Abstract
Background
A new manometric classification of esophageal achalasia has recently been proposed that also suggests a correlation with the final outcome of treatment. The aim of this study was to investigate this hypothesis in a large group of achalasia patients undergoing laparoscopic Heller–Dor myotomy.
Methods
We evaluated 246 consecutive achalasia patients who underwent surgery as their first treatment from 2001 to 2009. Patients with sigmoid-shaped esophagus were excluded. Symptoms were scored and barium swallow X-ray, endoscopy, and esophageal manometry were performed before and again at 6 months after surgery. Patients were divided into three groups: (I) no distal esophageal pressurization (contraction wave amplitude <30 mmHg); (II) rapidly propagating compartmentalized pressurization (panesophageal pressurization >30 mmHg); and (III) rapidly propagating pressurization attributable to spastic contractions. Treatment failure was defined as a postoperative symptom score greater than the 10th percentile of the preoperative score (i.e., >7).
Results
Type III achalasia coincided with a longer overall lower esophageal sphincter (LES) length, a lower symptom score, and a smaller esophageal diameter. Treatment failure rates differed significantly in the three groups: I = 14.6% (14/96), II = 4.7% (6/127), and III = 30.4% (7/23; p = 0.0007). At univariate analysis, the manometric pattern, a low LES resting pressure, and a high chest pain score were the only factors predicting treatment failure. At multivariate analysis, the manometric pattern and a LES resting pressure <30 mmHg predicted a negative outcome.
Conclusion
This is the first study by a surgical group to assess the outcome of surgery in 3 manometric achalasia subtypes: patients with panesophageal pressurization have the best outcome after laparoscopic Heller–Dor myotomy.





Similar content being viewed by others
References
Pandolfino JE, Kwiatek MA, Nealis T, Bulsiewicz W, Post J, Kahrilas PJ. Achalasia: a new clinically relevant classification by high-resolution manometry. Gastroenterology. 2008 Nov;135(5):1526–33.
Williams VA, Peters JH. Achalasia of the esophagus: a surgical disease. J Am Coll Surg. 2009 Jan;208(1):151–62.
Richter JE. Oesophageal motility disorders. Lancet. 2001 Sep 8;358(9284):823–8.
Boeckxstaens GE. Achalasia. Best Pract Res Clin Gastroenterol. 2007;21(4):595–608.
Zaninotto G, Costantini M, Rizzetto C, Zanatta L, Guirroli E, Portale G, Nicoletti L, Cavallin F, Battaglia G, Ruol A, Ancona E. Four hundred laparoscopic myotomies for esophageal achalasia: a single centre experience. Ann Surg. 2008 Dec;248(6):986–93.
Patti MG, Pellegrini CA, Horgan S, Arcerito M, Omelanczuk P, Tamburini A, Diener U, Eubanks TR, Way LW. Minimally invasive surgery for achalasia: an 8-year experience with 168 patients. Ann Surg. 1999 Oct;230(4):587–93.
Oelschlager BK, Chang L, Pellegrini CA. Improved outcome after extended gastric myotomy for achalasia. Arch Surg. 2003 May;138(5):490–5.
Khajanchee YS, Kanneganti S, Leatherwood AE, Hansen PD, Swanström LL. Laparoscopic Heller myotomy with Toupet fundoplication: outcomes predictors in 121 consecutive patients. Arch Surg. 2005 Sep;140(9):827–33.
Liu JF, Zhang J, Tian ZQ, Wang QZ, Li BQ, Wang FS, Cao FM, Zhang YF, Li Y, Fan Z, Han JJ, Liu H. Long-term outcome of esophageal myotomy for achalasia. World J Gastroenterol. 2004 Jan 15;10(2):287–91.
Kilic A, Schuchert MJ, Pennathur A, Gilbert S, Landreneau RJ, Luketich JD. Long-term outcomes of laparoscopic Heller myotomy for achalasia. Surgery. 2009 Oct;146(4):826–31.
Zaninotto G, Costantini M, Portale G, Battaglia G, Molena D, Carta A, Costantino M, Nicoletti L, Ancona E. Etiology, diagnosis, and treatment of failures after laparoscopic Heller myotomy for achalasia. Ann Surg. 2002 Feb;235(2):186–92.
Iqbal A, Tierney B, Haider M, Salinas VK, Karu A, Turaga KK, Mittal SK, Filipi CJ. Laparoscopic re-operation for failed Heller myotomy. Dis Esophagus. 2006;19(3):193–9.
Passaretti S, Zaninotto G, DiMartino N, Leo P, Costantini M, Baldi F. Standards for oesophageal manometry. A position statement from the Gruppo Italiano di Studio per la Motilità dell’Apparato Digerente. Dig Liv Dis 2000; 32: 46–55
Zaninotto G, Costantini M, Bonavina L, Merigliano S, Baessato M, Iuliani M, Anselmino M, Ancona. Manometric characteristics of the distal oesophageal sphincter and patterns of gastro-oesophageal reflux in healthy volunteers and patients. Eur Surg Res. 1987;19(4): 217–24.
Pandolfino JE, Ghosh SK, Zhang Q, Jarosz A, Shah N, Kahrilas PJ. Quantifying EGJ morphology and relaxation with high-resolution manometry: a study of 75 asymptomatic volunteers. Am J Physiol Gastrointest Liver Physiol. 2006 290(5):G1033-40
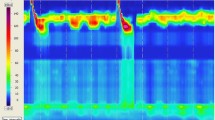
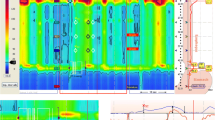
Salvador R, Dubecz A, Polomsky M, Gellerson O, Jones CE, Raymond DP, Watson TJ, Peters JH. A new era in esophageal diagnostics: the image-based paradigm of high-resolution manometry. J Am Coll Surg. 2009 Jun;208(6):1035–44.
Vantrappen G, Janssens J, Hellemans J, Coremans G. Achalasia, diffuse esophageal spasm, and related motility disorders. Gastroenterology 1979 Mar; 76:450–457.
Ancona E, Peracchia A, Zaninotto G, Rossi M, Bonavina L, Segalin A. Heller laparoscopic cardiomyotomy with antireflux anterior fundoplication (Dor) in the treatment of esophageal achalasia. Surg Endosc. 1993 Sep–Oct;7(5):459–61.
Zaninotto G, Costantini M, Molena D, Buin F, Carta A, Nicoletti L, Ancona E. Treatment of esophageal achalasia with laparoscopic Heller myotomy and Dor partial anterior fundoplication: prospective evaluation of 100 consecutive patients. J Gastrointest Surg. 2000 May–Jun;4(3):282–9.
Crookes PF, Corkill S, DeMeester TR. Gastroesophageal reflux in achalasia. When is reflux really reflux? Dig Dis Sci. 1997 Jul;42(7):1354–61.
Costantini M, Zaninotto G, Guirroli E, Rizzetto C, Portale G, Ruol A, Nicoletti L, Ancona E. The laparoscopic Heller-Dor operation remains an effective treatment for esophageal achalasia at a minimum 6-year follow-up. Surg Endosc. 2005 Mar;19(3):345–51.
Ellis HF. Failures after esophagomyotomy for esophageal motor disorders. Causes, prevention, and management. Chest Surg Clin North Am 1997;7:476–488.
Patti MG, Feo CV, Diener U, Tamburini A, Arcerito M, Safadi B, Way LW. Laparoscopic Heller myotomy relieves dysphagia in achalasia when the esophagus is dilated. Surg Endosc. 1999 Sep;13(9):843–7.
Omura N, Kashiwagi H, Ishibashi Y, Yano F, Tsuboi K, Kawasaki N, Suzuki Y, Yanaga K. Laparoscopic Heller myotomy and Dor fundoplication for the treatment of achalasia. Assessment in relation to morphologic type. Surg Endosc. 2006 Feb;20(2):210–3.
Portale G, Costantini M, Rizzetto C, Guirroli E, Ceolin M, Salvador R, Ancona E, Zaninotto G. Long-term outcome of laparoscopic Heller-Dor surgery for esophageal achalasia: possible detrimental role of previous endoscopic treatment. J Gastrointest Surg. 2005 Dec;9(9):1332―9.
Arain MA, Peters JH, Tamhankar AP, Portale G, Almogy G, DeMeester SR, Crookes PF, Hagen JA, Bremner CG, DeMeester TR. Preoperative lower esophageal sphincter pressure affects outcome of laparoscopic esophageal myotomy for achalasia. J Gastrointest Surg. 2004 Mar―Apr;8(3):328―34.
Torquati A, Richards WO, Holzman MD, Sharp KW. Laparoscopic myotomy for achalasia: predictors of successful outcome after 200 cases. Ann Surg. 2006 May;243(5):587―91.
Author information
Authors and Affiliations
Corresponding author
Additional information
Discussant
Dr. John E. Pandolfino (Chicago, IL): I would like to thank Dr. Salvador for a wonderful study. He spent some time with us in our lab, and he obviously extended this to a very nice piece of work. I think that when you look at achalasia, it’s still, even though it’s the most well-defined esophageal motor disorder, there’s still significant heterogeneity when we look at this. When you evaluate high-resolution manometry, you’re struck by the variability in the peristaltic contractions and the intrabolus pressure patterns.
So when we originally saw this, we theorized that there should be some predictive value of this. And subsequently, we validated this work, but it was difficult. And really, we were very happy to see Dr. Salvador’s work because this was a much-needed confirmation that there was something we can glean from high-resolution manometry.
I think the strengths of this particular study are: 1) the large numbers, 2) the fact that the patients underwent one particular type of therapy, surgery, and 3) also the novel concept of applying these patterns back to conventional manometry for other investigators and clinicians to utilize.
Once again, it’s logical that type 2 patients would do better. They have intact esophageal mechanics. They also have intact longitudinal muscle function. It’s also logical that the type 3 patients that we have identified with spastic features are going to do poorly.
So with that, I have a few questions:
And once again, congratulations on a very detailed and wonderful study. What do you actually do for the type 3 patients? I think that’s an important thing now that we have defined them.
The other issue was, how hard is it—and you are an experienced manometric evaluator—but how hard is it to take these concepts and apply them back to conventional tracing manometry?
Closing Discussant
Dr. Renato Salvador: The answer is: a longer myotomy, maybe. Before starting this study, especially after reading your own paper, we thought that maybe a myotomy extended into the chest could be the answer for the spastic type. However, when we analised our own data, we noticed that the spastic type had a longer lower esophageal sphincter, so maybe also a longer myotomy on the gastric side could be indicated in these patients. The answer is then probably a longer myotomy on both sides.
On the other hand, we do not know much about pneumatic dilations in these patients. In this very moment, the results at 2-year follow-up of the European trial (comparing dilations and laparoscopic myotomy) are presented in another room of this building. We actively participated in this trial. It could be interesting to go back to the manometric tracings of these patients and compare the results of myotomy and dilations in this particular group of patients (spastic type), and in the other two groups. It is important to underline that all the patients in the trial, as in this study, were patients with primary achalasia, without previous endoscopic treatment.
What about conventional manometry? In our study, the vast majority of patients had conventional manometry. As you know from the paper, we applied the concepts of high resolution manometry to the conventional tracings. It was quite easy for Group 1 and 2, a little more difficult for the 3rd Group (that also resulted to be the most intriguing group). By applying the parameters of other well known authors, we are confident that we have categorized the three groups of patients even with the old conventional manometry well. We agree with you, from the experience I personally had in Rochester, NY, with Dr. Peters, and now in Italy where we have lately acquired the system, that high resolution manometry provides us with a lot more details than conventional manometry, allowing a better characterisation of the motility of the esophagus before and after myotomy.
Discussant
Dr. Jeffrey Peters (Rochester, NY): I agree with John’s comments. First, I have a question about the classification. You have classified achalasia into three subsets, Group 1 was characterized by a cutoff of 30-millimeter mercury pressurization in the esophagus. That seems to be awful high. I wonder how the data would change if you change the 30-millimeter threshold and reanalyze the data at to 10 or 15. Second, as I’ve had the opportunity to see the manuscript, I wonder if there weren’t some patients in group 3 that have a normal residual pressure of their sphincter?
Closing Discussant
Dr. Renato Salvador: We chose a cut-off of 30 mmHg following Dr. Pandolfino et al. paper with the proposed new classification of achalasia based on high resolution manometry. Again, we applied those concepts to conventional manometry. We do not know if lowering the threshold to 15 or 10 mmHg could change the classification of patients in Group 1 or 2. That is something that we have to look at.
As far as the second question is concerned, we agree that in some patients of group 3 (but also in other groups) residual pressure may fall in the normal range. Unfortunately our protocol did not include a sleeve sensor to carefully evaluate the LES relaxation with conventional manometry and the patients studied with HRM are only a few. However, if we look at the percentage of patients with abnormal parameters of the LES (i.e.: resting and residual pressure, overall and abdominal lengths) we found no differences among the three groups of patients in all the parameters but in the overall length, that is longer in a significant percentage of pattern 3 patients.
Discussant
Dr. Michael S. Nussbaum (Jacksonville, FL): As a follow-up to what Dr. Peters was asking. How can you be certain that some of these failures or differences aren’t due to an incomplete myotomy? Have you considered performing intraoperative manometry in order to tailor the myotomy; particularly in the type 3 patients?
Closing Discussant
Dr. Renato Salvador: This is a good question. This is also exactly what we were discussing when we saw the final results of our study. Intraoperative manometry, that usually is not performed during myotomy, may play an important role in group 3 patients, and could represent the answer also to Dr. Pandolfino and Dr. Peters’ questions. Intraoperative manometry may be conclusive in objectively verifying the completeness of the myotomy in this particular group of patients that, as said before, also appeared to have a longer lower esophageal sphincter.
Rights and permissions
About this article
Cite this article
Salvador, R., Costantini, M., Zaninotto, G. et al. The Preoperative Manometric Pattern Predicts the Outcome of Surgical Treatment for Esophageal Achalasia. J Gastrointest Surg 14, 1635–1645 (2010). https://doi.org/10.1007/s11605-010-1318-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-010-1318-4