Abstract
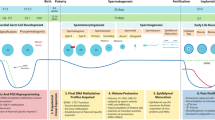
Male gamete development begins with the specification of primordial cells in the epiblast of the early embryo and is not complete until spermatozoa mature in the epididymis of adult males. This protracted developmental process involves extensive alteration of the paternal germline epigenome. Initially, epigenetic reprogramming in fetal germ cells results in removal of most DNA methylation, including parent-specific epigenetic information. The germ cells then establish sex-specific epigenetic information through de novo methylation and undergo spermatogenesis. Chromatin in haploid germ cells is repackaged into protamines during spermiogenesis, providing further widespread epigenetic reorganization. Finally, after fertilization, epigenetic reprogramming in the preimplantation embryo is necessary for regaining totipotency. These events provide substantial windows during which epigenetic errors either may be corrected or may occur in the germline. There is now increasing evidence that environmental factors such as exposure to toxicants, the parents’ and individual’s diet, and even infectious and inflammatory events in the male reproductive tract may influence epigenetic reprogramming. This, together with other damage inflicted on the germline chromatin, may result in negative consequences for fertility and health. Large epidemiological birth cohort studies have yielded insight into possible causative environmental factors. Together with experimental animal studies, a clearer view of environmental impacts on fetal development and their intergenerational and even transgenerational effects on reproductive health has emerged and is reviewed in this article.



Similar content being viewed by others
References
Lucas-Herald AK, Bashamboo A (2014) Gonadal development. Endocr Dev 27:1–16. doi:10.1159/000363608
Eggers S, Ohnesorg T, Sinclair A (2014) Genetic regulation of mammalian gonad development. Nat Rev Endocrinol 10(11):673–683. doi:10.1038/nrendo.2014.163
Shaw G, Renfree MB (2014) Wolffian duct development. Sex Dev 8(5):273–280. doi:10.1159/000363432
Hinton BT, Galdamez MM, Sutherland A, Bomgardner D, Xu B, Abdel-Fattah R, Yang L (2011) How do you get six meters of epididymis inside a human scrotum? J Androl 32(6):558–564. doi:10.2164/jandrol.111.013029
Branford WW, Benson GV, Ma L, Maas RL, Potter SS (2000) Characterization of Hoxa-10/Hoxa-11 transheterozygotes reveals functional redundancy and regulatory interactions. Dev Biol 224(2):373–387. doi:10.1006/dbio.2000.9809
Snyder EM, Small CL, Bomgardner D, Xu B, Evanoff R, Griswold MD, Hinton BT (2010) Gene expression in the efferent ducts, epididymis, and vas deferens during embryonic development of the mouse. Dev Dyn 239(9):2479–2491. doi:10.1002/dvdy.22378
Tomaszewski J, Joseph A, Archambeault D, Yao HH (2007) Essential roles of inhibin beta A in mouse epididymal coiling. Proc Natl Acad Sci U S A 104(27):11322–11327. doi:10.1073/pnas.0703445104
Winnall WR, Wu H, Sarraj MA, Rogers PA, de Kretser DM, Girling JE, Hedger MP (2013) Expression patterns of activin, inhibin and follistatin variants in the adult male mouse reproductive tract suggest important roles in the epididymis and vas deferens. Reprod Fertil Dev 25(3):570–580. doi:10.1071/RD11287
Stammler A, Hau T, Bhushan S, Meinhardt A, Jonigk D, Lippmann T, Pilatz A, Schneider-Huther I, Middendorff R (2015) Epididymitis: ascending infection restricted by segmental boundaries. Hum Reprod 30(7):1557–1565. doi:10.1093/humrep/dev112
Rowley MJ, Teshima F, Heller CG (1970) Duration of transit of spermatozoa through the human male ductular system. Fertil Steril 21(5):390–396
Aitken RJ, Baker HW (1995) Seminal leukocytes: passengers, terrorists or good samaritans? Hum Reprod 10(7):1736–1739
Aitken RJ, Baker MA (2013) Oxidative stress, spermatozoa and leukocytic infiltration: relationships forged by the opposing forces of microbial invasion and the search for perfection. J Reprod Immunol 100(1):11–19. doi:10.1016/j.jri.2013.06.005
Michel V, Pilatz A, Hedger MP, Meinhardt A (2015) Epididymitis: revelations at the convergence of clinical and basic sciences. Asian J Androl 17(5):756–763. doi:10.4103/1008-682X.155770
Fijak M, Bhushan S, Meinhardt A (2011) Immunoprivileged sites: the testis. Methods Mol Biol 677:459–470. doi:10.1007/978-1-60761-869-0_29
Fijak M, Meinhardt A (2006) The testis in immune privilege. Immunol Rev 213:66–81
Hedger MP, Hales DB (2006) Immunophysiology of the male reproductive tract. In: Knobil E, Neill J (eds) Physiology of reproduction, 3rd edn. Academic, Amsterdam, pp 1195–1286
Zhao S, Zhu W, Xue S, Han D (2014) Testicular defense systems: immune privilege and innate immunity. Cell Mol Immunol 11(5):428–437. doi:10.1038/cmi.2014.38
Hedger MP (2011) Immunophysiology and pathology of inflammation in the testis and epididymis. J Androl 32(6):625–640. doi:10.2164/jandrol.111.012989
Mahi-Brown CA, Yule TD, Tung KS (1988) Evidence for active immunological regulation in prevention of testicular autoimmune disease independent of the blood-testis barrier. Am J Reprod Immunol Microbiol 16(4):165–170
Head JR, Billingham RE (1985) Immunologically privileged sites in transplantation immunology and oncology. Perspect Biol Med 29(1):115–131
Head JR, Billingham RE (1985) Immune privilege in the testis. II Evaluation of potential local factors. Transplantation 40(3):269–275
Head JR, Neaves WB, Billingham RE (1983) Immune privilege in the testis. I. Basic parameters of allograft survival. Transplantation 36(4):423–431
Schuppe HC, Meinhardt A (2005) Immune privilege and inflammation of the testis. Chem Immunol Allergy 88:1–14
Hedger MP (1997) Testicular leukocytes: what are they doing? Rev Reprod 2(1):38–47
Winnall WR, Muir JA, Hedger MP (2011) Rat resident testicular macrophages have an alternatively activated phenotype and constitutively produce interleukin-10 in vitro. J Leukoc Biol 90(1):133–143. doi:10.1189/jlb.1010557
Hedger MP, Winnall WR (2012) Regulation of activin and inhibin in the adult testis and the evidence for functional roles in spermatogenesis and immunoregulation. Mol Cell Endocrinol 359(1–2):30–42. doi:10.1016/j.mce.2011.09.031
Bhushan S, Tchatalbachev S, Lu Y, Frohlich S, Fijak M, Vijayan V, Chakraborty T, Meinhardt A (2015) Differential activation of inflammatory pathways in testicular macrophages provides a rationale for their subdued inflammatory capacity. J Immunol 194(11):5455–5464. doi:10.4049/jimmunol.1401132
Bhushan S, Tchatalbachev S, Klug J, Fijak M, Pineau C, Chakraborty T, Meinhardt A (2008) Uropathogenic Escherichia coli block MyD88-dependent and activate MyD88-independent signaling pathways in rat testicular cells. J Immunol 180(8):5537–5547
Bhushan S, Hossain H, Lu Y, Geisler A, Tchatalbachev S, Mikulski Z, Schuler G, Klug J, Pilatz A, Wagenlehner F, Chakraborty T, Meinhardt A (2011) Uropathogenic E. coli induce different immune response in testicular and peritoneal macrophages: implications for testicular immune privilege. PLoS One 6(12):e28452. doi:10.1371/journal.pone.0028452
Bhushan S, Schuppe HC, Tchatalbachev S, Fijak M, Weidner W, Chakraborty T, Meinhardt A (2009) Testicular innate immune defense against bacteria. Mol Cell Endocrinol 306(1–2):37–44. doi:10.1016/j.mce.2008.10.017
Hutson JC (1994) Testicular macrophages. Int Rev Cytol 149:99–143
Bhushan S, Schuppe HC, Fijak M, Meinhardt A (2009) Testicular infection: microorganisms, clinical implications and host-pathogen interaction. J Reprod Immunol 83(1–2):164–167. doi:10.1016/j.jri.2009.07.007
Hedger MP (2002) Macrophages and the immune responsiveness of the testis. J Reprod Immunol 57(1–2):19–34
Nashan D, Malorny U, Sorg C, Cooper T, Nieschlag E (1989) Immuno-competent cells in the murine epididymis. Int J Androl 12(1):85–94
Nashan D, Cooper TG, Knuth UA, Schubeus P, Sorg C, Nieschlag E (1990) Presence and distribution of leukocyte subsets in the murine epididymis after vasectomy. Int J Androl 13(1):39–49
Shum WW, Smith TB, Cortez-Retamozo V, Grigoryeva LS, Roy JW, Hill E, Pittet MJ, Breton S, Da Silva N (2014) Epithelial basal cells are distinct from dendritic cells and macrophages in the mouse epididymis. Biol Reprod 90(5):90. doi:10.1095/biolreprod.113.116681
Da Silva N, Cortez-Retamozo V, Reinecker HC, Wildgruber M, Hill E, Brown D, Swirski FK, Pittet MJ, Breton S (2011) A dense network of dendritic cells populates the murine epididymis. Reproduction 141(5):653–663. doi:10.1530/REP-10-0493
Rival C, Wheeler K, Jeffrey S, Qiao H, Luu B, Tewalt EF, Engelhard VH, Tardif S, Hardy D, del Rio R, Teuscher C, Tung K (2013) Regulatory T cells and vasectomy. J Reprod Immunol 100(1):66–75. doi:10.1016/j.jri.2013.08.004
Wheeler K, Tardif S, Rival C, Luu B, Bui E, Del Rio R, Teuscher C, Sparwasser T, Hardy D, Tung KS (2011) Regulatory T cells control tolerogenic versus autoimmune response to sperm in vasectomy. Proc Natl Acad Sci U S A 108(18):7511–7516. doi:10.1073/pnas.1017615108
Ying Y, Qi X, Zhao GQ (2001) Induction of primordial germ cells from murine epiblasts by synergistic action of BMP4 and BMP8B signaling pathways. Proc Natl Acad Sci U S A 98(14):7858–7862. doi:10.1073/pnas.151242798
Gaskell TL, Esnal A, Robinson LL, Anderson RA, Saunders PT (2004) Immunohistochemical profiling of germ cells within the human fetal testis: identification of three subpopulations. Biol Reprod 71(6):2012–2021. doi:10.1095/biolreprod.104.028381
Western PS, Miles DC, van den Bergen JA, Burton M, Sinclair AH (2008) Dynamic regulation of mitotic arrest in fetal male germ cells. Stem Cells 26(2):339–347. doi:10.1634/stemcells.2007-0622
Hilscher B, Hilscher W, Bulthoff-Ohnolz B, Kramer U, Birke A, Pelzer H, Gauss G (1974) Kinetics of gametogenesis. I. Comparative histological and autoradiographic studies of oocytes and transitional prospermatogonia during oogenesis and prespermatogenesis. Cell Tissue Res 154(4):443–470
McLaren A (2003) Primordial germ cells in the mouse. Dev Biol 262(1):1–15
Bendsen E, Byskov AG, Laursen SB, Larsen HP, Andersen CY, Westergaard LG (2003) Number of germ cells and somatic cells in human fetal testes during the first weeks after sex differentiation. Hum Reprod 18(1):13–18
Oakberg EF (1956) Duration of spermatogenesis in the mouse and timing of stages of the cycle of the seminiferous epithelium. Am J Anat 99(3):507–516. doi:10.1002/aja.1000990307
Heller CG, Clermont Y (1963) Spermatogenesis in man: an estimate of its duration. Science 140(3563):184–186
Schagdarsurengin U, Paradowska A, Steger K (2012) Analysing the sperm epigenome: roles in early embryogenesis and assisted reproduction. Nat Rev Urol 9(11):609–619. doi:10.1038/nrurol.2012.183
Steger K, Klonisch T, Gavenis K, Drabent B, Doenecke D, Bergmann M (1998) Expression of mRNA and protein of nucleoproteins during human spermiogenesis. Mol Hum Reprod 4(10):939–945
Carrell DT (2008) Contributions of spermatozoa to embryogenesis: assays to evaluate their genetic and epigenetic fitness. Reprod Biomed Online 16(4):474–484
Lelancette C, Miller D, Li Y, Krawetz SA (2008) Paternal contributions: new functional insights for spermatozoal RNA. J Cell Biochem 104(5):1570–1579. doi:10.1002/jcb.21756
Yan W, Morozumi K, Zhang J, Ro S, Park C, Yanagimachi R (2008) Birth of mice after intracytoplasmic injection of single purified sperm nuclei and detection of messenger RNAs and microRNAs in the sperm nuclei. Biol Reprod 78(5):896–902. doi:10.1095/biolreprod.107.067033
Song R, Hennig GW, Wu Q, Jose C, Zheng H, Yan W (2011) Male germ cells express abundant endogenous siRNAs. Proc Natl Acad Sci U S A 108(32):13159–13164. doi:10.1073/pnas.1108567108
Krawetz SA, Kruger A, Lalancette C, Tagett R, Anton E, Draghici S, Diamond MP (2011) A survey of small RNAs in human sperm. Hum Reprod 26(12):3401–3412. doi:10.1093/humrep/der329
Valeri N, Vannini I, Fanini F, Calore F, Adair B, Fabbri M (2009) Epigenetics, miRNAs, and human cancer: a new chapter in human gene regulation. Mamm Genome 20(9–10):573–580. doi:10.1007/s00335-009-9206-5
Iorio MV, Piovan C, Croce CM (2010) Interplay between microRNAs and the epigenetic machinery: an intricate network. Biochim Biophys Acta 1799(10–12):694–701. doi:10.1016/j.bbagrm.2010.05.005
Miller D (2007) Ensuring continuity of the paternal genome: potential roles for spermatozoal RNA in mammalian embryogenesis. Soc Reprod Fertil Suppl 65:373–389
Liu WM, Pang RT, Chiu PC, Wong BP, Lao K, Lee KF, Yeung WS (2012) Sperm-borne microRNA-34c is required for the first cleavage division in mouse. Proc Natl Acad Sci U S A 109(2):490–494. doi:10.1073/pnas.1110368109
Baylin SB (2005) DNA methylation and gene silencing in cancer. Nat Clin Pract Oncol 2(Suppl 1):S4–S11. doi:10.1038/ncponc0354
Rice JC, Allis CD (2001) Histone methylation versus histone acetylation: new insights into epigenetic regulation. Curr Opin Cell Biol 13(3):263–273
Roth SY, Denu JM, Allis CD (2001) Histone acetyltransferases. Annu Rev Biochem 70:81–120. doi:10.1146/annurev.biochem.70.1.81
Thiagalingam S, Cheng KH, Lee HJ, Mineva N, Thiagalingam A, Ponte JF (2003) Histone deacetylases: unique players in shaping the epigenetic histone code. Ann N Y Acad Sci 983:84–100
Fischle W, Wang Y, Jacobs SA, Kim Y, Allis CD, Khorasanizadeh S (2003) Molecular basis for the discrimination of repressive methyl-lysine marks in histone H3 by Polycomb and HP1 chromodomains. Genes Dev 17(15):1870–1881. doi:10.1101/gad.1110503
Santos-Rosa H, Schneider R, Bannister AJ, Sherriff J, Bernstein BE, Emre NC, Schreiber SL, Mellor J, Kouzarides T (2002) Active genes are tri-methylated at K4 of histone H3. Nature 419(6905):407–411. doi:10.1038/nature01080
Kato Y, Kaneda M, Hata K, Kumaki K, Hisano M, Kohara Y, Okano M, Li E, Nozaki M, Sasaki H (2007) Role of the Dnmt3 family in de novo methylation of imprinted and repetitive sequences during male germ cell development in the mouse. Hum Mol Genet 16(19):2272–2280. doi:10.1093/hmg/ddm179
Bourc’his D, Bestor TH (2004) Meiotic catastrophe and retrotransposon reactivation in male germ cells lacking Dnmt3L. Nature 431(7004):96–99. doi:10.1038/nature02886
Kaneda M, Okano M, Hata K, Sado T, Tsujimoto N, Li E, Sasaki H (2004) Essential role for de novo DNA methyltransferase Dnmt3a in paternal and maternal imprinting. Nature 429(6994):900–903. doi:10.1038/nature02633
La Salle S, Oakes CC, Neaga OR, Bourc’his D, Bestor TH, Trasler JM (2007) Loss of spermatogonia and wide-spread DNA methylation defects in newborn male mice deficient in DNMT3L. BMC Dev Biol 7:104. doi:10.1186/1471-213X-7-104
Daxinger L, Oey H, Isbel L, Whitelaw NC, Youngson NA, Spurling A, Vonk KK, Whitelaw E (2016) Hypomethylation of ERVs in the sperm of mice haploinsufficient for the histone methyltransferase Setdb1 correlates with a paternal effect on phenotype. Sci Rep 6:25004. doi:10.1038/srep25004
Liu S, Brind’Amour J, Karimi MM, Shirane K, Bogutz A, Lefebvre L, Sasaki H, Shinkai Y, Lorincz MC (2014) Setdb1 is required for germline development and silencing of H3K9me3-marked endogenous retroviruses in primordial germ cells. Genes Dev 28(18):2041–2055. doi:10.1101/gad.244848.114
Dalgaard K, Landgraf K, Heyne S, Lempradl A, Longinotto J, Gossens K, Ruf M, Orthofer M, Strogantsev R, Selvaraj M, Lu TT, Casas E, Teperino R, Surani MA, Zvetkova I, Rimmington D, Tung YC, Lam B, Larder R, Yeo GS, O’Rahilly S, Vavouri T, Whitelaw E, Penninger JM, Jenuwein T, Cheung CL, Ferguson-Smith AC, Coll AP, Korner A, Pospisilik JA (2016) Trim28 haploinsufficiency triggers bi-stable epigenetic obesity. Cell 164(3):353–364. doi:10.1016/j.cell.2015.12.025
Weick EM, Miska EA (2014) piRNAs: from biogenesis to function. Development 141(18):3458–3471. doi:10.1242/dev.094037
Mu W, Starmer J, Fedoriw AM, Yee D, Magnuson T (2014) Repression of the soma-specific transcriptome by Polycomb-repressive complex 2 promotes male germ cell development. Genes Dev 28(18):2056–2069. doi:10.1101/gad.246124.114
Hogg K, Western PS (2015) Refurbishing the germline epigenome: out with the old, in with the new. Semin Cell Dev Biol 45:104–113. doi:10.1016/j.semcdb.2015.09.012
Lesch BJ, Dokshin GA, Young RA, McCarrey JR, Page DC (2013) A set of genes critical to development is epigenetically poised in mouse germ cells from fetal stages through completion of meiosis. Proc Natl Acad Sci U S A 110(40):16061–16066. doi:10.1073/pnas.1315204110
Hammoud SS, Nix DA, Zhang H, Purwar J, Carrell DT, Cairns BR (2009) Distinctive chromatin in human sperm packages genes for embryo development. Nature 460(7254):473–478. doi:10.1038/nature08162
Brykczynska U, Hisano M, Erkek S, Ramos L, Oakeley EJ, Roloff TC, Beisel C, Schubeler D, Stadler MB, Peters AH (2010) Repressive and active histone methylation mark distinct promoters in human and mouse spermatozoa. Nat Struct Mol Biol 17(6):679–687. doi:10.1038/nsmb.1821
Lesch BJ, Page DC (2014) Poised chromatin in the mammalian germ line. Development 141(19):3619–3626. doi:10.1242/dev.113027
Sonnack V, Failing K, Bergmann M, Steger K (2002) Expression of hyperacetylated histone H4 during normal and impaired human spermatogenesis. Andrologia 34(6):384–390
Fenic I, Sonnack V, Failing K, Bergmann M, Steger K (2004) In vivo effects of histone-deacetylase inhibitor trichostatin-A on murine spermatogenesis. J Androl 25(5):811–818
Siklenka K, Erkek S, Godmann M, Lambrot R, McGraw S, Lafleur C, Cohen T, Xia J, Suderman M, Hallett M, Trasler J, Peters AH, Kimmins S (2015) Disruption of histone methylation in developing sperm impairs offspring health transgenerationally. Science 350(6261):aab2006. doi:10.1126/science.aab2006
Balhorn R, Reed S, Tanphaichitr N (1988) Aberrant protamine 1/protamine 2 ratios in sperm of infertile human males. Experientia 44(1):52–55
Rogenhofer N, Dansranjavin T, Schorsch M, Spiess A, Wang H, von Schonfeldt V, Cappallo-Obermann H, Baukloh V, Yang H, Paradowska A, Chen B, Thaler CJ, Weidner W, Schuppe HC, Steger K (2013) The sperm protamine mRNA ratio as a clinical parameter to estimate the fertilizing potential of men taking part in an ART programme. Hum Reprod 28(4):969–978. doi:10.1093/humrep/des471
Hammoud SS, Purwar J, Pflueger C, Cairns BR, Carrell DT (2010) Alterations in sperm DNA methylation patterns at imprinted loci in two classes of infertility. Fertil Steril 94(5):1728–1733. doi:10.1016/j.fertnstert.2009.09.010
Weaver JR, Susiarjo M, Bartolomei MS (2009) Imprinting and epigenetic changes in the early embryo. Mamm Genome 20(9–10):532–543. doi:10.1007/s00335-009-9225-2
Ly L, Chan D, Trasler JM (2015) Developmental windows of susceptibility for epigenetic inheritance through the male germline. Semin Cell Dev Biol 43:96–105. doi:10.1016/j.semcdb.2015.07.006
Jones EL, Zalensky AO, Zalenskaya IA (2011) Protamine withdrawal from human sperm nuclei following heterologous ICSI into hamster oocytes. Protein Pept Lett 18(8):811–816
Jodar M, Selvaraju S, Sendler E, Diamond MP, Krawetz SA, Reproductive Medicine N (2013) The presence, role and clinical use of spermatozoal RNAs. Hum Reprod Update 19(6):604–624. doi:10.1093/humupd/dmt031
Kagiwada S, Kurimoto K, Hirota T, Yamaji M, Saitou M (2013) Replication-coupled passive DNA demethylation for the erasure of genome imprints in mice. EMBO J 32(3):340–353. doi:10.1038/emboj.2012.331
Hill PW, Amouroux R, Hajkova P (2014) DNA demethylation, Tet proteins and 5-hydroxymethylcytosine in epigenetic reprogramming: an emerging complex story. Genomics 104(5):324–333. doi:10.1016/j.ygeno.2014.08.012
Smallwood SA, Kelsey G (2012) De novo DNA methylation: a germ cell perspective. Trends Genet 28(1):33–42. doi:10.1016/j.tig.2011.09.004
Smith ZD, Chan MM, Mikkelsen TS, Gu H, Gnirke A, Regev A, Meissner A (2012) A unique regulatory phase of DNA methylation in the early mammalian embryo. Nature 484(7394):339–344. doi:10.1038/nature10960
Seisenberger S, Andrews S, Krueger F, Arand J, Walter J, Santos F, Popp C, Thienpont B, Dean W, Reik W (2012) The dynamics of genome-wide DNA methylation reprogramming in mouse primordial germ cells. Mol Cell 48(6):849–862. doi:10.1016/j.molcel.2012.11.001
Western P (2009) Foetal germ cells: striking the balance between pluripotency and differentiation. Int J Dev Biol 53(2–3):393–409. doi:10.1387/ijdb.082671pw
Seki Y, Hayashi K, Itoh K, Mizugaki M, Saitou M, Matsui Y (2005) Extensive and orderly reprogramming of genome-wide chromatin modifications associated with specification and early development of germ cells in mice. Dev Biol 278(2):440–458. doi:10.1016/j.ydbio.2004.11.025
Li JY, Lees-Murdock DJ, Xu GL, Walsh CP (2004) Timing of establishment of paternal methylation imprints in the mouse. Genomics 84(6):952–960. doi:10.1016/j.ygeno.2004.08.012
Arnaud P (2010) Genomic imprinting in germ cells: imprints are under control. Reproduction 140(3):411–423. doi:10.1530/REP-10-0173
Mochizuki K, Tachibana M, Saitou M, Tokitake Y, Matsui Y (2012) Implication of DNA demethylation and bivalent histone modification for selective gene regulation in mouse primordial germ cells. PLoS One 7(9):e46036. doi:10.1371/journal.pone.0046036
Sachs M, Onodera C, Blaschke K, Ebata KT, Song JS, Ramalho-Santos M (2013) Bivalent chromatin marks developmental regulatory genes in the mouse embryonic germline in vivo. Cell Rep 3(6):1777–1784. doi:10.1016/j.celrep.2013.04.032
Erkek S, Hisano M, Liang CY, Gill M, Murr R, Dieker J, Schubeler D, van der Vlag J, Stadler MB, Peters AH (2013) Molecular determinants of nucleosome retention at CpG-rich sequences in mouse spermatozoa. Nat Struct Mol Biol 20(7):868–875. doi:10.1038/nsmb.2599
Samans B, Yang Y, Krebs S, Sarode GV, Blum H, Reichenbach M, Wolf E, Steger K, Dansranjavin T, Schagdarsurengin U (2014) Uniformity of nucleosome preservation pattern in mammalian sperm and its connection to repetitive DNA elements. Dev Cell 30(1):23–35. doi:10.1016/j.devcel.2014.05.023
Gannon JR, Emery BR, Jenkins TG, Carrell DT (2014) The sperm epigenome: implications for the embryo. Adv Exp Med Biol 791:53–66. doi:10.1007/978-1-4614-7783-9_4
Brunner AM, Nanni P, Mansuy IM (2014) Epigenetic marking of sperm by post-translational modification of histones and protamines. Epigenetics Chromatin 7(1):2. doi:10.1186/1756-8935-7-2
Arpanahi A, Brinkworth M, Iles D, Krawetz SA, Paradowska A, Platts AE, Saida M, Steger K, Tedder P, Miller D (2009) Endonuclease-sensitive regions of human spermatozoal chromatin are highly enriched in promoter and CTCF binding sequences. Genome Res 19(8):1338–1349. doi:10.1101/gr.094953.109
Carone BR, Hung JH, Hainer SJ, Chou MT, Carone DM, Weng Z, Fazzio TG, Rando OJ (2014) High-resolution mapping of chromatin packaging in mouse embryonic stem cells and sperm. Dev Cell 30(1):11–22. doi:10.1016/j.devcel.2014.05.024
Waterland RA, Jirtle RL (2003) Transposable elements: targets for early nutritional effects on epigenetic gene regulation. Mol Cell Biol 23(15):5293–5300
Wolff GL, Kodell RL, Moore SR, Cooney CA (1998) Maternal epigenetics and methyl supplements affect agouti gene expression in Avy/a mice. FASEB J 12(11):949–957
Lambrot R, Xu C, Saint-Phar S, Chountalos G, Cohen T, Paquet M, Suderman M, Hallett M, Kimmins S (2013) Low paternal dietary folate alters the mouse sperm epigenome and is associated with negative pregnancy outcomes. Nat Commun 4:2889. doi:10.1038/ncomms3889
Stuppia L, Franzago M, Ballerini P, Gatta V, Antonucci I (2015) Epigenetics and male reproduction: the consequences of paternal lifestyle on fertility, embryo development, and children lifetime health. Clin Epigenetics 7:120. doi:10.1186/s13148-015-0155-4
Soubry A, Hoyo C, Jirtle RL, Murphy SK (2014) A paternal environmental legacy: evidence for epigenetic inheritance through the male germ line. Bioessays 36(4):359–371. doi:10.1002/bies.201300113
Wu H, Hauser R, Krawetz SA, Pilsner JR (2015) Environmental susceptibility of the sperm epigenome during windows of male germ cell development. Curr Environ Health Rep 2(4):356–366. doi:10.1007/s40572-015-0067-7
Oakes CC, La Salle S, Smiraglia DJ, Robaire B, Trasler JM (2007) Developmental acquisition of genome-wide DNA methylation occurs prior to meiosis in male germ cells. Dev Biol 307(2):368–379. doi:10.1016/j.ydbio.2007.05.002
Oakes CC, La Salle S, Smiraglia DJ, Robaire B, Trasler JM (2007) A unique configuration of genome-wide DNA methylation patterns in the testis. Proc Natl Acad Sci U S A 104(1):228–233. doi:10.1073/pnas.0607521104
Ni K, Spiess AN, Schuppe HC, Steger K (2016) The impact of sperm protamine deficiency and sperm DNA damage on human male fertility: a systematic review and meta-analysis. Andrology. doi:10.1111/andr.12216
Juul A, Almstrup K, Andersson AM, Jensen TK, Jorgensen N, Main KM, Rajpert-De Meyts E, Toppari J, Skakkebaek NE (2014) Possible fetal determinants of male infertility. Nat Rev Endocrinol 10(9):553–562. doi:10.1038/nrendo.2014.97
Skakkebaek NE, Rajpert-De Meyts E, Buck Louis GM, Toppari J, Andersson AM, Eisenberg ML, Jensen TK, Jorgensen N, Swan SH, Sapra KJ, Ziebe S, Priskorn L, Juul A (2016) Male reproductive disorders and fertility trends: influences of environment and genetic susceptibility. Physiol Rev 96(1):55–97. doi:10.1152/physrev.00017.2015
Sweeney MF, Hasan N, Soto AM, Sonnenschein C (2015) Environmental endocrine disruptors: effects on the human male reproductive system. Rev Endocr Metab Disord 16(4):341–357. doi:10.1007/s11154-016-9337-4
Dupont C, Cordier AG, Junien C, Mandon-Pepin B, Levy R, Chavatte-Palmer P (2012) Maternal environment and the reproductive function of the offspring. Theriogenology 78(7):1405–1414. doi:10.1016/j.theriogenology.2012.06.016
Anway MD, Leathers C, Skinner MK (2006) Endocrine disruptor vinclozolin induced epigenetic transgenerational adult-onset disease. Endocrinology 147(12):5515–5523. doi:10.1210/en.2006-0640
Howdeshell KL, Furr J, Lambright CR, Rider CV, Wilson VS, Gray LE Jr (2007) Cumulative effects of dibutyl phthalate and diethylhexyl phthalate on male rat reproductive tract development: altered fetal steroid hormones and genes. Toxicol Sci 99(1):190–202. doi:10.1093/toxsci/kfm069
Hutchison GR, Sharpe RM, Mahood IK, Jobling M, Walker M, McKinnell C, Mason JI, Scott HM (2008) The origins and time of appearance of focal testicular dysgenesis in an animal model of testicular dysgenesis syndrome: evidence for delayed testis development? Int J Androl 31(2):103–111. doi:10.1111/j.1365-2605.2007.00816.x
Kim TS, Jung KK, Kim SS, Kang IH, Baek JH, Nam HS, Hong SK, Lee BM, Hong JT, Oh KW, Kim HS, Han SY, Kang TS (2010) Effects of in utero exposure to DI(n-Butyl) phthalate on development of male reproductive tracts in Sprague-Dawley rats. J Toxicol Environ Health A 73(21–22):1544–1559. doi:10.1080/15287394.2010.511579
Klinefelter GR, Laskey JW, Winnik WM, Suarez JD, Roberts NL, Strader LF, Riffle BW, Veeramachaneni DN (2012) Novel molecular targets associated with testicular dysgenesis induced by gestational exposure to diethylhexyl phthalate in the rat: a role for estradiol. Reproduction 144(6):747–761. doi:10.1530/REP-12-0266
Manikkam M, Tracey R, Guerrero-Bosagna C, Skinner MK (2013) Plastics derived endocrine disruptors (BPA, DEHP and DBP) induce epigenetic transgenerational inheritance of obesity, reproductive disease and sperm epimutations. PLoS One 8(1):e55387. doi:10.1371/journal.pone.0055387
Abdel-Maksoud FM, Leasor KR, Butzen K, Braden TD, Akingbemi BT (2015) Prenatal exposures of male rats to the environmental chemicals bisphenol a and Di(2-ethylhexyl) phthalate impact the sexual differentiation process. Endocrinology 156(12):4672–4683. doi:10.1210/en.2015-1077
Kalb AC, Kalb AL, Cardoso TF, Fernandes CG, Corcini CD, Junior AS, Martinez PE (2016) Maternal transfer of bisphenol a during nursing causes sperm impairment in male offspring. Arch Environ Contam Toxicol 70(4):793–801. doi:10.1007/s00244-015-0199-7
Small CM, DeCaro JJ, Terrell ML, Dominguez C, Cameron LL, Wirth J, Marcus M (2009) Maternal exposure to a brominated flame retardant and genitourinary conditions in male offspring. Environ Health Perspect 117(7):1175–1179. doi:10.1289/ehp.0800058
Jensen MS, Anand-Ivell R, Norgaard-Pedersen B, Jonsson BA, Bonde JP, Hougaard DM, Cohen A, Lindh CH, Ivell R, Toft G (2015) Amniotic fluid phthalate levels and male fetal gonad function. Epidemiology 26(1):91–99. doi:10.1097/EDE.0000000000000198
Gaspari L, Paris F, Jandel C, Kalfa N, Orsini M, Daures JP, Sultan C (2011) Prenatal environmental risk factors for genital malformations in a population of 1442 French male newborns: a nested case-control study. Hum Reprod 26(11):3155–3162. doi:10.1093/humrep/der283
Gabel P, Jensen MS, Andersen HR, Baelum J, Thulstrup AM, Bonde JP, Toft G (2011) The risk of cryptorchidism among sons of women working in horticulture in Denmark: a cohort study. Environ Health 10:100. doi:10.1186/1476-069X-10-100
Trabert B, Longnecker MP, Brock JW, Klebanoff MA, McGlynn KA (2012) Maternal pregnancy levels of trans-nonachlor and oxychlordane and prevalence of cryptorchidism and hypospadias in boys. Environ Health Perspect 120(3):478–482. doi:10.1289/ehp.1103936
Manikkam M, Tracey R, Guerrero-Bosagna C, Skinner MK (2012) Pesticide and insect repellent mixture (permethrin and DEET) induces epigenetic transgenerational inheritance of disease and sperm epimutations. Reprod Toxicol 34(4):708–719. doi:10.1016/j.reprotox.2012.08.010
Ohsako S, Fukuzawa N, Ishimura R, Kawakami T, Wu Q, Nagano R, Zaha H, Sone H, Yonemoto J, Tohyama C (2010) Comparative contribution of the aryl hydrocarbon receptor gene to perinatal stage development and dioxin-induced toxicity between the urogenital complex and testis in the mouse. Biol Reprod 82(3):636–643. doi:10.1095/biolreprod.109.080812
Zhang L, Dong L, Ding S, Qiao P, Wang C, Zhang M, Zhang L, Du Q, Li Y, Tang N, Chang B (2014) Effects of n-butylparaben on steroidogenesis and spermatogenesis through changed E(2) levels in male rat offspring. Environ Toxicol Pharmacol 37(2):705–717. doi:10.1016/j.etap.2014.01.016
Strandberg-Larsen K, Jensen MS, Ramlau-Hansen CH, Gronbaek M, Olsen J (2009) Alcohol binge drinking during pregnancy and cryptorchidism. Hum Reprod 24(12):3211–3219. doi:10.1093/humrep/dep325
Ramlau-Hansen CH, Toft G, Jensen MS, Strandberg-Larsen K, Hansen ML, Olsen J (2010) Maternal alcohol consumption during pregnancy and semen quality in the male offspring: two decades of follow-up. Hum Reprod 25(9):2340–2345. doi:10.1093/humrep/deq140
Virtanen HE, Sadov S, Toppari J (2012) Prenatal exposure to smoking and male reproductive health. Curr Opin Endocrinol Diabetes Obes 19(3):228–232. doi:10.1097/MED.0b013e3283537cb8
Sobinoff AP, Sutherland JM, Beckett EL, Stanger SJ, Johnson R, Jarnicki AG, McCluskey A, St John JC, Hansbro PM, McLaughlin EA (2014) Damaging legacy: maternal cigarette smoking has long-term consequences for male offspring fertility. Hum Reprod 29(12):2719–2735. doi:10.1093/humrep/deu235
Palmer JR, Herbst AL, Noller KL, Boggs DA, Troisi R, Titus-Ernstoff L, Hatch EE, Wise LA, Strohsnitter WC, Hoover RN (2009) Urogenital abnormalities in men exposed to diethylstilbestrol in utero: a cohort study. Environ Health 8:37. doi:10.1186/1476-069X-8-37
Kristensen DM, Hass U, Lesne L, Lottrup G, Jacobsen PR, Desdoits-Lethimonier C, Boberg J, Petersen JH, Toppari J, Jensen TK, Brunak S, Skakkebaek NE, Nellemann C, Main KM, Jegou B, Leffers H (2011) Intrauterine exposure to mild analgesics is a risk factor for development of male reproductive disorders in human and rat. Hum Reprod 26(1):235–244. doi:10.1093/humrep/deq323
Comish PB, Drumond AL, Kinnell HL, Anderson RA, Matin A, Meistrich ML, Shetty G (2014) Fetal cyclophosphamide exposure induces testicular cancer and reduced spermatogenesis and ovarian follicle numbers in mice. PLoS One 9(4):e93311. doi:10.1371/journal.pone.0093311
Dean A, Mungall W, McKinnell C, Sharpe RM (2013) Prostaglandins, masculinization and its disorders: effects of fetal exposure of the rat to the cyclooxygenase inhibitor- indomethacin. PLoS One 8(5):e62556. doi:10.1371/journal.pone.0062556
Pedrana G, Viotti H, Lombide P, Sanguinetti G, Pino C, Cavestany D, Sloboda DM, Martin GB (2016) In utero betamethasone affects 3beta-hydroxysteroid dehydrogenase and inhibin-alpha immunoexpression during testis development. J Dev Orig Health Dis:1–8. doi:10.1017/S2040174416000118
Tertti K, Toppari J, Virtanen HE, Sadov S, Ronnemaa T (2016) Metformin treatment does not affect testicular size in offspring born to mothers with gestational diabetes. Rev Diabet Stud. doi:10.1900/RDS.2015.12.e2015013
Yamada K, Maeda N, Noguchi J, Yamada H, Morinaga E, Yatake H, Yamamoto Y, Tadokoro T, Kawata T (2013) Influences of maternal B12 and methionine intake during gestation and lactation on testicular development of offspring in rats. J Nutr Sci Vitaminol (Tokyo) 59(3):238–242
Recabarren MP, Rojas-Garcia PP, Einspanier R, Padmanabhan V, Sir-Petermann T, Recabarren SE (2013) Pituitary and testis responsiveness of young male sheep exposed to testosterone excess during fetal development. Reproduction 145(6):567–576. doi:10.1530/REP-13-0006
WHO (2010) WHO laboratory manual for the examination and processing of human semen, vol 5th edition
Wagenlehner F, Pilatz A, Linn T, Diemer T, Schuppe HC, Schagdarsurengin U, Hossain H, Meinhardt A, Ellem S, Risbridger G, Weidner W (2013) Prostatitis and andrological implications. Minerva Urol Nefrol 65(2):117–123
Pilatz A, Hossain H, Kaiser R, Mankertz A, Schuttler CG, Domann E, Schuppe HC, Chakraborty T, Weidner W, Wagenlehner F (2015) Acute epididymitis revisited: impact of molecular diagnostics on etiology and contemporary guideline recommendations. Eur Urol 68(3):428–435. doi:10.1016/j.eururo.2014.12.005
Rusz A, Pilatz A, Wagenlehner F, Linn T, Diemer T, Schuppe HC, Lohmeyer J, Hossain H, Weidner W (2012) Influence of urogenital infections and inflammation on semen quality and male fertility. World J Urol 30(1):23–30. doi:10.1007/s00345-011-0726-8
Pilatz A, Ceylan I, Schuppe HC, Ludwig M, Fijak M, Chakraborty T, Weidner W, Bergmann M, Wagenlehner F (2015) Experimental Escherichia coli epididymitis in rats: assessment of testicular involvement in a long-term follow-up. Andrologia 47(2):160–167. doi:10.1111/and.12239
Krieger JN (1984) Epididymitis, orchitis, and related conditions. Sex Transm Dis 11(3):173–181
Emerson C, Dinsmore WW, Quah SP (2007) Are we missing mumps epididymo-orchitis? Int J STD AIDS 18(5):341–342. doi:10.1258/095646207780749754
Eickhoff JH, Frimodt-Moller N, Walter S, Frimodt-Moller C (1999) A double-blind, randomized, controlled multicentre study to compare the efficacy of ciprofloxacin with pivampicillin as oral therapy for epididymitis in men over 40 years of age. BJU Int 84(7):827–834
Lang T, Dechant M, Sanchez V, Wistuba J, Boiani M, Pilatz A, Stammler A, Middendorff R, Schuler G, Bhushan S, Tchatalbachev S, Wubbeling F, Burger M, Chakraborty T, Mallidis C, Meinhardt A (2013) Structural and functional integrity of spermatozoa is compromised as a consequence of acute uropathogenic E. coli-associated epididymitis. Biol Reprod 89(3):59. doi:10.1095/biolreprod.113.110379
Hoppner W, Strohmeyer T, Hartmann M, Lopez-Gamarra D, Dreikorn K (1992) Surgical treatment of acute epididymitis and its underlying diseases. Eur Urol 22(3):218–221
Lu Y, Bhushan S, Tchatalbachev S, Marconi M, Bergmann M, Weidner W, Chakraborty T, Meinhardt A (2013) Necrosis is the dominant cell death pathway in uropathogenic Escherichia coli elicited epididymo-orchitis and is responsible for damage of rat testis. PLoS One 8(1):e52919. doi:10.1371/journal.pone.0052919
Fraczek M, Kurpisz M (2015) Mechanisms of the harmful effects of bacterial semen infection on ejaculated human spermatozoa: potential inflammatory markers in semen. Folia Histochem Cytobiol 53(3):201–217. doi:10.5603/fhc.a2015.0019
Piasecka M, Fraczek M, Gaczarzewicz D, Gill K, Szumala-Kakol A, Kazienko A, Laszczynska M, Lenart S, Beutin L, Kurpisz M (2014) Novel morphological findings of human sperm removal by leukocytes in in vivo and in vitro conditions: preliminary study. Am J Reprod Immunol 72(4):348–358. doi:10.1111/aji.12284
Diemer T, Weidner W, Michelmann HW, Schiefer HG, Rovan E, Mayer F (1996) Influence of Escherichia coli on motility parameters of human spermatozoa in vitro. Int J Androl 19(5):271–277
Florman HM, Jungnickel MK, Sutton KA (2008) Regulating the acrosome reaction. Int J Dev Biol 52(5–6):503–510. doi:10.1387/ijdb.082696hf
Hilbert DW, Paulish-Miller TE, Tan CK, Carey AJ, Ulett GC, Mordechai E, Adelson ME, Gygax SE, Trama JP (2012) Clinical Escherichia coli isolates utilize alpha-hemolysin to inhibit in vitro epithelial cytokine production. Microbes infect Inst Pasteur 14(7–8):628–638. doi:10.1016/j.micinf.2012.01.010
Stanley P, Koronakis V, Hughes C (1998) Acylation of Escherichia coli hemolysin: a unique protein lipidation mechanism underlying toxin function. Microbiol Mol Biol Rev 62(2):309–333
Speyer BE, Pizzey AR, Ranieri M, Joshi R, Delhanty JD, Serhal P (2010) Fall in implantation rates following ICSI with sperm with high DNA fragmentation. Hum Reprod 25(7):1609–1618. doi:10.1093/humrep/deq116
Robinson L, Gallos ID, Conner SJ, Rajkhowa M, Miller D, Lewis S, Kirkman-Brown J, Coomarasamy A (2012) The effect of sperm DNA fragmentation on miscarriage rates: a systematic review and meta-analysis. Hum Reprod 27(10):2908–2917. doi:10.1093/humrep/des261
Aitken J, Fisher H (1994) Reactive oxygen species generation and human spermatozoa: the balance of benefit and risk. Bioessays 16(4):259–267. doi:10.1002/bies.950160409
Sanchez V, Redmann K, Wistuba J, Wubbeling F, Burger M, Oldenhof H, Wolkers WF, Kliesch S, Schlatt S, Mallidis C (2012) Oxidative DNA damage in human sperm can be detected by Raman microspectroscopy. Fertil Steril 98(5):1124–1129 e1121-1123. doi:10.1016/j.fertnstert.2012.07.1059
De Iuliis GN, Thomson LK, Mitchell LA, Finnie JM, Koppers AJ, Hedges A, Nixon B, Aitken RJ (2009) DNA damage in human spermatozoa is highly correlated with the efficiency of chromatin remodeling and the formation of 8-hydroxy-2′-deoxyguanosine, a marker of oxidative stress. Biol Reprod 81(3):517–524. doi:10.1095/biolreprod.109.076836
Allam JP, Fronhoffs F, Fathy A, Novak N, Oltermann I, Bieber T, Schuppe HC, Haidl G (2008) High percentage of apoptotic spermatozoa in ejaculates from men with chronic genital tract inflammation. Andrologia 40(5):329–334. doi:10.1111/j.1439-0272.2008.00864.x
Schuppe HC, Meinhardt A, Allam JP, Bergmann M, Weidner W, Haidl G (2008) Chronic orchitis: a neglected cause of male infertility? Andrologia 40(2):84–91
La Vignera S, Condorelli RA, Vicari E, D’Agata R, Calogero AE (2012) Sperm DNA damage in patients with chronic viral C hepatitis. Eur J Intern Med 23(1):e19–e24. doi:10.1016/j.ejim.2011.08.011
Ochsendorf FR (1999) Infections in the male genital tract and reactive oxygen species. Hum Reprod Update 5(5):399–420
Henkel R, Maass G, Hajimohammad M, Menkveld R, Stalf T, Villegas J, Sanchez R, Kruger TF, Schill WB (2003) Urogenital inflammation: changes of leucocytes and ROS. Andrologia 35(5):309–313
Weidner W, Krause W, Ludwig M (1999) Relevance of male accessory gland infection for subsequent fertility with special focus on prostatitis. Hum Reprod Update 5(5):421–432
Fraczek M, Szumala-Kakol A, Dworacki G, Sanocka D, Kurpisz M (2013) In vitro reconstruction of inflammatory reaction in human semen: effect on sperm DNA fragmentation. J Reprod Immunol 100(1):76–85
Koppers AJ, Mitchell LA, Wang P, Lin M, Aitken RJ (2011) Phosphoinositide 3-kinase signalling pathway involvement in a truncated apoptotic cascade associated with motility loss and oxidative DNA damage in human spermatozoa. Biochem J 436(3):687–698. doi:10.1042/BJ20110114
Aitken RJ, Curry BJ (2011) Redox regulation of human sperm function: from the physiological control of sperm capacitation to the etiology of infertility and DNA damage in the germ line. Antioxid Redox Signal 14(3):367–381. doi:10.1089/ars.2010.3186
Barratt CL, Aitken RJ, Bjorndahl L, Carrell DT, de Boer P, Kvist U, Lewis SE, Perreault SD, Perry MJ, Ramos L, Robaire B, Ward S, Zini A (2010) Sperm DNA: organization, protection and vulnerability: from basic science to clinical applications—a position report. Hum Reprod 25(4):824–838. doi:10.1093/humrep/dep465
Xu DX, Shen HM, Zhu QX, Chua L, Wang QN, Chia SE, Ong CN (2003) The associations among semen quality, oxidative DNA damage in human spermatozoa and concentrations of cadmium, lead and selenium in seminal plasma. Mutat Res 534(1–2):155–163
Xu DX, Zhu QX, Zheng LK, Wang QN, Shen HM, Deng LX, Ong CN (2003) Exposure to acrylonitrile induced DNA strand breakage and sex chromosome aneuploidy in human spermatozoa. Mutat Res 537(1):93–100
Zhang Z, Wang M, Eisel F, Tchatalbachev S, Chakraborty T, Meinhardt A, Bhushan S (2016) Uropathogenic Escherichia coli epigenetically manipulate host cell death pathways. J Infect Dis 213(7):1198–1207. doi:10.1093/infdis/jiv569
Acknowledgments
The authors acknowledge the financial support of the Deutsche Forschungsgemeinschaft (KFO 181; GRK 1871; SCHA1531/2-1), the State of Hesse Landesoffensive zur Förderung der wissenschaftlichen Exzellenz (LOEWE) on ‘Male infertility due to infection and inflammation’ (MIBIE), National Health and Medical Research Council grants GNT1043939 and GNT1051223, and the Victorian Government’s Operational Infrastructure Support Program, Australia.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is a contribution to the special issue on Fetomaternal Cross Talk and Its Effect on Pregnancy Maintenance, Maternal and Offspring Health - Guest Editor: Petra Arck
Rights and permissions
About this article
Cite this article
Schagdarsurengin, U., Western, P., Steger, K. et al. Developmental origins of male subfertility: role of infection, inflammation, and environmental factors. Semin Immunopathol 38, 765–781 (2016). https://doi.org/10.1007/s00281-016-0576-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00281-016-0576-y