Abstract
Purpose
Carbapenem resistant K. pneumoniae (CRKP) has aroused widespread attention owing to its very limited therapeutic options, and this strain has increased rapidly in recent years. Although it is accepted that drug resistance is associated with increased mortality in general, but some other studies found no such relationship. To estimate mortality of patients infected with CRKP in general and analyze factors for mortality of this infection, thus, we conducted this systematic review and meta-analysis.
Methods
A systematic literature review of relevant studies published until December 2015 was conducted. We selected and assessed articles reporting mortality of patients infected with CRKP.
Results
Pooled mortality was 42.14% among 2462 patients infected with CRKP versus 21.16% in those infected with carbapenem-susceptible K. pneumoniae (CSKP). The mortality of patients with bloodstream infection (BSI) or urinary tract infection was 54.30 and 13.52%, respectively, and 48.9 and 43.13% in patients admitted to the intensive care unit (ICU) or who underwent solid organ transplantation (SOT). Mortality was 47.66% in patients infected with K. pneumoniae carbapenemase-producing K. pneumoniae and 46.71% in those infected with VIM-producing K. pneumoniae. Geographically, mortality reported in studies from North America, South America, Europe, and Asia was 33.24, 46.71, 50.06, and 44.82%, respectively.
Conclusions
Our study suggests that patients infected with CRKP have higher mortality than those infected with CSKP, especially in association with BSI, ICU admission, or SOT. We also considered that patients’ survival has a close relationship with their physical condition. Our results imply that attention should be paid to CRKP infection, and that strict infection control measures and new antibiotics are required to protect against CRKP infection.
Similar content being viewed by others
Background
It is well known that Klebsiella pneumoniae is ubiquitous in nature, one of the most relevant opportunistic pathogens, and causes various human infections such as bloodstream infection (BSI), urinary tract infection (UTI), surgical-site infection, and pneumonia [1–3]. Resistance can develop in K. pneumoniae isolates, notably producing extended-spectrum β-lactamases (ESBLs). ESBL-producing strains of K. pneumoniae are currently found throughout the world and have caused numerous outbreaks of infection [4, 5]. Carbapenems represent the first-line therapy for severe infection by ESBL-producing K. pneumoniae [6]. However, since Yigit et al. [7, 8] reported the first K. pneumoniae carbapenem (KPC)-producing K. pneumoniae isolate in North Carolina in 1996, carbapenem-resistant strains have increased rapidly, rising from 1.6 to 10.4% associated with central line blood-stream infections between 2001 and 2011 in the United States, and have aroused widespread attention, presenting a challenge because the antimicrobial treatment options remain very restricted [7, 9].
Carbapenem-resistant K. pneumoniae (CRKP) deactivates the carbapenems through two main mechanisms: (1) acquisition of carbapenemase genes that encode for enzymes capable of hydrolyzing carbapenems—the three most important carbapenemase types being KPC-type enzymes, metallo-β-lactamases (VIM, IMP, NDM), and OXA-48 type enzymes; and (2) reduction in the accumulation of antibiotics by a quantitative and/or qualitative deficiency of porin expression in combination with overexpression of β-lactamases that possess weak affinity for carbapenems [10].
Most researchers reported higher mortality rates among persons infected with CRKP isolates [11–30] while others reported contrary results [31, 32]. In recent years, many studies from single medical centers or individual countries have reported mortality rates in patients infected with CRKP, but until now there has been no systematic review focusing on mortality resulting from carbapenem-resistant infections in general. Although in a recent meta-analysis Falagas et al. [33] reported a higher all-cause mortality among patients infected with carbapenem-resistant Enterobacteriaceae than in those with carbapenem-susceptible infections, but their research included only nine studies. Considering this scenario, we conducted a systematic review and meta-analysis to estimate the mortality of patients infected with CRKP, and analyzed mortality resulting from multiple infection types and patients conditions.
Methods
Search strategy
Two independent examiners (LF.X. and XX.S.) searched entries in the PubMed and EMBASE databases from their inception until December 22, 2015 to identify potentially relevant studies. The search terms included “Klebsiella pneumoniae” AND resistance AND (“carbapenem” OR “imipenem” OR “meropenem” OR “ertapenem”). The language was restricted to English.
Inclusion and exclusion criteria
Studies were considered in accordance with inclusion criteria if articles reported mortality of patients infected with CRKP. Research that focused on children, did not differentiate mortality between infection and colonization, did not define the strains that were carbapenem resistant, and did not present the exact death toll were excluded. In this analysis, carbapenem resistance was defined as resistance to carbapenems such as imipenem, meropenem, and ertapenem, irrespective of susceptibility to other antibiotics.
Assessment of study quality
The articles were assessed for quality of the cohort or case–control studies included in the systematic analysis according to the Newcastle-Ottawa scale (NOS) score [34], ranging from 0 to 9. Studies with a NOS score of 5 or greater were included in this analysis.
Data extraction
Two independent investigators (LF.X. and XX.S.) extracted information from eligible articles. Divergences were solved by discussion and consultation of the relevant literature. The information extracted from original publications included title, first author, year of publication and experiment, type of study, sample size, characteristics of the study population (mean age, sex, type of infection, mean severity of underlying disease), and crude mortality rates in patients infected with CRKP and carbapenem-susceptible K. pneumoniae (CSKP). If articles reported mortality from both infection and colonization, we extracted information only regarding infections.
Statistical analysis
We calculated the pooled odds ratio (OR) and 95% confidence interval (CI) by comparing crude mortality in patients with CRKP with that in patients with CSKP. Between-study heterogeneity was assessed by the χ2 test (p < 0.10 was selected to indicate the presence of heterogeneity, in which case a random-effects model was adopted; otherwise a fixed-effects model was applied) and I 2 test (to assess the degree of heterogeneity) [35, 36]. We then calculated pooled rates of mortality in patients infected with CRKP, and stratified analyses with respect to geographic location, infection types, carbapenemase types, and patients conditions performed. Freeman–Tukey arcsine transformations were used to stabilize the variances, and after the meta-analysis we transformed the summary estimates and the CI boundaries back to proportions using the sine function [37]. We used Stata version 12.0 software for all statistical calculations.
Results
Results of the systematic literature search
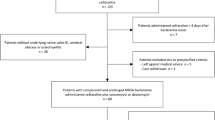
We identified and screened 3168 articles. After exclusion by title and abstract, the remaining 87 articles were subjected to full-text assessment for eligibility. Among these articles, 12 were duplicates, seven did not differentiate between infection- and colonization-related mortality, and six did not report valid data. Ultimately, 62 studies were analyzed based on the inclusion and exclusion criteria (Fig. 1).
The basic characteristics of these 62 studies are summarized in Table 1 [11–32, 38–77]. These articles were published from 1999 to 2015 and the sample size varied across studies, ranging from 7 to 1022. The total number of patients in this systematic review was 4701, of whom 2462 had CRKP infection and the remainder CSKP infection. Among these patients, the reported death was 1018 among the CRKP patients and 398 among the CSKP patients. In the pooled analysis, the overall mortality was 42.14% (95% CI 37.06–47.31) in patients infected with CRKP and 21.16% (95% CI 16.07–26.79) in CSKP patients (Table 2).
Comparison of mortality in CRKP and CSKP patients
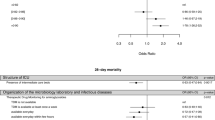
Among the included articles, 22 compared mortality between patients infected with CRKP and CSKP. The summary estimate of these studies from the random-effects model suggested that patients with CRKP had a significantly higher mortality than those with CSKP in the univariate analysis (pooled crude OR 2.80; 95% CI 2.15–3.65) with a moderate heterogeneity I 2 of 33.9% (p = 0.031) (Fig. 2).
Mortality in multiple patient conditions
As shown in Table 2, 722 patients had BSI and 284 had UTI, 479 were in an intensive care unit (ICU), and 362 underwent solid organ transplantation (SOT). In the pooled analysis, the mortality was 54.30% (95% CI 47.51–61.02), 13.52% (95% CI 7.50–20.92), 48.9% (95% CI 44.47–53.46), and 43.13% (95% CI 32.40–54.16) in BSI, UTI, ICU-admission, and SOT patients, respectively.
Mortality in multiple carbapenemase types
In this subgroup analysis, we mainly analyzed the mortality of patients infected with KPC-producing K. pneumoniae and VIM-producing K. pneumoniae. In the articles included, 302 patients were infected with KPC-producing K. pneumoniae and 73 were infected with VIM-producing K. pneumoniae. The mortality among these two types of carbapenemases was 47.66% (95% CI 38.61–56.79) and 46.71% (95% CI 35.81–57.73), respectively (Table 2).
Mortality in different geographic locations
Twenty-three studies were carried out in North America, eight in South America, twenty-one in Europe, and ten in Asia. The rate of mortality was 33.24% (95% CI 25.08–42.00) of 980 patients in North America, 46.71% (95% CI 39.83–53.66) of 191 in South America, 50.06% (95% CI 41.45–58.62) of 860 in Europe, and 44.82% (95% CI 37.83–51.91) of 431 in Asia (Table 2).
Discussion
ESBL-producing K. pneumoniae as an opportunistic pathogen is becoming more challenging to treat because of the emergence of carbapenem resistance, and has a significant influence on patient mortality. The primary result of this analysis was the pooled crude mortality of 42.14% among patients with CRKP, which is intimately connected with patients’ health and physical status.
Although it is accepted that drug resistance is associated with increased mortality because patients tend to receive inappropriate empiric therapy in general [4, 78], other studies have found no such relationship. Bhavnani et al. [79] reported that clinical success was similar between patients with ESBL and those with non-ESBL-producing K. pneumoniae, and ESBL production alone did not appear to be an independent risk factor for treatment failure. Kim et al. [80] also found that ESBL production was not significantly associated with death. In addition, García-Sureda et al. [81] reported that CRKP isolates are less virulent and fit than CSKP isolates in an antibiotic-free environment. We conducted this systematic review and meta-analysis to estimate the mortality of patients infected with CRKP in general and to study the factors related to mortality resulting from this infection. We found that patients infected with CRKP had significantly higher mortality in comparison with CSKP (crude OR 2.80). To identify risk factors associated with the higher mortality of CRKP infections, we conducted a stratified analysis of patient condition, carbapenemase types, and study location.
Based on multiple patient conditions, our analysis confirmed that patients with CRKP in association with BSI, ICU admission, or SOT have a higher mortality than the pooled mortality, although UTI patients have a lower mortality than the pooled overall mortality, even lower than that of CSKP patients. From this result, we assumed that patient survival has a close relationship with patients’ underlying illness and comorbidities. Mouloudi et al. [26] reported that BSI, ICU admission, and recent receipt of a SOT were associated with ICU and in-hospital mortality in patients infected with CRKP. In addition, patients who had undergone organ transplantation or ICU admission were always subjected to surgical procedures, prolonged ICU stay, preexisting immunosuppression, and the use of invasive devices, which contributed to patients’ poor physical condition and resultant higher mortality. In contrast, Daikos et al. suggested that UTI is a relatively mild infection that has only a slight influence on the general condition of patients, and carries a low mortality in general [25]. It has been shown that factors such as underlying illness and comorbidities have a more important influence on mortality than appropriate empiric treatment with multidrug-resistant Gram-negative bacteria [82]. Although the underlying patient’s condition is important for the outcome of such patients, meanwhile a timely effective treatment can also help to improve the survival rate. Patients in a poor state of health with CRKP were subjected to pathogens longer compared to CSKP infection due to lack of an effective therapy, ultimately, led to a higher mortality.
In the present analysis, patients infected with KPC-producing K. pneumoniae have a higher mortality than pooled overall mortality (47.66 vs 42.14%). This result may contribute to KPC-producing K. pneumoniae having stronger invasiveness, and the KPC-encoding blaKPC always carry other drug-resistant genes, leading to a pronounced drug resistant [83]. Previous studies have demonstrated K. pneumoniae-encoding blaKPC to be an independent risk factor in patient mortality [26, 27]. In addition, KPC-producing K. pneumoniae is considered a successful pathogen because of its ability to persist and spread, causing nosocomial outbreaks. Bratu et al. [84] reported that KPC-producing K. pneumoniae isolates are resistant to not only all β-lactam antimicrobials but also frequently other classes of antimicrobials, such as aminoglycosides and fluoroquinolones. In this systematic review, the patients from North America have lower mortality in comparison with the other three locations. This phenomenon may be attributed to a higher level of medical care and different treatment methods in North America, such as combination antibiotics, treatment with polymyxins and tigecycline, and adjunctive procedures (e.g., catheter removal, drainage, or debridement). There is evidence that tigecycline and polymyxins have activity against many CRKP isolates in vitro, and there have been cases reported of successful treatment of CRKP infection with polymyxins and tigecycline [85–87]. Patel et al. [30] also reported that removal of the focus of infection (i.e., debridement) was independently associated with patient survival.
There are several limitations to this analysis. First, as the included studies reported only unadjusted data on mortality, we analyzed only crude mortality among patients with CRKP. Second, most studies may have lacked power in differentiating death caused by CRKP from any other factors, and it is difficult to draw definitive conclusions from current evidence because of the residual confounding factors and small sample sizes in many studies. Third, some studies included in our meta-analysis did not define a cutoff value to judge the susceptibility of K. pneumoniae to carbapenems, and when defined the cutoff value varied among studies owing to different reference criteria. Thus, there exists the potential for heterogeneity. Fourth, most studies were retrospective in nature and thus susceptible to selection bias. Last, we selected only English-language articles, thus limiting the scope of our analysis.
Conclusions
Our study suggests that patients infected with CRKP have a higher mortality than those infected with CSKP, especially patients with BSI, ICU admission, or SOT intervention. We suggest that the survival of patients has a close relationship with their physical condition. Thus, our results imply that attention should be paid to CRKP infection in patients in a poor state of health, and that strict infection control measures and new antibiotics are required to protect against CRKP infection.
Abbreviations
- CRKP:
-
carbapenem-resistant Klebsiella pneumoniae
- CSKP:
-
carbapenem-suscepyible Klebsiella pneumoniae
- BSI:
-
bloodstream infection
- UTI:
-
urinary tract infection
- ICU:
-
intensive care unit
- SOT:
-
solid organ transplantation
References
Podschun R, Ullmann U. Klebsiella spp. as nosocomial pathogens: epidemiology, taxonomy, typing methods, and pathogenicity factors. Clin Microbiol Rev. 1998;11:589–603.
Daikos GL, Markogiannakis A, Souli M, Tzouvelekis LS. Bloodstream infections caused by carbapenemase-producing Klebsiella pneumoniae: a clinical perspective. Expert Rev Anti Infect Ther. 2012;10(12):1393–404.
Broberg CA, Palacios M, Miller VL. Klebsiella: a long way to go towards understanding this enigmatic jet-setter. F1000prime Rep. 2014;6:64.
Tumbarello M, Spanu T, Sanguinetti M, Citton R, Montuori E, Leone F, Fadda G, Cauda R. Bloodstream infections caused by extended-spectrum-beta-lactamase-producing Klebsiella pneumoniae: risk factors, molecular epidemiology, and clinical outcome. Antimicrob Agents Chemother. 2006;50(2):498–504.
Paterson DL, Yu VL. Editorial response: extended-spectrum β-lactamases: a call for improved detection and control. Clin Infect Dis. 1999;29:1419–22.
Pitout JDD, Laupland KB. Extended-spectrum β-lactamase-producing Enterobacteriaceae: an emerging public-health concern. Lancet Infect Dis. 2008;8(3):159–66.
Yigit H, Queenan AM, Anderson GJ, Domenech-Sanchez A, Biddle JW, Steward CD, Alberti S, Bush K, Tenover FC. Novel carbapenem-hydrolyzing beta-lactamase, KPC-1, from a carbapenem-resistant strain of Klebsiella pneumoniae. Antimicrob Agents Chemother. 2001;45(4):1151–61.
Jacob JT, Klein E, Laxminarayan R, Beldavs Z, Lynfield R, Kallen AJ, Ricks P, Edwards J, Srinivasan A, Fridkin S, et al. Vital signs: carbapenem-resistant Enterobacteriaceae. Morb Mortal Wkly Rep. 2013;62(9):165–70.
Nordmann P, Cuzon G, Naas T. The real threat of Klebsiella pneumoniae carbapenemase-producing bacteria. Lancet Infect Dis. 2009;9(4):228–36.
Nordmann P, Dortet L, Poirel L. Carbapenem resistance in Enterobacteriaceae: here is the storm! Trends Mol Med. 2012;18(5):263–72.
Vardakas KZ, Matthaiou DK, Falagas ME, Antypa E, Koteli A, Antoniadou E. Characteristics, risk factors and outcomes of carbapenem-resistant Klebsiella pneumoniae infections in the intensive care unit. J Infect. 2015;70(6):592–9.
Pouch SM, Kubin CJ, Satlin MJ, Tsapepas DS, Lee JR, Dube G, Pereira MR. Epidemiology and outcomes of carbapenem-resistant Klebsiella pneumoniae bacteriuria in kidney transplant recipients. Transpl Infect Dis. 2015;17(6):800–9.
Ny P, Nieberg P, Wong-Beringer A. Impact of carbapenem resistance on epidemiology and outcomes of nonbacteremic Klebsiella pneumoniae infections. Am J Infect Control. 2015;43(10):1076–80.
Hoxha A, Karki T, Giambi C, Montano C, Sisto A, Bella A, D’Ancona F, Study Working G. Attributable mortality of carbapenem-resistant Klebsiella pneumoniae infections in a prospective matched cohort study in Italy, 2012–2013. J Hosp Infect. 2015;92(1):61–6.
Cubero M, Cuervo G, Dominguez MA, Tubau F, Marti S, Sevillano E, Gallego L, Ayats J, Pena C, Pujol M, et al. Carbapenem-resistant and carbapenem-susceptible isogenic isolates of Klebsiella pneumoniae ST101 causing infection in a tertiary hospital. BMC Microbiol. 2015;15:177.
Brizendine KD, Richter SS, Cober ED, van Duin D. Carbapenem-resistant Klebsiella pneumoniae urinary tract infection following solid organ transplantation. Antimicrob Agents Chemother. 2015;59(1):553–7.
Simkins J, Muggia V, Cohen HW, Minamoto GY. Carbapenem-resistant Klebsiella pneumoniae infections in kidney transplant recipients: a case-control study. Transpl Infect Dis. 2014;16(5):775–82.
Rueda VG. Risk factors for infection with carbapenem-resistant Klebsiella pneumoniae: a case–case–control study. Colomb Méd. 2014;45(2):54–60.
Orsi GB, Bencardino A, Vena A, Carattoli A, Venditti C, Falcone M, Giordano A, Venditti M. Patient risk factors for outer membrane permeability and KPC-producing carbapenem-resistant Klebsiella pneumoniae isolation: results of a double case–control study. Infection. 2013;41(1):61–7.
Hussein K, Raz-Pasteur A, Finkelstein R, Neuberger A, Shachor-Meyouhas Y, Oren I, Kassis I. Impact of carbapenem resistance on the outcome of patients’ hospital-acquired bacteraemia caused by Klebsiella pneumoniae. J Hosp Infect. 2013;83(4):307–13.
Cober E, Brizendine K, Richter S, Koval C, Van Duin D. Impact of carbapenem resistance in Klebsiella pneumoniae blood stream infection in solid organ transplantation. Am J Transpl. 2013;13(SUPPL. 5):186.
Correa L, Martino MDV, Siqueira I, Pasternak J, Gales AC, Silva CV, Camargo TZS, Scherer PF, Marra AR. A hospital-based matched case–control study to identify clinical outcome and risk factors associated with carbapenem-resistant Klebsiella pneumoniae infection. BMC Infect Dis. 2013;13(1):80.
Liu SW, Chang HJ, Chia JH, Kuo AJ, Wu TL, Lee MH. Outcomes and characteristics of ertapenem-nonsusceptible Klebsiella pneumoniae bacteremia at a university hospital in Northern Taiwan: a matched case–control study. J Microbiol Immunol Infect. 2012;45(2):113–9.
Ben-David D, Kordevani R, Keller N, Tal I, Marzel A, Gal-Mor O, Maor Y, Rahav G. Outcome of carbapenem resistant Klebsiella pneumoniae bloodstream infections. Clin Microbiol Infect. 2012;18(1):54–60.
Orsi GB, Garcia-Fernandez A, Giordano A, Venditti C, Bencardino A, Gianfreda R, Falcone M, Carattoli A, Venditti M. Risk factors and clinical significance of ertapenem-resistant Klebsiella pneumoniae in hospitalised patients. J Hosp Infect. 2011;78(1):54–8.
Mouloudi E, Protonotariou E, Zagorianou A, Iosifidis E, Karapanagiotou A, Giasnetsova T, Tsioka A, Roilides E, Sofianou D, Gritsi-Gerogianni N. Bloodstream infections caused by metallo-beta-lactamase/Klebsiella pneumoniae carbapenemase-producing K. pneumoniae among intensive care unit patients in Greece: risk factors for infection and impact of type of resistance on outcomes. Infect Control Hosp Epidemiol. 2010;31(12):1250–6.
Gasink LB, Edelstein PH, Lautenbach E, Synnestvedt M, Fishman NO. Risk factors and clinical impact of Klebsiella pneumoniae carbapenemase-producing K. pneumoniae. Infect Control Hosp Epidemiol. 2009;30(12):1180–5.
Daikos GL, Petrikkos P, Psichogiou M, Kosmidis C, Vryonis E, Skoutelis A, Georgousi K, Tzouvelekis LS, Tassios PT, Bamia C, et al. Prospective observational study of the impact of VIM-1 metallo-beta-lactamase on the outcome of patients with Klebsiella pneumoniae bloodstream infections. Antimicrob Agents Chemother. 2009;53(5):1868–73.
Schwaber MJ, Klarfeld-Lidji S, Navon-Venezia S, Schwartz D, Leavitt A, Carmeli Y. Predictors of carbapenem-resistant Klebsiella pneumoniae acquisition among hospitalized adults and effect of acquisition on mortality. Antimicrob Agents Chemother. 2008;52(3):1028–33.
Patel G, Huprikar S, Factor SH, Jenkins SG, Calfee DP. Outcomes of carbapenem-resistant Klebsiella pneumoniae infection and the impact of antimicrobial and adjunctive therapies. Infect Control Hosp Epidemiol. 2008;29(12):1099–106.
Gaviria D, Bixler D, Thomas CA, Ibrahim SM. Carbapenem-resistant Klebsiella pneumoniae associated with a long-term-care facility—West Virginia, 2009–2011. Morb Mortal Wkly Rep. 2011;60:1418–20.
Falagas ME, Rafailidis PI, Kofteridis D, Virtzili S, Chelvatzoglou FC, Papaioannou V, Maraki S, Samonis G, Michalopoulos A. Risk factors of carbapenem-resistant Klebsiella pneumoniae infections: a matched case control study. J Antimicrob Chemother. 2007;60(5):1124–30.
Falagas ME, Tansarli GS, Karageorgopoulos DE, Vardakas KZ. Deaths attributable to carbapenem-resistant Enterobacteriaceae infections. Emerg Infect Dis. 2014;20(7):1170–5.
Wells, G. A. et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. (2014). Available at: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 15 Feb 2015.
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–58.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–88.
Freeman MF, Tukey JW. Transformations related to the angular and the square root. Ann Math Stat. 1950;21(4):607–11.
van Duin D, Cober E, Richter SS, Perez F, Kalayjian RC, Salata RA, Evans S, Fowler VG Jr, Kaye KS, Bonomo RA. Impact of therapy and strain type on outcomes in urinary tract infections caused by carbapenem-resistant Klebsiella pneumoniae. J Antimicrob Chemother. 2015;70(4):1203–11.
Girmenia C, Rossolini GM, Piciocchi A, Bertaina A, Pisapia G, Pastore D, Sica S, Severino A, Cudillo L, Ciceri F, et al. Infections by carbapenem-resistant Klebsiella pneumoniae in SCT recipients: a nationwide retrospective survey from Italy. Bone Marrow Transplant. 2015;50(2):282–8.
Chang YY, Chuang YC, Siu LK, Wu TL, Lin JC, Lu PL, Wang JT, Wang LS, Lin YT, Huang LJ, et al. Clinical features of patients with carbapenem nonsusceptible Klebsiella pneumoniae and Escherichia coli in intensive care units: a nationwide multicenter study in Taiwan. J Microbiol Immunol Infect. 2015;48(2):219–25.
van Duin D, Perez F, Rudin SD, Cober E, Hanrahan J, Ziegler J, Webber R, Fox J, Mason P, Richter SS, et al. Surveillance of carbapenem-resistant Klebsiella pneumoniae: tracking molecular epidemiology and outcomes through a regional network. Antimicrob Agents Chemother. 2014;58(7):4035–41.
Qureshi ZA, Syed A, Clarke LG, Doi Y, Shields RK. Epidemiology and clinical outcomes of patients with carbapenem-resistant Klebsiella pneumoniae bacteriuria. Antimicrob Agents Chemother. 2014;58(6):3100–4.
Mouloudi E, Massa E, Papadopoulos S, Iosifidis E, Roilides I, Theodoridou T, Piperidou M, Orphanou A, Passakiotou M, Imvrios G, et al. Bloodstream infections caused by carbapenemase-producing Klebsiella pneumoniae among intensive care unit patients after orthotopic liver transplantation: risk factors for infection and impact of resistance on outcomes. Transplant Proc. 2014;46(9):3216–8.
Gallagher JC, Kuriakose S, Haynes K, Axelrod P. Case-case-control study of patients with carbapenem-resistant and third-generation-cephalosporin-resistant Klebsiella pneumoniae bloodstream infections. Antimicrob Agents Chemother. 2014;58(10):5732–5.
Shilo S, Assous MV, Lachish T, Kopuit P, Bdolah-Abram T, Yinnon AM, Wiener-Well Y. Risk factors for bacteriuria with carbapenem-resistant Klebsiella pneumoniae and its impact on mortality: a case–control study. Infection. 2013;41(2):503–9.
Di Carlo P, Gulotta G, Casuccio A, Pantuso G, Raineri M, Farulla CA, Bonventre S, Guadagnino G, Ingrassia D, Cocorullo G, Mammina C, Giarratano A. KPC-3 Klebsiella pneumoniae ST258 clone infection in postoperative abdominal surgery patients in an intensive care setting: analysis of a case series of 30 patients. BMC Anesthesiol. 2013;13(1):13.
Pereira GH, Garcia DO, Mostardeiro M, Fanti KS, Levin AS. Outbreak of carbapenem-resistant Klebsiella pneumoniae: two-year epidemiologic follow-up in a tertiary hospital. Mem Inst Oswaldo Cruz. 2013;108(1):113–5.
Kontopidou F, Giamarellou H, Katerelos P, Maragos A, Kioumis I, Trikka-Graphakos E, Valakis C, Maltezou HC. Infections caused by carbapenem-resistant Klebsiella pneumoniae among patients in intensive care units in Greece: a multi-centre study on clinical outcome and therapeutic options. Clin Microbiol Infect. 2013;20(2):O117–23.
Clancy CJ, Chen L, Shields RK, Zhao Y, Cheng S, Chavda KD, Hao B, Hong JH, Doi Y, Kwak EJ, et al. Epidemiology and molecular characterization of bacteremia due to carbapenem-resistant Klebsiella pneumoniae in transplant recipients. Am J Transplant. 2013;13(10):2619–33.
Cicora F, Mos F, Paz M, Allende NG, Roberti J. Infections with blaKPC-2-producing Klebsiella pneumoniae in renal transplant patients: a retrospective study. Transplant Proc. 2013;45(9):3389–93.
Sanchez-Romero I, Asensio A, Oteo J, Munoz-Algarra M, Isidoro B, Vindel A, Alvarez-Avello J, Balandin-Moreno B, Cuevas O, Fernandez-Romero S, et al. Nosocomial outbreak of VIM-1-producing Klebsiella pneumoniae isolates of multilocus sequence type 15: molecular basis, clinical risk factors, and outcome. Antimicrob Agents Chemother. 2012;56(1):420–7.
Kalpoe JS, Sonnenberg E, Factor SH, del Rio Martin J, Schiano T, Patel G, Huprikar S. Mortality associated with carbapenem-resistant Klebsiella pneumoniae infections in liver transplant recipients. Liver Transplant. 2012;18(4):468–74.
Borer A, Saidel-Odes L, Eskira S, Nativ R, Riesenberg K, Livshiz-Riven I, Schlaeffer F, Sherf M, Peled N. Risk factors for developing clinical infection with carbapenem-resistant Klebsiella pneumoniae in hospital patients initially only colonized with carbapenem-resistant K. pneumoniae. Am J Infect Control. 2012;40(5):421–5.
Bergamasco MD, Barroso Barbosa M, de Oliveira Garcia D, Cipullo R, Moreira JC, Baia C, Barbosa V, Abboud CS. Infection with Klebsiella pneumoniae carbapenemase (KPC)-producing K. pneumoniae in solid organ transplantation. Transpl Infect Dis. 2012;14(2):198–205.
Balkhy HH, El-Saed A, Al Johani SM, Francis C, Al-Qahtani AA, Al-Ahdal MN, Altayeb HT, Arabi Y, Alothman A, Sallah M. The epidemiology of the first described carbapenem-resistant Klebsiella pneumoniae outbreak in a tertiary care hospital in Saudi Arabia: how far do we go? Eur J Clin Microbiol Infect Dis. 2012;31(8):1901–9.
Pereira GH, Garcia DO, Mostardeiro M, Ogassavara CT, Levin AS. Spread of carbapenem-resistant Klebsiella pneumoniae in a tertiary hospital in Sao Paulo, Brazil. J Hosp Infect. 2011;79(2):182–3.
Neuner EA, Yeh JY, Hall GS, Sekeres J, Endimiani A, Bonomo RA, Shrestha NK, Fraser TG, van Duin D. Treatment and outcomes in carbapenem-resistant Klebsiella pneumoniae bloodstream infections. Diagn Microbiol Infect Dis. 2011;69(4):357–62.
Beirão EM, Furtado JJD, Girardello R, Ferreira H, Gales AC. Clinical and microbiological characterization of KPC-producing Klebsiella pneumoniae infections in Brazil. Braz J Infect Dis. 2011;15(1):69–73.
Cuzon G, Ouanich J, Gondret R, Naas T, Nordmann P. Outbreak of OXA-48-positive carbapenem-resistant Klebsiella pneumoniae isolates in France. Antimicrob Agents Chemother. 2011;55(5):2420–3.
Nguyen M, Eschenauer GA, Bryan M, O’Neil K, Furuya EY, Della-Latta P, Kubin CJ. Carbapenem-resistant Klebsiella pneumoniae bacteremia: factors correlated with clinical and microbiologic outcomes. Diagn Microbiol Infect Dis. 2010;67(2):180–4.
Gregory CJ, Llata E, Stine N, Gould C, Santiago LM, Vazquez GJ, Robledo IE, Srinivasan A, Goering RV, Tomashek KM. Outbreak of carbapenem-resistant Klebsiella pneumoniae in Puerto Rico associated with a novel carbapenemase variant. Infect Control Hosp Epidemiol. 2010;31(5):476–84.
Borer A, Saidel-Odes L, Riesenberg K, Eskira S, Peled N, Nativ R, Schlaeffer F, Sherf M. Attributable mortality rate for carbapenem-resistant Klebsiella pneumoniae bacteremia. Infect Control Hosp Epidemiol. 2009;30(10):972–6.
Woodford N, Tierno PM Jr, Young K, Tysall L, Palepou MF, Ward E, Painter RE, Suber DF, Shungu D, Silver LL, et al. Outbreak of Klebsiella pneumoniae producing a new carbapenem-hydrolyzing class A beta-lactamase, KPC-3, in a New York Medical Center. Antimicrob Agents Chemother. 2004;48(12):4793–9.
Ahmad M, Urban C, Mariano N, Bradford PA, Calcagni E, Projan SJ, Bush K, Rahal JJ. Clinical characteristics and molecular epidemiology associated with imipenem-resistant Klebsiella pneumoniae. Clin Infect Dis. 1999;29(2):352–5.
Welch S, Neuner E, Lam S, Bauer S, van Duin D, Eric C, Bass S. Antimicrobial treatment and mortality risk for carbapenem-resistant Klebsiella pneumonia. Crit Care Med. 2015;43(12 suppl 1):115–6.
Madrigal MD, Blazquez C, Saldana R, Rubio V. Infection and colonization by carbapenem resistant Klebsiella pneumoniae in haematology patients. Haematologica. 2015;100(SUPPL 1):471.
Katsiari M, Panagiota G, Likousi S, Roussou Z, Polemis M, Alkiviadis Vatopoulos C, Evangelia Platsouka D, Maguina A. Carbapenem-resistant Klebsiella pneumoniae infections in a Greek intensive care unit: molecular characterisation and treatment challenges. J Glob Antimicrob Resist. 2015;3(2):123–7.
Chen I-L, Huang H-J, Toh H-S. Outbreak of carbapenem-resistant Klebsiella pneumoniae in a regional hospital of southern Taiwan. J Microbiol Immunol Infect. 2015;48(2):S151.
Freire MP, Abdala E, Moura ML, de Paula FJ, Spadao F, Caiaffa-Filho HH, David-Neto E, Nahas WC, Pierrotti LC. Risk factors and outcome of infections with Klebsiella pneumoniae carbapenemase-producing K. pneumoniae in kidney transplant recipients. Infection. 2015;43(3):315–23.
Bias T, Sharma A, Malat G, Lee D. Doyle A (2015) Outcomes associated with carbapenem-resistant Klebsiella pneumoniae (CRKP) in solid organ transplant (SOT) recipients. Am J Transpl. 2015;15(Suppl 3):1.
Lübbert C, Rodloff AC, Laudi S, Simon P, Busch T, Mössner J, Bartels M, Kaisers UX. Sa1016 lessons learned from excess mortality due to kpc-producing Klebsiella pneumoniae in liver transplant recipients. Gastroenterology. 2014;46(5):S-938.
Ozden K, Ozturk G, Aydinli B, Uyanik MH, Albayrak A, Arslan S. Carbapenem resistant Klebsiella pneumoniae infection in liver transplant recipients. Liver Transplant. 2014;20(Suppl 1):S-292.
Grossi P, Mularoni A, Campanella M, Vizzini G, Conaldi P, Gridelli B. Carbapenem resistant Klebsiella pneumoniae (CRKP) infection in solid organ transplant recipients (SOT): a single center analysis. Am J Transplant. 2013;13:343.
Rose CKS, Bhatt P, MacDougall C, Gallagher I. A cohort study of patients with klebsiella bacteremia with carbapenem resistance compared to those with third-generation cephalosporin resistance. Crit Care Med. 2012;40(12 SUPPL 1):84.
Gallagher J, Bhatt PD, Marino E. A comparison of patients with Klebsiella bacteremia with imipenem-resistance to those with 3rd generation cephalosporin resistance. Pharmacotherapy. 2011;31(10):346e–7e.
Vardakas K, Matthaiou D, Antupa E, Pappas E, Kechagioglou G, Koteli A. Antoniadou E (2010) Characteristics and outcomes of intensive care unit patients with carbapenem-resistant Klebsiella pneumoniae bacteraemia. Clin Microbiol Infect. 2010;16(Suppl 2):S358.
Balandin Moreno B, Isidoro Fernandez B, Vazquez Grande G, Ortega MA, Alcantara Carmona S, Alvarez Martinez L. Infections with metallo-b-lactamase (MBL)-producing Klebsiella pneumoniae: clinical features of a nosocomial oubreak in a spanish intensive care unit. Intensive Care Med. 2010;36(SUPPL 2):S256.
Cordery RJ, Roberts CH, Cooper SJ, Bellinghan G, Shetty N. Evaluation of risk factors for the acquisition of bloodstream infections with extended-spectrum beta-lactamase-producing Escherichia coli and Klebsiella species in the intensive care unit; antibiotic management and clinical outcome. J Hosp Infect. 2008;68(2):108–15.
Bhavnani SM, Ambrose PG, Craig WA, Dudley MN, Jones RN, Program SAS. Outcomes evaluation of patients with ESBL- and non-ESBL-producing Escherichia coli and Klebsiella species as defined by CLSI reference methods: report from the SENTRY Antimicrobial Surveillance Program. Diagn Microbiol Infect Dis. 2006;54(3):231–6.
Kim BN, Woo JH, Kim MN, Ryu J, Kim YS. Clinical implications of extended-spectrum β-lactamase-producing Klebsiella pneumoniae bacteraemia. J Hosp Infect. 2002;52(2):99–106.
Garcia-Sureda L, Domenech-Sanchez A, Barbier M, Juan C, Gasco J, Alberti S. OmpK26, a novel porin associated with carbapenem resistance in Klebsiella pneumoniae. Antimicrob Agents Chemother. 2011;55(10):4742–7.
Vardakas KZ, Rafailidis PI, Konstantelias AA, Falagas ME. Predictors of mortality in patients with infections due to multi-drug resistant Gram negative bacteria: the study, the patient, the bug or the drug? J Infect. 2013;66(5):401–14.
Villegas MV, Lolans K, Correa A, Kattan JN, Lopez JA, Quinn JP, Colombian Nosocomial Resistance Study G. First identification of Pseudomonas aeruginosa isolates producing a KPC-type carbapenem-hydrolyzing beta-lactamase. Antimicrob Agents Chemother. 2007;51(4):1553–5.
Bratu S, Landman D, Haag R, Recco R, Eramo A, Alam M, Quale J. Rapid spread of carbapenem-resistant Klebsiella pneumoniae in New York City: a new threat to our antibiotic armamentarium. Arch Intern Med. 2005;165(12):1430–5.
Bratu S, Tolaney P, Karumudi U, Quale J, Mooty M, Nichani S, Landman D. Carbapenemase-producing Klebsiella pneumoniae in Brooklyn, NY: molecular epidemiology and in vitro activity of polymyxin B and other agents. J Antimicrob Chemother. 2005;56(1):128–32.
Karabinis A, Paramythiotou E, Mylona-Petropoulou D. Colistin for Klebsiella pneumoniae—associated sepsis. Clin Infect Dis. 2004;38(1):e7–9.
Daly MW, Riddle DJ, Ledeboer NA, Dunne WM, Ritchie DJ. Tigecycline for the treatment of pneumonia and empyema caused by carbapenemase producing Klebsiella pneumoniae. Pharmacotherapy. 2007;27(7):1052–7.
Fligou F, Papadimitriou-Olivgeris M, Sklavou C, Anastassiou ED, Marangos M, Filos K. Risk factors and predictors of mortality for KPC-producing Klebsiella pneumoniae bactereamia during intensive care unit stay. Eur J Anaesthesiology. 2013;30(suppl 51):187.
Authors’ contributions
LX and XS designed the study, performed the articles search and screen. LX wrote the paper. LX and XS performed the Statistical analysis. XM reviewed the manuscript. All authors read and approved the final manuscript.
Acknowledgements
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
The data and material in this review is authentic and available.
Consent for publication
Informed consent was obtained from all individual participants included in the review.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Xu, L., Sun, X. & Ma, X. Systematic review and meta-analysis of mortality of patients infected with carbapenem-resistant Klebsiella pneumoniae . Ann Clin Microbiol Antimicrob 16, 18 (2017). https://doi.org/10.1186/s12941-017-0191-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12941-017-0191-3