Abstract
Introduction
Laparoscopic Heller-Dor surgery is the current treatment of choice for patients with esophageal achalasia, but elderly patients are generally referred for less invasive treatments (pneumatic dilations or botulinum toxin injections).
Aim
To assess the effect of age on the surgical outcome of patients receiving laparoscopic Heller-Dor as primary treatment.
Methods
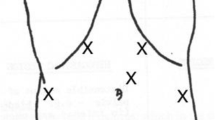
Demographic and clinical findings were prospectively collected on patients undergoing laparoscopic Heller-Dor from 1992 to 2012. Patients were classified in three age brackets: group A (≤45 years), group B (45–70), and group C (≥70). Treatment was defined as a failure if the postoperative symptom score was >10th percentile of the preoperative score (i.e., >8). We consecutively performed the Heller-Dor in 571 achalasia patients, 305 (53.4 %) in group A, 226 (39.6 %) in group B, and 40 (7 %) in group C.
Results
The mortality was nil; the conversion and morbidity rates were both 1.1 %. Group C patients had higher preoperative symptom scores (p = 0.02), while the symptom duration was similar in all three groups. Mucosal tears occurred in 17 patients (3 %): 6 (2 %) in group A, 8 (3.5 %) in group B, and 3 (7.5 %) in group C (p = 0.09). The postoperative hospital stay was slightly longer for group C (p = 0.06).
Discussion
The treatment failure rate was quite similar: 31 failures in group A (10.1 %), 19 in group B (8.4 %), and 3 in group C (7.5 %; p = 0.80). These failures were seen more in manometric pattern III (22.2 %, p = 0.002). Laparoscopic Heller-Dor can be used as the first therapeutic approach to achalasia even in elderly patients with an acceptable surgical risk.

Similar content being viewed by others
References
Richter JE. Achalasia. In: Richter JE, Castell DO (eds.). The esophagus, 4th ed. New York: Lippincott, 2005: pp 221–261.
Park W, Vaezi MF. Etiology and pathogenesis of achalasia: the current understanding. Am J Gastroenterol 2005;100:1404–14.
Sonnenberg A. Hospitalization for achalasia in the United States 1997–2006. Dig Dis Sci 2009;54:1680–85.
Gennaro N, Portale G, Gallo C, Rocchietto S, Caruso V et al. Esophageal achalasia in the Veneto region: epidemiology and treatment. Epidemiology and treatment of achalasia. J Gastrointest Surg 2011; 15:423–8.
Mayberry JF. Epidemiology and demographics of achalasia. Gastrointest Endosc Clin N Am. 2001;11:235–48.
Steven R, Bloomston M, Villadolid D. Age affects presenting symptoms of achalasia and outcomes after myotomy. Am Surg. 2005;71:424–29.
Gockel I, Junginger T, Eckardt VF. Long-term results of conventional myotomy in patients with achalasia: a prospective 20-year analysis. J Gastrointest Surg 2006;10:1400–10.
Triadafidapulos G, Boeckstaens GE, Gullo R, Patti MG, Pandolfino JE et al. The Kagoshima consensus on esophageal achalasia. Dis Esophagus 2012; 25:337–34.
Craft RO, Aguilar BE, Flahive C et al. Outcomes of minimally invasive myotomy for the treatment of achalasia in the elderly. JSLS. 2010;14:342–7.
Williams VA, Peters JH. Achalasia of the esophagus: a surgical disease. J Am Coll Surg. 2009; 208(1):151–62.
Richter JE. Oesophageal motility disorders. Lancet 2001; 358 (9284): 823–8.
Passaretti S, Zaninotto G, DiMartino N, Leo P, Costantini M, Baldi F. Standards for oesophageal manometry. A position statement from the Gruppo Italiano di Studio per la Motilità dell'Apparato Digerente. Dig Liv Dis 2001; 32: 46–55.
Zaninotto G, Costantini M, Bonavina L, Merigliano S, Baessato M, Iuliani M, Anselmino M, Ancona E. Manometric characteristics of the distal oesophageal sphincter and patterns of gastro-esophageal reflux in healthy volunteers and patients. Eur Surg Res. 1987; 19(4):217–24.
Pandolfino JE, Ghosh SK, Zhang Q, Jarosz A, Shah N, Kahrilas PJ. Quantifying EGJ morphology and relaxation with high-resolution manometry: a study of 75 asymptomatic volunteers. Am J Physiol Gastrointest Liver Physiol 2006; 290(5): G1033–40
Salvador R, Dubecz A, Polomsky M, Gellerson O, Jones CE, Raymond DP, Watson TJ, Peters JH. A new era in esophageal diagnostics: the image-based paradigm of high-resolution manometry. J Am Coll Surg 2009; 208(6):1035–44.
Pandolfino JE, Kwiatek MA, Nealis T, Bulsiewicz W, Post J, Kahrilas PJ. Achalasia: a new clinically relevant classification by high-resolution manometry. Gastroenterology 2009; 135 (5):1526–33.
Salvador R, Costantini M, Zaninotto G, Morbin T, Rizzetto C, Zanatta L, Ceolin M, Finotti E, Nicoletti L, Da Dalt G, Cavallin F, Ancona E. The preoperative manometric pattern predicts the outcome of surgical treatment for esophageal achalasia. J Gastrointest Surg 2010; 14(11):1635–45.
Ancona E, Peracchia A, Zaninotto G, Rossi M, Bonavina L, Segalin A. Heller laparoscopic cardiomyotomy with antireflux anterior fundoplication (Dor) in the treatment of esophageal achalasia. Surg Endosc 1993; 7 (5): 459–61.
Zaninotto G, Costantini M, Molena D, Buin F, Carta A, Nicoletti L, Ancona E. Treatment of esophageal achalasia with laparoscopic Heller myotomy and Dor partial anterior fundoplication: prospective evaluation of 100 consecutive patients. J Gastrointest Surg 2000; 4(3):282–9.
Crookes PF, Corkill S, DeMeester TR. Gastroesophageal reflux in achalasia. When is reflux really reflux? Dig Dis Sci 1997; 42(7):1354–61.
Zaninotto G, Costantini M, Rizzetto C, Zanatta L, Guirroli E, et al. Four hundred laparoscopic myotomies for esophageal achalasia: a single center experience. Ann Surg 2008; 248:986–93.
Boeckstaens GE, Annese V, des Varennes SB, Chaussade S Costantini M et al. Pneumatic dilation versus laparoscopic Heller's myotomy for idiopathic achalasia. New Engl J Med 2011; 364(19):1807–16
Roll GR, Sandi M, Gasper WJ, Patti M, Way LW, Carter J. Excellent outcomes of laparoscopic esophagomyotomy for achalasia patients older than 60 years of age. Surg Endosc 2010; 24:2562–66.
Gockel I, Gith A, Drescher D, Jungmann F, Eckhard L, Lang H. Minimally invasive surgery for achalasia patients >40 years: more favorable than anticipated . Langebeck Arch Surg 2012; 397:69–74.
Author information
Authors and Affiliations
Corresponding author
Additional information
Discussant
Dr. Stanley Ashley (Boston, MA, USA): Thank you Dr. Salvador for a great presentation. I want to congratulate you and your group on such a large series with such excellent outcomes. It is clear from your data that the Heller-Dor can be an effective approach to achalasia irrespective of the patient's age. I believe however that this was a select group that was referred for surgery. Can you tell us what percentage of all patients and what percentage of the group over 70 with achalasia at your institution underwent surgery?
I also wonder why you chose to exclude patients who had previously been treated—either with dilatation or botox? For many of us, this group represents a significant percentage of referrals and the question of whether to proceed with surgery or repeat the endoscopic treatment is always there, particularly in the elderly. Did this group do as well with operation?
Finally in group C, the type III patients, have you altered your approach because of the higher recurrence rate and need for dilatations?
Closing Discussant
Dr. Renato Salvador: At our department, laparoscopic Heller-Dor has become the treatment of choice for patients with esophageal achalasia over the last 20 years because, in our experience, it is less invasive and affords a better outcome. The percentage of patients undergoing surgery is very high, >90 %. If we consider only patients over 70 years old, the percentage decreases to around 60 % and our choice of therapy depends on the patients' surgical risk.
We decided to exclude patients who had already had other treatments for esophageal achalasia from the study in order to have more homogeneous groups of patients and clearer data for assessing the manometric findings (LES residual and resting pressure, manometric pattern, …) and the radiological findings. In 2008, our group published our global experience in the Annals of Surgery (Zaninotto et al. Four Hundred laparoscopic myotomies for esophageal achalasia: a single-center experience). In that study, we saw that previous endoscopic treatment(s) did not generally affect the chances of success of laparoscopic myotomy.
The answer is a longer myotomy. Before starting to assess the manometric pattern, we thought that a myotomy extending into the chest might be the answer for the spastic subtype. But when we analyzed our data, we found that the spastic type coincided with a longer LES, so we decided to perform a longer myotomy on the gastric side. The answer is therefore probably a longer myotomy on both sides. On the other hand, we saw in the European randomized trial comparing dilations with laparoscopic myotomy (in which our group took an active part) that the success rate in type III patients was higher after laparoscopic Heller Dor than after pneumatic dilations, reaching 86 and 40 %, respectively (Rohof W, Salvador R, et al. Treatment outcome of achalasia depends on the manometric subtype. Gastroenterology, December 2012).
Rights and permissions
About this article
Cite this article
Salvador, R., Costantini, M., Cavallin, F. et al. Laparoscopic Heller Myotomy Can Be Used As Primary Therapy for Esophageal Achalasia Regardless of Age. J Gastrointest Surg 18, 106–112 (2014). https://doi.org/10.1007/s11605-013-2334-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-013-2334-y