Abstract
Background
Studies on risk factors for carbapenem-resistant Klebsiella pneumoniae (CRKP) infection have provided inconsistent results, partly due to the choice of the control group. We conducted a systematic review and meta-analysis to assess the risk factors for CRKP infection by comparing CRKP-infected patients with two types of controls: patients infected with carbapenem-susceptible Klebsiella pneumoniae (comparison 1) or patients not infected with CRKP (comparison 2).
Methods
Data on potentially relevant risk factors for CRKP infection were extracted from studies indexed in PubMed, EMBASE, Web of Science or EBSCO databases from January 1996 to April 2019, and meta-analyzed based on the outcomes for each type of comparison.
Results
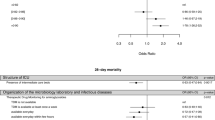
The meta-analysis included 18 studies for comparison 1 and 14 studies for comparison 2. The following eight risk factors were common to both comparisons: admission to intensive care unit (ICU; odds ratio, ORcomparison 1 = 3.20, ORcomparison 2 = 4.44), central venous catheter use (2.62, 3.85), mechanical ventilation (2.70, 4.78), tracheostomy (2.11, 8.48), urinary catheter use (1.99, 0.27), prior use of antibiotic (6.07, 1.61), exposure to carbapenems (4.16, 3.84) and exposure to aminoglycosides (1.85, 1.80). Another 10 risk factors were unique to comparison 1: longer length of hospital stay (OR = 15.28); prior hospitalization (within the previous 6 months) (OR = 1.91); renal dysfunction (OR = 2.17); neurological disorders (OR = 1.52); nasogastric tube use (OR = 2.62); dialysis (OR = 3.56); and exposure to quinolones (OR = 2.11), fluoroquinolones (OR = 2.03), glycopeptides (OR = 3.70) and vancomycin (OR = 2.82).
Conclusions
Eighteen factors may increase the risk of carbapenem resistance in K. pneumoniae infection; eight factors may be associated with both K. pneumoniae infections in general and CRKP in particular. The eight shared factors are likely to be ‘true’ risk factors for CRKP infection. Evaluation of risk factors in different situations may be helpful for empirical treatment and prevention of CRKP infections.
Similar content being viewed by others
Background
Carbapenem-resistant Gram-negative bacteria, mainly Klebsiella pneumoniae, are an emerging cause of healthcare-associated infections that pose a significant threat to public health [1]. The percentage of K. pneumoniae infections resistant to carbapenems continues to rise [2, 3], with proportions exceeding 50% in parts of the Eastern Mediterranean and Europe [1, 2]. K. pneumoniae carbapenemase originated in the northeastern USA in the early 2000s, but rapidly disseminated to other regions worldwide [4].
Carbapenem-resistant K. pneumoniae (CRKP) infection is difficult to treat since carbapenems are often considered last-resort antibiotics for severe K. pneumoniae infections. The most important genes that can confer carbapenem resistance (via carbapenemases) are present in K. pneumoniae, rendering almost all available treatment options ineffective [2]. Mortality rates reach 33–50% among CRKP-infected patients in different regions of the world [5], significantly higher than mortality caused by infection with carbapenem-susceptible K. pneumoniae (CSKP) [1]. Preventing CRKP infection is therefore important not only to avoid poor prognosis and even death, but also to prevent widespread transmission of carbapenem resistance through mobile genetic elements [6, 7].
Numerous studies have assessed risk factors for CRKP infection with different and sometimes even contradictory conclusions. A previous meta-analysis attempted to address this inconsistency [8] but did not take into consideration that different studies often use different control (reference) groups. The appropriate selection of the control group in the analysis of risk factors for antibiotic-resistant pathogen infections depends on the specific research question [9,10,11,12]. In studies analyzing risk factors for CRKP infection, two control groups are most often selected: patients infected with CSKP or patients without CRKP infection. The comparison of CRKP-infected with CSKP-infected patients may allow the identification of risk factors for carbapenem-resistant infections, although the results may be overestimated. In contrast, the comparison of CRKP-infected individuals with patients without CRKP infection may help to identify risk factors associated with both K. pneumoniae infections in general and CRKP in particular. Risk factors that are significant in both comparisons can be considered ‘true’ risk factors for CRKP infection [11, 12].
Thus, we performed a systematic review and meta-analysis to clarify risk factors for CRKP infection relative to infection with CSKP (comparison 1) or to the absence of CRKP infection (comparison 2). This design, similar to a case-control-control study, aimed to compare the results of the two analyses and their different implications for the clinical practice, allowing the identification of the likely true risk factors for CRKP infection.
Methods
This meta-analysis was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [13].
Search strategy
Two authors (H.Y.Z. and Z.Y.) searched for relevant studies in PubMed, EMBASE, Web of Science and EBSCO databases that were published from January 1996 to April 2019. The search terms included “Klebsiella pneumoniae” AND (“carbapenem-resistant” OR “imipenem-resistant” OR “meropenem-resistant” OR “ertapenem-resistant” OR “carbapenemase-producing” OR “Klebsiella pneumoniae carbapenemase”) AND (“risk factors” OR “risk” OR “factors”). Only studies published in English were considered. Reference lists in selected articles and relevant review articles were manually searched to identify additional studies.
Inclusion and exclusion criteria
Studies were included if they met the following criteria: (1) case-control or cohort study design, whether prospective or retrospective; (2) the risk factors for CRKP infection were reported; (3) either comparison 1 or comparison 2 was made; (4) CRKP and CSKP were classified based on K. pneumoniae isolate identification and tests for resistance to carbapenem (imipenem, meropenem, or ertapenem) involving well-defined microbiological methods; and (5) infection was explicitly defined. The inclusion criterion (3) led us to exclude studies comparing patients infected with carbapenemase-producing K. pneumoniae (CPKP) with controls without such infection, since such controls may have been infected with carbapenem-resistant, non-carbapenemase-producing K. pneumoniae. Studies were also excluded if they had the format of a report, review, comment, meeting abstract or letter to the editor; or if they reported insufficient data to assess outcomes.
Data extraction
Two authors (H.Y.Z. and W.M.Z.) independently evaluated and extracted data from the included studies using a predefined, standardized protocol. The extracted data on general characteristics of studies included the first author’s name, year of publication, journal of publication, country, study period, study design and setting, type of inter-group comparison, sample size, average age, and sex distribution. Potential risk factors were included in the meta-analysis only if at least three studies examined them and those studies reported the numbers of individuals in each comparison group. Disagreements about extracted data were resolved through discussion.
Quality assessment
Two authors (W.M.Z. and Z.Y.) independently evaluated the quality of each study using the Newcastle-Ottawa Scale (NOS), a scale for assessing the quality of published non-randomized studies in meta-analyses [14]. The scale contains eight items, categorized into three dimensions: selection, comparability, and outcome (cohort studies) or exposure (case-control studies) [14]. We developed a NOS-based scale ranging from 0 to 9 points: studies scoring 0–4 points were defined as low quality, while those scoring 5–9 points were defined as high quality. Differences were resolved by consensus.
Statistical analysis
The meta-analysis was performed using RevMan 5.2 software provided by The Cochrane Collaboration (Copenhagen: The Nordic Cochrane Centre, 2014). Pooled odds ratios (ORs) and 95% confidence intervals (CIs) were calculated for all outcomes. The Z-test was used to determine the significance of the pooled OR, and the results were considered statistically significant when P < 0.05. Statistical heterogeneity among studies was assessed using a chi-squared test in which P < 0.10 was taken as the threshold for significant heterogeneity, or by calculating I2 value, with I2 > 50% considered evidence of heterogeneity [15]. Depending on the assessed heterogeneity, the Mantel-Haenszel fixed- or random-effect methods were used to meta-analyze the outcomes.
Publication bias was quantitatively analyzed using Egger’s test in STATA software version 12.0 (College Station, TX: StataCorp LP) [16], and the results were considered statistically significant when P < 0.05. Sensitivity analyses were conducted by omitting studies one by one, and the P values of pooled ORs were compared. The results were considered robust when the P values were not substantially different.
Results
Study selection
A total of 428 unique records were retrieved from electronic databases, and 203 duplicate records were removed. After screening of titles and abstracts, 171 records were excluded. The remaining 54 studies were read in full to determine the eligibility. In the end, 18 studies performing comparison 1 [17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34] and 14 for comparison 2 [35,36,37,38,39,40,41,42,43,44,45,46,47,48] were included in the systematic review, while subsets of these studies were included in the meta-analyses of the various risk factors (Fig. 1).
Study characteristics
The main characteristics of the 18 studies included in comparison 1 are presented in Table 1. The studies were published from 2007 to 2019, and involved 1010 patients with CRKP infection and 1190 with CSKP infection from nine countries: China (6 studies), Greece (3), Israel (2), USA (2), Italy (1), Colombia (1), Turkey (1), Brazil (1), and Georgia (1). The designs of the 18 studies were case-control (12), retrospective cohort (3), case-case-control (1), nested case-control (1), and prospective cohort (1). The comparison and reference groups were matched in 11 studies. All but three studies enrolled patients from a single center, and six studies enrolled only patients in the intensive care unit (ICU).
The main characteristics of the 14 studies included in comparison 2 are presented in Table 2. These studies were published from 2012 to 2019, and involved 893 patients with CRKP infection and 3073 without CRKP infection from six countries: Italy (6), USA (2), Greece (2), Turkey (2), Israel (1), and China (1). The designs of the studies were case-control (6), retrospective cohort (4), prospective cohort (2), case-case-control (1), and case-cohort (1). In six of these studies the comparison and reference groups were matched. All but one study enrolled patients from a single center and three studies involved only patients in the ICU.
Quality assessment
All studies in the review were judged to be of high quality based on NOS assessment. The 18 studies in comparison 1 scored an average of 7 (range 5–8) (Table 1). The 14 studies in comparison 2 scored an average of 6 (range 5–8) (Table 2).
Risk factors for CRKP infection based on CRKP-CSKP comparison (comparison 1)
Table 3 shows the risk factors for CRKP infection for this comparison, as well as the heterogeneity in the meta-analysis. All 43 risk factors were dichotomous variables except for the following continuous variables: length of hospital stay (LOS), length of ICU stay, and Acute Physiology and Chronic Health Evaluation (APACHE) II score on ICU admission. Of the 43 factors, the following 18 were statistically significant: longer LOS, prior hospitalization (within the previous 6 months), admission to ICU, renal dysfunction, neurological disorders, tracheostomy, mechanical ventilation, central venous catheter (CVC) use, urinary catheter use, nasogastric tube use, implementation of dialysis, prior use of any antibiotic, and specific use of carbapenems, aminoglycosides, quinolones, fluoroquinolones, glycopeptides, or vancomycin.
Risk factors for CRKP infection compared with absence of CRKP infection (comparison 2)
Table 4 shows the risk factors for CRKP infection for this comparison, as well as the heterogeneity in the meta-analysis. All 20 risk factors were dichotomous variables, and the following eight were statistically significant: admission to ICU, tracheostomy, mechanical ventilation, CVC use, urinary catheter use, prior antibiotic use, and specific use of carbapenems or aminoglycosides.
Publication bias
Egger’s test showed no obvious asymmetry in the risk factors, suggesting low risk of publication bias (Tables 3 and 4).
Sensitivity analyses
The sensitivity analysis was performed by repeating the meta-analysis after omitting each study one by one and examining whether the results changed substantially. For most risk factors, no single study seemed to substantially alter the results. We noted two exceptions: in comparison 1, omitting the study by Mouloudi et al. from 2010 [30] made the factor “β-lactam + β-lactamase inhibitor” significant (OR 2.42, 95% CI 1.08 to 5.44); in comparison 2, removing the study by Mouloudi et al. in 2014 [37] made the factor “diabetes” significant (OR 1.39, 95% CI 1.01 to 1.90).
Discussion
CRKP is one of the most serious life-threating nosocomial pathogens worldwide, and CRKP infections are highly prevalent in most of the countries where the studies included in our review were performed (such as Italy, China, Greece, USA, Turkey and Israel). The proportion K. pneumoniae infections involving meropenem resistance in China increased from 14.1% in 2013 to 28.6% in 2018, with four provinces showing CRKP proportions > 10% in 2013 (the highest was Zhejiang province with 37.40%) and 13 in 2017 (the highest was Henan province with 53.01%) [49]. The proportion of K. pneumoniae infections involving meropenem resistance has grown steeply in the USA from 0.6% in 2004 to 10.8% in 2007 [50]. The most severely affected European countries are Greece and Italy, where 64.7 and 29.7% of K. pneumoniae infections in 2017 showed carbapenem resistance [3]. The proportion of CRKP infections in Turkey increased from 3.2% in 2010 to 66.9% in 2014 [39]. Israel faced a nationwide CRKP outbreak in 2006 that, by mid-2007, had infected 1275 patients in 27 hospitals [51]. The identification of risk factors of CRKP is the first step to discover high-risk patients and high-risk wards in order to channel limited resources most effectively into prevention and treatment.
Unfortunately, although many studies have investigated risk factors for CRKP infection, they have come to diverging, often conflicting, conclusions. For example, some studies have reported that exposure to carbapenems increased the risk of CRKP infection [17,18,19,20,21,22, 27, 29, 31, 33], but others did not find the same effect [24, 30]. These discrepancies may reflect differences in sample size and overall lack of statistical power, which prompted us to perform a systematic review in order to assess the associations as reliably and comprehensively as possible.
We based our review on the idea that the choice of the control group for risk assessment can provide different results, as suggested in several previous studies [9,10,11,12]. We meta-analyzed 32 studies in nine countries involving several thousands of patients. Consistent with our initial idea, the profiles of risk factors differed between comparisons 1 and 2, with immediate implications for clinical practice. Comparison 1 assessed risk factors for carbapenem-resistant infections, which are relevant for the situation when the patient is known to be infected with K. pneumoniae but tests of antibiotic susceptibility are pending. In this case, the clinician estimates the probability of resistance to carbapenem based on risk factors, adopting an empirical approach that prioritizes interventions to prevent transmission of carbapenem resistance at this early stage. In this type of comparison, our analysis identified the following risk factors: prior hospitalization (within the previous 6 months), longer length of stay, admission to the ICU, concomitant diseases (renal dysfunction, neurological disorders), certain invasive procedures (tracheostomy, mechanical ventilation, CVC, urinary catheter, nasogastric tube and dialysis), prior use of any antibiotic, and specific exposure to vancomycin or other five classes of antimicrobial agents (carbapenems, aminoglycosides, quinolones, fluoroquinolones, glycopeptides). These risk factors are more likely to be present in patients with more severe illness and greater susceptibility to infection, and who are therefore exposed to greater antibiotic selection pressure, which may ultimately increase the likelihood of infection with multidrug-resistant pathogens [20].
Comparison 2 is more relevant for the situation when hospitals need to identify patients at increased risk of suffering K. pneumoniae infection in general and CRKP in particular. The impact of risk factors on CRKP infection reflects an integrated effect of K. pneumoniae characteristics and carbapenem resistance. This may allow clinicians and hospital epidemiologists to take timely action to prevent CRKP transmission, even when no pathogen is detected in patient specimens, which may be due to their use of medications. In this type of comparison, our analysis identified the following risk factors: admission to ICU, certain invasive procedures (tracheostomy, mechanical ventilation, CVC, urinary catheter), prior use of any antibiotic, and exposure to carbapenems or aminoglycosides. Importantly, these risk factors were also statistically significant in comparison 1, which means that they are probably true risk factors for acquiring CRKP infection among hospitalized patients.
In contrast, dialysis and exposure to fluoroquinolones or glycopeptides were risk factors only for the first comparison. These factors may therefore increase primarily the risk of carbapenem resistance in K. pneumoniae. Indeed, fluoroquinolone exposure can generate resistance not only to fluoroquinolones but also to carbapenems, as fluoroquinolones lead to upregulation of the multidrug efflux pump MexEF-OprN and downregulation of the porin OprD, which is involved in carbapenem resistance [51, 52]. In addition, a quinolone resistance gene that causes low-level fluoroquinolone resistance is located on K. pneumoniae plasmids carrying carbapenemase genes [52]. Long-term administration of the glycopeptide vancomycin may disrupt the balance of microflora in the body, promoting the propagation of Gram-negative bacteria and increasing the rate of mutation and spread of carbapenemases, which may augment the risk of CRKP [18]. These considerations imply that restricting the use of fluoroquinolones and glycopeptides, whenever possible, may decrease the transmission of carbapenem resistance.
Our sensitivity analysis confirmed that meta-analysis results were robust, with the possible exceptions of exposure to β-lactam + β-lactamase inhibitor (comparison 1) and diabetes (comparision 2). The status of these variables as risk factors changed depending on the inclusion of two small studies [30, 37]. The heterogeneity surrounding these variables suggests the need for further studies to confirm their relationship with risk of CRKP infection.
Compared to a previous meta-analysis with a similar goal [8], the present work included 12 additional studies involving 2981 patients published after September 2016. In addition, we excluded studies comparing patients infected with CPKP with controls without CPKP infection, and our results for separate two comparisons contrast with a previous meta-analysis that aggregated both types of comparison. Consistent with our initial hypothesis, we identified several differences in the risk factors that were significant in each comparison, and we were able to derive a set of likely true risk factors of CRKP infection as those factors significant in both comparisons. The previous work identified the following significant risk factors: exposure to glycopeptides, parenteral nutrition, length of ICU stay and steroid therapy [8]. In our analysis, however, exposure to glycopeptides was significant only in comparison 1, while length of ICU stay and steroid therapy were not significant in comparison 1, and parenteral nutrition was not significant in either type of comparison, suggesting that these four factors may not be considered true risk factors. Furthermore, we found urinary catheter use to be a significant risk factor in both types of comparison, contrary to the previous meta-analysis.
Like the previously published meta-analysis on risk factors of CRKP infection [8], our exclusion criteria did not include that the source or base population of both case and control groups were identified with CRKP colonization based on rectal culture. With the exception of two studies [35, 36], the studies included in our meta-analysis did not perform rectal screening for CRKP, and thus potential CRKP rectal colonization was not identified. In these cases, it was difficult to judge whether the risk factors associated with the process of CRKP colonization developing into infection or acquiring CRKP and having it cause infection. Moreover, the relative timing of CRKP colonization and onset of risk factors is often difficult to determine [36]. Further studies are needed in which risk factors associated with CRKP colonization developing into infection, which would then allow meta-analysis to identify the risk factors for CRKP infection among patients with CRKP colonization.
The findings of our meta-analysis should be interpreted with caution given that some potential risk factors were analyzed based on data from a small number of studies. Indeed, data for some factors showed significant heterogeneity across studies, especially in comparison 2, probably because control patients included those without any infection as well as those infected with nosocomial pathogens other than CRKP. Most studies in our review were retrospective and all were observational, increasing the risk of patient selection bias, outcome reporting bias and confounding. Nevertheless, all studies received NOS scores indicating high quality, and no obvious publication bias was observed for any of the factors. Factors affecting risk of CRKP infection should be further examined in large, well-controlled prospective studies.
Conclusions
This meta-analysis identified 18 factors that increase the risk of carbapenem resistance in K. pneumoniae infection and eight factors which were associated with both K. pneumoniae infections in general and CRKP in particular. The eight shared factors are probably ‘true’ risk factors for CRKP infection. These findings may help clinicians and hospital epidemiologists estimate the likelihood of CRKP infection in different situations, and thereby initiate timely, targeted treatment and prevention measures.
Abbreviations
- APACHE:
-
Acute Physiology and Chronic Health Evaluation
- CI :
-
Confidence interval
- CPKP:
-
Carbapenemase-producing Klebsiella pneumoniae
- CRKP:
-
Carbapenem-resistant Klebsiella pneumoniae
- CSKP:
-
Carbapenem-susceptible Klebsiella pneumoniae
- CVC:
-
Central venous catheter
- HBV:
-
Hepatitis B virus
- HCC:
-
Hepatocellular carcinoma
- HCV:
-
Hepatitis C virus
- ICU:
-
Intensive care unit
- LOS:
-
Length of hospital stay
- MD:
-
Mean difference
- NA:
-
Not available
- NOS:
-
Newcastle-Ottawa Scale
- OR:
-
Odds ratio
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- SD:
-
Standard deviation
References
World Health Organization. Antimicrobial resistance global report on surveillance. https://apps.who.int/iris/bitstream/handle/10665/112642/9789241564748_eng.pdf;jsessionid=7CD2D037F35036393D8BC456B03B1991?sequence=1. Accessed 6 Apr 2019.
Prestinaci F, Pezzotti P, Pantosti A. Antimicrobial resistance: a global multifaceted phenomenon. Pathog Glob Health. 2015;109(7):309–18.
European Centre for Disease Prevention and Control. Surveillance of antimicrobial resistance in Europe - Annual report of the European Antimicrobial Resistance Surveillance Network (EARS-Net) 2017. Available at: https://ecdc.europa.eu/sites/portal/files/. Accessed 30 Nov 2018.
Tzouvelekis LS, Markogiannakis A, Psichogiou M, Tassios PT, Daikos GL. Carbapenemases in Klebsiella pneumoniae and other Enterobacteriaceae: an evolving crisis of global dimensions. Clin Microbiol Rev. 2012;25(4):682–707.
Xu L, Sun X, Ma X. Systematic review and meta-analysis of mortality of patients infected with carbapenem-resistant Klebsiella pneumoniae. Ann Clin Microbiol Antimicrob. 2017;16(1):18.
Gupta N, Limbago BM, Patel JB, Kallen AJ. Carbapenem-resistant Enterobacteriaceae: epidemiology and prevention. Clin Infect Dis. 2011;53(1):60–7.
Yigit H, Queenan AM, Anderson GJ, Domenech-Sanchez A, Biddle JW, Steward CD, et al. Novel carbapenem-hydrolyzing beta-lactamase, KPC-1, from a carbapenem-resistant strain of Klebsiella pneumoniae. Antimicrob Agents Chemother. 2001;45(4):1151–61.
Liu P, Li X, Luo M, Xu X, Su K, Chen S, et al. Risk factors for carbapenem-resistant Klebsiella pneumoniae infection: a meta-analysis. Microb Drug Resist. 2018;24(2):190–8.
Behar PR, Teixeira PJ, Fachel JM, Kalil AC. The effect of control group selection in the analysis of risk factors for extended spectrum beta-lactamase-producing Klebsiella pneumoniae infections. A prospective controlled study. J Hosp Infect. 2008;68(2):123–9.
Kaye KS, Harris AD, Samore M, Carmeli Y. The case-case-control study design: addressing the limitations of risk factor studies for antimicrobial resistance. Infect Control Hosp Epidemiol. 2005;26(4):346–51.
Harris AD, Karchmer TB, Carmeli Y, Samore MH. Methodological principles of case-control studies that analyzed risk factors for antibiotic resistance: a systematic review. Clin Infect Dis. 2001;32:1055–61.
Rodriguez-Bano J, Picon E, Gijon P, et al. Risk factors and prognosis of nosocomial bloodstream infections caused by extended-spectrum-beta-lactamase-producing Escherichia coli. J Clin Microbiol. 2010;48:1726–31.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62(10):1006–12.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–5.
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–58.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Gomez Rueda V, Zuleta Tobon JJ. Risk factors for infection with carbapenem-resistant Klebsiella pneumoniae: a case-case-control study. Colomb Med (Cali). 2014;45(2):54–60.
Wu D, Cai J, Liu J. Risk factors for the acquisition of nosocomial infection with carbapenem-resistant Klebsiella pneumoniae. South Med J. 2011;104(2):106–10.
Falagas ME, Rafailidis PI, Kofteridis D, Virtzili S, Chelvatzoglou FC, Papaioannou V, et al. Risk factors of carbapenem-resistant Klebsiella pneumoniae infections: a matched case control study. J Antimicrob Chemother. 2007;60(5):1124–30.
Patel G, Huprikar S, Factor SH, Jenkins SG, Calfee DP. Outcomes of carbapenem-resistant Klebsiella pneumoniae infection and the impact of antimicrobial and adjunctive therapies. Infect Control Hosp Epidemiol. 2008;29(12):1099–106.
Simkins J, Muggia V, Cohen HW, Minamoto GY. Carbapenem-resistant Klebsiella pneumoniae infections in kidney transplant recipients: a case-control study. Transpl Infect Dis. 2014;16(5):775–82.
Hu Y, Ping Y, Li L, Xu H, Yan X, Dai H. A retrospective study of risk factors for carbapenem-resistant Klebsiella pneumoniae acquisition among ICU patients. J Infect Dev Ctries. 2016;10(3):208–13.
Candevir Ulu A, Kurtaran B, Inal AS, Komur S, Kibar F, Yapici Cicekdemir H, et al. Risk factors of carbapenem-resistant Klebsiella pneumoniae infection: a serious threat in ICUs. Med Sci Monit. 2015;21:219–24.
Vardakas KZ, Matthaiou DK, Falagas ME, Antypa E, Koteli A, Antoniadou E. Characteristics, risk factors and outcomes of carbapenem-resistant Klebsiella pneumoniae infections in the intensive care unit. J Inf Secur. 2015;70(6):592–9.
Correa L, Martino MD, Siqueira I, Pasternak J, Gales AC, Silva CV, et al. A hospital-based matched case-control study to identify clinical outcome and risk factors associated with carbapenem-resistant Klebsiella pneumoniae infection. BMC Infect Dis. 2013;13:80.
Zheng X, Wang JF, Xu WL, Xu J, Hu J. Clinical and molecular characteristics, risk factors and outcomes of Carbapenem-resistant Klebsiella pneumoniae bloodstream infections in the intensive care unit. Antimicrob Resist Infect Control. 2017;6:102.
Zheng B, Dai Y, Liu Y, Shi W, Dai E, Han Y, et al. Molecular epidemiology and risk factors of carbapenem-resistant Klebsiella pneumoniae infections in eastern China. Front Microbiol. 2017;8:1061.
Shilo S, Assous MV, Lachish T, Kopuit P, Bdolah-Abram T, Yinnon AM, et al. Risk factors for bacteriuria with carbapenem-resistant Klebsiella pneumoniae and its impact on mortality: a case-control study. Infection. 2013;41(2):503–9.
Wang Z, Qin RR, Huang L, Sun LY. Risk factors for carbapenem-resistant Klebsiella pneumoniae infection and mortality of Klebsiella pneumoniae infection. Chin Med J. 2018;131(1):56–62.
Mouloudi E, Protonotariou E, Zagorianou A, Iosifidis E, Karapanagiotou A, Giasnetsova T, et al. Bloodstream infections caused by metallo-beta-lactamase/Klebsiella pneumoniae carbapenemase-producing K. pneumoniae among intensive care unit patients in Greece: risk factors for infection and impact of type of resistance on outcomes. Infect Control Hosp Epidemiol. 2010;31(12):1250–6.
Hussein K, Raz-Pasteur A, Finkelstein R, Neuberger A, Shachor-Meyouhas Y, Oren I, et al. Impact of carbapenem resistance on the outcome of patients’ hospital-acquired bacteraemia caused by Klebsiella pneumoniae. J Hosp Infect. 2013;83(4):307–13.
Pan H, Lou Y, Zeng L, Wang L, Zhang J, Yu W, et al. Infections caused by carbapenemase-producing Klebsiella pneumoniae: microbiological characteristics and risk factors. Microb Drug Resist. 2019;25(2):287–96.
Tsereteli M, Sidamonidze K, Tsereteli D, Malania L, Vashakidze E. Epidemiology of carbapenem-resistant Klebsiella pneumoniae in intensive care units of multiprofile hospitals in Tbilisi, Georgia. Georgian Med News. 2018;7-8(280–281):164–8.
Hoxha A, Karki T, Giambi C, Montano C, Sisto A, Bella A, et al. Attributable mortality of carbapenem-resistant Klebsiella pneumoniae infections in a prospective matched cohort study in Italy, 2012-2013. J Hosp Infect. 2016;92(1):61–6.
Borer A, Saidel-Odes L, Eskira S, Nativ R, Riesenberg K, Livshiz-Riven I, et al. Risk factors for developing clinical infection with carbapenem-resistant Klebsiella pneumoniae in hospital patients initially only colonized with carbapenem-resistant K. pneumoniae. Am J Infect Control. 2012;40(5):421–5.
Giannella M, Trecarichi EM, De Rosa FG, Del Bono V, Bassetti M, Lewis RE, et al. Risk factors for carbapenem-resistant Klebsiella pneumoniae bloodstream infection among rectal carriers: a prospective observational multicentre study. Clin Microbiol Infect. 2014;20(12):1357–62.
Mouloudi E, Massa E, Papadopoulos S, Iosifidis E, Roilides I, Theodoridou T, et al. Bloodstream infections caused by carbapenemase-producing Klebsiella pneumoniae among intensive care unit patients after orthotopic liver transplantation: risk factors for infection and impact of resistance on outcomes. Transplant Proc. 2014;46(9):3216–8.
Giannella M, Bartoletti M, Morelli MC, Tedeschi S, Cristini F, Tumietto F, et al. Risk factors for infection with carbapenem-resistant Klebsiella pneumoniae after liver transplantation: the importance of pre- and posttransplant colonization. Am J Transplant. 2015;15(6):1708–15.
Akgul F, Bozkurt I, Sunbul M, Esen S, Leblebicioglu H. Risk factors and mortality in the Carbapenem-resistant Klebsiella pneumoniae infection: case control study. Pathog Glob Health. 2016;110(7–8):321–5.
Yang D, Xie Z, Xin X, Xue W, Zhang M. A model for predicting nosocomial carbapenem-resistant Klebsiella pneumoniae infection. Biomed Rep. 2016;5(4):501–5.
Micozzi A, Gentile G, Minotti C, Cartoni C, Capria S, Ballaro D, et al. Carbapenem-resistant Klebsiella pneumoniae in high-risk haematological patients: factors favouring spread, risk factors and outcome of carbapenem-resistant Klebsiella pneumoniae bacteremias. BMC Infect Dis. 2017;17(1):203.
Mazza E, Prosperi M, Panzeri MF, Limuti R, Nichelatti M, De Gasperi A. Carbapenem-resistant Klebsiella pneumoniae infections early after liver transplantation: a single-center experience. Transplant Proc. 2017;49(4):677–81.
Varotti G, Dodi F, Terulla A, Santori G, Mariottini G, Bertocchi M, et al. Impact of carbapenem-resistant Klebsiella pneumoniae (CR-KP) infections in kidney transplantation. Transpl Infect Dis. 2017;19(6):e12757.
Salsano A, Giacobbe DR, Sportelli E, Olivieri GM, Brega C, Di Biase C, et al. Risk factors for infections due to carbapenem-resistant Klebsiella pneumoniae after open heart surgery. Interact Cardiovasc Thorac Surg. 2016;23(5):762–8.
Kontopoulou K, Iosifidis E, Antoniadou E, Tasioudis P, Petinaki E, Malli E, et al. The clinical significance of carbapenem-resistant Klebsiella pneumoniae rectal colonization in critically ill patients: from colonization to bloodstream infection. J Med Microbiol. 2019;68(3):326–35.
Gallagher JC, Kuriakose S, Haynes K, Axelrod P. Case-case-control study of patients with carbapenem-resistant and third-generation-cephalosporin-resistant Klebsiella pneumoniae bloodstream infections. Antimicrob Agents Chemother. 2014;58(10):5732–5.
Kalpoe JS, Sonnenberg E, Factor SH, del Rio MJ, Schiano T, Patel G, et al. Mortality associated with carbapenem-resistant Klebsiella pneumoniae infections in liver transplant recipients. Liver Transpl. 2012;18(4):468–74.
Akturk H, Sutcu M, Somer A, Aydin D, Cihan R, Ozdemir A, et al. Carbapenem-resistant Klebsiella pneumoniae colonization in pediatric and neonatal intensive care units: risk factors for progression to infection. Braz J Infect Dis. 2016;20(2):134–40.
CHINET. China antimicrobial resistance surveillance system report. Available at: http://www.chinets.com/Home/Login?return URL = http://www.chinets.com/. Accessed 30 Mar 2019.
Rhomberg PR, Jones RN. Summary trends for the Meropenem yearly susceptibility test information collection program: a 10-year experience in the United States (1999-2008). Diagn Microbiol Infect Dis. 2009;65(4):414–26.
Schwaber MJ, Lev B, Israeli A, Solter E, Smollan G, Rubinovitch B, et al. Containment of a country-wide outbreak of carbapenem-resistant Klebsiella pneumoniae in Israeli hospitals via a nationally implemented intervention. Clin Infect Dis. 2011;52(7):848–55.
Jiao Y, Qin Y, Liu J, Li Q, Dong Y, Shang Y, et al. Risk factors for carbapenem-resistant Klebsiella pneumoniae infection/colonization and predictors of mortality: a retrospective study. Pathog Glob Health. 2015;109(2):68–74.
Acknowledgements
We thank the authors of the studies included in our meta-analysis for sharing their data.
Funding
This work was supported by the Humanities and Social Sciences Research Project of the Chongqing Education Commission, China [grant number 17SKG019].
Author information
Authors and Affiliations
Contributions
WmZ, ZY and HyZ designed the study. WmZ and HyZ searched the literature and extracted data, which HyZ analyzed. WmZ, ZY and HyZ drafted the manuscript, which all authors revised. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Zhu, Wm., Yuan, Z. & Zhou, Hy. Risk factors for carbapenem-resistant Klebsiella pneumoniae infection relative to two types of control patients: a systematic review and meta-analysis. Antimicrob Resist Infect Control 9, 23 (2020). https://doi.org/10.1186/s13756-020-0686-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13756-020-0686-0