Abstract
Purpose of Review
Fracture fixation aims to provide stability and promote healing, but remains challenging in unstable and osteoporotic fractures with increased risk of construct failure and nonunion. The first part of this article reviews the clinical motivation behind finite element analysis of fracture fixation, its strengths and weaknesses, how models are developed and validated, and how outputs are typically interpreted. The second part reviews recent modeling studies of the femur and proximal humerus, areas with particular relevance to fragility fractures.
Recent Findings
There is some consensus in the literature around how certain modeling aspects are pragmatically formulated, including bone and implant geometries, meshing, material properties, interactions, and loads and boundary conditions. Studies most often focus on predicted implant stress, bone strain surrounding screws, or interfragmentary displacements. However, most models are not rigorously validated.
Summary
With refined modeling methods, improved validation efforts, and large-scale systematic analyses, finite element analysis is poised to advance the understanding of fracture fixation failure, enable optimization of implant designs, and improve surgical guidance.



Similar content being viewed by others
Availability of Data and Material
Not applicable
Code Availability
Not applicable
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res. 2007;22:465–75.
Brinker MR, Hanus BD, Sen M, O’Connor DP. The devastating effects of tibial nonunion on health-related quality of life. J Bone Joint Surg Am. 2013;95:2170–6.
Brinker MR, Trivedi A, OʼConnor DP. Debilitating Effects of femoral nonunion on health-related quality of life. J Orthop Trauma. 2017;31:e37–42.
Hak DJ, Fitzpatrick D, Bishop JA, Marsh JL, Tilp S, Schnettler R, et al. Delayed union and nonunions: epidemiology, clinical issues, and financial aspects. Injury. 2014;45(Suppl 2):S3–7.
Rupp M, Biehl C, Budak M, Thormann U, Heiss C, Alt V. Diaphyseal long bone nonunions - types, aetiology, economics, and treatment recommendations. Int Orthop. 2018;42:247–58.
Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006;17:1726–33.
Maradit Kremers H, Larson DR, Crowson CS, Kremers WK, Washington RE, Steiner CA, et al. Prevalence of total hip and knee replacement in the United States. J Bone Joint Surg Am. 2015;97:1386–97.
Abdel MP, Watts CD, Houdek MT, Lewallen DG, Berry DJ. Epidemiology of periprosthetic fracture of the femur in 32 644 primary total hip arthroplasties: a 40-year experience. Bone Joint J. 2016;98-B:461–7.
Scolaro JA, Schwarzkopf R. Management of interprosthetic femur fractures. J Am Acad Orthop Surg. 2017;25:e63–9.
Elliott DS, Newman KJH, Forward DP, Hahn DM, Ollivere B, Kojima K, et al. A unified theory of bone healing and nonunion: BHN theory. Bone Joint J. 2016;98-B:884–91.
Perren SM. Physical and biological aspects of fracture healing with special reference to internal fixation. Clin Orthop Relat Res. 1979:175–96.
Cheng C, Shoback D. Mechanisms underlying normal fracture healing and risk factors for delayed healing. Curr Osteoporos Rep. 2019;17:36–47.
Einhorn TA, Gerstenfeld LC. Fracture healing: mechanisms and interventions. Nat Rev Rheumatol. 2015;11:45–54.
• Elkins J, Marsh JL, Lujan T, Peindl R, Kellam J, Anderson DD, et al. Motion predicts clinical callus formation. J Bone Joint Surg Am. 2016;98:276–84 This study developed semi-patient specific models of a series of patients. Correlations between predicted interfragmentary motions (axial and shear) and clinical callus formation were examined.
Augat P, Burger J, Schorlemmer S, Henke T, Peraus M, Claes L. Shear movement at the fracture site delays healing in a diaphyseal fracture model. J Orthop Res. 2003;21:1011–7.
Claes LE, Meyers N. The direction of tissue strain affects the neovascularization in the fracture-healing zone. Med Hypotheses. 2020;137:109537.
Epari DR, Kassi J-P, Schell H, Duda GN. Timely fracture-healing requires optimization of axial fixation stability. J Bone Joint Surg Am. 2007;89:1575–85.
Panteli M, Pountos I, Jones E, Giannoudis PV. Biological and molecular profile of fracture non-union tissue: current insights. J Cell Mol Med. 2015;19:685–713.
Kostenuik P, Mirza FM. Fracture healing physiology and the quest for therapies for delayed healing and nonunion. J Orthop Res. 2017;35:213–23.
Lewis GS, Wee H, Vicory J, Armstrong A, Reid JS. Virtual simulation for interactive visualization of 3D fracture fixation biomechanics. J Am Acad Orthop Surg. (Accepted, in press)
Taylor M, Prendergast PJ. Four decades of finite element analysis of orthopaedic devices: where are we now and what are the opportunities? J Biomech. 2015;48:767–78.
Lambert S, Mischler D, Windolf M, Regazzoni P, Dell’Oca AF, Gueorguiev B, et al. From creative thinking to scientific principles in clinical practice. Injury. 2021;52:32–6.
Dailey HL, Schwarzenberg P, Daly CJ, Boran SAM, Maher MM, Harty JA. Virtual mechanical testing based on low-dose computed tomography scans for tibial fracture: a pilot study of prediction of time to union and comparison with subjective outcomes scoring. J Bone Joint Surg Am. 2019;101:1193–202.
Varga P, Inzana JA, Gueorguiev B, Südkamp NP, Windolf M. Validated computational framework for efficient systematic evaluation of osteoporotic fracture fixation in the proximal humerus. Med Eng Phys. 2018;57:29–39.
Wee H, Reid JS, Chinchilli VM, Lewis GS. Finite element-derived surrogate models of locked plate fracture fixation biomechanics. Ann Biomed Eng. 2017;45:668–80.
Pankaj P. Patient-specific modelling of bone and bone-implant systems: the challenges. Int J Numer Method Biomed Eng. 2013;29:233–49.
Steiner JA, Hofmann UAT, Christen P, Favre JM, Ferguson SJ, van Lenthe GH. Patient-specific in silico models can quantify primary implant stability in elderly human bone. J Orthop Res. 2018;36:954–62.
Wieding J, Souffrant R, Fritsche A, Mittelmeier W, Bader R. Finite element analysis of osteosynthesis screw fixation in the bone stock: an appropriate method for automatic screw modelling. PLoS One. 2012;7:e33776.
Morgan EF, Unnikrisnan GU, Hussein AI. Bone mechanical properties in healthy and diseased states. Annu Rev Biomed Eng. 2018;20:119–43.
Panagiotopoulou VC, Ovesy M, Gueorguiev B, Richards RG, Zysset P, Varga P. Experimental and numerical investigation of secondary screw perforation in the human proximal humerus. J Mech Behav Biomed Mater. 2021;116:104344.
Fleps I, Bahaloo H, Zysset PK, Ferguson SJ, Pálsson H, Helgason B. Empirical relationships between bone density and ultimate strength: a literature review. J Mech Behav Biomed Mater. 2020;110:103866.
Helgason B, Perilli E, Schileo E, Taddei F, Brynjólfsson S, Viceconti M. Mathematical relationships between bone density and mechanical properties: a literature review. Clin Biomech (Bristol, Avon). 2008;23:135–46.
Nobakhti S, Shefelbine SJ. On the relation of bone mineral density and the elastic modulus in healthy and pathologic bone. Curr Osteoporos Rep. 2018;16:404–10.
Synek A, Chevalier Y, Baumbach SF, Pahr DH. The influence of bone density and anisotropy in finite element models of distal radius fracture osteosynthesis: evaluations and comparison to experiments. J Biomech. 2015;48:4116–23.
• MacLeod AR, Simpson AHRW, Pankaj P. Reasons why dynamic compression plates are inferior to locking plates in osteoporotic bone: a finite element explanation. Computer Methods in Biomechanics and Biomedical Engineering Taylor & Francis. 2015;18:1818–25 This study modeled the two fundamentally different types of plate-screw connection mechanisms, applied to either healthy or simulated osteoporotic bone.
Inzana JA, Varga P, Windolf M. Implicit modeling of screw threads for efficient finite element analysis of complex bone-implant systems. J Biomech. 2016;49:1836–44.
MacLeod A, Simpson AHRW, Pankaj P. Experimental and numerical investigation into the influence of loading conditions in biomechanical testing of locking plate fracture fixation devices. Bone Joint Res. 2018;7:111–20.
• Tucker SM, Wee H, Fox E, Reid JS, Lewis GS. Parametric finite element analysis of intramedullary nail fixation of proximal femur fractures. J Orthop Res. 2019;37:2358–66 This study investigated combined effects of nail diameter, nail length, nail material, and presence of distal fixation screws for nine clinically important fracture patterns.
Bergmann G, Graichen F, Rohlmann A, Bender A, Heinlein B, Duda GN, et al. Realistic loads for testing hip implants. Bio-Medical Materials & Engineering. 2010;20:65–75.
Heller MO, Bergmann G, Kassi J-P, Claes L, Haas NP, Duda GN. Determination of muscle loading at the hip joint for use in pre-clinical testing. J Biomech. 2005;38:1155–63.
Heyland M, Trepczynski A, Duda GN, Zehn M, Schaser K-D, Märdian S. Selecting boundary conditions in physiological strain analysis of the femur: balanced loads, inertia relief method and follower load. Med Eng Phys. 2015;37:1180–5.
Speirs AD, Heller MO, Duda GN, Taylor WR. Physiologically based boundary conditions in finite element modelling. J Biomech. 2007;40:2318–23.
Klein P, Schell H, Streitparth F, Heller M, Kassi J-P, Kandziora F, et al. The initial phase of fracture healing is specifically sensitive to mechanical conditions. J Orthop Res. 2003;21:662–9.
Bayraktar HH, Morgan EF, Niebur GL, Morris GE, Wong EK, Keaveny TM. Comparison of the elastic and yield properties of human femoral trabecular and cortical bone tissue. J Biomech. 2004;37:27–35.
Schileo E, Taddei F, Cristofolini L, Viceconti M. Subject-specific finite element models implementing a maximum principal strain criterion are able to estimate failure risk and fracture location on human femurs tested in vitro. J Biomech. 2008;41:356–67.
Feng X, Lin G, Fang CX, Lu WW, Chen B, Leung FKL. Bone resorption triggered by high radial stress: the mechanism of screw loosening in plate fixation of long bone fractures. J Orthop Res. 2019;37:1498–507.
Gee A, Bougherara H, Schemitsch EH, Zdero R. Biomechanical design using in-vitro finite element modeling of distal femur fracture plates made from semi-rigid materials versus traditional metals for post-operative toe-touch weight-bearing. Med Eng Phys. 2021;87:95–103.
Kandemir U, Augat P, Konowalczyk S, Wipf F, von Oldenburg G, Schmidt U. Implant material, type of fixation at the shaft, and position of plate modify biomechanics of distal femur plate osteosynthesis. J Orthop Trauma. 2017;31:e241–6.
Klima ML. Comparison of early fatigue failure of the TFNa and gamma 3 cephalomedullary nails in the United States from 2015 to 2019. J Orthop Trauma. 2021;35:e39–44.
McDonald TC, Lambert JJ, Hulick RM, Graves ML, Russell GV, Spitler CA, et al. Treatment of distal femur fractures with the DePuy-Synthes variable angle locking compression plate. J Orthop Trauma. 2019;33:432–7.
Zhang JY, Tornetta P, Jones B, Zheng Y, Whitten A, Cartner J, et al. Locking hole inserts: effect of insertion torque on fatigue performance and insert loosening in locking plates. J Orthop Trauma. 2019;33:120–4.
Parr WCH, Wang T, Tan C, Dan MJ, Walsh WR, Morberg P. Fatigue implications for bending orthopaedic plates. Injury. 2021.
Tidwell JE, Roush EP, Ondeck CL, Kunselman AR, Reid JS, Lewis GS. The biomechanical cost of variable angle locking screws. Injury. 2016;47:1624–30.
MacLeod AR, Pankaj P, Simpson AHRW. Does screw–bone interface modelling matter in finite element analyses? J Biomech. 2012;45:1712–6.
Moazen M, Mak JH, Jones AC, Jin Z, Wilcox RK, Tsiridis E. Evaluation of a new approach for modelling the screw-bone interface in a locking plate fixation: a corroboration study. Proc Inst Mech Eng H. 2013;227:746–56.
Torcasio A, Zhang X, Van Oosterwyck H, Duyck J, van Lenthe GH. Use of micro-CT-based finite element analysis to accurately quantify peri-implant bone strains: a validation in rat tibiae. Biomech Model Mechanobiol. 2012;11:743–50.
Affes F, Ketata H, Kharrat M, Dammak M. How a pilot hole size affects osteosynthesis at the screw–bone interface under immediate loading. Med Eng Phys. 2018;60:14–22.
Pankaj P, Xie S. The risk of loosening of extramedullary fracture fixation devices. Injury. 2019;50:S66–72.
Steiner JA, Ferguson SJ, van Lenthe GH. Computational analysis of primary implant stability in trabecular bone. J Biomech. 2015;48:807–15.
Wirth AJ, Müller R, van Lenthe GH. Computational analyses of small endosseous implants in osteoporotic bone. Eur Cell Mater. 2010;20:58–71.
Van den Abbeele M, Valiadis J-M, Lima LVPC, Khalifé P, Rouch P, Skalli W. Contribution to FE modeling for intraoperative pedicle screw strength prediction. Comput Methods Biomech Biomed Engin. 2018;21:13–21.
• Varga P, Grünwald L, Inzana JA, Windolf M. Fatigue failure of plated osteoporotic proximal humerus fractures is predicted by the strain around the proximal screws. J Mech Behav Biomed Mater. 2017;75:68–74 This validation study included 19 specimen-specific finite element models and corresponding cadaveric cyclic loading experiments. Average strain computed around the screws was found to correlate strongly with number of cycles to failure, forming the basis for follow-up investigations of surgical variations.
Widmer J, Fasser M-R, Croci E, Spirig J, Snedeker JG, Farshad M. Individualized prediction of pedicle screw fixation strength with a finite element model. Comput Methods Biomech Biomed Engin. 2020;23:155–67.
Marcián P, Borák L, Zikmund T, Horáčková L, Kaiser J, Joukal M, et al. On the limits of finite element models created from (micro)CT datasets and used in studies of bone-implant-related biomechanical problems. J Mech Behav Biomed Mater. 2021;117:104393.
Wirth AJ, Müller R, Harry van Lenthe G. The discrete nature of trabecular bone microarchitecture affects implant stability. J Biomech. 2012;45:1060–7.
Ruffoni D, Wirth AJ, Steiner JA, Parkinson IH, Müller R, van Lenthe GH. The different contributions of cortical and trabecular bone to implant anchorage in a human vertebra. Bone. 2012;50:733–8.
Wirth AJ, Goldhahn J, Flaig C, Arbenz P, Müller R, van Lenthe GH. Implant stability is affected by local bone microstructural quality. Bone. 2011;49:473–8.
Wirth AJ, Müller R, van Lenthe GH. Augmentation of peri-implant bone improves implant stability: quantification using simulated bone loss. J Orthop Res. 2012;30:178–84.
Steiner JA, Christen P, Affentranger R, Ferguson SJ, van Lenthe GH. A novel in silico method to quantify primary stability of screws in trabecular bone. J Orthop Res. 2017;35:2415–24.
Chevalier Y, Matsuura M, Krüger S, Fleege C, Rickert M, Rauschmann M, et al. Micro-CT and micro-FE analysis of pedicle screw fixation under different loading conditions. J Biomech. 2018;70:204–11.
Wirth AJ, Mueller TL, Vereecken W, Flaig C, Arbenz P, Müller R, et al. Mechanical competence of bone-implant systems can accurately be determined by image-based micro-finite element analyses. Arch Appl Mech. 2010;80:513–25.
MacLeod AR, Serrancoli G, Fregly BJ, Toms AD, Gill HS. The effect of plate design, bridging span, and fracture healing on the performance of high tibial osteotomy plates. Bone Joint Res. 2019;7:639–49.
Märdian S, Schaser K-D, Duda GN, Heyland M. Working length of locking plates determines interfragmentary movement in distal femur fractures under physiological loading. Clin Biomech. 2015;30:391–6.
Matsuura Y, Rokkaku T, Suzuki T, Thoreson AR, An K-N, Kuniyoshi K. Evaluation of bone atrophy after treatment of forearm fracture using nonlinear finite element analysis: a comparative study of locking plates and conventional plates. The Journal of Hand Surgery. 2017;42:659.e1–9.
Schwarzenberg P, Klein K, Ferguson SJ, von Rechenberg B, Darwiche S, Dailey HL. Virtual mechanical tests out-perform morphometric measures for assessment of mechanical stability of fracture healing in vivo. J Orthop Res. 2021;39:727–38.
Shefelbine SJ, Simon U, Claes L, Gold A, Gabet Y, Bab I, et al. Prediction of fracture callus mechanical properties using micro-CT images and voxel-based finite element analysis. Bone. 2005;36:480–8.
Erdemir A, Mulugeta L, Ku JP, Drach A, Horner M, Morrison TM, et al. Credible practice of modeling and simulation in healthcare: ten rules from a multidisciplinary perspective. J Transl Med. 2020;18:369.
Henninger HB, Reese SP, Anderson AE, Weiss JA. Validation of computational models in biomechanics. Proc Inst Mech Eng H. 2010;224:801–12.
Viceconti M, Pappalardo F, Rodriguez B, Horner M, Bischoff J, Musuamba TF. In silico trials: verification, validation and uncertainty quantification of predictive models used in the regulatory evaluation of biomedical products. Methods. 2021;185:120–7.
Assessing credibility of computational modeling through verification and validation: application to medical devices. Am Soc Mech Eng; 2018.
Eberle S, Gerber C, von Oldenburg G, Hungerer S, Augat P. Type of hip fracture determines load share in intramedullary osteosynthesis. Clin Orthop Relat Res. 2009;467:1972–80.
Epari DR, Gurung R, Hofmann-Fliri L, Schwyn R, Schuetz M, Windolf M. Biphasic plating improves the mechanical performance of locked plating for distal femur fractures. J Biomech. 2021;115:110192.
Burkhart TA, Andrews DM, Dunning CE. Finite element modeling mesh quality, energy balance and validation methods: a review with recommendations associated with the modeling of bone tissue. J Biomech. 2013;46:1477–88.
Ernst M, Richards RG, Windolf M. Smart implants in fracture care - only buzzword or real opportunity? Injury. 2020;9021.
Liu SZ, Cao Q, Osgood GM, Siewerdsen JH, Stayman JW, Zbijewski W. Quantitative assessment of weight-bearing fracture biomechanics using extremity cone-beam CT. Proc SPIE Int Soc Opt Eng. 2020;11317.
Finnilä S, Moritz N, Strandberg N, Alm JJ, Aro HT. Radiostereometric analysis of the initial stability of internally fixed femoral neck fractures under differential loading. J Orthop Res. 2019;37:239–47.
Galea VP, Botros MA, McTague MF, Weaver MJ, Vrahas MS, Malchau H, et al. Radiostereometric analysis of stability and inducible micromotion after locked lateral plating of distal femur fractures. J Orthop Trauma. 2020;34:e60–6.
Zura R, Xiong Z, Einhorn T, Watson JT, Ostrum RF, Prayson MJ, et al. Epidemiology of fracture nonunion in 18 human bones. JAMA Surg. 2016;151:e162775.
Campbell ST, Lim PK, Kantor AH, Gausden EB, Goodnough LH, Park AY, et al. Complication rates after lateral plate fixation of periprosthetic distal femur fractures: a multicenter study. Injury. 2020;51:1858–62.
Giaretta S, Momoli A, Porcelli G, Micheloni GM. Diagnosis and management of periprosthetic femoral fractures after hip arthroplasty. Injury. 2019;50(Suppl 2):S29–33.
Albareda-Albareda J, Gabarre-Raso S, Rosell-Pradas J, Puértolas-Broto S, Ibarz-Montaner E, Redondo-Trasobares B, et al. Biomechanical behavior of retrograde intramedullary nails in distal femoral fractures. Injury. 2021
Ali AA, Cristofolini L, Schileo E, Hu H, Taddei F, Kim RH, et al. Specimen-specific modeling of hip fracture pattern and repair. J Biomech. 2014;47:536–43.
Arnone JC, Crist BD, Ward CV, El-Gizawy AS, Pashuck T, Rocca GJD. Variability of human femoral geometry and its implications on nail design. Injury. Elsevier; 2021;52:109–16.
Cordeiro M, Caskey S, Frank C, Martin S, Srivastava A, Atkinson T. Hybrid triad provides fracture plane stability in a computational model of a Pauwels type III hip fracture. Comput Methods Biomech Biomed Engin. 2020;23:476–83.
Gabarre S, Albareda J, Gracia L, Puértolas S, Ibarz E, Herrera A. Influence of gap size, screw configuration, and nail materials in the stability of anterograde reamed intramedullary nail in femoral transverse fractures. Injury. 2017;48(Suppl 6):S40–6.
Goffin JM, Pankaj P, Simpson AHRW, Seil R, Gerich TG. Does bone compaction around the helical blade of a proximal femoral nail anti-rotation (PFNA) decrease the risk of cut-out?: A subject-specific computational study. Bone Joint Res. 2013;2:79–83.
Herrera A, Albareda J, Gabarre S, Ibarz E, Puértolas S, Mateo J, et al. Comparative analysis of the biomechanical behavior of anterograde/retrograde nailing in supracondylar femoral fractures. Injury. 2020;51(Suppl 1):S80–8.
Lee WC, Chou SM, Tan CW, Chng LS, Yam GJM, Chua THI. Intertrochanteric fracture with distal extension: when is the short proximal femoral nail antirotation too short? Injury. 2020.
Li J, Yin P, Zhang L, Chen H, Tang P. Medial anatomical buttress plate in treating displaced femoral neck fracture a finite element analysis. Injury. 2019;50:1895–900.
Li J, Han L, Zhang H, Zhao Z, Su X, Zhou J, et al. Medial sustainable nail versus proximal femoral nail antirotation in treating AO/OTA 31-A2.3 fractures: finite element analysis and biomechanical evaluation. Injury. 2019;50:648–56.
Li J, Wang M, Zhou J, Zhang H, Li L. Finite element analysis of different screw constructs in the treatment of unstable femoral neck fractures. Injury. 2020;51:995–1003.
Mortazavi J, Farahmand F, Behzadipour S, Yeganeh A, Aghighi M. A patient specific finite element simulation of intramedullary nailing to predict the displacement of the distal locking hole. Med Eng Phys. 2018;55:34–42.
Peng MJ-Q, Xu H, Chen H-Y, Lin Z, Li X, Shen C, et al. Biomechanical analysis for five fixation techniques of Pauwels-III fracture by finite element modeling. Comput Methods Prog Biomed. 2020;193:105491.
Samsami S, Augat P, Rouhi G. Stability of femoral neck fracture fixation: a finite element analysis. Proc Inst Mech Eng H. 2019;233:892–900.
Sarwar A, Gee A, Bougherara H, Kuzyk PRT, Schemitsch EH, Zdero R. Biomechanical optimization of the far cortical locking technique for early healing of distal femur fractures. Med Eng Phys. 2021;89:63–72.
Wang C, Li X, Chen W, Wang C, Guo Y, Guo H. Three-dimensional finite element analysis of intramedullary nail with different materials in the treatment of intertrochanteric fractures. Injury. 2020;
Zeng W, Liu Y, Hou X. Biomechanical evaluation of internal fixation implants for femoral neck fractures: a comparative finite element analysis. Comput Methods Prog Biomed. 2020;196:105714.
Zhang W, Hao M, Chang Z, Wu Y, Tang P, Chen H. Comparison of a multidimensional cross locking plate versus a locking compression plate for the treatment of femoral shaft nonunion: finite element analysis. Med Eng Phys. 2020;83:106–11.
Goffin JM, Pankaj P, Simpson AH. The importance of lag screw position for the stabilization of trochanteric fractures with a sliding hip screw: a subject-specific finite element study. J Orthop Res. 2013;31:596–600.
Fjalestad T, Hole MØ, Hovden IAH, Blücher J, Strømsøe K. Surgical treatment with an angular stable plate for complex displaced proximal humeral fractures in elderly patients: a randomized controlled trial. J Orthop Trauma. 2012;26:98–106.
Handoll HH, Keding A, Corbacho B, Brealey SD, Hewitt C, Rangan A. Five-year follow-up results of the PROFHER trial comparing operative and non-operative treatment of adults with a displaced fracture of the proximal humerus. Bone Joint J. 2017;99-B:383–92.
Olerud P, Ahrengart L, Ponzer S, Saving J, Tidermark J. Internal fixation versus nonoperative treatment of displaced 3-part proximal humeral fractures in elderly patients: a randomized controlled trial. J Shoulder Elb Surg. 2011;20:747–55.
Kralinger F, Blauth M, Goldhahn J, Käch K, Voigt C, Platz A, et al. The influence of local bone density on the outcome of one hundred and fifty proximal humeral fractures treated with a locking plate. J Bone Joint Surg Am. 2014;96:1026–32.
Panagiotopoulou VC, Varga P, Richards RG, Gueorguiev B, Giannoudis PV. Late screw-related complications in locking plating of proximal humerus fractures: a systematic review. Injury. 2019;50:2176–95.
Krappinger D, Bizzotto N, Riedmann S, Kammerlander C, Hengg C, Kralinger FS. Predicting failure after surgical fixation of proximal humerus fractures. Injury. 2011;42:1283–8.
Hepp P, Lill H, Bail H, Korner J, Niederhagen M, Haas NP, et al. Where should implants be anchored in the humeral head? Clin Orthop Relat Res. 2003;415:139–47.
Kamer L, Noser H, Popp AW, Lenz M, Blauth M. Computational anatomy of the proximal humerus: an ex vivo high-resolution peripheral quantitative computed tomography study. J Orthop Translat. 2016;4:46–56.
Schiuma D, Brianza S, Tami AE. Development of a novel method for surgical implant design optimization through noninvasive assessment of local bone properties. Med Eng Phys. 2011;33:256–62.
Castro-Franco AD, Mendoza-Muñoz I, González-Ángeles Á, Cruz-Sotelo SE, Castañeda AM, Siqueiros-Hernández M. Trends in the characterization of the proximal humerus in biomechanical studies: a review. Appl Sci Multidisciplinary Digital Publishing Institute. 2020;10:6514.
Ye Y, You W, Zhu W, Cui J, Chen K, Wang D. The applications of finite element analysis in proximal humeral fractures. Comput Math Methods Med [Internet]. 2017 [cited 2021 Mar 25];2017. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5610852/
Chen H, Zhu Z, Li J, Chang Z, Tang P. Finite element analysis of an intramedulary anatomical strut for proximal humeral fractures with disrupted medial column instability: a cohort study. Int J Surg. 2020;73:50–6.
Chen Y-N, Chang C-W, Lin C-W, Wang C-W, Peng Y-T, Chang C-H, et al. Numerical investigation of fracture impaction in proximal humeral fracture fixation with locking plate and intramedullary nail. Int Orthop. 2017;41:1471–80.
Čukelj F, Knezević J, Kodvanj J, Bandalović A, Ostojić M, Bilan K, et al. Computer representation of osteosynthesis stability in locking plates used for the treatment of osteoporotic proximal humerus fractures. Psychiatria Danubina Medicinska Naklada Zagreb. 2014;26:14–9.
Feerick EM, Kennedy J, Mullett H, FitzPatrick D, McGarry P. Investigation of metallic and carbon fibre PEEK fracture fixation devices for three-part proximal humeral fractures. Med Eng Phys. 2013;35:712–22.
Fletcher JWA, Windolf M, Grünwald L, Richards RG, Gueorguiev B, Varga P. The influence of screw length on predicted cut-out failures for proximal humeral fracture fixations predicted by finite element simulations. Arch Orthop Trauma Surg. 2019;139:1069–74.
Fletcher JWA, Windolf M, Richards RG, Gueorguiev B, Buschbaum J, Varga P. Importance of locking plate positioning in proximal humeral fractures as predicted by computer simulations. J Orthop Res. 2019;37:957–64.
Fletcher JWA, Windolf M, Richards RG, Gueorguiev B, Varga P. Screw configuration in proximal humerus plating has a significant impact on fixation failure risk predicted by finite element models. J Shoulder Elb Surg. 2019;28:1816–23.
He Y, He J, Wang F, Zhou D, Wang Y, Wang B, et al. Application of additional medial plate in treatment of proximal humeral fractures with unstable medial column. Medicine (Baltimore) [Internet]. 2015 [cited 2021 Mar 25];94. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4616805/
He Y, Zhang Y, Wang Y, Zhou D, Wang F. Biomechanical evaluation of a novel dualplate fixation method for proximal humeral fractures without medial support. J Orthop Surg Res. 2017;12:72.
Jabran A, Peach C, Ren L. Biomechanical analysis of plate systems for proximal humerus fractures: a systematic literature review. Biomed Eng Online. 2018;17:47.
Kennedy J, Feerick E, McGarry P, FitzPatrick D, Mullett H. Effect of calcium triphosphate cement on proximal humeral fracture osteosynthesis: a finite element analysis. J Orthop Surg (Hong Kong). 2013;21:167–72.
Kim H, Lee W, Choi S, Kholinne E, Lee E, Alzahrani WM, et al. Role of additional inferomedial supporting screws in osteoporotic 3-part proximal humerus fracture: finite element analysis. Geriatr Orthop Surg Rehabil SAGE Publications Inc. 2020;11:2151459320956958.
Le L, Jabran A, Peach C, Ren L. Effect of screw thread length on stiffness of proximal humerus locking plate constructs: a finite element study. Med Eng Phys. 2019;63:79–87.
Maldonado ZM, Seebeck J, Heller MOW, Brandt D, Hepp P, Lill H, et al. Straining of the intact and fractured proximal humerus under physiological-like loading. J Biomech. 2003;36:1865–73.
Mendoza-Munoz I, Gonzalez-Angeles A, Gil-Samaniego-Ramos M, L-Avitia R, Gonzalez-Toxqui C. Evaluation of significant effects on locking plates design for a 2-part fracture of the surgical neck of the humerus using finite element and statistical analysis. Biomedical Research; 2018 [cited 2021 Mar 25]; Available from: https://www.biomedres.info/abstract/evaluation-of-significant-effects-on-locking-plates-design-for-a-2part-fracture-of-the-surgical-neck-of-the-humerus-using-finite-e-10296.html
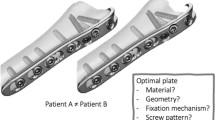
Mischler D, Babu S, Osterhoff G, Pari C, Fletcher J, Windolf M, et al. Comparison of optimal screw configurations in two locking plate systems for proximal humerus fixation - a finite element analysis study. Clin Biomech (Bristol, Avon). 2020;78:105097.
Mischler D, Windolf M, Gueorguiev B, Nijs S, Varga P. Computational optimisation of screw orientations for improved locking plate fixation of proximal humerus fractures. J Orthop Translat. 2020;25:96–104.
Tilton M, Armstrong AD, Wee H, Hast MW, Manogharan G, Lewis GS. Finite element-predicted effects of screw configuration in proximal humerus fracture fixation. Journal of Biomechanical Engineering [Internet]. 2020 [cited 2021 Mar 25];142. Available from: https://doi.org/10.1115/1.4045907
Tilton M, Lewis GS, Bok Wee H, Armstrong A, Hast MW, Manogharan G. Additive manufacturing of fracture fixation implants: design, material characterization, biomechanical modeling and experimentation. Additive Manufacturing. 2020;33:101137.
Varga P, Inzana JA, Fletcher JWA, Hofmann-Fliri L, Runer A, Südkamp NP, et al. Cement augmentation of calcar screws may provide the greatest reduction in predicted screw cut-out risk for proximal humerus plating based on validated parametric computational modelling: augmenting proximal humerus fracture plating. Bone Joint Res. 2020;9:534–42.
Yang P, Zhang Y, Liu J, Xiao J, Ma LM, Zhu CR. Biomechanical effect of medial cortical support and medial screw support on locking plate fixation in proximal humeral fractures with a medial gap: a finite element analysis. Acta Orthop Traumatol Turc. 2015;49:203–9.
Zhang Y-K, Wei H-W, Lin K-P, Chen W-C, Tsai C-L, Lin K-J. Biomechanical effect of the configuration of screw hole style on locking plate fixation in proximal humerus fracture with a simulated gap: a finite element analysis. Injury. 2016;47:1191–5.
Gross T, Pahr DH, Peyrin F, Zysset PK. Mineral heterogeneity has a minor influence on the apparent elastic properties of human cancellous bone: a SRμCT-based finite element study. Comput Methods Biomech Biomed Engin. 2012;15:1137–44.
Perren SM. Evolution of the internal fixation of long bone fractures. The scientific basis of biological internal fixation: choosing a new balance between stability and biology. J Bone Joint Surg (Br). 2002;84:1093–110.
Baumann AP, Graf T, Peck JH, Dmitriev AE, Coughlan D, Lotz JC. Assessing the use of finite element analysis for mechanical performance evaluation of intervertebral body fusion devices. JOR Spine. 2021;4:e1137.
Funding
GSL, HW, and JSR were supported by the National Institute of Biomedical Imaging and Bioengineering (1R01EB029207-01). DM and PV were supported by the AO Foundation via the AOTRAUMA Network (Grant No.: AR 2018/01).
Author information
Authors and Affiliations
Contributions
Not applicable
Corresponding author
Ethics declarations
Conflict of Interest
GSL receives research support for an unrelated project from Arthrex Inc. GSL and JSR are co-inventors on the patent: “Individualized preoperative planning system and method.” JSR and GSL have received materials for a biomechanical research project from Depuy Synthes (Johnson and Johnson). JSR is consultant for Depuy Synthes (Johnson and Johnson) and Osteocentric, and stockholder for ROMtech. None of the above indirectly related interests has influenced the present paper. No other competing interests are present.
Human and Animal Rights and Informed Consent
All procedures performed by the authors in studies involving human or animal subjects were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Biomechanics
Supplementary Information
Supplementary Table 1
(XLSX 20 kb)
Supplementary Table 2
(XLSX 20 kb)
Rights and permissions
About this article
Cite this article
Lewis, G.S., Mischler, D., Wee, H. et al. Finite Element Analysis of Fracture Fixation. Curr Osteoporos Rep 19, 403–416 (2021). https://doi.org/10.1007/s11914-021-00690-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11914-021-00690-y