Abstract
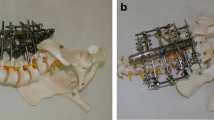
The operative results of 23 patients with a specific or unspecific spondylodiscitis were documented over 2 years after the focus of the inflammation had been eradicated, bone chip had been interposed and a CDH instrumentation had been performed by an anterior approach only. These outcomes were compared with the results of 32 patients in whom the focus had been removed and the defect had been filled with bone graft from an anterior approach, followed by stabilisation with CD instrumentation through an additional dorsal approach. In the cases where CDH instrumentation was applied, the range of fusion averaged 1.3 segments. This was clearly less extensive than in dorsoventral stabilisation, in which on average 3.5 segments were fused. In 47 of 55 cases mobilisation was achieved without orthesis. Eight months after the operations bony fusion could be observed radiologically in all patients. The mean preoperative kyphotic angle of the affected segments was 14.4°, compared to 4° after the operation. The mean loss of reposition was measured to be about 2.7° in both groups. Average operation time and blood loss were about 50% higher in the patients treated dorsoventrally. We conclude that even in the case of florid spondylodiscitis, a short-range anterior fusion of the affected spinal segment may be performed by use of a stable-angle implant without an increased risk of infection-related loosening.
Similar content being viewed by others
References
Aliabadi H, Johnson C, Cass AS, Mayfild J, Vandenbrink K (1984) Ureteral obstruction following the Dwyer procedure in a patient with an ileal loop urinary diversion. Spine 9: 819–821
Brown LP, Bridwell KH, Holt RT, Jennings J (1986) Aortic erosion and laceration associated with the Dunn anterior spinal instrumentation. Orthop Trans 10: 16–17
Brussatis F, Blümlein H, Wunderlich T (1983) Ergebnisse nach Ausräumung and ventraler Fusion bei Spondylitiden. Z Orthop Ihre Grenzgeb 121: 458–459
Buchner H, Pink P (1981) Die Spondylitis tuberculosa. Orthopdde 10: 119–132
Chan FL, Chow SP (1983) Retroperitoneal fibrosis after anterior spinal fusion. Clin Radiol 34:331–335
Cleveland RH, Gilsanz V, Lebowitz RL, Wilkinson RH (1978) Hydronephrosis from retroperitoneal fibrosis after anterior spine fusion: J Bone Joint Surg Am 60: 996–997
Collert S (1977) Osteomyelitis of the spine. Acta Orthop Scand 48: 283–290
Colton CL, Hall AJ (1991) Atlas of orthopaedic surgical approaches. Butterworth Heinemann, Stonehem
Costerton JW, Irvin RT, Cheng KJ (1981) The bacterial glycocalyx in nature and disease. Ann Rev Microbiol 35:299–324
Dick W, Graf R, Morscher E (1984) Konservative and operative Therapie der Spondylitis. Therapiewoche 34: 448–452
Digby JM, Kersley JB (1979) Pyogenic non-tuberculoss spinal infection. J Bone Joint Surg Br 61: 47–55
Dufek P, von Salis-Soglio G, Bozdech Z (1987) Die unspezifische bakterielle Spondylitis – eine Analyse von 32 Fallen. Z Orthop Ihre Grenzgeb 125: 225–261
Dunn HK (1984) Anterior stabilisation of thoracolumbar injuries. Clin Orthop 189:116–124
Dunn HK (1986) Anterior spine stabilization and decompression for thoracolumbar injuries. Orthop Clin North Am 17: 113–119
Dunn HK, Daniels AU, McBride GG (1980) Comparative assessment of spine stability achieved with a new anterior spine fixation system. Orthop Trans 4: 268–269
Dunn HK, Globe EM, McBride GG, Daniels AU (1981) An implant system for anterior spine stabilization. Orthop Trans 5: 433–434
Dwyer AF, Yau AC, Hsu L, O'Brien JP, Hodgson AR (1976) Deep paravertebral infection following Dwyer anterior spinal instrumentation. A report of three cases. Spine 1: 201–206
Eichenauer M, van der Lan EO, Mostegl A (1987) Vorwiegend ambulant-konservative Behandlung der unkomplizierten Spondylitis tuberculosa. Therapiewoche 37:122–131
Eismont FJ, Bohlman HH, Soni PL, Goldberg VM, Freehafer AA (1983) Pyogenic and fungal vertebral osteomyelitis with paralysis. J Bone Joint Surg [Am] 65: 19–29
Enderle A, Schmitt E, Zichner L (1981) Zur Diagnostik herdförmiger Wirbelsdulenerkrankungen — eine kritische Betrachtung. Z Orthop Ihre Grenzgeb 119:193–205
Eysel P, Hopf C, Diop A, Lavaste F (1995) Die mehr-segmentale ventrale Stabilisierung der Lendenwirbelsäule: eine vergleichende biomechanische Studie. Z Orthop Ihre Grenzgeb 133: 242–248
Flynn JC, Price CT (1984) Sexual complications of anterior fusion of the lumbar spine. Spine 9: 489–492
Giehl JP, Zielke K, Hack HP (1989) Die ventrale Derotationsspondylodese nach Zielke. Orthopäde 18: 101–117
Gristina AG, Costerton JW (1985) Bacterial adherence and the glycocalyx and their role in musculoskeletal infection. Orthop Clin North Am 15: 517–535
Gristina AG, Oga M, Webb LX, Hobgood DC (1985) Bacterial adherence and the pathogenesis of osteomyelitis. Science 228: 990–993
Harmon PH (1964) A simplified surgical technique for anterior lumbar discectomy and fusion. Avoidance of complications. Anatomy of the retroperitoneal veins. Clin Orthop 37: 130–144
Heine J, Immenkamp M, Matthiass HH (1983) Ergebnisse der operativen Behandlung der Spondylitis tuberculosa. Z Orthop Ihre Grenzgeb 121: 457–461
Hodgson AR, Stock FE (1960) Anterior spine fusion for the treatment of tuberculosis of the spine. J Bone Joint Surg [Am] 42: 295–310
Hopf C, Eysel P, Dubousset J (1995) CDH: preliminary report on a new anterior spinal instrumentation. Eur Spine J 4: 194–199
Ito H, Tsuchiy J, Asami G (1934) A new radical operation for potts disease. J Bone Joint Surg [Am] 16: 499–511
Jäger M, Springer HH (1981) Die entzündlichen Erkrankungen der Wirbelsäule. Orthopäde 10: 106–113
Jendrisak MD (1986) Spontaneous abdominal aortic rupture from erosion by a lumbar spine fixation device. A case report. Surgery 99: 631–633
Johnson RM, McGuire EJ (1981) Urogenital complications of anterior approaches to the lumbar spine. Clin Orthop 154: 114–118
Kaneda K (1981) Anterior approach and Kaneda instrumentation for lesions of the thoracic and lumbar spine. In: Bridwell KH, Dewald RL (eds) Textbook of spinal surgery. Lippincott, Philadelphia, pp 959–990
Kemp HBS, Jackson JW, Jeremiah JD, Hall AJ (1973a) Pyogenic infections occurring primarily in intervertebral discs. J Bone Joint Surg [Br] 55: 699–714
Kemp HBS, Jackson JW, Jeremiah JD, Cook J (1973b) Anterior fusion of the Spine for Infective Lesions in Adults. J Bone Joint Surg [Br] 55: 715–734
King DM, Mayo KM (1973) Infective lesion of the vertebral column. Clin Orthop 96:248–253
Kirkaldy-Willis WH, Thomas TG (1965) Anterior approaches in the diagnosis and treatment of infections of the vertebral bodies. J Bone Joint Surg [Am] 47: 87–110
Krbdel A, Stürz H (1989) Differenzierte operative and konservative Therapie der Spondylitis and Spondylodiscitis. Z Orthop Ihre Grenzgeb 127: 587–596
La Rocca H (1978) Infections of the spine. Clin Neurosurg 25: 296–304
Leong JCY (1990) Anterior spinal fusion for low back syndrome. In: Floman Y (ed) Disorders of lumbar spine, Aspen, Gaithersburg, pp 332–373
Lifeso RM, Weaver P, Harder EH (1985) Tuberculous spondylitis in adults. J Bone Joint Surg [Am] 67: 1405–1413
Manner G, Parsch K (1983) Spondylitis and Spondylodiscitis beim Kind. Z Orthop Ihre Grenzgeb 121: 455–456
Martin NS (1970) Tuberculosis of the spine. J Bone Joint Surg [Br] 52: 613–621
McMaster WC, Silber I (1975) A urological complication of Dwyer instrumentation. J Bone Joint Surg [Am] 57: 710–711
Medical Research Council Working Party on Tuberculosis of the Spine (1985) A 10-year assessment of controlled trials of inpatient and outpatient treatment and of plaster-of-paris jackets for tuberculosis of the spine in children on standard chemotherapy. J Bone Joint Surg [Br] 67: 103–110
Meurer A, Eysel P, Heine J (1995) Ergebnisse der operativen Behandlung der Spondylitis tuberculosa. Z Orthop Ihre Grenzgeb 144: 227–245
Nasca JR, Mc Elvein RB (1985)Aspergillus fumigatus osteomyelitis of the thoracic spine treated by excision and interbody fusion. Spine 10: 848–851
Oga M, Sugioka Y, Hobgood CD, Gristina AG, Myrvik QN (1988) Surgical biomaterials and differential colonization by Staphylococcus epidermidis. Biomaterials 9: 285–289
Oga M, Arizono T, Takasita M, Sugioka Y (1993) Evaluation of the risk of instrumentation as a foreign body in spinal tuberculosis. Spine 18: 1890–1894
Parthasarathy R (1985) Madras study of tuberculosis of spine. assessment and follow-up. In: Shanmugasundaram TK (ed) Current concepts in bone and joint tuberculosis. International Bone and Joint Tuberculosis Club, Madras, pp 10–12
Peters KM, Schwanitz B, Zilkens KW (1992) Spondylodiscitis -eine häufig spat gestellte Diagnose. Orthop Prax 28: 108–112
Rajasekaran S, Shanmugasundaram TK (1987) Prediction of the Angle of Gibbus Deformity in Tuberculosis of the Spine. J Bone Joint Surg [Am] 69: 503–509
Rajasekaran S, Soundarapandian S (1989) Progression of kyphosis in tuberculosis of the spine treated by anterior arthrodesis. J Bone Joint Surg [Am] 71: 1314–1323
Robinson BHB, Lessof MHJ (1972) Osteomyelitis of the spine. Gays Hosp Rep 110: 303–309
Schulze W (1979) Entzündliche Wirbelsäulenprozesse. Wirbelsäule Forsch Prax 83: 147–150
Silber I, McMaster W (1977) Retroperitoneal fibrosis with hydronephrosis as a complication of the Dwyer procedure. J Pediatr Surg 12: 255–257
Stevenson FH, Manning CW (1962) Tuberculosis of the spine treated conservatively with chemotherapy. Tubercle 43: 406–410
Stolke D, Seifert V, Kunz U (1988) Die postoperative Discitis intervertebralis lumbalis. Z Orthop Ihre Grenzgeb 126: 666–670
Wedge JH, Oryschak AF, Robertson DE, Kirkaldy-Willis WH (1977) Atypical manifestations of spinal infections. Clin Orthop 123: 155–263
Woolsey RM (1986) Aortic laceration after anterior spinal fusion. Surg Neurol 25:267–268
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Eysel, P., Hopf, C., Vogel, I. et al. Primary stable anterior instrumentation or dorsoventral spondylodesis in spondylodiscitis?. Eur Spine J 6, 152–157 (1997). https://doi.org/10.1007/BF01301428
Received:
Revised:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF01301428