Abstract
Amyotrophic lateral sclerosis (ALS) is an adult-onset paralytic disease characterized by progressive degeneration of upper and lower motor neurons in the motor cortex, brainstem and spinal cord. Motor neuron degeneration is typically caused by a combination of intrinsic neuronal (cell autonomous) defects as well as extrinsic (non-cell autonomous) factors such as astrocyte-mediated toxicity. Astrocytes are highly plastic cells that react to their microenvironment to mediate relevant responses. In neurodegeneration, astrocytes often turn reactive and in turn secrete a slew of factors to exert pro-inflammatory and neurotoxic effects. Various efforts have been carried out to characterize the diseased astrocyte secretome over the years, revealing that pro-inflammatory chemokines, cytokines and microRNAs are the main players in mediating neuronal death. As metabolomic technologies mature, these studies begin to shed light on neurotoxic metabolites such as secreted lipids. In this focused review, we will discuss changes in the astrocyte secretome during ALS. In particular, we will discuss the components of the reactive astrocyte secretome that contribute to neuronal death in ALS.
Similar content being viewed by others
Introduction
Amyotrophic lateral sclerosis (ALS) is an adult-onset paralytic disease characterized by progressive degeneration of upper (cortical) and lower (spinal) motor neurons from motor cortex, brainstem and spinal cord [1]. Motor neurons serve as important communication links between the brain and voluntary muscles, so the progressive neurological deterioration of motor neurons results in muscular atrophy and ultimately death from respiratory failure within 1–5 years after disease onset [2]. About 5%–10% of ALS cases are familial and the remaining 90% are sporadic [3]. Beyond motor neurons, numerous studies also support the roles of astrocyte-mediated toxicity in the onset and progression of ALS [4,5,6]. Astrocytes are the major glial cell type in the adult central nervous system (CNS), constituting 20%–40% of the human brain [7, 8]. Despite their abundance, the roles of astrocytes in modulating neurodegeneration are just starting to be uncovered. Astrocytes are highly secretory cells that play diverse roles in supporting neuronal health, such as modulating the blood-brain barrier [9], regulating synaptogenesis [10, 11] and neurotransmitter recycling [12], providing metabolic support to neurons [13], and regulating CNS inflammatory responses [14], which have been extensively reviewed previously [15,16,17]. It has also been well-documented that diseased astrocytes contribute to neuronal defects and death. Healthy neurons co-cultured with ALS astrocytes display neuronal deficits that result in cell death [6, 18,19,20,21,22]. In addition to reduced secretion of neurotrophic factors and metabolites that support neuronal survival and function [23], the neurotoxic effects are also considered to be mediated by secreted “toxic factors” [22] such as pro-inflammatory cytokines. ALS astrocytes are known to take on an inflammatory reactive state [24], which triggers the release of pro-inflammatory cytokines and chemokines that initiate an inflammatory cascade that results in neuronal damage and death [25]. An increasing body of evidence also suggests contribution of multiple other bioactive molecules to ALS astrocyte-mediated toxicity, such as lipids, metabolites, microRNAs and even extracellular matrix proteins [24, 26, 27].
Major challenges exist in studies of astrocyte-mediated toxicity, as the components of astrocyte secretome and their changes in disease conditions remain poorly understood. What constitute a healthy astrocyte secretome? How do the secretory profiles of astrocytes change with ALS progression? Do the changes in ALS astrocyte secretome contribute to motor neuron damage and death? In this review, we aim to shed light on some of these questions by summarizing the key findings supporting the relevance of astrocyte secretome with ALS and discuss the efforts made to elucidate components of the astrocyte secretome. Finally, we will discuss if the astrocyte secretome can be exploited for therapeutic intervention for treatment of ALS.
Astrocytes are not static cell types, but rather adapt quickly to extrinsic stimuli
Astrocytes are highly plastic cell types, and can acquire different phenotypes in response to pathological stimuli during neurodegeneration, injury or infection [28]. In healthy nervous tissues, astrocytes are quiescent and support normal neuronal metabolism and function [13]. However, upon injury of nervous tissue caused either by trauma or neurodegeneration, astrocytes are activated through a process known as reactive astrogliosis with a change of phenotype aimed to regulate neuroinflammation [17]. Known molecular triggers of reactive astrogliosis include pro-inflammatory molecules such as tumor necrosis factor alpha (TNF-α) and IL-1β [29], which have the ability to induce changes in gene and protein levels of quiescent astrocytes, leading to secretion of neurotoxic factors.
Reactive astrocytes are defined by their neurotoxic, proinflammatory (A1) phenotype or neuroprotective, anti-inflammatory (A2) phenotype
Astrocyte activation is a defense to CNS insults and pathologies, aimed at minimizing and repairing the damage [30]. Reactive astrogliosis is the process where astrocytes remodel their transcriptome, metabolome, secretome and morphology in response to pathology. Although reactive astrocytes have been classified into A1 and A2 phenotypes based on their respective neurotoxic or neuroprotective properties [31,32,33,34,35], it is increasingly recognized that such binary classifications do not fully represent the heterogeneity of reactive astrocytes [36, 37]. However, at the time of writing this review, the extent of reactive astrocyte heterogeneity in ALS is not entirely elucidated. Therefore, we will discuss changes in ALS astrocytes based on this binary A1 versus A2 astrocyte classification to explain how understanding astrocyte remodeling is important for the discovery of novel therapeutics targeting astrocyte-mediated toxicity.
A1 reactive astrocytes promote cytotoxicity in part by secreting toxic factors that result in neuronal death and demyelination [31, 32] while A2 astrocytes are neuroprotective and promote nervous system repair by upregulating pro-survival factors [33,34,35]. At the molecular level, A1 and A2 astrocytes differ in their gene expression signature. The A1 astrocytes are defined by expression of the complement cascade component C3 and interferon-induced guanylate-binding protein 2, and activation of the nuclear factor kappa B (NF-κB) pathway [32, 38]. On the other hand, the neuroprotective A2 astrocytes are defined by expression of S100A10, which promotes cell proliferation and membrane repair and inhibits apoptosis [32]. The A2 astrocytes also promote expression of epithelial membrane protein EMP1 [39] and anti-inflammatory cytokine transforming growth factor beta (TGF-β), which prevents synaptic loss and neuronal damage [40, 41].
Recent studies have investigated extracellular and intracellular signaling pathways which determine the A1 or A2 fate of astrocytes. Microglia and neurons are major sources of extracellular signals (such as chemokines and cytokines) that polarize astrocytes into its neurotoxic or neuroprotective state. Liddelow and colleagues have demonstrated that complement component 1 subcomponent q (C1q), interleukin-1α (IL-lα), and TNF-α secreted by lipopolysaccharide (LPS)-activated microglia can induce the A1 phenotype of astrocytes in vitro and in vivo [32]. In another study, activation of nod-like receptor family pyrin domain-containing 3 (NLRP3) by microglia was demonstrated to transform astrocytes into the cytotoxic A1 phenotype [42]. The NLRP3 inflammasomes can further process pro-IL-18 into IL-18. When added exogenously into primary astrocyte cultures, IL-18 induces downregulation of A2 astrocytic markers and upregulation of A1 neurotoxic markers [32, 43]. Ultimately, these various exogenous signals converge to the NF-κB signaling pathway, which modulates the A1 neuroinflammatory response [32, 44]. Elevated NF-κB activity has also been detected within the spinal cord astrocytes of ALS patients [45]. Interestingly, physiological aging has also been shown to induce A1-like astrocyte reactivity [39], likely due to the activated microglial cells that are formed during aging, as mice lacking the microglial-secreted cytokines IL-1α, C1q and TNF-α show low expression of A1-reactive astrocyte markers [32].
On the other hand, the anti-inflammatory cytokine IL-10 secreted predominantly by astrocytes and microglia has been shown to induce the neuroprotective A2 phenotype. Astrocytes derived from mice with low expression of IL-10 have elevated levels of A1-type markers as compared to wild-type mice under normal conditions or when challenged with LPS. When astrocytes are pre-treated with IL-10, the A1 transcripts are decreased and behavioral deficits are reduced, suggesting that IL-10 is an inhibitor for A1 astrogliosis [46]. Prokineticin-2 (PK2) is a secreted neuropeptide and plays a neuroprotective role [47]. Astrocytes express high levels of the PK2 receptor PKR1. It has been shown that PK2 treatment or overexpression in primary astrocyte cultures can promote the A2 astrocyte fate. Likewise, depletion of PKR1 in mice results in a decrease in A2 markers while chemical agonists of PKR1 promote the A2 neuroprotective phenotype in astrocytes [48]. A summary of A1 versus A2 reactive astrocytes is provided in Fig. 1.
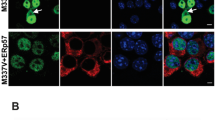
Changes in astrocyte secretome when a quiescent astrocyte takes on an A2 or A1 phenotype. A1 and A2 reactive astrocytes have distinct intracellular markers, as well as different secretory profiles. A2 reactive astrocytes promote neuroprotection through secretion of anti-inflammatory cytokines and chemokines as well as anti-apoptotic non-coding RNAs. In addition, enhanced secretion of metabolites such as lactate and alpha-ketoglutarate provides additional metabolic support for neurons. A1 reactive astrocytes, on the other hand, are neurotoxic, and promote neurodegeneration through secretion of pro-inflammatory cytokines and chemokines. Recent studies also show that these astrocytes secrete neurotoxic fatty acids and lipids, which represents a paradigm shift in the field of neurodegeneration
Astrocytes become reactive in response to ALS-associated misfolded proteins
A major pathological hallmark of ALS is the presence and accumulation of cytoplasmic inclusions containing TAR DNA-binding protein 43 (TDP43), FUS or superoxide dismutase 1 (SOD1) protein [49,50,51,52] in neurons and astrocytes. Studies suggest that these protein aggregates form insoluble fibrils that may propagate in a prion-like manner where the fibrils act as seeds to trigger aggregation of native counterparts [52, 53]. Sequestration of native proteins such as TDP43, FUS and SOD1 into insoluble aggregates within the cytosol would effectively mimic a loss-of-function mutation since the mislocalization and the sequestration of the native proteins imply that their physiological activities are compromised [54, 55]. Astrocytic depletion of TDP43 has been shown to cause reactive astrogliosis with a pro-inflammatory phenotype [56, 57]. Notably, mice with selective TDP43 deletion in astrocytes (GFAP-Cre; tardbpfl/fl mice) have enhanced GFAP immunoreactivity with longer astrocytic processes along with increased C1q expression, indicative of astrogliosis. Additionally, RNA sequencing of these TDP43-deficient astrocytes reveals a molecular signature of pro-inflammatory A1 reactive astrocytes [57].
Insoluble fibrils themselves may also be triggers of astrogliosis, which has been demonstrated in other adult-onset neurodegenerative diseases such as Parkinson’s disease that fibrillar alpha-synuclein species induce neurotoxic A1-type astrogliosis via NFκB activation [58]. In the context of ALS, overexpression of TDP43 in astrocytes, which likely results in cytoplasmic aggregation [59], induces secretion of pro-inflammatory cytokines (such as TNF-α and IL-6) and causes neurotoxicity in a neuron-astrocyte coculture system [60].
There is also accumulating evidence suggesting that soluble oligomeric forms of protein aggregates are responsible for neurotoxicity in diseases where protein misfolding is a prominent feature. For instance, in Alzheimer’s disease, oligomeric forms of amyloid-beta induce high levels of pro-inflammatory molecules such as IL-1β, inducible nitric oxide synthase, NO and TNF-α in cultured rat astrocytes, consistent with an A1-reactive phenotype [61]. In ALS, TDP43 has been shown to be capable of forming oligomeric protofibrils [62, 63]. Exogenous TDP43 oligomers are found to be toxic to motor neurons but not to astrocytes [64]. Since Patani and colleagues showed that TDP43 oligomers trigger aggregation in astrocyte cultures, it is plausible that they would also lead to astrogliosis, although there are currently no available transcriptomic or protein expression data to confirm this. Apart from TDP43, mutant SOD1 can also form corkscrew oligomers which result in axonopathies and mitochondria defects, two hallmarks of ALS-linked pathologies [65].
Within the spinal cord, reactive astrocytes induce motor neuron pathologies similar to that seen in ALS [66], where proteostasis and autophagy are dysregulated in motor neurons, which eventually result in their selective death [67]. Altogether, these various studies highlight that astrocytes respond to various stimuli, including factors secreted by microglia and neurons, affecting the balance between A1 and A2 reactive astrogliosis. In ALS patients, astrocytes display the A1-type characteristics and are major players in motor neuron degeneration [19]. Corroborating this finding, Ziff and colleagues performed a systemic meta-analysis of publicly-available sequencing data of ALS astrocytes, which included human induced pluripotent stem cell-derived astrocytes and mouse primary astrocytes carrying various ALS-associated mutations. They concluded that ALS astrocytes are characterized by an “A1-like” inflammatory reactive signature, defined by upregulation of genes involved in extracellular matrix remodeling, cellular stress and immune response, while expression of genes involved in astrocyte functions such as glutamate uptake and other neuronal support mechanisms is suppressed [24].
Astrocytes respond to neurotransmitters by modulating endocytosis, exocytosis, and survival
In addition to their immunomodulatory roles, astrocytes also play a role in neurotransmitter recycling. Excitotoxicity is thought to be a major contributor to motor neuron degeneration in ALS [68,69,70]. Riluzole, a food and drug administration (FDA)-approved drug for ALS, works by blocking excitotoxicity through inhibiting glutamatergic neurotransmission in the central nervous system [71, 72]. Edaravone and AMX0035 are two other FDA-approved drugs for treatment of ALS. Edaravone works as a reactive oxygen species (ROS) scavenger [73]. AMX0035 is a combination of two drugs phenylbutyrate and tauroursodeoxycholic acid, and works by inhibiting endoplasmic reticulum stress response and blocking mitochondria-mediated apoptosis and ROS production [74,75,76]. Of the three approved drugs, only Riluzole works by suppressing excitotoxicity and therefore reducing astrocyte toxicity.
Glutamate is the most abundant excitatory neurotransmitter in the nervous system and is found with high concentrations in synaptic vesicles in pre-synaptic nerve terminals where it is released by exocytosis. After exocytosis, glutamate binds to several receptors at the post-synaptic membrane including N-methyl-D-aspartate (NMDA), α-amino-3-hydroxy-5-methy-4-isoxazolepropionic acid (AMPA), kainate and mGluR receptors. Excitotoxicity occurs when neurons are exposed to high levels of glutamate, which results in persistent activation of NMDA receptor, AMPA receptor, and voltage-gated calcium channels, and consequently a lethal influx of extracellular calcium [77]. Therefore, rapid glutamate clearance at the synaptic cleft is necessary and this process is mediated by glutamate transporters or excitatory amino acid transporters (EAATs). Five EAATs have been identified to date (EAAT-1 to EAAT-5), of which EAAT-1 and EAAT-2 are primarily expressed on astrocytes [78]. Notably, EAAT-2 expression is altered in ALS, which may contribute to the excessive levels of glutamate in the cerebrospinal fluid in patients [70, 79, 80]. In astrocytes, glutamate is converted into glutamine by the enzyme glutamine synthetase, and is released back into the extracellular space, where it will be taken up by neurons to produce glutamate. This process is known as the glutamate-glutamine cycle.
High levels of glutamate can cause astrocyte depolarization [81, 82], which leads to the exocytosis of gliotransmitters such as glutamate, ATP and neurotrophic factors and less commonly, D-serine, adenosine and prostaglandins [83]. In ALS patients, high levels of cerebrospinal fluid (CSF) glutamate have been found compared to the control population, and they correlate with more severe motor impairment [84]. In ALS mice overexpressing human SOD1G93A, exposure to glutamate results in focal degeneration of spinal cord astrocytes, which is not observed in mice overexpressing wild-type SOD1 [85]. This selective vulnerability to glutamate is caused by mGluR5 activation, as a selective mGluR5 antagonist blocks the glutamate toxicity in ALS astrocytes [85].
Glutamate toxicity is of high relevance in ALS, and contributes to ALS pathology via multiple pathways, exerting effects directly on motor neurons as well as on astrocytes, modulating the astrocytic exocytosis of gliotransmitters, thus providing paracrine signals on neighboring neurons.
Astrocytes remodel their secretome in ALS
It is increasingly evident that ALS astrocytes contribute to neuronal dysfunction and death [18]. A number of landmark papers have demonstrated that co-culture of healthy motor neurons with ALS astrocytes or exposing them to ALS astrocyte-conditioned media results in motor neuron death [6, 86]. This suggests that ALS astrocytes secrete soluble factors that are toxic to motor neurons. Interestingly, Birger et al. [87] demonstrated that the cytotoxicity of patient-derived mutant astrocytes is positively correlated with their duration in culture, implying that aged astrocytes are more neurotoxic and this is consistent with the fact that ALS is an age-onset neurodegenerative disease. Mass spectrometry experiment comparing conditioned medium (CM) of ALS astrocytes to that of healthy control revealed up-regulation of extracellular matrix proteins (collagen, lumican, olfactomedin-like protein 3 and protein-lysine 6 oxidase) and also downregulation of antioxidant proteins (SOD1, SOD2, glutathione synthetase) and motor neuron pro-survival factors (miR-494-3p), resulting in elevated stress and senescence in both astrocytes and motor neurons [87, 88]. In another study, Skorupa et al. [89] used quantitative proteomics to profile astrocytic secretome with angiogenin exposure. Angiogenin is a neuroprotective factor secreted by motor neurons and it modulates astrocytic secretome after being taken up by astrocytes. Loss-of-function mutation of this gene has been documented in ALS patients. Astrocytes exposed to angiogenin have also been demonstrated to express significantly different levels of chemokines, cytokines, proteases, and ECM proteins.
Astrocyte-secreted cytokines, chemokines and complements act as immunomodulatory molecules
ALS astrocytes are also known to secrete chemokines, complements and cytokines [33]. Of them, TNF-α is known to play a major role in motor neuron toxicity as neutralizing antibodies for TNF-α can partly rescue motor neuron death when co-cultured with ALS astrocytes [90]. This is not surprising given the role of TNF-α in promoting reactive astrogliosis and the A1 phenotype of astrocytes. Although the complete list of A1 astrocyte-secreted toxic factors has not been worked out, some pro-inflammatory cytokines and chemokines have been demonstrated to result in poor prognosis of ALS. In a recent study, Tortelli and colleagues reported that a panel of cytokines (IL-2, IL-6, IL-10, interferon-gamma [IFN-γ], and TNF-α) is elevated in plasma of ALS patients, with IL-6 having the highest discriminatory power between patients and control [91]. Also, a post-mortem study found changes in expression of both chemokines and cytokines in astrocytes from patients with familial amyotrophic lateral sclerosis (fALS) and sporadic amyotrophic lateral sclerosis (sALS), including upregulated chemokine (C-C motif) ligand (CCL) 2, CCL11, CCL13, CCL20, chemokine (C-X-C motif) ligand (CXCL) 1, CXCL2, CXCL3, CXCL5, CXCL6, CXCL10, CXCL11, and CXCL12, all of which are involved in the regulation of inflammation [6, 92]. These pro-inflammatory cytokines and chemokines secreted by A1-subtype ALS astrocytes can lead to activation of the NF-κB signaling, and prolonged activation of this inflammatory pathway would lead to accelerated disease progression and eventual collapse of the blood-spinal cord barrier [93].
At present, the exact mechanisms of how astrocyte-mediated neuroinflammation leads to motor neuron death in ALS still remain to be fully investigated. Apart from inducing neuroinflammation, the secreted cytokines such as TGF-β1 cause cellular toxicity through dysregulation of autophagy, resulting in aberrant protein aggregation [67]. Furthermore, A1 astrocytes also secrete IL-6, IFN-γ and prostaglandins, which, together with increased ROS, glutamate and nitric oxide, lead to reduction of neurotrophic factors such as vascular endothelial growth factor, brain-derived neurotrophic factor and ultimately neuronal degeneration [51, 94]. In recent years, efforts have been made to target neuroinflammation in ALS by altering the astrocytic secretome. Izrael and colleagues demonstrated a therapeutic effect of injecting “young” astrocytes derived from embryonic stem cells in ALS mice [95]. These young astrocytes secrete pro-survival factors and remodel the extracellular matrix to support neuronal growth. Specifically, young astrocytes behave as protective A2 astrocytes secreting neuroprotective chemokines such as CXCL16 and macrophage migration inhibitory factor (MIF) [39]. CXCL16 has been shown to protect neurons from excitotoxicity cell death [96] and MIF functions as chaperone preventing ALS motor neurons from degeneration caused by misfolded SOD1 [97]. Removing factors known to induce astrogliosis has been shown to improve the survival of ALS mice. Guttenplan and colleagues performed triple knockout of IL-1α, TNFα, and C1q and observed a reduction in astrogliosis and longest extension of lifespan ever reported in SOD1G93A mice [98]. Collectively, ALS astrocytes play a role in the progression of disease by secreting cytokines for neuroinflammation and protein aggregation, and there is accumulating evidence suggesting that altering the secretory profiles of astrocytes can delay the progression of ALS [26, 87, 99].
Astrocyte-secreted lipids are gaining attention as a novel class of neurotoxic molecules in ALS
In pathological conditions, lipids are a class of bioactive macromolecules that are secreted by astrocytes as potential toxic factors. Lipid droplets act as a store for excessive fatty acids and their formation can be induced by cellular stress such as hypoxia and starvation. Disrupted astrocytic lipid metabolism has also been linked to ALS. Astrocytes expressing mutant TDP43 exhibit higher accumulation of lipid droplets [100], suggesting an imbalance between lipid biosynthesis or uptake by ALS astrocytes and catabolism. Polyunsaturated fatty acids, in particular arachidonic acid, are also mediators of neurodegeneration in ALS, and are found at high levels in ALS spinal cords and cerebrospinal fluid samples [101,102,103]. These polyunsaturated fatty acids are possibly produced and secreted by astrocytes [104, 105], although some neurons are also known to release arachidonic acid upon depolarization [106, 107].
Arachidonic acid also serves as a precursor for prostaglandin E2 (PGE2), an eicosanoid that acts as a potent inflammatory mediator which contributes to neuroinflammation and motor neuron death. Elevated levels of PGE2 are a signature of ALS, with a majority of ALS patients having up to ten-fold higher levels of PGE2 in the CSF [108, 109]. Cyclo-oxygenase 2 (COX2) catalyzes the conversion of arachidonic acid to PGE2 [110]. Pharmacological inhibition of COX2 by specific inhibitors such as celecoxib or rofecoxib delays the development and progression of ALS by suppressing excitotoxicity, promoting the survival of motor neurons and reducing astrogliosis [111, 112].
Astrocyte-secreted long-chain saturated free fatty acids have also been implicated in neurotoxicity [113]. Fractionation of reactive-astrocyte conditioned media using biochemical purification columns revealed that hydrophobic and charged components contribute most significantly to oligodendrocyte death. The lipids bound to APOE and APOJ lipoproteins mediate the toxicity. Unbiased lipidomics of more than 1500 lipids from 10 classes revealed a significant upregulation of long-chain saturated free fatty acids in the reactive-astrocyte conditioned media. To investigate if these saturated free fatty acids are the mediators of neurotoxicity, Liddelow and colleagues generated astrocyte-specific elongation of very long chain fatty acids protein 1 (ELOVL1) conditional knockout (Elovl1 cKO) mice, as ELOVL1 is the enzyme that catalyzes the synthesis of long-chain (more than 16 carbons), saturated lipids and its expression is upregulated in reactive astrocytes. Reactive-astrocyte conditioned media from Elovl1 cKO mice are less toxic than that of wild-type mice, confirming the lipidomics findings [113]. In the context of ALS, enhanced expression or activity of astrocytic ELOVL1 or elevated production of saturated long-chain free fatty acids, has been reported, which warrants further investigations.
Astrocytes are the primary cell type that produces cholesterol in the adult CNS, and the production is regulated by the transcription factor sterol regulatory element binding protein-2 (SREBP2). Dodge et al. showed that overexpression of SREBP2 in the CNS results in accumulation of cholesterol and neutral lipids, as well as ALS-like symptoms in mice, such as progressive hindlimb paralysis, spasticity and reduced lifespan, suggesting that accumulation of neutral lipids is associated with spinal neuron degeneration [114]. Consistently, SOD1-G93A rodents display increased levels of lipid droplets and severe astrogliosis in the late symptomatic stage [101]. Additionally, lipids such as sphingolipids, ceramides and cholesterol are found in higher levels in ALS spinal cords [101]. However, it remains unclear if these neurotoxic lipids are primarily secreted by astrocytes or other neural cells in the spinal cord.
Extracellular vesicles contain cargos and may reflect disease status in ALS
As highly secretory cells, astrocytes release membrane-bound vesicles or extracellular vesicles (EVs). These astrocyte-derived EVs (ADEVs) are membrane-bound vesicles released by astrocytes into the extracellular space and include exosomes and microvesicles. More importantly, ADEVs carry cargos such as peptides, nucleic acids and lipids that are key signaling entities modulating neuronal function, survival and regeneration [115]. In the healthy CNS, ADEVs play a neuroprotective role by promoting dendritic growth, survival and electrophysiological activities of neurons [116, 117]. However, under pathological conditions, reactive ADEVs accelerate disease progression and aggravate neuroinflammation [118], indicating key alterations of the cargos contained within these vesicles. To characterize the protein components of ADEVs from control and activated astrocytes, You et al. [119] first treated primary human astrocytes with IL-1β to induce astrogliosis, and performed label-free mass spectrometry to identify changes in the composition of reactive ADEVs. They found that ADEVs released by astrocytes in response to IL-1β impair neuronal functions, resulting in shorter neurite lengths and reduced neuronal firing. Mechanistically, this can be attributed to the reactive ADEV peptides associated with cellular metabolism, migration and inflammatory response. Additionally, a separate study aimed at elucidating microRNA (miRNA) cargo changes upon astrocyte activation found that reactive astrocytes triggered by stimulation with either TNFα or IL-1β release higher levels of miR-125a-5p and miR-15-5p, which target the neurotrophic tyrosine kinase receptor NTKR3 or TrkC. Upon binding to its ligand neurotrophin-3, TrkC autophosphorylates and activates downstream signaling pathways that regulate synaptic development and expression of pro-survival factor Bcl-2 [117].
Elevated levels of the pro-inflammatory cytokine IL-6 have been also detected in ADEVs derived from sporadic ALS patients [120], suggesting that cytokines can be packaged into EVs to mediate astrocyte–neuron signaling in ALS. ALS astrocytes are also known to package pathogenic proteins such as misfolded SOD1 and TDP43 into EVs, contributing to the propagation of ALS pathology in the CNS [121, 122]. A study that profiled microRNAs in ADEVs isolated from ALS patients carrying the C9ORF72 mutations revealed that the downregulation of miR-494-3p in ALS ADEVs results in decreased axonal maintenance and motor neuron survival [123]. Although emerging studies suggest that ADEVs and their cargos are responsible for the progression of ALS, the exact compositions of ADEVs and changes of ADEV contents are still not completely understood.
Discussion: multi-omics approaches to elucidating the astrocyte secretome
Given the vital role astrocyte-secreted factors play in maintenance of neuronal health and disease progression, it is important to identify key astrocyte targets that can complement drug development efforts for neurodegenerative diseases (Fig. 2), which tend to be heavily focused on cell-autonomous pathways in neurons. Currently, the comprehensive catalog of astrocyte-secreted factors remains to be revealed. Advancement in proteomics and deep sequencing technologies in the past decade has accelerated the identification of proteins and RNA molecules secreted by healthy and diseased astrocytes [89, 124,125,126,127]. Emerging evidence suggests that astrocyte-secreted metabolites and lipid molecules are also crucial factors that mediate neuronal health and function [128,129,130]. One of the most well-characterized metabolites secreted by astrocytes is lactate, the end-product of anaerobic glycolysis [131]. In the CNS, lactate is mainly produced by astrocytes, and released to be taken up by surrounding neurons at metabolic needs [132]. In the astrocyte-neuron lactate shuttle hypothesis, electrically-active neurons release the neurotransmitter glutamate, which is mainly taken up by astrocytes through glutamate transporters on their plasma membranes. This glutamatergic activation then leads to increased astrocytic glycolysis and release of lactate in the extracellular space [133]. The extracellular lactate can be transported into neurons through monocarboxylate transporter 2 to sustain neuronal activity [134]. Although this hypothesis is still debatable [133], there is increasing evidence that astrocytes provide metabolites including lactate to neurons for their various metabolic needs and function [135, 136], and changes in these metabolites can contribute to neuronal dysfunction and death.
Multi-omics approaches to attenuating astrocyte-mediated toxicity. Under pre-symptomatic conditions, astrocytes play a supporting role in maintaining normal functioning of neurons and the central nervous system. As reactive oxygen species (ROS), inflammation and protein aggregates begin to accumulate, coupled with decreased ability to clear waste (autophagy), quiescent astrocytes may be activated to become ALS astrocytes which are highly secretive. These astrocyte-derived extracellular vesicles contain harmful proinflammatory cytokines and chemokines which ultimately result in degeneration of motor neurons and dysfunctional motor unit. The use of multi-omics (e.g., genomics, transcriptomics, proteomics, metabolomics) will allow for in-depth understanding of complex and multifactorial diseases such as ALS. Integration of different omics layers is crucial for uncovering changes in ALS astrocytes during disease onset and progression, paving the way for development of new therapeutics which can revert A1-like ALS astrocytes to A2 neuroprotective astrocytes
Reactive astrocytes undergo metabolic transformations during neurodegeneration [137]. For instance, in Huntington’s disease, striatal astrocytes switch from glycolysis to fatty acid oxidation [138], while in ALS, lipid metabolism is impaired as manifested by accumulation of lipid droplets [139]. As many metabolites can become secreted, changes in metabolism during astrogliosis may lead to corresponding alterations in secretome. While proteomics and transcriptomics studies have largely elucidated the peptide and RNA components of astrocyte secretome in healthy and diseased conditions, emerging metabolomics and lipidomics studies have shown that metabolites and lipids are also relevant to astrocyte biology.
Proteomics shows that cytokines, chemokines and neurotrophic factors are the most abundant proteins secreted by ALS astrocytes
Secreted proteins and peptides such as neurotrophic factors, anti-inflammatory cytokines (such as TGFβ and IL-10), pro-inflammatory cytokines and chemokines, and extracellular matrix proteins are thought to be a major class of functional biomolecules secreted by astrocytes [140], and many of these factors are known to alter neuronal function and activity. To elucidate secreted proteins associated with diseased astrocytes, Choi and colleagues [92] harvested human fetal astrocytes, stimulated them with IL-1β and TNF-α to mimic reactive astrogliosis, and collected their conditioned media for profiling in comparison to unstimulated astrocytes. Results revealed that stimulated and unstimulated astrocytes secrete distinct sets of cytokines and chemokines. Most of the cytokines and chemokines produced by non-stimulated and activated astrocytes are direct targets of NF-κB that plays immunomodulatory roles in the CNS. In another study relevant to neurodegeneration, conditioned media collected from spinal astrocytes derived from ALS transgenic mice overexpressing the human SOD1-G93A mutant were compared to wild-type astrocyte condition media using quantitative proteomics. Similar to previous report of activation of NF-κB and pro-inflammatory pathways, ALS astrocytes are shown to be depleted of metabolites involved in glutathione metabolism that plays a crucial role in redox signaling [141].
Across various disease conditions, reactive astrocytes consistently produce and secrete lower levels of neuroprotective neurotrophic factors while releasing higher amounts of neurotoxic cytokines and chemokines [33]. Additionally, other secreted factors have also been identified to play a role in neurodegeneration. Lipocalin-2 (Lcn2) secretion by astrocytes can be triggered by hypoxia [142], neurodegeneration [143,144,145], traumatic brain injury [146, 147] or spinal cord injury [148, 149]. Elevated Lcn2 levels have been found in the motor cortex, spinal cord, and plasma samples of post-mortem ALS patients. The secreted Lcn2 results in selective degeneration of neurons, by upregulating pro-apoptotic factor Bim and disrupting iron metabolism and inflammatory gene expression [145]. Importantly, Lcn2 shows promise as a therapeutic target. In wild-type mice, reactive astrocytes show robust expression of pro-inflammatory cytokines, such as IL-6 and CXCL10, which is attenuated in Lcn2-deficient mice [142, 145]. As a result, Lcn2 depletion promotes cell survival by reducing neuroinflammation, suggesting that manipulation of Lcn2 levels could regulate the progression of neurodegeneration.
Transcriptomics reveals disease-associated non-coding RNAs (ncRNAs) in ADEVs
Meanwhile, it is increasingly recognized that astrocytes also secrete ncRNAs that are packaged within extracellular vesicles known as ADEVs. These ncRNAs, which include miRNAs and long non-coding RNAs (lncRNAs), have been reported to contribute to neurodegeneration, promoting astrogliosis [150] and degeneration of neuronal networks [123]. Deep sequencing approaches have accelerated the identification of RNA species that exist in ADEVs. In an earlier section, we have discussed how deep sequencing of small RNAs has identified changes within the miRNA content in ADEVs in response to astrogliosis [117]. Disease-specific miRNAs have also been described for ALS [151, 152], traumatic brain injury and spinal cord injury [153, 154], and some of them have been identified as potential therapeutic targets because abrogation of them slows down the disease progression [155,156,157].
The lncRNAs, defined as noncoding transcripts longer than 200 nucleotides, are highly expressed in the brain. Many of these lncRNAs are bioactive molecules that play a role in modulating gene expression and signaling pathways [158, 159]. In traumatic brain injury, astrocytes show increased expression and secretion of the lncRNA NKILA, which exerts neuroprotective properties by depleting miR-195, an miRNA associated with apoptosis [160]. However, despite the large quantity of lncRNAs expressed by astrocytes [161], comprehensive studies of astrocyte-secreted lncRNAs in disease conditions are still needed.
Metabolomic-based studies will yield important information on disease-relevant changes of astrocyte-secreted metabolites and lipids
Astrocytes store energy in forms of glycogen and lipid droplets and mobilize metabolic stores to support neuronal function. While astrocytes normally produce ATP through complete glycolysis, they can also switch to fatty acid oxidation to supplement their energy requirements, especially in neurodegenerative conditions such as Huntington’s disease and ALS [138]. As fatty acid oxidation involves breaking down of fatty acids into acetyl-coA units to fuel the tricarboxylic acid cycle and mitochondrial respiration, lipid droplets are considered to be an important energy reservoir in astrocytes.
Defects in lipid metabolism have been linked to ALS [162,163,164]. Since lipids can be secreted by astrocytes, it can be expected that changes in lipid metabolism would alter the lipid secretory profile of diseased astrocytes. Blasco and colleagues in 2017 compared lipid content of CSF between ALS patients and neurotypical controls, and found a unique lipidomic signature in ALS, characterized by high levels of phosphotidylcholine, ceramides and glucosylceramides [165]. Since the CSF surrounds the brain and the spinal cord where astrocytes make up the majority of cells, it can be inferred that astrocytes contribute to the lipidomic signature in ALS CSF. Indeed, other independent studies have detected ceramides in ADEVs [166], suggesting that ceramides and other lipids highly secreted by ALS astrocytes may contribute to the astrocyte-mediated toxicity.
Conclusion
Studies on neurodegeneration tend to be neuro-centric, where research aims to elucidate the intrinsic dysfunctions of neuronal pathways and functions that precede neuronal death. Recent studies have shown that the non-cell autonomous contributions to neurodegeneration are not negligible. Astrocytes play a more critical role in governing the health of the central nervous system than previously appreciated. They are highly responsive to environmental cues such as pro-inflammatory cytokines and chemokines, and adjust their secretome accordingly to produce either neuroprotective or neurotoxic effects (Fig. 1). Understanding the astrocyte secretome is key to dissecting molecular mechanisms underlying the progression of neurological disorders. To do so, a multi-omics approach is needed. While proteomics and transcriptomics studies have been carried out, key information is still lacking. When do A2 astrocytes turn reactive and is this process reversible? Are lncRNAs abundantly secreted by astrocytes and what roles do they play in ALS pathogenesis and progression? What metabolites and lipid molecules are secreted by astrocytes and how do they change in ALS? Can changes in metabolites be used as diagnostic biomarkers for early diagnosis of ALS? Are there neurotoxic amino acids or lipid species that compromise the function and survival of motor neurons? In this multi-omics era, we envision that characterization of diseased astrocyte secretome by proteomics, transcriptomics, metabolomics and lipidomics approaches would reveal novel insights into the disease progression as well as uncovering new disease targets, for ALS and therapeutic development (Fig. 2).
Availability of data and materials
References’ information used in this manuscript will be available on demand.
Abbreviations
- ADEV:
-
Astrocyte-derived extracellular vesicle
- ALS:
-
Amytrophic lateral sclerosis
- AMPA:
-
α-amino-3-hydroxy-5-methy-4-isoxazolepropionic acid
- C1q:
-
Complement component 1q
- CCL:
-
Chemokine (C-C motif) ligand
- CNS:
-
Central nervous system
- CSF:
-
Cerebrospinal fluid
- CXCL:
-
Chemokine (C-X-C motif) ligand
- CXCR:
-
C-X-C chemokine receptor
- EAAT:
-
Excitatory amino acid transporter
- ELOVL1:
-
Elongation of very long chain fatty acids protein 1
- EV:
-
Extracellular vesicles
- IFN-γ:
-
Interferon-gamma
- IL:
-
Interleukin
- LPS:
-
Lipopolysaccharide
- MIF:
-
Macrophage migration inhibitory factor
- NF-κB:
-
Nuclear factor kappa B
- NLRP3:
-
NOD-, LRR- and pyrin domain-containing protein 3
- NMDA:
-
N-methyl-D-aspartate
- PGE2:
-
Prostaglandin E2
- PK-2:
-
Prokineticin-2
- SOD:
-
Superoxide dismutase
- SREBP2:
-
Sterol regulatory element-binding protein 2
- TDP43:
-
TAR DNA-binding protein 43
- TGF-β:
-
Transforming growth factor beta
- Trk:
-
Tropomyosin receptor kinase
- TNF-α:
-
Tumor necrosis factor alpha
References
Taylor JP, Brown RH Jr, Cleveland DW. Decoding ALS: from genes to mechanism. Nature. 2016;539(7628):197–206.
Swinnen B, Robberecht W. The phenotypic variability of amyotrophic lateral sclerosis. Nat Rev Neurol. 2014;10(11):661–70.
Rosen DR, Siddique T, Patterson D, Figlewicz DA, Sapp P, Hentati A, et al. Mutations in Cu/Zn superoxide dismutase gene are associated with familial amyotrophic lateral sclerosis. Nature. 1993;362(6415):59–62.
Nagai M, Re DB, Nagata T, Chalazonitis A, Jessell TM, Wichterle H, et al. Astrocytes expressing ALS-linked mutated SOD1 release factors selectively toxic to motor neurons. Nat Neurosci. 2007;10(5):615–22.
Di Giorgio FP, Carrasco MA, Siao MC, Maniatis T, Eggan K. Non-cell autonomous effect of glia on motor neurons in an embryonic stem cell-based ALS model. Nat Neurosci. 2007;10(5):608–14.
Haidet-Phillips AM, Hester ME, Miranda CJ, Meyer K, Braun L, Frakes A, et al. Astrocytes from familial and sporadic ALS patients are toxic to motor neurons. Nat Biotechnol. 2011;29(9):824–8.
Verkhratsky A, Zorec R, Parpura V. Stratification of astrocytes in healthy and diseased brain. Brain Pathol. 2017;27(5):629–44.
Westergard T, Rothstein JD. Astrocyte diversity: current insights and future directions. Neurochem Res. 2020;45(6):1298–305.
Cabezas R, Avila M, Gonzalez J, El-Bacha RS, Baez E, Garcia-Segura LM, et al. Astrocytic modulation of blood brain barrier: perspectives on Parkinson’s disease. Front Cell Neurosci. 2014;8:211.
Baldwin KT, Eroglu C. Molecular mechanisms of astrocyte-induced synaptogenesis. Curr Opin Neurobiol. 2017;45:113–20.
Chung WS, Allen NJ, Eroglu C. Astrocytes control synapse formation, function, and elimination. Cold Spring Harb Perspect Biol. 2015;7(9):a020370.
Weber B, Barros LF. The astrocyte: powerhouse and recycling center. Cold Spring Harb Perspect Biol. 2015;7(12):a020396.
Turner DA, Adamson DC. Neuronal-astrocyte metabolic interactions: understanding the transition into abnormal astrocytoma metabolism. J Neuropathol Exp Neurol. 2011;70(3):167–76.
Sofroniew MV. Astrocyte barriers to neurotoxic inflammation. Nat Rev Neurosci. 2015;16(5):249–63.
Farhy-Tselnicker I, Allen NJ. Astrocytes, neurons, synapses: a tripartite view on cortical circuit development. Neural Dev. 2018;13(1):7.
Reemst K, Noctor SC, Lucassen PJ, Hol EM. The indispensable roles of microglia and astrocytes during brain development. Front Hum Neurosci. 2016;10:566.
Sofroniew MV, Vinters HV. Astrocytes: biology and pathology. Acta Neuropathol. 2010;119(1):7–35.
Phatnani H, Maniatis T. Astrocytes in neurodegenerative disease. Cold Spring Harb Perspect Biol. 2015;7(6):a020628.
Ilieva H, Polymenidou M, Cleveland DW. Non-cell autonomous toxicity in neurodegenerative disorders: ALS and beyond. J Cell Biol. 2009;187(6):761–72.
Thangavelu SR, Tripathi PP, Arya U, Mishra HK, Subramaniam JR. ALS associated mutant SOD1 impairs the motor neurons and astrocytes and wild type astrocyte secreted-factors reverse the impaired motor neurons. Ann Neurosci. 2011;18(2):48–55.
Zhao C, Devlin AC, Chouhan AK, Selvaraj BT, Stavrou M, Burr K, et al. Mutant C9orf72 human iPSC-derived astrocytes cause non-cell autonomous motor neuron pathophysiology. Glia. 2020;68(5):1046–64.
Di Giorgio FP, Boulting GL, Bobrowicz S, Eggan KC. Human embryonic stem cell-derived motor neurons are sensitive to the toxic effect of glial cells carrying an ALS-causing mutation. Cell Stem Cell. 2008;3(6):637–48.
Pehar M, Cassina P, Vargas MR, Castellanos R, Viera L, Beckman JS, et al. Astrocytic production of nerve growth factor in motor neuron apoptosis: implications for amyotrophic lateral sclerosis. J Neurochem. 2004;89(2):464–73.
Ziff OJ, Clarke BE, Taha DM, Crerar H, Luscombe NM, Patani R. Meta-analysis of human and mouse ALS astrocytes reveals multi-omic signatures of inflammatory reactive states. Genome Res. 2022;32(1):71–84.
Sussmuth SD, Sperfeld AD, Hinz A, Brettschneider J, Endruhn S, Ludolph AC, et al. CSF glial markers correlate with survival in amyotrophic lateral sclerosis. Neurology. 2010;74(12):982–7.
Gomes C, Sequeira C, Likhite S, Dennys CN, Kolb SJ, Shaw PJ, et al. Neurotoxic astrocytes directly converted from sporadic and familial ALS patient fibroblasts reveal signature diversities and miR-146a theragnostic potential in specific subtypes. Cells. 2022;11(7):1186.
Gomes C, Sequeira C, Barbosa M, Cunha C, Vaz AR, Brites D. Astrocyte regional diversity in ALS includes distinct aberrant phenotypes with common and causal pathological processes. Exp Cell Res. 2020;395(2):112209.
Karve IP, Taylor JM, Crack PJ. The contribution of astrocytes and microglia to traumatic brain injury. Br J Pharmacol. 2016;173(4):692–702.
Hyvarinen T, Hagman S, Ristola M, Sukki L, Veijula K, Kreutzer J, et al. Co-stimulation with IL-1beta and TNF-alpha induces an inflammatory reactive astrocyte phenotype with neurosupportive characteristics in a human pluripotent stem cell model system. Sci Rep. 2019;9(1):16944.
Lee KM, MacLean AG. New advances on glial activation in health and disease. World J Virol. 2015;4(2):42–55.
Li T, Liu T, Chen X, Li L, Feng M, Zhang Y, et al. Microglia induce the transformation of A1/A2 reactive astrocytes via the CXCR7/PI3K/Akt pathway in chronic post-surgical pain. J Neuroinflamm. 2020;17(1):211.
Liddelow SA, Guttenplan KA, Clarke LE, Bennett FC, Bohlen CJ, Schirmer L, et al. Neurotoxic reactive astrocytes are induced by activated microglia. Nature. 2017;541(7638):481–7.
Li K, Li J, Zheng J, Qin S. Reactive astrocytes in neurodegenerative diseases. Aging Dis. 2019;10(3):664–75.
Christopherson KS, Ullian EM, Stokes CC, Mullowney CE, Hell JW, Agah A, et al. Thrombospondins are astrocyte-secreted proteins that promote CNS synaptogenesis. Cell. 2005;120(3):421–33.
Hayakawa K, Pham LD, Arai K, Lo EH. Reactive astrocytes promote adhesive interactions between brain endothelium and endothelial progenitor cells via HMGB1 and beta-2 integrin signaling. Stem Cell Res. 2014;12(2):531–8.
Escartin C, Galea E, Lakatos A, O’Callaghan JP, Petzold GC, Serrano-Pozo A, et al. Reactive astrocyte nomenclature, definitions, and future directions. Nat Neurosci. 2021;24(3):312–25.
Xiong XY, Tang Y, Yang QW. Metabolic changes favor the activity and heterogeneity of reactive astrocytes. Trends Endocrinol Metab. 2022;33(6):390–400.
Hartmann K, Sepulveda-Falla D, Rose IVL, Madore C, Muth C, Matschke J, et al. Complement 3(+)-astrocytes are highly abundant in prion diseases, but their abolishment led to an accelerated disease course and early dysregulation of microglia. Acta Neuropathol Commun. 2019;7(1):83.
Clarke LE, Liddelow SA, Chakraborty C, Munch AE, Heiman M, Barres BA. Normal aging induces A1-like astrocyte reactivity. Proc Natl Acad Sci U S A. 2018;115(8):E1896-E905.
Cekanaviciute E, Dietrich HK, Axtell RC, Williams AM, Egusquiza R, Wai KM, et al. Astrocytic TGF-beta signaling limits inflammation and reduces neuronal damage during central nervous system Toxoplasma infection. J Immunol. 2014;193(1):139–49.
Diniz LP, Tortelli V, Matias I, Morgado J, Bergamo Araujo AP, Melo HM, et al. Astrocyte transforming growth factor beta 1 protects synapses against Abeta oligomers in Alzheimer’s disease model. J Neurosci. 2017;37(28):6797–809.
Xiao T, Ji H, Shangguan X, Qu S, Cui Y, Xu J. NLRP3 inflammasome of microglia promotes A1 astrocyte transformation, neo-neuron decline and cognition impairment in endotoxemia. Biochem Biophys Res Commun. 2022;602:1–7.
Hou B, Zhang Y, Liang P, He Y, Peng B, Liu W, et al. Inhibition of the NLRP3-inflammasome prevents cognitive deficits in experimental autoimmune encephalomyelitis mice via the alteration of astrocyte phenotype. Cell Death Dis. 2020;11(5):377.
Lian H, Yang L, Cole A, Sun L, Chiang AC, Fowler SW, et al. NFkappaB-activated astroglial release of complement C3 compromises neuronal morphology and function associated with Alzheimer’s disease. Neuron. 2015;85(1):101–15.
Swarup V, Phaneuf D, Dupre N, Petri S, Strong M, Kriz J, et al. Deregulation of TDP-43 in amyotrophic lateral sclerosis triggers nuclear factor kappab-mediated pathogenic pathways. J Exp Med. 2011;208(12):2429–47.
Zhang HY, Wang Y, He Y, Wang T, Huang XH, Zhao CM, et al. A1 astrocytes contribute to murine depression-like behavior and cognitive dysfunction, which can be alleviated by IL-10 or fluorocitrate treatment. J Neuroinflammation. 2020;17(1):200.
Gordon R, Neal ML, Luo J, Langley MR, Harischandra DS, Panicker N, et al. Prokineticin-2 upregulation during neuronal injury mediates a compensatory protective response against dopaminergic neuronal degeneration. Nat Commun. 2016;7:12932.
Neal M, Luo J, Harischandra DS, Gordon R, Sarkar S, Jin H, et al. Prokineticin-2 promotes chemotaxis and alternative A2 reactivity of astrocytes. Glia. 2018;66(10):2137–57.
Kwiatkowski TJ Jr, Bosco DA, Leclerc AL, Tamrazian E, Vanderburg CR, Russ C, et al. Mutations in the FUS/TLS gene on chromosome 16 cause familial amyotrophic lateral sclerosis. Science. 2009;323(5918):1205–8.
Forsberg K, Graffmo K, Pakkenberg B, Weber M, Nielsen M, Marklund S, et al. Misfolded SOD1 inclusions in patients with mutations in C9orf72 and other ALS/FTD-associated genes. J Neurol Neurosurg Psychiatry. 2019;90(8):861–9.
Yamanaka K, Komine O. The multi-dimensional roles of astrocytes in ALS. Neurosci Res. 2018;126:31–8.
Blokhuis AM, Groen EJ, Koppers M, van den Berg LH, Pasterkamp RJ. Protein aggregation in amyotrophic lateral sclerosis. Acta Neuropathol. 2013;125(6):777–94.
Lee S, Kim HJ. Prion-like mechanism in amyotrophic lateral sclerosis: are protein aggregates the Key? Exp Neurobiol. 2015;24(1):1–7.
Budini M, Romano V, Quadri Z, Buratti E, Baralle FE. TDP-43 loss of cellular function through aggregation requires additional structural determinants beyond its C-terminal Q/N prion-like domain. Hum Mol Genet. 2015;24(1):9–20.
Che MX, Jiang YJ, Xie YY, Jiang LL, Hu HY. Aggregation of the 35-kDa fragment of TDP-43 causes formation of cytoplasmic inclusions and alteration of RNA processing. FASEB J. 2011;25(7):2344–53.
LaRocca TJ, Mariani A, Watkins LR, Link CD. TDP-43 knockdown causes innate immune activation via protein kinase R in astrocytes. Neurobiol Dis. 2019;132:104514.
Peng AYT, Agrawal I, Ho WY, Yen YC, Pinter AJ, Liu J, et al. Loss of TDP-43 in astrocytes leads to motor deficits by triggering A1-like reactive phenotype and triglial dysfunction. Proc Natl Acad Sci U S A. 2020;117(46):29101–12.
Chou TW, Chang NP, Krishnagiri M, Patel AP, Lindman M, Angel JP, et al. Fibrillar alpha-synuclein induces neurotoxic astrocyte activation via RIP kinase signaling and NF-kappaB. Cell Death Dis. 2021;12(8):756.
Johnson BS, Snead D, Lee JJ, McCaffery JM, Shorter J, Gitler AD. TDP-43 is intrinsically aggregation-prone, and amyotrophic lateral sclerosis-linked mutations accelerate aggregation and increase toxicity. J Biol Chem. 2009;284(30):20329–39.
Lee S, Kim S, Kang HY, Lim HR, Kwon Y, Jo M, et al. The overexpression of TDP-43 in astrocytes causes neurodegeneration via a PTP1B-mediated inflammatory response. J Neuroinflamm. 2020;17(1):299.
White JA, Manelli AM, Holmberg KH, Van Eldik LJ, Ladu MJ. Differential effects of oligomeric and fibrillar amyloid-beta 1–42 on astrocyte-mediated inflammation. Neurobiol Dis. 2005;18(3):459–65.
French RL, Grese ZR, Aligireddy H, Dhavale DD, Reeb AN, Kedia N, et al. Detection of TAR DNA-binding protein 43 (TDP-43) oligomers as initial intermediate species during aggregate formation. J Biol Chem. 2019;294(17):6696–709.
Pirie E, Oh CK, Zhang X, Han X, Cieplak P, Scott HR, et al. S-nitrosylated TDP-43 triggers aggregation, cell-to-cell spread, and neurotoxicity in hiPSCs and in vivo models of ALS/FTD. Proc Natl Acad Sci U S A. 2021;118(11):e2021368118. https://doi.org/10.1073/pnas.2021368118
Smethurst P, Risse E, Tyzack GE, Mitchell JS, Taha DM, Chen YR, et al. Distinct responses of neurons and astrocytes to TDP-43 proteinopathy in amyotrophic lateral sclerosis. Brain. 2020;143(2):430–40.
Sangwan S, Zhao A, Adams KL, Jayson CK, Sawaya MR, Guenther EL, et al. Atomic structure of a toxic, oligomeric segment of SOD1 linked to amyotrophic lateral sclerosis (ALS). Proc Natl Acad Sci U S A. 2017;114(33):8770–5.
Pirooznia SK, Dawson VL, Dawson TM. Motor neuron death in ALS: programmed by astrocytes? Neuron. 2014;81(5):961–3.
Tripathi P, Rodriguez-Muela N, Klim JR, de Boer AS, Agrawal S, Sandoe J, et al. Reactive astrocytes promote als-like degeneration and intracellular protein aggregation in human motor neurons by disrupting autophagy through TGF-beta1. Stem Cell Rep. 2017;9(2):667–80.
Brockington A, Ning K, Heath PR, Wood E, Kirby J, Fusi N, et al. Unravelling the enigma of selective vulnerability in neurodegeneration: motor neurons resistant to degeneration in ALS show distinct gene expression characteristics and decreased susceptibility to excitotoxicity. Acta Neuropathol. 2013;125(1):95–109.
King AE, Woodhouse A, Kirkcaldie MT, Vickers JC. Excitotoxicity in ALS: overstimulation, or overreaction? Exp Neurol. 2016;275(1):162–71.
Leigh PN, Meldrum BS. Excitotoxicity in ALS. Neurology. 1996;47(6 Suppl 4):221–7.
Saitoh Y, Takahashi Y. Riluzole for the treatment of amyotrophic lateral sclerosis. Neurodegener Dis Manag. 2020;10(6):343–55.
Andrews JA, Jackson CE, Heiman-Patterson TD, Bettica P, Brooks BR, Pioro EP. Real-world evidence of riluzole effectiveness in treating amyotrophic lateral sclerosis. Amyotroph Lateral Scler Frontotemp Degener. 2020;21(7–8):509–18.
Writing G, Edaravone ALSSG. Safety and efficacy of edaravone in well defined patients with amyotrophic lateral sclerosis: a randomised, double-blind, placebo-controlled trial. Lancet Neurol. 2017;16(7):505–12.
Elia AE, Lalli S, Monsurro MR, Sagnelli A, Taiello AC, Reggiori B, et al. Tauroursodeoxycholic acid in the treatment of patients with amyotrophic lateral sclerosis. Eur J Neurol. 2016;23(1):45–52.
Cudkowicz ME, Andres PL, Macdonald SA, Bedlack RS, Choudry R, Brown RH Jr, et al. Phase 2 study of sodium phenylbutyrate in ALS. Amyotroph Lateral Scler. 2009;10(2):99–106.
Paganoni S, Hendrix S, Dickson SP, Knowlton N, Berry JD, Elliott MA, et al. Effect of sodium phenylbutyrate/taurursodiol on tracheostomy/ventilation-free survival and hospitalisation in amyotrophic lateral sclerosis: long-term results from the CENTAUR trial. J Neurol Neurosurg Psychiatry. 2022;93(8):871–5. https://doi.org/10.1136/jnnp-2022-329024.
Maher P, van Leyen K, Dey PN, Honrath B, Dolga A, Methner A. The role of ca(2+) in cell death caused by oxidative glutamate toxicity and ferroptosis. Cell Calcium. 2018;70:47–55.
Zagami CJ, O’Shea RD, Lau CL, Cheema SS, Beart PM. Regulation of glutamate transporters in astrocytes: evidence for a relationship between transporter expression and astrocytic phenotype. Neurotox Res. 2005;7(1–2):143–9.
Rothman DL, Behar KL, Hyder F, Shulman RG. In vivo NMR studies of the glutamate neurotransmitter flux and neuroenergetics: implications for brain function. Annu Rev Physiol. 2003;65:401–27.
Kanamori K, Kondrat RW, Ross BD. 13 C enrichment of extracellular neurotransmitter glutamate in rat brain–combined mass spectrometry and NMR studies of neurotransmitter turnover and uptake into glia in vivo. Cell Mol Biol (Noisy-le-grand). 2003;49(5):819–36.
Meeks JP, Mennerick S. Astrocyte membrane responses and potassium accumulation during neuronal activity. Hippocampus. 2007;17(11):1100–8.
Hosli L, Andres PF, Hosli E. Depolarization of cultured astrocytes by glutamate and aspartate. Neuroscience. 1979;4(11):1593–8.
Parpura V, Zorec R. Gliotransmission. Exocytotic release from astrocytes. Brain Res Rev. 2010;63(1–2):83–92.
Spreux-Varoquaux O, Bensimon G, Lacomblez L, Salachas F, Pradat PF, Le Forestier N, et al. Glutamate levels in cerebrospinal fluid in amyotrophic lateral sclerosis: a reappraisal using a new HPLC method with coulometric detection in a large cohort of patients. J Neurol Sci. 2002;193(2):73–8.
Rossi D, Brambilla L, Valori CF, Roncoroni C, Crugnola A, Yokota T, et al. Focal degeneration of astrocytes in amyotrophic lateral sclerosis. Cell Death Differ. 2008;15(11):1691–700.
Meyer K, Ferraiuolo L, Miranda CJ, Likhite S, McElroy S, Renusch S, et al. Direct conversion of patient fibroblasts demonstrates non-cell autonomous toxicity of astrocytes to motor neurons in familial and sporadic ALS. Proc Natl Acad Sci U S A. 2014;111(2):829–32.
Birger A, Ben-Dor I, Ottolenghi M, Turetsky T, Gil Y, Sweetat S, et al. Human iPSC-derived astrocytes from ALS patients with mutated C9ORF72 show increased oxidative stress and neurotoxicity. EBioMedicine. 2019;50:274–89.
Rajpurohit CS, Kumar V, Cheffer A, Oliveira D, Ulrich H, Okamoto OK, et al. Mechanistic insights of astrocyte-mediated hyperactive autophagy and loss of motor neuron function in SOD1(L39R) linked amyotrophic lateral sclerosis. Mol Neurobiol. 2020;57(10):4117–33.
Skorupa A, Urbach S, Vigy O, King MA, Chaumont-Dubel S, Prehn JH, et al. Angiogenin induces modifications in the astrocyte secretome: relevance to amyotrophic lateral sclerosis. J Proteom. 2013;91:274–85.
Kia A, McAvoy K, Krishnamurthy K, Trotti D, Pasinelli P. Astrocytes expressing ALS-linked mutant FUS induce motor neuron death through release of tumor necrosis factor-alpha. Glia. 2018;66(5):1016–33.
Tortelli R, Zecca C, Piccininni M, Benmahamed S, Dell’Abate MT, Barulli MR, et al. Plasma inflammatory cytokines are elevated in ALS. Front Neurol. 2020;11:552295.
Choi SS, Lee HJ, Lim I, Satoh J, Kim SU. Human astrocytes: secretome profiles of cytokines and chemokines. PLoS ONE. 2014;9(4):e92325.
Ouali Alami N, Schurr C, Olde Heuvel F, Tang L, Li Q, Tasdogan A, et al. NF-kappaB activation in astrocytes drives a stage-specific beneficial neuroimmunological response in ALS. EMBO J. 2018;37:16.
Mishra PS, Dhull DK, Nalini A, Vijayalakshmi K, Sathyaprabha TN, Alladi PA, et al. Astroglia acquires a toxic neuroinflammatory role in response to the cerebrospinal fluid from amyotrophic lateral sclerosis patients. J Neuroinflamm. 2016;13(1):212.
Izrael M, Slutsky SG, Admoni T, Cohen L, Granit A, Hasson A, et al. Safety and efficacy of human embryonic stem cell-derived astrocytes following intrathecal transplantation in SOD1(G93A) and NSG animal models. Stem Cell Res Ther. 2018;9(1):152.
Rosito M, Deflorio C, Limatola C, Trettel F. CXCL16 orchestrates adenosine A3 receptor and MCP-1/CCL2 activity to protect neurons from excitotoxic cell death in the CNS. J Neurosci. 2012;32(9):3154–63.
Israelson A, Ditsworth D, Sun S, Song S, Liang J, Hruska-Plochan M, et al. Macrophage migration inhibitory factor as a chaperone inhibiting accumulation of misfolded SOD1. Neuron. 2015;86(1):218–32.
Guttenplan KA, Weigel MK, Adler DI, Couthouis J, Liddelow SA, Gitler AD, et al. Knockout of reactive astrocyte activating factors slows disease progression in an ALS mouse model. Nat Commun. 2020;11(1):3753.
Yamanaka K, Chun SJ, Boillee S, Fujimori-Tonou N, Yamashita H, Gutmann DH, et al. Astrocytes as determinants of disease progression in inherited amyotrophic lateral sclerosis. Nat Neurosci. 2008;11(3):251–3.
Velebit J, Horvat A, Smolic T, Prpar Mihevc S, Rogelj B, Zorec R, et al. Astrocytes with TDP-43 inclusions exhibit reduced noradrenergic cAMP and ca(2+) signaling and dysregulated cell metabolism. Sci Rep. 2020;10(1):6003.
Chaves-Filho AB, Pinto IFD, Dantas LS, Xavier AM, Inague A, Faria RL, et al. Alterations in lipid metabolism of spinal cord linked to amyotrophic lateral sclerosis. Sci Rep. 2019;9(1):11642.
Lee H, Lee JJ, Park NY, Dubey SK, Kim T, Ruan K, et al. Multi-omic analysis of selectively vulnerable motor neuron subtypes implicates altered lipid metabolism in ALS. Nat Neurosci. 2021;24(12):1673–85.
Lawton KA, Brown MV, Alexander D, Li Z, Wulff JE, Lawson R, et al. Plasma metabolomic biomarker panel to distinguish patients with amyotrophic lateral sclerosis from disease mimics. Amyotroph Lateral Scler Frontotemp Degener. 2014;15(5–6):362–70.
Moore SA, Yoder E, Murphy S, Dutton GR, Spector AA. Astrocytes, not neurons, produce docosahexaenoic acid (22:6 omega-3) and arachidonic acid (20:4 omega-6). J Neurochem. 1991;56(2):518–24.
Stella N, Tence M, Glowinski J, Premont J. Glutamate-evoked release of arachidonic acid from mouse brain astrocytes. J Neurosci. 1994;14(2):568–75.
Dumuis A, Pin JP, Oomagari K, Sebben M, Bockaert J. Arachidonic acid released from striatal neurons by joint stimulation of ionotropic and metabotropic quisqualate receptors. Nature. 1990;347(6289):182–4.
Dumuis A, Sebben M, Fagni L, Prezeau L, Manzoni O, Cragoe EJ Jr, et al. Stimulation by glutamate receptors of arachidonic acid release depends on the Na+/Ca2+ exchanger in neuronal cells. Mol Pharmacol. 1993;43(6):976–81.
Almer G, Teismann P, Stevic Z, Halaschek-Wiener J, Deecke L, Kostic V, et al. Increased levels of the pro-inflammatory prostaglandin PGE2 in CSF from ALS patients. Neurology. 2002;58(8):1277–9.
Ilzecka J. Prostaglandin E2 is increased in amyotrophic lateral sclerosis patients. Acta Neurol Scand. 2003;108(2):125–9.
Xia Q, Hu Q, Wang H, Yang H, Gao F, Ren H, et al. Induction of COX-2-PGE2 synthesis by activation of the MAPK/ERK pathway contributes to neuronal death triggered by TDP-43-depleted microglia. Cell Death Dis. 2015;6:e1702.
Zou YH, Guan PP, Zhang SQ, Guo YS, Wang P. Rofecoxib attenuates the pathogenesis of amyotrophic lateral sclerosis by alleviating cyclooxygenase-2-mediated mechanisms. Front Neurosci. 2020;14:817.
Pompl PN, Ho L, Bianchi M, McManus T, Qin W, Pasinetti GM. A therapeutic role for cyclooxygenase-2 inhibitors in a transgenic mouse model of amyotrophic lateral sclerosis. FASEB J. 2003;17(6):725–7.
Guttenplan KA, Weigel MK, Prakash P, Wijewardhane PR, Hasel P, Rufen-Blanchette U, et al. Neurotoxic reactive astrocytes induce cell death via saturated lipids. Nature. 2021;599(7883):102–7.
Dodge JC, Jensen EH, Yu J, Sardi SP, Bialas AR, Taksir TV, et al. Neutral lipid cacostasis contributes to disease pathogenesis in amyotrophic lateral sclerosis. J Neurosci. 2020;40(47):9137–47.
Gharbi T, Zhang Z, Yang GY. The function of astrocyte mediated extracellular vesicles in central nervous system diseases. Front Cell Dev Biol. 2020;8:568889.
Chun C, Smith AST, Kim H, Kamenz DS, Lee JH, Lee JB, et al. Astrocyte-derived extracellular vesicles enhance the survival and electrophysiological function of human cortical neurons in vitro. Biomaterials. 2021;271:120700.
Chaudhuri AD, Dastgheyb RM, Yoo SW, Trout A, Talbot CC Jr, Hao H, et al. TNFalpha and IL-1beta modify the miRNA cargo of astrocyte shed extracellular vesicles to regulate neurotrophic signaling in neurons. Cell Death Dis. 2018;9(3):363.
Zhao S, Sheng S, Wang Y, Ding L, Xu X, Xia X, et al. Astrocyte-derived extracellular vesicles: a double-edged sword in central nervous system disorders. Neurosci Biobehav Rev. 2021;125:148–59.
You Y, Borgmann K, Edara VV, Stacy S, Ghorpade A, Ikezu T. Activated human astrocyte-derived extracellular vesicles modulate neuronal uptake, differentiation and firing. J Extracell Vesicles. 2020;9(1):1706801.
Chen Y, Xia K, Chen L, Fan D. Increased interleukin-6 levels in the astrocyte-derived exosomes of sporadic amyotrophic lateral sclerosis patients. Front Neurosci. 2019;13:574.
Silverman JM, Christy D, Shyu CC, Moon KM, Fernando S, Gidden Z, et al. CNS-derived extracellular vesicles from superoxide dismutase 1 (SOD1)(G93A) ALS mice originate from astrocytes and neurons and carry misfolded SOD1. J Biol Chem. 2019;294(10):3744–59.
Feiler MS, Strobel B, Freischmidt A, Helferich AM, Kappel J, Brewer BM, et al. TDP-43 is intercellularly transmitted across axon terminals. J Cell Biol. 2015;211(4):897–911.
Varcianna A, Myszczynska MA, Castelli LM, O’Neill B, Kim Y, Talbot J, et al. Micro-RNAs secreted through astrocyte-derived extracellular vesicles cause neuronal network degeneration in C9orf72 ALS. EBioMedicine. 2019;40:626–35.
Keene SD, Greco TM, Parastatidis I, Lee SH, Hughes EG, Balice-Gordon RJ, et al. Mass spectrometric and computational analysis of cytokine-induced alterations in the astrocyte secretome. Proteomics. 2009;9(3):768–82.
Moore NH, Costa LG, Shaffer SA, Goodlett DR, Guizzetti M. Shotgun proteomics implicates extracellular matrix proteins and protease systems in neuronal development induced by astrocyte cholinergic stimulation. J Neurochem. 2009;108(4):891–908.
Greco TM, Seeholzer SH, Mak A, Spruce L, Ischiropoulos H. Quantitative mass spectrometry-based proteomics reveals the dynamic range of primary mouse astrocyte protein secretion. J Proteome Res. 2010;9(5):2764–74.
Hedl TJ, San Gil R, Cheng F, Rayner SL, Davidson JM, De Luca A, et al. Proteomics approaches for biomarker and drug target discovery in ALS and FTD. Front Neurosci. 2019;13:548.
Barber CN, Raben DM. Lipid metabolism crosstalk in the brain: glia and neurons. Front Cell Neurosci. 2019;13:212.
Ioannou MS, Jackson J, Sheu SH, Chang CL, Weigel AV, Liu H, et al. Neuron-astrocyte metabolic coupling protects against activity-induced fatty acid toxicity. Cell. 2019;177(6):1522–35.
Staurenghi E, Giannelli S, Testa G, Sottero B, Leonarduzzi G, Gamba P. Cholesterol dysmetabolism in Alzheimer’s disease: a starring role for astrocytes? Antioxidants (Basel). 2021;10(12):1890.
Genc S, Kurnaz IA, Ozilgen M. Astrocyte-neuron lactate shuttle may boost more ATP supply to the neuron under hypoxic conditions–in silico study supported by in vitro expression data. BMC Syst Biol. 2011;5:162.
Cali C, Tauffenberger A, Magistretti P. The strategic location of glycogen and lactate: from body energy reserve to brain plasticity. Front Cell Neurosci. 2019;13:82.
Mason S. Lactate shuttles in neuroenergetics-homeostasis, allostasis and beyond. Front Neurosci. 2017;11:43.
Belanger M, Allaman I, Magistretti PJ. Brain energy metabolism: focus on astrocyte-neuron metabolic cooperation. Cell Metab. 2011;14(6):724–38.
Descalzi G, Gao V, Steinman MQ, Suzuki A, Alberini CM. Lactate from astrocytes fuels learning-induced mRNA translation in excitatory and inhibitory neurons. Commun Biol. 2019;2:247.
Sun Y, Wang Y, Chen ST, Chen YJ, Shen J, Yao WB, et al. Modulation of the astrocyte-neuron lactate shuttle system contributes to neuroprotective action of fibroblast growth factor 21. Theranostics. 2020;10(18):8430–45.
Afridi R, Kim JH, Rahman MH, Suk K. Metabolic regulation of glial phenotypes: implications in neuron-glia interactions and neurological disorders. Front Cell Neurosci. 2020;14:20.
Van Houten B. Huntington’s disease: astrocytes shift to fatty acid metabolism. Trends Endocrinol Metab. 2019;30(9):575–7.
Farmer BC, Kluemper J, Johnson LA. Apolipoprotein E4 alters astrocyte fatty acid metabolism and lipid droplet formation. Cells. 2019;8(2):182.
Dowell JA, Johnson JA, Li L. Identification of astrocyte secreted proteins with a combination of shotgun proteomics and bioinformatics. J Proteome Res. 2009;8(8):4135–43.
Stella R, Bonadio RS, Cagnin S, Massimino ML, Bertoli A, Peggion C. Perturbations of the proteome and of secreted metabolites in primary astrocytes from the hSOD1(G93A) ALS mouse model. Int J Mol Sci. 2021;22(13):7028.
Ranjbar Taklimie F, Gasterich N, Scheld M, Weiskirchen R, Beyer C, Clarner T, et al. Hypoxia induces astrocyte-derived Lipocalin-2 in ischemic stroke. Int J Mol Sci. 2019;20(6):1271.
Kim BW, Jeong KH, Kim JH, Jin M, Kim JH, Lee MG, et al. Pathogenic upregulation of glial Lipocalin-2 in the parkinsonian dopaminergic system. J Neurosci. 2016;36(20):5608–22.
Bi F, Huang C, Tong J, Qiu G, Huang B, Wu Q, et al. Reactive astrocytes secrete lcn2 to promote neuron death. Proc Natl Acad Sci U S A. 2013;110(10):4069–74.
Mesquita SD, Ferreira AC, Falcao AM, Sousa JC, Oliveira TG, Correia-Neves M, et al. Lipocalin 2 modulates the cellular response to amyloid beta. Cell Death Differ. 2014;21(10):1588–99.
Suk K. Lipocalin-2 as a therapeutic target for brain injury: an astrocentric perspective. Prog Neurobiol. 2016;144:158–72.
Jin M, Kim JH, Jang E, Lee YM, Soo Han H, Woo DK, et al. Lipocalin-2 deficiency attenuates neuroinflammation and brain injury after transient middle cerebral artery occlusion in mice. J Cereb Blood Flow Metab. 2014;34(8):1306–14.
Rathore KI, Berard JL, Redensek A, Chierzi S, Lopez-Vales R, Santos M, et al. Lipocalin 2 plays an immunomodulatory role and has detrimental effects after spinal cord injury. J Neurosci. 2011;31(38):13412–9.
Behrens V, Voelz C, Muller N, Zhao W, Gasterich N, Clarner T, et al. Lipocalin 2 as a putative modulator of local inflammatory processes in the spinal cord and component of organ cross talk after spinal cord injury. Mol Neurobiol. 2021;58(11):5907–19.
Wei H, Wu X, You Y, Duran RC, Zheng Y, Narayanan KL, et al. Systematic analysis of purified astrocytes after SCI unveils Zeb2os function during astrogliosis. Cell Rep. 2021;34(5):108721.
Joilin G, Leigh PN, Newbury SF, Hafezparast M. An overview of MicroRNAs as biomarkers of ALS. Front Neurol. 2019;10:186.
Ricci C, Marzocchi C, Battistini S. MicroRNAs as biomarkers in amyotrophic lateral sclerosis. Cells. 2018;7(11):219.
Madathil SK, Nelson PT, Saatman KE, Wilfred BR. MicroRNAs in CNS injury: potential roles and therapeutic implications. BioEssays. 2011;33(1):21–6.
Di Pietro V, Yakoub KM, Scarpa U, Di Pietro C, Belli A. MicroRNA signature of traumatic brain injury: from the biomarker discovery to the point-of-care. Front Neurol. 2018;9:429.
Stoica L, Todeasa SH, Cabrera GT, Salameh JS, ElMallah MK, Mueller C, et al. Adeno-associated virus-delivered artificial microRNA extends survival and delays paralysis in an amyotrophic lateral sclerosis mouse model. Ann Neurol. 2016;79(4):687–700.
Thomsen GM, Gowing G, Latter J, Chen M, Vit JP, Staggenborg K, et al. Delayed disease onset and extended survival in the SOD1G93A rat model of amyotrophic lateral sclerosis after suppression of mutant SOD1 in the motor cortex. J Neurosci. 2014;34(47):15587–600.
Martier R, Liefhebber JM, Garcia-Osta A, Miniarikova J, Cuadrado-Tejedor M, Espelosin M, et al. Targeting RNA-mediated toxicity in C9orf72 ALS and/or FTD by RNAi-based gene therapy. Mol Ther Nucleic Acids. 2019;16:26–37.
Clark BS, Blackshaw S. Understanding the role of lncRNAs in nervous system development. Adv Exp Med Biol. 2017;1008:253–82.
Ponting CP, Oliver PL, Reik W. Evolution and functions of long noncoding RNAs. Cell. 2009;136(4):629–41.
He B, Chen W, Zeng J, Tong W, Zheng P. Long noncoding RNA NKILA transferred by astrocyte-derived extracellular vesicles protects against neuronal injury by upregulating NLRX1 through binding to mir-195 in traumatic brain injury. Aging. 2021;13(6):8127–45.
Zhu J, Tang J. LncRNA Gm14205 induces astrocytic NLRP3 inflammasome activation via inhibiting oxytocin receptor in postpartum depression. Biosci Rep. 2020;40(8):BSR20200672. https://doi.org/10.1042/BSR20200672.
Yadav RS, Tiwari NK. Lipid integration in neurodegeneration: an overview of Alzheimer’s disease. Mol Neurobiol. 2014;50(1):168–76.
Colombelli C, Aoun M, Tiranti V. Defective lipid metabolism in neurodegeneration with brain iron accumulation (NBIA) syndromes: not only a matter of iron. J Inherit Metab Dis. 2015;38(1):123–36.
Farmer BC, Walsh AE, Kluemper JC, Johnson LA. Lipid droplets in neurodegenerative disorders. Front Neurosci. 2020;14:742.
Blasco H, Veyrat-Durebex C, Bocca C, Patin F, Vourc’h P, Kouassi Nzoughet J, et al. Lipidomics reveals cerebrospinal-fluid signatures of ALS. Sci Rep. 2017;7(1):17652.
Wang G, Dinkins M, He Q, Zhu G, Poirier C, Campbell A, et al. Astrocytes secrete exosomes enriched with proapoptotic ceramide and prostate apoptosis response 4 (PAR-4): potential mechanism of apoptosis induction in Alzheimer disease (AD). J Biol Chem. 2012;287(25):21384–95.
Acknowledgements
We thank the Institute of Molecular and Cell Biology (A*STAR), Singapore for providing institutional support.
Funding
This review was funded by the National Research Foundation Fellowship (NRF-NRFF-2018-003) and the Intra-CREATE Thematic Grant (THE-002-0001).
Author information
Authors and Affiliations
Contributions
SYN conceptualized this work; both SYN and WN wrote the manuscript; WN designed the graphics in this manuscript. Both authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
All authors consent to the publication of this manuscript.
Competing interests
The authors declare no competing interests.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ng, W., Ng, SY. Remodeling of astrocyte secretome in amyotrophic lateral sclerosis: uncovering novel targets to combat astrocyte-mediated toxicity. Transl Neurodegener 11, 54 (2022). https://doi.org/10.1186/s40035-022-00332-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40035-022-00332-y