Abstract
Intra-abdominal candidiasis (IAC) is one of the most common of invasive candidiasis observed in critically ill patients. It is associated with high mortality, with up to 50% of deaths attributable to delays in source control and/or the introduction of antifungal therapy. Currently, there is no comprehensive guidance on optimising antifungal dosing in the treatment of IAC among the critically ill. However, this form of abdominal sepsis presents specific pharmacokinetic (PK) alterations and pharmacodynamic (PD) challenges that risk suboptimal antifungal exposure at the site of infection in critically ill patients. This review aims to describe the peculiarities of IAC from both PK and PD perspectives, advocating an individualized approach to antifungal dosing. Additionally, all current PK/PD studies relating to IAC are reviewed in terms of strength and limitations, so that core elements for the basis of future research can be provided.
Highlights
-
Intra-abdominal candidiasis presents specific pharmacokinetic (PK) and pharmacodynamic (PD) challenges where suboptimal antifungal concentrations are likely to occur leading to high risk of treatment failure.
-
The intra-abdominal cavity has been highlighted as a hidden reservoir for resistance to antifungals including echinocandins.
-
To date, all antifungal PK/PD studies in intra-abdominal candidiasis have enrolled small cohorts and have only provided post-operative antifungal concentrations analysis.
-
Based on current evidence, high dosing regimens of antifungals should be strongly considered, especially at the onset of infection.
-
The place of new antifungals (rezafungin, ibrexafungerp) requires more robust clinical studies including PK/PD analysis in critically ill patients.
Similar content being viewed by others
Introduction
Intra-abdominal candidiasis (IAC) is defined as the isolation of Candida from a sterile intra-abdominal sample along with symptoms of intra-abdominal infection [1, 2]. Current epidemiological data quantifies IAC having a cumulative incidence of 1.84 cases per 1,000 ICU admissions and a mortality up to 50% [3, 4]. C. albicans accounts for most infections followed by non-albicans species such as C. glabrata and C. parapsilosis [5, 6].
The management of IAC requires initiating early and adequate source control, and prompt initiation of antifungal therapy [7, 8]. Current guidelines recommend echinocandins as the first-line agent for empirical treatment of IAC in critically ill patients [8,9,10]. Fluconazole has been recommended for clinically stable patients with no recent exposure to azoles in the setting of fluconazole-susceptible pathogens [10, 11]. Second-line agents include the liposomal formulation of amphotericin B [10, 11] and voriconazole [12]. However, these guidelines do not provide any specific recommendations regarding alternative dosing regimens in the critically ill [7]. Indeed, only standardized antifungal dosing regimens are proposed. Of note, specific guidelines in cases of critically ill obese patients or those receiving extracorporeal support are lacking, even though IAC is common to these situations which are associated with difficult-to-predict antifungal concentrations [13]. The considerable pharmacokinetics (PK) inter-variability of antifungals was highlighted in the multinational Defining Antibiotic Levels in Intensive care Unit (DALI) study [14].
Most of the studies providing antifungal dosing recommendations for invasive candidiasis generally include more patients with candidemia than IAC [15]. Thus, most studies describe antifungal exposure in the central compartment (i.e., blood). However, it has been demonstrated that many antifungals diffuse poorly into intra-abdominal collections [13, 16]. Therefore, considering that critically ill patients may have lower plasma antifungal concentrations compared to other population groups, the risk of suboptimal concentrations at the site of infection may be even higher [17, 18].
This review explores the pharmacokinetic and pharmacodynamic considerations for antifungal therapy in the treatment of IAC among critically ill patients. Additionally, it proposes dose optimisation strategies of the most used antifungals in the treatment of IAC.
Pharmacokinetic considerations
Critically ill patients have severe pathophysiological changes driven by a change in the volume of distribution (Vd) and/or modified renal and/or hepatic clearances [19]. Altered Vd is characterized by the expansion of the interstitial space secondary to an increase in capillary permeability, vascular filling, and change in protein binding. “Capillary leakage” is caused by systemic inflammation, a common feature during sepsis that is even more pronounced in septic shock. In critically ill patients with intra-abdominal infections, sepsis and septic shock affect more than 60% and 30% of them, respectively [20]. Abdominal sepsis is also associated with a cytokine “storm”, further aggravating the patient’s inflammatory state compared to sepsis of other origins [21]. Besides, abdominal surgery induced-trauma results in post-operative inflammation [22, 23]. The degree of post-operative inflammation depends on the surgical approach [24]. Laparotomy, which is the most commonly used [25], is more aggressive and thereby highly “inflammatory” compared to laparoscopic surgery. In addition to this “high” inflammatory state, abdominal sepsis is characterized by severe hypovolemia caused by a high prevalence of fever and other sources of fluid loss including anorexia, nausea, and vomiting [26]. Surgery also provides changes in extracellular fluid space mostly driven by neuroendocrine mechanisms. Indeed, part of the endocrine response to surgery involves the increased secretion of antidiuretic hormone and aldosterone leading to salt and water retention [27]. Sequestration of fluids may also occur due to large volume of fluids lost into a distended gut or the peritoneal cavity [28]. Thus, vascular filling is potentially massive in the sickest of these patients, with up to 10 L administered during the first days of fluid resuscitation [17, 29]. An increase in the drug Vd equates to insufficient drug concentrations within the central compartment (i.e. plasma). Lastly, surgery itself affects drug distribution by changes in blood volume (blood and fluid losses during laparotomy) and altered regional perfusion secondary to an increase in circulating catecholamines induced by surgical trauma [28]. Local inflammation combined with decreases in regional blood flow contribute to drug diffusion impairment.
During the post-operative period, interventions that utilise extracorporeal circuits such as renal replacement therapy (RRT) or extracorporeal membrane oxygenation (ECMO) may also contribute to changes in drug clearance depending on the physicochemical properties of the drug [30, 31]. In addition, alterations of protein binding are highly frequent in surgical ICU patients because of a physiological decrease of pre-albumin and albumin in response to an increase of inflammatory protein. Hypoalbuminemia is worsened by vascular filling, malnutrition and a catabolic state, frequent situations seen in post-operative surgical patients [32]. Lastly, indwelling abdominal drains left in situ post-operatively also contribute to an increased elimination of drug [33]. Indeed, previous studies have reported that the increase in drug clearance is proportional to drainage output [34]. Therefore, critically ill patients with IAC have significant drug PK alteration that potentially predisposes them to inadequate drug concentrations that can be exacerbated by surgical interventions during their ICU admission.
Pharmacokinetic properties of parenteral antifungals used in intra-abdominal candidiasis
Table 1 summarises the PK of antifungal agents used in the treatment of intra-abdominal candidiasis. Dosing regimens and therapeutic ranges for therapeutic drug monitoring (TDM) are proposed based on current evidence.
First-line agents
Fluconazole
Fluconazole is a triazole which inhibits the 14-α-demethylase which is an enzyme required for conversion of lanosterol into ergosterol. It has low plasma protein binding of 12% and is a weakly basic, highly polar, hydrophilic (LogP 0.5) drug with a small molecular weight [35]. These physicochemical properties expose fluconazole to unpredictable concentrations in the critically ill patient [36, 37]. Indeed, hydrophilic, low protein-binding and low molecular weight are highly influenced by increased Vd and renal clearance; leading to low drug exposure [19].
Fluconazole exhibits concentration- and time-dependent antifungal activity with a prolonged post-antifungal effect. The predictive PK/PD index associated with maximal fungal killing is the ratio of free-drug area under the concentration time curve (from 0 to 24 h) to minimum inhibitory concentration of the fungal organism (fAUC0-24/MIC). An fAUC0-24/MIC of greater than 100 is associated with optimal fungicidal activity and positive outcomes in critically ill patients [38, 39]. Current dosing regimens in critically ill patients with normal renal function recommend a loading dose of 12 mg/kg intravenously followed by a maintenance dose of 6—12 mg/kg/day [40]. Maintenance doses of up to 18 mg/kg per day have been proposed [41]. Factors associated with suboptimal fluconazole exposure include obesity, high renal clearance and patients undergoing continuous RRT [42, 43]. In obese patients, total body weight has been used to calculate doses [44]. In the setting of RRT, adjusting the maintenance dose to 800 mg (400 mg q12h) has been suggested [45]. In contrast, ECMO by itself does not seem to influence fluconazole PK [31]. Indeed, PK alteration under ECMO is mostly related to lipophilicity or changes in Vd and to date, no sequestration in the ECMO circuit has been demonstrated with fluconazole. However, data in adult patients are scarce and more studies are warranted to better address optimal dosing of fluconazole in patients undergoing ECMO.
Regarding abdominal diffusion of fluconazole, very few data are available [46]. Sinnollareddy et al. [47] have measured subcutaneous concentrations of fluconazole in critically ill patients and reported an AUC0-24 50% lower than in plasma. A mini-case series of three liver transplant patients reported that the ascites-to-plasma ratio of fluconazole was 0.85 [48]. A case report of a patient with cholecystitis showed that biliary fluconazole concentrations were 50% lower than in the plasma [49]. Lastly, relatively good penetration (88 to 91%) of fluconazole in the pancreas has been reported [50]. This is of significance given that pancreatic necrosis is a frequent source of IAC. Therefore, if tissue penetration based on small studies advocate for relatively good penetration of fluconazole (> 50%), physicochemical properties of fluconazole expose it to suboptimal plasma concentrations in critically ill patients. As low plasma concentrations are associated with even lower tissue concentrations for hydrophilic drugs [51], the risk of suboptimal fluconazole concentrations at the site of infection must be considered very high. Thus, higher doses and TDM should be considered when treating IAC with fluconazole. However, data regarding the therapeutic range of fluconazole are lacking [40, 52, 53]. For instance, a mean trough concentration of 14 mg/L ± 11 mg/L was reported in the DALI study [14]. A trough concentration of 10 to 15 mg/L has been proposed as a basis for fluconazole TDM [52].
Echinocandins
General considerations
Echinocandins are cyclic hexa-lipopeptides targeting the fungal wall by inhibiting 1.3 beta-d-glucan synthesis [54]. They are fungicidal against most pathogenic species of Candida [55].
Echinocandins are highly protein-bound (≥ 90%), hydrophilic molecules which are eliminated through ubiquitous spontaneous degradation. The PK/PD index most frequently reported for echinocandins is AUC/MIC [56, 57]. The AUC/MIC ratios ranged from > 250 (caspofungin/C. tropicalis) to > 10,000 (micafungin/C. albicans) [58] (Table 1). Thanks to low drug-drug interactions, non-renal elimination, and less extensive hepatic clearance, echinocandins are often considered easy-to-dose drugs [13]. Reported adverse events to date have not established any exposure-related toxicity [56]. Additionally, high doses in the treatment of endocarditis are well tolerated [59]. However, a growing body of evidence has challenged the concept of fixed standard doses [18, 56, 60]. Higher body weights may require higher dosing [61, 62], whilst patients with hypoalbuminemia may have an increased Vd and clearance [13]. Most studies point towards a 20% lower exposures in critically ill patients when compared with healthy volunteers [63,64,65].
Caspofungin
It has been suggested to increase the loading dose to 140 mg in critically ill patients [66]. Likewise, a higher, weight-based dose of 2 mg/kg as a loading dose and 1.25 mg/kg as a maintenance dose have been recommended in critically ill obese patients [67]. Regarding ECMO, caspofungin loss via sequestering within the ECMO circuit was reported, suggesting to increase the loading and 24-hourly maintenance dose to 70 mg, respectively [31, 68].
Micafungin
It has been proposed to increase the maintenance dose from 150 mg to between 200 to 300 mg 24-hourly in critically ill obese patients (> 125 kg), depending on the MIC [61]. In patients with ECMO, it has been suggested to increase the micafungin loading and 24-hourly maintenance dose to 150 and 70 mg, respectively [31].
Anidulafungin
If suboptimal exposures have been reported (~ 30% lower concentrations compared to healthy volunteers [69]), current data does not define what higher doses should be used [68]. No dosing adjustments are currently recommended for anidulafungin during ECMO.
Peritoneal diffusion of echinocandins
Regarding peritoneal diffusion of echinocandins, eight PK studies [57, 70,71,72,73,74,75,76] (Table 2) were performed and reported an overall penetration ratio of ~ 30%, knowing that no PK/PD target in the peritoneum has been defined to date. One study also reported highly variable ascites-to-plasma echinocandin penetration ratios ranging from 0.02 to 0.46 in ascitic fluids [48].
Which lessons?
Recent data supporting the need for higher echinocandin doses are mostly from PK studies. This data does not demonstrate, however, that the use of these proposed higher echinocandin doses is associated with better clinical outcomes.
Considering the PK variability of echinocandins in the plasma and the low to moderate penetration ratios in the peritoneal fluid, the risk of suboptimal echinocandin exposures at the site of infection remains high. Thus, use of higher doses and TDM are valid considerations. However, there are currently no defined therapeutic ranges for echinocandins [40, 52, 53]. Some authors have proposed a total trough concentration > 1 mg/L or between 1 and 3 mg/L [52, 53].
Second-line agents
Liposomal amphotericin B
The lipid formulations of amphotericin B deoxycholate (L-AmB) are recommended as alternatives in cases of echinocandin-resistant Candida infections [10, 11]. L-AmB has many PK/PD advantages such as broad-spectrum coverage, rapid time-kill rate, post-antifungal effect, and action against biofilm formation [77, 78]. PK/PD studies of L-AmB involving critically ill patients are scarce and reported lower Vd with considerable variability in L-AmB concentrations [79,80,81]. Furthermore, no clear PK/PD target has been defined for the liposomal formulation. Table 1 provides general PK data and influence of RRT [54], ECMO [82,83,84], and obesity on L-AmB dosing [85]. Considering the high variability of L-AmB concentrations with a high risk of underdosing, it seems reasonable to propose the dose of 5 mg/kg/day in critically ill patients with IAC which has been reported to be safe [86]. Last, one pediatric study has evaluated peritoneal diffusion and reported lower peritoneal L-AmB concentrations than plasma concentrations [87].
Voriconazole
Voriconazole is the second most used azole in critically ill patients with IAC [88]. It has been proposed as an alternative option in severe intra-abdominal infections that have a risk of fluconazole-resistant Candida strains [12]. Data in critically ill patients are scarce and reported large interindividual variability [89, 90]. PK/PD main characteristics of voriconazole are provided in Table 1 [54, 90] with influence of various clinical situations [13, 91,92,93,94] and extracorporeal supports [31, 54, 92, 95,96,97,98]. Considering the high interindividual variability and high occurrence of drug-drug interactions, voriconazole TDM is strongly recommended [13, 40]. Last, one study reported a peritoneal penetration ratio of 0.54 and 0.67 for single and multiple doses, respectively (Table 3) [99].
New antifungals
Among new antifungals arriving through the development pipeline [100], Rezafungin and Ibrexafungerp have been evaluated within phase 3 clinical trials in patients with invasive candidiasis [101,102,103]. Rezafungin is a new echinocandin with extended half-life and improved tissue penetration compared to other echinocandins [104,105,106]. The main PK/PD parameters [106, 107] and spectrum of activity [108, 109] are described in Table 2. Rezafungin PK is not affected by age, sex, race, body weight (34–155 kg), renal clearance (9.3 to > 120 ml/min), continuous RRT [110], and impaired liver function (Child Pugh B or C) [111]. The PK/PD properties of rezafungin may advocate its use in IAC. Indeed, as it has been reported that IAC could provide a reservoir for the emergence of Candida resistance [112], considering the front-loaded exposure and higher tissue penetration, rezafungin may be associated with a lower risk of emergence of resistance compared to the other echinocandins [113]. However, its half-life precludes dose adjustment before one week. Considering the dynamic process of PK alteration in critically ill patients, clinical studies are warranted to quantify rezafungin exposure at the onset of infection.
Ibrexafungerp inhibits the production of 1.3-beta-glucan through non-competitive inhibition of the 1.3-beta-glucan synthase complex [114, 115]. The main PK/PD parameters [116,117,118,119] and spectrum of activity [114, 119] are described in Table 2. No dosage adjustment is recommended in patients with renal and mild-to-moderate hepatic impairment. Excellent tissue penetration has been reported in the liver, lung, kidney, spleen, skin and bone [114]. Regarding IAC, one murine model has confirmed excellent penetration of ibrexafungerp penetration in the liver with prolonged therapeutic exposure [120].
In addition to its interest in echinocandin Candida resistant strains, ibrexafungerp could be useful as an oral drug in replacement of azoles for de-escalation, especially when azoles are not well-tolerated. Ibrexafungerp is currently under investigation for step-down therapy after initial empirical treatment with echinocandins (clinicalTrials.gov number NCT02244606).
Pharmacodynamic considerations
Mechanisms of antifungal resistance
An increase in fluconazole and echinocandin resistance has been reported in both C. albicans and non-albicans species. This increase in antifungal resistance is mainly associated with an increased exposure to antifungal therapy in the ICU [112, 121, 122].
Mechanisms of antifungal resistance depend on the Candida species as well as the antifungal [123]. Broadly, there are three main mechanisms of antifungal resistance:
-
Presence of biofilm, where the highest MICs have been observed mostly from in vitro studies [124],
-
Increased number of efflux pumps which precludes accumulation of antifungal in the fungal cell [125],
-
Reduced 1.3 beta-d-glucan synthase sensitivity [125].
These three mechanisms have been observed in C. albicans. The reduction in 1.3 beta-d-glucan synthase sensitivity caused by a mutation in FKS1 and FKS2 genes has been demonstrated to confer a cross resistance to azoles and echinocandins. C. glabrata has a reduced susceptibility to azoles secondary to an overexpression of efflux pumps [125] and a reduced susceptibility to echinocandins through mutations in the FKS1 or FKS2 genes [126].
Antifungal resistance in IAC is due to poor tissue diffusion
Studies focusing on IAC are scarce and mostly come from animal model. Zhao et al. [105] reported a poor diffusion within the lesion during the first 6h after a single dose in a murine model of IAC. These results highlighted, especially during the first day of therapy, insufficient drug exposure which potentially promotes development of antifungal resistance. A second study from Cheng et al. [127] used a murine model of IAC to address the virulence of C. glabrata. They reported that if the inoculum was not controlled at the onset of infection, it led to a high occurrence of candidemia with 100% of mice death. Then, if C. glabrata was not eradicate, abscess formation could occur, which persisted in most of the mice for at least 28 days. This study describes the dynamic process of IAC depending on the size of the inoculum and highlights the importance of adequate antifungal exposure at the onset of IAC to avoid candidemia, and thereafter to avoid abscess and/or tertiary peritonitis where antifungal diffusion remains challenging. One study has evaluated the prevalence of antifungal resistance among patients with IAC and prior echinocandin exposure. FKS mutant Candida isolates were identified in 24% (6/25) of patients [128], with the presence of FKS mutations associated with prolonged echinocandin exposure (P = 0.01) and therapeutic failures despite source control interventions (100%). The authors suggest that IAC acts as a hidden reservoir for the emergence of echinocandin-resistant Candida. These observations were supported by the ongoing challenge of insufficient drug penetration during therapy for IAC supported by animal studies and clinical studies.
The C. auris threat
In the last decade, an increased number of outbreaks involving C. auris has been reported worldwide [129, 130]. C. auris has reduced susceptibility to the predominantly used antifungals (i.e. azoles, echinocandins, amphotericin B) [131, 132]. Current microbiological data reported that 90% of C. auris strains demonstrated resistance to fluconazole, 30% to amphotericin B, and 5% to echinocandins [133]. Rezafungin and ibrexafungerp demonstrated better susceptibility and a reduction in mortality using an animal C. auris candidemia model [131]. Thus, considering the risk suboptimal antifungal concentrations during IAC and the ability to develop resistance to antifungal of C. auris, the choice of antifungal and dose are of paramount importance in case of IAC caused by this difficult-to-treat pathogen.
Which role for the immune response?
Lastly, the role of immunological processes during IAC must be considered when determining antifungal PK/PD targets, as both innate and adaptive immunity are important for defence against Candida [134]. Neutrophils and macrophages have an important role in Candida recognition and activation of the immune response thereafter. As mentioned above, abdominal surgery induced-trauma provides peri- and post-operative inflammation followed by immunosuppression [22]. Impairment of the immune response during this period can promote Candida growth and exacerbate virulence [135, 136]. Besides, Candida is frequently encountered in post-operative peritonitis [137]. As it has been suggested to aim for higher PK/PD targets for antibiotics in the case of neutropenia [138], we wonder if in post-operative peritonitis, a more aggressive antifungal PK/PD target may need to be considered. Thus, studies including immunosuppressed critically ill patients with IAC exploring the relationship between antifungal exposure and clinical outcomes are also warranted.
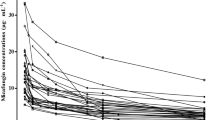
Figure 1 summarises the PK and PD considerations when treating critically ill patients with IAC requiring surgery.
PK/PD alterations during intra-abdominal candidiasis. PK: pharmacokinetic; PD: pharmacodynamic; Vd: volume of distribution; CL: clearance; ICU: intensive care unit; ATF: antifungal; TDM: therapeutic drug monitoring. Figure 1 is split twice: vertically, where left side represents the per-operative phase and right side the post-operative period, and horizontally, where the upper case described the sources of pharmacokinetic alterations, and the lower case, the sources of pharmacodynamic alterations. In the operating room, sources of PK variability are driven by the sepsis/shock, the resuscitation (fluid resuscitation and catecholamines), the anaesthesia, and inflammation caused by the surgical trauma. Together they contribute to a high risk of suboptimal antifungal concentrations by increase in volume of distribution and clearance in both the plasma and the peritoneum. From a pharmacodynamic perspective, before the source control is performed by the surgeon, high inoculum potentially protect by Candida biofilm and low tissue penetration could promote antifungal resistance. Thus, increased PK/PD target and high dose of antifungal are required. During the post-operative period, the source control is supposed to be achieved and thereby the sepsis/shock should be less important. However, organ failures caused by the abdominal sepsis could occur, and provide the need for extracorporeal support such as renal replacement therapy or ECMO. The presence of surgical drains could increase drug clearance. Therefore, antifungal concentrations are highly unpredictable, from low to high concentration. From a pharmacodynamic perspective, source control has been performed but an immunoparalysis could be present and candidemia and/or abscess/tertiary peritonitis could occur. Therefore, therapeutic drug monitoring of antifungal should be considered
Lessons learned from PK/PD studies conducted in critically ill patients with IAC
Table 3 provides a summary of retrieved PK/PD studies which have focused on the use of antifungal during IAC. Details regarding study selection are provided in the Additional file 1 with the ClinPK statement checklist [139] for each included study (Additional file 1: Table S2). Overall, the studies fulfilled more than 80% of PK analysis checklist items (namely, use of valid quantitative bioanalytical methods, description of the PK modelling methods and software used, and adequate detail of the PK analysis performed). The main weakness across all studies was related to patient selection and follow-up from a clinical perspective.
Population consideration
All study investigators acknowledged the small size of their cohorts (between 3 and 31 patients) and highlighted a high inter-subject variability. Moreover, the case-mix of patients was mostly composed of secondary peritonitis, with IAC suspected rather than confirmed in most cases. Thus, the impact of PK/PD target attainment on mortality cannot be addressed due to the small sample sizes and the low number of confirmed cases of IAC. Echinocandin is the most evaluated antifungal class in IAC. Only one case-series addressed the PK of fluconazole in abdominal samples, in a non-ICU population.
Laboratory consideration
In all studies, only the total concentration was measured. However, from a tissue diffusion perspective, the unbound concentration should be assessed in further studies, especially in critically ill patients because of a high prevalence of hypoalbuminemia and marked fluctuations in serum albumin concentrations during acute illness [140]. Regarding peritoneal samples, most studies obtained samples from in situ abdominal drains and acknowledged less data compared to blood samples given these drains were usually removed after 72 h post-operatively. Therefore, peritoneal fluid samples obtained intra-operatively would allow for more accurate PK data describing antifungal abdominal diffusion.
Clinical course of IAC consideration
All studies analysed the PK/PD targets based on antifungal concentrations obtained from the post-operative period, often two to three days after surgery to evaluate steady-state concentrations. In our opinion, except perhaps for tertiary peritonitis (poorly studied thus far), the post-operative period has lower impact on mortality compared to the surgical period. Indeed, mortality increases with delay in source control and commencement of antifungal therapy [4]. Thus, if a PK/PD study aims to evaluate the impact of PK/PD target attainment on mortality, intra-operative sampling must be considered because: (i) this is the phase where inoculum is potentially the highest, (ii) the PK alterations from sepsis, surgery, and resuscitation therapeutics are maximized, and (iii) source control is ongoing.
However, there is still a risk of unpredictable antifungal concentrations during the post-operative period. Indeed, because of all other sources of PK variability in critically ill patients such as renal failure or extracorporeal support, the risk of suboptimal exposure can persist throughout the course of therapy [19, 141]. Therefore, in cases of either candidemia, tertiary peritonitis or inadequate source control, ensuring optimal antifungal exposure is crucial, knowing that these situations require longer antifungal duration [142].
Further perspectives
Based on the PK and PD challenges noted, we believe that further clinical studies evaluating impact of antifungal PK/PD parameters on outcome such as mortality are warranted and of crucial importance, especially studies that sample during the peri-operative phase during surgical intervention. This observation implies that antifungal therapy should commence before surgery, which is not always the case because of the diagnostic difficulties associated with identifying IAC [143]. Indeed, in the AMARCAND-2 study, antifungal therapy was started after Candida documentation in 70% of the patients, thus noting that few patients received antifungal at the onset of IAC [88]. Performing PK/PD analysis during and after surgery would allow to describe important fluctuations in antifungal exposure, some of which may impact on patient outcomes. Certainly, the identification of critically ill patients with intra-abdominal infection who then develop IAC remains a challenge [144, 145]. The future consensus definition of IAC from the FUNDICU project [146] is eagerly awaited and would certainly help identifying the right population.
An additional difficulty when addressing clinical outcome such as mortality in critically ill patients with IAC is related to the Candida itself [147,148,149]. Although the presence of Candida in peritoneal samples is associated with poor outcomes [150], other studies have been inconsistent [151]. This may be due to whether the Candida isolated is a true pathogen responsible for mortality. Indeed, the pathogenicity of Candida has been questioned, with suggestion that it may be dependent on the clinical situation and/or underlying condition of the patient [152,153,154].
In the interim of obtaining more robust PK/PD data linked to patient outcomes, using antifungal TDM in critically ill patients with IAC, especially in cases with high prevalence of non-albicans species, should be advocated. In the absence of clear recommendations specifically for IAC in critically ill patients [52], and based on available PK/PD data [48, 57, 73, 74], we suggest trough concentrations between 10 and 20 mg/L for fluconazole, and 1 to 10 mg/L for echinocandins. Further studies aiming to evaluate these therapeutic ranges in critically ill patients are, however, required.
It is noteworthy that data regarding antifungal dose optimization using dosing software are scarce. In invasive candidiasis, only one study has been reported. Bayesian analysis using a limited sampling strategy has been evaluated for anidulafungin using data from 20 critically ill patients and showed reasonable prediction [69]. Given that use of TDM in combination with dosing software may become more common practice in the ICU, assessment of these dose optimization interventions is a future consideration.
Conclusion
Due to the specific pathophysiology and associated interventions, IAC must be considered differently compared to other forms of invasive candidiasis such as candidemia. High-quality PK/PD studies are required to better describe the rate of antifungal target attainment in both plasma and peritoneal fluid, during and after the surgery, and when the patient is transferred to the ICU. The lack of intra-operative data is a current weakness. Proposed PK/PD targets, derived mostly from animal models, have yet to be validated in the critically ill population. To study the impact of antifungal PK/PD target attainment on clinical outcomes, larger sample sizes and multicentre studies are needed. In the meantime, antifungal TDM in critically ill patients with IAC should be considered, especially in cases of high prevalence of non-albicans species or when fluconazole is prescribed. Regarding the interest in new antifungals, studies involving critically ill patients coupled with rigorous PK/PD analysis are warranted before a more widespread use.
Availability of data and materials
Not applicable.
Abbreviations
- AUC:
-
Area under the curve
- ECMO:
-
Extra-corporeal membrane oxygenation
- fAUC:
-
Area under the curve of the free (unbound) concentration
- IAC:
-
Intra-abdominal candidiasis
- ICU:
-
Intensive care unit
- L-AmB:
-
Liposomal amphotericin B
- PD:
-
Pharmacodynamic
- PK:
-
Pharmacokinetic
- RCT:
-
Randomized controlled trial
- RRT:
-
Renal replacement therapy
- TDM:
-
Therapeutic drug monitoring
- Vd:
-
Volume of distribution
References
Montravers P, Dupont H, Eggimann P. Intra-abdominal candidiasis: the guidelines—forgotten non-candidemic invasive candidiasis. Intens Care Med. 2013;39:2226–30. https://doi.org/10.1007/s00134-013-3134-2.
Bassetti M, Azoulay E, Kullberg B-J, Ruhnke M, Shoham S, Vazquez J, et al. EORTC/MSGERC definitions of invasive fungal diseases: summary of activities of the intensive care unit working group. Clin Infect Dis. 2021;72:S121–7. https://doi.org/10.1093/cid/ciaa1751.
Bassetti M, Vena A, Giacobbe DR, Trucchi C, Ansaldi F, Antonelli M, et al. Risk factors for intra-abdominal candidiasis in intensive care units: results from EUCANDICU study. Infect Dis Ther. 2022;11:827–40. https://doi.org/10.1007/s40121-021-00585-6.
Vergidis P, Clancy CJ, Shields RK, Park SY, Wildfeuer BN, Simmons RL, et al. Intra-abdominal candidiasis: the importance of early source control and antifungal treatment. PLoS ONE. 2016;11: e0153247. https://doi.org/10.1371/journal.pone.0153247.
Bassetti M, Giacobbe DR, Vena A, Trucchi C, Ansaldi F, Antonelli M, et al. Incidence and outcome of invasive candidiasis in intensive care units (ICUs) in Europe: results of the EUCANDICU project. Crit Care. 2019;23:219. https://doi.org/10.1186/s13054-019-2497-3.
Hoenigl M, Salmanton-García J, Egger M, Gangneux J-P, Bicanic T, Arikan-Akdagli S, et al. Guideline adherence and survival of patients with candidaemia in Europe: results from the ECMM Candida III multinational European observational cohort study. Lancet Infect Dis. 2023;23:751–61. https://doi.org/10.1016/S1473-3099(22)00872-6.
Peçanha-Pietrobom PM, Colombo AL. Mind the gaps: challenges in the clinical management of invasive candidiasis in critically ill patients. Curr Opin Infect Dis. 2020;33:441–8. https://doi.org/10.1097/QCO.0000000000000684.
Montravers P, Assadi M, Gouel-Cheron A. Priorities in peritonitis. Curr Opin Crit Care. 2021;27:201. https://doi.org/10.1097/MCC.0000000000000805.
Montravers P, Dupont H, Leone M, Constantin J-M, Mertes P-M, Société française d’anesthésie et de réanimation (Sfar), et al. Guidelines for management of intra-abdominal infections. Anaesth Crit Care Pain Med 2015;34:117–30. https://doi.org/10.1016/j.accpm.2015.03.005.
Pappas PG, Kauffman CA, Andes DR, Clancy CJ, Marr KA, Ostrosky-Zeichner L, et al. Clinical practice guideline for the management of candidiasis: 2016 update by the infectious diseases society of America. Clin Infect Dis. 2016;62:e1-50. https://doi.org/10.1093/cid/civ933.
Martin-Loeches I, Antonelli M, Cuenca-Estrella M, Dimopoulos G, Einav S, De Waele JJ, et al. ESICM/ESCMID task force on practical management of invasive candidiasis in critically ill patients. Intens Care Med. 2019;45:789–805. https://doi.org/10.1007/s00134-019-05599-w.
Mazuski JE, Tessier JM, May AK, Sawyer RG, Nadler EP, Rosengart MR, et al. The surgical infection society revised guidelines on the management of intra-abdominal infection. Surg Infect. 2017;18:1–76. https://doi.org/10.1089/sur.2016.261.
Pea F, Lewis RE. Overview of antifungal dosing in invasive candidiasis. J Antimicrob Chemother. 2018;73:i33-43. https://doi.org/10.1093/jac/dkx447.
Sinnollareddy MG, Roberts JA, Lipman J, Akova M, Bassetti M, De Waele JJ, et al. Pharmacokinetic variability and exposures of fluconazole, anidulafungin, and caspofungin in intensive care unit patients: data from multinational defining antibiotic levels in intensive care unit (DALI) patients study. Crit Care. 2015;19:33. https://doi.org/10.1186/s13054-015-0758-3.
Kullberg BJ, Arendrup MC. Invasive candidiasis. N Engl J Med. 2015;373:1445–56. https://doi.org/10.1056/NEJMra1315399.
Maseda E, Martín-Loeches I, Zaragoza R, Pemán J, Fortún J, Grau S, et al. Critical appraisal beyond clinical guidelines for intraabdominal candidiasis. Crit Care. 2023;27:382. https://doi.org/10.1186/s13054-023-04673-6.
Jacobs R, Wise RD, Myatchin I, Vanhonacker D, Minini A, Mekeirele M, et al. Fluid management, intra-abdominal hypertension and the abdominal compartment syndrome: a narrative review. Life. 2022;12:1390. https://doi.org/10.3390/life12091390.
Baracaldo-Santamaría D, Cala-Garcia JD, Medina-Rincón GJ, Rojas-Rodriguez LC, Calderon-Ospina C-A. Therapeutic drug monitoring of antifungal agents in critically Ill patients: is there a need for dose optimisation? Antibiotics. 2022;11:645. https://doi.org/10.3390/antibiotics11050645.
Roberts JA, Lipman J. Pharmacokinetic issues for antibiotics in the critically ill patient. Crit Care Med. 2009;37:840–51. https://doi.org/10.1097/CCM.0b013e3181961bff.
De Pascale G, Antonelli M, Deschepper M, Arvaniti K, Blot K, Brown BC, et al. Poor timing and failure of source control are risk factors for mortality in critically ill patients with secondary peritonitis. Intensive Care Med. 2022;48:1593–606. https://doi.org/10.1007/s00134-022-06883-y.
Zhao J, Zhang T, Deng Z, Han X, Ma T, Xie K. Evaluation of biomarkers from peritoneal fluid as predictors of severity for abdominal sepsis patients following emergency laparotomy. J Inflamm Res. 2023;16:809–26. https://doi.org/10.2147/JIR.S401428.
Hogan BV, Peter MB, Shenoy HG, Horgan K, Hughes TA. Surgery induced immunosuppression. Surgeon. 2011;9:38–43. https://doi.org/10.1016/j.surge.2010.07.011.
Shan C-X, Ni C, Qiu M, Jiang D-Z, Li M. Influence of laparoscopy vs laparotomy on bacterial translocation and systemic inflammatory responses in a porcine model with peritonitis. J Invest Surg. 2014;27:73–80. https://doi.org/10.3109/08941939.2013.837564.
Evans C, Galustian C, Kumar D, Hagger R, Melville DM, Bodman-Smith M, et al. Impact of surgery on immunologic function: comparison between minimally invasive techniques and conventional laparotomy for surgical resection of colorectal tumors. Am J Surg. 2009;197:238–45. https://doi.org/10.1016/j.amjsurg.2008.01.021.
van de Groep K, Verhoeff TL, Verboom DM, Bos LD, Schultz MJ, Bonten MJM, et al. Epidemiology and outcomes of source control procedures in critically ill patients with intra-abdominal infection. J Crit Care. 2019;52:258–64. https://doi.org/10.1016/j.jcrc.2019.02.029.
Skipworth RJE, Fearon KCH. Acute abdomen: peritonitis. Surgery. 2008;26:98–101. https://doi.org/10.1016/j.mpsur.2008.01.004.
Küllmar M, Saadat-Gilani K, Weiss R, Massoth C, Lagan A, Cortés MN, et al. Kinetic changes of plasma renin concentrations predict acute kidney injury in cardiac surgery patients. Am J Respir Crit Care Med. 2021;203:1119–26. https://doi.org/10.1164/rccm.202005-2050OC.
Kennedy JM, Van Riji AM. Effects of surgery on the pharmacokinetic parameters of drugs. Clin Pharmacokinet. 1998;35:293–312. https://doi.org/10.2165/00003088-199835040-00003.
Wiedermann CJ. Phases of fluid management and the roles of human albumin solution in perioperative and critically ill patients. Curr Med Res Opin. 2020;36:1961–73. https://doi.org/10.1080/03007995.2020.1840970.
Roberts JA, Bellomo R, Cotta MO, Koch BC, Lyster H, Ostermann M, et al. Machines that help machines to help patients: optimising antimicrobial dosing in patients receiving extracorporeal membrane oxygenation and renal replacement therapy using dosing software. Intens Care Med. 2022. https://doi.org/10.1007/s00134-022-06847-2.
Patel JS, Kooda K, Igneri LA. A narrative review of the impact of extracorporeal membrane oxygenation on the pharmacokinetics and pharmacodynamics of critical care therapies. Ann Pharmacother. 2022. https://doi.org/10.1177/10600280221126438.
Larsen PB, Liest S, Hannani D, Jørgensen HL, Sørensen LT, Jørgensen LN. Preoperative hypoalbuminemia predicts early mortality following open abdominal surgery in patients above 60 years of age. Scand J Surg. 2021;110:29–36. https://doi.org/10.1177/1457496919888598.
Adnan S, Paterson DL, Lipman J, Kumar S, Li J, Rudd M, et al. Pharmacokinetics of beta-lactam antibiotics in patients with intra-abdominal disease: a structured review. Surg Infect. 2012;13:9–17. https://doi.org/10.1089/sur.2011.046.
Adnan S, Li JX, Wallis SC, Rudd M, Jarrett P, Paterson DL, et al. Pharmacokinetics of meropenem and piperacillin in critically ill patients with indwelling surgical drains. Int J Antimicrob Agents. 2013;42:90–3. https://doi.org/10.1016/j.ijantimicag.2013.02.023.
Sinnollareddy M, Peake SL, Roberts MS, Lipman J, Roberts JA. Using pharmacokinetics and pharmacodynamics to optimise dosing of antifungal agents in critically ill patients: a systematic review. Int J Antimicrob Agents. 2012;39:1–10. https://doi.org/10.1016/j.ijantimicag.2011.07.013.
Sinnollareddy M, Peake SL, Roberts MS, Playford EG, Lipman J, Roberts JA. Pharmacokinetic evaluation of fluconazole in critically ill patients. Expert Opin Drug Metab Toxicol. 2011;7:1431–40. https://doi.org/10.1517/17425255.2011.615309.
Bienvenu AL, Pradat P, Matusik E, Piriou V, Rimmelé T, Parant F, et al. Suboptimal exposure to fluconazole in critically ill patients: pharmacokinetic analysis and determinants. Infect Dis Now. 2023;53: 104630. https://doi.org/10.1016/j.idnow.2022.10.002.
Cuesta I, Bielza C, Larrañaga P, Cuenca-Estrella M, Laguna F, Rodriguez-Pardo D, et al. Data mining validation of fluconazole breakpoints established by the European committee on antimicrobial susceptibility testing. Antimicrob Agents Chemother. 2009;53:2949–54. https://doi.org/10.1128/AAC.00081-09.
Rodríguez-Tudela JL, Almirante B, Rodríguez-Pardo D, Laguna F, Donnelly JP, Mouton JW, et al. Correlation of the MIC and dose/MIC ratio of fluconazole to the therapeutic response of patients with mucosal candidiasis and candidemia. Antimicrob Agents Chemother. 2007;51:3599–604. https://doi.org/10.1128/AAC.00296-07.
Abdul-Aziz MH, Alffenaar JWC, Bassetti M, Bracht H, Dimopoulos G, Marriott D, et al. Antimicrobial therapeutic drug monitoring in critically ill adult patients: a Position Paper. Intens Care Med. 2020;46:1127–53. https://doi.org/10.1007/s00134-020-06050-1.
De Bellis P, Bonfiglio M, Gerbi G, Bacigalupo P, Buscaglia G, Guido P, et al. High-dose fluconazole therapy in Intensive Care Unit. Minerva Anestesiol. 2003;69(145–52):153–7.
Sandaradura I, Marriott DJE, Day RO, Norris RLG, Pang E, Stocker SL, et al. Current fluconazole treatment regimens result in under-dosing of critically ill adults during early therapy. Eur J Clin Microbiol Infect Dis. 2021;40:1521–8. https://doi.org/10.1007/s10096-021-04201-w.
Chen L, van Rhee KP, Wasmann RE, Krekels EHJ, Wiezer MJ, van Dongen EPA, et al. Total bodyweight and sex both drive pharmacokinetic variability of fluconazole in obese adults. J Antimicrob Chemother. 2022;77:2217–26. https://doi.org/10.1093/jac/dkac160.
Alobaid AS, Wallis SC, Jarrett P, Starr T, Stuart J, Lassig-Smith M, et al. Effect of obesity on the population pharmacokinetics of fluconazole in critically Ill patients. Antimicrob Agents Chemother. 2016;60:6550–7. https://doi.org/10.1128/AAC.01088-16.
Muilwijk EW, de Lange DW, Schouten JA, Wasmann RE, Ter Heine R, Burger DM, et al. Suboptimal dosing of fluconazole in critically Ill patients: time to rethink dosing. Antimicrob Agents Chemother. 2020;64:e00984-e1020. https://doi.org/10.1128/AAC.00984-20.
Felton T, Troke PF, Hope WW. Tissue penetration of antifungal agents. Clin Microbiol Rev. 2014;27:68–88. https://doi.org/10.1128/CMR.00046-13.
Sinnollareddy MG, Roberts MS, Lipman J, Lassig-Smith M, Starr T, Robertson T, et al. In vivo microdialysis to determine subcutaneous interstitial fluid penetration and pharmacokinetics of fluconazole in intensive care unit patients with sepsis. Antimicrob Agents Chemother. 2016;60:827–32. https://doi.org/10.1128/AAC.02461-15.
Pea F, Righi E, Cojutti P, Carnelutti A, Baccarani U, Soardo G, et al. Intra-abdominal penetration and pharmacodynamic exposure to fluconazole in three liver transplant patients with deep-seated candidiasis. J Antimicrob Chemother. 2014;69:2585–6. https://doi.org/10.1093/jac/dku169.
Bozzette SA, Gordon RL, Yen A, Rinaldi M, Ito MK, Fierer J. Biliary concentrations of fluconazole in a patient with candidal cholecystitis: case report. Clin Infect Dis. 1992;15:701–3. https://doi.org/10.1093/clind/15.4.701.
Shrikhande S, Friess H, Issenegger C, Martignoni ME, Yong H, Gloor B, et al. Fluconazole penetration into the pancreas. Antimicrob Agents Chemother. 2000;44:2569–71. https://doi.org/10.1128/AAC.44.9.2569-2571.2000.
Jager NGL, van Hest RM, Lipman J, Roberts JA, Cotta MO. Antibiotic exposure at the site of infection: principles and assessment of tissue penetration. Expert Rev Clin Pharmacol. 2019;12:623–34. https://doi.org/10.1080/17512433.2019.1621161.
Gómez-López A. Antifungal therapeutic drug monitoring: focus on drugs without a clear recommendation. Clin Microbiol Infect. 2020;26:1481–7. https://doi.org/10.1016/j.cmi.2020.05.037.
Kably B, Launay M, Derobertmasure A, Lefeuvre S, Dannaoui E, Billaud EM. Antifungal drugs TDM: trends and update. Ther Drug Monit. 2022;44:166. https://doi.org/10.1097/FTD.0000000000000952.
Bellmann R, Smuszkiewicz P. Pharmacokinetics of antifungal drugs: practical implications for optimized treatment of patients. Infection. 2017;45:737–79. https://doi.org/10.1007/s15010-017-1042-z.
Barchiesi F, Spreghini E, Tomassetti S, Della Vittoria A, Arzeni D, Manso E, et al. Effects of caspofungin against Candida guilliermondii and Candida parapsilosis. Antimicrob Agents Chemother. 2006;50:2719–27. https://doi.org/10.1128/AAC.00111-06.
Kim HY, Baldelli S, Märtson A-G, Stocker S, Alffenaar J-W, Cattaneo D, et al. Therapeutic drug monitoring of the echinocandin antifungal agents: is there a role in clinical practice? a position statement of the anti-infective drugs committee of the international association of therapeutic drug monitoring and clinical toxicology. Ther Drug Monit. 2022;44:198–214. https://doi.org/10.1097/FTD.0000000000000931.
Garbez N, Mbatchi LC, Wallis SC, Muller L, Lipman J, Roberts JA, et al. Caspofungin population pharmacokinetic analysis in plasma and peritoneal fluid in septic patients with intra-abdominal infections: a prospective cohort study. Clin Pharmacokinet. 2022;61:673–86. https://doi.org/10.1007/s40262-021-01062-6.
Andes D, Diekema DJ, Pfaller MA, Bohrmuller J, Marchillo K, Lepak A. In vivo comparison of the pharmacodynamic targets for echinocandin drugs against candida species. Antimicrob Agents Chemother. 2010;54:2497–506. https://doi.org/10.1128/AAC.01584-09.
Thompson GR, Jenks JD, Baddley JW, Lewis JS, Egger M, Schwartz IS, et al. Fungal endocarditis: pathophysiology, epidemiology, clinical presentation, diagnosis, and management. Clin Microbiol Rev. 2023. https://doi.org/10.1128/cmr.00019-23.
Agrifoglio A, Cachafeiro L, Herrero E, Sánchez M, García de Lorenzo A. Are we near to the end of the standard dose of micafungin? Crit Care. 2018;22:149. https://doi.org/10.1186/s13054-018-2068-z.
Maseda E, Grau S, Luque S, Castillo-Mafla M-P, Suárez-de-la-Rica A, Montero-Feijoo A, et al. Population pharmacokinetics/pharmacodynamics of micafungin against Candida species in obese, critically ill, and morbidly obese critically ill patients. Crit Care. 2018;22:94. https://doi.org/10.1186/s13054-018-2019-8.
Wasmann RE, Ter Heine R, van Dongen EP, Burger DM, Lempers VJ, Knibbe CA, et al. Pharmacokinetics of anidulafungin in obese and normal-weight adults. Antimicrob Agents Chemother. 2018;62:e00063-e118. https://doi.org/10.1128/AAC.00063-18.
Brüggemann RJM, Middel-Baars V, de Lange DW, Colbers A, Girbes ARJ, Pickkers P, et al. Pharmacokinetics of anidulafungin in critically Ill intensive care unit patients with suspected or proven invasive fungal infections. Antimicrob Agents Chemother. 2017;61:e01894-e1916. https://doi.org/10.1128/AAC.01894-16.
Lempers VJ, Schouten JA, Hunfeld NG, Colbers A, van Leeuwen HJ, Burger DM, et al. Altered micafungin pharmacokinetics in intensive care unit patients. Antimicrob Agents Chemother. 2015;59:4403–9. https://doi.org/10.1128/AAC.00623-15.
Martial LC, Ter Heine R, Schouten JA, Hunfeld NG, van Leeuwen HJ, Verweij PE, et al. Population pharmacokinetic model and pharmacokinetic target attainment of micafungin in intensive care unit patients. Clin Pharmacokinet. 2017;56:1197–206. https://doi.org/10.1007/s40262-017-0509-5.
Bailly S, Gautier-Veyret E, Lê MP, Bouadma L, Andremont O, Neuville M, et al. Impact of loading dose of caspofungin in pharmacokinetic-pharmacodynamic target attainment for severe candidiasis infections in patients in intensive care units: the CASPOLOAD Study. Antimicrob Agents Chemother. 2020;64:e01545-e1620. https://doi.org/10.1128/AAC.01545-20.
Märtson A-G, van der Elst KCM, Veringa A, Zijlstra JG, Beishuizen A, van der Werf TS, et al. Caspofungin weight-based dosing supported by a population pharmacokinetic model in critically Ill patients. Antimicrob Agents Chemother. 2020;64:e00905-e920. https://doi.org/10.1128/AAC.00905-20.
Liu X, Liu D, Pan Y, Li Y. Pharmacokinetic/pharmacodynamics variability of echinocandins in critically ill patients: a systematic review and meta-analysis. J Clin Pharm Ther. 2020;45:1207–17. https://doi.org/10.1111/jcpt.13211.
van Wanrooy MJP, Proost JH, Rodgers MGG, Zijlstra JG, Uges DRA, Kosterink JGW, et al. Limited-sampling strategies for anidulafungin in critically ill patients. Antimicrob Agents Chemother. 2015;59:1177–81. https://doi.org/10.1128/AAC.03375-14.
Grau S, Luque S, Campillo N, Samsó E, Rodríguez U, García-Bernedo CA, et al. Plasma and peritoneal fluid population pharmacokinetics of micafungin in post-surgical patients with severe peritonitis. J Antimicrob Chemother. 2015;70:2854–61. https://doi.org/10.1093/jac/dkv173.
Dupont H, Massias L, Jung B, Ammenouche N, Montravers P. Pharmacokinetic study of anidulafungin in ICU patients with intra-abdominal candidiasis. J Antimicrob Chemother. 2017;72:1429–32. https://doi.org/10.1093/jac/dkw568.
Garbez N, Mbatchi L, Wallis SC, Muller L, Lipman J, Roberts JA, et al. Prospective cohort study of micafungin population pharmacokinetic analysis in plasma and peritoneal fluid in septic patients with intra-abdominal infections. Antimicrob Agent Chemother. 2021. https://doi.org/10.1128/aac.02307-20.10.1128/aac.02307-20.
Gioia F, Gomez-Lopez A, Alvarez ME, Gomez-García de la Pedrosa E, Martín-Davila P, Cuenca-Estrella M, et al. Pharmacokinetics of echinocandins in suspected candida peritonitis: a potential risk for resistance. Int J Infect Dis. 2020;101:24–8. https://doi.org/10.1016/j.ijid.2020.09.019.
Welte R, Oberacher H, Gasperetti T, Pfisterer H, Griesmacher A, Santner T, et al. Pharmacokinetics and antifungal activity of echinocandins in ascites fluid of critically Ill patients. Antimicrob Agents Chemother. 2021;65: e0256520. https://doi.org/10.1128/AAC.02565-20.
Pérez Civantos DV, Robles Marcos M, Azanza Perea JR, Pazos Pacheco C, García-Montoto Pérez F, Jerez G-C. Pharmacokinetics of anidulafungin in critically ill patients with Candida peritonitis. Int J Infect Dis. 2019;86:142–6. https://doi.org/10.1016/j.ijid.2019.07.008.
García-de-Lorenzo A, Luque S, Grau S, Agrifoglio A, Cachafeiro L, Herrero E, et al. Comparative population plasma and tissue pharmacokinetics of micafungin in critically Ill patients with severe burn injuries and patients with complicated intra-abdominal infection. Antimicrob Agents Chemother. 2016;60:5914–21. https://doi.org/10.1128/aac.00727-16.
Di Bonaventura G, Spedicato I, Picciani C, D’Antonio D, Piccolomini R. In vitro pharmacodynamic characteristics of amphotericin B, caspofungin, fluconazole, and voriconazole against bloodstream isolates of infrequent Candida species from patients with hematologic malignancies. Antimicrob Agents Chemother. 2004;48:4453–6. https://doi.org/10.1128/AAC.48.11.4453-4456.2004.
Maertens J, Pagano L, Azoulay E, Warris A. Liposomal amphotericin B-the present. J Antimicrob Chemother. 2022;77:11–20. https://doi.org/10.1093/jac/dkac352.
Van Daele R, Wauters J, Elkayal O, Dreesen E, Debaveye Y, Lagrou K, et al. Liposomal amphotericin B exposure in critically ill patients: a prospective pharmacokinetic study. Med Mycol. 2022;60:myac074. https://doi.org/10.1093/mmy/myac074.
Heinemann V, Bosse D, Jehn U, Kähny B, Wachholz K, Debus A, et al. Pharmacokinetics of liposomal amphotericin B (Ambisome) in critically ill patients. Antimicrob Agents Chemother. 1997;41:1275–80. https://doi.org/10.1128/AAC.41.6.1275.
Stone NR, Bicanic T, Salim R, Hope W. Liposomal Amphotericin B (AmBisome®): a review of the pharmacokinetics, pharmacodynamics, clinical experience and future directions. Drugs. 2016;76:485–500. https://doi.org/10.1007/s40265-016-0538-7.
Zhao Y, Seelhammer TG, Barreto EF, Wilson JW. Altered pharmacokinetics and dosing of liposomal amphotericin B and isavuconazole during extracorporeal membrane oxygenation. Pharmacotherapy. 2020;40:89–95. https://doi.org/10.1002/phar.2348.
Sato S, Kamata W, Fukaguchi K, Tsunoda S, Kamio T, Koyama H, et al. Successful treatment of invasive tracheobronchial pulmonary aspergillosis with venovenous extracorporeal membrane oxygenation and combined systemic, intratracheal instillation of liposomal amphotericin B: a case report. J Med Case Rep. 2022;16:470. https://doi.org/10.1186/s13256-022-03692-1.
Branick K, Taylor MJ, Trump MW, Wall GC. Apparent interference with extracorporeal membrane oxygenation by liposomal amphotericin B in a patient with disseminated blastomycosis receiving continuous renal replacement therapy. Am J Health Syst Pharm. 2019;76:810–3. https://doi.org/10.1093/ajhp/zxz054.
Ting MH, Spec A, Micek ST, Ritchie DJ, Krekel T. Evaluation of total body weight versus adjusted body weight liposomal amphotericin B dosing in obese patients. Antimicrob Agents Chemother. 2021;65: e0236620. https://doi.org/10.1128/AAC.02366-20.
Rinaldi M, Bartoletti M, Bonazzetti C, Caroccia N, Gatti M, Tazza B, et al. Tolerability of pulse high dose L-AmB as pre-emptive therapy in patients at high risk for intra-abdominal candidiasis: a phase 2 study (LAMBDA study). Int J Antimicrob Agents. 2023. https://doi.org/10.1016/j.ijantimicag.2023.106998.
Tortora F, Dei Giudici L, Simeoli R, Chiusolo F, Cairoli S, Bernaschi P, et al. Therapeutic drug monitoring of amphotericin-B in plasma and peritoneal fluid of pediatric patients after liver transplantation: a case series. Antibiotics. 2022;11:640. https://doi.org/10.3390/antibiotics11050640.
Leroy O, Bailly S, Gangneux J-P, Mira J-P, Devos P, Dupont H, et al. Systemic antifungal therapy for proven or suspected invasive candidiasis: the AmarCAND 2 study. Ann Intensive Care. 2016;6:2. https://doi.org/10.1186/s13613-015-0103-7.
Myrianthefs P, Markantonis SL, Evaggelopoulou P, Despotelis S, Evodia E, Panidis D, et al. Monitoring plasma voriconazole levels following intravenous administration in critically ill patients: an observational study. Int J Antimicrob Agents. 2010;35:468–72. https://doi.org/10.1016/j.ijantimicag.2009.12.021.
Troke PF, Hockey HP, Hope WW. Observational study of the clinical efficacy of voriconazole and its relationship to plasma concentrations in patients. Antimicrob Agents Chemother. 2011;55:4782–8. https://doi.org/10.1128/AAC.01083-10.
Weiler S, Zoller H, Graziadei I, Vogel W, Bellmann-Weiler R, Joannidis M, et al. Altered pharmacokinetics of voriconazole in a patient with liver cirrhosis. Antimicrob Agents Chemother. 2007;51:3459–60. https://doi.org/10.1128/AAC.00791-07.
Fuhrmann V, Schenk P, Jaeger W, Miksits M, Kneidinger N, Warszawska J, et al. Pharmacokinetics of voriconazole during continuous venovenous haemodiafiltration. J Antimicrob Chemother. 2007;60:1085–90. https://doi.org/10.1093/jac/dkm349.
Jeu L, Piacenti FJ, Lyakhovetskiy AG, Fung HB. Voriconazole. Clin Ther. 2003;25:1321–81. https://doi.org/10.1016/s0149-2918(03)80126-1.
Diller E, Krekel T, Spec A, Klaus J. Evaluation of total body weight versus adjusted body weight voriconazole dosing in obese patients. Antimicrob Agents Chemother. 2021;65: e0246020. https://doi.org/10.1128/AAC.02460-20.
Radej J, Krouzecky A, Stehlik P, Sykora R, Chvojka J, Karvunidis T, et al. Pharmacokinetic evaluation of voriconazole treatment in critically ill patients undergoing continuous venovenous hemofiltration. Ther Drug Monit. 2011;33:393–7. https://doi.org/10.1097/FTD.0b013e3182205d93.
Ruiz S, Papy E, Da Silva D, Nataf P, Massias L, Wolff M, et al. Potential voriconazole and caspofungin sequestration during extracorporeal membrane oxygenation. Intensive Care Med. 2009;35:183–4. https://doi.org/10.1007/s00134-008-1269-3.
Spriet I, Annaert P, Meersseman P, Hermans G, Meersseman W, Verbesselt R, et al. Pharmacokinetics of caspofungin and voriconazole in critically ill patients during extracorporeal membrane oxygenation. J Antimicrob Chemother. 2009;63:767–70. https://doi.org/10.1093/jac/dkp026.
Ronda M, Llop-Talaveron JM, Fuset M, Leiva E, Shaw E, Gumucio-Sanguino VD, et al. Voriconazole pharmacokinetics in critically Ill patients and extracorporeal membrane oxygenation support: a retrospective comparative case-control study. Antibiotics. 2023;12:1100. https://doi.org/10.3390/antibiotics12071100.
Lin XB, Hu XG, Tang ZX, Guo PH, Liu XM, Liang T, et al. Pharmacokinetics of Voriconazole in peritoneal fluid of critically Ill patients. Antimicrob Agents Chemother. 2023;67: e0172122. https://doi.org/10.1128/aac.01721-22.
Lamoth F. Novel therapeutic approaches to invasive candidiasis: considerations for the clinician. Infect Drug Resist. 2023;16:1087–97. https://doi.org/10.2147/IDR.S375625.
Thompson GR, Soriano A, Skoutelis A, Vazquez JA, Honore PM, Horcajada JP, et al. Rezafungin versus Caspofungin in a phase 2, randomized, double-blind study for the treatment of Candidemia and invasive candidiasis: the STRIVE trial. Clin Infect Dis. 2021;73:e3647–55. https://doi.org/10.1093/cid/ciaa1380.
Thompson GR, Soriano A, Cornely OA, Kullberg BJ, Kollef M, Vazquez J, et al. Rezafungin versus caspofungin for treatment of candidaemia and invasive candidiasis (ReSTORE): a multicentre, double-blind, double-dummy, randomised phase 3 trial. Lancet. 2023;401:49–59. https://doi.org/10.1016/S0140-6736(22)02324-8.
Spec A, Pullman J, Thompson GR, Powderly WG, Tobin EH, Vazquez J, et al. MSG-10: a phase 2 study of oral ibrexafungerp (SCY-078) following initial echinocandin therapy in non-neutropenic patients with invasive candidiasis. J Antimicrob Chemother. 2019;74:3056–62. https://doi.org/10.1093/jac/dkz277.
James KD, Laudeman CP, Malkar NB, Krishnan R, Polowy K. Structure-activity relationships of a series of Echinocandins and the discovery of CD101, a highly stable and soluble Echinocandin with distinctive pharmacokinetic properties. Antimicrob Agents Chemother. 2017;61:e01541-e1616. https://doi.org/10.1128/AAC.01541-16.
Zhao Y, Prideaux B, Nagasaki Y, Lee MH, Chen P-Y, Blanc L, et al. Unraveling drug penetration of Echinocandin antifungals at the site of infection in an intra-abdominal abscess model. Antimicrob Agents Chemother. 2017;61:e01009-e1017. https://doi.org/10.1128/AAC.01009-17.
Syed YY. Rezafungin: first approval. Drugs. 2023;83:833–40. https://doi.org/10.1007/s40265-023-01891-8.
Lepak AJ, Zhao M, Andes DR. Determination of pharmacodynamic target exposures for rezafungin against Candida tropicalis and Candida dubliniensis in the neutropenic mouse disseminated Candidiasis model. Antimicrob Agents Chemother. 2019;63:e01556-e1619. https://doi.org/10.1128/AAC.01556-19.
Tóth Z, Forgács L, Locke JB, Kardos G, Nagy F, Kovács R, et al. In vitro activity of rezafungin against common and rare Candida species and Saccharomyces cerevisiae. J Antimicrob Chemother. 2019;74:3505–10. https://doi.org/10.1093/jac/dkz390.
Pfaller MA, Messer SA, Rhomberg PR, Jones RN, Castanheira M. Activity of a long-acting echinocandin, CD101, determined using CLSI and EUCAST reference methods, against Candida and Aspergillus spp., including echinocandin-and azole-resistant isolates. J Antimicrob Chemother. 2016;71:2868–73. https://doi.org/10.1093/jac/dkw214.
Jang SM, Hough G, Mueller BA. Ex vivo rezafungin adsorption and clearance during continuous renal replacement therapy. Blood Purif. 2018;46:214–9. https://doi.org/10.1159/000489212.
Rubino CM, Flanagan S. Population pharmacokinetics of rezafungin in patients with fungal infections. Antimicrob Agents Chemother. 2021;65: e0084221. https://doi.org/10.1128/AAC.00842-21.
Díaz-García J, Machado M, Alcalá L, Reigadas E, Sánchez-Carrillo C, Pérez-Ayala A, et al. Antifungal resistance in Candida spp. within the intra-abdominal cavity: study of resistance acquisition in patients with serial isolates. Clin Microbiol Infect. 2023;S1198–743(23):00404. https://doi.org/10.1016/j.cmi.2023.08.021.
Ordaya EE, Clement J, Vergidis P. The role of novel antifungals in the management of Candidiasis: a clinical perspective. Mycopathologia. 2023. https://doi.org/10.1007/s11046-023-00759-5.
Wiederhold NP. Pharmacodynamics, mechanisms of action and resistance, and spectrum of activity of new antifungal agents. J Fungi. 2022;8:857. https://doi.org/10.3390/jof8080857.
Jiménez-Ortigosa C, Perez WB, Angulo D, Borroto-Esoda K, Perlin DS. De Novo acquisition of resistance to SCY-078 in Candida glabrata involves FKS mutations that both overlap and are distinct from those conferring Echinocandin resistance. Antimicrob Agents Chemother. 2017;61:e00833-e917. https://doi.org/10.1128/AAC.00833-17.
Angulo DA, Alexander B, Rautemaa-Richardson R, Alastruey-Izquierdo A, Hoenigl M, Ibrahim AS, et al. Ibrexafungerp, a novel triterpenoid antifungal in development for the treatment of mold infections. J Fungi. 2022;8:1121. https://doi.org/10.3390/jof8111121.
Jallow S, Govender NP. Ibrexafungerp: a first-in-class oral triterpenoid glucan synthase inhibitor. J Fungi. 2021;7:163. https://doi.org/10.3390/jof7030163.
Lepak AJ, Marchillo K, Andes DR. Pharmacodynamic target evaluation of a novel oral glucan synthase inhibitor, SCY-078 (MK-3118), using an in vivo murine invasive candidiasis model. Antimicrob Agents Chemother. 2015;59:1265–72. https://doi.org/10.1128/AAC.04445-14.
Ghannoum M, Arendrup MC, Chaturvedi VP, Lockhart SR, McCormick TS, Chaturvedi S, et al. Ibrexafungerp: a novel oral triterpenoid antifungal in development for the treatment of candida auris infections. Antibiotics. 2020;9:539. https://doi.org/10.3390/antibiotics9090539.
Lee A, Prideaux B, Zimmerman M, Carter C, Barat S, Angulo D, et al. Penetration of Ibrexafungerp (Formerly SCY-078) at the site of infection in an intra-abdominal candidiasis mouse model. Antimicrob Agents Chemother. 2020;64:e02268-e2319. https://doi.org/10.1128/AAC.02268-19.
Fournier P, Schwebel C, Maubon D, Vesin A, Lebeau B, Foroni L, et al. Antifungal use influences Candida species distribution and susceptibility in the intensive care unit. J Antimicrob Chemother. 2011;66:2880–6. https://doi.org/10.1093/jac/dkr394.
Bailly S, Maubon D, Fournier P, Pelloux H, Schwebel C, Chapuis C, et al. Impact of antifungal prescription on relative distribution and susceptibility of Candida spp.—Trends over 10 years. J Infect. 2016;72:103–11. https://doi.org/10.1016/j.jinf.2015.09.041.
Pristov KE, Ghannoum MA. Resistance of Candida to azoles and echinocandins worldwide. Clin Microbiol Infect. 2019;25:792–8. https://doi.org/10.1016/j.cmi.2019.03.028.
Tobudic S, Kratzer C, Lassnigg A, Presterl E. Antifungal susceptibility of Candida albicans in biofilms. Mycoses. 2012;55:199–204. https://doi.org/10.1111/j.1439-0507.2011.02076.x.
Sanguinetti M, Posteraro B, Lass-Flörl C. Antifungal drug resistance among Candida species: mechanisms and clinical impact. Mycoses. 2015;58(Suppl 2):2–13. https://doi.org/10.1111/myc.12330.
Alexander BD, Johnson MD, Pfeiffer CD, Jiménez-Ortigosa C, Catania J, Booker R, et al. Increasing echinocandin resistance in Candida glabrata: clinical failure correlates with presence of FKS mutations and elevated minimum inhibitory concentrations. Clin Infect Dis. 2013;56:1724–32. https://doi.org/10.1093/cid/cit136.
Cheng S, Clancy CJ, Hartman DJ, Hao B, Nguyen MH. Candida glabrata intra-abdominal candidiasis is characterized by persistence within the peritoneal cavity and abscesses. Infect Immun. 2014;82:3015–22. https://doi.org/10.1128/IAI.00062-14.
Shields RK, Nguyen MH, Press EG, Clancy CJ. Abdominal Candidiasis is a hidden reservoir of echinocandin resistance. Antimicrob Agents Chemother. 2014;58:7601–5. https://doi.org/10.1128/AAC.04134-14.
Benedict K, Forsberg K, Gold JAW, Baggs J, Lyman M. Candida auris-associated hospitalizations, United States, 2017–2022. Emerg Infect Dis. 2023;29:1485–7. https://doi.org/10.3201/eid2907.230540.
Kohlenberg A, Monnet DL, Plachouras D. Candida auris survey collaborative group, Candida auris survey collaborative group includes the following national experts. Increasing number of cases and outbreaks caused by Candida auris in the EU/EEA. Euro Surveill. 2022;27:2200846. https://doi.org/10.2807/1560-7917.ES.2022.27.46.2200846.
de Treviño-Rangel RJ, González GM, Montoya AM, Rojas OC, Elizondo-Zertuche M, Álvarez-Villalobos NA. Recent antifungal pipeline developments against Candida auris: a systematic review. J Fungi. 2022;8:1144. https://doi.org/10.3390/jof8111144.
de Cássia Orlandi Sardi J, Silva DR, Soares Mendes-Giannini MJ, Rosalen PL. Candida auris: epidemiology, risk factors, virulence, resistance, and therapeutic options. Microb Pathog. 2018;125:116–21. https://doi.org/10.1016/j.micpath.2018.09.014.
Chaabane F, Graf A, Jequier L, Coste AT. Review on antifungal resistance mechanisms in the emerging pathogen Candida auris. Front Microbiol. 2019;10:2788. https://doi.org/10.3389/fmicb.2019.02788.
Netea MG, Joosten LAB, van der Meer JWM, Kullberg B-J, van de Veerdonk FL. Immune defence against Candida fungal infections. Nat Rev Immunol. 2015;15:630–42. https://doi.org/10.1038/nri3897.
Fried E, Weissman C, Sprung C. Postoperative sepsis. Curr Opin Crit Care. 2011;17:396–401. https://doi.org/10.1097/MCC.0b013e328348bee2.
van Till JWO, van Veen SQ, van Ruler O, Lamme B, Gouma DJ, Boermeester MA. The innate immune response to secondary peritonitis. Shock. 2007;28:504–17. https://doi.org/10.1097/shk.0b013e318063e6ca.
Bassetti M, Eckmann C, Giacobbe DR, Sartelli M, Montravers P. Post-operative abdominal infections: epidemiology, operational definitions, and outcomes. Intensive Care Med. 2020;46:163–72. https://doi.org/10.1007/s00134-019-05841-5.
Guo B, Abdelraouf K, Ledesma KR, Chang K-T, Nikolaou M, Tam VH. Quantitative impact of neutrophils on bacterial clearance in a murine pneumonia model. Antimicrob Agents Chemother. 2011;55:4601–5. https://doi.org/10.1128/AAC.00508-11.
Kanji S, Hayes M, Ling A, Shamseer L, Chant C, Edwards DJ, et al. Reporting guidelines for clinical pharmacokinetic studies: the ClinPK statement. Clin Pharmacokinet. 2015;54:783–95. https://doi.org/10.1007/s40262-015-0236-8.
Ulldemolins M, Roberts JA, Rello J, Paterson DL, Lipman J. The effects of hypoalbuminaemia on optimizing antibacterial dosing in critically ill patients. Clin Pharmacokinet. 2011;50:99–110. https://doi.org/10.2165/11539220-000000000-00000.
Novy E, Martinière H, Roger C. The current status and future perspectives of beta-lactam therapeutic drug monitoring in critically Ill patients. Antibiotics. 2023;12:681. https://doi.org/10.3390/antibiotics12040681.
Bassetti M, Giacobbe DR, Berruti M, Del Puente F, Vena A. Adequate duration of therapy in severe fungal infections. Curr Opin Crit Care. 2020;26:466–72. https://doi.org/10.1097/MCC.0000000000000758.
Clancy CJ, Nguyen MH. Non-culture diagnostics for invasive candidiasis: promise and unintended consequences. J Fungi. 2018;4:27. https://doi.org/10.3390/jof4010027.
Soulountsi V, Schizodimos T, Kotoulas SC. Deciphering the epidemiology of invasive candidiasis in the intensive care unit: is it possible? Infection. 2021;49:1107–31. https://doi.org/10.1007/s15010-021-01640-7.
Montravers P, Blot S, Dimopoulos G, Eckmann C, Eggimann P, Guirao X, et al. Therapeutic management of peritonitis: a comprehensive guide for intensivists. Intens Care Med. 2016;42:1234–47. https://doi.org/10.1007/s00134-016-4307-6.
Bassetti M, Scudeller L, Giacobbe DR, Lamoth F, Righi E, Zuccaro V, et al. Developing definitions for invasive fungal diseases in critically ill adult patients in intensive care units. Protocol of the FUNgal infections Definitions in ICU patients (FUNDICU) project. Mycoses. 2019;62:310–9. https://doi.org/10.1111/myc.12869.
Rex JH. Candida in the peritoneum: passenger or pathogen? Crit Care Med. 2006;34:902–3. https://doi.org/10.1097/01.CCM.0000202129.19154.64.
Montravers P, Leroy O, Eckmann C. Intra-abdominal candidiasis: it’s still a long way to get unquestionable data. Intens Care Med. 2015;41:1682–4. https://doi.org/10.1007/s00134-015-3894-y.
Novy E, Esposito M, Birckener J, Germain A, Losser M-R, Machouart M-C, et al. Reappraisal of intra-abdominal candidiasis: insights from peritoneal fluid analysis. Intens Care Med Exp. 2023;11:67. https://doi.org/10.1186/s40635-023-00552-0.
Montravers P, Dupont H, Gauzit R, Veber B, Auboyer C, Blin P, et al. Candida as a risk factor for mortality in peritonitis. Crit Care Med. 2006;34:646–52. https://doi.org/10.1097/01.CCM.0000201889.39443.D2.
Sartelli M, Coccolini F, Kluger Y, Agastra E, Abu-Zidan FM, Abbas AES, et al. WSES/GAIS/SIS-E/WSIS/AAST global clinical pathways for patients with intra-abdominal infections. World J Emerg Surg. 2021;16:49. https://doi.org/10.1186/s13017-021-00387-8.
Krüger W, Vielreicher S, Kapitan M, Jacobsen ID, Niemiec MJ. Fungal-bacterial interactions in health and disease. Pathogens. 2019;8:70. https://doi.org/10.3390/pathogens8020070.
Desai JV, van de Veerdonk FL, Lionakis MS. Understanding the role of host immune responses in invasive candidiasis. Intensive Care Med. 2018;44:1310–4. https://doi.org/10.1007/s00134-017-4988-5.
Menz J, Hundt L, Schulze T, Schmoeckel K, Menges P, Domanska G. Increased mortality and altered local immune response in secondary peritonitis after previous visceral operations in mice. Sci Rep. 2021;11:16175. https://doi.org/10.1038/s41598-021-95592-5.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
EN: Conceptualization, Investigation, Visualization, Writing-original draft. CR: Conceptualization, Writing—review & editing. JAR: Writing—review & editing, Supervision, funding acquisition. MOC: Conceptualization, Investigation, Visualization, Writing-original draft, Supervision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Not applicable.
Competing interest
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. Supplementary material S1: Methodology of the literature review for pharmacokinetic studies evaluating antifungals in IAC. Supplementary material S2: ClinPK checklist applied to evaluated pharmacokinetic studies.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Novy, E., Roger, C., Roberts, J.A. et al. Pharmacokinetic and pharmacodynamic considerations for antifungal therapy optimisation in the treatment of intra-abdominal candidiasis. Crit Care 27, 449 (2023). https://doi.org/10.1186/s13054-023-04742-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-023-04742-w