Abstract
Background
Adaptations of dynamic balance performance are related to sway excursions in older adults with chronic low back pain (LBP). However, there is a lack of understanding on postural control within different thresholds of radius from the center of pressure (COP).
Purpose
This study was conducted to compare the normalized stability based on the time-in-boundary (TIB) during repeated unilateral limb standing trials between subjects with and without chronic LBP.
Methods
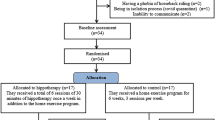
There were 26 older adults with LBP and 39 control subjects who completed three trials of repeated unilateral limb standing on a force plat.
Results
The TIB based on the seven thresholds was analyzed, and the groups demonstrated a significant interaction on thresholds for TIB (F = 8.76, p = 0.01). The TIB was significantly different in the 10 mm (F = 4.01, p = 0.04), 15 mm (F = 5.21, p = 0.03), and 20 mm (F = 4.48, p = 0.04) radius of thresholds only in the second trial. However, there was no group difference on TIB at the first and third trials due to potential compensatory and/or adaptive reactions to avoid fall risks.
Conclusion
The LBP group lacked postural stability within the thresholds less than a 20 mm radius at the second trial of unilateral standing. The significant group interaction with the thresholds indicates an adaptation strategy on sway thresholds. This postural reaction from repeated trials should be considered with sway excursion adjustments and fall prevention in older adults with LB.




Similar content being viewed by others
Data availability
The data that support the findings of this study are not openly available due to the conditions of ethics approval for the study and current data protection legislation. Dependent on compliance with data protection legislation and ethical approval, they may be available from the corresponding author upon reasonable request.
References
Weiner DK, Rudy TE, Morrow L, Slaboda J, Lieber S (2006) The relationship between pain, neuropsychological performance, and physical function in community-dwelling older adults with chronic low back pain. Pain Med 7:60–70
Ge L, Wang C, Zhou H, Yu Q, Li X (2021) Effects of low back pain on balance performance in elderly people: a systematic review and meta-analysis. Eur Rev Aging Phys Act 18:8
Hlaing SS, Puntumetakul R, Wanpen S, Boucaut R (2020) Balance control in patients with subacute non-specific low back pain, with and without lumbar instability: a cross-sectional study. J Pain Res 13:795–803
Muir SW, Berg K, Chesworth B, Klar N, Speechley M (2010) Application of a fall screening algorithm stratified fall risk but missed preventive opportunities in community-dwelling older adults: a prospective study. J Geriatr Phys Ther 33:165–172
Montero-Odasso MM, Kamkar N, Pieruccini-Faria F, Osman A, Sarquis-Adamson Y, Close J et al (2021) Evaluation of clinical practice guidelines on fall prevention and management for older adults: a systematic review. JAMA Netw Open 4:e2138911
Beauchet O, Fantino B, Allali G, Muir SW, Montero-Odasso M, Annweiler C (2011) Timed up and go test and risk of falls in older adults: a systematic review. J Nutr Health Aging 15:933–938
Berenshteyn Y, Gibson K, Hackett GC, Trem AB, Wilhelm M (2019) Is standing balance altered in individuals with chronic low back pain? A Syst Rev Disabil Rehabil 41:1514–1523
da Silva RA, Vieira ER, Fernandes KBP, Andraus RA, Oliveira MR, Sturion LA et al (2018) People with chronic low back pain have poorer balance than controls in challenging tasks. Disabil Rehabil 40:1294–1300
Michikawa T, Nishiwaki Y, Takebayashi T, Toyama Y (2009) One-leg standing test for elderly populations. J Orthop Sci 14:675–685
Mancini M, Horak FB (2010) The relevance of clinical balance assessment tools to differentiate balance deficits. Eur J Phys Rehabil Med 46:239–248
Hertel J, Olmsted-Kramer LC (2007) Deficits in time-to-boundary measures of postural control with chronic ankle instability. Gait Posture 25:33–39
Peterson DS, Phan V, Richmond SB, Lee H (2021) Effects of dual-tasking on time-to-boundary during stance in people with PD: a preliminary study. Clin Biomech 88:105420
Hou ZC, Su T, Ao YF, Hu YL, Jiao C, Guo QW et al (2022) Arthroscopic modified Brostrom procedure achieves faster return to sports than open procedure for chronic ankle instability. Knee Surg Sports Traumatol Arthrosc 30:3570–3578
Arnold BL, De La Motte S, Linens S, Ross SE (2009) Ankle instability is associated with balance impairments: a meta-analysis. Med Sci Sports Exerc 41:1048–1062
Song K, Burcal CJ, Hertel J, Wikstrom EA (2016) Increased visual use in chronic ankle instability: a meta-analysis. Med Sci Sports Exerc 48:2046–2056
Richmond SB, Dames KD, Shad JM, Sutherlin MA, Fling BW (2020) Setting boundaries: utilization of time to boundary for objective evaluation of the balance error scoring system. J Sports Sci 38:21–28
Meinke A, Maschio C, Meier ML, Karlen W, Swanenburg J (2022) The association of fear of movement and postural sway in people with low back pain. Front Psychol 13:1006034
Lascurain-Aguirrebena I, Newham D, Critchley DJ (2016) Mechanism of action of spinal mobilizations: a systematic review. Spine 41:159–172
Sung PS, Spratt KF, Wilder DG (2004) A possible methodological flaw in comparing dominant and nondominant sided lumbar spine muscle responses without simultaneously considering hand dominance. Spine 29:1914–1922
Promsri A, Haid T, Federolf P (2018) How does lower limb dominance influence postural control movements during single leg stance? Hum Mov Sci 58:165–174
Fairbank JC (2014) Oswestry disability index. J Neurosurg Spine 20:239–241
Moghadam M, Ashayeri H, Salavati M, Sarafzadeh J, Taghipoor KD, Saeedi A et al (2011) Reliability of center of pressure measures of postural stability in healthy older adults: effects of postural task difficulty and cognitive load. Gait Posture 33:651–655
Blodgett JM, Ventre JP, Mills R, Hardy R, Cooper R (2022) A systematic review of one-legged balance performance and falls risk in community-dwelling adults. Ageing Res Rev 73:101501
Ferreira RN, Ribeiro NF, Figueiredo J, Santos CP (2022) Provoking artificial slips and trips towards perturbation-based balance training: a narrative review. Sensors 22:9254
Sung PS, Leininger PM (2015) A kinematic and kinetic analysis of spinal region in subjects with and without recurrent low back pain during one leg standing. Clin Biomech 30:696–702
da Silva RA, Vieira ER, Leonard G, Beaulieu LD, Ngomo S, Nowotny AH et al (2019) Age- and low back pain-related differences in trunk muscle activation during one-legged stance balance task. Gait Posture 69:25–30
Sung PS, Yoon B, Lee DC (2010) Lumbar spine stability for subjects with and without low back pain during one-leg standing test. Spine 35:E753–E760
Ostrowska B, Giemza C, Wojna D, Skrzek A (2008) Postural stability and body posture in older women: comparison between fallers and non-fallers. Ortop Traumatol Rehabil 10:486–495
Maiers M, Forte ML (2021) Association between psychosocial parameters and response to chiropractic care among older adults with chronic low back pain: secondary analysis of a randomized clinical trial. J Manip Physiol Ther 44:675–682
Sung PS, Park MS (2023) Delayed response in rectus abdominis muscle following a step perturbation in subjects with and without recurrent low back pain. Eur Spine J 32:1842–1849
Langevin HM (2021) Reconnecting the brain with the rest of the body in musculoskeletal pain research. J Pain 22:1–8
van Dieen JH, Reeves NP, Kawchuk G, van Dillen LR, Hodges PW (2019) Motor control changes in low back pain: divergence in presentations and mechanisms. J Orthop Sports Phys Ther 49:370–379
Acknowledgements
The authors thank the subjects at Indiana Wesleyan University as well as Dr. Phyllis Rowland, Matt Lavin and the students in the Doctoral Program in Physical Therapy for their technical assistance for data analyses and contributions to the study.
Funding
This study was supported by the Scholarship Council, Lilly Faculty Scholarship Award at Indiana Wesleyan University (2573877).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has any financial or personal conflicts of interest in relation to the submission, other people, or any organizations.
Ethical approval
Ethics approval for the study was granted from the Indiana Wesleyan University Institutional Review Board (Project ID: (#1653.21; approval date: 12 October 2022). All study participants provided written informed consent to partake in the study. The study adhered to the Declaration of Helsinki on ethical principles for medical research involving human subjects.
Consent to participate
All subjects provided written, explicit, informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lee, D., Sung, P.S. Postural adaptations within normalized stability between older adults with and without chronic low back pain. Eur Spine J 32, 4420–4427 (2023). https://doi.org/10.1007/s00586-023-07939-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07939-3