000) Brain involvement in systemic immune mediated diseases: magnetic resonance and magnetisation transfer imaging study. J Neurol Neurosurg Psychiatry 68:170–177
Rubin M, Karpati G, Carpenter S (1987) Combined central and peripheral myelinopathy. Neurology 37:1287–1290
Russell DS (1955) The neurological unity of acute haemorrhagic leukoencephalitis and acute disseminated encephalomyelitis. Brain 78:369–376
Russell DS, Rubenstein LJ (1977) Pathology of tumours of the nervous system, 4th edn. Arnold, London, p 103, 151f, 240f
Scherer JJ (1938) La “Glioblastomatose en plaques”. J Belge Neurol Psychiatr 38:1–17
Scherer JJ (1940) The forms of growth in gliomas and their pathological significance. Brain 63:1–35
Schoene WC, Carpenter S, Behan PO, Geschwind N (1977) ‘Onion bulb’ formations in the central and peripheral nervous system in association with multiple sclerosis and hypertrophic polyneuropathy. Brain 100:755–773
Schwentker FF, Rivers TM (1934) The antibody response of rabbits to injections of emulsions and extracts of homologous brain. J Exp Med 60:559–574
Scully RE, Galdabani JJ, McNeely BU (1978) Weekly clinicopathological exercise—case 44. N Eng J Med 299:1060–1067
Seitelberger F (1960) Histochemistry of demyelinating diseases proper including allergic encephalomyelitis and Perlizaeus-Merzbacher’s disease. In: Cummings NJ (ed) Modern scientific aspects of neurology. Edward Arnold, London, pp 146–187
Shakir RA, Hussien JM, Trontelj JJ (1983) Myasthenia gravis and neuromyelitis optica. J Neuroimmunol 4:161–165
Shankar SK, Rao TV, Srivastav VK et al (1989) Balo’s concentric sclerosis: a variant of multiple sclerosis associated with oligodendroglioma. Neurosurgery 25(6):982–986
Sharma KR, Saadia D, Facca AG, Bhatia R, Ayyar DR, Sheremata W (2008) Chronic inflammatory demyelinating polyradiculoneuropathy associated with multiple sclerosis. J Clin Neuromuscul Dis 9(4):385–396
Shaw CM, Alvord EC (1987) Multiple sclerosis beginning in infancy. J Child Neurol 2:252–256
Sibley WA, Bamford CR, Clark K et al (1991) A prospective study of physical trauma and multiple sclerosis. J Neurol Neurosurg Psychiatry 54:584–589
Simpson JA (1960) Myasthenia gravis. A new hypothesis. Scot Med J 5:419–436
Sluga E (1969) Beitrag zur Feinstruktur der Lasionen bei der multiplen Sklerose des Menschen. Wein Z Nervenheilkd Grenzgeb (Suppl):2, 59–69
Sorensen AG, Wu O, Copen WA et al (1999) Human acute cerebral ischaemia; detection of changes by water diffusion anisotropy by using MR imaging. Radiology 212:785–792
Spaar FW, Wikstrom J (1978) Multiple sclerosis and malignant neoplasm of the central nervous system. A clinical anatomical report of three cases. J Neurol 218:23–33
Steiner I, Wirguin I (2000) Multiple sclerosis—in need of a critical reappraisal. Med Hypotheses 54(1):99–106
Stone LA, Frank JA, Albert PS et al (1995) The effect of interferon-beta on blood-brain barrier disruptions demonstrated by contrast-enhanced magnetic resonance imaging in relapsing-remitting multiple sclerosis. Ann Neurol 37:611–619
Tachi N, Ishikawa Y, Tsuzuki A, Minami R, Sasaki K, Shinoda M (1985) A case of childhood multiple sclerosis with peripheral neuropathy. Neuropediatrics 16:231–234
Tanaka R, Iwasaki Y, Koprowski H (1975) Ultrastructural studies of perivascular cuffing cells in multiple sclerosis brain. Am J Pathol 81(3):467–478
Taylor D, Cuendet F (1986) Optic neuritis in childhood. In: Hess RF, Plant GT (eds) Optic neuritis. Cambridge University Press, Cambridge, pp 73–85
The Canadian Cooperative Multiple Sclerosis Study Group (1991) The Canadian cooperative trial of cyclophosphamide and plasma exchange in progressive multiple sclerosis. Lancet 337:441–446
The Multiple Sclerosis Study Group (1990) Efficacy and toxicity of cyclosporine in chronic progressive multiple sclerosis: a randomised, double-blinded, placebo-controlled clinical trial. Ann Neurol 27:591–605
Thomas DGT, Lannigan CB, Behan PO (1975) Impaired cell-mediated immunity in human brain tumours. Lancet i:1389–1390
Thomas PK, Walker RWH, Rudge P, Morgan-Hughes JA, King RHM, Jacobs JM et al (1987) Chronic demyelinating peripheral neuropathy associated with multifocal central nervous system demyelination. Brain 110:53–76
Tivesky AL, Ptak T, Farkas J (1999) Investigation of apparent diffusion coefficient and diffusion tensor anisotropy in acute and chronic multiple sclerosis lesions. Am J Neuroradiol 20:1491–1499
Tobinick EL, Gross H (2008) Rapid cognitive improvement in Alzheimer’s disease following perispinal etanercept administration. J Neuroinflammation 5:2
Tortorella C, Viti B, Bozzali M et al (2000) A magnetization transfer histogram study of normal appearing brain tissue in MS. Neurology 54:186–193
Tournier-Lasserve E, Hashim GA, Bach MA (1988) Human T-cell response to myelin basic protein in multiple sclerosis patients and healthy subjects. J Neurosci Res 19:149–156
Tourtellotte WW, Tumani H (1997) Multiple sclerosis cerebrospinal fluid. In: Raine CS, McFarland HF, Tourtellotte WW (eds) Multiple sclerosis: clinical and pathogenic basis. Chapman & Hall, London, pp 57–79
Tourtellotte WW, Potvin AR, Baumhefner RW et al (1980) Multiple sclerosis de novo CNS IgG synthesis: effect of CNS irradiation. Arch Neurol 37:620–624
Truyen L, Gheuens J, Parizel PM et al (1991) Long-term follow-up of multiple sclerosis by standardised, non-contrast-enhanced magnetic resonance imaging. J Neurol Sci 106:35–40
Umehara F, Qin YF, Goto M et al (1990) Experimental autoimmune encephalomyelitis in the maturing central nervous system. Transfer of myelin basic protein-specific T line lymphocytes to neonatal Lewis rats. Lab Invest 62(2):147–155
van Noort J, van Sechel AC, Bajramovic et al (1995) The small heat-shock protein and β crystalline as candidate autoantigen in multiple sclerosis. Nature 375:798–810
van Waderveen MAA, Truyen L, van Oosten BW et al (1999) Development of hypointense lesions in T1-weighted spin-echi magnetic resonance images in multiple sclerosis: relation to inflammatory activity. Arch Neurol 56:345–351
van Waesberghe JHTM, van Walderveen MAA, Catelijns JA et al (1998) Patterns of lesion development in multiple sclerosis: longitudinal observations with T1-weighted spin-echo and magnetization transfer MR. Am J Neuroradiol 19:675–683
van Waesberghe JHTM, Kamphorst W, De Groot CJA et al (1999) Axonal loss in multiple sclerosis lesions: magnetic resonance imaging insights into substrates of disability. Ann Neurol 46:747–754
Vieregge P, Nahser HC, Gerhard L et al (1984) Multiple sclerosis and cerebral tumour. Clin Neuropathol 3(1):10–21
von Andrian UH, Engelhardt B (2003) α4 Integrins as therapeutic targets in autoimmune disease. N Engl J Med 348:68–72
von Deimling A, Krone W, Menon AG (1995) Neurofibromatosis type 1: Pathology, clinical features and molecular genetics. Brain Pathol 5:153–162
Warren SA, Warren KG (1982) Multiple sclerosis and diabetes mellitus: further evidence of a relationship. Can J Neurol Sci 9:415–419
Weir A, Hansen S, Ballantyne JP (1979) Single fiber electromyographic jitter in multiple sclerosis. J Neurol Neurosurg Psychiatry 42:1146–1150
Werring DJ, Clar CA, Barker GJ et al (1999) Diffusion tensor imaging of lesions and normal-appearing white matter in multiple sclerosis. Neurology 52:1626–1632
Wolfgram F (1979) What if multiple sclerosis isn’t an immunological or a viral disease? The case for a circulating toxin. Neurochem Res 4:1–14
Wrabetz ML, Feltin CO, Hanemann et al (2001) The molecular genetics of hereditary demyelinating neuropathies. In: Jessen KR, Richardson WD (eds) Glial cell development. Oxford University Press, Oxford, pp 331–354
Yudkin PL, Ellison GW, Ghezzi A et al (1991) Overview of azathioprine treatment in multiple sclerosis. Lancet 338:1051–1055
Zamvil SS, Steinman L (1990) The T lymphocyte in experimental allergic encephalomyelitis. Annu Rev Immunol 8:579–621
Zimmerman HM, Netsky MG (1950) The pathology of multiple sclerosis. Res Publ Assoc Nerv Ment Dis 28:271–312
Acknowledgment
This work was supported by the Sir David and Sir Frederick Barclay Foundation.
Author information
Authors and Affiliations
Corresponding author
Additional information
An erratum to this article can be found at http://dx.doi.org/10.1007/s10787-010-0074-0
Appendix
Appendix
Types of glioma occurring with multiple sclerosis
Year | Author | Age/sex | Neoplasm | Multicentric | Connected with plaque |
|---|---|---|---|---|---|
1938 | Scherer | 29 F | Glioblastomatosis | + | + |
1949 | Munch-Peterson | 49 F | Glioblastoma | − | − |
1950 | Zimmerman and Netsky | 61 M | Glioblastoma | − | N/A |
1962 | Matthews | 51 F | Astrocytoma | − | − |
1963 | Brihaye et al. | 62 M | Astrocytoma | − | + |
1967 | Boyazis et al. | 54 F | Glioblastoma | − | − |
1967 | Barnard and Jellinek | 44 F | Oligodendroglioma | + | + |
1968 | Aubert et al. | 50 F | Glioblastoma | − | − |
1972 | Mathews and Moosy | 44 M | Mixed astrocytoma and oligodendroglioma | − | − |
1973 | Reagan and Freiman | 40 F | Glioblastoma | + | + |
1974 | Lynch | 44 F | Glioblastoma | + | + |
1974 | Currie and Urich | 37 F | Glioblastoma | − | − |
63 M | Glioblastoma/Astrocyte | + | + | ||
53 M | Glioblastoma | − | + | ||
1977 | Russell and Rubinstein | 36 F | Astrocytoma (glioblastoma), glioblastoma | + | + |
66 M | Subependydoma | + | − | ||
? M | Gemistocytic astrocytomaa | − | + | ||
1977 | Palo et al. | 52 F | Astrocytoma | N/A | N/A |
1978 | Spaar and Wikstorm | 63 F | Semimalignant meningioma | N/A | N/A |
1978 | Scully et al. | 57 F | Mixed astrocytoma and ependymoma | − | − |
1979 | Kalimo et al. | 36 F | Astrocytoma | − | − |
1980 | Lahl | 50 M | Glioblastoma with cerebral gliomatosis | + | + |
1981 | Ho and Wolfe | 63 F | Protoplasmic astrocytoma | − | − |
1984 | Vieregge et al. | 43 F | Astrocytoma grade II | − | − |
49 M | Astrocytoma | + | − | ||
1984 | Malmgren et al. | 54 M | Glioma | − | − |
1986 | Nahser et al. | 42 F | Astrocytoma grade II | − | − |
49 M | Astrocytoma | + | − | ||
1987 | Barnard and Geddes | 43 F | Malignant oligodendroglioma | + | − |
?? | Glioblastoma | − | − | ||
1989 | Aarli et al. | 63 M | Glioblastoma | − | − |
1989 | Shankar et al. | 34 F | Oligodendroglioma | − | − |
2000 | De Caso et al. | 63 F | Ependymoma Meningioma | N/A | N/A |
Rights and permissions
About this article
Cite this article
Behan, P.O., Chaudhuri, A. The sad plight of multiple sclerosis research (low on fact, high on fiction): critical data to support it being a neurocristopathy. Inflammopharmacol 18, 265–290 (2010). https://doi.org/10.1007/s10787-010-0054-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10787-010-0054-4