Abstract
Background
Over the last two decades, the scale-up of vector control and changes in the first-line anti-malarial, from chloroquine (CQ) to sulfadoxine-pyrimethamine (SP) and then to artemether-lumefantrine (AL), have resulted in significant decreases in malaria burden in western Kenya. This study evaluated the long-term effects of control interventions on molecular markers of Plasmodium falciparum drug resistance using parasites obtained from humans and mosquitoes at discrete time points.
Methods
Dried blood spot samples collected in 2012 and 2017 community surveys in Asembo, Kenya were genotyped by Sanger sequencing for markers associated with resistance to SP (Pfdhfr, Pfdhps), CQ, AQ, lumefantrine (Pfcrt, Pfmdr1) and artemisinin (Pfk13). Temporal trends in the prevalence of these markers, including data from 2012 to 2017 as well as published data from 1996, 2001, 2007 from same area, were analysed. The same markers from mosquito oocysts collected in 2012 were compared with results from human blood samples.
Results
The prevalence of SP dhfr/dhps quintuple mutant haplotype C50I51R59N108I164/S436G437E540A581A613 increased from 19.7% in 1996 to 86.0% in 2012, while an increase in the sextuple mutant haplotype C50I51R59N108I164/H436G437E540A581A613 containing Pfdhps-436H was found from 10.5% in 2012 to 34.6% in 2017. Resistant Pfcrt-76 T declined from 94.6% in 2007 to 18.3% in 2012 and 0.9% in 2017. Mutant Pfmdr1-86Y decreased across years from 74.8% in 1996 to zero in 2017, mutant Pfmdr1-184F and wild Pfmdr1-D1246 increased from 17.9% to 58.9% in 2007 to 55.9% and 90.1% in 2017, respectively. Pfmdr1 haplotype N86F184S1034N1042D1246 increased from 11.0% in 2007 to 49.6% in 2017. No resistant mutations in Pfk13 were found. Prevalence of Pfdhps-436H was lower while prevalence of Pfcrt-76 T was higher in mosquitoes than in human blood samples.
Conclusion
This study showed an increased prevalence of dhfr/dhps resistant markers over 20 years with the emergence of Pfdhps-436H mutant a decade ago in Asembo. The reversal of Pfcrt from CQ-resistant to CQ-sensitive genotype occurred following 19 years of CQ withdrawal. No Pfk13 markers associated with artemisinin resistance were detected, but the increased haplotype of Pfmdr1 N86F184S1034N1042D1246 was observed. The differences in prevalence of Pfdhps-436H and Pfcrt-76 T SNPs between two hosts and the role of mosquitoes in the transmission of drug resistant parasites require further investigation.
Similar content being viewed by others
Background
Over the last two decades, increased malaria control efforts have saved millions of lives globally and reduced malaria mortality in Africa by 44.0% [1]. Like other malaria endemic areas, malaria control has significantly decreased malaria morbidity and all-cause mortality in western Kenya [1, 2] by increasing access to effective anti-malarial treatment and scale-up of long-lasting insecticide-treated nets (LLINs) [2]. However, progress is threatened by the potential emergence and spread of anti-malarial drug resistance.
In Kenya, Ministry of Health guidelines for the treatment of malaria have changed in response to the spread of drug resistant parasites. Due to widespread CQ resistance, sulfadoxine-pyrimethamine (SP) replaced chloroquine (CQ) as first-line treatment for uncomplicated malaria in 1998. However, resistance to SP rapidly developed and in 2004, artemether-lumefantrine (AL), an artemisinin-based combination therapy (ACT), was recommended as the first-line anti-malarial for uncomplicated malaria [3]. Because of AL supply shortage, amodiaquine (AQ) was temporarily used as first-line treatment between 2004 and 2006 [4]. SP remains the drug of choice for intermittent preventive treatment in pregnancy (IPTp), which has been widely implemented in western Kenya [5].
In Asembo, Siaya County, western Kenya, malaria vector control started in 1997 with a large-scale trial of insecticide-treated nets (ITNs). Nationally, ITNs were initially distributed to pregnant women and children through social marketing schemes. In 2006, the first mass distribution campaign of long-lasting insecticidal nets (LLINs) was implemented to target children under 5 years of age and pregnant women. Subsequent mass campaigns in 2011 and 2014 targeted all age groups to achieve universal coverage. The scale-up of ITNs was associated with changes in the predominant mosquito species with substantial reductions in Anopheles gambiae sensu stricto (s.s.) and Anopheles funestus that resulted in a predominance of Anopheles arabiensis [6]. However, An. funestus has resurged and became the predominant species since 2010 in the Asembo area [7]. It is unknown whether the temporal changes in mosquito vector species influenced the spread of drug resistant parasites in mosquito populations in addition to anti-malarial drug pressures in humans in this area.
Molecular surveillance is essential to detect trends in known drug-resistant mutations as well as emerging mutations. Single nucleotide polymorphisms (SNPs) in the genes for dihydrofolate reductase (DHFR) and dihydropteroate synthase (DHPS) are known to cause resistance to SP. Triple mutations of Pfdhfr 51I, 59R, and 108 N combined with double mutations of Pfdhps 437G and 540E (a quintuple set of mutations) are strongly associated with SP treatment failure [8], and a high prevalence of sextuple-mutant parasites containing the 581G mutation (Pfdhfr I51R59N108 and Pfdhps G437E540G581) has been associated with reduced IPTp-SP efficacy in sub-Saharan Africa [9]. Plasmodium falciparum chloroquine resistance transporter gene (Pfcrt) 76 T and multi-drug resistant gene 1 (Pfmdr1) 86Y are key molecular markers associated with the emergence and spread of resistance to CQ and AQ [10, 11]. In the Greater Mekong Subregion, multiple SNP mutations in the Kelch 13 gene (Pfk13) are associated with resistance to artemisinin, the drug currently used widely in ACTs [12,13,14]. In Africa, the selection of wild type Pfmdr1-N86 and the haplotype N86F184D1246 by ACT partner drug, lumefantrine, has been documented [15, 16] with a possible association with reduced susceptibility to treatment [15, 17, 18]. More recent reports show that artemisinin resistant mutation Pfk13 R561H in Rwanda and Pfk13 A675V and C469Y in Uganda are associated with delayed clearance of malaria parasites [19, 20].
The spread of resistant parasites also depends on non-drug pressure factors, including immune clearance in human host, multiplicity of infection, fitness cost in both human and vector, vector species, genetic recombination, and mid-gut microbiota in mosquitoes [21,22,23]. Previous studies conducted in different transmission settings have suggested that selection of some drug-resistant molecular markers in malaria parasites may occur during transmission by mosquitoes [24,25,26]. Different drug-resistant mutations of parasites selected in humans and mosquitoes have been reported in some studies [25, 26] while similar molecular resistant profiles of Pfdhfr, Pfdhps, Pfk13, Pfcrt, Pfmdr1 between human and mosquito populations were found in others [27, 28]. The different results from different malaria endemic areas warranted the examination of whether profiles of molecular markers of parasite drug resistance in mosquitoes differ from those in human blood in this high transmission area of western Kenya.
To evaluate the impact of malaria control on drug-resistant markers in the Asembo area of western Kenya, samples from community cross-sectional surveys in 1996, 2001, and 2007 were previously tested for molecular markers of resistance [29, 30]. Those studies showed that the prevalence of molecular markers of resistance to CQ and SP continued to increase even after withdrawal of these drugs as first-line treatment and with the sustained use of ITNs in western Kenya [30]. The present study extends these observations to include survey samples from 2012 to 2017 by testing the resistance markers associated with previously and currently used anti-malarial drugs to further evaluate the temporal trends in these drug-resistance markers between 1996 and 2017. This study also compares the prevalence of molecular markers of drug resistance between P. falciparum parasites isolated from mosquito oocysts and from human blood samples collected in 2012.
Methods
Ethics statement
This study was approved by the Ethical Review Committee of KEMRI, Nairobi, Kenya, the Institutional Review Board of Michigan State University, East Lansing, Michigan, and the Institutional Review Board of the Centers for Disease Control and Prevention (CDC), Atlanta, USA.
Study area and sample collection
This study was part of a series of community-based household surveys to evaluate the impact of malaria control interventions within the Kenya Medical Research Institute and Centers for Disease Control and Prevention (KEMRI/CDC) Health and Demographic Surveillance System (HDSS) in Asembo, Siaya County, western Kenya [31]. Surveys carried out in 2012 and 2017 utilized systematic random selection of households to estimate population representative prevalence. Among households selected, all individuals above 1 months of age were eligible for inclusion. Dried blood spot (DBS) from smear-positive participants between June and August from the survey in 2012 (N = 225) and between June and September in the 2017 survey (N = 121) were used for this parasite genotyping study.
Mosquitoes were collected using prokopack aspiration of indoor resting mosquitoes [32] from May to September in 2012 in a single village in the Asembo area. Approximately 20 houses were sampled each morning from 7 to 11 am. Collections were done 5 days during one week each month with collectors using prokopack aspirators to capture mosquitoes resting on the walls, the roof, under furniture and from hangings within the house. Collectors spent 15–20 min in each house before moving to a new house. Houses were selected non-randomly with the aim to maximize mosquito collections but efforts were made to ensure that all houses within the village were sampled at least once during the collection period.
Collected mosquitoes were transferred into adult mosquito cage (30 × 30× 30 cm) from where the fed, gravid and half gravid female anophelines were sorted out and held separately in paper cups while the rest were killed and discarded in the field. Fed, gravid and half gravid female mosquitoes collected from the field were returned to the KEMRI/CDC facilities in Kisian and held in the insectary, sustained with sugar solution. Blood fed and half-gravid mosquitoes were held for 6 to 8 daysbefore oocyst dissection, while gravid females were dissected after 4 days. The identified oocysts were preserved in absolute ethanol and stored at − 20 °C, then shipped to the CDC malaria lab in Atlanta for sequencing. Because the midgut was preserved in absolute ethanol, the midgut sample was dried on filter paper and transferred to a 1.5 ml tube and ground with a sterile blue Kontes pestle in lysis buffer before DNA extraction. Before dissection, mosquitoes were identified morphologically using the published keys for the Anophelinae of Africa [33]. Mosquitoes from the An. gambiae complex were further identified as An. gambiae s.s. or Anopheles arabiensis using the methods of Scott et al. [34].
DNA extraction
A whole spot (50 µl blood) from a DBS sample was cut from which DNA was extracted. Parasite genomic DNA from DBS samples was extracted using QIAamp® DNA Mini Kit (QIAGEN, Valencia, CA) and from the mosquito midguts using QIAmp DNA Micro kit following manufacturer’s instructions (QIAGEN). Extracted DNA samples were stored at − 20 °C until use.
Nested PCR amplification for Pfdhfr and Pfdhps genes
Nested PCR was used to amplify the Pfdhfr gene covering codons 51, 59, 108, and 164 and the Pfdhps gene covering codons 436, 437, 540, 581 and 613 for all blood and mosquito samples collected. Primers were designed using Primer3web (Github Inc, San Francisco, CA) and synthesized at the CDC Core Facility in Atlanta, GA. All primary and secondary PCRs were performed in a 25 µl reaction with Premixed 2 × PCR Master Mix (Promega Corporation, Madison, WI). For both of Pfdhfr and Pfdhps primary PCR, a 25 µl reaction contained 12.5 µl 2 × master mix, 1 µl (400 nM) each primer, 2 µl DNA template and 8.5 µl PCR-grade water. For secondary PCR, reaction system is the same except for template with 2 µl primary PCR products for both genes. After secondary PCRs, 1% agarose gel was prepared and gel electrophoreses were run for the amplification of sample PCR bands, and positive, negative and blank controls. The final PCR products of 542 bp and 675 bp of Pfdhfr and Pfdhps genes, respectively, were used for Sanger sequencing. The PCR primers and recycling conditions are shown in Additional file 1: Table S1.
Nested PCR amplification for Pfcrt, Pfmdr1 and Pfk13 genes
The primers and PCR conditions used for Pfcrt, Pfmdr1 and Pfk13 amplification were adapted from previously published work [35,36,37] (see Additional file 2: Table S2). For Pfmdr1 gene, the first fragment, covering codons 86 and184, was amplified using the same primers as shown in the publication [36]. The second fragment amplification covering codons 1034, 1042 and 1246 was modified by adding 2 internal primers (forward primer: 5ʹGCAATCGTTGGAGAAACAGG-3ʹ and reverse primer: 5ʹTTTTGCATTTTCTGAATCTCCTT-3ʹ) in the secondary PCR. Thus, the final secondary PCR products included a 298 bp amplicon covering codons 1034–1042 and a 414 bp amplicon covering codon 1246 were produced in the current study. After secondary PCR, 1% agarose gel was prepared and gel electrophoreses were run for the amplification of sample PCR bands, and positive, negative and blank controls.
Sanger sequencing of amplified drug-resistant genes
Nested PCR products were purified with ExoSAP (New England Biolabs, Ipswich, MA, USA). The cycling sequencing was carried out using Big Dye Terminator v3.1 cycle sequencing kit on Bio-Rad C1000 thermal cycler (Bio-Rad, Hercules, CA, USA). Dye terminators were cleaned by precipitating reactions with EDTA/NaOAc/Ethanol precipitation and rehydrating in 10 μl HiDi formamide. Capillary electrophoresis was performed in ABI 3730 or 3730xl genetic analyzer (Applied Biosystems, Foster City, USA). Sequence data were analysed using the Geneious Prime R10 and R11 (Biomatters, San Francisco, CA, USA). The mixed SNPs were identified where the minor peak was ≥ 30% of the major peak. SNPs at Pfdhfr, Pfdhps, Pfcrt, Pfmdr1 genes and Pfk13 propeller region were identified by comparing sequences with reference 3D7 strains from GenBank XM_001351443.1, Z30654.1, XM_001348968.1, XM_001351751 and MW712622.1), respectively. PCR reaction systems and cycling conditions were detailed in Additional files 1, 2.
Genetic definitions
As with previous studies [29, 30], all SNPs related to drug resistance molecular markers were classified as either wild, mutant or mixed. When calculating the prevalence and constructing haplotypes, mixed genotypes were considered as resistant mutant [30]. The Pfdhfr haplotypes in codons 50, 51, 59, 108 and 164 were classified as wild type, single, double, triple, and quadruple mutants. The Pfdhps haplotypes in codons 436, 437, 540, 581 and 613 were classified as wild type, single, double and triple haplotypes. The combined dhfr/dhps haplotypes (codons of Pfdhfr 50, 51, 59, 108, 164 and Pfdhps 436, 437, 540, 581, 613) were classified as wild type, single, double, triple, quadruple, quintuple and sextuple mutants. Pfcrt haplotypes based on codons 72, 73, 74, 75, 76 and Pfmdr1 haplotypes based on codons 86, 184, 1034, 1042, 1246 were also constructed. The SNPs in Pfk13 domain at nine codons 446, 458, 476, 493, 539, 543, 553, 561, 580 were assessed for the presence of mutations known to be associated with artemisinin resistance by the World Health Organization (WHO) 2018 standards [38].
Statistical analysis
Because age is not a confounding factor for the prevalence of drug-resistant molecular markers in our previous study [30], analyses of temporal trends between different sampling years were not adjusted for age in this study. The temporal trends in the prevalence of resistant markers were analysed using the exact version of the Cochran-Armitage test for trend. Differences in the prevalence of SNPs and haplotypes between mosquito and human samples in 2012 survey were assessed using Pearson Chi-square tests (exact version) and exact 95% confidence intervals (CIs) for the prevalence of SNPs and haplotypes in mosquitoes and human samples were also calculated. These statistical analyses were conducted using SAS v9.4. All statistical tests were two-tailed and statistical significance was defined as p < 0.05. Marginal differences were defined as 0.05 ≤ p < 0.10. The prevalence of SNPs and haplotypes were not adjusted for sampling weights.
Results
Prevalence of Pfdhfr and Pfdhps resistant SNPs and haplotypes in 2012 and 2017 surveys
The prevalence of SP resistance mutations at Pfdhfr-51I, -59R, -108 N and Pfdhps-437G, -540E approached fixation (96.4–100%) with no significant differences in frequencies observed between 2012 and 2017 (Table 1), while the prevalence of the Pfdhps-436H mutation increased significantly from 10.5% in 2012 to 34.6% in 2017 (p = 0.001). In contrast, the Pfdhfr-164L mutation which was detected previously in a cotrimoxazole prophylaxis study in the Kisumu region of western Kenya [39] and the Pfdhps-581G mutation which was reported in patients registered at the outpatient clinic of New Nyanza Provincial Hospital, Kisumu, Kenya [40], were observed in only two samples in the 2012 survey (0.9% and 1.0%, respectively) and none in 2017 in the Asembo area (Table 1). There was no Pfdhfr-164L mutation found in Asembo in 1996, 2001, or 2007 [29, 30] and no Pfdhps-581G mutation found in 2007 [30] (codon Pfdhps-581 was not tested in the 1996 & 2001 surveys). Comparison of mutant haplotypes between 2012 and 2017 showed no significant increase in the prevalence of all haplotypes but a significant increase in Pfdhps triple mutants (H436G437E540A581A613), reflecting the increase in the Pfdhps-436H mutation (p = 0.001). In parallel, the prevalence of the combined haplotype of dhfr/dhps sextuple mutant C50I51R59N108I164/H436G437E540A581A613 containing Pfdhps-436H was 10.5% in 2012 and 34.6% in 2017 (p = 0.001, Table 1).
Temporal trend in the prevalence of dhfr/dhps haplotypes from 1996 to 2017
The prevalence of combined dhfr/dhps double, triple, and quadruple mutant haplotypes decreased significantly over time (all haplotypes p < 0.01), reflecting initially the increasing prevalence of the combined dhfr/dhps quintuple mutant haplotype (C50I51R59N108I164/S436G437E540 A581A613) from 19.7% in 1996 to 85.2% in 2012 (p < 0.01, Fig. 1). The prevalence of the quintuple mutant then declined slightly to 59.8% in 2017 as sextuple mutants increased. There was no Pfdhps-436H mutation found in 1996, 2001 and 2007 surveys in Asembo [29, 30]. The prevalence of sextuple mutant haplotypes in 2012 was 12.4% including 4 different sextuple haplotypes (Table 1). Of the four sextuple haplotypes, the haplotype C50I51R59N108I164/H436G437E540 A581A613 containing Pfdhps-436H appeared in 2012 and became the most common sextuple haplotype accounting for 10.5% in 2012 (Sextuple1, green bar in Fig. 1). This haplotype increased to 34.6% in 2017 (p < 0.01, green bar in Fig. 1 and Table 1).
Prevalence of Pfcrt and Pfmdr1 resistant SNPs and haplotypes in the 2012 and 2017 surveys
In 2012, the prevalence of Pfcrt SNPs was 17.3% for mutant Pfcrt-74I and 18.3% for both Pfcrt-75D/E and -76 T (Table 2). The prevalence of all three SNPs significantly decreased to 0.9% in 2017 (p = 0.001, Table 2). There were no mutations at codons 72 and 73 in either the 2012 or the 2017 samples. The prevalence of CQ-sensitive Pfcrt-K76 increased from 81.7% 2012 to 99.1% in 2017 (p = 0.001). Similarly, the wild haplotype C72V73M74N75K76 (CVMNK) also increased from 81.7% in 2012 to 99.1% in 2017 (p = 0.001), while the mutant haplotype C72V73I74E75T76 (CVIET) decreased from 10.6% to 0.9% (1/110) (p = 0.003), and the mutant haplotype C72V73I74D75T76 (CVIDT) from 6.7% to 0.0% (p = 0.013).
The prevalence of mutant SNPs Pfmdr1-86Y,-184F, and -1246Y was 10.2%, 52.2% and 13.6%, respectively in 2012, and zero, 55.9% and 9.9%, respectively in 2017 (Table 2) with a significant decline of Pfmdr1-86Y in 2017 (p = 0.001). No samples carried mutations for Pfmdr1-1034 or Pfmdr1-1042 in either the 2012 or the 2017 samples. There were no statistically significant differences in the prevalence of wild haplotype N86Y184S1034N1042D1246 (NYSND) or the major mutant haplotype N86F184S1034N1042D1246 (NFSND) between 2012 and 2017 (Table 2). However, the prevalence of mutant haplotypes Y86Y184S1034N1042Y1246 (YYSNY) decreased significantly (p = 0.043) and Y86F184S1034N1042D1246 (YFSND) marginally (p = 0.055).
Temporal trend in prevalence of Pfcrt and Pfmdr1 SNPs and haplotypes from 1996 to 2017
Since previous studies using samples from the 1996 and 2001 surveys by this research group in the same area only tested the key markers of Pfcrt K76T and Pfmdr1 N86Y by real-time PCR [30], these were the only SNPs evaluated in the temporal trends from 1996 to 2017; for the temporal trends from 2007 to 2017, other SNPs and haplotypes of Pfcrt and Pfmdr 1 were included. The prevalence of mutant Pfcrt-76 T SNP was 81.6% and 81.8% in 1996 and 2001 and increased to 94.6% in 2007. Thereafter, the prevalence declined sharply to 18.3% in 2012 and 0.9% in 2017 (p < 0.01, Fig. 2). The wild type Pfcrt-K76 significantly increased from 18.4% to 99.1% from 1996 to 2017 a period of over 20 years (p < 0.01). Changing trends were also observed for Pfmdr1 codons 86, 184 and 1246 over years. The prevalence of mutant Pfmdr1-86Y slowly decreased to 71.0% in 2007, then declined to zero in 2017 (p < 0.01, Fig. 2). The prevalence of mutant Pfmdr1-1246Y decreased from 41.1% in 2007 to 9.9% in 2017 (p < 0.01). In contrast, mutant Pfmdr1-184F increased from 17.9% in 2007 to 55.9% in 2017 (p < 0.01, Fig. 2).
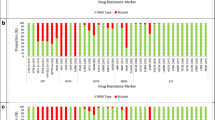
Figure 3a shows the decline of major mutant haplotype C72V73I74E75T76 (CVIET) of Pfcrt from 75.0% to 0.9% from 2007 to 2017 (p < 0.01) while the wild haplotype C72V73M74N75K76 (CVMNK) of Pfcrt increased from 4.0% of 2007 to 99.1% in 2017 (p < 0.01). The parasites carrying Pfmdr1 N86F184S1034N1042D1246 (NFSND) haplotype (containing a mutant SNP at codon 184F), possibly associated with reduced lumefantrine susceptibility, increased from 11.0% in 2007 to 49.6% in 2017 (p < 0.01, Fig. 3b). There was a significant increase in the prevalence of wild haplotype N86Y184S1034N1042D1246 (NYSND) from 11.1% to 40.5% (p < 0.01) as well as a decrease in the prevalence of two other mutant haplotypes, Y86Y184S1034N1042Y1246 (YYSNY) from 34.0% to 4.8% (p < 0.01) and Y86Y184S1034N1042D1246 (YYSND) from 34.0% to 2.9% (p < 0.01), from 2007 to 2017.
Temporal trend in the prevalence of Pfcrt and Pfmdr1 haplotypes from 2007 to 2017. 3a The construction of Pfcrt haplotype includes codons 72, 73, 74, 75, 76. Codons at 72 and 73 were wild type in all samples tested in this paper. CVMNK, the first label, is the wild haplotype of Pfcrt and remaining labels are all mutant haplotypes. 3b The construction of Pfmdr1 haplotype includes codons 86, 184, 1034, 1042, 1246. Codons at 1034 and 1042 were wild types in all samples tested in this paper. NYSND, the first label, is the wild haplotype of Pfmdr1 and remaining labels are all mutant haplotypes. Symbols “*” indicate statistical significance in prevalence of haplotypes over time (p < 0.01). The data in 2007 were extracted from publications [30]
Artemisinin resistance marker Pfk13 gene at the 2012 and 2017 surveys
There were no artemisinin-associated resistant Pfk13 mutations at the nine validated codons or other candidate codons listed by the WHO (2018) [38] in any of the samples tested in the 2012 and 2017 surveys in the Asembo area. Two samples from the 2017 survey had the Pfk13 synonymous mutation at codons 504 and 510, respectively.
Comparison of drug resistance molecular markers in parasites from mosquitoes and humans in 2012 survey
A total of 66 mosquitoes collected in 2012 were found to be oocyst positive and analysed for the frequency of molecular markers of drug resistance. Among oocyst-positive mosquitoes, An.s funestus was the predominant species (87.9%), compared to An. gambiae s.s. (6.1%) and An. arabiensis (4.5%). Species identification by PCR failed for one mosquito sample. There were marginal differences in the prevalence of three drug resistant SNPs in the parasites from mosquitos compared to human, with a lower frequency of Pfdhps-436H (p = 0.059) and a higher frequency of Pfcrt-75D/E, − 76 T in mosquito oocysts (p = 0.051) (Table 3). The prevalence of parasites carrying wild haplotype Pfcrt C72V73M74N75K76 (CVMNK) was lower in mosquitoes than in human blood with marginal statistical significance (p = 0.051, Fig. 4). There were eight Pfmdr1 haplotypes of parasites in humans but seven haplotypes in mosquitoes with Y86Y184S1034N1042D1246 (YYSND) not observed in mosquitoes. The prevalence of Pfmdr1 wild haplotype N86Y184S1034N1042D1246 (NYSND) was marginally higher in mosquito oocysts than in human blood samples (p = 0.070, Fig. 4). Since mosquitoes were collected from a single village while sampling of parasites from humans was 54 villages across the entire HDSS area, additional analyses were conducted to assess whether the observed marginal differences in drug resistance markers were the result of biases due to the limited geographic sampling area for mosquitoes. The distance from the household of each human sampled for parasite infection to the centroid of the village where mosquitoes were collected was calculated. Households were then categorized as < 7 km, < 14 km and < 27 km from the centroid of the village where mosquitoes were collected. The initial selection of 7 km distance was based on the upper limit of a basic mosquito reproductive unit as assessed by kinship analysis of An. gambiae s.s. using microsatellite loci in this area [41]. Comparisons of the frequency of drug resistance SNP markers between human blood samples and oocysts in mosquitoes showed similar trends with similar marginal p-values within the different distance categories. These analyses suggest that there was no substantial variation in the frequency of molecular markers of drug resistance across the investigation and that the marginal differences observed between parasites from humans versus mosquitoes were not substantially biased by the limited geographic sampling area for mosquitoes (see Additional file 3).
Discussion
This time series analysis of changes in the prevalence of molecular markers of anti-malarial drug resistance over 20 years in western Kenya showed a near fixation of the Pfdhfr-51I, -59R, -108 N and Pfdhps-437G, -540E resistance markers and a significant increase in the sextuple mutant haplotype containing the Pfdhps-436H allele between 2012 and 2017. In contrast, a near complete return of the wild type haplotype of Pfcrt and Pfmdr1 was observed in 2017, 19 years after the withdrawal of CQ and 12 years after the wide-scale uptake of AL in the study area. No validated or candidate mutations in the Pfk13 propeller domain associated with artemisinin resistance were found in 2012 or 2017 based on WHO 2018 standards [38]. Marginal differences in the prevalence of Pfdhps-436H and Pfcrt-76 T were observed between parasites from human blood samples and mosquitoes.
Despite the discontinuation of SP as first line treatment for uncomplicated malaria in the general population in 2004, the prevalence of combined SP dhfr/dhps quintuple mutant haplotype (C50I51R59N108I164/S436/G437E540A581A613) steadily increased to 85.2% in 2012, then decreased in 2017 to 59.8%. However, this decrease was largely due to an increased prevalence of sextuple mutant haplotype (C50I51R59N108I164/H436G437E540A581A613), resulting from the rise in Pfdhps-436H allele in the Asembo area from 0.0% in 2007 [30] to 10.5% in 2012 and 34.6% in 2017. This trend was consistent with other studies in western Kenya reporting that Pfdhps-436H allele was undetectable in 2005, 14.1% between 2010 and 2013 in samples collected from children in the Bondo District Hospital and the Siaya District Hospital of western Kenya [42], and 28.0% in 2018 in children enrolled at the Siaya County Referral Hospital [43]. In addition, the Pfdhps-436H mutation was observed at 3.8% in pregnant women in 2008 to 2009 in western Kenya [44]. Taken together, it is plausible that the increase in prevalence of Pfdhps-436H mutant allele and sextuple mutant haplotype in the parasites in general population might originate from a slow expansion of such mutant parasites from the pregnant women on IPTp-SP. It is also possible that cross-resistance to other antifolate drugs, such as cotrimoxazole (CTX) commonly used as prophylaxis against opportunistic infection in HIV infected individuals or as treatment for other bacterial infections in general populations [45,46,47], could select for the Pfdhps-436H in this area. However, a recent trial has shown that CTX does not select for SP resistance [48]. Although the effect of the Pfdhps-436H mutation on SP resistance is not yet known, the progressive increase of this mutant allele indicates a need to closely monitor its impact on the effectiveness of IPTp with SP in western Kenya.
The temporal trend analysis showed that the prevalence of Pfcrt-76 T mutants increased from 81.0% in 2001 to a peak prevalence (94.6%) in 2007, during which AQ, which may exert similar selective pressure as CQ, was still used in this area [29, 30, 42]. This was then followed by the sharp decline in resistance marker Pfcrt-76 T from 94.6% in 2007 to 18.3% in 2012 and 0.9% in 2017 and a marked increase in the CQ-sensitive haplotype (C72V73M74N75K76) from 4.0% in 2007 to 81.7% in 2012 and to 99.1% in 2017. This reversal of Pfcrt from CQ-resistant to CQ-sensitive genotype, after long-term withdrawal of CQ (19 years), has been reported previously in other countries [49], as well as in coastal Kenya and other areas of western Kenya [50]. The reduced prevalence of CQ-resistant genotypes reflects a fitness cost to the parasites after long-term withdrawal of CQ and less use of AQ [51].
However, the strong temporal trend, following the widespread introduction of artemether-lumefantrine as first-line treatment in the study area in 2006, suggests that counter-selection pressure from lumefantrine on this gene may have also played an important role. AL and CQ or AQ exert opposite selection pressure on the Pfcrt genotypes as AL selects Pfcrt-K76 while AQ and CQ select Pfcrt-76 T [52, 53]. Overall, the reversal of Pfcrt to CQ sensitive genotype may indicate the option of re-introducing CQ as a component of ACT using a strategy of negative cross-resistance or as part of a triple-drug ACT combination [54,55,56] though there are debates on this re-introduction of CQ.
CQ and AQ also select for Pfmdr1-86Y and -1246Y SNPs, while AL selects for the Pfmdr1-N86, -184F, and -D1246 alleles [52]. Previous studies have shown a strong selection of wild Pfmdr1-N86 in re-infection after treatment with AL [57, 58] and the increase of Pfmdr1-N86 is associated with reduced susceptibility to AL treatment [52]. It has been reported that the selection of wild Pfmdr1-N86 is mediated by lumefantrine drug pressure in vitro [59, 60]. The counter-selection of wild type Pfmdr1-N86 has also been observed in use of other antimalarials, such as mefloquine vs CQ/AQ [55, 61]. In addition, mutant SNP Pfmdr1-184F was considered to be under selection by AL [36] and was associated with reduced lumefantrine susceptibility in vivo and ex vivo [18, 62]. The Pfmdr1 haplotype N86F184D1246 was significantly associated with AL treatment failures in Nigerian children [15]. The temporal analysis in this study showed that wild type Pfmdr1-N86 increased across years from 25.2% in 1996 at baseline to 100% in 2017 and mutant SNP Pfmdr1-184F increased in 2012 and 2017 in the Asembo area. Accordingly, both wild haplotype N86Y184S1034N1042D1246 and the haplotype carrying 184F mutant codon, N86F184S1034N1042D1246 steadily increased over years. These results are consistent with previous findings in other areas of western Kenya [63, 64] and other African countries [65, 66]. There are two combined effects for this phenomenon. First, the increase in wild haplotype N86Y184S1034N1042D1246 indicates returning to CQ sensitivity by changes from Pfmdr1-86Y to Pfmdr1-N86 and from Pfmdr1-1246Y to Pfmdr1-D1246 (Fig. 2) after withdrawal of CQ or AQ in the area [30, 53]. Second, counter-selection of wild Pfmdr1-N86, -D1246 and selection of mutant Pfmdr1-184F by use of AL [15] over a decade could result in the increase of mutant N86F184S1034N1042D1246 haplotype.
AL was officially recommended as first-line ACT for treatment of uncomplicated malaria in 2004 with widespread implementation since the end of 2006 [5] in Kenya. In the current 2012 and 2017 community surveys, no artemisinin-associated drug resistant mutations were found after a decade of AL use in the Asembo area based on WHO 2018 standard [38]. These molecular Pfk13 findings were consistent with the previous report in a 2016–2017 TES conducted in Siaya county of western Kenya [67]. There were no overt signs of delayed parasite clearance on day 3 [Nelli Westercamp et al. unpublished data] and no mutations associated with artemisinin resistance [67]. However, the PCR-corrected adequate sustained clinical and parasitological response (ACPR) for AL was 88.5% on day 28 while that for dihydroartemisinin–piperaquine remained high at day 42 in the same TES study [Nelli Westercamp et al. unpublished data]. This may suggest parasite sensitivity to the Artemisinin partner drug, lumefantrine is waning. Although the prevalence of Pfmdr1-184F mutations was high, their association with treatment failure was not statistically significant [67]. These results are poorly understood and further investigation of association between Pfmdr1-184F and lumefantrine is warranted in Kenya. Moreover, Pfk13 mutations associated with delayed parasite clearance have been locally emerged in Rwanda (Pfk13 R561H SNP) and Uganda (Pfk13 A675V and C469Y SNPs), respectively [68, 69]. Therefore, continued monitoring of Pfk13 molecular markers is necessary in African countries including Kenya for early detection of AL drug resistance.
The present study showed a marginally higher prevalence of mutant Pfcrt-76 T SNP in mosquito oocysts compared to human blood samples, suggesting that Pfcrt mutation-bearing parasites might be more transmissible in this setting of western Kenya. In contrast, the lower prevalence of Pfdhps-436H mutant in mosquito oocysts compared to humans was observed in this study, indicating that there could be a fitness cost in An. funestus mosquitoes for transmission of the Pfdhps-436H mutation bearing parasites in the Asembo area. Differences in mutation profiles between human and mosquito hosts and among species of mosquitoes have been documented previously. For instance, a previous study in a high transmission area of Zambia has shown that the prevalence of resistant SNP of cycloguanil (Proguanil metabolite), Pfdhfr-108 T, is high in human blood (> 90.0%), but very rare in the midgut of An. arabiensis [26]. In Southern Zambia, there was a lower prevalence of mutant Pfcrt-76 T SNP bearing parasites in An. arabiensis mosquitoes compared to human blood samples [24]. However, in Uganda significantly higher prevalence of mutant Pfcrt-76 T and Pfmdr1-86Y was observed in An. gambiae complex mosquitoes than in human blood [25]. Another study conducted in Tanzania showed that An. arabiensis consistently carried a lower proportion of Pfcrt-76 T mutant than both An. funestus and An. gambiae s.s. from the salivary glands [27]. These studies highlight the heterogeneity in transmission of different markers of anti-malarial drug resistance, which is likely affected by the species of mosquito, the individual markers of drug resistance and the transmission settings. These studies also suggest that mosquito-parasite interactions have the potential for either accelerating or slowing the transmission of drug resistance, although the mechanisms involved are still unknown. Further studies are needed to understand how different mosquito vectors transmit parasites with different drug resistance markers in different transmission settings.
Limitations
There were a few limitations in the present study. First, the sample size for genotyping drug resistance markers of parasites in mosquito oocysts was small, which could affect statistical power for detecting statistically significant differences between the two hosts. Second, the mosquitoes collected were not from the same houses where the human blood samples were collected, and there was a slight difference in the months between the collection of mosquitoes (May to September) and human blood (June to August). This limited us from conducting true pair-wise comparisons. However, the marginal differences in prevalence of Pfdhps-436H and Pfcrt-76 T mutant SNPs at population level between two hosts observed in this study deserve further investigation.
Conclusions
This study showed an increased prevalence of dhfr/dhps resistant markers over 20 years with the emergence of Pfdhps-436H mutant a decade ago in Asembo. CQ-sensitive haplotype reached nearly 100% in 2017, a reversal from CQ-resistant to CQ-sensitive genotype at the Pfcrt gene after 19 years of the withdrawal of CQ. No Pfk13 markers associated with artemisinin resistance were detected, but the increasing prevalence of Pfmdr1 N86F184S1034N1042D1246 haplotype was observed. The differences in prevalence of Pfdhps-436H and Pfcrt-76 T SNPs between two hosts and the role of mosquitoes in the transmission of drug resistant parasites require further investigation. Continued monitoring of the molecular resistance markers in this area is imperative to guide anti-malarial policy and delay the emergence and spread of drug resistance.
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Availability of data and materials
The molecular dataset used in this study is available and can be shared upon reasonable request to the corresponding authors.
Abbreviations
- ACPR:
-
Adequate sustained clinical and parasitological response
- ACT:
-
Artemisinin-based combination therapy
- AL:
-
Artemether-lumefantrine
- AQ:
-
Amodiaquine
- DBS:
-
Dried blood spot
- CQ:
-
Chloroquine
- CTX:
-
Cotrimoxazole
- DHA:
-
Dihydroartemisinin
- HDSS:
-
Health and demographic surveillance system
- Pfdhfr :
-
Plasmodium falciparum Dihydrofolate reductase
- Pfdhps :
-
Plasmodium falciparum Dihydropteroate synthase
- ITN:
-
Insecticide-treated net
- IPTp:
-
Intermittent preventive treatment during pregnancy
- LLIN:
-
Long lasting insecticide-treated bed nets
- PCR:
-
Polymerase chain reaction
- Pfcrt :
-
Plasmodium falciparum Chloroquine resistance transporter gene
- Pfk13 :
-
Plasmodium falciparum Kelch 13
- Pfmdr1 :
-
Multi-drug resistance protein 1
- SNP:
-
Single nucleotide polymorphism
- SP:
-
Sulfadoxine-pyrimethamine
- TES:
-
Therapeutic efficacy study
- WHO:
-
World Health Organization
References
Desai M, Buff AM, Khagayi S, Byass P, Amek N, van Eijk A, et al. Age-specific malaria mortality rates in the KEMRI/CDC health and demographic surveillance system in western Kenya, 2003–2010. PLoS ONE. 2014;9: e106197.
Cibulskis RE, Alonso P, Aponte J, Aregawi M, Barrette A, Bergeron L, et al. Malaria: global progress 2000–2015 and future challenges. Infect Dis Poverty. 2016;5:61.
Amin AA, Zurovac D, Kangwana BB, Greenfield J, Otieno DN, Akhwale WS, et al. The challenges of changing national malaria drug policy to artemisinin-based combinations in Kenya. Malar J. 2007;6:72.
Sasi P, Abdulrahaman A, Mwai L, Muriithi S, Straimer J, Schieck E, et al. In vivo and in vitro efficacy of amodiaquine against Plasmodium falciparum in an area of continued use of 4-aminoquinolines in east Africa. J Infect Dis. 2009;199:1575–82.
Ministry of Health. The Kenya Malaria Strategy 2009–2018 (Revised 2014). Nairobi, Kenya, 2014.
Taylor KA, Koros JK, Nduati J, Copeland RS, Collins FH, Brandling-Bennett AD. Plasmodium falciparum infection rates in Anopheles gambiae, An. arabiensis, and An. funestus in western Kenya. Am J Trop Med Hyg. 1990;43:124–9.
McCann RS, Ochomo E, Bayoh MN, Vulule JM, Hamel MJ, Gimnig JE, et al. Reemergence of Anopheles funestus as a vector of Plasmodium falciparum in western Kenya after long-term implementation of insecticide-treated bed nets. Am J Trop Med Hyg. 2014;90:597–604.
Gregson A, Plowe C. Mechanisms of resistance of malaria parasites to antifolates. Pharmacol Rev. 2005;57:117–45.
van Eijk AM, Larsen DA, Kayentao K, Koshy G, Slaughter DEC, Roper C, et al. Effect of Plasmodium falciparum sulfadoxine-pyrimethamine resistance on the effectiveness of intermittent preventive therapy for malaria in pregnancy in Africa: a systematic review and meta-analysis. Lancet Infect Dis. 2019;19:546–56.
Wellems TE, Plowe CV. Chloroquine-resistant malaria. J Infect Dis. 2001;184:770–6.
Holmgren G, Hamrin J, Svärd J, Mårtensson A, Gil JP, Björkman A. Selection of pfmdr1 mutations after amodiaquine monotherapy and amodiaquine plus artemisinin combination therapy in East Africa. Infect Genet Evol. 2007;7:562–9.
Noedl H, Se Y, Schaecher K, Smith BL, Socheat D, Fukuda MM. Evidence of artemisinin-resistant malaria in western Cambodia. N Engl J Med. 2008;359:2619–20.
Dondorp AM, Nosten F, Yi P, Das D, Phyo AP, Tarning J, et al. Artemisinin resistance in Plasmodium falciparum malaria. N Engl J Med. 2009;361:455–67.
Ashley EA, Dhorda M, Fairhurst RM, Amaratunga C, Lim P, Suon S, et al. Spread of artemisinin resistance in Plasmodium falciparum malaria. N Engl J Med. 2014;371:411–23.
Happi CT, Gbotosho GO, Folarin OA, Sowunmi A, Hudson T, O’Neil M. Selection of Plasmodium falciparum multidrug resistance gene 1 alleles in asexual stages and gametocytes by artemether-lumefantrine in Nigerian children with uncomplicated falciparum malaria. Antimicrob Agents Chemother. 2009;53:888–95.
Lobo E, de Sousa B, Rosa S, Figueiredo P, Lobo L, Pateira S. Prevalence of pfmdr1 alleles associated with artemether-lumefantrine tolerance/resistance in Maputo before and after the implementation of artemisinin-based combination therapy. Malar J. 2014;13:300.
Otienoburu SD, Maïga-Ascofaré O, Schramm B, Jullien V, Jones JJ. Selection of Plasmodium falciparum pfcrt and pfmdr1 polymorphisms after treatment with artesunate–amodiaquine fixed dose combination or artemether–lumefantrine in Liberia. Malar J. 2016;15:452.
Malmberg M, Ferreira PE, Tarning J, Ursing J, Ngasala B, Björkman A, et al. Plasmodium falciparum drug resistance phenotype as assessed by patient antimalarial drug levels and its association with pfmdr1 polymorphisms. J Infect Dis. 2012;207:842–7.
Uwimana A, Umulisa N, Venkatesan M, Svigel SS, Zhou Z, Munyaneza T, et al. Association of Plasmodium falciparum kelch13 R561H genotypes with delayed parasite clearance in Rwanda: an open-label, single-arm, multicentre, therapeutic efficacy study. Lancet Infect Dis. 2021;21:1120–8.
Balikagala B, Fukuda N, Ikeda M, Katuro OT, Tachibana SI, Yamauchi M, et al. Evidence of artemisinin-resistant malaria in Africa. N Engl J Med. 2021;385:1163–71.
Klein EY. Antimalarial drug resistance: a review of the biology and strategies to delay emergence and spread. Int J Antimicrob Agents. 2013;41:311–7.
Mendes C, Salgueiro P, Gonzalez V, Berzosa P, do BenitoRosário AVE, et al. Genetic diversity and signatures of selection of drug resistance in Plasmodium populations from both human and mosquito hosts in continental equatorial Guinea. Malar J. 2013;12:114.
Hastings I, Watkins W. Intensity of malaria transmission and the evolution of drug resistance. Acta Trop. 2005;94:218–29.
Mharakurwa S, Sialumano M, Liu K, Scott A, Thuma P. Selection for chloroquine-sensitive Plasmodium falciparum by wild Anopheles arabiensis in southern Zambia. Malar J. 2013;12:453.
Conrad MD, Mota D, Musiime A, Kilama M, Rek J, Kamya M. Comparative prevalence of Plasmodium falciparum resistance-associated genetic polymorphisms in parasites infecting humans and mosquitoes in Uganda. Am J Trop Med Hyg. 2017;97:1576–80.
Mharakurwa S, Kumwenda T, Mkulama MA, Musapa M, Chishimba S, Shiff CJ, et al. Malaria antifolate resistance with contrasting Plasmodium falciparum dihydrofolate reductase (DHFR) polymorphisms in humans and Anopheles mosquitoes. Proc Natl Acad Sci USA. 2011;108:18796–801.
Temu EA, Kimani I, Tuno N, Kawada H, Minjas JN, Takagi M. Monitoring chloroquine resistance using Plasmodium falciparum parasites isolated from wild mosquitoes in Tanzania. Am J Trop Med Hyg. 2006;75:1182–7.
Smith-Aguasca R, Gupta H, Uberegui E, Maquina M, Saute F, Paaijmans KP, et al. Mosquitoes as a feasible sentinel group for anti-malarial resistance surveillance by next generation sequencing of Plasmodium falciparum. Malar J. 2019;18:351.
Shah M, Kariuki S, Vanden Eng J, Blackstock AJ, Garner K, Gatei W, et al. Effect of transmission reduction by insecticide-treated bednets (ITNs) on antimalarial drug resistance in western Kenya. PLoS ONE. 2011;6: e26746.
Shah M, Omosun Y, Lal A, Odero C, Gatei W, Otieno K, et al. Assessment of molecular markers for anti-malarial drug resistance after the introduction and scale-up of malaria control interventions in western Kenya. Malar J. 2015;14:75.
Odhiambo FO, Laserson KF, Sewe M, Hamel MJ, Feikin DR, Adazu K. Profile: the KEMRI/CDC health and demographic surveillance system-western Kenya. Int J Epidemiol. 2012;41:977–87.
Vazquez-Prokopec GM, Galvin WA, Kelly R, Kitron U. A new, cost-effective, battery-powered aspirator for adult mosquito collections. J Med Entomol. 2009;46:1256–9.
Gillies MT, Coetzee M. A supplement to the Anophelinae of Africa south of the Sahara. S Afr Inst Med R. 1987;55:1–143.
Scott JA, Brogdon WG, Collins FH. Identification of single specimens of the Anopheles gambiae complex by the polymerase chain-reaction. Am J Trop Med Hyg. 1993;49:520–9.
Mejia Torres RE, Banegas EI, Mendoza M, Diaz C, Bucheli STM, Fontecha GA, et al. Efficacy of chloroquine for the treatment of uncomplicated Plasmodium falciparum malaria in Honduras. Am J Trop Med Hyg. 2013;88:850–4.
Vinayak S, Alam MT, Sem R, Shah NK, Susanti AI, Lim P, et al. Multiple genetic backgrounds of the amplified Plasmodium falciparum multidrug resistance (pfmdr1) gene and selective sweep of 184F mutation in Cambodia. J Infect Dis. 2010;201:1551–60.
Talundzic E, Okoth SA, Congpuong K, Plucinski MM, Morton L, Goldman IF, et al. Selection and spread of artemisinin-resistant alleles in Thailand prior to the global artemisinin resistance containment campaign. PLoS Pathog. 2015;11:e1004789.
WHO. Artemisinin resistance and artemisinin-based combination therapy efficacy: status report. Geneva, World Health Organization, 2018. Accessed 2020.
McCollum AM, Poe AC, Hamel M, Huber C, Zhou Z, Shi YP, et al. Antifolate resistance in Plasmodium falciparum: multiple origins and identification of novel dhfr alleles. J Infect Dis. 2006;194:189–97.
Spalding MD, Eyase FL, Akala HM, Bedno SA, Prigge ST, Coldren RL, et al. Increased prevalence of the pfdhfr/phdhps quintuple mutant and rapid emergence of pfdhps resistance mutations at codons 581 and 613 in Kisumu, Kenya. Malar J. 2010;24(9):338.
Lehmann T, Licht M, Gimnig JE, Hightower A, Vulule JM, Hawley WA. Spatial and temporal variation in kinship among Anopheles gambiae (Diptera: Culicidae) mosquitoes. J Med Entomol. 2003;40:421–9.
Lucchi NW, Okoth SA, Komino F, Onyona P, Goldman IF, Ljolje D, et al. Increasing prevalence of a novel triple-mutant dihydropteroate synthase genotype in Plasmodium falciparum in western Kenya. Antimicrob Agents Chemother. 2015;59:3995–4002.
Pacheco MA, Schneider KA, Cheng Q, Munde EO, Ndege C, Onyango C, et al. Changes in the frequencies of Plasmodium falciparum dhps and dhfr drug-resistant mutations in children from Western Kenya from 2005 to 2018: the rise of Pfdhps S436H. Malar J. 2020;19:378.
Iriemenam NC, Shah M, Gatei W, van Eijk AM, Ayisi J, Kariuki S, et al. Temporal trends of sulphadoxine-pyrimethamine (SP) drug-resistance molecular markers in Plasmodium falciparum parasites from pregnant women in western Kenya. Malar J. 2012;11:134.
White NJ. Antimalarial drug resistance. J Clin Invest. 2004;113:1084–92.
Kateera F, Nsobya SL, Tukwasibwe S, Hakizimana E, Mutesa L, Mens PF, et al. Molecular surveillance of Plasmodium falciparum drug resistance markers reveals partial recovery of chloroquine susceptibility but sustained sulfadoxine-pyrimethamine resistance at two sites of different malaria transmission intensities in Rwanda. Acta Trop. 2016;164:329–36.
Sugaram R, Suwannasin K, Kunasol C, Vivek Bhakta Mathema VB, Day NPJ, Sudathip P, et al. Molecular characterization of Plasmodium falciparum antifolate resistance markers in Thailand between 2008 and 2016. Malar J. 2020;19:107.
Juma DW, Muiruri P, Yuhas K, John-Stewart G, Ottichilo R, Waitumbi J, et al. The prevalence and antifolate drug resistance profiles of Plasmodium falciparum in study participants randomized to discontinue or continue cotrimoxazole prophylaxis. PLoS Neglect Trop Dis. 2019;13:e0007223.
Frosch AEP, Laufer MK, Mathanga DP, Takala-Harrison S, Skarbinski J, Claassen CW, et al. Return of widespread chloroquine-sensitive Plasmodium falciparum to Malawi. J Infect Dis. 2014;210:1110–4.
Bwire GM, Ngasala B, Mikomangwa WP, Kilonzi M, Kamuhabwa AAR. Detection of mutations associated with artemisinin resistance at k13-propeller gene and a near complete return of chloroquine susceptible falciparum malaria in Southeast of Tanzania. Sci Rep. 2020;10:3500.
Takala-Harrison S, Laufer MK. Antimalarial drug resistance in Africa: key lessons for the future. Ann N Y Acad Sci. 2015;1342:62–7.
Venkatesan M, Gadalla NB, Stepniewska K, Dahal P, Nsanzabana C, Moriera C, et al. Polymorphisms in Plasmodium falciparum chloroquine resistance transporter and multidrug resistance 1 genes: parasite risk factors that affect treatment outcomes for P. falciparum malaria after artemether-lumefantrine and artesunate-amodiaquine. Am J Trop Med Hyg. 2014;91:833–43.
Baliraine FN, Rosenthal PJ. Prolonged selection of pfmdr1 polymorphisms after treatment of falciparum malaria with artemether-lumefantrine in Uganda. J Infect Dis. 2011;204:1120–4.
Thomsen TT, Madsen LB, Hansson HH, Tomás EV, Charlwood D, Bygbjerg IC, et al. Rapid selection of Plasmodium falciparum chloroquine resistance transporter gene and multidrug resistance gene-1 haplotypes associated with past chloroquine and present artemether-lumefantrine use in Inhambane District, southern Mozambique. Am J Trop Med Hyg. 2013;88:536–41.
Huijben S, Macete E, Mombo-Ngoma G, Ramharter M, Kariuki S, Desai M, et al. Counter-selection of antimalarial resistance polymorphisms by intermittent preventive treatment in pregnancy. J Infect Dis. 2019;221:293–303.
White NJ. Triple artemisinin-containing combination anti-malarial treatments should be implemented now to delay the emergence of resistance. Malar J. 2019;18:338.
Sisowath C, Ferreira PE, Bustamante LY, Dahlström S, Mårtensson A, Björkman A, et al. The role of pfmdr1 in Plasmodium falciparum tolerance to artemether-lumefantrine in Africa. Trop Med Int Health. 2007;12:736–42.
Mårtensson A, Strömberg J, Sisowath C, Msellem MI, Gil JP, Montgomery SM, et al. Efficacy of artesunate plus amodiaquine versus that of artemether-lumefantrine for the treatment of uncomplicated childhood Plasmodium falciparum malaria in Zanzibar. Tanzania Clin Infect Dis. 2005;41:1079–86.
Muiruri P, Juma DW, Ingasia LA, Chebon LJ, Opot B, Ngalah BS, et al. Selective sweeps and genetic lineages of Plasmodium falciparum multi-drug resistance (pfmdr1) gene in Kenya. Malar J. 2018;17:398.
Mwai L, Kiara SM, Abdirahman A, Pole L, Rippert A, Diriye A, et al. In vitro activities of piperaquine, lumefantrine, and dihydroartemisinin in Kenyan Plasmodium falciparum isolates and polymorphisms in pfcrt and pfmdr1. Antimicrob Agents Chemother. 2009;53:5069–73.
Okell LC, Reiter LM, Ebbe LS, Baraka V, Bisanzio D, Watson OJ, et al. Emerging implications of policies on malaria treatment: genetic changes in the Pfmdr-1 gene affecting susceptibility to artemether-lumefantrine and artesunate-amodiaquine in Africa. BMJ Glob Health. 2018;3: e000999.
Mbaye A, Dieye B, Ndiaye YD, Bei AK, Muna A, Deme AB, et al. Selection of N86F184D1246 haplotype of Pfmrd1 gene by artemether–lumefantrine drug pressure on Plasmodium falciparum populations in Senegal. Malar J. 2016;15:433.
Achieng AO, Muiruri P, Ingasia LA, Opot BH, Juma DW, Yeda R, et al. Temporal trends in prevalence of Plasmodium falciparum molecular markers selected for by artemether–lumefantrine treatment in pre-ACT and post-ACT parasites in western Kenya. Int J Parasitol Drugs Drug Resist. 2015;5:92–9.
Henriques G, Hallett RL, Beshir KB, Gadalla NB, Johnson RE, Burrow R, et al. Directional selection at the pfmdr1, pfcrt, pfubp1, and pfap2mu Loci of Plasmodium falciparum in Kenyan children treated with ACT. J Infect Dis. 2014;210:2001–8.
Mwaiswelo R, Ngasala B, Gil JP, Malmberg M, Jovel I, Xu W, et al. Sustained high cure rate of artemether-lumefantrine against uncomplicated Plasmodium falciparum malaria after 8 years of its wide-scale use in Bagamoyo District. Tanzania Am J Trop Med Hyg. 2017;97:526–32.
Raman J, Kagoro FM, Mabuza A, Malatje G, Reid A, Frean J, et al. Absence of kelch13 artemisinin resistance markers but strong selection for lumefantrine-tolerance molecular markers following 18 years of artemisinin-based combination therapy use in Mpumalanga Province, South Africa (2001–2018). Malar J. 2019;18:280.
Chebore W, Zhou Z, Westercamp N, Otieno K, Shi YP, Sergent SB, et al. Assessment of molecular markers of anti-malarial drug resistance among children participating in a therapeutic efficacy study in western Kenya. Malar J. 2020;19:291.
Uwimana A, Legrand E, Stokes BH, Mangala Ndikumana J-L, Warsame M, Umulisa N, et al. Emergence and clonal expansion of in vitro artemisinin-resistant Plasmodium falciparum kelch13 R561H mutant parasites in Rwanda. Nat Med. 2020;26:1602–8.
Asua V, Conrad MD, Aydemir O, Duvalsaint M, Legac J, Duarte E, et al. Changing prevalence of potential mediators of aminoquinoline, antifolate, and artemisinin resistance across Uganda. J Infect Dis. 2020;223:985–94.
Acknowledgements
We thank all field staff for supporting community-based surveys and the entomologic component of this study, including field logistics. We also thank Dr. Kimbely Lindblade for her leading role in 2001 community survey which makes this study possible. We also thank Dr. Maurice Ombok for calculating distance data that were used in Additional file 3. We thank all families and people who participated in community surveys in the Asembo area, western Kenya. We thank the Director of KEMRI for the permission to publish this data.
Funding
This study was supported partially by the US National Science Foundation, Ecology of Infectious Diseases Grant #EF-0723770 through Michigan State University and by the Malaria Branch, Division of Parasitic Diseases and Malaria, CGH, CDC, USA.
Author information
Authors and Affiliations
Contributions
YPS, JEG, and EDW conceived, designed and coordinated this study and participated in the interpretation of data. SBS, YL, ZZ performed the PCR and sequencing analysis. JW performed statistical analyses. ZZ analyzed and interpreted the data. AMS, MD, SK, KO, WC, MS, FtK, and MJH led or participated in community-based surveys, including blood sample collection and processing as well as preparing data for previous publications. JEG, EDW, BA, SK and KO coordinated or participated entomological component of this study, including mosquito sample collection and processing. ZZ, JEG and YPS wrote this manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
: Table S1. Primer sequences and reaction conditions for nested PCRs of Pfdhfr and Pfdhps.
Additional file 2: Table S2.
Primers used for PCR and sequencing for Pfcrt, Pfmdr1 and Pfk13 genes.
Additional file 3:
Table S3. Comparison in prevalence of drug resistance SNPs of parasites between mosquitoes and human blood samples collected by three categories of distances.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhou, Z., Gimnig, J.E., Sergent, S.B. et al. Temporal trends in molecular markers of drug resistance in Plasmodium falciparum in human blood and profiles of corresponding resistant markers in mosquito oocysts in Asembo, western Kenya. Malar J 21, 265 (2022). https://doi.org/10.1186/s12936-022-04284-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-022-04284-6