Abstract
Purpose
The incidence of spondylodiscitis is increasing. This study evaluates the behavior of cervical spondylodiscitis over a period of two decades in a single institution and compares the findings with the literature.
Methods
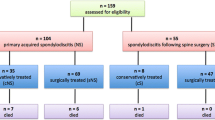
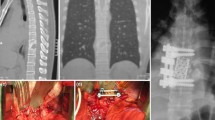
Between 1994 and 1999, 20 consecutive patients (group A) suffering from cervical spondylodiscitis underwent surgical treatment in our institution. These were compared to another group consisting of 30 patients (group B) undergoing surgery for the same disease between 2004 and 2009 again in our institution. All patients in both series underwent surgical debridement and reconstruction followed by antibiotic therapy for 8–12 weeks.
Results
The mean age at presentation increased significantly from 59.7 to 64.5 years. Male predominance was noticed in both groups. Accompanying neurological deficit was almost the same (40–45 %), while septicaemia increased from 15 to 40 %. Radiologically, epidural abscess formation increased from 60 to 80 %. The disease was mostly monosegmental in group A (85 %); while in group B, the disease became significantly more aggressive affecting two and three segments in 43.3 % of the cases. There was an increased tendency toward anterior alone surgery in group B (56.7 %) in comparison to group A (35 %). Mean period of follow-up was 2.8 years. Healing of the inflammation was the rule. Mortality rate increased from 5 to 10 %.
Conclusions
Cervical spondylodiscitis has increased and became more aggressive. While radical surgical debridement, stable reconstruction together with antibiotic therapy remained a reliable approach to achieve complete healing of the inflammation, anterior alone surgery became more applicable.



Similar content being viewed by others
References
Al-Nammari SS, Lucas JD, Lam KS (2007) Hematogenous methicillin-resistant Staphylococcus aureus spondylodiscitis. Spine (Phila Pa 1976) 32(22):2480–2486
Barrecheguren EG, Barriga A, Barroso JL, Villas C (2001) Cervical spondylodiscitis. Rev Med Univ Navarra 45(4):11–14 17–18
Currier BL, Kim CW, Heller JG, Eismont FJ (2005) Cervical spinal infections. In: Clark CR (ed) The cervical spine. Lippincott Williams & Wilkins, Philadelphia, pp 858–890
D’Agostino C, Scorzolini L, Massetti AP, Carnevalini M, d’Ettorre G, Venditti M, Vullo V, Orsi GB (2010) A seven-year prospective study on spondylodiscitis: epidemiological and microbiological features. Infection 38(2):102–107
Endress C, Guyot DR, Fata J, Salciccioli G (1990) Cervical osteomyelitis due to i.v. heroin use: radiologic findings in 14 patients. AJR Am J Roentgenol 155(2):333–335
Hadjipavlou AG, Mader JT, Necessary JT, Muffoletto AJ (2000) Hematogenous pyogenic spinal infections and their surgical management. Spine (Phila Pa 1976) 25(13):1668–1679
Kapteyn A (2010) What can we learn from (and about) global aging? Demography 47(Suppl):S191–S209
Karadimas EJ, Bunger C, Lindblad BE, Hansen ES, Høy K, Helmig P, Kannerup AS, Niedermann B (2008) Spondylodiscitis. A retrospective study of 163 patients. Acta Orthop 79(5):650–659
Krödel A, Stürz H, Siebert CH (1991) Indications for and results of operative treatment of spondylitis and spondylodiscitis. Arch Orthop Trauma Surg 110(2):78–82
Liebergall M, Chaimsky G, Lowe J, Robin GC, Floman Y (1991) Pyogenic vertebral osteomyelitis with paralysis. Prognosis and treatment. Clin Orthop Relat Res 269:142–150
Lu DC, Wang V, Chou D (2009) The use of allograft or autograft and expandable titanium cages for the treatment of vertebral osteomyelitis. Neurosurgery 64(1):122–130
Malawski SK, Lukawski S (1991) Pyogenic infection of the spine. Clin Orthop Relat Res 272:58–66
Mondorf Y, Gaab MR, Oertel JM (2009) PEEK cage cervical ventral fusion in spondylodiscitis. Acta Neurochir (Wien) 151(11):1537–1541
Muzii VF, Mariottini A, Zalaffi A, Carangelo BR, Palma L (2006) Cervical spine epidural abscess: experience with microsurgical treatment in eight cases. J Neurosurg Spine 5(5):392–397
Przybylski GJ, Sharan AD (2001) Single-stage autogenous bone grafting and internal fixation in the surgical management of pyogenic discitis and vertebral osteomyelitis. J Neurosurg 94(1 Suppl):1–7
Reihsaus E, Waldbaur H, Seeling W (2000) Spinal epidural abscess: a meta-analysis of 915 patients. Neurosurg Rev 23(4):175–205
Schimmer RC, Jeanneret C, Nunley PD, Jeanneret B (2002) Osteomyelitis of the cervical spine: a potentially dramatic disease. J Spinal Disord Tech 15(2):110–117
Schinkel C, Gottwald M, Andress HJ (2003) Surgical treatment of spondylodiscitis. Surg Infect (Larchmt) 4(4):387–391
Shad A, Shariff S, Fairbank J, Byren I, Teddy PJ, Cadoux-Hudson TA (2003) Internal fixation for osteomyelitis of cervical spine: the issue of persistence of culture positive infection around the implants. Acta Neurochir (Wien) 145(11):957–960
Spies EH, Stücker R, Reichelt A (1999) Conservative management of pyogenic osteomyelitis of the occipitocervical junction. Spine (Phila Pa 1976) 24(8):818–822
Stone JL, Cybulski GR, Rodriguez J, Gryfinski ME, Kant R (1989) Anterior cervical debridement and strut-grafting for osteomyelitis of the cervical spine. J Neurosurg 70(6):879–883
Suess O, Weise L, Brock M, Kombos T (2007) Debridement and spinal instrumentation as a single-stage procedure in bacterial spondylitis/spondylodiscitis. Zentralbl Neurochir 68(3):123–132
Walter J, Kuhn SA, Reichart R, Kalff R, Ewald C (2010) PEEK cages as a potential alternative in the treatment of cervical spondylodiscitis: a preliminary report on a patient series. Eur Spine J 19(6):1004–1009
Zigler JE, Bohlman HH, Robinson RA, Riley LH, Dodge LD (1987) Pyogenic osteomyelitis of the occiput, the atlas, and the axis. A report of five cases. J Bone Joint Surg Am 69(7):1069–1073
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shousha, M., Heyde, C. & Boehm, H. Cervical spondylodiscitis: change in clinical picture and operative management during the last two decades. A series of 50 patients and review of literature. Eur Spine J 24, 571–576 (2015). https://doi.org/10.1007/s00586-014-3672-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-014-3672-5