Abstract
Background
Recommendations for the operative treatment of spondylodiscitis are still a controversial issue.
Methods
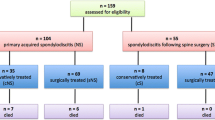
A retrospective review identified 113 consecutive patients who underwent surgical debridement and instrumentation for spondylodiscitis between 2006 and 2010 at our department.
Results
The mean age at presentation was 65 years; 78 patients were male (69 %). Distribution of the inflammation was lumbar in 68 (60 %), thoracic in 19 (17 %) and cervical in 20 (18 %) cases. Six patients (5 %) had two concomitant non-contiguous spondylodiscitis foci in different segments of the spine. Epidural abscess was found in 33 patients (29 %). One hundred four patients (92 %) had pain. Neurological deficit was found in 40 patients (35 %). In the thoracic and lumbar cases, dorsal instrumentation alone was considered sufficient in 26 cases; additional interbody fusion from the posterior was performed in 44 cases. A 360° instrumentation was performed in 22 cases. In the cervical cases, only ventral spondylodesis and plating were performed in eight cases, only dorsal instrumentation in five and 360° instrumentation in seven. Postoperative intravenous antibiotics were administered for 14.4 ± 9.3 (mean ± SD) days followed by 3.2 ± 0.8 (mean ± SD) months of oral antibiosis. Complete healing of the inflammation was achieved in 111 (98 %) cases. Two patients died because of septic shock, both with fulminant endocarditis. Pain resolved in all cases. Neurological deficits were completely resolved in 20 patients, and 14 patients had a partial recovery.
Conclusion
The results of our retrospective study show that surgical treatment of spondylodiscitis with a staged surgical approach (if needed) and a short 1-2-week period of intravenous antibiotics followed by 3 months of oral antibiotics is appropriate for most patients in whom conservative treatment has failed or is not advisable. Furthermore, surgical treatment of newly diagnosed spondylodiscitis might be recommended as an initial treatment option in many cases. Thereby the choice of fusion material (autologous bone, titanium, PEEK) seems less important.





Similar content being viewed by others
References
Al-Nammari SS, Lucas JD, Lam KS (2007) Hematogenous methicillin-resistant Staphylococcus aureus spondylodiscitis. Spine (Phila Pa 1976) 15:2480–2386
Belzunegui J, Intxausti JJ, De Dios JR, Del Val N, Rodríguez Valverde V, González C, Queiro R, Figueroa M (2000) Haematogenous vertebral osteomyelitis in the elderly. Clin Rheumatol 19:344–347
Bettini N, Girardo M, Dema E, Cervellati S (2009) Evaluation of conservative treatment of non specific spondylodiscitis. Eur Spine J 1:143–150
Brase A, Ringel F, Stüer C, Meyer B, Stoffel M (2010) Debridement and fusion with polyetheretherketone implants in purulent spondylodiscitis: a clinical experience with nine patients. Acta Neurochir 152:2001–2004
Carragee EJ (1997) Instrumentation of the infected and unstable spine: a review of 17 cases from the thoracic and lumbar spine with pyogenic infections. J Spinal Disord 10:317–324
Carragee EJ (1997) Pyogenic vertebral osteomyelitis. J Bone Joint Surg Am 79:874–880
Chang CC, Merritt K (1994) Infection at the site of implanted materials with and without preadhered bacteria. J Orthop Res 12:526–531
Cottle L, Riodan T (2008) Infectious spondylodiscitis. J Infect 56:401–412
Deininger MH, Unfried MI, Vougioukas VI, Hubbe U (2009) Minimally invasive dorsal percutaneous spondylodesis for the treatment of adult pyogenic spondylodiscitis. Acta Neurochir 151:1451–1457
Dimar JR, Carreon LY, Glassman SD, Campbell MJ, Hartman MJ, Johnson JR (2004) Treatment of pyogenic vertebral osteomyelitis with anterior debridement and fusion followed by delayed posterior spinal fusion. Spine 29:326–332
Dufour V, Feydy A, Rillardon L, Redondo A, Le Page L, Bert F, Belmatoug N, Fantin B (2005) Comparative study of postoperative and spontaneous pyogenic spondylodiscitis. Semin Arthritis Rheum 34:766–771
Euba G, Narváez JA, Nolla JM, Murillo O, Narváez J, Gómez-Vaquero C, Ariza J (2008) Long-term clinical and radiological magnetic resonance imaging outcome of abscess-associated spontaneous pyogenic vertebral osteomyelitis under conservative management. Semin Arthritis Rheum 38:28–40
Eysel P, Hopf C, Vogel I, Rompe JD (1997) Primary stable anterior instrumentation or dorsoventral spondylodesis in spondylodiscitis? Results of a comparative study. Eur Spine J 6:152–157
Fang D, Cheung KM, Dos Remedios ID, Lee YK, Leong JC (1994) Pyogenic vertebral osteomyelitis: treatment by anterior spinal debridement and fusion. J Spinal Disord 7:173–180
Fukuta S, Miyamoto K, Masuda T, Hosoe H, Kodama H, Nishimoto H, Sakaeda H, Shimizu K (2003) Two-stage (posterior and anterior) surgical treatment using posterior spinal instrumentation for pyogenic and tuberculotic spondylitis. Spine 28:E 302–308
Hadjipavlou AG, Mader JT, Necessary JT, Muffoletto AJ (2000) Hematogenous pyogenic spinal infections and their surgical management. Spine 25:1668–1679
Hanaoka N, Kawasaki Y, Sakai T, Nakamura T, Nanamori K, Nakamura E, Uchida K, Yamada H (2006) Percutaneous drainage and continuous irrigation in patients with severe pyogenic spondylitis, abscess formation, and marked bone destruction. J Neurosurg Spine 4:374–379
Hee HT, Majd ME, Holt RT, Pienkowski D (2002) Better treatment of vertebral osteomyelitis using posterior stabilization and titanium mesh cages. J Spinal Disord Tech 15:149–156
Heyde CE, Boehm H, El Saghir H, Tschöke SK, Kayser R (2006) Surgical treatment of spondylodiscitis in the cervical spine: a minimum 2-year follow-up. Eur Spine J 15:1380–1387
Hopf C, Meurer A, Eysel P, Rompe JD (1998) Operative treatment of spondylodiscitis—what is the most effective approach? Neurosurg Rev 21:217–225
Hopkinson N, Stevenson J, Benjamin S (2001) A case ascertainment study of septic discitis: clinical, microbiological and radiological features. QJM 94:465–470
Ito M, Abumi K, Kotani Y, Kadoya K, Minami A (2007) Clinical outcome of posterolateral endoscopic surgery for pyogenic spondylodiscitis: results of 15 patients with serious comorbid conditions. Spine 32:200–206
Kuklo TR, Potter BK, Bell RS, Moquin RR, Rosner MK (2006) Single-stage treatment of pyogenic spinal infection with titanium mesh cages. J Spinal Disord Tech 19:376–382
Karadimas EJ, Bunger C, Lindblad BE, Hansen ES, Høy K, Helmig P, Kannerup AS, Niedermann B (2008) Spondylodiscitis. A retrospective study of 163 patients. Acta Orthop 79:650–659
Khan IA, Vaccaro AR, Zlotolow DA (1999) Management of vertebral discitis and osteomyelitis. Orthopedics 22:758–765
Klockner C, Valencia R (2003) Sagittal alignment after anterior debridement and fusion with or without additional posterior instrumentation in the treatment of pyogenic and tuberculous spondylodiscitis. Spine 28:1036–1042
Klockner C, Valencia R, Weber U (2001) Sagittal alignment following surgical therapy of destructive spondylodiscitis: ventral or ventrodorsal procedure—a comparison of results. Orthopade 30:965–976
Krödel A, Krüger A, Lohscheidt K, Pfahler M, Refior HJ (1999) Anterior debridement, fusion, and extrafocal stabilization in the treatment of osteomyelitis of the spine. J Spinal Disord 12:17–26
Krodel A, Sturz H (1989) Differentiated surgical and conservative treatment of spondylitis and spondylodiscitis. Z Orthop Ihre Grenzgeb 127:589–596
Krodel A, Sturz H, Siebert CH (1991) Indications for and results of operative treatment of spondylitis and spondylodiscitis. Arch Orthop Trauma Surg 110:78–82
Korovessis P, Petsinis G, Koureas G, Iliopoulos P, Zacharatos S (2006) Anterior surgery with insertion of titanium mesh cage and posterior instrumented fusion performed sequentially on the same day under one anesthesia for septic spondylitis of thoracolumbar spine: is the use of titanium mesh cages safe? Spine 31:1014–1019
Korovessis P, Repantis T, Iliopoulos P, Hadjipavlou A (2008) Beneficial influence of titanium mesh cage on infection healing and spinal reconstruction in hematogenous septic spondylitis: a retrospective analysis of surgical outcome of twenty-five consecutive cases and review of literature. Spine (Phila Pa 1976) 33:E759–67
Lee JS, Suh KT (2006) Posterior lumbar interbody fusion with an autogenous iliac crest bone graft in the treatment of pyogenic spondylodiscitis. J Bone Joint Surg Br 88:765–770
Linhardt O, Kruger A, Krodel A (2004) First results of anterior versus posterior instrumentation-fusion in the treatment of spondylodiscitis. Z Orthop Ihre Grenzgeb 142:73–78
Mann S, Schütze M, Sola S, Piek J (2004) Nonspecific pyogenic spondylodiscitis: clinical manifestations, surgical treatment, and outcome in 24 patients. Neurosurg Focus 17(6):E3
McGuire RA, Eismont FJ (1994) The fate of autogenous bone graft in surgically treated pyogenic vertebral osteomyelitis. J Spinal Disord 7:206–215
Mondorf Y, Gaab MR, Oertel JM (2009) PEEK cage cervical ventral fusion in spondylodiscitis. Acta Neurochir 151:1537–1541
Mylona E, Samarkos M, Kakalou E, Fanourgiakis P, Skoutelis A (2009) Pyogenic vertebral osteomyelitis: a systematic review of clinical characteristics. Semin Arthritis Rheum 39:10–17
Nagata K, Ohashi T, Ariyoshi M, Sonoda K, Imoto H, Inoue A (1998) Percutaneous suction aspiration and drainage for pyogenic spondylitis. Spine 23:1600–1606
O’Daly BJ, Morris SF, O’Rouke SK (2008) Long-term function outcome in pyogenic spinal infection. Spine 33:E246–E253
Ogden AT, Kaiser MG (2004) Single stage debridement and instrumentation for pyogenic spinal infections. Neurosurg Focus 17:E5,1–5
Pavlov PW, Meijers H, van Limbeek J, Jacobs WC, Lemmens JA, Obradov-Rajic M, de Kleuver M (2004) Good outcome and restoration of lordosis after anterior lumbar interbody fusion with additional posterior fixation. Spine 29:1893–1900
Pee YH, Park JD, Choi YG, Lee SH (2008) Anterior debridement and fusion followed by posterior pedicle screw fixation in pyogenic spondylodiscitis: autologous iliac bone strut versus cage. J Neurosurg Spine 8:405–412
Pigrau C, Almirante B, Flores X, Falco V, Rodríguez D, Gasser I, Villanueva C, Pahissa A (2005) Spontaneous pyogenic vertebral osteomyelitis and endocarditis: incidence, risk factors, and outcome. Am J Med 118:1287
Przybylski GJ, Sharan AD (2001) Single-stage autogenous bone grafting and internal fixation in the surgical management of pyogenic discitis and vertebral osteomyelitis. J Neurosurg Spine 94:1–7
Quiñones-Hinojosa A, Jun P, Jacobs R, Rosenberg WS, Weinstein PR (2004) General principles in the medical and surgical management of spinal infections: a multidisciplinary approach. Neurosurg Focus 17:E1,1–15
Rath SA, Neff U, Schneider O, Richter HP (1996) Neurosurgical management of thoracic and lumbar vertebral osteomyelitis and discitis in adults: a review of 43 consecutive surgically treated patients. Neurosurg 38:926–933
Roblot F, Besnier JM, Juhel L, Vidal C, Ragot S, Bastides F (2007) Optimal duration of antibiotic therapy in vertebral oseomylitis. Semin Arthritis Rheum 36:269–277
Sakkas LI, Davas EM, Kapsalaki E, Boulbou M, Makaritsis K, Alexiou I, Tsikrikas T, Stathakis N (2009) Hematogenous spinal infection in central Greece. Spine (Phila Pa 1976) 34:E513–518
Schinkel C, Gottwald M, Andress HJ (2003) Surgical treatment of spondylodiscitis. Surg Infect 4:387–391
Sindern E, Gläser E, Bötel U, Malin JP (1993) Spondylodiscitis with spinal and radicular deficits. Limits of conservative treatment. Nervenarzt 64:801–805
Valancius K, Hansen ES, Høy K, Helmig P, Niedermann B, Bünger C (2012) Failure modes in conservative and surgical management of infectious spondylodiscitis. Eur Spine J 22:1837–1844
Walter J, Kuhn SA, Reichart R, Kalff R, Ewald C (2010) PEEK cages as a potential alternative in the treatment of cervical spondylodiscitis: a preliminary report on a patient series. Eur Spine J 19:1004–1009
Zarrouk V, Feydy A, Sallès F, Dufour V, Guigui P, Redondo A (2007) Imaging does not predict the clinical outcome of bacterial vertebral osteomyelitis. Rheumatology (Oxford) 46:292–295
Conflicts of interest
The authors declare that they have no conflict of interest affecting this study. The study was completely financed by the Department of Neurosurgery.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shiban, E., Janssen, I., Wostrack, M. et al. A retrospective study of 113 consecutive cases of surgically treated spondylodiscitis patients. A single-center experience. Acta Neurochir 156, 1189–1196 (2014). https://doi.org/10.1007/s00701-014-2058-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-014-2058-0