Abstract
Naegleria fowleri is a pathogenic free-living amoeba which causes primary amoebic meningoencephalitis in humans and experimental animals. To investigate the mechanisms of such inflammatory diseases, potential chemokine gene activation in human astroglial cells was investigated following treatment with N. fowleri lysates. We demonstrated that N. fowleri are potent inducers for the expression of interleukin-8 (IL-8) genes in human astroglial cells which was preceded by activation of extracellular signal-regulated kinase (ERK). In addition, N. fowleri lysates induces the DNA binding activity of activator protein-1 (AP-1), an important transcription factor for IL-8 induction. The specific mitogen-activated protein kinase kinase/ERK inhibitor, U0126, blocks N. fowleri-mediated AP-1 activation and subsequent IL-8 induction. N. fowleri-induced IL-8 expression requires activation of ERK in human astroglial cells. These findings indicate that treatment of N. fowleri on human astroglial cells leads to the activation of AP-1 and subsequent expression of IL-8 which are dependent on ERK activation. These results may help understand the N. fowleri-mediated upregulation of chemokine and cytokine expression in the astroglial cells.
Similar content being viewed by others
Introduction
Naegleria fowleri, a free-living amoeba, is found in a variety of natural environments including soil, ponds, and freshwater. N. fowleri cause primary amoebic meningoencephalitis (PAM) in human and mammals (Culbertson 1971; John 1982; Ma et al. 1990; Marciano-Cabral 1988; Schuster and Visvesvara 2004). The infection of N. fowleri occurs by inhalation or aspirating of water contaminated with the amoeba into the nasal cavity, and subsequently, the invasive N. fowleri enter the central nervous system (CNS) through the olfactory apparatus. PAM has an acute onset, usually fatal, necrotizing, and hemorrhagic meningoencephalitis (Carter 1970; Martinez and Visvesvara 1997). Invasive N. fowleri capable of entering the nervous system usually digest neuronal tissue and other mammalian cells by effective cytolysis and phagocytosis, as observed in culture or in infected sections of the brain tissue (Brown 1979; Herbst et al. 2002).
Astrocytes, the major glial cells in the CNS, maintain the homeostatic environment and also play an important role in immune regulation, acting as a source of chemokines, cytokines, and adhesion molecules (Dong and Benveniste 2001; Kwon et al. 2004). Thus, activated astrocytes play important roles as inflammatory or immunoregulatory cells in the immune system of the CNS.
Chemokines are a family of molecules associated with the trafficking of leukocytes in normal immune surveillance and recruitment of inflammatory cells in host defense (Park et al. 2004). Among the chemokines, interleukin-8 (IL-8) is a member of CXC chemokines and important mediators of the inflammatory response to many stimuli, including microbe infections. IL-8 has multiple biological functions in inflammatory responses, such as chemoattraction of a variety of cells, angiogenesis of endothelial cells, and blood–brain barrier dysfunction (Kossmann et al. 1997; Lane et al. 2002). IL-8 was expressed in various cells, monocytes, lymphocytes, neutrophils, and epithelial cells (van Eeden and Terashima 2000; Jung et al. 2002; Kim et al. 2006).
An innate immune response to viral and bacterial infection often results in the production of immune molecules, including cytokines, chemokines, major histocompatibility complex, and enzymes that act in concert to control the infectious agents (Palma et al. 2003; Kwon et al. 2004). N. fowleri has developed mechanisms to evade the host immune system. There are many reports to investigate pathogenesis and immune responses caused by N. fowleri, such as heat-shock protein, IgA antibody response, innate immunity, humoral immunity, the complement system, neutrophils, macrophages, and cell-mediated immunity (Rivera-Aguilar et al. 2000; Marciano-Cabral and Cabral 2007; Song et al. 2007). Recently, Cervantes-Sandoval et al. (2009) reported that N. fowleri induces the expression of host innate defense mechanisms, such as mucin secretion (MUC5AC) and local inflammation (IL-8 and IL-1β) in respiratory epithelial cells.
In the present study, we have examined chemokine gene activation in human astroglial cells following treatment with N. fowleri lysates. We demonstrated that treatment of N. fowleri lysates on human astroglial cells leads to the activation of activator protein-1 (AP-1) and subsequent expression of IL-8 which are dependent on extracellular signal-regulated kinase (ERK) activation.
Materials and methods
Cultivation of N. fowleri and preparation of N. fowleri lysate
N. fowleri (Carter NF69 strain, ATCC#30215) were cultured under axenic conditions in Nelson’s medium at 37°C, as previously described (Willaert 1971). Harvested N. fowleri trophozoites were suspended in 200 μl of phosphate-buffered saline (PBS; pH 7.4; 137 mM NaCl, 2.7 mM KCl, 10 mM Na2HPO4, 1.8 mM KH2PO4) and solubilized by the freeze–thaw method and filtered using the syringe filter to obtain lysates. Protein content from cellular extracts was determined by Bradford method (Bradford 1976).
Cell culture and reagents
CRT-MG human astrocytoma cells were maintained in 10 % FBS (Gibco/BRL, Gaithersburg, MD, USA)-RPMI 1640 (Gibco/BRL) medium with 10 mM HEPES (pH 7.2) and 1 mM Earle’s balanced salt solution supplemented with 2 mM l-glutamine, 100 U/ml of penicillin, and 100 μg/ml of streptomycin. For experiments, 2 × 105 cells were prepared per well in 6-well plates. The mitogen-activated protein kinase kinase (MEK)/ERK inhibitor (U0126) and a negative chemical control of U0126 (U0124) were purchased from Calbiochem (San Diego, CA, USA).
RNase protection assay
Cells were washed with ice-cold PBS, and then RNA was isolated as previously described (Kwon et al. 2004). RNase protection assay (RPA) was used to determine the expression levels of various chemokines mRNA, using the RiboQuant multiprobe (hCK-5) system (Pharmingen, San Diego, CA, USA). The probe set was transcribed with T7 RNA polymerase, hybridized overnight, and then analyzed according to the manufacturer’s instructions. Values for mRNA levels were normalized to those for GAPDH mRNA levels for each experimental condition.
Western blot
Protein was extracted by RIPA buffer (25 mM Tris–HCl, pH 7.6, 1 % Triton X-100, 150 mM NaCl, 0.1 % sodium dodecyl sulfate (SDS), 1 % sodium deoxycholate) and centrifuged to remove cell debris. The resulting supernatant was quantified using the Bradford method (Bradford 1976). Fifty micrograms of protein was then loaded onto 12 % Tris–HCl SDS–polyacrylamide gel electrophoresis (PAGE) and transferred to a nitrocellulose transfer membrane (GE Healthcare, Buckinghamshire, UK). ERK or phospho-ERK were determined using anti-ERK or phospho-ERK monoclonal antibodies (Cell Signaling, Beverly, MA, USA) diluted 1:500, and anti-mouse rabbit antibody (Cell Signaling) was used as a secondary antibody. Proteins were visualized using the ECL technique (GE Healthcare).
Electrophoretic mobility shift assay
Nuclear extracts from CRT-MG cells incubated with N. fowleri lysates were prepared as previously described (Kwon et al. 2004). The nuclei were pelleted at 3,000×g for 10 min and resuspended in 200 μl of high salt buffer (10 mM HEPES, pH 7.9, 1 mM MgCl2, 10 mM KCl, 0.1 mM EDTA, 400 mM NaCl, 15 % glycerol, 1 mM dithiothreitol (DTT), 0.4 mM phenylmethylsulfonyl fluoride, 1 mM sodium fluoride, 10 μg/ml aprotinin, 10 μg/ml leupeptin, and 1 mM sodium orthovanadate). The suspension was rocked gently for 30 min at 4°C followed by microcentrifugation at 12,000×g for 10 min at 4°C. The protein concentration in the supernatant was determined with the Bradford method. Double-stranded oligonucleotides containing consensus AP-1 sequences (Santa Cruz, Santa Cruz, CA, USA) were used in the electrophoretic mobility shift assay (EMSA). Oligonucleotides were end-labeled with [γ-32P] ATP (Dupont-NEN, Boston, MA, USA) using T4 polynucleotide kinase. Typically, 10 μg of nuclear extracts was equilibrated for 15 min in binding buffer (10 mM Tris–HCl, pH 8.0, 75 mM KCl, 2.5 mM MgCl2, 0.1 mM EDTA, 10 % glycerol, 0.25 mM DTT) and 1 μg of poly-dI/dC (Amersham Pharmacia Biotech, Piscataway, NJ, USA). 32P-labeled oligonucleotide probe (20,000 cpm) was added to the extracts and incubated for an additional 20 min at 4°C. Bound and unbound probes were then separated by electrophoresis on a 5 % native polyacrylamide gel.
ELISA
The levels of IL-8 secreted by human astroglial cells after treatment of N. fowleri lysates were assessed using ELISA kits (BD-Pharmingen, San Diego, CA, USA). Supernatants from human astroglial cell cultures treated with N. fowleri lysate were measured for the levels of IL-8 production.
Statistical analysis
Data are presented as mean ± SD. Levels of significance for comparisons between samples were determined using Student’s t test distribution. Statistical analyses between more than three samples were performed by ANOVA with Tukey’s honest significant difference post hoc test applied to significant main effects or interactions (SPSS 12.0 K for Windows, SPSS, Chicago, IL, USA).
Results and discussion
To investigate the mechanisms involved in the inflammatory responses with N. fowleri lysates, we treated N. fowleri lysates to CRT-MG cells, human astroglial cells. Treatment with 1–1.5 mg/ml of N. fowleri lysates induced ~60 % of cell death by CRT-MG cells, while 0.5 mg/ml of N. fowleri lysates induced ~30 % of cell death (Fig. 1). We hypothesized that N. fowleri lysates might be provoked inflammatory response in human astroglial cells. Previously, we have demonstrated that human viruses induced pro-inflammatory gene expression such as monocyte chemoattractant protein-1 and IL-8 by human astroglial cells (Kwon et al. 2004).
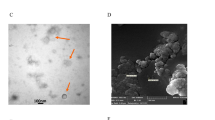
N. fowleri lysates induce cell death in human astroglial cells. a Light microscopic image of N. fowleri trophozoites (×200) and SDS–PAGE pattern of N. fowleri lysates (M molecular size marker, lysate N. fowleri lysates). b Human CRT-MG cells were treated with N. fowleri lysates (0–1.5 mg/ml) for 24 h, and cell death was measured after staining with Annexin V-FITC and PI
Among various pro-inflammatory chemokines, we analyzed IL-8 gene expression since IL-8 is one of the most important pro-inflammatory factors in human infectious diseases. We treated with N. fowleri lysates for varying (0–12 h) time periods in CRT-MG cells. RPA analysis showed that N. fowleri lysates strongly induced mRNA expression of IL-8 in CRT-MG cells (Fig. 2a). ELISA analysis showed that consistent with mRNA results, N. fowleri lysates enhanced IL-8 protein expression in CRT-MG cells (Fig. 2b). These results clearly indicated that N. fowleri induces IL-8 expression in mRNA and protein level.
N. fowleri lysates induce IL-8 expression in human astroglial cells. a CRT-MG cells were incubated with N. fowleri lysates (250 μg/ml) for varying (0–12 h) time periods, and total RNA was examined for IL-8 mRNA expression by RPA. Fold induction of mRNA was normalized to the level of GAPDH mRNA expression. Data shown are representative of three independent experiments. b CRT-MG cells were incubated with N. fowleri lysates (250 μg/ml) for 24 h, and then IL-8 protein expression in the culture supernatants was analyzed with ELISA. *P < 0.0001
To assess the mechanisms involved in the induction of IL-8 gene by N. fowleri lysates treatment, we investigated the involvement of mitogen-activated protein kinases (MAPKs). CRT-MG cells were treated with N. fowleri lysates for varying (0–12 h) time periods. Western blot analysis indicated that ERK was activated as early as 0.5–1 h after N. fowleri lysates treatment. Activation of ERK was persisted at 12 h (Fig. 3a). We further investigated whether AP-1, a well-known transcription factor, was also activated with treatment of N. fowleri lysates. EMSA clearly showed that DNA binding activity of AP-1 was markedly increased upon N. fowleri lysates treatment in a time-dependent manner (2–8 h) and increased activity gradually returned to basal levels by 12 h (Fig. 3b). We next investigated whether N. fowleri-mediated ERK activation is necessary for N. fowleri-mediated AP-1 activation in CRT-MG cells by using a pharmacological MEK inhibitor, U0126. Pre-treatment of U0126 for 1 h blocked N. fowleri-mediated AP-1 activation in CRT-MG cells, suggesting that activation of ERK is required for N. fowleri-mediated AP-1 activation (Fig. 3c).
N. fowleri lysates induce the activation of ERK and AP-1 in human astroglial cells. a CRT-MG cells were treated with N. fowleri lysates (250 μg/ml) for varying (0–12 h) time periods. Activation of ERK was examined by the level of phosphorylation with western blot. Total ERK was assessed as internal controls for protein concentrations loaded. b CRT-MG cells were incubated with N. fowleri lysates (250 μg/ml) for varying (0–12 h) time periods. Nuclear AP-1 binding activity was analyzed by EMSA using the human consensus AP-1 probe. c CRT-MG cells were pre-incubated with MEK inhibitor, U0126 (10 μM), for 1 h, and then the cells were treated with N. fowleri lysates (250 μg/ml) for 4 h. Nuclear AP-1 binding activity was analyzed by EMSA using the human consensus AP-1 probe. U0124 (10 μM) was used for the negative control against U0126. Data shown are representative of three independent experiments
We next examined whether N. fowleri-mediated ERK activation is necessary for inducing of IL-8 expression in human astroglial cells. Pre-treatment with U0126 for 1 h blocked N. fowleri-induced IL-8 mRNA expression in a dose-dependent manner (Fig. 4a). Also ELISA analysis showed that pre-treatment with U0126 for 1 h blocked N. fowleri-induced IL-8 protein expression, while pre-incubation with U0124, a negative chemical control of U0126, had no effect on N. fowleri-induced IL-8 expression (Fig. 4a, b). The results collectively suggest that N. fowleri-induced IL-8 expression requires activation of ERK in human astroglial cells.
Inhibition of ERK activation abrogates N. fowleri-mediated IL-8 induction. a CRT-MG cells were pre-incubated with three different concentrations (0.1, 1, 10 μM) of MEK inhibitor, U0126, for 1 h, and then the cells were treated with N. fowleri lysates (250 μg/ml) for 12 h. The expression of IL-8 mRNA was measured by RPA. Data shown are representative of three independent experiments. b CRT-MG cells were pre-incubated with U0126 (10 μM) for 1 h, and then the cells were treated with N. fowleri lysates (250 μg/ml) for 24 h. IL-8 protein expression was measured by ELISA analysis
To understand the pathogenic mechanisms involved in the initiation of inflammatory responses in the CNS with N. fowleri lysates, chemokine production in human astroglial cells was analyzed upon treatment with N. fowleri. Our results demonstrated that IL-8 is activated in human astroglial cells by treatment of N. fowleri lysates. Recent studies show that human astroglial cells produce IL-8 following infection with HIV-1, or picornavirus (Kutsch et al. 2000; Kwon et al. 2004). MAPKs are regarded as important signal mediators for IL-8 expression in various cell types and stimuli. HIV-1 induces IL-8 expression in human astrocyte cells through activation of ERK, Jun NH2-terminal kinases, and p38 MAPK (Zheng et al. 2008), and Coronavirus induces IL-8 expression in human lung epithelial cell via MAPK and AP-1 activation (Chang et al. 2004). In this study, we demonstrated that N. fowleri lysates induced activates the ERK pathway and that inhibition of ERK activation blocks N. fowleri-induced IL-8 expression in human astroglial cells. The 5′ flanking region of the IL-8 gene contains binding sites for AP-1 (Iguchi et al. 2000; Chang et al. 2004). We showed that inhibition of ERK activation blocks N. fowleri-induced activity of AP-1, suggesting that activation of ERK plays an essential role in N. fowleri-mediated AP-1 activation and subsequent IL-8 expression in human astroglial cells. However, it remains unclear how the ERK-1/2 activation pathway is associated with IL-8 gene expression.
It is interesting to note that IL-8 is a potent chemoattractant and activator of neutrophils, basophils, monocytes, and endothelial cells (van Eeden and Terashima 2000; Kim et al. 2006; Stillie et al. 2009). This chemokine appears to play a major role in the early defense against infectious diseases (Jeyaseelan et al. 2005; Cortez et al. 2006). These chemokines have also been found in various inflammatory responses and at the sites of inflammatory diseases (Kossmann et al. 1997; Polyak et al. 2001; Stillie et al. 2009). N. fowleri enters the CNS through the nasal cavity and the olfactory apparatus (Brown 1979; Rojas-Hernández et al. 2004). Of the two neurogenic regions in the CNS, the subventricular zone generates by new neurons, and these are destined for the olfactory bulb (Garcia-Verdugo et al. 1998; Luskin 1998). These multipotent precursors with similarities to astrocytes contribute to adult neurogenesis in olfactory bulb (Laywell et al. 2000). Astrocytes play an important role in immune regulation, acting as a source of chemokines, cytokines, and adhesion molecules in the immune system. In this study, we observed that IL-8 appears to play a major role in the expansion of inflammatory responses of astrocytes against N. fowleri lysates. In previous work, we observed that microglial cells co-cultured with N. fowleri trophozoites secreted the pro-inflammatory cytokines, tumor necrosis factor-alpha, IL-1β, and IL-6 (Oh et al. 2005). Collectively, N. fowleri infection induces chemokine and cytokines expression in the CNS. Although PAM is a rapidly fatal disease of CNS and the immune response of CNS against N. fowleri trophozoites infection remains incompletely understood, it is thought that our findings may help understand the N. fowleri-mediated upregulation of chemokine and cytokine expression in the astroglial cells.
References
Bradford MM (1976) A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal Biochem 7:248–254
Brown T (1979) Observations by immunofluorescence microscopy and electron microscopy on the cytopathogenicity of Naegleria fowleri in mouse embryo-cell cultures. J Med Microbiol 12:363–371
Carter RF (1970) Description of Naegleria sp. isolated from two cases of primary amoebic meningoencephalitis, and the experimental pathological changes induced by it. J Pathol 100:217–244
Cervantes-Sandoval I, Serrano-Luna JdJ, Meza-Cervantez P, Arroyo R, Tsutsumi V, Shibayama M (2009) Naegleria fowleri induces MUC5AC and pro-inflammatory cytokines in human epithelial cells via ROS production and EGFR activation. Microbiology 155:3739–3747
Chang YJ, Liu CY, Chiang BL, Chao YC, Chen CC (2004) Induction of IL-8 release in lung cells via activator protein-1 by recombinant baculovirus displaying severe acute respiratory syndrome-coronavirus spike proteins: identification of two functional regions. J Immunol 173:7602–7614
Cortez KJ, Lyman CA, Kottilil S, Kim HS, Roilides E, Yang J, Fullmer B, Lempicki R, Walsh TJ (2006) Functional genomics of innate host defense molecules in normal human monocytes in response to Aspergillus fumigatus. Infect Immun 74:2353–2365
Culbertson CG (1971) The pathogenicity of soil amebas. Annu Rev Microbiol 25:231–254
Dong Y, Benveniste EN (2001) Immune function of astrocytes. Glia 36:180–190
Garcia-Verdugo JM, Doetsch F, Wichterle H, Lim DA, Alvarez-Buylla A (1998) Architecture and cell types of the adult subventricular zone: in search of the stem cells. J Neurobiol 36:234–248
Herbst R, Ott C, Jacobs T, Marti T, Marciano-Cabral F, Leippe M (2002) Pore-forming polypeptides of the pathogenic protozoon Naegleria fowleri. J Biol Chem 277:22353–22360
Iguchi A, Kitajima I, Yamakuchi M, Ueno S, Aikou T, Kubo T, Matsushima K, Mukaida N, Maruyama I (2000) PEA3 and AP-1 are required for constitutive IL-8 gene expression in hepatoma cells. Biochem Biophys Res Commun 279:166–171
Jeyaseelan S, Manzer R, Young SK, Yamamoto M, Akira S, Mason RJ, Worthen GS (2005) Toll-IL-1 receptor domain-containing adaptor protein is critical for early lung immune responses against Escherichia coli lipopolysaccharide and viable Escherichia coli. J Immunol 175:7484–7495
John DT (1982) Primary amebic meningoencephalitis and the biology of Naegleria fowleri. Annu Rev Microbiol 36:101–123
Jung YD, Fan F, McConkey DJ, Jean ME, Liu W, Reinmuth N, Stoeltzing O, Ahmad SA, Parikh AA, Mukaida N, Ellis LM (2002) Role of P38 MAPK, AP-1, and NF-kappaB in interleukin-1beta-induced IL-8 expression in human vascular smooth muscle cells. Cytokine 18:206–213
Kim YM, Reed W, Wu W, Bromberg PA, Graves LM, Samet JM (2006) Zn2+-induced IL-8 expression involves AP-1, JNK, and ERK activities in human airway epithelial cells. Am J Physiol Lung Cell Mol Physiol 290:L1028–L1035
Kossmann T, Stahel PF, Lenzlinger PM, Redl H, Dubs RW, Trentz O, Schlag G, Morganti-Kossmann MC (1997) Interleukin-8 released into the cerebrospinal fluid after brain injury is associated with blood–brain barrier dysfunction and nerve growth factor production. J Cereb Blood Flow Metab 17:280–289
Kutsch O, Oh J, Nath A, Benveniste EN (2000) Induction of the chemokines interleukin-8 and IP-10 by human immunodeficiency virus type 1 tat in astrocytes. J Virol 74:9214–9221
Kwon D, Fuller AC, Palma JP, Choi IH, Kim BS (2004) Induction of chemokines in human astrocytes by picornavirus infection requires activation of both AP-1 and NF-kappa B. Glia 45:287–296
Lane BR, Liu J, Bock PJ, Schols D, Coffey MJ, Strieter RM, Polverini PJ, Markovitz DM (2002) Interleukin-8 and growth-regulated oncogene alpha mediate angiogenesis in Kaposi’s sarcoma. J Virol 76:11570–11583
Laywell ED, Rakic P, Kukekov VG, Holland EC, Steindler DA (2000) Identification of a multipotent astrocytic stem cell in the immature and adult mouse brain. Proc Natl Acad Sci U S A 97:13883–13888
Luskin MB (1998) Neuroblasts of the postnatal mammalian forebrain: their phenotype and fate. J Neurobiol 36:221–233
Ma P, Visvesvara GS, Martinez AJ, Theodore FH, Gaggett PM, Sawyer TK (1990) Naegleria and Acanthamoeba infections: review. Rev Infect Dis 12:490–513
Marciano-Cabral F (1988) Biology of Naegleria spp. Microbiol Rev 52:114–133
Marciano-Cabral F, Cabral GA (2007) The immune response to Naegleria fowleri amoebae and pathogenesis of infection. FEMS Immunol Med Microbiol 51:243–259
Martinez AJ, Visvesvara GS (1997) Free-living, amphizoic and opportunistic amebas. Brain Pathol 7:583–598
Oh YH, Jeong SR, Kim JH, Song KJ, Kim K, Park S, Sohn S, Shin HJ (2005) Cytopathic changes and pro-inflammatory cytokines induced by Naegleria fowleri trophozoites in rat microglial cells and protective effects of an anti-Nfa1 antibody. Parasite Immunol 27:453–459
Palma JP, Kwon D, Clipstone NA, Kim BS (2003) Infection with Theiler’s murine encephalomyelitis virus directly induces proinflammatory cytokines in primary astrocytes via NF-kappaB activation: potential role for the initiation of demyelinating disease. J Virol 77:6322–6331
Park J, Choi K, Jeong E, Kwon D, Benveniste EN, Choi C (2004) Reactive oxygen species mediate chloroquine-induced expression of chemokines by human astroglial cells. Glia 47:9–20
Polyak SJ, Khabar KS, Rezeiq M, Gretch DR (2001) Elevated levels of interleukin-8 in serum are associated with hepatitis C virus infection and resistance to interferon therapy. J Virol 75:6209–6211
Rivera-Aguilar V, Hernández-Martínez D, Rojas-Hernández S, Oliver-Aguillón G, Tsutsumi V, Herrera-González N, Campos-Rodríguez R (2000) Immunoblot analysis of IgA antibodies to Naegleria fowleri in human saliva and serum. Parasitol Res 86:775–780
Rojas-Hernández S, Jarillo-Luna A, Rodríguez-Monroy M, Moreno-Fierros L, Campos-Rodríguez R (2004) Immunohistochemical characterization of the initial stages of Naegleria fowleri meningoencephalitis in mice. Parasitol Res 94:31–36
Schuster FL, Visvesvara GS (2004) Free-living amoebae as opportunistic and non-opportunistic pathogens of humans and animals. Int J Parasitol 34:1001–1027
Song KJ, Song KH, Na BK, Kim JH, Kwon D, Park S, Pak JH, Im KI, Shin HJ (2007) Molecular cloning and characterization of a cytosolic heat shock protein 70 from Naegleria fowleri. Parasitol Res 100:1083–1089
Stillie R, Farooq SM, Gordon JR, Stadnyk AW (2009) The functional significance behind expressing two IL-8 receptor types on PMN. J Leukoc Biol 86:529–543
van Eeden SF, Terashima T (2000) Interleukin 8 (IL-8) and the release of leukocytes from the bone marrow. Leuk Lymphoma 37:259–271
Willaert E (1971) Isolation and in vitro culture of the amoeba of the genus Naegleria. Ann Soc Belges Med Trop Parasitol Mycol 51:701–708
Zheng JC, Huang Y, Tang K, Cui M, Niemann D, Lopez A, Morgello S, Chen S (2008) HIV-1-infected and/or immune-activated macrophages regulate astrocyte CXCL8 production through IL-1beta and TNF-alpha: involvement of mitogen-activated protein kinases and protein kinase R. J Neuroimmunol 200:100–110
Acknowledgments
This study was supported by a grant (no. R01-2005-000-10118-0) from the Basic Research Program of the Korea Science & Engineering Foundation.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Kim, JH., Sohn, HJ., Lee, SH. et al. Induction of interleukin-8 by Naegleria fowleri lysates requires activation of extracellular signal-regulated kinase in human astroglial cells. Parasitol Res 111, 587–592 (2012). https://doi.org/10.1007/s00436-012-2872-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00436-012-2872-3