Abstract
Purpose
In vivo studies of continuous lumbar sagittal plane motion have found passive intervertebral motion to be more uneven in patients with chronic nonspecific low back pain (CNSLBP) than healthy controls, but the mechanisms are unclear. This study aimed to compare patients with CNSLBP with a matched group of pain-free controls for intervertebral restraint during passive recumbent bending.
Methods
Seventeen patients with CNSLBP and minimal disc degeneration who had quantitative fluoroscopy investigations were matched to 17 healthy controls from a database acquired using the same imaging protocol. The entire database (n = 136) was examined for clustering of peaking times, magnitudes and ROM of the first derivatives of the intervertebral angle/motion curves (PTFD, PMFD and ROM) during flexion and return that might introduce confounding. The groups were then compared for differences in these variables.
Results
There were significant segmental ROM differences among clusters in the database when PMFD and ROM were used as clustering variables, indicating heterogeneity. However, in the patient–control study, it was PTFD (velocity) that differentiated the groups. At L5-S1, this was at 10.82% of the motion path compared with 25.06% in the controls (p = 0.0002). For L4-5, PTFD was at 23.42% of the motion path in patients and 16.33% in controls (p = 0.0694) suggesting a reduced initial bending moment there. There were no significant differences for PMFD or ROM.
Conclusion
Peaking time of passive intervertebral velocity occurs early at L5-S1 in patients with CNSLBP; however, these findings should be treated with caution pending their replication. Future studies should explore relationships with altered disc pressures and biochemistry. Usefulness for monitoring regenerative disc therapies should be considered.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Nonspecific low back pain is a multifaceted disorder with the highest population impact on Years Lived with Disability [1]. Mechanical abnormalities linked to degeneration are suspected of playing a part, but there has been little objective evidence of this in terms of the usual measures of mechanical disruption (i.e. reduced disc pressure, increased range of motion (ROM), translation and laxity) [2,3,4]. However, lesser disruption, resulting in disco-ligamentous sub-failure, has been suggested as an underlying contributor to pain [5]. In a review of the role of biomechanics in intervertebral disc degeneration and regenerative therapies, Iatridis et al. emphasised the importance of disc pressure loss and the need for safe and minimally invasive interventions that may mitigate or repair structural defects at earlier stages of degeneration, where instability has been found to be more prevalent [6, 7]. However, how early-stage loss of intervertebral restraint would be monitored in lesser degenerative states is unclear.
Exploration of the microinjury concept in chronic back pain has prompted studies of relationships between abnormal intervertebral velocities and disc pressures and the material properties of passive spinal tissues [8,9,10,11]. There is evidence from histologic studies that the disc annulus undergoes greater damage under rapid loading than under quasistatic loading, signalling the importance of velocity in intervertebral kinematics and the need to take account of this in vivo [12]. A finite element study by Mithani et al. [13] found that changes to the material properties of passive spinal tissues elicit compensatory changes in lumbar intervertebral ranges, “underscoring the significance of passive tissue properties in regulating segmental mobility and geometric compensation to maintain spinal congruency”. This has also been proposed as a plausible mechanism underlying the development of low back pain.
Two studies of passive lumbar flexion have revealed a biomarker for chronic, nonspecific low back pain (CNSLBP) in the form of motion sharing inequality (MSI) across the range in patients with CNSLBP during passive recumbent motion. This also suggests the involvement of passive intervertebral restraint [2, 14]. MSI is measured using quantitative fluoroscopy (QF). Moving vertebral images are digitised semi-automatically and processed using a custom algorithm to output the intervertebral motion patterns in terms of rotation, translation and finite centre of rotation [15, 16]. MSI is a measure that has been added to this and is fully described in Breen 2018 [14]. It consists of the average difference between the largest and smallest shares of segmental motion that is accepted by intervertebral levels from L2-S1 across the whole bending sequence. When applied during passive recumbent motion, it is a summary measure of the evenness of intervertebral passive restraint.
The QF technology responds to the need to reduce measurement variability when comparing small amounts of intervertebral displacement [17,18,19,20]. Early weight-bearing fluoroscopic studies explored the inflexion points of intervertebral rotation curves in small numbers of healthy participants and proposed normal patterns for these as a top-down cascade during flexion [21, 22]. Recently, four significantly different spatiotemporal clusters of peak intervertebral rotation velocities were found in a sample of healthy controls during standing QF (n-127) [23]. Reminiscent of the previous studies, the greatest proportion of these also exhibited a top-down cascade of peak velocities during standing flexion.
The MSI variable, measured in the passive recumbent configuration, is highly correlated with age and degree of disc degeneration, but in CNSLP patients only, indicating a biomarker for CNSLBP [14]. In addition, a multivariate analysis of continuous passive intervertebral motion data comparing CNSLBP sufferers and controls confirmed the presence of an acceleration/deceleration principal component in the measurement of passive restraint between vertebrae, supporting the prospect of an additional kinematic biomarker [24].
As a basis for conducting patient-specific comparisons, two open-source reference databases of standardised, continuous lumbar intervertebral rotational motion (presented as midplane angles) in 136 healthy volunteers during flexion and extension have been published [25]. One was recorded using QF during passive recumbent motion and the other during weight-bearing active motion in the same population. The present study investigated the prospect of making patient-specific comparisons based on spatiotemporal interactions, based on ranges and velocities, between levels compared with the passive recumbent database. It was first, however, necessary to determine if there are spatiotemporal clusters of movement patterns in the database, suggesting inhomogeneity.
The main purpose of this study was, therefore, to compare a matched subgroup of healthy controls to a group of patients with treatment-resistant CNSLBP who received the same passive recumbent QF examination in an investigation to inform their management. The aims were: (1) to assess the passive recumbent database for the absence of significant clusters indicating heterogeneity and (2) to compare the degree of altered passive restraint in a population of CNSLBP patients compared to healthy controls for velocity and range peaking points. The hypotheses were that there would be (1) no significant clusters in the passive recumbent normative database and (2) statistically significant differences between patients and controls for peaking points within intervertebral levels.
Methods
Participants
One hundred and thirty-six healthy volunteers were recruited from staff, students and visitors at our institution and received passive recumbent and weight-bearing active quantitative fluoroscopy (QF) scans. Radiographic disc degeneration was assessed from the fluoroscopic images for all participants using the Kellgren and Lawrence scale [26]. Seventeen of those in the passive recumbent study were matched in pairs to a group of 17 patients with CNSLBP and minimal disc degeneration for age, sex and BMI for a sub-study of spatiotemporal differences between patients and controls. The study received a favourable ethical opinion (National Research Ethics Service South-West 3, REC reference10/H0106/65).
Inclusion criteria
All participants were males and females aged 18–71 with minimal radiographic evidence of disc degeneration, no medical radiation exposure of > 8 mSv in the previous 2 years, no pregnancy (females) and having given informed consent. Controls had to have been free of any back pain that limited their normal activity for more than 1 day in the previous year. Patients had to have been referred to investigate treatment-resistant back pain of more than 3 months’ duration as specified by the referrer. Patients whose pain was associated with nerve compression or serious spinal pathology were excluded.
Data collection and image analysis
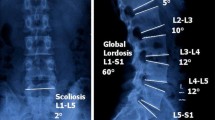
All participants received the same standardised passive recumbent flexion and return lumbar fluoroscopy examination as previously described [14] (Fig. 1). The image analysis involved a semi-automated tracking process to determine the position of each vertebra (L2, L3, L4, L5 and S1) in each recorded image during the flexion and return motion. The midplane angles of all vertebrae were then extracted and smoothed using a Tikhonov regularisation to reduce noise in the output [27].
Participant positioned for passive recumbent flexion motion recording: a neutral position and b fully flexed (40o) position (from Breen and Breen [2])
Kinematic analysis
The kinematic analysis of the passive recumbent midplane angles database followed a similar protocol to the weight-bearing active one [23]. The spatiotemporal variables chosen for comparison at each level from L2-3 to L5-S1 were in terms of the peak intervertebral ranges and velocities as follows: (1) the peak range of motion (ROM) (o), wherever it occurred in the sequence, (2) the time in the sequence (%) of the peaking of the first derivative (PTFD) of the angle/% motion curve (velocity) and (3) the peak magnitude (o) of the first derivative (PMFD)(velocity) of the peak velocity across the sequence wherever it occurred.
Statistical analysis
A custom algorithm was used to cluster the passive recumbent normative study participants based on these three variables to investigate the possible existence of clusters as was found in the weight-bearing normative study of the same participants [23]. The Shapiro–Wilk test was used to assess normality in the patient–control populations. Normally distributed spatiotemporal data were compared using two-sided paired t-tests and non-normal data using the Wilcoxon rank-sum test. All statistical analyses were performed using SPSS software (version 27, Chicago, Il).
Peaking times and magnitudes of the first derivative (velocity) of the rotational motion of each motion segment taken separately (PTFD), along with the ranges of motion (ROM and PMFD), were calculated and compared between the 17 patients with CNSLBP and 17 matched controls from the normative study during flexion and return motion. Statistical parametric mapping (SPM) was used to test the significance of differences between patients and controls’ time-series data (spm1d.stats.ttest) using the open-source software package: (https://www.spm1d.org) [28].
Results
There were 136 healthy volunteers in the recumbent reference database (68 males, mean age 43 (sd 13) and mean BMI 25 (sd 2.33); 68 females, mean age 43 (sd 13) and mean BMI 23 (sd 3.05)). The results of the analyses for motion clusters of the three spatiotemporal variables for both outward and return motion are shown in Supplementary Material. Although there were several spatiotemporal clusters for ROM, PTFD and PMFD, none of the PTFD clusters was significant (p > 0.05), indicating greater population homogeneity for this variable than in the weight-bearing database [23].
The matching demographics of reference, normative and sub-study populations are shown in Table 1. There were no significant differences between patients and controls in terms of age, sex, height, weight or BMI. However, two of the patients and two of the controls in the sub-study had a small amount of disc degeneration at one or two levels.
Comparison of spatiotemporal variables of patients and controls
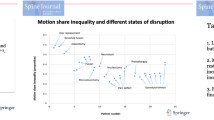
Table 2 shows that the median velocity peaking time for flexion PTFD for L4-5 was at 23.42% of the motion in patients and 16.33% of the motion in controls (p = 0.0694). For L5-S1, the mean velocities were at 10.82% in patients and 25.06% in controls (p = 0.0002). There were no significant differences for any variable during the return phase, although a slightly greater mean value for L4-5 PMFD in patients approached significance (p = 0.0808).
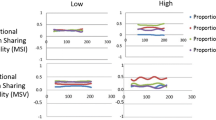
Figure 2a–d shows the ensemble means of the intervertebral velocities in patients and controls from L2-3 to L5-S1 throughout passive recumbent flexion and return motion in patients and controls. SPM showed that only differences in velocities towards the end of the return phase at L4-5 were statistically significant (p < 0.015) (Fig. 3a–d).
Figure 4a–d shows the ensemble means of the magnitudes and locations of the motion ranges of these levels for flexion and return. These found symmetrical patterns in both patients and controls, but no significant differences between them for range or magnitude (p > 0.05).
Discussion
Healthy control reference study
The population of healthy controls in this study showed different patterns of velocities in the previous weight-bearing study (Fig. 5a) compared to the recumbent configuration of the same population (Fig. 5b) [23]. The distribution of PTFD/velocity peaking points in the previous weight-bearing study also portrayed a top-down cascade (Fig. 6a), unlike the similar peaking points at all levels in the current recumbent reference study (Fig. 6b). The passive recumbent population also showed no statistically significant spatiotemporal clusters for PTFD, where there were significantly different peaking times at L4-5 and L5-S1 between patients and controls (Table 2). This means that the passive recumbent method for measuring restraint confers greater homogeneity for PTFD and is less likely to result in confounding when making comparisons with other population groups and supports Hypothesis 1 for this variable.
Patient–control sub-study
The patient/control sub-study was equally represented in terms of age, gender and BMI. The significant differences in PTFD (velocity peaking times) at L5-S1 between patients and controls during passive recumbent flexion thus represent a further biomarker for CNSLBP in populations with minimal disc degeneration, which, like the MSI measure, is based on pure restraint. However, the ranges of motion (ROM) and peak magnitudes of the velocities (PMFD) were not significantly different in patients at any level, and no significant differences were found during the return phase.
These findings, together with the uneven motion sharing biomarker found previously, suggest that early peaking of passive flexion velocity at L5-S1 and (probably) late peaking at L4-5 occur more frequently in people with CNSLBP and are associated with reduced restraint of flexion at L5-S1, supporting Hypothesis 2. This seems consistent with the microstructural sub-failure concept of chronic back pain and the higher frequency of disc degeneration at these levels in older populations [29]. It also seems consistent with a reduction in intradiscal pressure at L5-S1, resulting in a compensatory reduction in passive stiffness in the neutral zone and a compensatory delay in peak velocity at L4-5 above [13].
Experiments in the rat model found that a stab lesion to the disc annulus resulted in significantly reduced peak stiffness, peak moment and hysteresis in all directions [30]. However, while this provides evidence of links between disc injury and biomechanical changes, it may have less in common with the more intrinsic mechanisms that might be expected in the less destructive disc microstructural changes that may have been present in this study.
Deconstructing the biomarker
Imaging studies of disc deformation, biochemical change and the environment for neuropathic pain generation have suggested links to disc disruption in back pain and its kinematics [3, 31,32,33]. Recent in vivo intervertebral kinematic studies have advocated comparison of the functional integrity of motion segments in symptomatic and asymptomatic populations: For example, it has been shown that in pain-free populations, there is no correlation between ROM, translation, laxity or MSI and degree of disc degeneration up to moderate levels [34]. However, in patients with treatment-resistant CNSLBP, there is a high correlation between disc degeneration and passive recumbent MSI, significantly higher levels of MSI and (in the present study), earlier peak L5-S1 passive flexion velocities [2, 14]. These findings suggest a biomarker for CNSLBP and prompt the question of whether the early peaking of L5-S1 velocity in CNSLBP patients is also accompanied by lowered intradiscal pressure [35]. If so, this would confirm a further relationship between kinematics and early structural disruption in vivo and may provide a way of monitoring the clinical course of CNSLBP and/or the outcome of regenerative disc therapies [6].
Limitations and further work
This is the first study to compare intervertebral spatiotemporal interactions in patients and controls in vivo in terms of pure restraint. However, its findings should be treated with caution, and it would be advisable to replicate the sub-study to ensure that the findings are robust. This could be achieved by matching an additional patient cohort with minimal disc degeneration to a further set of controls from the same database, which is publicly available [25]. If they are, the next step would be to generate hypotheses around its relationship between these altered peak velocities, and some of the factors described above [35]. What mainly remains to be understood is what drives the relationships between CNSLBP, velocity peaking time (PTFD) during passive recumbent intervertebral motion, MSI and early disc degeneration. Another route for further research could, therefore, be to investigate possible relationships between indicators of lowered intradiscal pressure, increased neutral zone slope and length (measured as laxity or initial attainment rate in vivo) and lowered L5-S1 velocity peaking times in patients [36, 37]. This may confirm or otherwise relationships between kinematics and early structural disruption in vivo. Such investigations could use MRI to assess biochemical markers and QF the kinematic markers. Together, these could constitute additional minimally invasive methods to better understand and monitor disc health, regeneration and repair.
Conclusion
This study found that in vivo intervertebral rotational velocity during passive recumbent flexion in healthy controls to be homogeneous across the motion sequence for velocity peaking time and thus unlikely to confound clinical studies that depend on this variable for normative values. In patients with CNSLBP, rotational velocity reaches its peak significantly earlier at L5-S1 than in healthy controls. This may be due to changes in intervertebral disc structure and function and indicate relationships between passive disc restraint and the mechanisms of CNSLBP. These findings could be used to help guide future research into the relationships between intervertebral kinematics, disc microstructure and CNSLBP, as well as to monitor the mechanical effects of therapies that target the disc.
References
Ferreira ML, Luca K de, Haile L, et al (2023) Global, Regional, and National Burden of Low Back Pain, 1990–2020, Its Attributable Risk Factors, And Projections to 2050: A Systematic Analysis of the Global Burden of Disease Study 2021. https://doi.org/10.2139/ssrn.4318392
Breen A, Mellor F, Breen AC (2018) Aberrant intervertebral motion in patients with treatment-resistant nonspecific low back pain: a retrospective cohort study and control comparison. Eur Spine J 27:2831–2839. https://doi.org/10.1007/s00586-018-5666-1
Brayda-Bruno M, Tibiletti M, Ito K et al (2014) Advances in the diagnosis of degenerated lumbar discs and their possible clinical application. Eur Spine J 23:315–323. https://doi.org/10.1007/s00586-013-2960-9
Oxland TR, Niosi CA (2004) Degenerative mechanics of the lumbar spine. Spine J 4:202S-208S. https://doi.org/10.1016/j.spinee.2004.07.013
Panjabi MM (2006) A hypothesis of chronic back pain: ligament subfailure injuries lead to muscle control dysfunction. Eur Spine J 15:668–676. https://doi.org/10.1007/s00586-005-0925-3
Iatridis JC, Nicoll SB, Michalek AJ, Walter BA, Gupta MS (2013) Role of biomechanics on intervertebral disc degeneration and regenerative therapies: what needs repairing in the disc and what are promising biomaterials for its repair? Spine J 13:243–262. https://doi.org/10.1016/jspinee.2012.12.002
Iguchi T, Kanemura A, Kasahara K et al (2003) Age distribution of three radiologic factors for lumbar instability: probable aging process of the instability with disc degeneration. Spine 23:2628–2633. https://doi.org/10.1097/01.BRS.0000097162.80495.66
Zhou M, Archibeck ES, Feteih Y et al (2023) Non-enzymatic glycation increases the failure risk of annulus fibrosus by predisposing the extrafibrillar matrix to greater stresses. Acta Biomater 168:223–234. https://doi.org/10.1016/j.actbio.2023.07.003
Ellingson AM, Mehta H, Polly DW et al (2013) Disc degeneration assessed by Quantitative T2* (T2 star) correlated with functional lumbar mechanics. Spine 38:E1533–E1540. https://doi.org/10.1097/brs.0b013e3182a59453
Mulholland RC, McNally DS, Shackleford IM, Goodship AE (1996) In vivo stress measurement can predict pain on discography. Spine 21:2580–2587
Tanaka N, An HS, Lim T-H et al (2001) The relationship between disc degeneration and flexibility of the lumbar spine. Spine J 1:47–56. https://doi.org/10.1016/S1529-9430(01)00006-7
McMorran J (2023) An exploration of the link between vertebral endplate fracture, velocity, and health of the intervertebral disc. Dissertation, Wilfred Laurier University
Mithani A, Aoude A, Driscoll M (2023) Impact of passive spinal soft tissues on spinal geometric compensation: a finite element modeling investigation. https://doi.org/10.36227/techrxiv.23206988.v1
Breen A, Breen A (2018) Uneven intervertebral motion sharing is related to disc degeneration and is greater in patients with chronic, non-specific low back pain: an in vivo, cross-sectional cohort comparison of intervertebral dynamics using quantitative fluoroscopy. Eur Spine J 27:145–153. https://doi.org/10.1007/s00586-017-5155-y
Breen A, Breen A (2016) Accuracy and repeatability of quantitative fluoroscopy for the measurement of sagittal plane translation and finite centre of rotation in the lumbar spine. Med Eng Phys 38:607–614. https://doi.org/10.1016/j.medengphy.2016.03.009
Breen AC, Teyhen DS, Mellor FE, Breen AC, Wong K, Deitz A (2012) Measurement of inter-vertebral motion using quantitative fluoroscopy: report of an international forum and proposal for use in the assessment of degenerative disc disease in the lumbar spine. Adv Orthop. https://doi.org/10.1155/2012/802350
du Rose A, Breen A (2016) Relationships between lumbar inter-vertebral motion and lordosis in healthy adult males: a cross sectional cohort study. BMC Musculoskelet Disord 17:121. https://doi.org/10.1186/s12891-016-0975-1
Yeager MS, Cook DJ, Cheng BC (2014) Reliability of computer-assisted lumbar intervertebral measurements using a novel vertebral motion analysis system. Spine J 14:274–281. https://doi.org/10.1016/j.spinee.2013.10.048
Breen A, Hemming R, Mellor F, Breen A (2019) Intrasubject repeatability of in vivo intervertebral motion parameters using quantitative fluoroscopy. Eur Spine J 28:450–460. https://doi.org/10.1007/s00586-018-5849-9
To D, Breen A, Breen A, Mior S (2020) Investigator analytic repeatability of two new intervertebral motion biomarkers for chronic, nonspecific low back pain in a cohort of healthy controls. Chiropr Man Ther. https://doi.org/10.1186/s12998-020-00350-5
Harada M, Abumi K, Ito M, Kaneda K (2000) Cineradiographic motion analysis of normal lumbar spine during forward and backward flexion. Spine 25:1932–1937. https://doi.org/10.1097/00007632-200008010-00011
Kanayama M, Abumi K, Kaneda K et al (1996) Phase lag of the intersegmental motion in flexion-extension of the lumbar and lumbosacral spine. An In Vivo Study Spine 21:1416–1422. https://doi.org/10.1097/00007632-199606150-00004
Nematimoez M, Breen A, Breen A (2023) Spatio-temporal clustering of lumbar intervertebral flexion interactions in 127 asymptomatic individuals. J Biomech 154:111634. https://doi.org/10.1016/j.jbiomech.2023.111634
Brownhill K, Mellor F, Breen A, Breen A (2020) Passive intervertebral motion characteristics in chronic mid to low back pain: a multivariate analysis. Méd Eng Phys 84:115–125. https://doi.org/10.1016/j.medengphy.2020.08.006
Breen A, Breen A (2022) Reference database of continuous vertebral flexion and return. Open Sci Framew. https://doi.org/10.17605/OSF.IO/A27PY
Kellgren JH, Lawrence JS (1958) Osteo-arthrosis and disk degeneration in an Urban population *. Ann Rheum Dis 17:388. https://doi.org/10.1136/ard.17.4.388
Eilers PH (2003) A perfect smoother. Anal Chem 75(14):3631–3636
Pataky TC, Robinson MA, Vanrenterghem J (2013) Vector field statistical analysis of kinematic and force trajectories. J Biomech 46:2394–2401. https://doi.org/10.1016/j.jbiomech.2013.07.031
Teraguchi M, Yoshimura N, Hashizume H et al (2014) Prevalence and distribution of intervertebral disc degeneration over the entire spine in a population-based cohort: the Wakayama Spine Study. Osteoarthr Cartil 22:104–110. https://doi.org/10.1016/j.joca.2013.10.019
Xiao F, van Dieën JH, Han J, Maas H (2023) Stab lesion of the L4/L5 intervertebral disc in the rat causes acute changes in disc bending mechanics. J Biomech. https://doi.org/10.1016/j.jbiomech.2023.111830
Singer KPF, Song PJ, Monsas S, Johansson A, Haukalid L, Price RI (2006) An MRI investigation of intervertebral disc deformation in response to torsion. Clin Biomech 21:538–542. https://doi.org/10.1016/j.clinbiomech.2005.12.008
Ogon I, Takebayashi T, Takashima H et al (2019) Analysis of neuropathic pain using magnetic resonance imaging T2 mapping of intervertebral disc in chronic low back pain. Asian Spine J 13:403–409. https://doi.org/10.31616/asj.2018.0147
Lama P, Maitre CLL, Harding IJ et al (2018) Nerves and blood vessels in degenerated intervertebral discs are confined to physically disrupted tissue. J Anat 233:86–97. https://doi.org/10.1111/joa.12817
Breen A, Breen AC, Mellor F, Morris A (2020) An in-vivo study exploring correlations between early-to-moderate disc degeneration and flexion mobility in the lumbar spine. Eur Spine J 29:2629–2627. https://doi.org/10.1007/s00586-020-06526-0
Reckziegel D, Vachon-Presseau E, Petre D et al (2019) Deconstructing biomarkers for chronic pain: context- and hypothesis-dependent biomarker types in relation to chronic pain. Pain 160:S37–S48. https://doi.org/10.1097/j.pain.0000000000001529
Teyhen DS, Flynn TW, Childs JD et al (2007) Fluoroscopic video to identify aberrant lumbar motion. Spine 32:E220–E229. https://doi.org/10.1097/01.brs.0000259206.38946.cb
Breen AC, Dupac M, Osborne N (2015) Attainment rate as a surrogate indicator of the intervertebral neutral zone length in lateral bending: an in vitro proof of concept study. Chiropr Man Ther 23:28. https://doi.org/10.1186/s12998-015-0073-8
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Breen, A., Nematimoez, M., Branney, J. et al. Passive intervertebral restraint is different in patients with treatment-resistant chronic nonspecific low back pain: a retrospective cohort study and control comparison. Eur Spine J 33, 2405–2419 (2024). https://doi.org/10.1007/s00586-024-08249-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-024-08249-y