Abstract
Background
Malaria mixed infections are often unrecognized by microscopists in the hospitals, and a delay or failure to treat Plasmodium-mixed infection may lead to aggravated morbidity and increased mortality. The present study aimed to quantify the pooled proportion and risk of malarial recurrences after the treatment of Plasmodium-mixed infection. The results of the study may provide benefits in the management of Plasmodium-mixed infection in co-endemic regions.
Methods
This systematic review and meta-analysis searched the international Prospective Register of Systematic Reviews (PROSPERO; ID = CRD42020199709), MEDLINE, Web of Science, and Scopus for potentially relevant studies in any language published between January 1, 1936, and July 20, 2020, assessing drug efficacy in patients with Plasmodium-mixed infection. The primary outcome was the pooled prevalence of Plasmodium parasitemia after initiating antimalarial treatment for Plasmodium-mixed infection. The secondary outcome was the pooled risk ratio (RR) of malarial recurrence in Plasmodium-mixed infection compared with those in Plasmodium falciparum and Plasmodium vivax mono-infection. The pooled analyses were calculated by random-effects meta-analysis. After the initial treatment in different days of recurrences (≤ 28 days or > 28 days), the risk of Plasmodium parasitemia was compared in subgroup analysis.
Results
Out of 5217 screened studies, 11 were included in the meta-analysis, including 4390 patients from six countries. The pooled prevalence of all recurrences of Plasmodium-mixed parasitemia was 30% (95% confidence interval (CI) 16–43; I2: 99.2%; 11 studies). The RR of malarial recurrence within 28 days after the initial treatment (clinical treatment failure) of Plasmodium-mixed parasitemia compared with the treatment of P. falciparum was 1.22 (p: 0.029; 95% CI 1.02–1.47; Cochran Q: 0.93; I2: 0%; six studies), while there was no significant difference in the risk of recurrence 28 days after initial treatment compared with the treatment of P. falciparum (p: 0.696, RR: 1.14; 95% CI 0.59–2.18; Cochran Q < 0.05; I2: 98.2%; four studies). The subgroup analysis of antimalarial drugs showed that significant malarial recurrence within 28 days was observed in patients treated with artemisinin-based combination therapies (ACTs) with no significant heterogeneity (p: 0.028, RR: 1.31; 95% CI 1.03–1.66; Cochran Q: 0.834; I2: 0%).
Conclusions
The present findings showed a high prevalence of malarial recurrence after the initial treatment of Plasmodium-mixed infection. Moreover, significant malaria recurrence of mixed infection occurred within 28 days after treatment with ACTs.
Graphical Abstract

Similar content being viewed by others
Background
Malaria remains important to global health, as it is related to severe disease morbidity and mortality [1]. Although five species of Plasmodium are recognized as the cause of malarial diseases in humans, Plasmodium falciparum and Plasmodium vivax are the most common Plasmodium species infecting humans worldwide [1,2,3]. P. falciparum infection is the most common cause of death from malaria, particularly in endemic areas of stable transmission or high malaria endemicity [3, 4]. P. vivax is the most common cause of benign malaria in Central America, South America, and Asia [5,6,7,8]. However, severe malaria and poor outcome in patients with P. vivax infection can occur [9, 10]. P. malariae and P. ovale are recognized as benign malaria parasites, but may cause severe malaria [11]. P. ovale parasites are divided into P. ovale curtisi and P. ovale wallikeri according to the dimorphism in defined genes [12, 13].
The coexistence of two or more Plasmodium species in a single-host or mixed-species infection can occur in an endemic area [14], and this has disrupted the diagnosis and treatment of malaria. A previous study suggested that Plasmodium-mixed infection may be acquired by simultaneous inoculation of sporozoites from multiple infected anopheline mosquitoes [15]. Although the interaction of two Plasmodium species in a single host remains controversial, a previous study demonstrated that a mixed infection of P. falciparum and P. vivax in a single human host can exhibit clinical signs in two ways: (1) suppressing each other and therefore reducing the severity of malaria, or (2) enhancing each other and therefore leading to an increased risk of severe malaria [16]. Mixed infections are often unrecognized by microscopists in hospitals. The sensitivity of microscopic observation of stained thick and thin blood films, as the gold standard for malaria parasite detection, is too low to detect Plasmodium-mixed species due to very low parasitemia in mixed infections. Recently, the polymerase chain reaction (PCR) method has been conducted to detect Plasmodium mono-infection [17] and Plasmodium-mixed infection with high evidence of sensitivity and specificity for detecting low parasitemia [18,19,20]. Furthermore, a delay or failure to treat Plasmodium-mixed infection may lead to aggravated morbidity and increased mortality rate. Therefore, the consideration of Plasmodium-mixed infection and its management have important clinical and therapeutic implications, particularly in patients who are co-infected with P. falciparum and P. vivax. The present study aimed to quantify the pooled proportion and risk of malarial recurrences after treatment of Plasmodium-mixed infection. The results of this study may provide benefits to the management of Plasmodium-mixed infection in co-endemic regions.
Methods
The protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO) (ID = CRD42020199709).
Search strategy
MEDLINE, Web of Science, and Scopus were searched for potentially relevant studies on drug efficacy in patients with Plasmodium-mixed infection in any language published between January 1, 1936, and July 20, 2020. The search strategy was used as previously described [21], with some modifications in search terms for the present study (Additional file 1: Table S1).
Eligibility criteria
Studies in any language published between January 1, 1936, and July 20, 2020, were included in the analysis if they explicitly reported the presence of recurrent parasitemia with any Plasmodium species after treatment for Plasmodium-mixed infection. The following studies were excluded: studies reporting the prevalence of Plasmodium-mixed infection, in vitro studies, genetic studies, case reports or series, studies with animal models, reviews, studies on co-infection of malaria and other agents, studies where all data on recurrence could not be extracted, studies with pregnant women, and studies where full-text manuscripts were unavailable. Studies were selected by two authors (AM and MK), and discrepancies were resolved by a discussion with a third author (KUK). The results of this study were reported according to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines [22].
Data extraction
The data from the included studies were extracted independently by two authors (AM and MK); any discrepancies between them were resolved by discussion for consensus. The following details were extracted into a standardized pilot datasheet (Excel form) before further analysis: authors, year of publication, study site, year of the experiment, and information on patients, including age, gender, clinical signs, number of patients with recurrence, number of patients with Plasmodium-mixed infection at baseline, number of patients with Plasmodium falciparum and Plasmodium vivax infections at baseline, day of recurrence after the initial treatment, antimalarial drugs used, and number of any Plasmodium species after treatment. Antimalarial drugs used in the included studies were categorized as artemisinin-based combination therapies (ACTs) or chloroquine for subgroup analysis. Based on 2015 [23] and 2021 [24] World Health Organization (WHO) guidelines for the treatment of malaria, recurrence was defined as (1) recurrence within 4 weeks of treatment, which was considered as a “treatment failure,” and (2) recurrence of fever and parasitemia more than 4 weeks after treatment, which may be due to either recrudescence or new infection. Therefore, the recurrence data extracted in this study were grouped into “recurrence within 28 days” and “recurrence after > 28 days”. The upper time limit of the definition of recurrence for people with multiple malaria episodes was up to 365 days from treatment.
Quality of the included studies
The quality of the included studies was assessed using a tool developed by the Joanna Briggs Institute (checklist for quasi-experimental studies) [25].
Statistical analysis
The pooled prevalence of recurrence of any Plasmodium parasitemia after treatment was estimated using random-effects meta-analysis with proportions pooled using the Freeman-Tukey double arcsine transformation. The risk ratio (RR) of malarial recurrence after treatment of Plasmodium-mixed infection compared with those after treatment of P. falciparum and P. vivax were estimated using random-effects meta-analysis. The subgroup analysis of days of recurrence (≤ 28 days and > 28 days) was conducted to determine whether recurrence was caused by clinical treatment failure or by other causes. The subgroup analysis of antimalarial drugs (ACTs or chloroquine) and clinical signs (severe or uncomplicated malaria) was also conducted. Data heterogeneity among the included studies was assessed using Cochran's heterogeneity statistic and quantified by the I2 statistic. All analyses were performed using Stata version 15 software (StataCorp LLC, College Station, TX, USA).
Publication bias
Publication bias across the included studies was assessed using funnel plots and Egger’s test. In the funnel plot, the precision of the estimated intervention effect increases with the size of the study. Therefore, the effect estimates from small studies will scatter more widely at the bottom of the graph, with the spread narrowing among larger studies. Without bias, the plot should approximately resemble a symmetrical (inverted) funnel. For Egger’s test, the significance of the coefficients is based on a Student t distribution (t test) instead of the normal distribution (z-test). If a small-study effect was found by Egger’s test, the contour-enhanced funnel plot was further analyzed to explore the source of publication bias.
Results
Search results
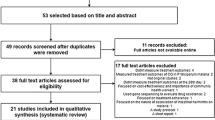
After screening the titles and abstracts of 5271 studies published between January 1, 1936, and July 20, 2020, the full texts of 443 potentially relevant studies were reviewed. A total of 432 out of 443 studies did not meet the inclusion criteria and were excluded: 166 studies that reported the prevalence of mixed Plasmodium infection, 82 in vitro studies, 58 genetic studies, 24 case report/series, 19 animal models, 17 studies that reported mixed infection at enrollment but with no data on its recurrence during follow-up, 16 studies without mixed Plasmodium infection, 16 review articles, 8 studies with no full text, 8 studies that reported malaria and other pathogens, 8 studies in pregnant women, 5 knowledge/attitude/practice studies, 3 mathematic models, and 2 guidelines (Fig. 1). Eleven studies [26,27,28,29,30,31,32,33,34,35,36] were included in the present analysis (Table 1).
Characteristics of the included studies
Of the 11 included studies (Table 1), seven (63.6%) were conducted in the WHO South-East Asian Region, including Indonesia [30, 31, 33, 34], Thailand [28], India [26], and Myanmar [35] during 1991–2015. Three studies were conducted in Papua New Guinea during 1994–2010 [29, 32, 36], and one was conducted in Ghana during 2010 [27]. Two studies [26, 33] enrolled patients with severe malaria, while eight studies [27,28,29,30, 32, 34,35,36] enrolled patients with uncomplicated malaria. One study [31] enrolled patients with both severe and uncomplicated malaria in their study. The list of drugs for the treatment of malaria is shown in Table 1: one study [26] with intravenous quinine and oral quinine, six studies [27, 28, 30,31,32, 35] with ACTs, three studies [29, 34, 36] with chloroquine, and one study [33] with intravenous artesunate and dihydroartemisinin–piperaquine or intravenous and oral quinine. Most of the included studies (9/11, 81.8%) reported Plasmodium-mixed species after treatment of Plasmodium-mixed infection. One study [32] reported P. falciparum or P. vivax mono-infection, while another study [35] reported P. vivax mono-infection after treatment of Plasmodium-mixed infection. Recurrence caused by clinical treatment failure (≤ 28 days) was demonstrated in six studies [26, 27, 29, 33, 34, 36], while recurrence after treatment (> 28 days) was demonstrated in four studies [28, 31, 32, 35]. One study demonstrated recurrence on both ≤ 28 and > 28 days after treatment [30]. Assessment of risk of bias relating to individual studies is shown in Table 2.
The pooled prevalence estimates of malarial recurrence
The prevalence of Plasmodium parasitemia was present in all 11 studies from six countries. The prevalence of all Plasmodium parasitemia after treatment ranged from 5–74%. The highest proportion of recurrence (74%; 95% CI: 65–80) was demonstrated in a study by Smithuis et al. [35], while the lowest proportion of recurrence was demonstrated in a study by Lubis et al. 2020 (5%; 95% CI 1–17) [30]. Overall, the estimated pooled prevalence of Plasmodium parasitemia after treatment of Plasmodium-mixed infection was 30% (95% CI 16–43; I2: 99.2%) (Fig. 2).
The risk of Plasmodium-mixed species recurrence compared with P. falciparum recurrence
The risk of malarial recurrence after treatment of Plasmodium-mixed infection was compared with malarial recurrence after treatment of P. falciparum infection. Overall, no significant difference in the risk of any recurrent parasitemia was observed when the recurrence risks from the 11 studies were pooled (p: 0.266, RR: 1.23; 95% CI 0.85–1.78; Cochran Q < 0.05; I2: 94%) (Fig. 3).
Subgroup analysis of the days of recurrence
A subgroup analysis of the days of recurrence (≤ 28 days or > 28 days) was conducted for the 11 studies. A significantly higher risk of malarial recurrence within 28 days after the treatment of mixed Plasmodium infection was found, with no significant heterogeneity across the studies analyzed (p: 0.029, RR: 1.22; 95% CI 1.02–1.47; Cochran Q: 0.93; I2: 0%; six studies) (Fig. 4). A study by Sikora et al. in 2019 demonstrated a higher risk of malarial recurrence within 28 days after treatment (RR: 1.30; 95% CI 1.02–1.66). No significant difference was observed in the risk of malarial recurrence after 28 days of treatment for mixed Plasmodium infection, with significant heterogeneity across the studies analyzed (p: 0.696, RR: 1.14; 95% CI 0.59–2.18; Cochran Q < 0.05; I2: 98.2%; four studies). A higher risk of malarial recurrence after 28 days of treatment was demonstrated in the studies by Douglas et al. [28] and Smithuis et al. [35], while a lower risk of recurrence after 28 days of treatment was demonstrated in a study by Patriani et al. [31].
Subgroup analysis of antimalarial drugs
A subgroup analysis of antimalarial drugs was conducted using the data from 11 studies. Overall, no significant difference in the risk of malarial recurrence after treatment with ACTs was found between mixed Plasmodium infection and P. falciparum infection (p: 0.423, RR: 1.27; 95% CI 0.71–2.27; Cochran Q < 0.05; I2: 97%; six studies) (Fig. 5). No significant difference in the risk of malarial recurrence was found between Plasmodium-mixed infection and P. falciparum infection (p: 0.546, RR: 1.10; 95% CI 0.82–1.47; Cochran Q: 0.83; I2: 0%; three studies) after treatment with chloroquine. A subgroup analysis of antimalarial drugs was further performed in six studies [26, 27, 29, 33, 34, 36] which reported the recurrence of all Plasmodium parasitemia within 28 days after treatment. The results showed that the malarial recurrence within 28 days was significantly observed in patients treated with ACTs, with no significant heterogeneity (p: 0.028, RR: 1.31; 95% CI 1.03–1.66; Cochran Q: 0.834; I2: 0%), while there was no significant difference in the risk of malarial recurrence within 28 days in patients treated with chloroquine (p: 0.546, RR: 1.10; 95% CI 0.82–1.47; Cochran Q: 0.828; I2: 0%) (Fig. 6).
Subgroup analysis of clinical signs
A subgroup analysis of clinical signs (severe or uncomplicated malaria) was conducted. The results showed that a significantly higher risk of malarial recurrence after treatment of Plasmodium-mixed infection was observed in patients with severe malaria, with no significant heterogeneity across the studies analyzed (p: 0.029, RR: 1.30; 95% CI 1.03–1.65; Cochran Q: 0.88; I2: 0%; two studies). In addition, a significantly higher risk of malarial recurrence after treatment of Plasmodium-mixed infection was also observed in patients with uncomplicated malaria, with no significant heterogeneity across the studies analyzed (p < 0.001, RR: 1.46; 95% CI 1.33–1.61; Cochran Q: 0.37; I2: 7.5%; eight studies) (Fig. 7).
The risk of Plasmodium-mixed species recurrence compared with P. vivax recurrence
The risk of malarial recurrence after treatment of Plasmodium-mixed infection was compared with malarial recurrence after treatment of P. vivax infection. Overall, no significant difference in the risk of any recurrent parasitemia was observed when the recurrence risks from the seven studies were pooled (p: 0.847, RR: 0.94, 95% CI 0.53–1.68, Cochran Q < 0.05, I2: 89.9%) (Fig. 8).
Publication bias
The publication bias is shown in Fig. 9, in which the dispersion of the nine-point estimates was close to the true intervention or pooled estimate. This result indicates the symmetry of the funnel plot. However, two studies exhibited a wide dispersion of the point estimates from the center, indicating the possibility of publication bias among the included studies. The possibility of publication bias due to smaller studies was further investigated by Egger’s test. The results of Egger’s test demonstrated that no small-study effects were found (p: 0.934; t: 0.09; coefficients: 0.15; standard error: 1.78), indicating that the publication bias might be due to other causes, such as the variability in included studies, especially concerning the prevailing Plasmodium species and resistance pattern driven by drug pressure.
Discussion
Infection by Plasmodium-mixed species, if left untreated or managed poorly, can lead to severe malaria [37]. A previous systematic review and meta-analysis demonstrated that either Plasmodium-mixed infection or P. falciparum mono-infection showed a similar trend of complications in which severe anemia, pulmonary failure, and renal impairment were the three most common complications found [37]. The present study found a high estimated prevalence of Plasmodium parasitemia after treatment of Plasmodium-mixed infection (30%). This result indicated that treatment failure, relapse, or recrudescence might have occurred in these patients. The present study also demonstrated clearly that a significantly higher risk of malarial recurrence occurred within 28 days after treatment of Plasmodium-mixed infection compared to those with P. falciparum infection, while no significant recurrence was observed between the two groups after 28 days. This implies that the cause of malarial recurrence in patients with mixed infection might be due to early or late clinical treatment failure. In comparison to the treatment of P. falciparum, the treatment of Plasmodium-mixed infection significantly led to malaria recurrence within 28 days as observed in patients treated with ACTs, while no significant malarial recurrence within 28 days in patients treated with chloroquine was observed. This indicated that patients with Plasmodium-mixed infection who are treated with ACTs similar to the treatment of patients with P. falciparum can still experience treatment failure, particularly patients with severe malaria. This result was supported in studies by Sikora et al. [33] and Ahmed et al. [26], which reported that malarial recurrence was caused by clinical treatment failure among patients with severe malaria. Nevertheless, after treatment of Plasmodium-mixed infection, malarial recurrence can occur in patients with uncomplicated malaria, as demonstrated in the subgroup analysis of clinical signs. The risk of malarial recurrence was not observed in patients with mixed infections compared to those with P. vivax mono-infection. The significance of malarial recurrence in patients with uncomplicated malaria was observed in studies by Douglas et al. in Thailand [28] and Smithuis et al. in Myanmar [35]. This result indicated that the recurrence of malaria after treatment of Plasmodium-mixed infection might be caused by many factors, including drug resistance or inappropriate antimalarial drugs [23], severity signs, lack of malarial immunity [38, 39], or no additional dose of primaquine to reduce potential P. vivax transmission substantially [35].
Treatment decisions on malaria infection are different based on Plasmodium species and disease severity. In uncomplicated malaria, chloroquine and primaquine drugs are administered to treat P. vivax, while ACTs are administered to treat P. falciparum malaria since P. falciparum is resistant to chloroquine [23]. For the treatment of Plasmodium-mixed species, WHO suggested that ACTs (except artesunate + sulfadoxine–pyrimethamine) are effective against all malaria species and are the treatment of choice against mixed infection in co-endemic areas of P. falciparum and P. vivax [23]. In all severe malaria cases, intravenous artesunate or quinine is administered for at least 24 h before patients can tolerate oral medication [23]. Since misdiagnosis of mixed species of malaria infection might lead to severe malaria [37], intravenous artesunate or quinine was used to treat severe mixed malaria infection in two of the included studies [26, 33].
Most of the studies included in this meta-analysis were performed on the Asian continent because of the emergence of multidrug resistance in driving the treatment policy changes, but fewer malaria treatment options are available in Asian countries. It was also due to the potential spread of ACT resistance in sub-Saharan Africa because of the progression of chloroquine resistance and sulfadoxine–pyrimethamine resistance from Asia to sub-Saharan Africa in the past, which contributed to millions of childhood deaths [40, 41]. Previous studies reported the incidence of P. vivax parasitemia after the treatment of P. falciparum or mixed Plasmodium species in Southeast Asia [21, 28, 42]. Therefore, the efficacy of antimalarial treatment to prevent the recurrence of P. vivax parasitemia is an important consideration for clinical drug trials of malaria control strategies in this region.
This study had limitations. First, there was a limited number of studies reporting the treatment of mixed Plasmodium infection, which might result in a low statistical power to be applied over a large population. Some potentially eligible studies did not report the exact number of Plasmodium recurrences after treatment with antimalarial drugs, and no studies reported in non-English language were found for the present study, leading to a limited number of included studies. Second, the baseline characteristics of patients, such as age, could not be extracted in all the included studies since the treatment efficacy of malaria was improved as the age increased [43]. Therefore, the subgroup analysis and meta-regression analysis of age as a confounder for risk of recurrence could not be performed. Third, looking at the range of values for recurrence reported (5–74%), it is likely that the differences in human, vector, and parasite dynamics, study methodology, follow-up time, and treatment efficacy may account for some of the variations in recurrence. Fourth, the “true” RR and funnel plots of this study may be misleading due to the variability in the included studies, especially concerning the prevailing Plasmodium species and resistance pattern driven by drug pressure. Therefore, there is a need for a careful interpretation of the RR of malarial recurrence in patients with mixed Plasmodium infection after treatment with antimalarial drugs. Fifth, the present meta-analysis included the publication of Douglas et al. [28] that pooled the findings of multiple studies that applied different study designs, different medications, and outcome assessment; in essence, this is a pooling of study findings but without the statistical benefits of a meta-analysis. This is akin to including a meta-analysis in the present meta-analytic data. Therefore, the interpretation of meta-analysis in the present study requires major attention for this included study.
Conclusion
The present findings showed a high prevalence of malarial recurrence after initial treatment of Plasmodium-mixed species. Moreover, significant malaria recurrence of mixed infection occurred within 28 days after treatment with ACTs. Therefore, in regions where more than one Plasmodium species are endemic, the use of appropriate antimalarial drugs with increased vigilance is required and should be strengthened during and after treatment. Further research is required to gain a better understanding of the mechanisms involved in the recurrence observed after treatment with ACTs.
Availability of data and materials
All data in the manuscript and supplementary files are available.
Abbreviations
- ACTs:
-
Artemisinin-based combination therapies
- CI:
-
Confidence interval
- PCR:
-
Polymerase chain reaction
- PRISMA:
-
Preferred reporting items for systematic reviews and meta-analyses
- RR:
-
Risk ratio
- WHO:
-
World Health Organization
References
World Health Organization. Malaria. https://www.who.int/news-room/fact-sheets/detail/malaria. Accessed 20 August 2020.
Greenwood BM, Bojang K, Whitty CJ, Targett GA. Malaria. Lancet. 2005;365(9469):1487–98.
Snow RW, Guerra CA, Noor AM, Myint HY, Hay SI. The global distribution of clinical episodes of Plasmodium falciparum malaria. Nature. 2005;434:214–7.
Autino B, Noris A, Russo R, Castelli F. Epidemiology of malaria in endemic areas. Mediterr J Hematol Infect Dis. 2012;4:e2012060.
Price RN, Tjitra E, Guerra CA, Yeung S, White NJ, Anstey NM. Vivax malaria: neglected and not benign. Am J Trop Med Hyg. 2007;77:79–87.
Dayananda KK, Achur RN, Gowda DC. Epidemiology, drug resistance, and pathophysiology of Plasmodium vivax malaria. J Vector Borne Dis. 2018;55:1–8.
Anvikar AR, Shah N, Dhariwal AC, Sonal GS, Pradhan MM, Ghosh SK, et al. Epidemiology of Plasmodium vivax malaria in India. Am J Trop Med Hyg. 2016;95:108–20.
Musset L, Heugas C, Naldjinan R, Blanchet D, Houze P, Abboud P, et al. Emergence of Plasmodium vivax resistance to chloroquine in French Guiana. Antimicrob Agents Chemother. 2019;63:e02116-e2118.
Kotepui M, Kotepui KU, Milanez GJ, Masangkay FR. Prevalence and risk factors related to poor outcome of patients with severe Plasmodium vivax infection: a systematic review, meta-analysis, and analysis of case reports. BMC Infect Dis. 2020;20:363.
Mitra S, Abhilash K, Arora S, Miraclin A. A prospective study from south India to compare the severity of malaria caused by Plasmodium vivax, P. falciparum and dual infection. J Vector Borne Dis. 2015;52:281–6.
Kotepui M, Kotepui KU, Milanez GD, Masangkay FR. Severity and mortality of severe Plasmodium ovale infection: a systematic review and meta-analysis. PLoS One. 2020;15:e0235014.
Sutherland CJ, Tanomsing N, Nolder D, Oguike M, Jennison C, Pukrittayakamee S, et al. Two nonrecombining sympatric forms of the human malaria parasite Plasmodium ovale occur globally. J Infect Dis. 2010;201:1544–50.
Calderaro A, Piccolo G, Gorrini C, Rossi S, Montecchini S, Dell’Anna ML, et al. Accurate identification of the six human Plasmodium spp. causing imported malaria, including Plasmodium ovale wallikeri and Plasmodium knowlesi. Malar J. 2013;12:321.
Kotepui M, Kotepui KU, Milanez GD, Masangkay FR. Prevalence and proportion of Plasmodium spp. triple mixed infections compared with double mixed infections: a systematic review and meta-analysis. Malar J. 2020;19:224.
Imwong M, Nakeesathit S, Day NP, White NJ. A review of mixed malaria species infections in anopheline mosquitoes. Malar J. 2011;10:253.
Mohapatra MK, Dash LK, Barih PK, Karua PC. Profile of mixed species (Plasmodium vivax and falciparum) malaria in adults. J Assoc Physicians India. 2012;60:20–4.
Snounou G, Viriyakosol S, Jarra W, Thaithong S, Brown KN. Identification of the four human malaria parasite species in field samples by the polymerase chain reaction and detection of a high prevalence of mixed infections. Mol Biochem Parasitol. 1993;58:283–92.
Rodulfo H, De Donato M, Mora R, Gonzalez L, Contreras CE. Comparison of the diagnosis of malaria by microscopy, immunochromatography and PCR in endemic areas of Venezuela. Braz J Med Biol Res. 2007;40:535–43.
Mixson-Hayden T, Lucchi NW, Udhayakumar V. Evaluation of three PCR-based diagnostic assays for detecting mixed Plasmodium infection. BMC Res Notes. 2010;3:88.
Tajebe A, Magoma G, Aemero M, Kimani F. Detection of mixed infection level of Plasmodium falciparum and Plasmodium vivax by SYBR Green I-based real-time PCR in North Gondar, north-west Ethiopia. Malar J. 2014;13:411.
Commons RJ, Simpson JA, Thriemer K, Hossain MS, Douglas NM, Humphreys GS, et al. Risk of Plasmodium vivax parasitaemia after Plasmodium falciparum infection: a systematic review and meta-analysis. Lancet Infect Dis. 2019;19:91–101.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097.
World Health Organization. Guidelines for the treatment of malaria. https://apps.who.int/iris/handle/10665/162441. Accessed 5 Aug 2020.
World Health Organization. WHO guidelines for malaria. https://www.who.int/publications/i/item/WHO-UCN-GMP-2021.01. Accessed 20 Apr 2021.
Munn Z, Moola S, Lisy K, Riitano D, Tufanaru C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int J Evid Based Healthc. 2015;13:147–53.
Ahmed S, Adil F, Shahzad T, Yahiya Y. Severe malaria in children: Factors predictive of outcome and response to Quinine. J Pak Med Assoc. 2011;61:54–8.
Dinko B, Oguike MC, Larbi JA, Bousema T, Sutherland CJ. Persistent detection of Plasmodium falciparum, P. malariae, P. ovale curtisi and P. ovale wallikeri after ACT treatment of asymptomatic Ghanaian school-children. Int J Parasitol Drugs Drug Resist. 2013;3:45–50.
Douglas NM, Nosten F, Ashley EA, Phaiphun L, Van Vugt M, Singhasivanon P, et al. Plasmodium vivax recurrence following falciparum and mixed species malaria: risk factors and effect of antimalarial kinetics. Clin Infect Dis. 2011;52:612–20.
Genton B, Baea K, Lorry K, Ginny M, Wines B, Alpers MP. Parasitological and clinical efficacy of standard treatment regimens against Plasmodium falciparum, P. vivax and P. malariae in Papua New Guinea. P N G Med J. 2005;48:141–50.
Lubis IND, Wijaya H, Lubis M, Lubis CP, Beshir KB, Staedke SG, et al. Recurrence of Plasmodium malariae and P. falciparum following treatment of uncomplicated malaria in North Sumatera with dihydroartemisinin-piperaquine or artemether-lumefantrine. Open Forum Infect. 2020;7:116.
Patriani D, Arguni E, Kenangalem E, Dini S, Sugiarto P, Hasanuddin A, et al. Early and late mortality after malaria in young children in Papua, Indonesia. BMC Infect Dis. 2019;19:13.
Senn N, Rarau P, Manong D, Salib M, Siba P, Reeder JC, et al. Effectiveness of artemether/lumefantrine for the treatment of uncomplicated Plasmodium vivax and P. falciparum malaria in young children in Papua New Guinea. Clin Infect Dis. 2013;56:1413–20.
Sikora SA, Poespoprodjo JR, Kenangalem E, Lampah DA, Sugiarto P, Laksono IS, et al. Intravenous artesunate plus oral dihydroartemisinin-piperaquine or intravenous quinine plus oral quinine for optimum treatment of severe malaria: lesson learnt from a field hospital in Timika, Papua, Indonesia. Malar J. 2019;18:448.
Siswantoro H, Ratcliff A, Kenangalem E, Wuwung M, Maristela R, Rumaseuw R, et al. Efficacy of existing antimalarial drugs for uncomplicated malaria in Timika, Papua, Indonesia. Med J Indonesia. 2006;15:251–8.
Smithuis F, Kyaw MK, Phe O, Win T, Aung PP, Oo APP, et al. Effectiveness of five artemisinin combination regimens with or without primaquine in uncomplicated falciparum malaria: an open-label randomised trial. Lancet Infect Dis. 2010;10:673–81.
Sumawinata IW, Leksana B, Sutamihardja A, Purnomo A, Subianto B, et al. Very high risk of therapeutic failure with chloroquine for uncomplicated Plasmodium falciparum and P. vivax malaria in Indonesian Papua. Am J Trop Med Hyg. 2003;68:416–20.
Kotepui M, Kotepui KU, De Jesus Milanez G, Masangkay FR. Plasmodium spp. mixed infection leading to severe malaria: a systematic review and meta-analysis. Sci Rep. 2020;10:11068.
O’Flaherty K, Maguire J, Simpson JA, Fowkes FJI. Immunity as a predictor of anti-malarial treatment failure: a systematic review. Malar J. 2017;16:158.
Greenhouse B, Slater M, Njama-Meya D, Nzarubara B, Maiteki-Sebuguzi C, Clark TD, et al. Decreasing efficacy of antimalarial combination therapy in Uganda is explained by decreasing host immunity rather than increasing drug resistance. J Infect Dis. 2009;199:758–65.
Trape JF. The public health impact of chloroquine resistance in Africa. Am J Trop Med Hyg. 2001;64:12–7.
Roper C, Pearce R, Nair S, Sharp B, Nosten F, Anderson T. Intercontinental spread of pyrimethamine-resistant malaria. Science. 2004;305:1124.
Hossain MS, Commons RJ, Douglas NM, Thriemer K, Alemayehu BH, Amaratunga C, et al. The risk of Plasmodium vivax parasitaemia after P. falciparum malaria: an individual patient data meta-analysis from the World Wide Antimalarial Resistance Network. PLoS Med. 2020;17:e1003393.
Staedke SG, Sendagire H, Lamola S, Kamya MR, Dorsey G, Rosenthal PJ. Relationship between age, molecular markers, and response to sulphadoxine-pyrimethamine treatment in Kampala. Uganda Trop Med Int Health. 2004;9:624–9.
Acknowledgements
The authors would like to thank the authors of all the published research that contributed to the data used in this study.
Funding
This research was partially supported by the New Strategic Research (P2P) project, Walailak University, Thailand. The funders had a role in the collection, analysis, and interpretation of data.
Author information
Authors and Affiliations
Contributions
AM, MK, KUK, GDM, and FRM participated in the study design, data analysis, and writing of the paper. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that there is no conflict of interest regarding the publication of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Search terms.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mahittikorn, A., Masangkay, F.R., Kotepui, K.U. et al. The high risk of malarial recurrence in patients with Plasmodium-mixed infection after treatment with antimalarial drugs: a systematic review and meta-analysis. Parasites Vectors 14, 280 (2021). https://doi.org/10.1186/s13071-021-04792-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13071-021-04792-5