Abstract
Background
Invasive pulmonary Aspergillus and invasive bronchial aspergillosis is a life-threatening opportunistic fungal infection that predominantly affects immunocompromised hosts. A case series and review found that the mortality rate of invasive bronchial aspergillosis is high, at about 40%, and 23.7% of invasive bronchial aspergillosis patients require mechanical ventilator management. There are few reports of life-saving cases with venovenous extracorporeal membrane oxygenation as rescue therapy in invasive pulmonary Aspergillus and invasive bronchial aspergillosis. Here, we report a case of invasive bronchial aspergillosis and invasive pulmonary Aspergillus that was successfully treated with venovenous extracorporeal membrane oxygenation, and combined systemic and intratracheal instillation of liposomal amphotericin B.
Case presentation
We present the case of a 61-year-old Japanese man with invasive tracheobronchial-pulmonary aspergillosis while receiving chemotherapy for malignant lymphoma. Bronchoscopy revealed trachea covered with pseudomembranous necrotizing tissue, the culture revealed Aspergillus fumigatus, and the histological findings of pseudomembranous revealed fungal hyphae. The patient required venovenous extracorporeal membrane oxygenation because of respiratory failure for atelectasis and obstructive pneumoniae. While continuing systemic administration of liposomal amphotericin B, intratracheal instillation liposomal amphotericin B was performed by bronchoscopy three times a week. Although the respiratory conditions improved and the patient was discontinued on venovenous extracorporeal membrane oxygenation, he ultimately died of recurrence of malignant lymphoma.
Conclusion
Intratracheal instillation of liposomal amphotericin B is safe, and liposomal amphotericin B instillation allowed a targeted high local drug concentration, which led to improvement in the invasive bronchial aspergillosis. In addition, since the patient was supported with venovenous extracorporeal membrane oxygenation, we were able to perform safe bronchoscopic debridement of airway lesions and intratracheal instillation of liposomal amphotericin B.
Similar content being viewed by others
Introduction
Invasive pulmonary Aspergillus (IPA) is a life-threatening opportunistic fungal infection that predominantly affects immunocompromised hosts [1]. Invasive bronchial aspergillosis (ITBA) is rare, accounting for 7% of IPA cases [2]. ITBA is an unusual form of IPA; in most cases, it is likely to be associated with IPA infiltration into the central airways [2,3,4]. In a case series and review, the mortality rate of ITBA is found to be high at about 40%, and 23.7% of ITBA patients require mechanical ventilator management [5]. However, to our knowledge, there are few reports of life-saving cases with venovenous extracorporeal membrane oxygenation (VV-ECMO) as rescue therapy in IPA and ITBA.
As per the proposal of the Infectious Disease Society of America (IDSA) guidelines in 2016 for Aspergillus infections, treatment with a mold-active triazole or intravenous liposomal amphotericin B (L-AmB) and bronchoscopic debridement of airway lesions in selected cases is recommended for ITBA, and especially for lung transplant recipients, adjunctive inhaled amphotericin (AmB) in the setting of ITBA is recommended [1], but as far as we have been able to determine, there were been no report of intratracheal instillation of L-AmB for ITBA.
Here, we report a case of ITBA and IPA that was successfully treated with VV-ECMO, and combined systemic and intratracheal instillation of L-AmB.
Case presentation
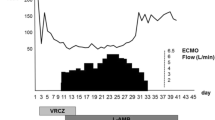
A 61-year-old Japanese man who had no significant medical, family, or psycho–social history was admitted with a 2-week history of fever, whole-body lymph node swelling, and abdominal swelling caused by hepatosplenomegaly. He was diagnosed with peripheral T-cell lymphoma, not otherwise specified (PTCL-NOS), by histopathological analysis of the lymph nodes. On admission, his laboratory data showed pancytopenia, hyperbilirubinemia, acute kidney injury (AKI), and disseminated intravascular coagulation (DIC) (Table 1). Bone marrow aspiration revealed proliferating hemophagocytosis and lymphocytes, and we diagnosed the patient with lymphoma associated with hemophagocytic lymphoma (LAHS). The day after he was admitted to our hospital, he was treated with etoposide, prednisone, vincristine, cyclophosphamide, doxorubicin (EPOCH) chemotherapy. He responded to the chemotherapy; on day 9 after admission, DIC, hyperbilirubinemia, AKI, and hepatosplenomegaly improved. However, the period of bone marrow suppression from day 9 to day 19, lasted for 11 days, and he developed febrile neutropenia (FN). From day 9 after admission, he was treated for FN with meropenem 6 g/day and micafungin 100 mg/day, and was administered granulocyte colony-stimulating factor (G-CSF). His blood cultures were negative. On day 10, computed tomography of the chest revealed bilateral diffuse infiltration shadow of the lungs, and due to progressive respiratory failure, he required noninvasive positive pressure ventilation (Fig. 1). However, on day 15, type 2 respiratory failure progressed. The findings from a blood gas test were as follows; pH 7.18, PaO2 77.6 mmHg, PaCO2 72.3 mmHg, \({\text{HCO}}_{3}^{ - }\) 26.8 mmol/L, and PaO2 to FiO2 (P/F) ratio 110. He underwent tracheal intubation for mechanical ventilation. Bronchoscopic findings revealed a widespread pseudomembranous necrotizing tissue formation covering the trachea and the bronchi, and numerous filamentous fungal hyphae infiltration were revealed in the pathologic examination (Fig. 2a–c). In addition, the β-d-glucan level was significantly increased to 1160 pg/mL, and the Aspergillus galactomannan antigen level [on enzyme-linked immunosorbent assay(ELISA)] was > 5.0. Aspergillus fumigatus was isolated from a pseudomembrane culture. We started L-AmB at 3 mg/kg/day. After intubation, he developed AKI with worsening of his general condition; therefore, we started continuous renal replacement therapy (CRRT). We performed daily bronchoscopy for pseudomembrane and necrotic tissue removal to release atelectasis. However, he was placed under deep sedation and fully controlled ventilation, and type 2 respiratory failure was worsened for atelectasis and obstructive pneumoniae. The findings from a blood gas test were as follows; pH 7.141, PaO2 67.9 mmHg, PaCO2 67.9 mmHg, \({\text{HCO}}_{3}^{ - }\) 22.9 mmol/L, (FiO2 0.8, PEEP 15 mmHg), and P/F ratio, 86. The patient showed severe hypoxemia (P/F = 86) under PEEP 15 mmHg, and severe respiratory acidosis with a Murray score of 4, so we initiated VV-ECMO as a reversible condition. Since severe respiratory failure occurred due to Aspergillus pseudomembrane that fills the tracheobronchial airway, systemic administration of only L-AmB was thought to be inadequate. After VV-ECMO, we continued to perform bronchoscopy three times a week for pseudomembrane removal and intratracheal instillation of aerosolized L-AmB. With the informed consent of his family, off-label use of L-AmB was administered via intratracheal instillation as a life saver. The L-AmB dose was referenced as an AmB attachment; 1 vial (50 mg) was dissolved in 10 mL of distilled water and 0.2–4 mL (1–20 mg) of the vial was added to it and further diluted (0.1–2 mg/mL of amphotericin B) in about 10 mL of distilled water. The L-AmB instillation allowed targeted high local drug concentration, which led to an improvement. In addition, we increased the systemic dose of the L-AmB to 6 mg/kg/day (the dose was increased to twice the normal dosage). Ten days after initiating VV-ECMO, a bleeding event from the gastric vestibular area was reported; however, VV-ECMO was successfully weaned after 14 days, with the improvement of lung function. Bronchoscopy revealed disappeared pseudomembrane necrotizing tissue (Fig. 2d). However, although ITBA improved, the patient developed an impairment of consciousness caused by central nervous system involvement of the lymphoma, at the same time, splenomegaly and enlarged inguinal lymph nodes were revealed again, soluble IL2 receptor was elevated (8527 U/mL), and uncontrollable metabolic acidosis had developed by lymphoma; the patient developed recurrent lymphoma and he died 50 days after admission.
Bronchoscopy revealed diffuse wide raised pseudomembrane necrotizing tissue at right upper lobe (a). Pseudomembrane obstruction from the trachea to the left main bronchus resulted in atelectasis (b). Pathological finding of pseudomembrane showed numerous filamentous fungal hyphae (Grocott–Gomori’s methenamine silver stain, ×100) (c). After systemic and intratracheal instillation of liposomal amphotericin B, pseudomembrane necrotizing tissue disappeared (d)
Discussion
Krenke et al. reported that ITBA in severely immunocompromised hosts with hematologic malignancies is characterized by a pseudomembranous overlying of the mucosal surface that is extensively involved in the lower airways. On the other hand, ITBA in those who have undergone a heart or lung transplant, is characterized by ulcerative types or plaque-like lesions in the bronchial walls [2]. In this case, the pseudomembrane necrotizing tissue caused severe respiratory distress that required ECMO support. Mario et al. reported that the overall in-hospital mortality rate of ITBA was 39.1%, with neutropenia [odds ratio (OR) 20.47; p < 0.001) and acute respiratory distress at presentation (OR 9.54; p = 0.002) being independent prognostic factors, indicating that the prognosis of ITBA in severely immunocompromised hosts with hematologic malignancies is worse than that of ITBA with other diseases [5]. In this case, severe neutropenia lasted for more than a week during bone marrow suppression following chemotherapy due to LAHS, and the patient had acute respiratory distress, and presented two poor prognostic factors. The IDSA guidelines recommend ITBA treatment with a mold-active triazole or intravenous L-AmB and bronchoscopic debridement of airway lesions in selected cases [1]. In this case, removal of atelectasis and obstructive pneumonia caused by pseudomembranes was considered necessary. However, bronchoscopic debridement of the the pseudomembrane may not be practicable due to high risk of hypoxia and progressive respiratory acidosis in cases of severe respiratory failure, even under mechanical ventilator control. Since the patient had severe respiratory failure, we started VV-ECMO management as rescue therapy, and then bronchoscopy could be performed safely and we were able to release atelectasis due to the pseudomembrane.
There is usually a delay in culture and pathology reports, and there is often a delay in fungal identification because some tests for species identification cross-react with other fungi. Also, in the present case, it took several days from the progression of type 2 respiratory failure to the diagnosis of fungal infection. Thair et al. reported that the cell-free DNA, which is collected for plasma next-generation sequencing (NGS) testing at the time of initial blood culture, identified a broad range of pathogens such as viruses, bacteria, and eukaryotic pathogens, which can provide valuable information to help clinicians better target antimicrobial therapy for septic patients [6]. It is hoped that NGS will become more accessible in clinical practice.
VV-ECMO is an effective treatment to support patients with severe respiratory failure who are unresponsive to conventional therapies [7]. Aspergillus spp. are identified more frequently (approximately 7%) in ECMO patients compared with patients without ECMO who are critically ill [8, 9]. However, to our knowledge, there is only one a single report of life-saving cases with VV-ECMO as rescue therapy in IPA [10], and there are no reports of cases with ECMO support in ITBA. In patients receiving VV-ECMO, drug pharmacokinetics may be significantly altered. Yanjun et al. reported a twofold increase in the standard total daily dose of both drugs to overcome low serum concentrations thought to be secondary to drug loss from ECMO circuit sequestration [11]. We upped the amount of L-AmB to 6 mg/kg/day, while the patient was treated with VV-ECMO and CRRT.
L-AmB is a unique lipid formulation of AmB. AmB binds to ergosterol in the fungal cell membrane, which leads to the formation of pores, ion leakage, and ultimately fungal cell death [12]. L-AmB is currently the most common type of AmB in distribution because intravenous AmB (Fungizone) is often complicated by nephrotoxicity [13]. The efficacy and safety of intratracheal inhaled L-AmB or AmB lipid complex for prophylaxis IPA have also been reported in hematopoietic stem cell transplant patients and in solid organ transplantation recipients [14,15,16,17], and efficacy and safety of intratracheal instillation of L-AmB was reported in treatment of endobronchial mucormycosis [18]. In addition, inhaling L-AmB for Aspergillus infection does not cause changes in the lipid content of the pulmonary surfactant [19]. Although only AmB has been approved for intratracheal inhalation and instillation, L-AmB is not indicated. This study was done in accordance with the institutional guidelines and the principles of the Declaration of Helsinki, which were ethically reviewed and approved by our hospital; informed consent was also obtained. This is the first report of an intratracheal instillation of L-AmB for ITBA. In this case, intratracheal instillation of aerosolized L-AmB by bronchoscopy was effective and safe for severe ITBA. At a time when AmB is not widely distributed, L-AmB is becoming more mainstream; therefore, intratracheal inhalation and instillation of LAmB will be even more necessary in the future to treat severe ITBA.
Conclusions
In this case, we successfully treated severe respiratory failure associated with ITBA with timely implementation of systemic and intratracheal instillation of aerosolized L-AmB and maximal supportive care, including VV-ECMO. The L-AmB instillation allowed a targeted high local drug concentration, which led to an improvement. Because an intratracheal instillation of L-AmB is safe and effective, it could be a treatment option for ITBA. In addition, since the patient was supported with VV-ECMO, we were able to safely perform bronchoscopic debridement of airway lesions and intratracheal instillation of L-AmB.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- IPA:
-
Invasive pulmonary Aspergillus
- ITBA:
-
Invasive bronchial aspergillosis
- VV-ECMO:
-
Venovenous extracorporeal membrane oxygenation
- IDSA:
-
Infectious Disease Society of America
- L-AmB:
-
Liposomal amphotericin B
- PTCL-NOS:
-
Peripheral T-cell lymphoma, not otherwise specified
- AKI:
-
Acute kidney injury
- DIC:
-
Disseminated intravascular coagulation
- FN:
-
Febrile neutropenia
- LAHS:
-
Lymphoma associated with hemophagocytic lymphoma
- P/F:
-
PaO2 to FiO2
- CRRT:
-
Continuous renal replacement therapy
- NGS:
-
Next-generation sequencing
References
Patterson TF, Tompson GR 3rd, Dwnning DW, et al. Practice guidelines for the diagnosis and management of Aspergillosis: 2016 Update by the Infections Disease Society of America. Clin Infect Dis. 2016;63:e1–60.
Krenke R, Grabczak EM. Tracheobronchial manifestations of Aspergillus infections. ScientificWorldJournal. 2011;11:2310–29.
Logan PM, Primack SL, Miller RR, Mullar NL. Invasive aspergillosis of the airways: radiographic, CT, and patholocig findings. Radiology. 1994;193:383–8.
Kemper CA, Hostetler JS, Follansbee SE, et al. Ulcerative and plaque-like tracheobronchitis due to infection with Aspergillus in patients with AIDS. Clin Infect Dis. 1993;17:344–52.
Fernández-Ruiz M, Silva JT, San-Juan R, et al. Aspergillus tracheobronchitis: report of 8 cases and review of the literature. Medicine (Baltimore). 2012;91:261–73.
Thair S, Seng H, Hollemon D, et al. The SEP-SEQ Trial: clinical validation of the Karius plasma next-generation sequencing test for pathogen detection in sepsis. Open Forum Infect Dis. 2017;4(Suppl 1):S735.
Mi MY, Matthay MA, Morris AH. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome. N Engl J Med. 2018;30:884–7.
Aubron C, Cheng AC, Pilcher D, et al. Infectious acquired by adults who receive extracorporeal membrane oxygenation risk factors and outcome. Infect Control Hosp Epidemiol. 2013;34:24–30.
Rodriguwz-Goncer I, Thomas S, Foden P, et al. Invasive pulmonary aspergillosis is associated with adverse clinical outcomes in critically ill patients receiving veno-venous extramembrane oxygenation. Eur J Clin Microbiol Infect Dis. 2018;37:1251–7.
Jenny Y, Abdurrahman H, Jeremy O. Invasive aspergillosis causing severe ARDS in an immunocompetent patient. Chest. 2019;156:A552.
Zhao Y, Seelhammer TG, Barreto EF, Wilson JW. Altered pharmacokinetics and dosing of liposomal amphotericin B and Isavuconazole during extracorporeal membrane oxygenation. Pharmacotherapy. 2020;40:89–95.
Stone NR, Bicanic T, Salim R, Hope W. Liposomal amphotericin B (AmBisome(®)): a review of the pharmacokinetics, pharmacodynamics. Clin Exp Future Direct Drugs. 2016;76:485–500.
Bates DW, Su L, Yu DT, et al. Correlates of acute renal failure in patients receiving parenteral amphotericin B. Kidney Int. 2001;60:1452–9.
Rijnders BJ, Cornelissen JJ, Slobbe L, et al. Aerosolized liposomal amphotericin B for the prevention of invasive pulmonary aspergillosis during prolonged neutropenia: a randomized, placebo-controlled trial. Clin Infect Dis. 2008;46:1401–8.
Minari A, Husni R, Avery RK, et al. The incidence of invasive aspergillosis among solid organ transplant recipient and implications for prophylaxis in lung transplants. Transpl Infect Dis. 2002;4:195–200.
Xia D, Sun WK, Tan MM, et al. Aerosolized amphotericin B as prophylaxis for invasive pulmonary aspergillosis: a meta-analysis. Int J Infect Dis. 2015;30:78–84.
Monforte V, Ussetti P, Lopez R, et al. Nebulized liposomal amphotericin B prophylaxis for Aspergillus infection in lung transplantation: pharmacokinetics and safety. J Heart Lung Transplant. 2009;28:170–5.
Nattusamy L, Kalai H, Hadda V, Mohan A, Guleria R, Madan K. Bronchoscopic instillation of liposomal amphotericin B in management of nonresponding endobronchial mucormycosis. Lung India. 2017;34:208–9.
Monforte V, Lopez-Sanchez A, Zurbano F, et al. Prophylaxis with nebulized liposomal amphotericin B for Aspergillus infection in lung transplant patients does not cause changes in the lipid content of pulmonary surfactant. J Heart Lung Transpl. 2013;32:313–9.
Acknowledgements
Not applicable.
Funding
There is no funding for this case report.
Author information
Authors and Affiliations
Contributions
SS performed the manuscript preparation. SS, WK, and ST were involved in the hematological treatment, and KF, TK and HK were involved in the critical care. HS performed the bronchoscopy. YT read and approved the final manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sato, S., Kamata, W., Fukaguchi, K. et al. Successful treatment of invasive tracheobronchial pulmonary aspergillosis with venovenous extracorporeal membrane oxygenation and combined systemic, intratracheal instillation of liposomal amphotericin B: a case report. J Med Case Reports 16, 470 (2022). https://doi.org/10.1186/s13256-022-03692-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-022-03692-1