Abstract
Background
Computer-assisted surgery is a wide field of technologies with the potential to enable the surgeon to improve efficiency and efficacy of diagnosis, treatment, and clinical management.
Purpose
This review provides an overview of the most important new technologies and their applications.
Methods
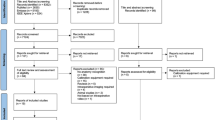
A MEDLINE database search was performed revealing a total of 1702 references. All references were considered for information on six main topics, namely image guidance and navigation, robot-assisted surgery, human-machine interface, surgical processes and clinical pathways, computer-assisted surgical training, and clinical decision support. Further references were obtained through cross-referencing the bibliography cited in each work. Based on their respective field of expertise, the authors chose 64 publications relevant for the purpose of this review.
Conclusion
Computer-assisted systems are increasingly used not only in experimental studies but also in clinical studies. Although computer-assisted abdominal surgery is still in its infancy, the number of studies is constantly increasing, and clinical studies start showing the benefits of computers used not only as tools of documentation and accounting but also for directly assisting surgeons during diagnosis and treatment of patients. Further developments in the field of clinical decision support even have the potential of causing a paradigm shift in how patients are diagnosed and treated.




Similar content being viewed by others
References
Foundation W (2015) Computer-assisted. http://en.wikipedia.org/wiki/Computer-aided. Accessed 25 Jan 2015
Mezger U, Jendrewski C, Bartels M (2013) Navigation in surgery. Langenbeck’s Arch Surg 398(4):501–514. doi:10.1007/s00423-013-1059-4
Marescaux J, Rubino F, Arenas M, Mutter D, Soler L (2004) Augmented-reality-assisted laparoscopic adrenalectomy. JAMA 292(18):2214–2215. doi:10.1001/jama.292.18.2214-c
Ieiri S, Uemura M, Konishi K, Souzaki R, Nagao Y, Tsutsumi N, Akahoshi T, Ohuchida K, Ohdaira T, Tomikawa M, Tanoue K, Hashizume M, Taguchi T (2012) Augmented reality navigation system for laparoscopic splenectomy in children based on preoperative CT image using optical tracking device. Pediatr Surg Int 28(4):341–346. doi:10.1007/s00383-011-3034-x
Onda S, Okamoto T, Kanehira M, Suzuki F, Ito R, Fujioka S, Suzuki N, Hattori A, Yanaga K (2014) Identification of inferior pancreaticoduodenal artery during pancreaticoduodenectomy using augmented reality-based navigation system. J Hepato-Biliary-Pancreat Sci 21(4):281–287. doi:10.1002/jhbp.25
Kenngott HG, Neuhaus J, Muller-Stich BP, Wolf I, Vetter M, Meinzer HP, Koninger J, Buchler MW, Gutt CN (2008) Development of a navigation system for minimally invasive esophagectomy. Surg Endosc 22(8):1858–1865. doi:10.1007/s00464-007-9723-9
Okamoto T, Onda S, Matsumoto M, Gocho T, Futagawa Y, Fujioka S, Yanaga K, Suzuki N, Hattori A (2013) Utility of augmented reality system in hepatobiliary surgery. J Hepato-Biliary-Pancreat Sci 20(2):249–253. doi:10.1007/s00534-012-0504-z
Kingham TP, Scherer MA, Neese BW, Clements LW, Stefansic JD, Jarnagin WR (2012) Image-guided liver surgery: intraoperative projection of computed tomography images utilizing tracked ultrasound. HPB (Oxford) 14(9):594–603. doi:10.1111/j.1477-2574.2012.00487.x
Peterhans M, vom Berg A, Dagon B, Inderbitzin D, Baur C, Candinas D, Weber S (2011) A navigation system for open liver surgery: design, workflow and first clinical applications. Int J Med Robot 7(1):7–16. doi:10.1002/rcs.360
Nozaki T, Fujiuchi Y, Komiya A, Fuse H (2013) Efficacy of DynaCT for surgical navigation during complex laparoscopic surgery: an initial experience. Surg Endosc 27(3):903–909. doi:10.1007/s00464-012-2531-x
Nozaki T, Iida Y, Morii A, Fujiuchi Y, Fuse H (2012) Laparoscopic radical nephrectomy under near real-time three-dimensional surgical navigation with C-arm cone beam computed tomography. Surg Innov 19(3):263–267. doi:10.1177/1553350611429690
Kenngott HG, Wagner M, Gondan M, Nickel F, Nolden M, Fetzer A, Weitz J, Fischer L, Speidel S, Meinzer HP, Bockler D, Buchler MW, Muller-Stich BP (2014) Real-time image guidance in laparoscopic liver surgery: first clinical experience with a guidance system based on intraoperative CT imaging. Surg Endosc 28(3):933–940. doi:10.1007/s00464-013-3249-0
Tsutsumi N, Tomikawa M, Uemura M, Akahoshi T, Nagao Y, Konishi K, Ieiri S, Hong J, Maehara Y, Hashizume M (2013) Image-guided laparoscopic surgery in an open MRI operating theater. Surg Endosc 27(6):2178–2184. doi:10.1007/s00464-012-2737-y
Lamade W, Vetter M, Hassenpflug P, Thorn M, Meinzer HP, Herfarth C (2002) Navigation and image-guided HBP surgery: a review and preview. J Hepato-Biliary-Pancreat Sci 9(5):592–599. doi:10.1007/s005340200079
Beller S, Hunerbein M, Eulenstein S, Lange T, Schlag PM (2007) Feasibility of navigated resection of liver tumors using multiplanar visualization of intraoperative 3-dimensional ultrasound data. Ann Surg 246(2):288–294. doi:10.1097/01.sla.0000264233.48306.99
Buchs NC, Volonte F, Pugin F, Toso C, Fusaglia M, Gavaghan K, Majno PE, Peterhans M, Weber S, Morel P (2013) Augmented environments for the targeting of hepatic lesions during image-guided robotic liver surgery. J Surg Res 184(2):825–831. doi:10.1016/j.jss.2013.04.032
Kranzfelder M, Staub C, Fiolka A, Schneider A, Gillen S, Wilhelm D, Friess H, Knoll A, Feussner H (2013) Toward increased autonomy in the surgical OR: needs, requests, and expectations. Surg Endosc 27(5):1681–1688. doi:10.1007/s00464-012-2656-y
Pandya A, Reisner L, King B, Lucas N, Composto A, Klein M, Ellis R (2014) A review of camera viewpoint automation in robotic and laparoscopic surgery. Robotics 3(3):310–329. doi:10.3390/robotics3030310
Gutt CN, Oniu T, Mehrabi A, Kashfi A, Schemmer P, Buchler MW (2004) Robot-assisted abdominal surgery. Br J Surg 91(11):1390–1397. doi:10.1002/bjs.4700
Kenngott HG, Fischer L, Nickel F, Rom J, Rassweiler J, Muller-Stich BP (2012) Status of robotic assistance—a less traumatic and more accurate minimally invasive surgery? Langenbeck’s Arch Surg 397(3):333–341. doi:10.1007/s00423-011-0859-7
Robertson C, Close A, Fraser C, Gurung T, Jia X, Sharma P, Vale L, Ramsay C, Pickard R (2013) Relative effectiveness of robot-assisted and standard laparoscopic prostatectomy as alternatives to open radical prostatectomy for treatment of localised prostate cancer: a systematic review and mixed treatment comparison meta-analysis. BJU Int 112(6):798–812. doi:10.1111/bju.12247
Moran PS, O’Neill M, Teljeur C, Flattery M, Murphy LA, Smyth G, Ryan M (2013) Robot-assisted radical prostatectomy compared with open and laparoscopic approaches: a systematic review and meta-analysis. Int J Urol Off J Jpn Urol Assoc 20(3):312–321. doi:10.1111/iju.12070
Sood A, Jeong W, Peabody JO, Hemal AK, Menon M (2014) Robot-assisted radical prostatectomy: inching toward gold standard. Urol Clin N Am 41(4):473–484. doi:10.1016/j.ucl.2014.07.002
Kim CW, Kim CH, Baik SH (2014) Outcomes of robotic-assisted colorectal surgery compared with laparoscopic and open surgery: a systematic review. J Gastrointest Surg 18(4):816–830. doi:10.1007/s11605-014-2469-5
Turchetti G, Palla I, Pierotti F, Cuschieri A (2012) Economic evaluation of da Vinci-assisted robotic surgery: a systematic review. Surg Endosc 26(3):598–606. doi:10.1007/s00464-011-1936-2
Park JS, Choi GS, Park SY, Kim HJ, Ryuk JP (2012) Randomized clinical trial of robot-assisted versus standard laparoscopic right colectomy. Br J Surg 99(9):1219–1226. doi:10.1002/bjs.8841
Muller-Stich BP, Reiter MA, Wente MN, Bintintan VV, Koninger J, Buchler MW, Gutt CN (2007) Robot-assisted versus conventional laparoscopic fundoplication: short-term outcome of a pilot randomized controlled trial. Surg Endosc 21(10):1800–1805. doi:10.1007/s00464-007-9268-y
Mi J, Kang Y, Chen X, Wang B, Wang Z (2010) Whether robot-assisted laparoscopic fundoplication is better for gastroesophageal reflux disease in adults: a systematic review and meta-analysis. Surg Endosc 24(8):1803–1814. doi:10.1007/s00464-009-0873-9
Gumbs AA, Croner R, Rodriguez A, Zuker N, Perrakis A, Gayet B (2013) 200 consecutive laparoscopic pancreatic resections performed with a robotically controlled laparoscope holder. Surg Endosc 27(10):3781–3791. doi:10.1007/s00464-013-2969-5
Gillen S, Pletzer B, Heiligensetzer A, Wolf P, Kleeff J, Feussner H, Furst A (2014) Solo-surgical laparoscopic cholecystectomy with a joystick-guided camera device: a case-control study. Surg Endosc 28(1):164–170. doi:10.1007/s00464-013-3142-x
Nicolau S, Soler L, Mutter D, Marescaux J (2011) Augmented reality in laparoscopic surgical oncology. Surg Oncol 20(3):189–201. doi:10.1016/j.suronc.2011.07.002
John S, Poh AC, Lim TC, Chan EH (2012) The iPad tablet computer for mobile on-call radiology diagnosis? Auditing discrepancy in CT and MRI reporting. J Digit Imaging 25(5):628–634
Berger E (2010) The iPad: gadget or medical godsend? Ann Emerg Med 56(1):A21–A22
Robinson JD (2012) The skeptical technophile: iPad review. J Digit Imaging 25(3):365–368. doi:10.1007/s10278-012-9467-5
Volonte F, Robert JH, Ratib O, Triponez F (2011) A lung segmentectomy performed with 3D reconstruction images available on the operating table with an iPad. Interact Cardiovasc Thorac Surg 12(6):1066–1068. doi:10.1510/icvts.2010.261073
MEVIS DF-IfBM Mobile Liver Explorer. Accessed 04 May 2014
Deng W, Li F, Wang M, Song Z (2013) Easy-to-use augmented reality neuronavigation using a wireless tablet PC. Stereotact Funct Neurosurg 92(1):17–24. doi:10.1159/000354816
Rassweiler JJ, Muller M, Fangerau M, Klein J, Goezen AS, Pereira P, Meinzer HP, Teber D (2012) iPad-assisted percutaneous access to the kidney using marker-based navigation: initial clinical experience. Eur Urol 61(3):628–631. doi:10.1016/j.eururo.2011.12.024
Muller M, Rassweiler MC, Klein J, Seitel A, Gondan M, Baumhauer M, Teber D, Rassweiler JJ, Meinzer HP, Maier-Hein L (2013) Mobile augmented reality for computer-assisted percutaneous nephrolithotomy. Int J Comput Assist Radiol Surg 8(4):663–675. doi:10.1007/s11548-013-0828-4
Peregrin T (2014) Surgeons see future applications for Google Glass. Bull Am Coll Surg 99(7):9–16
Inc TL (2015) Touch Free: The Myo Armband in Surgery. Thalmic Labs Inc. https://www.thalmic.com/blog/myo-armband-surgery/. Accessed 26 Jan 2015
Iannessi A, Marcy PY, Clatz O, Ayache N, Fillard P (2014) Touchless user interface for intraoperative image control: almost there. Radiographics 34(4):1142–1144. doi:10.1148/rg.344135158
Perrakis A, Hohenberger W, Horbach T (2013) Integrated operation systems and voice recognition in minimally invasive surgery: comparison of two systems. Surg Endosc 27(2):575–579. doi:10.1007/s00464-012-2488-9
Schreinemacher MH, Graafland M, Schijven MP (2014) Google glass in surgery. Surg Innov 21(6):651–652. doi:10.1177/1553350614546006
Rotter T, Kinsman L, James E, Machotta A, Gothe H, Willis J, Snow P, Kugler J (2010) Clinical pathways: effects on professional practice, patient outcomes, length of stay and hospital costs. Cochrane Database Syst Rev 3, CD006632. doi:10.1002/14651858.CD006632.pub2
Strasser M, Pfeifer F, Helm E, Schuler A, Altmann J (2011) Defining and reconstructing clinical processes based on IHE and BPMN 2.0. Stud Health Technol Inform 169:482–486
Scheuerlein H, Rauchfuss F, Dittmar Y, Molle R, Lehmann T, Pienkos N, Settmacher U (2012) New methods for clinical pathways-Business Process Modeling Notation (BPMN) and Tangible Business Process Modeling (t.BPM). Langenbeck’s Arch Surg 397(5):755–761. doi:10.1007/s00423-012-0914-z
Poulymenopoulou M, Papakonstantinou D, Malamateniou F, Vassilacopoulos G (2014) Adaptive healthcare processes for personalized emergency clinical pathways. Stud Health Technol Inform 205:423–427
Doebbeling BN, Burton MM, Wiebke EA, Miller S, Baxter L, Miller D, Alvarez J, Pekny J (2012) Optimizing perioperative decision making: improved information for clinical workflow planning. AMIA Annu Symp Proc 2012:154–163
Aggarwal R, Balasundaram I, Darzi A (2008) Training opportunities and the role of virtual reality simulation in acquisition of basic laparoscopic skills. J Surg Res 145(1):80–86. doi:10.1016/j.jss.2007.04.027
Aggarwal R, Darzi A (2005) Training in laparoscopy—which model to use? Indian J Gastroenterol 24(3):95–96
Aggarwal R, Moorthy K, Darzi A (2004) Laparoscopic skills training and assessment. Br J Surg 91(12):1549–1558. doi:10.1002/bjs.4816
Korndorffer JR Jr, Stefanidis D, Scott DJ (2006) Laparoscopic skills laboratories: current assessment and a call for resident training standards. Am J Surg 191(1):17–22. doi:10.1016/j.amjsurg.2005.05.048
Undre S, Darzi A (2007) Laparoscopy simulators. J Endourol 21(3):274–279. doi:10.1089/end.2007.9980
EU Hernia Trialists Collaboration (2000) Laparoscopic compared with open methods of groin hernia repair: systematic review of randomized controlled trials. Br J Surg 87(7):860–867. doi:10.1046/j.1365-2168.2000.01540.x
Clinical Outcomes of Surgical Therapy Study Group (2004) A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 350(20):2050–2059. doi:10.1056/NEJMoa032651
Hamad GG, Curet M (2010) Minimally invasive surgery. Am J Surg 199(2):263–265. doi:10.1016/j.amjsurg.2009.05.008
Harrell AG, Heniford BT (2005) Minimally invasive abdominal surgery: lux et veritas past, present, and future. Am J Surg 190(2):239–243
Ayodeji ID, Schijven M, Jakimowicz J, Greve JW (2007) Face validation of the Simbionix LAP Mentor virtual reality training module and its applicability in the surgical curriculum. Surg Endosc 21(9):1641–1649. doi:10.1007/s00464-007-9219-7
Schijven MP, Jakimowicz JJ, Broeders IA, Tseng LN (2005) The Eindhoven laparoscopic cholecystectomy training course—improving operating room performance using virtual reality training: results from the first E.A.E.S. accredited virtual reality trainings curriculum. Surg Endosc 19(9):1220–1226. doi:10.1007/s00464-004-2240-1
Zendejas B, Cook DA, Bingener J, Huebner M, Dunn WF, Sarr MG, Farley DR (2011) Simulation-based mastery learning improves patient outcomes in laparoscopic inguinal hernia repair: a randomized controlled trial. Ann Surg 254(3):502–509. doi:10.1097/SLA.0b013e31822c6994, discussion 509–511
Pape-Koehler C, Chmelik C, Aslund AM, Heiss MM (2010) An interactive and multimedia-based manual of surgical procedures: Webop—an approach to improve surgical education. Zentralbl Chir 135(5):467–471. doi:10.1055/s-0030-1262538
Mutter D, Vix M, Dallemagne B, Perretta S, Leroy J, Marescaux J (2011) WeBSurg: an innovative educational Web site in minimally invasive surgery—principles and results. Surg Innov 18(1):8–14. doi:10.1177/1553350611398880
Pape-Koehler C, Immenroth M, Sauerland S, Lefering R, Lindlohr C, Toaspern J, Heiss M (2013) Multimedia-based training on Internet platforms improves surgical performance: a randomized controlled trial. Surg Endosc 27(5):1737–1747. doi:10.1007/s00464-012-2672-y
Muller-Stich BP, Lob N, Wald D, Bruckner T, Meinzer HP, Kadmon M, Buchler MW, Fischer L (2013) Regular three-dimensional presentations improve in the identification of surgical liver anatomy—a randomized study. BMC Med Educ 13:131. doi:10.1186/1472-6920-13-131
Nickel F, Bintintan VV, Gehrig T, Kenngott HG, Fischer L, Gutt CN, Muller-Stich BP (2013) Virtual reality does not meet expectations in a pilot study on multimodal laparoscopic surgery training. World J Surg 37(5):965–973. doi:10.1007/s00268-013-1963-3
Brinkman WM, Havermans SY, Buzink SN, Botden SM, Jakimowicz JJ, Schoot BC (2012) Single versus multimodality training basic laparoscopic skills. Surg Endosc 26(8):2172–2178. doi:10.1007/s00464-012-2184-9
Zimmerman H, Latifi R, Dehdashti B, Ong E, Jie T, Galvani C, Waer A, Wynne J, Biffar D, Gruessner R (2011) Intensive laparoscopic training course for surgical residents: program description, initial results, and requirements. Surg Endosc 25(11):3636–3641. doi:10.1007/s00464-011-1770-6
Eberhardt J, Bilchik A, Stojadinovic A (2012) Clinical decision support systems: potential with pitfalls. J Surg Oncol 105(5):502–510. doi:10.1002/jso.23053
Musen MA, Middleton B, Greenes RA (2014) Clinical decision-support systems. In: Biomedical informatics. Springer, pp 643–674
Shortliffe EH (1976) Computer-based medical consultations, MYCIN. Artificial intelligence series, vol 2. Elsevier, New York
Stojadinovic A, Bilchik A, Smith D, Eberhardt JS, Ward EB, Nissan A, Johnson EK, Protic M, Peoples GE, Avital I, Steele SR (2013) Clinical decision support and individualized prediction of survival in colon cancer: bayesian belief network model. Ann Surg Oncol 20(1):161–174. doi:10.1245/s10434-012-2555-4
Cucchetti A, Vivarelli M, Heaton ND, Phillips S, Piscaglia F, Bolondi L, La Barba G, Foxton MR, Rela M, O’Grady J, Pinna AD (2007) Artificial neural network is superior to MELD in predicting mortality of patients with end-stage liver disease. Gut 56(2):253–258. doi:10.1136/Gut.2005.084434
Hsieh CH, Lu RH, Lee NH, Chiu WT, Hsu MH, Li YC (2011) Novel solutions for an old disease: diagnosis of acute appendicitis with random forest, support vector machines, and artificial neural networks. Surgery 149(1):87–93. doi:10.1016/J.Surg.2010.03.023
Prabhudesai SG, Gould S, Rekhraj S, Tekkis PP, Glazer G, Ziprin P (2008) Artificial neural networks: useful aid in diagnosing acute appendicitis. World J Surg 32(2):305–309. doi:10.1007/s00268-007-9298-6, discussion 310-301
Acknowledgments
This study has been conducted within the Transregional Collaborative Research Center (TCRC) 125 “Cognition-Guided Surgery”, funded by the German Research Foundation (DFG).
We thank Ms. Béivin-Vanessa Pyne for reviewing the manuscript as a native speaker.
Compliance with Ethical Standards
This study has been conducted in compliance with ethical standards as set in the declaration of Helsinki. The figures supplied were conducted within our working group; detailed results are yet to be published. Informed consent was obtained for the tablet-based augmented reality experiment (Fig. 3). An animal trial (Fig. 2) has been approved by the local authorities.
Conflicts of interest
None.
Author’s contributions
Kenngott HG: study conception and design, acquisition of data, analysis and interpretation of data, and drafting of manuscript.
Wagner M: acquisition of data, analysis and interpretation of data, and drafting of manuscript.
Nickel F: acquisition of data, analysis and interpretation of data, and drafting of manuscript.
Wekerle AL: acquisition of data, analysis and interpretation of data, and drafting of manuscript.
Preukschas A: acquisition of data, analysis and interpretation of data, and drafting of manuscript.
Apitz M: acquisition of data, analysis and interpretation of data, and drafting of manuscript.
Schulte T: acquisition of data, analysis and interpretation of data, and drafting of manuscript.
Rempel R: acquisition of data, analysis and interpretation of data, and drafting of manuscript
Mietkowski P: acquisition of data, analysis and interpretation of data, and drafting of manuscript
Wagner F: acquisition of data, analysis and interpretation of data, and drafting of manuscript
Termer A: acquisition of data, analysis and interpretation of data, and drafting of manuscript
Beat P. Müller-Stich: study conception and design, analysis and interpretation of data, and drafting of manuscript
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kenngott, H.G., Wagner, M., Nickel, F. et al. Computer-assisted abdominal surgery: new technologies. Langenbecks Arch Surg 400, 273–281 (2015). https://doi.org/10.1007/s00423-015-1289-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-015-1289-8