Abstract
Background
The aim of this study was to assess the long-term outcome of laparoscopic Heller-Dor (LHD) myotomy to treat achalasia at a single high-volume institution in the past 25 years.
Methods
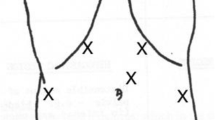
Patients undergoing LHD from 1992 to 2017 were prospectively registered in a dedicated database. Those who had already undergone surgical or endoscopic myotomy were ruled out. Symptoms were collected and scored using a detailed questionnaire; barium swallow, endoscopy, and manometry were performed before and after surgery; and 24-h pH monitoring was done 6 months after LHD.
Results
One thousand one patients underwent LHD (M:F = 536:465), performed by six staff surgeons. The surgical procedure was completed laparoscopically in all but 8 patients (0.8%). At a median of follow-up of 62 months, the outcome was positive in 896 patients (89.5%), and the probability of being cured from symptoms at 20 years exceeded 80%. Among the patients who had previously received other treatments, there were 25/182 failures (13.7%), while the failures in the primary treatment group were 80/819 (9.8%) (p = 0.19). All 105 patients whose LHD failed subsequently underwent endoscopic pneumatic dilations with an overall success rate of 98.4%. At univariate analysis, the manometric pattern (p < 0.001), the presence of a sigmoid megaesophagus (p = 0.03), and chest pain (p < 0.001) were the factors that predicted a poor outcome. At multivariate analysis, all three factors were independently associated with a poor outcome. Post-operative 24-h pH monitoring was abnormal in 55/615 patients (9.1%).
Conclusions
LHD can durably relieve achalasia symptoms in more than 80% of patients. The pre-operative manometric pattern, the presence of a sigmoid esophagus, and chest pain represent the strongest predictors of outcome.







Similar content being viewed by others
References
Boeckxstaens GE, Zaninotto G, Richter JE. Achalasia. Lancet 2014; 383(9911): 83–93.
Moonen A, Annese V, Belmans A, Bredenoord AJ, Bruley des Varannes S, Costantini M, Dousset B, Elizalde JI, Fumagalli U, Gaudric M, Merla A, Smout AJ, Tack J, Zaninotto G, Busch OR, Boeckxstaens GE. Long-term results of the European achalasia trial: a multicentre randomised controlled trial comparing pneumatic dilation versus laparoscopic Heller myotomy. Gut 2016; 65(5): 732–739.
Shimi S, Nathanson LK, Cuschieri A. Laparoscopic cardiomyotomy for achalasia. J R Coll Surg Edinb 1991; 36: 152–154.
Bonavina L, Nosadini A, Bardini R, Baessato M, Peracchia A. Primary treatment of esophageal achalasia. Long-term results of myotomy and Dor fundoplication. Arch Surg 1992; 127(2): 222–227.
Ancona E, Peracchia A, Zaninotto G, Rossi M, Bonavina L, Segalin A. Heller laparoscopic cardiomyotomy with antireflux anterior fundoplication (Dor) in the treatment of esophageal achalasia. Surg Endosc 1993; 7(5): 459–461.
Patti MG, Pellegrini CA, Horgan S, Arcerito M, Omelanczuk P, Tamburini A, Diener U, Eubanks TR, Way LW. Minimally invasive surgery for achalasia: an 8-year experience with 168 patients. Ann Surg 1999; 230(4): 587–593.
Omura N, Kashiwagi H, Ishibashi Y, Yano F, Tsuboi K, Kawasaki N, Suzuki Y, Yanaga K. Laparoscopic Heller myotomy and Dor fundoplication for the treatment of achalasia. Assessment in relation to morphologic type. Surg Endosc 2006; 20(2): 210–213.
Zaninotto G, Costantini M, Rizzetto C, Zanatta L, Guirroli E, Portale G, Nicoletti L, Cavallin F, Battaglia G, Ruol A, Ancona E. Four hundred laparoscopic myotomies for esophageal achalasia: a single centre experience. Ann Surg 2008; 248(6): 986–993.
Inoue H, Minami H, Kobayashi Y, Sato Y, Kaga M, Suzuki M, Satodate H, Odaka N, Itoh H, Kudo S. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy 2010; 42: 265–271.
Akintoye E, Kumar N, Obaitan I, Alayo QA, Thompson CC. Peroral endoscopic myotomy: a meta-analysis. Endoscopy 2016; 48(12): 1059–1068.
Zaninotto G, Annese V, Costantini M, Del Genio A, Costantino M, Epifani M, Gatto G, D’onofrio V, Benini L, Contini S, Molena D, Battaglia G, Tardio B, Andriulli A, Ancona E. Randomized controlled trial of botulinum toxin versus laparoscopic Heller myotomy for esophageal achalasia. Ann Surg 2004; 239(3): 364–370.
Boeckxstaens GE, Annese V, des Varannes SB, Chaussade S, Costantini M, Cuttitta A, Elizalde JI, Fumagalli U, Gaudric M, Rohof WO, Smout AJ, Tack J, Zwinderman AH, Zaninotto G, Busch OR. European Achalasia Trial Investigators. Pneumatic dilation versus laparoscopic Heller’s myotomy for idiopathic achalasia. N Engl J Med 2011; 364(19): 1807–1816.
Salvador R, Savarino E, Pesenti E, Spadotto L, Capovilla G, Cavallin F, Galeazzi F, Nicoletti L, Merigliano S, Costantini M. The Impact of Heller Myotomy on Integrated Relaxation Pressure in Esophageal Achalasia. J Gastrointest Surg 2016; 20(1): 125–131.
Kahrilas PJ, Bredenoord AJ, Fox M, Gyawali CP, Roman S, Smout AJ, Pandolfino JE. International High Resolution Manometry Working Group. The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil 2015; 27(2): 160–174.
Salvador R, Costantini M, Cavallin F, Zanatta L, Finotti E, Pozza G, Longo C, Nicoletti L, Capovilla G, Bardini R, Ancona E, Zaninotto G. Laparoscopic Heller myotomy can be used as primary therapy for esophageal achalasia regardless of age. J Gastrointest Surg 2014; 18(1): 106–112.
Henderson RD, Barichello AW, Pearson FG, Mugashe F, Szczepanski M. Diagnosis of achalasia. Can J Surg 1972; 15(3): 190–201.
Passaretti S, Zaninotto G, DiMartino N, Leo P, Costantini M, Baldi F. Standards for oesophageal manometry. A position statement from the Gruppo Italiano di Studio per la Motilità dell’Apparato Digerente. Dig Liv Dis 2001; 32: 46–55.
Salvador R, Dubecz A, Polomsky M, Gellerson O, Jones CE, Raymond DP, Watson TJ, Peters JH. A new era in esophageal diagnostics: the image-based paradigm of high-resolution manometry. J Am Coll Surg 2009; 208(6): 1035–1044.
Salvador R, Costantini M, Zaninotto G, Morbin T, Rizzetto C, Zanatta L, Ceolin M, Finotti E, Guirroli E, Nicoletti L, Da Dalt GF, Cavallin F, Ancona E. The preoperative manometric pattern predicts the outcome of surgical treatment for esophageal achalasia. J Gastrointestinal Surg 2010; 211(6): 754–761.
Dor J, Humbert P, Paoli JM, Miorclerc M, Aubert J. Treatment of reflux by the so-called modified Heller-Nissen technic. Presse Med 1967; 75(50): 2563–2565.
Crookes PF, Corkill S, De Meester TR. Gastroesophageal reflux in achalasia. When is reflux really reflux? Dig Dis Sci 1997; 42(7): 1354–1361.
Zaninotto G, Costantini M, Portale G, Battaglia G, Molena D, Carta A, Costantino M, Nicoletti L, Ancona E. Etiology, Diagnosis and treatment of failures after laparoscopic Heller myotomy for achalasia. Ann Surg 2002; 235: 186–192.
Zaninotto G, Costantini M, Molena D, Buin F, Carta A, Nicoletti L, Ancona E. Treatment of esophageal achalasia with laparoscopic Heller myotomy and Dor partial anterior fundoplication: prospective evaluation of 100 consecutive patients. J Gastrointest Surg 2000; 4(3): 282–289.
Campos GM, Vittinghoff E, Rabl C, Takata M, Gadenstätter M, Lin F, Ciovica R. Endoscopic and surgical treatments for achalasia: a systematic review and meta-analysis. Ann Surg 2009; 249(1): 45–57.
Costantini M, Zaninotto G, Guirroli E, Rizzetto C, Portale G, Ruol A, Nicoletti L, Ancona E. Laparoscopic Heller-Dor operation remains an effective treatment for esophageal achalasia at a minimum six-year follow-up. Surg Endosc 2005; 19: 345–351.
Jeansone LO, White BC, Pilger KE, Shane MD, Zagorski S, Davis SS, Hunter JG, Lin E, Smith CD. Ten-year follow-up of laparoscopic Heller myotomy for achalasia shows durability. Surg Endosc 2007; 21: 1498–1502.
Cowgill SM, Villadolid D, Boyle R, Al-Saadi S, Ross S, Rosemurgy AS. Laparoscopic Heller myotomy for achalasia: results after 10 years. Surg Endosc 2009; 23: 2644–2649.
IIKrishnamohan P, Allen MS, Shen KR, Wigle DA, Nichols FC 3rd, Cassivi SD, Harmsen WS, Deschamps C. Long-term outcome after laparoscopic myotomy for achalasia. J Thorac Cardiovasc Surg 2014; 147(2): 730–736.
Rosemurgy AS, Morton CA, Rosas M, Albrink M, Ross SB. A single institution's experience with more than 500 laparoscopic Heller myotomies for achalasia. J Am Coll Surg 2010; 210(5): 637–645, 645-647.
Lynch KL, Pandolfino JE, Howden CW, Kahrilas PJ. Major complications of pneumatic dilation and Heller myotomy for achalasia: single-center experience and systematic review of the literature. Am J Gastroenterol 2012; 107(12): 1817–1825.
Wang YR, Dempsey DT, Friedenberg FK, Richter JE. Trends of Heller myotomy hospitalizations for achalasia in the United States, 1993-2005: effect of surgery volume on perioperative outcomes. Am J Gastroenterol 2008; 103(10): 2454–2464.
Ross SW, Oommen B, Wormer BA, Walters AL, Matthews BD, Heniford BT, Augenstein VA. National outcomes of laparoscopic Heller myotomy: operative complications and risk factors for adverse events. Surg Endosc 2015; 29(11): 3097–3105.
Ehlers AP, Oelschlager BK, Pellegrini CA, Wright AS, Saunders MD, Flum DR, He H, Farjah F. Achalasia Treatment, Outcomes, Utilization, and Costs: A Population-Based Study from the United States. J Am Coll Surg 2017; 225(3): 380–386.
Haisley KR, Preston JF, Dolan JP, Diggs BS, Hunter JG. Twenty-year trends in the utilization of Heller myotomy for achalasia in the United States. Am J Surg 2017; 214(2): 299–302.
Kilic A, Schuchert MJ, Pennathur A, Landreneau RJ, Alvelo-Rivera M, Christie NA, Gilbert S, Abbas G, Luketich JD. Minimally invasive myotomy for achalasia in the elderly. Surg Endosc 2008; 22: 862–865.
Roll GR, Ma S, Gasper WJ, Patti M, Way LW, Carter J. Excellent outcomes of laparoscopic esophagomyotomy for achalasia in patients older than 60 years of age. Surg Endosc 2010; 24: 2562–2566.
Salvador R, Spadotto L, Capovilla G, Voltarel G, Pesenti E, Longo C, Cavallin F, Nicoletti L, Ruol A, Valmasoni M, Merigliano S, Costantini M. Mucosal Perforation During Laparoscopic Heller Myotomy Has No Influence on Final Treatment Outcome. J Gastrointest Surg 2016; 20(12): 1923–1930.
Patti MG, Arcerito M, Tong J, De Pinto M, de Bellis M, Wang A, Feo CV, Mulvihill SJ, Way LW. Importance of preoperative and postoperative pH monitoring in patients with esophageal achalasia. J Gastrointest Surg 1997; 1: 505–510.
Patti MG, Fernando HA. Fundoplication after laparoscopic Heller myotomy for esophageal achalasia: What type? J Gastrointest Surg 2010; 14: 1453–1458.
Pechlivanides G, Chrysos E, Athanasakis E, Tsiaoussis J, Vassilakis JS, Xynos E. Laparoscopic Heller cardiomyotomy and Dor fundoplication for esophageal achalasia: possible factors predicting outcome. Arch Surg 2001; 136(11): 1240–1243.
Patti MG, Andolfi C, Bowers SP, Soper NJ. POEM vs Laparoscopic Heller myotomy and fundoplication: which is now the gold standard for treatment of achalasia? J Gastrointest Surg 2017; 21: 207–214.
Vela MF, Richter JE, Khandwala F, Blackstone EH, Wachsberger D, Baker ME, Rice TW. The long-term efficacy of pneumatic dilatation and Heller myotomy for the treatment of achalasia. Clin Gastroenterol Hepatol 2006; 4(5): 580–587.
Dobrucali A, Erzin Y, Tuncer M, Dirican A. Long-term results of graded pneumatic dilatation under endoscopic guidance in patients with primary esophageal achalasia. World Journal of Gastroenterology : WJG 2004; 10(22): 3322–3327.
Novais PA, Lemme EM. 24-h pH monitoring patterns and clinical response after achalasia treatment with pneumatic dilation or laparoscopic Heller myotomy. Aliment Pharmacol Ther 2010; 32(10): 1257–1265.
Familiari P, Greco S, Gigante G, Calì A, Boškoski I, Onder G, Perri V, Costamagna G. Gastroesophageal reflux disease after peroral endoscopic myotomy: Analysis of clinical, procedural and functional factors, associated with gastroesophageal reflux disease and esophagitis. Dig Endosc 2016; 28(1): 33–41.
Salvador R, Pesenti E, Gobbi L, Spadotto L, Voltarel G, Cavallin F, Nicoletti L, Capovilla G, Ruol A, Valmasoni M, Merigliano S, Costantini M. Post-operative Gastroesophageal Reflux after laparoscopic Heller-Dor for Achalasia: True incidence with an objective evaluation. Journal Gastrointestinal Surgery 2017; 21(1): 17–22.
Richards WO, Torquati A, Holzman MD, Khaitan L, Byrne D, Lutfi R, Sharp KW. Heller myotomy versus Heller myotomy with Dor fundoplication for achalasia: a prospective randomized double-blind clinical trial. Ann Surg 2004; 240(3): 405–412.
Kummerow Broman K, Phillips SE, Faqih A, Kaiser J, Pierce RA, Poulose BK, Richards WO, Sharp KW, Holzman MD. Heller myotomy versus Heller myotomy with Dor fundoplication for achalasia: long-term symptomatic follow-up of a prospective randomized controlled trial. Surg Endosc 2018; 32(4): 1668–1674.
Rawlings A, Soper NJ, Oelshlager B, Swanstrom L, Matthews BD, Pellegrini C, Pierce RA, Pryor A, Martin V, Frisella MM, Cassera M, Brunt LM. Laparoscopic Dor versus Toupet fundoplication following Heller myotomy for achalasia: results of a multicenter, prospective, randomized-controlled trial. Surg Endosc 2012;26:18–26.
Yano F, Omura N, Tsuboi K, Hoshino M, Yamamoto S, Akimoto S, Masuda T, Kashiwagi H, Yanaga K. Learning curve for laparoscopic Heller myotomy and Dor fundoplication for achalasia. PLoS One 2017; 12(7): e0180515.
Swanstrom LL, Kurian A, Dunst CM, Sharata A, Bhayani N, Rieder E. Long-term outcomes of an endoscopic myotomy for achalasia: the POEM procedure. Ann Surg 2012; 256(4): 659–667.
Von Renteln D, Fuchs KH, Fockens P, Bauerfeind P, Vassiliou MC, Werner YB, Fried G, Breithaupt W, Heinrich H, Bredenoord AJ, Kersten JF, Verlaan T, Trevisonno M, Rösch T. Peroral endoscopic myotomy for the treatment of achalasia: an international prospective multicenter study. Gastroenterology 2013; 145(2): 309–311.
Patel K, Abbassi-Ghadi N, Markar S, Kumar S, Jethwa P, Zaninotto G. Peroral endoscopic myotomy for the treatment of esophageal achalasia: systematic review and pooled analysis. Dis Esophagus 2016; 29(7): 807–819.
Repici A, Fuccio L, Maselli R, Mazza F, Correale L, Mandolesi D, Bellisario C, Sethi A, Khashab MA, Rösch T, Hassan C. GERD after per-oral endoscopic myotomy as compared with Heller’s myotomy with fundoplication: a systematic review with meta-analysis. Gastrointest Endosc 2018; 87(4): 934–943.
Leeuwenburgh I, Scholten P, Alderliesten J, Tilanus HW, Looman CW, Steijerberg EW, Kuipers EJ. Long-term esophageal cancer risk in patients with primary achalasia: a prospective study. Am J Gastroenterol 2010; 105(10): 2144–2149.
Ríos-Galvez S, Meixueiro-Daza A, Remes-Troche JM. Achalasia: a risk factor that must not be forgotten for esophageal squamous cell carcinoma. BMJ Case Rep 2015; 2015.
Zaninotto G, Rizzetto C, Zambon P, Guzzinati S, Finotti E, Costantini M. Long-term outcome and risk of oesophageal cancer after surgery for achalasia. Br J Surg 2008; 95(12): 1488–1494.
Guo JP, Gilman PB, Thomas RM, Fisher RS, Parkman HP. Barrett’s esophagus and achalasia. J Clin Gastroenterol 2002; 34: 439–443.
Zendehdel K, Nyrén O, Edberg A, Ye W. Risk of esophageal adenocarcinoma in achalasia patients, a retrospective cohort study in Sweden. Am J Gastroenterol 2011; 106(1): 57–61.
Patti MG, Feo CV, Diener U, Tamburini A, Arcerito M, Safadi B, Way LW. Laparoscopic Heller myotomy relieves dysphagia in achalasia when the esophagus is dilated. Surg Endosc 1999; 13(9): 843–847.
Herbella FAM, Patti MG. Laparoscopic Heller myotomy and fundoplication in patients with end-stage achalasia. World J Surg 2015; 39: 1631–1633.
Sweet MP, Nipomnick I, Gasper WJ, Bagatelos K, Ostroff JW, Fisichella PM, Way LW, Patti MG. The outcome of laparoscopic Heller myotomy for achalasia is not influenced by the degree of esophageal dilatation. J Gastrointest Surg 2008; 12(1): 159–165.
Pandolfino JE, Kwiatek MA, Nealis T, Bulsiewicz W, Post J, Kahrilas PJ. Achalasia: a new clinically relevant classification by high-resolution manometry. Gastroenterology 2008; 135(5): 1526–1533.
Rohof WO, Salvador R, Annese V, Bruley des Varannes S, Chaussade S, Costantini M, Elizalde JI, Gaudric M, Smout AJ, Tack J, Busch OR, Zaninotto G, Boeckxstaens GE. Outcomes of treatment for achalasia depend on manometric subtype. Gastroenterology 2013; 144(4): 718–725.
Salvador R, Voltarel G, Savarino E, Capovilla G, Pesenti E, Perazzolo A, Nicoletti L, Costantini A, Merigliano S, Costantini M. The natural history of achalasia: Evidence of a continuum-“The evolutive pattern theory”. Dig Liver Dis 2018; 50(4): 342–347.
Crespin OM, Tatum RP, Xiao K, Martin AV, Khandelwal S, Pellegrini CA, Oelschlager BK. The relationship between manometric subtype and outcomes of surgical treatment for patients with achalasia. Surg Endosc 2017; 31: 5066–5075.
Zhang W, Linghu E-Q. Peroral Endoscopic Myotomy for type III achalasia of Chicago classification: Outcomes with a minimum follow-up of 24 months. J Gastrointest Surg 2017; 21: 785–791.
Kumbhari V, Tieu AH, Onimaru M, El Zein MH, Teitelbaum EN, Ujiki MB, Gitelis ME, Modayil RJ, Hungness ES, Stavropoulos SN, Shiwaku H, Kunda R, Chiu P, Saxena P, Messallam AA, Inoue H, Khashab, MA. Peroral endoscopic myotomy (POEM) vs laparoscopic Heller myotomy (LHM) for the treatment of Type III achalasia in 75 patients: a multicenter comparative study. Endoscopy International Open 2015; 3(3): E195–E201.
Horgan S, Hudda K, Eubanks T, McAllister J, Pellegrini CA. Does botulinum toxin injection make esophagomyotomy a more difficult operation? Surg Endosc 1999; 13(6): 576–579.
Patti MG, Feo CV, Arcerito M, De Pinto M, Tamburini A, Diener U, Gantert W, Way LW. Effects of previous treatment on results of laparoscopic Heller myotomy for achalasia. Dig Dis Sci 1999; 44(11): 2270–2276.
Morino M, Rebecchi F, Festa V, Garrone C. Preoperative pneumatic dilatation represents a risk factor for laparoscopic Heller myotomy. Surg Endosc 1997; 11: 359–361.
Souma Y, Nakajima K, Taniguchi E, Takahashi T, Kurokawa Y, Yamasaki M, Miyazaki Y, Makino T, Hamada T, Yasuda J, Yumiba T, Ohashi S, Takiguchi S, Mori M, Doki Y. Mucosal perforation during laparoscopic surgery for achalasia: impact of preoperative pneumatic balloon dilation. Surg Endosc 2017; 31(3): 1427–1435.
Bonavina L, Incarbone R, Reitano M, Antoniazzi L, Peracchia A. Does previous endoscopic treatment affect the outcome of laparoscopic Heller myotomy? Ann Chir 2000; 125: 45–49.
Ferguson MK, Reeder LB, Olak J. Results of myotomy and partial fundoplication after pneumatic dilation for achalasia. Ann Thorac Surg 1996; 62(2): 327–330.
Holzman MD, Sharp KW, Ladipo JK, Eller RF, Holcomb GW 3rd, Richards WO. Laparoscopic surgical treatment of achalasia. Am J Surg 1997; 173(4): 308–311.
Tsuboi K, Omura N, Yano F, Kashiwagi H, Kawasaki N, Suzuki Y, Yanaga K. Preoperative dilatation does not affect the surgical outcome of laparoscopic Heller myotomy and Dor fundoplication for esophageal achalasia. Surg Laparosc Endosc Percutan Tech 2009; 19: 98–100.
Portale G, Costantini M, Rizzetto C, Guirroli E, Ceolin M, Salvador R, Ancona E, Zaninotto G. Long-term outcome of laparoscopic Heller-Dor surgery for esophageal achalasia: possible detrimental role of previous endoscopic treatment. J Gastrointest Surg 2005; 9(9): 1332–1339.
Acknowledgments
The authors acknowledge all the other surgeons who performed LHD at the Padova University Department of Surgery during the study period: Ermanno Ancona (1992–2012), Mauro Rossi (1992–2001), Giovanni Zaninotto (1995–2007), Christian Rizzetto (2009). Without their work and dedication, this study would not have been possible.
Author information
Authors and Affiliations
Contributions
Study design: Costantini M, Salvador, Briscolini, Merigliano
Data acquisition: Salvador, Vallese, Briscolini, Capovilla, Valmasoni, Nicoletti, Costantini A
Data interpretation: Costantini M, Salvador, Briscolini, Merigliano
Drafting of manuscript: Costantini M, Salvador, Costantini A, Vallese, Briscolini, Valmasoni, Capovilla, Nicoletti, Merigliano
Final approval: Costantini M, Salvador, Vallese, Briscolini, Capovilla, Valmasoni, Costantini A, Nicoletti, Merigliano
Agreement to be accountable for all aspects of the work: Costantini M, Salvador, Vallese, Briscolini, Capovilla, Valmasoni, Costantini A, Nicoletti, Merigliano
Corresponding author
Rights and permissions
About this article
Cite this article
Costantini, M., Salvador, R., Capovilla, G. et al. A Thousand and One Laparoscopic Heller Myotomies for Esophageal Achalasia: a 25-Year Experience at a Single Tertiary Center. J Gastrointest Surg 23, 23–35 (2019). https://doi.org/10.1007/s11605-018-3956-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-018-3956-x