Abstract
Over the past 2 years, SARS-CoV-2 infection has resulted in numerous hospitalizations and deaths worldwide. As young intensivists, we have been at the forefront of the fight against the COVID-19 pandemic and it has been an intense learning experience affecting all aspects of our specialty. Critical care was put forward as a priority and managed to adapt to the influx of patients and the growing demand for beds, financial and material resources, thereby highlighting its flexibility and central role in the healthcare system. Intensivists assumed an essential and unprecedented role in public life, which was important when claiming for indispensable material and human investments. Physicians and researchers around the world worked hand-in-hand to advance research and better manage this disease by integrating a rapidly growing body of evidence into guidelines. Our daily ethical practices and communication with families were challenged by the massive influx of patients and restricted visitation policies, forcing us to improve our collaboration with other specialties and innovate with new communication channels. However, the picture was not all bright, and some of these achievements are already fading over time despite the ongoing pandemic and hospital crisis. In addition, the pandemic has demonstrated the need to improve the working conditions and well-being of critical care workers to cope with the current shortage of human resources. Despite the gloomy atmosphere, we remain optimistic. In this ten-key points review, we outline our vision on how to capitalize on the lasting impact of the pandemic to face future challenges and foster transformative changes of critical care for the better.
Similar content being viewed by others
Background
Over the past 2 years, more than six million deaths due to Coronavirus Disease 2019 (COVID-19) have been recorded worldwide [1] and this death toll may even be significantly underestimated [2]. The pandemic has led to an unprecedented increase in the number of patients admitted to intensive care units (ICU) [3, 4]. As young critical care caregivers in the early stages of their professional careers, we have been and remain at the forefront of the management of this enduring health crisis. While still in the throes of the current pandemic, it has already disrupted our newly acquired vision of critical care [5]. Since this disruption is likely to be systemic, the pandemic will have a lasting impact on critical care and it is important to introspect without further ado, in order to actively build up the framework for tomorrow's critical care.
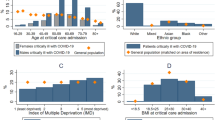
In this review, we examine how critical care has coped with some of the challenges posed by this pandemic (Fig. 1 and Table 1) in ten key points, and we make proposals for how we should capitalize on this experience to foster the transformative changes we hope for to provide better critical care, for caregivers and patients alike.
Main text
Central role and adaptability of intensive care within the healthcare system
To face this unprecedented influx of patients, the whole healthcare system was forced to adapt, from hospital to ambulatory care. Indeed, according to a 2018 international annual report, nearly half (43%) of 182 countries were not prepared to prevent, detect and control the outbreak of a new infectious disease [6]. The chaos of the first few weeks of the pandemic revealed that actually no countries were operationally equipped to deal with an outbreak of such magnitude. Given the potential severity of the disease, intensive care had a central role to deal with this pandemic and was on the frontline of a massive reorganization [7, 8]. All across the world, different strategies were set up to lower the pressure on overwhelmed ICUs [9,10,11], from the creation of temporary ICU beds through repurposing of non-critical care beds [12,13,14,15] and upgrading intermediate care beds to admit severe intubated patients, to inter-hospital transfer of critically ill patients, even across borders (Table 2). The latter strategy appears to be both effective and safe [16,17,18]. However, it may have increased the emotional burden on families and its cost-effectiveness is more than questionable in comparison to increasing ICU capacities. Moreover, this strategy may not be feasible in a pandemic in which all regions/countries are similarly affected.
Another lever of this reorganization was the redistribution of tasks and reallocation of resources from less essential activities, which was not without detrimental consequences. First, the suboptimal management of patients in structures not initially designed to host critically ill patients [19, 20] had a well demonstrated negative impact on the outcomes [21, 22]. And second, the reorganization of care to almost ‘‘100% COVID-19’’ was done at the expense of non-COVID-19 patients [23, 24], in particular patients with chronic diseases, such as cancer patients awaiting chemotherapy or surgery [25,26,27] (Table 2). Lastly, a reduction of Emergency Department visits was observed with an increased out-of-hospital mortality [28, 29].
While the COVID-19 pandemic is still active today, and in order to deal with future outbreaks, terrorist attacks [30,31,32], or environmental threats such as heat waves [33, 34], and in addition to investments in equipment, funding should support flexible ICU designs and expandable ICU bed capacity. An efficient approach to public–private partnership combined with a centralized health care system would improve the redistribution of medical devices and human resources in response to fluctuations in demand [5, 48] (Table 3). Critical care flexibility should be anticipated via predefined crisis protocols not only on a national and regional scale, but also on a local scale. Such protocols should identify a coordination team in advance, composed of both caregivers and administrative staff. It should also include stepwise measures to increase ICU capacity on the scale of each institution while providing continuity of essential tasks when coping with the influx of patients [35, 36]. In addition, critical care should be coordinated region- and nation-wide with the development of online registries allowing for real-time tracking of available ICU beds through an intuitive web application, such as COORD-REA® or the Repertoire Opérationnel des Ressources de l’offre de santé [37,38,39,40] in France, to facilitate the dispatching of patients in private or public institutions and prevent center overcrowding (Table 3).
As a result, critical care has had a central role in patient management and within the hospital health care system resulting in unprecedented visibility for our specialty.
Unprecedented visibility and recognition of intensive care
During the COVID-19 pandemic, and for the first time [41, 42], major decisions were taken by public health institutions in partnership with intensivists, including containment measures, vaccination strategies, welfare policies, healthcare system management and coordination to prevent ICU overflowing [43] (Table 1). We should be proud of the intensivists’ role in public health and their shared responsibility with governments [44].
Alongside policy makers, ICU caregivers have also gained recognition in the media through daily televised interventions, newspaper editorials [45,46,47] and social media involvement [48]. Here again, these interventions have positively contributed to the notoriety of intensive care. Yet, they have sometimes led to premature claims and misunderstandings that we should be careful to avoid in the future. To this end, we believe we should resist the siren’s call of short-term commentary when no scientific evidence exists. We should also prioritize long format and pedagogic interventions allowing to present controversies and doubt as one of the cornerstones of scientific reasoning and legitimate debate rather than a mere expression of division and incompetence that would ultimately lead to distrust [49]. Following this line of thought, we should also encourage every initiative to spread scientific culture that is too often lacking, including among the policy makers [50], through interventions in educational programs or in high-quality popular science channels that are flourishing on the web. Social media could rightly serve this purpose and we should definitely seize this opportunity to be in direct contact with the public. However, this will require adequate training to avoid some of the pitfalls of these new communication channels and protect ourselves against the fierceness of social networks [51]. Leading this media and digital campaign should be a priority of our academic organizations and professional unions to increase the visibility of all critical care professions.
As time passes by, we fear that the social legitimacy obtained during the first wave ultimately turns out to be more emotional than a genuine collective awareness of our importance in healthcare. Even if this was not the case, we may wonder how long this memory will last as indifference seems to be growing while people are still dying in the ICU during an umpteenth wave. Now that we have a foot in the door, we should all pursue the collective effort to nurture this unprecedented role of intensivists in public life.
Outstanding research dynamics
Thanks to political decisions and the mobilization of medical and scientific communities, the extraordinary dynamics of clinical, fundamental and translational research has been one of the genuine breakthroughs in the fight against COVID-19 [52] (Table 1). Since the early 2020s, the human investment in research from all specialties has led to a better understanding of the virus, its pathophysiology, and its impact on dysfunction organ allowing for better patient management in record time. Critical care research has been particularly efficient, accounting for more than 10% of global COVID-19-related publications [53, 54]. The surge in research has been supported by combined efforts of critical care professionals, fast-track institutional review processes and ethics committee approval [45]. Early large-scale studies including critically ill COVID-19 patients have impacted COVID-19 therapeutic strategies [7, 55,56,57,58]. The development of international collaborations, adaptive and pragmatic designs, and the use of platform trials have enabled practice-changing trials such as the Randomised Evaluation of COVID-19 Therapy (RECOVERY) which enrolled over 10,000 patients in 176 hospitals within three months [59]. In addition, the World Health Organization and international intensive care societies have been extremely efficient in incorporating this growing body of evidence into guidelines, for the benefit of the whole community, both researchers and civil society [60].
Yet, this era was also marked by a massive scientific production, with sometimes low standards and several design pitfalls that generally lead to inconclusive or futile results, e.g., insufficient power to prove working hypotheses, flexible endpoints subject to assessment bias in open-label studies, lack of appropriate comparators, non-randomized allocation of treatments, duplication or fragmentation of data, and retrospective analyses of observational data. This is how the use of treatments such as hydroxychloroquine was promoted, whereas it has ultimately been proved to be detrimental in high-quality clinical trials [61] (Table 1). This should be a strong reminder that all treatments should be tested in methodologically rigorous trials prior to their implementation in clinical practice, even in case of strong biological plausibility and presumed safety [62]. The scientific community, as well as civil society and politicians, have become aware of this methodological disparity and the hazardous conclusions, leading to distrust of the medical profession, which we experienced during the vaccination campaigns. Methodological education in response to the quality of COVID-19 publications has been published [63]. Rushing is not good for scientific rigor and in this sense, indeed, fast-track procedures have been abandoned.
Lastly, research on COVID-19 has affected the production of non-COVID-19 research. This phenomenon, criticized by many key opinion leaders, may be due to a redirection of funding allocations, shifts in editorial strategies and limited access to patients during containment periods [64, 65].
Intensive care clinical research will surely benefit from these advances. National intensive care registries would become systematic, promoting large-scale adaptive studies worldwide [63, 66, 67]. The rigorousness of methodological requirements combined with improved clinical research coordination would curb the risk of duplication and underpowered studies while providing a faster, simplified process of ethics approval. International research collaborations would benefit from harmonized institutional review board procedures [68] (Table 3). A transparent editorial and an open-access review process would contribute to effective knowledge sharing which would be incorporated into real-time international guidelines.
Global improvement of critically ill patient outcome
The abundant research has led to conclusive evidence to improve patient outcome in an extremely short period of time [69]. In patients requiring ICU admission, dexamethasone [59, 70], IL-6 receptor antagonists [71] and neutralizing antibodies for Delta and Omicron variants [72,73,74] have shown a significant beneficial impact. The heterogeneity in critically ill COVID-19 patients’ response to corticosteroids and the disappointing results of other therapeutic interventions underscore the importance of the timing of treatment onset with respect to the disease course of inflammatory response and lung injury [75].
Another improvement during the pandemic was the shift in therapeutic strategy from a one-size-fits-all approach to more targeted interventions in subpopulations such as patients with high prevalence of underlying immune effect [76], B-cell lymphoid malignancies [77] or seronegative patients [74] illustrating the necessary evolution of intensive care towards personalized and precision medicine [78]. Post-COVID-19 critical care strategy will integrate disease time-course, clinical phenotypes, omics tools and new biomarkers in order to rapidly detect treatment responders and avoid immunomodulatory side effects in others.
In parallel, outcomes of critically ill patients have mostly been improved by refinement of non-specific supportive care strategies such as high-flow nasal cannula oxygen and non-invasive ventilation [79,80,81,82,83], awake prone-positioning [84, 85], all of which were not as widely used for the treatment of acute respiratory failure due to non-COVID-19 pneumonia. Non-COVID-19 patients will benefit from these therapeutic breakthroughs, as this progress in non-specific supportive interventions is most likely to be broadly applicable to patients with non-COVID-19 acute respiratory distress syndrome (ARDS).
Innovative communication with patients and families
The first waves of the pandemic, marked by lockdowns, social distancing measures, visit restrictions and even bans, undermined “patient- and family-centered care”. The restrictions led to extreme seclusion situations for ICU patients, although it is proven that a flexible family visitation policy is associated with a better patient experience of the ICU stay and a potential reduction of delirium and anxiety symptoms [86,87,88]. These restrictions also negatively impacted patients’ relatives due to limited access to medical teams and subsequent limited information [89, 90]. Here again, healthcare professionals showed unprecedented adaptability, making use of new multimedia communication tools with video-calls and virtual visits [91] as well as writing and drawing in daily diaries [87] (Tables 1, 3). Moreover, hindsight in the aftermath of the pandemic and the effectiveness of vaccination campaigns and social distancing measures have allowed for a gradual lifting of visiting restrictions for relatives to complete reopening, notably for dying patients. This should remind us that face-to-face communication remains the gold standard for all.
The negative experience of visiting policy restrictions during the pandemic period clearly supports the adoption of a flexible opening policy, ideally not less than 12 h per day. Moreover, the production of structured effective communication guidelines [87, 92, 93] associated with new possibilities offered by multimedia tools to maintain connections between patients and relatives, and between families and medical staff, will undoubtedly change the future of critical care communication strategies, always prioritizing patient and family comfort, well-being and quality of life [94].
Facing ethical dilemmas: from individual to collective choices
Early on, the pandemic highlighted some key ethical issues regarding life support withdrawal decisions, quality of end-of-life support and above all admission strategies (i.e., triage) [95,96,97] (Table 1). These issues were particularly related to the extreme strain on ICU beds, given that delayed ICU admission due to a full unit is associated with increased mortality [98].
Good practice regarding patient admission recommends a patient-centered collective shared-decision process involving the referring physicians and taking into account the patient’s premorbid conditions, frailty and anticipated prognosis of the acute illness as well as their wishes concerning their quality of life and the degree of disability they are willing to accept [7, 99] (Table 3). The overall goal of this multifactorial approach is to propose a tailored, personalized "treatment plan", which can be re-evaluated during the ICU stay according to the patient’s progression, thereby allowing for transparent communication with the patient and his family regarding the goals of care.
However, it should be acknowledged that these good practices have not always been followed with disparities between centers and countries. It has been suggested that the high between-center heterogeneity of patient trajectories and outcomes may be at least partially due to a wide disparity in triage criteria [100], including age [96, 101]. It should be pointed out that the personalized benefit/risk balance of triage decisions in an unprecedented situation with a lack of evidence regarding disease progression, prognostic factors, and potential sequelae is a difficult matter, and that simple severity scores developed outside COVID have been shown to be inaccurate [102]. Although it is desirable to develop more accurate and earlier prognostic tools based on patient-reported outcome measures, it is misleading to believe that a single criterion and/or score could ever supplant the complex decision-making process guiding ICU admission. As there is no universal consensus on some of the basic principles that should prevail [103], we should rather acknowledge this complexity and promote distributive justice, postulating fairness and equity in the allocation of resources, accounting for potential socioeconomic and demographic inequities [104, 105], especially in case of ICU bed shortages [106, 107]. It has been proposed that critical care teams responsible for patient care should be relieved of the responsibility for admission or non-admission decisions. The decisions must be informed by objective elements that can change over time, taking into account the opinion of the patient (or, failing that, the family) throughout the course of treatment. This work would thus be performed by a dedicated triage team [108, 109]. The advantage of this approach is that it avoids the emotional impact of choosing whether or not to admit a patient to an ICU [110]. However, the composition of these teams must be specified to avoid hurting and/or guilt for the health care team [107, 111].
All these debates, which were not restricted to caregivers, revealed the complexity of emergency ethical decisions to the general population and political stakeholders, and they should ultimately be beneficial in improving our daily ethical practices beyond the COVID-19 pandemic. But most importantly, the general population must be encouraged to participate in the discussion, firstly through national communication campaigns, and also through anticipated decisions with the family and the referring team (Table 3). Indeed, each patient followed for a chronic disease at risk of worsening and each hospitalized inpatient should be informed and encouraged to express his/her wishes regarding the goals of care via advance directives (Table 3). Patients’ wishes should be written in the patient’s medical record, accessible to all practitioners and communicated to all physicians in charge of the patient. The shared-decision process should be implemented during regular multidisciplinary meetings and updated throughout the time course of the disease. Moreover, in each structure, a dedicated team of independent experts from various fields as well as non-experts from the civil society should be available as recourse for difficult cases. Lastly, ethics education should be reinforced by specialized courses in continuing medical education, by participation in ethics boards of critical care societies, and in debate sessions during national and international symposiums.
Post-intensive care syndrome awareness
Prior to the pandemic, a growing body of evidence had already been accumulated regarding potential persistent disabilities in ICU survivors, notably after sepsis and ARDS [112,113,114,115,116,117,118], pooled together under the concept of ‘Post-Intensive Care Syndrome’ (PICS) [119,120,121] (Table 1). These sequelae range from physical disabilities such as gait disorders and fatigue due to ICU-acquired weakness and/or persistent organ dysfunction such as kidney, cardiac or respiratory failure, to psychiatric and cognitive disorders, all impairing the quality of life of ICU survivors. Their pathophysiology remains poorly understood, but intensity of the initial episode with persistent inflammatory and metabolic alterations are thought to be important mechanisms [122]. PICS is observed in approximately half of ICU survivors [123], and prior to the pandemic, considerable efforts had been made to improve PICS recognition and management [124]. However, despite multi-organ involvement of PICS and a myriad of negative consequences for patients, increasing PICS awareness was mostly limited to critical care and rehabilitation communities. With thousands of ICU survivors discharged from hospital after severe COVID across countries after the first waves, this question became relevant to all [125].
Thus, recent reports have shown that incidence of PICS following severe COVID-19 is particularly high [126,127,128], with clinical features similar to non-COVID acute respiratory failure requiring invasive mechanical ventilation [129]. Patients with COVID-19 ARDS have been shown to require more sedation (propofol and benzodiazepine) than non-COVID-19 patients to achieve the same median levels of sedation [130, 131]. In this context, early mobilization of mechanically ventilated patients, daily discontinuation and/or nurse-protocolized targeted sedation, management of physical and psychological discomfort and avoidance of prodelirious drugs are crucial points in ICU patient rehabilitation [132]. Despite growing recognition, PICS management is likely to be insufficient after ICU discharge due to the lack of specific structures and data regarding how post-ICU follow-up should be organized [119, 124]. Though data from the pandemic have not yielded definitive answers for these critical questions, increased global PICS awareness will help us to communicate not only with patients and their relatives regarding PICS, but also with other care providers that might be involved in the management. At the end, the high prevalence and poor functional prognosis associated with COVID-19 highlight the urgent need for reorganization of post-ICU care, including respiratory and neurological rehabilitation with a multidisciplinary approach involving intensivists, rehabilitation physicians, physiotherapists, psychologists, organ subspecialists and general practitioners (Table 3).
Massive material and human investments in intensive care
The fight against COVID-19 was marked at the onset by an unparalleled mobilization—both in terms of scale and speed—of human, material and financial resources (Table 1). Countries spent trillions of dollars to support the economic cost of containment measures but also to purchase personal protective equipment, ICU devices such as ventilators, consumables and pharmaceuticals [133, 134]. Facing major logistical constraints (shortages of medical devices, personal protective equipment and drugs, inadequate gas supply) and human challenges [135, 136], the extraordinary mobilization and joint efforts of medical, paramedical and administrative staff allowed to cope with the massive influx of patients. This mobilization helped to support enhanced ICU bed capacity while trying to maintain safe nurse/patient ratios and intensivist/patients ratios [137,138,139]. The youngest largely contributed to this effort with great flexibility and adaptability. Indeed, many trainees engaged in a research year interrupted their doctorate or master's degree to help at the bedside and students from nursing schools were sent into the field in a great participatory impulse.
Despite these efforts, many ICU departments faced major shortages of human resources and medical devices, jeopardizing both patients’ and healthcare workers’ safety [140]. Moreover, the response of healthcare systems to the COVID-19 pandemic was hampered by a lack of public policy coordination both at national and international levels, deficient cooperation between governments and industry [5, 141] and the lack of international solidarity. It is now our responsibility to capitalize on this acknowledgment so as to remind the policy makers and civil society how important it is to build resilient and effective critical care that will need to outlast the current pandemic [142]. The public financial concessions achieved so far will not be enough.
Efforts should also be made to align research funding in critical care to the financial burden of critical illnesses [143]. But above all, if we want to be able to provide high-quality care in the future, focus should be on the investment in human resources, to increase the safety of patients, the well-being of caregivers and the overall attractiveness of critical care.
Caring for caregivers is a health priority
Awareness of the paramount importance of healthcare workers’ well-being has taken on a very new scope with this health crisis [144, 145] (Table 1). Working conditions during the pandemic were negatively impacted by many factors, notably a heavier workload (high number of patients, organizational changes with an increase in ICU beds usually not matched by an adequate increase in staffing resources) and a high emotional burden (high, persistent levels of stress due to the uncertainty about the evolution of the pandemic, shortage of personal protective equipment, difficult ethical triage decisions, fear of being sick and of transmitting the virus to relatives) [144,145,146,147,148,149,150]. The 2020 National Physician Burnout and Suicide Report showed a 44% rate of burnout among ICU physicians [151]. The COVID-19 pandemic has increased this rate not only due to dying patients [152] but also to additional physical and psychological demands with a poor recognition of their work [153, 154]. We are at a watershed moment for caregivers and proffering “resilience” as the solution to the burn-out crisis is no longer acceptable [155].
To improve healthcare professionals’ ICU experience, policy makers should provide a more motivating, positive work environment to foster emotional well-being and empathy [156, 157] through multiscale interventions [158]. Notably, fostering communication among the team and with external consultants (dedicated training in communication and conflict resolution, multidisciplinary rounds [159]) and giving access to well-being programs [148, 160, 161] should be promoted to mitigate burn-out symptoms. But, more importantly, increasing staffing resources appears to be a prerequisite to prevent work-related stress [148]. It is indeed a priority to train and recruit physicians, nurses, nursing auxiliaries, psychologists, physical therapists and secretaries to allow for part-time work with flexible schedules [162], to reduce the burden of administrative tasks, to foster teamwork and the strengthened nurse–physician pairing, and to encourage communication and open dialogue concerning mental health issues. Emphasis should now be put on matching healthcare workers' cognitive assessment of the perceived demands with their perceived capability, skills and resources to deal with those demands [144, 146, 148].
The involvement of all stakeholders will be needed to guarantee a better understanding of caregivers’ expectations, which will be the main concern for the next generation of ICU healthcare professionals and an absolute necessity for critical care to remain attractive (Table 3). It is definitely time to care for caregivers.
The challenge of intensive care attractiveness
As previously discussed, the omnipresence of the pandemic in everyday life with its associated coverage in the media shed light on our specialty, hitherto unknown to the public. The community became aware not only of our highly technical environment and the very specific skills it requires, but also of our genuine dedication to patients and their families, especially the dedication of the youngest physicians, who have little media exposure but were at the bedside. Society became aware of our resilience [136] (Table 1). Yet, after a brief period of recognition and applause by the general population, and government promises of improved working conditions, we must acknowledge that ICU attractiveness has not improved and may even have deteriorated. The pandemic has exposed and aggravated the long-lasting hospital crisis, hence accelerating the massive departure of physicians, nurses and nurse assistants from the ICU and from public hospitals to private structures, or even engaging in professional retraining due to perceived loss of meaning [163, 164].
Nevertheless, we remain hopeful that the pandemic and this spotlight on our specialty will help to attract young healthcare workers interested in complex pathophysiological concepts and in patients with multiple organ failure, who wish to provide state-of-the-art multidisciplinary care combining advanced techniques while being constantly concerned by the ethics of care. The two main levers to achieve this are firstly a substantial increase of nurses and nurses assistants’ wages and secondly a better recognition of the specific skills of critical physicians, nurses and caregivers, opening opportunities for career development. This recognition will require the development of dedicated diploma (such as the recent advanced nurses practitioners status) and training programs for all caregivers [165, 166] (such as European Society of Intensive Care Medicine and Société de Réanimation de Langue Française training programs).
In the end, we believe that recognition of the specific challenges of intensive care medicine by society, political leaders and other medical specialties, will promote the attractiveness of critical care medicine [136]. It is time for our critical care community to take advantage of this publicity to nurture vocations and foster the emergence of young critical care leaders. We invite you to participate in on our optimism and join our group of motivated young intensivist (icufrenchfoxesstudygroup@gmail.com).
Conclusion
The unprecedented COVID-19 pandemic has upset the convictions and beliefs of all: caregivers, politicians and society alike. From the initial diagnosis of severe SARS-CoV-2 infection to the management of organ failure in the ICU to hospital discharge, the intensive care medicine community assumed a major role in the care pathway of patients. This central place has highlighted three essential points: the difficulty for intensivists to decide whether or not to admit a patient in ICU despite regular use of pre-existing ethics committees, the now well described long-term consequences of critical care, and the importance of communication between caregivers, families and patients. Although these essential points had previously been acknowledged, the COVID-19 pandemic shed a new light on them. Critical care also took an essential place in the healthcare system thanks to its adaptability, the human investment, and the rapid research response to improve patient outcome. Pursuing these efforts, notably through the promotion of facilities and funding for further research will be warranted to maintain and strengthen these impressive achievements. Finally, intensive care became the focus of attention of the whole society. The caregivers’ resilience in such difficult and uncertain conditions were exposed in the media and social network, raising awareness of their dedication and priority to foster well-being at work in the midst of growing indifference as the pandemic pressed on.
Notwithstanding this gloomy atmosphere, we, as young critical care caregivers, are determined to maintain a positive and optimistic outlook on intensive care and we are convinced we can capitalize on these achievements to build better critical care. We realize that this hard-won new recognition should not be taken for granted and that it will have to be defended tooth and nail. This is thus a momentum for our specialty. Now is the time for us to actively engage to convert the lessons learnt from these unprecedented challenges into transformative changes. All colleagues are welcome to join in on our optimism.
Availability of data and materials
Not applicable.
Abbreviations
- ARDS:
-
Acute respiratory distress syndrome
- COVID-19:
-
Coronavirus disease 2019
- ICU:
-
Intensive care unit
- PICS:
-
Post-intensive care syndrome
References
WHO Coronavirus (COVID-19) Dashboard. Disponible. https://covid19.who.int.
Jha P, Deshmukh Y, Tumbe C, Suraweera W, Bhowmick A, Sharma S, et al. COVID mortality in India: national survey data and health facility deaths. Science. 2022;375(6581):667–71.
Ritchie H, Mathieu E, Rodés-Guirao L, Appel C, Giattino C, Ortiz-Ospina E, et al. Coronavirus Pandemic (COVID-19). Our World Data. 2020. https://ourworldindata.org/coronavirus.
Data on hospital and ICU admission rates and current occupancy for COVID-19. European centre for disease prevention and control. 2022. https://www.ecdc.europa.eu/en/publications-data/download-data-hospital-and-icu-admission-rates-and-current-occupancy-covid-19.
Arabi YM, Azoulay E, Al-Dorzi HM, Phua J, Salluh J, Binnie A, et al. How the COVID-19 pandemic will change the future of critical care. Intensive Care Med mars. 2021;47(3):282–91.
Kandel N, Chungong S, Omaar A, Xing J. Health security capacities in the context of COVID-19 outbreak: an analysis of international health regulations annual report data from 182 countries. Lancet Lond Engl. 2020;395(10229):1047–53.
COVID-ICU Group on behalf of the REVA Network and the COVID-ICU Investigators. Clinical characteristics and day-90 outcomes of 4244 critically ill adults with COVID-19: a prospective cohort study. Intensive Care Med. 2021;47(1):60–73.
Verdonk F, Zacharowski K, Ahmed A, Orliaguet G, Pottecher J. A multifaceted approach to intensive care unit capacity. Lancet Public Health. 2021;6(7): e448.
Taccone FS, Goethem NV, Pauw DE, R, VAN Beckhoven D, Meyfroidt G, Blot K. Organizational characteristics: effect on outcome of ICU COVID-19 patients in Belgium—authors’ reply. Lancet Reg Health Eur avr. 2021;3: 100070.
Bauer J, Brüggmann D, Klingelhöfer D, Maier W, Schwettmann L, Weiss DJ, et al. Access to intensive care in 14 European countries: a spatial analysis of intensive care need and capacity in the light of COVID-19. Intensive Care Med. 2020;46(11):2026–34.
Squara P. The Ockham’s razor for estimating the needs of ICU beds during a pandemic. Ann Intensive Care. 2021;11(1):94.
Grasselli G, Pesenti A, Cecconi M. Critical care utilization for the COVID-19 outbreak in lombardy, italy: early experience and forecast during an emergency response. JAMA. 2020;323(16):1545–6.
Fagiuoli S, Lorini FL, Remuzzi G, Covid-19 Bergamo Hospital Crisis Unit. Adaptations and lessons in the province of Bergamo. N Engl J Med. 2020;382(21):e71.
Lefrant JY, Fischer MO, Potier H, Degryse C, Jaber S, Muller L, et al. A national healthcare response to intensive care bed requirements during the COVID-19 outbreak in France. Anaesth Crit Care Pain Med déc. 2020;39(6):709–15.
Peters AW, Chawla KS, Turnbull ZA. Transforming ORs into ICUs. N Engl J Med. 2020;382(19):e52.
Painvin B, Messet H, Rodriguez M, Lebouvier T, Chatellier D, Soulat L, et al. Inter-hospital transport of critically ill patients to manage the intensive care unit surge during the COVID-19 pandemic in France. Ann Intensive Care. 2021;11(1):54.
Sanchez MA, Vuagnat A, Grimaud O, Leray E, Philippe JM, Lescure FX, et al. Impact of ICU transfers on the mortality rate of patients with COVID-19: insights from comprehensive national database in France. Ann Intensive Care. 2021;11(1):151.
Chen E, Longcoy J, McGowan SK, Lange-Maia BS, Avery EF, Lynch EB, et al. Interhospital transfer outcomes for critically ill patients with coronavirus disease 2019 requiring mechanical ventilation. Crit Care Explor. 2021;3(10): e0559.
Rimmelé T, Pascal L, Polazzi S, Duclos A. Organizational aspects of care associated with mortality in critically ill COVID-19 patients. Intensive Care Med janv. 2021;47(1):119–21.
Greco M, De Corte T, Ercole A, Antonelli M, Azoulay E, Citerio G, et al. Clinical and organizational factors associated with mortality during the peak of first COVID-19 wave: the global UNITE-COVID study. Intensive Care Med juin. 2022;48(6):690–705.
Soares M, Bozza FA, Angus DC, Japiassú AM, Viana WN, Costa R, et al. Organizational characteristics, outcomes, and resource use in 78 Brazilian intensive care units: the ORCHESTRA study. Intensive Care Med déc. 2015;41(12):2149–60.
Guillon A, Laurent E, Duclos A, Godillon L, Dequin PF, Agrinier N, et al. Case fatality inequalities of critically ill COVID-19 patients according to patient-, hospital- and region-related factors: a French nationwide study. Ann Intensive Care. 2021;11(1):127.
Zampieri FG, Bastos LSL, Soares M, Salluh JI, Bozza FA. The association of the COVID-19 pandemic and short-term outcomes of non-COVID-19 critically ill patients: an observational cohort study in Brazilian ICUs. Intensive Care Med déc. 2021;47(12):1440–9.
Kim S, Choi H, Sim JK, Jung WJ, Lee YS, Kim JH. Comparison of clinical characteristics and hospital mortality in critically ill patients without COVID-19 before and during the COVID-19 pandemic: a multicenter, retrospective, propensity score-matched study. Ann Intensive Care. 2022;12(1):57.
Einstein AJ, Shaw LJ, Hirschfeld C, Williams MC, Villines TC, Better N, et al. International impact of COVID-19 on the diagnosis of heart disease. J Am Coll Cardiol. 2021;77(2):173–85.
Wadhera RK, Shen C, Gondi S, Chen S, Kazi DS, Yeh RW. Cardiovascular deaths during the COVID-19 Pandemic in the United States. J Am Coll Cardiol. 2021;77(2):159–69.
Riera R, Bagattini ÂM, Pacheco RL, Pachito DV, Roitberg F, Ilbawi A. Delays and disruptions in cancer health care due to covid-19 pandemic: systematic review. JCO Glob Oncol févr. 2021;7:311–23.
Santi L, Golinelli D, Tampieri A, Farina G, Greco M, Rosa S, et al. Non-COVID-19 patients in times of pandemic: emergency department visits, hospitalizations and cause-specific mortality in Northern Italy. PLoS ONE. 2021;16(3): e0248995.
Teoh SE, Masuda Y, Tan DJH, Liu N, Morrison LJ, Ong MEH, et al. Impact of the COVID-19 pandemic on the epidemiology of out-of-hospital cardiac arrest: a systematic review and meta-analysis. Ann Intensive Care. 2021;11(1):169.
Cushman JG, Pachter HL, Beaton HL. Two New York City hospitals’ surgical response to the september 11 2001 terrorist attack in New York City. J Trauma. 2003;54(1):147–54.
Hirsch M, Carli P, Nizard R, Riou B, Baroudjian B, Baubet T, et al. The medical response to multisite terrorist attacks in Paris. Lancet Lond Engl. 2015;386(10012):2535–8.
Carli P, Pons F, Levraut J, Millet B, Tourtier JP, Ludes B, et al. The French emergency medical services after the Paris and nice terrorist attacks: what have we learnt? Lancet Lond Engl. 2017;390(10113):2735–8.
Misset B, De Jonghe B, Bastuji-Garin S, Gattolliat O, Boughrara E, Annane D, et al. Mortality of patients with heatstroke admitted to intensive care units during the 2003 heat wave in France: a national multiple-center risk-factor study. Crit Care Med avr. 2006;34(4):1087–92.
Kaiser R, Le Tertre A, Schwartz J, Gotway CA, Daley WR, Rubin CH. The effect of the 1995 heat wave in Chicago on all-cause and cause-specific mortality. Am J Public Health avr. 2007;97(Suppl 1):S158-162.
Lefrant JY, Pirracchio R, Benhamou D, Dureuil B, Pottecher J, Samain E, et al. ICU bed capacity during COVID-19 pandemic in France: from ephemeral beds to continuous and permanent adaptation. Anaesth Crit Care Pain Med juin. 2021;40(3): 100873.
Litton E, Huckson S, Chavan S, Bucci T, Holley A, Everest E, et al. 2021 Increasing ICU capacity to accommodate higher demand during the COVID-19 pandemic. Med J Aust. 2021;215(11):513–7.
Le répertoire national de l’offre de santé et d’accompagnement médicosocial—ROR —Ministère de la Santé et de la Prévention. https://solidarites-sante.gouv.fr/systeme-de-sante-et-medico-social/e-sante/sih/article/le-repertoire-national-de-l-offre-de-sante-et-d-accompagnement-medicosocial-ror.
Le Répertoire ROR. https://esante.gouv.fr/produits-services/repertoire-ror.
Terrasi B, Arnaud E, Abou-Arab O, Bessserve P, Mahjoub Y. Les réanimations françaises se mobilisent : un exemple d’organisation régionale contre l’épidémie de COVID-19. Anesth Réanimation mai. 2020;6(3):350–2.
ICUBAM GitHub. https://github.com/icubam.
ANZIC Influenza Investigators, Webb SAR, Pettilä V, Seppelt I, Bellomo R, Bailey M, et al. Critical care services and 2009 H1N1 influenza in Australia and New Zealand. N Engl J Med. 2009;361(20):1925–34.
Al-Dorzi HM, Aldawood AS, Khan R, Baharoon S, Alchin JD, Matroud AA, et al. The critical care response to a hospital outbreak of middle east respiratory syndrome coronavirus (MERS-CoV) infection: an observational study. Ann Intensive Care déc. 2016;6(1):101.
Rasmussen SA, Jamieson DJ. Public health decision making during Covid-19—fulfilling the CDC pledge to the American people. N Engl J Med. 2020;383(10):901–3.
Rajan D, Koch K, Rohrer K, Bajnoczki C, Socha A, Voss M, et al. Governance of the covid-19 response: a call for more inclusive and transparent decision-making. BMJ Glob Health mai. 2020;5(5): e002655.
L’appel des médecins réanimateurs à Olivier Véran pour sortir enfin de la saturation permanente https://www.lefigaro.fr/vox/societe/l-appel-des-medecins-reanimateurs-a-olivier-veran-pour-sortir-enfin-de-la-saturation-permanente-20211231.
EXCLUSIF. L’alerte de 41 directeurs de crise de l’AP-HP : « Nous serons contraints de faire un tri des patients » https://www.lejdd.fr/Societe/exclusif-lalerte-de-41-medecins-face-a-la-crise-nous-serons-contraints-de-faire-un-tri-des-patients-4034448.
Covid-19 : une centaine de spécialistes réclament d’augmenter «le recrutement des médecins» en reanimation—Le Parisien. https://www.leparisien.fr/societe/sante/covid-19-une-centaine-de-specialistes-reclament-daugmenter-le-recrutement-des-medecins-en-reanimation-31-12-2021-DYH75GQA7FGU7PBRB3C5KIMWIE.php.
Cinelli M, Quattrociocchi W, Galeazzi A, Valensise CM, Brugnoli E, Schmidt AL, et al. The COVID-19 social media infodemic. Sci Rep. 2020;10:16598.
Horton R. Offline: science and the breakdown of trust. Lancet Lond Engl. 2020;396(10256):945.
« Les décideurs publics français, éloignés du monde de la recherche, accordent peu de valeur à la démarche scientifique ». Le Monde.fr. 2022 https://www.lemonde.fr/idees/article/2022/01/19/les-decideurs-publics-francais-eloignes-du-monde-de-la-recherche-accordent-peu-de-valeur-a-la-demarche-scientifique_6110060_3232.html.
Media and Medicine Certificate Program. https://ghsm.hms.harvard.edu/education/media-and-medicine-certificate-program.
Salluh JIF, Arabi YM, Binnie A. COVID-19 research in critical care: the good, the bad, and the ugly. Intensive Care Med avr. 2021;47(4):470–2.
Citerio G, The ICM Editorial Board. And once the storm is over ICM will remain the intensivist’s beacon. Intensive Care Med. 2021;47(6):687–91.
Martinez-Simon A, Honorato-Cia C, Cacho-Asenjo E, Aquerreta I, Panadero-Sanchez A, Núñez-Córdoba JM. COVID-19 publications in anaesthesiology journals: a bibliometric analysis. Br J Anaesth. 2021. https://doi.org/10.1016/j.bja.2021.12.003.
COVID-ICU group, for the REVA network, COVID-ICU investigators. Benefits and risks of noninvasive oxygenation strategy in COVID-19: a multicenter, prospective cohort study (COVID-ICU) in 137 hospitals. Crit Care Lond Engl. 2021;25(1):421.
Schmidt M, Guidet B, Demoule A, Ponnaiah M, Fartoukh M, Puybasset L, et al. Predicting 90-day survival of patients with COVID-19: survival of severely Ill COVID (SOSIC) scores. Ann Intensive Care. 2021;11(1):170.
Barbaro RP, MacLaren G, Boonstra PS, Iwashyna TJ, Slutsky AS, Fan E, et al. Extracorporeal membrane oxygenation support in COVID-19: an international cohort study of the extracorporeal life support organization registry. Lancet Lond Engl. 2020;396(10257):1071–8.
Hendren NS, de Lemos JA, Ayers C, Das SR, Rao A, Carter S, et al. Association of body mass index and age with morbidity and mortality in patients hospitalized with COVID-19: results from the american heart association covid-19 cardiovascular disease registry. Circulation. 2021;143(2):135–44.
RECOVERY Collaborative Group, Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, et al. Dexamethasone in hospitalized patients with covid-19. N Engl J Med. 2021;384(8):693–704.
Arrizabalaga O, Otaegui D, Vergara I, Arrizabalaga J, Méndez E. Open Access of COVID-19-related publications in the first quarter of a preliminary study based in PubMed. Research. 2020. https://doi.org/10.12688/f1000research.24136.1.
RECOVERY Collaborative Group, Horby P, Mafham M, Linsell L, Bell JL, Staplin N, et al. Effect of hydroxychloroquine in hospitalized patients with covid-19. N Engl J Med. 2020;383(21):2030–40.
Young PJ, Lamontagne F. VitaminC in sepsis. Intensive Care Med. 2022. https://doi.org/10.1007/s00134-022-06822-x.
Andreotti F, Gervasoni C, Di Pasquale G, Maggioni AP. Methodological education in response to the quality of COVID-19 publications. Pharmacol Res févr. 2021;164: 105381.
Raynaud M, Goutaudier V, Louis K, Al-Awadhi S, Dubourg Q, Truchot A, et al. Impact of the COVID-19 pandemic on publication dynamics and non-COVID-19 research production. BMC Med Res Methodol. 2021;21(1):255.
Tuttle KR. Impact of the COVID-19 pandemic on clinical research. Nat Rev Nephrol. 2020;16(10):562–4.
Collins R, Bowman L, Landray M, Peto R. The magic of randomization versus the myth of real-world evidence. N Engl J Med. 2020;382(7):674–8.
Maggioni AP, Andreotti F, Gervasoni C, Pasquale GD. COVID-19 trials in Italy a call for simplicity top standards and global pooling. Int J Cardiol. 2020. https://doi.org/10.1016/j.ijcard.2020.06.043.
Timmers M, van Dijck JTJM, van Wijk RPJ, Legrand V, van Veen E, Maas AIR, et al. How do 66 European institutional review boards approve one protocol for an international prospective observational study on traumatic brain injury? Experiences from the CENTER-TBI study. BMC Med Ethics. 2020;21(1):36.
Dongelmans DA, Termorshuizen F, Brinkman S, Bakhshi-Raiez F, Arbous MS, de Lange DW, et al. Characteristics and outcome of COVID-19 patients admitted to the ICU: a nationwide cohort study on the comparison between the first and the consecutive upsurges of the second wave of the COVID-19 pandemic in the Netherlands. Ann Intensive Care. 2022;12(1):5.
Raymond M, Le Thuaut A, Asfar P, Darreau C, Reizine F, Colin G, et al. Association of early dexamethasone therapy with mortality in critically Ill COVID-19 patients: a French multicenter study. Ann Intensive Care. 2022;12(1):102.
Investigators RC, Gordon AC, Mouncey PR, Al-Beidh F, Rowan KM, Nichol AD, et al. Interleukin-6 receptor antagonists in critically Ill patients with covid-19. N Engl J Med. 2021;384(16):1491–502.
Gottlieb RL, Nirula A, Chen P, Boscia J, Heller B, Morris J, et al. Effect of bamlanivimab as monotherapy or in combination with etesevimab on viral Load in patients with mild to moderate COVID-19. JAMA. 2021;325(7):632–44.
Dunne C, Lang E. WHO provides 2 conditional recommendations for casirivimab-imdevimab combination therapy in COVID-19. Ann Intern Med. 2022. https://doi.org/10.7326/J21-0009.
Weinreich DM, Sivapalasingam S, Norton T, Ali S, Gao H, Bhore R, et al. REGN-COV2, a neutralizing antibody cocktail, in outpatients with covid-19. N Engl J Med. 2021;384(3):238–51.
Wick KD, McAuley DF, Levitt JE, Beitler JR, Annane D, Riviello ED, et al. Promises and challenges of personalized medicine to guide ARDS therapy. Crit Care Lond Engl. 2021;25(1):404.
Saade A, Moratelli G, Dumas G, Mabrouki A, Tudesq JJ, Zafrani L, et al. Infectious events in patients with severe COVID-19: results of a cohort of patients with high prevalence of underlying immune defect. Ann Intensive Care. 2021;11(1):83.
Hueso T, Godron AS, Lanoy E, Pacanowski J, Levi LI, Gras E, et al. Convalescent plasma improves overall survival in patients with B cell lymphoid malignancy and a longitudinal cohort and propensity score analysis. Leukemia. 2022;136:2290.
Vincent JL. The coming era of precision medicine for intensive care. Crit Care Lond Engl. 2017. https://doi.org/10.1186/s13054-017-1910-z.
Demoule A, Vieillard Baron A, Darmon M, Beurton A, Géri G, Voiriot G, et al. High-flow nasal cannula in critically III patients with severe COVID-19. Am J Respir Crit Care Med. 2020;202(7):1039–42.
Raoof S, Nava S, Carpati C, Hill NS. High-flow, noninvasive ventilation and awake (nonintubation) proning in patients with coronavirus disease 2019 with respiratory failure. Chest. 2020;158(5):1992–2002.
Ospina-Tascón GA, Calderón-Tapia LE, García AF, Zarama V, Gómez-Álvarez F, Álvarez-Saa T, et al. Effect of high-flow oxygen therapy vs conventional oxygen therapy on invasive mechanical ventilation and clinical recovery in patients with severe COVID-19: a randomized clinical trial. JAMA. 2021;326(21):2161–71.
Perkins GD, Ji C, Connolly BA, Couper K, Lall R, Baillie JK, et al. Effect of noninvasive respiratory strategies on intubation or mortality among patients with acute hypoxemic respiratory failure and COVID-19: the recovery-RS randomized clinical trial. JAMA. 2022;327(6):546–58.
Li J, Fink JB, Ehrmann S. High-flow nasal cannula for COVID-19 patients: low risk of bio-aerosol dispersion. Eur Respir J mai. 2020;55(5):2000892.
Guérin C, Reignier J, Richard JC, Beuret P, Gacouin A, Boulain T, et al. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013;368(23):2159–68.
Ehrmann S, Li J, Ibarra-Estrada M, Perez Y, Pavlov I, McNicholas B, et al. Awake prone positioning for COVID-19 acute hypoxaemic respiratory failure: a randomised, controlled, multinational, open-label meta-trial. Lancet Respir Med déc. 2021;9(12):1387–95.
Piscitello GM, Fukushima CM, Saulitis AK, Tian KT, Hwang J, Gupta S, et al. Family meetings in the intensive care unit during the coronavirus disease 2019 pandemic. Am J Hosp Palliat Care mars. 2021;38(3):305–12.
Mistraletti G, Giannini A, Gristina G, Malacarne P, Mazzon D, Cerutti E, et al. Why and how to open intensive care units to family visits during the pandemic. Crit Care Lond Engl. 2021;25(1):191.
Nassar Junior AP, Besen BAMP, Robinson CC, Falavigna M, Teixeira C, Rosa RG. Flexible versus restrictive visiting policies in ICUs: a systematic review and meta-analysis. Crit Care Med juill. 2018;46(7):1175–80.
Chen C, Wittenberg E, Sullivan SS, Lorenz RA, Chang YP. The experiences of family members of ventilated COVID-19 patients in the intensive care unit: a qualitative study. Am J Hosp Palliat Care. 2021;38(7):869–76.
Kentish-Barnes N, Cohen-Solal Z, Morin L, Souppart V, Pochard F, Azoulay E. Lived experiences of family members of patients with severe COVID-19 who died in intensive care units in France. JAMA Netw Open. 2021. https://doi.org/10.1001/jamanetworkopen.2021.13355.
Rose L, Cook A, Onwumere J, Terblanche E, Pattison N, Metaxa V, et al. Psychological distress and morbidity of family members experiencing virtual visiting in intensive care during COVID-19 an observational cohort study. Intensive Care Med. 2022. https://doi.org/10.1007/s00134-022-06824-9.
Mistraletti G, Gristina G, Mascarin S, Iacobone E, Giubbilo I, Bonfanti S, et al. How to communicate with families living in complete isolation. BMJ Support Palliat Care. 2020. https://doi.org/10.1136/bmjspcare-2020-002633.
Azoulay E, Kentish-Barnes N. A 5-point strategy for improved connection with relatives of critically ill patients with COVID-19. Lancet Respir Med juin. 2020;8(6): e52.
Kennedy NR, Steinberg A, Arnold RM, Doshi AA, White DB, DeLair W, et al. Perspectives on telephone and video communication in the intensive care unit during COVID-19. Ann Am Thorac Soc mai. 2021;18(5):838–47.
Depuydt P, Guidet B. Triage policy of severe Covid-19 patients: what to do now? Ann Intensive Care. 2021;11(1):18.
Dres M, Hajage D, Lebbah S, Kimmoun A, Pham T, Béduneau G, et al. Characteristics, management, and prognosis of elderly patients with COVID-19 admitted in the ICU during the first wave: insights from the COVID-ICU study : prognosis of COVID-19 elderly critically ill patients in the ICU. Ann Intensive Care. 2021;11(1):77.
Bruno RR, Wernly B, Flaatten H, Fjølner J, Artigas A, Baldia PH, et al. The association of the activities of daily living and the outcome of old intensive care patients suffering from COVID-19. Ann Intensive Care. 2022;12(1):26.
Robert R, Reignier J, Tournoux-Facon C, Boulain T, Lesieur O, Gissot V, et al. Refusal of intensive care unit admission due to a full unit: impact on mortality. Am J Respir Crit Care Med. 2012;185(10):1081–7.
van Veenendaal N, van der Meulen IC, Onrust M, Paans W, Dieperink W, van der Voort PHJ. Six-month outcomes in COVID-19 ICU patients and their family members: a prospective cohort study. Healthc Basel Switz. 2021;9(7):865.
Pitrowsky MT, Quintairos A, Salluh JIF. ICU organization and disparities in clinical trajectories and outcomes during the pandemic. Intensive Care Med. 2022;48(8):1120–1.
Guidet B, Jung C, Flaatten H, Fjølner J, Artigas A, Pinto BB, et al. Increased 30-day mortality in very old ICU patients with COVID-19 compared to patients with respiratory failure without COVID-19. Intensive Care Med avr. 2022;48(4):435–47.
Raschke RA, Agarwal S, Rangan P, Heise CW, Curry SC. Discriminant accuracy of the SOFA score for determining the probable mortality of patients with COVID-19 pneumonia requiring mechanical ventilation. JAMA. 2021;325(14):1469–70.
Vinay R, Baumann H, Biller-Andorno N. Ethics of ICU triage during COVID-19. Br Med Bull. 2021. https://doi.org/10.1093/bmb/ldab009.
Galiatsatos P, Kachalia A, Belcher HME, Hughes MT, Kahn J, Rushton CH, et al. xsHealth equity and distributive justice considerations in critical care resource allocation. Lancet Respir Med août. 2020;8(8):758–60.
Reid L. Triage of critical care resources in COVID-19: a stronger role for justice. J Med Ethics août. 2020;46(8):526–30.
Sprung CL, Geber D, Eidelman LA, Baras M, Pizov R, Nimrod A, et al. Evaluation of triage decisions for intensive care admission. Crit Care Med juin. 1999;27(6):1073–9.
Robert R, Kentish-Barnes N, Boyer A, Laurent A, Azoulay E, Reignier J. Ethical dilemmas due to the Covid-19 pandemic. Ann Intensive Care. 2020;10(1):84.
Daugherty Biddison EL, Faden R, Gwon HS, Mareiniss DP, Regenberg AC, Schoch-Spana M, et al. Too many patients a framework to guide statewide allocation of scarce mechanical ventilation during disasters. Chest avr. 2019;155(4):848–54.
Truog RD, Mitchell C, Daley GQ. The toughest triage—allocating ventilators in a pandemic. N Engl J Med. 2020;382(21):1973–5.
White DB, Lo B. A framework for rationing ventilators and critical care beds during the COVID-19 pandemic. JAMA. 2020;323(18):1773–4.
Laurent A, Bonnet M, Capellier G, Aslanian P, Hebert P. Emotional impact of end-of-life decisions on professional relationships in the icu: an obstacle to collegiality? Crit Care Med déc. 2017;45(12):2023–30.
Pandharipande PP, Girard TD, Jackson JC, Morandi A, Thompson JL, Pun BT, et al. Long-term cognitive impairment after critical illness. N Engl J Med. 2013;369(14):1306–16.
Iwashyna TJ, Ely EW, Smith DM, Langa KM. Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA. 2010;304(16):1787–94.
Herridge MS, Cheung AM, Tansey CM, Matte-Martyn A, Diaz-Granados N, Al-Saidi F, et al. One-year outcomes in survivors of the acute respiratory distress syndrome. N Engl J Med. 2003;348(8):683–93.
Herridge MS, Tansey CM, Matté A, Tomlinson G, Diaz-Granados N, Cooper A, et al. Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med. 2011;364(14):1293–304.
Carenzo L, Protti A, Dalla Corte F, Aceto R, Iapichino G, Milani A, et al. Short-term health-related quality of life, physical function and psychological consequences of severe COVID-19. Ann Intensive Care. 2021;11(1):91.
Demoule A, Morawiec E, Decavele M, Ohayon R, Malrin R, Galarza-Jimenez MA, et al. Health-related quality of life of COVID-19 two and 12 months after intensive care unit admission. Ann Intensive Care. 2022;12(1):16.
Li D, Liao X, Ma Z, Zhang L, Dong J, Zheng G, et al. Clinical status of patients 1 year after hospital discharge following recovery from COVID-19: a prospective cohort study. Ann Intensive Care. 2022;12(1):64.
Needham DM, Davidson J, Cohen H, Hopkins RO, Weinert C, Wunsch H, et al. Improving long-term outcomes after discharge from intensive care unit: report from a stakeholders’ conference. Crit Care Med févr. 2012;40(2):502–9.
Elliott D, Davidson JE, Harvey MA, Bemis-Dougherty A, Hopkins RO, Iwashyna TJ, et al. Exploring the scope of post-intensive care syndrome therapy and care: engagement of non-critical care providers and survivors in a second stakeholders meeting. Crit Care Med déc. 2014;42(12):2518–26.
Norman BC, Jackson JC, Graves JA, Girard TD, Pandharipande PP, Brummel NE, et al. Employment outcomes after critical illness: an analysis of the bringing to light the risk factors and incidence of neuropsychological dysfunction in icu survivors cohort. Crit Care Med. 2016;44(11):2003–9.
Voiriot G, Oualha M, Pierre A, Salmon-Gandonnière C, Gaudet A, Jouan Y, et al. Chronic critical illness and post-intensive care syndrome: from pathophysiology to clinical challenges. Ann Intensive Care. 2022;12(1):58.
Marra A, Pandharipande PP, Girard TD, Patel MB, Hughes CG, Jackson JC, et al. Co-occurrence of post-intensive care syndrome problems among 406 survivors of critical illness. Crit Care Med sept. 2018;46(9):1393–401.
Brown SM, Bose S, Banner-Goodspeed V, Beesley SJ, Dinglas VD, Hopkins RO, et al. Approaches to addressing post-intensive care syndrome among intensive care unit survivors a narrative review. Ann Am Thorac Soc. 2019;16(8):947–56.
Fink S. ‘It Takes Time’: I.C.U. Workers Help Their Former Covid Patients Mend. The New York Times. 2021 https://www.nytimes.com/2021/04/01/us/coronavirus-hospitals-recovery.html.
Writing Committee for the COMEBAC Study Group, Morin L, Savale L, Pham T, Colle R, Figueiredo S, et al. Four month clinical status of a cohort of patients after hospitalization for COVID-19. JAMA. 2021. https://doi.org/10.1001/jama.2021.3331.
Rousseau AF, Minguet P, Colson C, Kellens I, Chaabane S, Delanaye P, et al. Post-intensive care syndrome after a critical COVID-19: cohort study from a Belgian follow-up clinic. Ann Intensive Care. 2021;11(1):118.
Martillo MA, Dangayach NS, Tabacof L, Spielman LA, Dams-O’Connor K, Chan CC, et al. Postintensive care syndrome in survivors of critical illness related to coronavirus disease 2019: cohort study from a new york city critical care recovery clinic*. Crit Care Med. 2021;49(9):1427–38.
Hodgson CL, Higgins AM, Bailey MJ, Mather AM, Beach L, Bellomo R, et al. Comparison of 6-month outcomes of survivors of COVID-19 versus Non-COVID-19 critical illness. Am J Respir Crit Care Med. 2022;205(10):1159–68.
Tapaskar N, Colon Hidalgo D, Koo G, Shingada K, Rao S, Rodriguez R, et al. Sedation usage in COVID-19 acute respiratory distress syndrome: a multicenter study. Ann Pharmacother févr. 2022;56(2):117–23.
Flinspach AN, Booke H, Zacharowski K, Balaban Ü, Herrmann E, Adam EH. High sedation needs of critically ill COVID-19 ARDS patients-a monocentric observational study. PLoS ONE. 2021;16(7): e0253778.
Reade MC, Finfer S. Sedation and delirium in the intensive care unit. N Engl J Med. 2014;370(5):444–54.
Tan-Torres Edejer T, Hanssen O, Mirelman A, Verboom P, Lolong G, Watson OJ, et al. Projected health-care resource needs for an effective response to COVID-19 in 73 low-income and middle-income countries: a modelling study. Lancet Glob Health. 2020;8(11):e1372–9.
Fiscal Policies Database. IMF. https://www.imf.org/en/Topics/imf-and-covid19/Fiscal-Policies-Database-in-Response-to-COVID-19.
Xie J, Tong Z, Guan X, Du B, Qiu H, Slutsky AS. Critical care crisis and some recommendations during the COVID-19 epidemic in China. Intensive Care Med mai. 2020;46(5):837–40.
Wahlster S, Sharma M, Lewis AK, Patel PV, Hartog CS, Jannotta G, et al. The coronavirus disease 2019 pandemic’s effect on critical care resources and health-care providers: a global survey. Chest févr. 2021;159(2):619–33.
Jung M, Park H, Kang D, Park E, Jeon K, Chung CR, et al. The effect of bed-to-nurse ratio on hospital mortality of critically ill children on mechanical ventilation: a nationwide population-based study. Ann Intensive Care. 2020;10(1):159.
Needleman J, Buerhaus P, Pankratz VS, Leibson CL, Stevens SR, Harris M. Nurse staffing and inpatient hospital mortality. N Engl J Med. 2011;364(11):1037–45.
McHugh MD, Aiken LH, Sloane DM, Windsor C, Douglas C, Yates P. Effects of nurse-to-patient ratio legislation on nurse staffing and patient mortality, readmissions, and length of stay: a prospective study in a panel of hospitals. Lancet Lond Engl. 2021;397(10288):1905–13.
Tabah A, Ramanan M, Laupland KB, Buetti N, Cortegiani A, Mellinghoff J, et al. Personal protective equipment and intensive care unit healthcare worker safety in the COVID-19 era (PPE-SAFE): An international survey. J Crit Care. 2020;59:70–5.
Brownscombe JJ. Australian medical device regulation during COVID-19: has the Australian regulatory framework for medical devices been effective during the COVID-19 pandemic? J Law Med mars. 2021;28(3):745–59.
Salluh JIF, Kurtz P, Bastos LSL, Quintairos A, Zampieri FG, Bozza FA. The resilient intensive care unit. Ann Intensive Care. 2022;12(1):37.
Coopersmith CM, Wunsch H, Fink MP, Linde-Zwirble WT, Olsen KM, Sommers MS, et al. A comparison of critical care research funding and the financial burden of critical illness in the United States. Crit Care Med avr. 2012;40(4):1072–9.
Rotenstein LS, Sinsky C, Cassel CK. How to measure progress in addressing physician well-being: beyond burnout. JAMA. 2021;326(21):2129–30.
Wozniak H, Benzakour L, Moullec G, Buetti N, Nguyen A, Corbaz S, et al. Mental health outcomes of ICU and non-ICU healthcare workers during the COVID-19 outbreak: a cross-sectional study. Ann Intensive Care. 2021;11(1):106.
Shanafelt TD. Physician well-being 2.0: Where are we and where are we going? Mayo Clin Proc. 2021;96(10):2682–93.
Busch IM, Moretti F, Mazzi M, Wu AW, Rimondini M. What we have learned from two decades of epidemics and pandemics: a systematic review and meta-analysis of the psychological burden of frontline healthcare workers. Psychother Psychosom. 2021;90(3):178–90.
Khan A, Vinson AE. Physician well-being in practice. Anesth Analg. 2020;131(5):1359–69.
Kisely S, Warren N, McMahon L, Dalais C, Henry I, Siskind D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ. 2020. https://doi.org/10.1136/bmj.m1642.
Laurent A, Fournier A, Lheureux F, Louis G, Nseir S, Jacq G, et al. Mental health and stress among ICU healthcare professionals in France according to intensity of the COVID-19 epidemic. Ann Intensive Care. 2021;11(1):90.
Medscape National Physician Burnout and Suicide report. The generational divide. medscape. 2020. https://www.medscape.com/slideshow/2020-lifestyle-burnout-6012460.
Prokopová T, Hudec J, Vrbica K, Stašek J, Pokorná A, Štourač P, et al. Palliative care practice and moral distress during COVID-19 pandemic (PEOpLE-C19 study): a national, cross-sectional study in intensive care units in the Czech Republic. Crit Care Lond Engl. 2022;26(1):221.
Restauri N, Sheridan AD. Burnout and posttraumatic stress disorder in the coronavirus disease 2019 (COVID-19) pandemic: intersection, impact, and interventions. J Am Coll Radiol JACR. 2020;17(7):921–6.
Cole SP, Siddiqui S. Well-being in the intensive care unit: looking beyond COVID-19. Anesthesiol Clin juin. 2022;40(2):373–82.
Murthy VH. Confronting health worker burnout and well-being. N Engl J Med. 2022. https://doi.org/10.1056/NEJMp2207252.
Giordano F, Cipolla A, Ungar M. Building resilience for healthcare professionals working in an Italian red zone during the COVID-19 outbreak: a pilot study stress health. J Int Soc Investig Stress. 2022;38(2):234–48.
Cole SP, Siddiqui S. Well-being in the intensive care unit. Anesthesiol Clin juin. 2022;40(2):373–82.
Latour JM, Kentish-Barnes N, Jacques T, Wysocki M, Azoulay E, Metaxa V. Improving the intensive care experience from the perspectives of different stakeholders. Crit Care Lond Engl. 2022;26(1):218.
O’Brien A, O’Reilly K, Dechen T, Demosthenes N, Kelly V, Mackinson L, et al. Redesigning rounds in the ICU: standardizing key elements improves interdisciplinary communication. Jt Comm J Qual Patient Saf. 2018;44(10):590–8.
Clough BA, March S, Chan RJ, Casey LM, Phillips R, Ireland MJ. Psychosocial interventions for managing occupational stress and burnout among medical doctors: a systematic review. Syst Rev. 2017;6(1):144.
National Academies of Sciences, Engineering, and Medicine; National Academy of Medicine; Committee on Systems Approaches to Improve Patient Care by Supporting Clinician Well-Being. Taking action against clinician burnout: a systems approach to professional well-being. Washington: National Academies Press; 2019.
Geva A, Landrigan CP, van der Velden MG, Randolph AG. Simulation of a novel schedule for intensivist staffing to improve continuity of patient care and reduce physician burnout. Crit Care Med juill. 2017;45(7):1138–44.
De la pénurie de généralistes jusqu’aux urgences, le système de soins à l’hôpital est au bord de la noyade. https://www.lemonde.fr/societe/article/2022/07/13/crise-de-l-hopital-de-la-penurie-de-generalistes-jusqu-aux-urgences-un-systeme-de-soins-au-bord-de-la-noyade_6134576_3224.html.
AP-HP: « Les directions doivent courir après des soignants en désamour hospitalier ». https://www.lemonde.fr/idees/article/2022/03/12/ap-hp-les-directions-doivent-courir-apres-des-soignants-en-desamour-hospitalier_6117191_3232.html.
Master Classes. ESICM. https://www.esicm.org/education/courses-2/.
Formations | SRLF. https://www.srlf.org/formations.
Acknowledgements
We thank Professor Elie Azoulay (MD, PhD, Service de Médecine intensive Réanimation, Hôpital Saint-Louis, AP-HP, Paris, France), Professor Nadia Aissaoui (MD, PhD, Service de Médecine intensive Réanimation, Hôpital Cochin, AP-HP, Paris, France) and Professor Stephan Ehrmann (MD, PhD, Service de Médecine intensive Réanimation, CHRU de Tours, France). We thank Rama Levin and the French college of critical care scholars (Collège des Enseignants de Médecine Intensive Réanimation) for their help and careful english editing.
Funding
No funding.
Author information
Authors and Affiliations
Consortia
Contributions
BH, AL and AB wrote the review design. BH, SB, YJ, AL and AB wrote the main manuscript. SB and YJ prepared Fig. 1. All authors reviewed the manuscript. BH and AB approved the final version. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hermann, B., Benghanem, S., Jouan, Y. et al. The positive impact of COVID-19 on critical care: from unprecedented challenges to transformative changes, from the perspective of young intensivists. Ann. Intensive Care 13, 28 (2023). https://doi.org/10.1186/s13613-023-01118-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13613-023-01118-9