Abstract
Dystonia is a movement disorder characterized by involuntary muscle contractions resulting in abnormal postures. Although common in the clinic, the etiology of dystonia remains unclear. Most dystonias are idiopathic and are not associated with clear pathological brain abnormalities. Attempts to genetically model these dystonias in rodents have failed to replicate dystonic symptoms. This is at odds with the fact that rodents can exhibit dystonia. Because of this discrepancy, it is necessary to consider alternative approaches to generate phenotypically and genotypically faithful models of dystonia. Conditional knockout of dystonia-related genes is 1 technique that may prove useful for modeling genetic dystonias. Lentiviral-mediated small or short hairpin RNA (shRNA) knockdown of particular genes is another approach. Finally, in cases in which the function of a dystonia-related gene is well-known, pharmacological blockade of the protein product can be used. Such an approach was successfully implemented in the case of rapid-onset dystonia parkinsonism, DYT12. This (DYT12) is a hereditary dystonia caused by mutations in the α3 isoform of the sodium potassium adenosine triphosphatase (ATPase) pump (sodium pump), which partially hampers its physiological function. It was found that partial selective pharmacological block of the sodium pumps in the cerebellum and basal ganglia of mice recapitulates all of the salient features of DYT12, including dystonia and parkinsonism induced by stress. This DYT12 model is unique in that it faithfully replicates human symptoms of DYT12, while targeting the genetic cause of this disorder. Acute disruption of proteins implicated in dystonia may prove a generally fruitful method to model dystonia in rodents.
Similar content being viewed by others
The Neurological Basis of Dystonia
Dystonia is the third most common movement disorder trailing only Parkinson’s disease and essential tremor [1]. It is characterized by involuntary and prolonged co-contraction of agonist–antagonist muscle pairs, often causing patients to adopt twisting postures [2]. As with many movement disorders, dystonia is extremely debilitating and can dramatically impact the quality of life of patients [3]. Despite its widespread occurrence, the neural mechanism underlying dystonia is poorly understood.
Clues from Secondary Dystonias
Much of the insight into the origins of dystonia has come from patients with secondary dystonias, in which the pathology in specific brain regions can be identified [4]. Case studies have demonstrated that structural lesions to the basal ganglia and particularly the striatum caused by tumor, stroke, hemorrhage, or trauma can be associated with the onset of dystonia [5–7]. Degenerative disorders preferentially affecting the basal ganglia, such as early-onset Huntington’s disease and the syndromes of neurodegeneration with brain iron accumulation, often have dystonia as a prominent symptom [8–11]. From these findings it is clear that insult to the basal ganglia can result in dystonia. However, lesions in other brain areas have also been associated with dystonia [4]. Regions as diverse as the thalamus, the parietal cortex, and the brainstem have been implicated in a few cases of secondary dystonia [12]. Another region implicated in some secondary dystonias that has received increasing attention in recent years is the cerebellum [13, 14]. Historically there are numerous case reports linking cerebellar insult with dystonic symptoms [15–18] and recent studies corroborate association of dystonic symptoms with cerebellar injury [19–22].
Clues from Imaging Studies
Imaging and neurophysiological studies in patients with dystonia have revealed a number of abnormalities throughout the motor circuits of the brain [23–25]. Importantly, both the cerebellum and basal ganglia routinely exhibit abnormal function [26]. For example, in patients with DYT1 genetic dystonia, abnormal activity has been recorded in the nuclei of the basal ganglia [27]. In the same disorder, positron emission tomography indicates that the cerebellum has increased metabolic activity [28], and diffusion tensor imaging studies demonstrate altered anatomical connectivity of the cerebellar output pathways [29]. A shortcoming of these studies is that while they attempt to delineate which brain areas have altered activity or connectivity in the dystonic condition, they do not distinguish causal changes from compensatory ones.
Clues from Surgical Interventions
Experimental neurosurgical interventions on dystonia patients refractory to other forms of treatment have provided insight into how dystonic symptoms can be alleviated in some patients. Deep brain stimulation of 1 of the output nuclei of the basal ganglia, the globus pallidus internus, can alleviate symptoms in a variety of dystonia patients, and it is currently the most common and well-studied site of surgical intervention [30–33]. Although this intervention can be quite successful, it is clear that some patient populations respond better than others, possibly reflecting underlying differences in the neural basis of dystonia generation between these populations [34]. It is historically noteworthy that the intervention at a number of sites throughout the brain has been attempted to treat dystonia. Two notable sites explored are the thalamus and cerebellum. Early studies demonstrated that stimulations or lesions of specific thalamic nuclei could alleviate dystonia in some patients [35–38]. In a few patients, surgical lesion of the dentate output nucleus of the cerebellum was also shown to alleviate dystonia [16–18, 39–42] suggesting the involvement of this structure in the generation of some dystonia. However, a major caveat of these early surgical interventions is that the results were simply reported as case studies without the scientific rigor to allow unbiased evaluation of their efficacy. As a consequence the efficacies of these interventions in alleviating dystonia have been questioned, and even though there are no studies that actually refute their value, they are now rarely used.
Idiopathic Dystonias
Despite the clues obtained from secondary dystonias and surgical interventions regarding the brain regions affected in dystonia, the most common dystonias seen in the clinic are not secondary, and it remains unclear which of these brain areas play a causative role in a typical dystonic patient. Indeed most dystonias are idiopathic and show no clear or consistent pathological aberrations of the brain [2, 43–45]. Many common dystonias have been linked to mutations in 1 of at least 18 genetic loci [2, 46–48]. These mutations are responsible for disorders encompassing pure dystonias in which the patients exhibit no other symptoms, and dystonia-plus syndromes in which dystonia is part of a constellation of neurological findings. Therefore, although many regions of abnormality have been identified in idiopathic dystonias, studies have failed to identify a consistent pathophysiological mechanism for dystonia induction. Moreover, in these patient groups, the efficacy of common neurosurgical interventions also varies, suggesting that different dystonias may have distinct mechanisms of disease induction. To offer these patients effective therapy, clearly it is necessary to identify the causes of the disease and the brain regions affected. Given the limited insights that are attainable from patient studies alone, appropriate animal models of these disorders are vital to understanding the mechanism by which dystonia is generated in these conditions.
Rodent Models of Dystonia
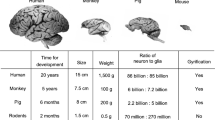
Despite the identification of genes underlying many dystonias, the most common genetic manipulations (i.e, namely knockout of the suspected gene, knock-in of mutated versions of the causative human gene, and transgenics overexpressing the mutated human gene) have failed to recapitulate dystonia in rodents [49–51]. This is surprising because it is clear that rodents can exhibit dystonia, and in fact multiple strains of rodents suffer from dystonia due to spontaneous genetic mutations [52–55].
The reason why transgenic generation of genotypic models of human dystonia that replicate phenotypic symptoms has failed is unclear. One theory is that the late onset of some dystonias requires years of aberrant neuronal function, and because mice have a limited lifespan, neurons never become dysfunctional enough to produce dystonia [56]. Some genetic dystonias have an autosomal dominant inheritance pattern, and these disorders may be due to a gain of pathological function in the mutated gene. If this is the case, the mutated protein may function differently in humans and mice, explaining the phenotype difference between these 2 species. Another possibility is that rodents have different compensatory mechanisms from humans in response to loss of a particular protein. For example the loss may be lethal in rodents, but cause dystonia in humans. Conversely, rodents may be more capable of compensating, and therefore loss of the protein may manifest as a lesser dysfunction compared to humans. Because the present genetic dystonia rodent models that have been generated are knock-ins, knockouts, or transgenics; the disrupted gene is present from conception [48, 57–59]. Embryonic alterations in gene expression may be able to compensate for the loss of gene in mice, but not in humans.
Despite the shortcomings of the current genetic models of dystonia, they have in some cases demonstrated that loss or mutation of a particular dystonia gene can alter the function of neurons and connectivity of brain regions [29, 44, 50, 60–63]. Whether or not these dysfunctions are compensatory or causal in nature remains to be established. For example, abnormalities in the cerebello-thalamo-cortical pathway have been identified in dystonic patients and also in transgenic mice with the identical mutated gene [29, 64]. However, the same changes are also seen in nonmanifesting human carriers [29], suggesting that this change is not, on its own, sufficient to cause dystonia and may be related to compensation. In general, the role of these identified functional changes in causing dystonia is unclear and will remain so until there are phenotypically and genotypically faithful rodent models of dystonia.
Alternative Approaches for the Generation of Rodent Models of Dystonia
Because current genetic mouse models of dystonia are not symptomatically dystonic, it is necessary to consider alternative methods to generate models that both target genes directly implicated in human dystonias and replicate dystonia.
Given that compensation in rodents may be a concern, the cre-lox and creER-lox systems combined with tamoxifen induction protocols can be used to control the regional and temporal expression of genes of interest [65–67]. The creER-lox system can be used to systematically dissect whether loss of a protein in a particular brain region or neuronal population at a specific point of time in the life of the animal can result in dystonia. Furthermore, if a specific mutation is suspected to produce a gain-of-function, it may be beneficial to overexpress the mutated protein in select cell populations or at specific time points.
The implementation of these molecular techniques is likely to be informative. However, these approaches are not without limitations. For example, although cre-lox systems can be used to target precise regions or populations of cells, the targeted tissue-specific promoter may not be as specific [28]. Also, recent studies suggest that for a single dose of tamoxifen, recombination efficiency can vary, and therefore different animals with the same treatment may have a different number of cells in which the flanked gene is removed [68]. Because of these complications, it is useful to consider other tools that can be used in parallel with these.
Stereotaxic injection of lentiviruses or adeno-associated viruses containing small or short hairpin RNA (shRNA) against dystonia-related genes into specific brain areas is another method that can be used to acutely induce gene knockdown [69, 70]. Recent advances have used viruses to routinely deliver constructs to cells. These viruses deliver genomic elements, such as shRNA, to a small population of cells near the injection site. ShRNA mediates knockdown of the protein of interest via RNA interference. This technique allows acute knockdown of a particular protein in small subregions without the risk of knockdown in distant areas [71]. Expression can be further limited to specific cells in a given region by combining lentivirus and cre-lox systems or by altering the promoter of the shRNA [72, 73]. For example, by injecting a virus with shRNA containing a premature stop codon that is floxed into Cre-CaMKIIα mice, a neuron specific knockdown can be achieved [74].
Although lentiviral-mediated knockdown of genes is a powerful technique for acute regional knockdown of dystonia-related genes, it is an inherently biased approach because the investigator needs to make an a priori decision on regions of interest. Depending on the goals of the study, this may be acceptable. For example, secondary dystonias have suggested specific brain regions whose dysfunction may be associated with dystonia. Nonetheless, it is very important to be aware of this bias, and to explore the impact of genetic knockdown of the protein of interest in other brain regions. Another concern with this technique is that shRNA generates a knockdown in the expression of a particular gene rather than its complete knockout [39]. This can be useful if mutations in a dystonia gene are believed to diminish but not ablate function [75]. However, other genes may require complete knockout to generate dystonic symptoms. A final caveat is that the time course of shRNA mediated knockdown is partially determined by the turnover time of the protein of interest. For example, it will take longer to knockdown proteins which turnover infrequently and only require rare replacement than to knockdown those that are constantly and rapidly replaced. Even though initiation of knockdown may take some time, lentiviral and adenoviral-mediated genetic knock-in or knockdown can continue for more than 6 months [76].
If the gene associated with a particular dystonia has a protein product that is well understood, pharmacologically inhibiting the protein by stereotaxically injecting the blocker into select brain regions may be a suitable alternative approach to genetic knockdown for modeling dystonia in rodents. This technique may also require a priori selection of infusion sites, and as such it is also a biased approach. Unfortunately, some of the most common dystonia genes code for proteins that function in a variety of processes important for cell signaling, stability, and maintenance [48, 77–80]. In these cases, finding a compound that inhibits a specific function of the protein of interest is likely to be difficult or even impossible. Furthermore, in these dystonias, it is unclear which function of the protein is most relevant to dystonia. There are only a small number of dystonia genes that code for proteins with a specific and well-studied function. Nonetheless, such dystonias exist with rapid-onset dystonia Parkinsonism, DYT12, being a prime example.
DYT12 is a dystonia-plus syndrome caused by mutations in the α3 isoform of the sodium potassium ATPase (sodium pump), which render the protein partially dysfunctional [75]. The sodium pump is a transporter whose function in maintaining cellular ionic gradients has been known for nearly 50 years [81]. Further, the affinity and mechanism of action of a selective inhibitor of the sodium pump (ouabain) has been well worked out [82, 83]. Therefore, DYT12 is an ideal candidate for generation of a pharmacologic animal model in rodents.
Rapid Onset Dystonia Parkinsonism (DYT12)
Rapid onset dystonia parkinsonism was first described in 1993 [84]. The disorder has since been found in at least 21 families throughout the world [85]. DYT12 is characterized by a normal or near-normal childhood with the onset of severe dystonia and parkinsonism after a stressful event [84]. The triggers are variable and include head trauma, childbirth, and prolonged exposure to heat or exercise [85]. However, even severe emotional stress can bring on symptoms [86]. Importantly, once DYT12 patients become symptomatic, their disability persists and patients largely do not recover function with time [85]. In 2004, the causative gene in DYT12 was identified as ATP1A3, which codes for the α3 isoform of the sodium pump [75]. The sodium pump is well-known as a homeostatic pump that uses ATP to power the exchange of 3 sodium ions out of the cell for the entry of 2 potassium ions, thus maintaining proper ionic gradients in all cells. The alpha isoform is the catalytic subunit of the pump [87]. Although the sodium pump is expressed ubiquitously, the α3 isoform is specifically expressed at high levels in some neurons [88]. Research into the mutations of ATP1A3 causing DYT12 suggest that in this disorder, pumps with the α3 isoform exhibit decreased stability and hindered function [75].
Identification of the causative gene inspired a number of groups to generate genetic knockouts of ATP1A3 in the rodent to model DYT12. Unfortunately, mice homozygous for the ATP1A3 knockout are neonatal lethal and mice heterozygous for ATP1A3 show no dystonia [51, 89].
A Pharmacological Model of DYT12
Transgenic mouse models of DYT12 have failed to replicate symptoms seen in the human disorder. However, studies of the mutations seen in patients with DYT12 have revealed a partial loss of function of sodium pumps containing the α3 isoform [75]. Therefore, if an acute and incomplete inhibition of sodium pumps containing the α3 isoform could be achieved, it may replicate what is seen in humans with the disorder. It has been known for decades that ouabain binds to the alpha subunit of the sodium pump and selectively inhibits its function [90]. Although ouabain can affect all sodium pump isoforms, it has especially high affinities for the α3 and α2 isoforms [91, 92]. Interestingly, neurons express primarily the α1 and α3 isoforms, and therefore, application of low concentrations of ouabain selectively inhibit the α3 sodium pump in neurons [93]. Therefore, it is possible to target α3 containing sodium pumps in neurons using infusion of low concentrations of ouabain.
In 2011, Calderon et al. [94] hypothesized that the failure of genetic models of DYT12 to reproduce dystonia is due to compensation and that acute partial inhibition of α3 sodium pump function in the adult mouse using ouabain will recapitulate dystonic symptoms. Initially, they infused ouabain into gross brain regions that were believed to be involved in dystonia, including basal ganglia, motor cortex, thalamus, and cerebellum. This was accomplished by implanting subcutaneous pumps that chronically infuse low concentrations of ouabain into specific regions through stereotaxically implanted cannula for several days. Fluorescently tagged ouabain and postmortem quantitative microscopy was used to estimate the extent of diffusion and ensure that the application of ouabain was limited to the sites of interest.
The group first focused on the basal ganglia because, as discussed, it has been routinely implicated in human dystonia. Infusion of ouabain to the basal ganglia resulted in a dose- and time-dependent induction of parkinsonism-like symptoms, but not dystonia. The parkinsonism-like features were characterized by hypokinesia and akinesia reflected as a decrease in step size, number of steps taken, and a heightened locomotor disability score, as rated by trained observers blinded to the condition of the animal. Therefore, the authors concluded that dysfunction of the α3 isoform of the sodium pump in the basal ganglia is not directly responsible for dystonia. Interestingly, and in stark contrast to the basal ganglia, infusion of the cerebellum was sufficient to induce dystonia. The α3 malfunction was suspected to be especially detrimental for cerebellar function because Purkinje cells, the sole output of the cerebellar cortex express only this isoform [88, 95]. At this point, dystonia was characterized by persistent co-contraction of agonist and antagonist muscle pairs quantified using electromyography and the appearance of prolonged abnormal postures rated by observers blinded to the condition of the animal on a dystonia scale. Furthermore, ablating cerebellar output prevented dystonia. Taken together, these data suggest that sodium pump malfunction specifically in the cerebellum causes dystonia.
Although infusion of a single region was capable of replicating certain symptoms of DYT12, no region in isolation replicated all of the features of DYT12. Moreover, infusion of either the cerebellum or basal ganglia alone was not sufficient to replicate the stress-induced aspect of the disorder. Interestingly, the authors found that concomitant perfusion of both the cerebellum and basal ganglia was necessary to replicate all of the salient aspects of DYT12 [94]. In these mice, stress induced severe and persistent dystonia and parkinsonism-like symptoms.
Future Directions in Dystonia Research
The pharmacological model of DYT12 previously described is the first rodent model that is both genetically and symptomatically faithful to the human dystonic disorder. However, the model is somewhat laborious and with the advent of modern genetic technology it is possible that even better models can be generated. For example, the success of sodium pump block in generating dystonic symptoms suggests that other alterations causing an acute functional loss of α3 isoform of the sodium pump should also induce dystonia in rodents. To test this directly, 1 could generate a mouse with floxed inactivation alleles for ATP1A3 and either use L7-creER mice or a cre-expressing lentivirus. Alternatively, lentiviral-mediated shRNA knockdown of ATP1A3 in the same regions that are implicated in generating dystonia in the pharmacological model of DYT12 would accomplish the same thing. This biased approach is warranted in the case of DYT12 because of the findings in the pharmacological model. However, for other dystonias, a thorough investigation of multiple neural regions should be attempted. Furthermore, a conditional transgenic model of DYT12 would be optimal to relate findings in the mouse back to humans, in which there is global α3 isoform dysfunction. Of course, the ideal model would be 1 in which the specific human mutations of ATP1A3 known to cause DYT12 are knocked into a mouse replacing the normal protein.
These continued studies are especially important because of the caveats of pharmacological models in general. Foremost, all drugs can have nonspecific side effects. These effects can be due to the toxic nature of the compound itself or the ability of the compound to interact with off-target proteins. For the pharmacological model of DYT12, a major concern is that at high concentrations ouabain can inhibit all isoforms of the sodium pump and some of the behavioral effects seen in the model may be due to nonspecific sodium pump malfunction. Directly disrupting ATP1A3 alone is a necessary next step in understanding DYT12. Nevertheless, valuable insights into DYT12 have been gained by the generation of the DYT12 pharmacological model.
For other genetic dystonias, in which the function of the causative protein is well understood, it may prove fruitful to attempt acute pharmacological disruption of function. For example, DYT18 or paroxysmal exercise-induced dyskinesia is known to be due to mutations in the SLC2A1 gene, which codes for the glucose transporter GLUT1 [48, 96]. DYT18 is characterized by the onset of dystonic movements that last from minutes to hours after periods of intense exercise [47]. Unlike DYT12, the dystonia in DYT18 is not persistent and abates with time. However, patients have repeated dystonic attacks. GLUT1 has been known and studied for a long time. Furthermore, compounds, such as ML-9, verapamil, and tyrphostins, can block GLUT1 [97, 98]. Therefore, it is possible to attempt acute and partial pharmacological block of GLUT1 to determine whether this is sufficient to induce the symptoms of DYT18.
The pharmacological model of DYT12 is the first to target a protein mutated in a human disorder and replicate dystonic symptoms. The generation of this model has revealed the importance of both the basal ganglia and cerebellum in DYT12. Specifically, it has demonstrated that sodium pump malfunction in the cerebellum is sufficient to induce dystonia, consistent with a growing body of literature supporting cerebellar involvement in dystonia [14, 99–101]. It has also been revealed that the interaction between these 2 regions is key in this disorder. In the future, acute targeting of dystonia-related genes may lead to a better understanding of the etiology of other dystonias.
References
Stacy MA. Handbook of Dystonia. New York: Informa Health Care 2006:1–412.
Phukan J, Albanese A, Gasser T, Warner T. Primary dystonia and dystonia-plus syndromes: clinical characteristics, diagnosis, and pathogenesis. Lancet Neurol 2011;10:1074–1085.
Gudex CM, Hawthorne MR, Butler AG, Duffey P. Effect of dystonia and botulinum toxin treatment on health-related quality of life. Mov Disord 1998;13:941–946.
Guehl D, Cuny E, Ghorayeb I, Michelet T, Bioulac B, Burbaud P. Primate models of dystonia. Prog Neurobiol 2009;87:118–131.
Bhatia KP, Marsden CD. The behavioural and motor consequences of focal lesions of the basal ganglia in man. Brain 1994;117(pt 4):859–876.
Svetel M, Kozic D, Stefanova E, Semnic R, Dragasevic N, Kostic VS. Dystonia in Wilson's disease. Mov Disord 2001;16:719–723.
Schneider SA, Bhatia KP. Secondary dystonia--clinical clues and syndromic associations. Eur J Neurol 2010;17(suppl 1):52–57.
Dewhurst K, Oliver J. Huntington's disease of young people. Eur Neurol 1970;3:278–289.
Oliver J, Dewhurst K. Childhood and adolescent forms of Huntington's disease. J Neurol Neurosurg Psychiatry 1969;32:455–459.
Gonzalez-Alegre P, Afifi AK. Clinical characteristics of childhood-onset [juvenile) Huntington disease: report of 12 patients and review of the literature. J Child Neurol 2006;21:223–229.
Schneider SA, Hardy J, Bhatia KP. Syndromes of neurodegeneration with brain iron accumulation [NBIA): An update on clinical presentations, histological and genetic underpinnings, and treatment considerations. Mov Disord 2012;27:42–53.
Neychev VK, Gross RE, Lehericy S, Hess EJ, Jinnah HA. The functional neuroanatomy of dystonia. Neurobiol Dis 2011;42:185–201.
LeDoux MS, Brady KA. Secondary cervical dystonia associated with structural lesions of the central nervous system. Mov Disord 2003;18:60–69.
Jinnah HA, Hess EJ. A new twist on the anatomy of dystonia: the basal ganglia and the cerebellum? Neurology 2006;67:1740–1741.
Cooper IS. Neurosurgical treatment of the dyskinesias. Clin Neurosurg 1977;24:367–390.
Fraioli B, Guidetti. Effects of stereotactic lesions of the dentate nucleus of the cerebellum in man. Appl Neurophysiol 1975;38:81–90.
Heimburger RF. Dentatectomy in the treatment of dyskinetic disorders. Confin Neurol 1967;29:101–106.
Zervas NT, Horner FA, Pickren KS. The treatment of dyskinesia by stereotxic dentatectomy. Confin Neurol 1967;29:93–100.
Alarcon F, Tolosa E, Munoz E. Focal limb dystonia in a patient with a cerebellar mass. Arch Neurol 2001;58:1125–1127.
Rousseaux M, Cassim F, Benaim C, Lahousse V, Pruvo JP, Steinling M. [Dystonia and tremor in bilateral lesion of the posterior mesencephalon and the vermis]. Rev Neurol (Paris) 1996;152:732–737.
Rumbach L, Barth P, Costaz A, Mas J. Hemidystonia consequent upon ipsilateral vertebral artery occlusion and cerebellar infarction. Mov Disord 1995;10:522–525.
O'Rourke K, O'Riordan S, Gallagher J, Hutchinson M. Paroxysmal torticollis and blepharospasm following bilateral cerebellar infarction. J Neurol 2006;253:1644–1645.
Asanuma K, Carbon-Correll M, Eidelberg D. Neuroimaging in human dystonia. J Med Invest 2005;52(suppl):272–279.
Edwards MJ, Huang YZ, Wood NW, Rothwell JC, Bhatia KP. Different patterns of electrophysiological deficits in manifesting and non-manifesting carriers of the DYT1 gene mutation. Brain 2003;126:2074–2080.
Starr PA, Rau GM, Davis V, et al. Spontaneous pallidal neuronal activity in human dystonia: comparison with Parkinson's disease and normal macaque. J Neurophysiol 2005;93:3165–3176.
Thompson VB, Jinnah HA, Hess EJ. Convergent mechanisms in etiologically-diverse dystonias. Expert Opin Ther Targets 2011;15:1387–1403.
Sanghera MK, Grossman RG, Kalhorn CG, Hamilton WJ, Ondo WG, Jankovic J. Basal ganglia neuronal discharge in primary and secondary dystonia in patients undergoing pallidotomy. Neurosurgery 2003;52:1358–1370.
Carbon M, Su S, Dhawan V, Raymond D, Bressman S, Eidelberg D. Regional metabolism in primary torsion dystonia: effects of penetrance and genotype. Neurology 2004;62:1384–1390.
Argyelan M, Carbon M, Niethammer M, et al. Cerebellothalamocortical connectivity regulates penetrance in dystonia. J Neurosci 2009;29:9740–9747.
Isaias IU, Volkmann J, Kupsch A, et al. Factors predicting protracted improvement after pallidal DBS for primary dystonia: the role of age and disease duration. J Neurol 2011;258:1469–1476.
Mueller J, Skogseid IM, Benecke R, et al. Pallidal deep brain stimulation improves quality of life in segmental and generalized dystonia: results from a prospective, randomized sham-controlled trial. Mov Disord 2008;23:131–134.
Kupsch A, Benecke R, Muller J, et al. Pallidal deep-brain stimulation in primary generalized or segmental dystonia. N Engl J Med 2006;355:1978–1990.
Stavrinou LC, Boviatsis EJ, Leonardos A, Panourias IG, Sakas DE. Current concepts on the mechanisms of dystonia and the beneficial effects of deep brain stimulation. Cen Eur Neurosurg 2011;72:144–148.
Andrews C, Aviles-Olmos I, Hariz M, Foltynie T. Which patients with dystonia benefit from deep brain stimulation? A metaregression of individual patient outcomes. J Neurol Neurosurg Psychiatry 2010;81:1383–1389.
Andrew J, Fowler CJ, Harrison MJ. Stereotaxic thalamotomy in 55 cases of dystonia. Brain 1983;106(Pt 4):981–1000.
Cardoso F, Jankovic J, Grossman RG, Hamilton WJ. Outcome after stereotactic thalamotomy for dystonia and hemiballismus. Neurosurgery 1995;36:501–507.
Cooper IS, Riklan M. Cryothalamectomy for abnormal movement disorders. St Barnabas Hosp Med Bull 1962;1:17–23.
Cooper IS. 20-year followup study of the neurosurgical treatment of dystonia musculorum deformans. Adv Neurol 1976;14:423–452.
Hitchcock E. Dentate lesions for involuntary movement. Proc R Soc Med 1973;66:877–879.
Davis R. Cerebellar stimulation for cerebral palsy spasticity, function, and seizures. Arch Med Res 2000;31:290–299.
Davis R, Cullen RF Jr., Flitter MA, et al. Control of spasticity and involuntary movements — cerebellar stimulation. Appl Neurophysiol 1977;40:135–140.
Tasker RR. Ablative procedures for dystonia. In: Germano IM, ed. Neurosurgical treatments of movement disorders. Park Ridge, IL: AANS Publications Committee 1988:255–267.
Standaert DG. Update on the pathology of dystonia. Neurobiol Dis 2011;42:148–151.
Bragg DC, Armata IA, Nery FC, Breakefield XO, Sharma N. Molecular pathways in dystonia. Neurobiol Dis 2011;42:136–147.
Breakefield XO, Blood AJ, Li Y, Hallett M, Hanson PI, Standaert DG. The pathophysiological basis of dystonias. Nat Rev Neurosci 2008;9:222–234.
Bruggemann N, Klein C. Genetics of primary torsion dystonia. Curr Neurol Neurosci Rep 2010;10:199–206.
Schmidt A, Klein C. The role of genes in causing dystonia. Eur J Neurol 2010;17(suppl 1):65–70.
Muller U. The monogenic primary dystonias. Brain 2009;132:2005–2025.
Vidailhet M, Grabli D, Roze E. Pathophysiology of dystonia. Curr Opin Neurol 2009;22:406–413.
Goodchild RE, Kim CE, Dauer WT. Loss of the dystonia-associated protein torsinA selectively disrupts the neuronal nuclear envelope. Neuron 2005;48:923–932.
Moseley AE, Williams MT, Schaefer TL, et al. Deficiency in Na,K-ATPase alpha isoform genes alters spatial learning, motor activity, and anxiety in mice. J Neurosci 2007;27:616–626.
Jinnah HA, Hess EJ, LeDoux MS, Sharma N, Baxter MG, DeLong MR. Rodent models for dystonia research: characteristics, evaluation, and utility. Mov Disord 2005;20:283–292.
Richter A, Loscher W. Pathology of idiopathic dystonia: findings from genetic animal models. Prog Neurobiol 1998;54:633–677.
LeDoux MS, Lorden JF. Abnormal cerebellar output in the genetically dystonic rat. Adv Neurol 1998;78:63–78.
Ledoux MS. Animal models of dystonia: lessons from a mutant rat. Neurobiol Dis 2011;42:152–161.
Defazio G, Berardelli A, Hallett M. Do primary adult-onset focal dystonias share aetiological factors? Brain 2007;130:1183–1193.
Dang MT, Yokoi F, McNaught KS, et al. Generation and characterization of Dyt1 DeltaGAG knock-in mouse as a model for early-onset dystonia. Exp Neurol 2005;196:452–463.
Shashidharan P, Sandu D, Potla U, et al. Transgenic mouse model of early-onset DYT1 dystonia. Hum Mol Genet 2005;14:125–133.
Yokoi F, Dang MT, Li J, Li Y. Myoclonus, motor deficits, alterations in emotional responses and monoamine metabolism in epsilon-sarcoglycan deficient mice. J Biochem 2006;140:141–146.
Martella G, Tassone A, Sciamanna G, et al. Impairment of bidirectional synaptic plasticity in the striatum of a mouse model of DYT1 dystonia: role of endogenous acetylcholine. Brain 2009;132:2336–2349.
Pisani A, Martella G, Tscherter A, et al. Altered responses to dopaminergic D2 receptor activation and N-type calcium currents in striatal cholinergic interneurons in a mouse model of DYT1 dystonia. Neurobiol Dis 2006;24:318–325.
Tanabe LM, Kim CE, Alagem N, Dauer WT. Primary dystonia: molecules and mechanisms. Nat Rev Neurol 2009;5:598–609.
Goodchild RE, Dauer WT. Mislocalization to the nuclear envelope: an effect of the dystonia-causing torsinA mutation. Proc Natl Acad Sci U S A 2004;101:847–852.
Ulug AM, Vo A, Argyelan M, et al. Cerebellothalamocortical pathway abnormalities in torsinA DYT1 knock-in mice. Proc Natl Acad Sci U S A 2011;108:6638–6643.
Sauer B. Inducible gene targeting in mice using the Cre/lox system. Methods 1998;14:381–392.
Gingrich JR, Roder J. Inducible gene expression in the nervous system of transgenic mice. Annu Rev Neurosci 1998;21:377–405.
Brown A, Brown S, Ellisor D, Hagan N, Normand E, Zervas M. A practical approach to genetic inducible fate mapping: a visual guide to mark and track cells in vivo. J Vis Exp 2009. doi:10.3791/1687.
Ellisor D, Zervas M. Tamoxifen dose response and conditional cell marking: is there control? Mol Cell Neurosci 2010;45:132–138.
Tiscornia G, Singer O, Ikawa M, Verma IM. A general method for gene knockdown in mice by using lentiviral vectors expressing small interfering RNA. Proc Natl Acad Sci U S A 2003;100:1844–1848.
Davidson BL, Breakefield XO. Viral vectors for gene delivery to the nervous system. Nat Rev Neurosci 2003;4:353–364.
Jakobsson J, Lundberg C. Lentiviral vectors for use in the central nervous system. Mol Ther 2006;13:484–493.
Nielsen TT, Marion I, Hasholt L, Lundberg C. Neuron-specific RNA interference using lentiviral vectors. J Gene Med 2009;11:559–569.
Gussing F, van Marion I, Ralets I, Lundberg C. Selective protein expression within the CNS using hybrid lentivirus. Methods Mol Biol 2009;515:215–226.
Baranova O, Miranda LF, Pichiule P, Dragatsis I, Johnson RS, Chavez JC. Neuron-specific inactivation of the hypoxia inducible factor 1 alpha increases brain injury in a mouse model of transient focal cerebral ischemia. J Neurosci 2007;27:6320–6332.
De Carvalho AP, Sweadner KJ, Penniston JT, et al. Mutations in the Na+/K + −ATPase alpha3 gene ATP1A3 are associated with rapid-onset dystonia parkinsonism. Neuron 2004;43:169–175.
Thomas DR, Atkinson PJ, Ho M, et al. [(3)H]-SB-269970 — A selective antagonist radioligand for 5-HT [7) receptors. Br J Pharmacol 2000;130:409–417.
Kaiser FJ, Osmanoric A, Rakovic A, et al. The dystonia gene DYT1 is repressed by the transcription factor THAP1 [DYT6). Ann Neurol 2010;68:554–559.
Clouaire T, Roussigne M, Ecochard V, Mathe C, Amalric F, Girard JP. The THAP domain of THAP1 is a large C2CH module with zinc-dependent sequence-specific DNA-binding activity. Proc Natl Acad Sci U S A 2005;102:6907–6912.
Roussigne M, Cayrol C, Clouaire T, Amalric F, Girard JP. THAP1 is a nuclear proapoptotic factor that links prostate-apoptosis-response-4 [Par-4) to PML nuclear bodies. Oncogene 2003;22:2432–2442.
Sciamanna G, Bonsi P, Tassone A, et al. Impaired striatal D2 receptor function leads to enhanced GABA transmission in a mouse model of DYT1 dystonia. Neurobiol Dis 2009;34:133–145.
Skou JC. Nobel Lecture. The identification of the sodium pump. Biosci Rep 1998;18:155–169.
Blanco G, Mercer RW. Isozymes of the Na-K-ATPase: heterogeneity in structure, diversity in function. Am J Physiol 1998;275:F633-F650.
Sandtner W, Egwolf B, Khalili-Araghi F, et al. Ouabain binding site in a functioning na+/k + ATPase. J Biol Chem 2011;286:38177–38183.
Dobyns WB, Ozelius LJ, Kramer PL, et al. Rapid-onset dystonia-parkinsonism. Neurology 1993;43:2596–2602.
Brashear A, Dobyns WB, De Carvalho AP, et al. The phenotypic spectrum of rapid-onset dystonia-parkinsonism [RDP) and mutations in the ATP1A3 gene. Brain 2007;130:828–835.
Pittock SJ, Joyce C, O'Keane V, et al. Rapid-onset dystonia-parkinsonism: a clinical and genetic analysis of a new kindred. Neurology 2000;55:991–995.
Sweadner KJ. Isozymes of the Na+/K + −ATPase. Biochim Biophys Acta 1989;988:185–220.
Hieber V, Siegel GJ, Fink DJ, Beaty MW, Mata M. Differential distribution of [Na, K)-ATPase alpha isoforms in the central nervous system. Cell Mol Neurobiol 1991;11:253–262.
Deandrade MP, Yokoi F, van Groen T, Lingrel JB, Li Y. Characterization of Atp1a3 mutant mice as a model of rapid-onset dystonia with parkinsonism. Behav Brain Res 2011;216:659–665.
Deandrade MP, Yokoi F, van Groen T, Lingrel JB, Li Y. Characterization of Atp1a3 mutant mice as a model of rapid-onset dystonia with parkinsonism. Behav Brain Res 2011; 216:659–665.
Marks MJ, Seeds NW. A heterogeneous ouabain-ATPase interaction in mouse brain. Life Sci 1978;23:2735–2744.
Urayama O, Sweadner KJ. Ouabain sensitivity of the alpha 3 isozyme of rat Na,K-ATPase. Biochem Biophys Res Commun 1988;156:796–800.
Dobretsov M, Stimers JR. Neuronal function and alpha3 isoform of the Na/K-ATPase. Front Biosci 2005;10:2373–2396.
Calderon DP, Fremont R, Kraenzlin F, Khodakhah K. The neural substrates of rapid-onset Dystonia-Parkinsonism. Nat Neurosci 2011;14:357–365.
McGrail KM, Phillips JM, Sweadner KJ. Immunofluorescent localization of three Na,K-ATPase isozymes in the rat central nervous system: both neurons and glia can express more than one Na,K-ATPase. J Neurosci 1991;11:381–391.
Weber YG, Storch A, Wuttke TV, et al. GLUT1 mutations are a cause of paroxysmal exertion-induced dyskinesias and induce hemolytic anemia by a cation leak. J Clin Invest 2008;118:2157–2168.
Louters LL, Stehouwer N, Rekman J, Tidball A, Cok A, Holstege CP. Verapamil inhibits the glucose transport activity of GLUT1. J Med Toxicol 2010;6:100–105.
Vera JC, Reyes AM, Velasquez FV, et al. Direct inhibition of the hexose transporter GLUT1 by tyrosine kinase inhibitors. Biochemistry 2001;40:777–790.
Pizoli CE, Jinnah HA, Billingsley ML, Hess EJ. Abnormal cerebellar signaling induces dystonia in mice. J Neurosci 2002;22:7825–7833.
Nitschke MF, Erdmann C, Trillenberg P, et al. Functional MRI reveals activation of a subcortical network in a 5-year-old girl with genetically confirmed myoclonus-dystonia. Neuropediatrics 2006;37:79–82.
Ritz K, van Schaik BD, Jakobs ME, et al. SGCE isoform characterization and expression in human brain: implications for myoclonus-dystonia pathogenesis? Eur J Hum Genet 2011;19:438–444.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(PDF 510 kb)
Rights and permissions
About this article
Cite this article
Fremont, R., Khodakhah, K. Alternative Approaches to Modeling Hereditary Dystonias. Neurotherapeutics 9, 315–322 (2012). https://doi.org/10.1007/s13311-012-0113-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13311-012-0113-1