Abstract
Background
Existing evidence concerning the management of traumatic brain injury (TBI) patients underlines the importance of appropriate treatment strategies in both prehospital and early in-hospital care. The objectives of this study were to analyze the current state of early TBI care in Austria with its physician-based emergency medical service. Subsequently, identified areas for improvement were transformed into treatment recommendations. The proposed changes were implemented in participating emergency medical services and hospitals and evaluated for their effect.
Methods
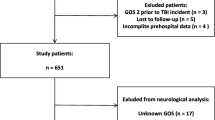
14 Austrian centers treating TBI patients participated in the study. Between 2009 and 2012 all patients with Glasgow Coma Scale score < 13 and/or AIS head > 2 within 48 h after the accident, were enrolled. Data were collected in 2 phases: in the first phase data of 408 patients were analyzed. Based on this, a set of recommendations expected to improve outcomes was developed by the study group and implemented in participating centers. Recommendations included time factors (transport to appropriate trauma center, avoiding secondary transfer), adequate treatment strategies (prehospital fluid and airway management, anesthesia, ventilation), monitoring (pulse oximetry and blood pressure monitoring in all patients, capnography in ventilated patients) for prehospital treatment. In the emergency department focus was on first CT scan as soon as possible, short interval between CT scan and surgery and early use of thrombelastometry to optimize coagulation. Following implementation of these recommendations, data on 325 patients were collected and analyzed in phase 2. Final analysis investigated the impact of the recommendations on patient outcomes.
Results
Patients in both data collection phases showed comparable demographic and injury severity characteristics. Treatment changes, especially in terms of fluid management, monitoring and normoventilation as well as thrombelastometry measurements were implemented successfully in phase 2, and led to significant improvement of patient outcomes. Hospital mortality was reduced from 31 % to 23 %. We found a lower rate of unfavorable outcomes, a significant increase in unexpected survivors and more patients with unexpected favorable outcomes as well.
Conclusions
The results of this study clearly demonstrate that the outcomes of TBI patients can be improved with appropriate early care.
Similar content being viewed by others
Background
Traumatic brain injury (TBI) is still a leading cause of death and disability [1, 2], despite concentrated efforts during the last decades towards the improvement of prevention [3–6] and care. Globally, the incidence of TBI is increasing, mainly due to growing use of motor vehicles in low- and middle-income countries [7, 8] and to the aging of the population in developed countries [9]. As a common condition with serious consequences for the patient, it is important that treatment strategies are optimized, and it is known that the outcome of TBI patients might be improved by the implementation of, and adherence to, effective treatment guidelines [10, 11].
Evidence-based guidelines for treatment of TBI have been developed by the Brain Trauma Foundation (BTF) in 1995, and have first been published in 1996 [12]. A previous Austrian study (2002–2005) investigated the effects of compliance with these guidelines on outcomes of patients with severe TBI. This study revealed that nearly all of the standards, most of the guidelines, and some of the options mentioned in the BTF document had been followed in the participating Austrian hospitals [13]. Compliance with the recommendation for rapid resuscitation to achieve normal blood pressure and adequate oxygenation significantly improved Intensive Care Unit (ICU) survival (odds ratio (OR) 1.25 (CI 95 % [confidence interval] 1.12–1.39), and the rate of favorable outcome OR = 1.18 (CI95% 1.04–1.34). Based on this study we concluded that improved early TBI care will have an important role in achieving overall improvements in outcomes.
In Austria early TBI care in the field is done by emergency physicians whose primary specialty is in (almost 50 %) anesthesiology; internal medicine specialists, general practitioners and (trauma) surgeons participate in Emergency Medical Services (EMS), too. Prior to this project, some recommendations on prehospital treatment of TBI patients had been available in Austria; notably the guidelines on prehospital management of patients with TBI published by the BTF [14] in 2002 were incorporated into most of these local recommendations. However, these recommendations did not include treatment in the emergency room, which is mainly done by the anesthesiologists. The development and implementation of recommendations that included prehospital as well as early hospital care seemed thus warranted as it was usually physicians who treated patients in the field and in the emergency room, too.
The goals of this project were:
-
▪ To analyze the “status quo” of early TBI care in Austria, using “comparative effectiveness” as the main tool
-
▪ To define areas where a change of prehospital and early hospital treatment would improve outcomes
-
▪ To develop a set of recommendations for practical changes that were most likely to improve outcomes
-
▪ To implement the proposed changes in practice
-
▪ To analyze the effects of these changes
Our hypothesis was that we would be able to define areas for improvement, and that the proposed changes would improve outcomes of patients with moderate or severe TBI.
Methods
The Austrian Ministry of Health and the Austrian Worker’s Compensation Board (AUVA) decided to fund the project, managed by the International Neurotrauma Research Organization (INRO). In 10/2008 all Austrian hospitals that treat patients with severe TBI were invited to participate in the study. 15 centers completed both data collection phases. One of them had very few patients in the second phase due to personnel issues. Therefore in final analyses we included 14 centers that participated in both phases and included patients according the inclusion criteria.
In Austria, out of approximately 120 hospitals treating any kind of traumatic brain injury (TBI) 30 hospitals treat more than 10 patients with severe TBI annually. According to patient load, hospitals participating in our study belong to this latter group.
In 11/2008, representatives from participating centers met in Vienna and founded the “Austrian Working Group on Improvement of Early TBI Care” (Working Group). The Working Group discussed and modified the study protocol prepared by INRO, and decided on a strategy for data collection. The Working Group made the following decisions used as inclusion criteria for the study:
-
To enroll patients with moderate and severe TBI; these were defined as having a Glasgow Coma Scale score (GCS) <13 [15] without sedation within 48 h of the accident and/or having an Abbreviated Injury Scale (AIS) score of the region “head” >2 [16].
-
To enroll all patients who were admitted during the 2 data collection phases. There were no age limits, and all patients fulfilling the defined criteria were to be enrolled, regardless whether they died in the trauma room or were transferred from another hospital.
-
In-hospital patient management was supposed to be based on the 2007 version of the BTF guidelines on TBI treatment, and was to continue as usual in each center.
-
To use of “off-line” documentation, in order to make this as simple as possible for the local study managers.
The study was approved by the ethical committees of all participating centers.
First data collection phase (Phase 1)
Between 5/2009 and 4/2010 a total of 408 patients were enrolled by 14 participating centers. In each center one or more persons (local study manager) were in charge of patient enrollment. Information was collected on patient folders containing paper forms (mostly multiple-choice check-boxes, some fields for numbers, dates and times) for demographic and trauma data, prehospital status and treatment, trauma room status and treatment, computed tomography (CT) findings, data on surgical procedures, intensive care unit (ICU) status and treatment, and hospital outcome. Copies of relevant records (prehospital, trauma room, and anesthesia records, first laboratory results, DVDs with CT scan data) were included in these folders. Prehospital data were collected from Emergency Medical Services (EMS) protocols; any missing information was obtained from EMS by the local study managers and transcribed into study patients’ files. Each patient or a close relative gave written informed consent to agree to the follow-up.
The patient folders were collected at regular intervals by the project manager (AB) from the local study managers who were responsible for data collection. The data were then entered into an online database, created by INRO for this project. The database consisted of electronic transcript of patient folders used for data collection, separate sheets on Patient & Trauma data, Trauma Room data, CT & Operation data, Intensive Care Unit data, Outcome data. The online database was used for continuous data storage. In most cases data were entered on site, and missing data were obtained directly from the local study managers. In some cases data were entered in the INRO office, and missing data were obtained via phone call or e-mail. The DVDs with CT scan data were viewed by an intensive care specialist (WM), a radiologist, and a trauma surgeon (JL); judgement differences (e.g., with regard to the predominant injury) were resolved by a conference. All data collection forms were checked for completeness, and the local study managers were asked to provide missing information, if available. All information was checked for inconsistencies and/or implausible values; obvious errors were corrected. Six months after trauma the Extended Glasgow Outcome Scale (GOSE) score was obtained by phone interviews with patients and/or relatives and/or caregivers; this information was then entered into the database [17]. Ratings for the GOSE range from 1 to 8 (Dead to Upper Good Recovery). The 6-month outcome was dichotomized into unfavorable (GOSE score 1-6) and favorable (GOSE score 7–8) outcome groups.
First data analysis
From the online database data were exported to an Excel™ file. Time intervals (EMS arrival – hospital arrival; hospital arrival – CT scan, CT scan- Operating Room, etc.), injury severity scores (ISS), and probabilities of mortality and of unfavorable 6-month-outcome were calculated. Outcome probabilities were calculated using the IMPACT core model [18] which has been validated for our sample [19]. Expected mortality and unfavorable outcome were calculated for the whole study group with all known values. Based on the calculated probabilities and real outcomes, ratios of observed versus expected mortality and of observed versus expected rates of unfavorable outcome (O/E ratios) were calculated (in the patient group with known outcome values). These O/E ratios were used to analyze the effectiveness of treatment options. Individual treatment options (e.g., use of monitoring, use of fluids, prehospital intubation, interval between hospital admission and CT scan, etc.) were analyzed by comparing O/E ratios of patients with or without a specific treatment option, respectively (“comparative effectiveness analysis”). A treatment option was considered to be effective if the O/E ratios of patients that had received this treatment were <1 (i.e., if rates of mortality and of unfavorable outcome were lower than expected). A treatment option was thus considered to be not effective if the O/E ratios of patients were >1 (i.e., if rates of mortality and of unfavorable outcome were higher than expected).
The differences between the numbers of observed and expected survivors (or observed and expected favorable outcome at 6 months after injury) were defined as “unexpected survivors“(or “unexpected favorable outcomes“).
Development and implementation of recommendations
In 11/2010, the full Working Group met again, studied the results of the first phase data analysis, and developed recommendations for the early management of TBI patients. The important aspects of these recommendations included:
-
time factors: fast transport to an appropriate center if field GCS score <13 or other signs of neurological impairment, first CT scan within 20–30 min after arrival, in cases of intracranial hematoma interval between CT scan and surgery <60 min.
-
adequate monitoring: use of capnography in all ventilated patients, use of pulse oximetry, and use of blood pressure monitoring
-
fluid resuscitation: avoid hypotonic solutions, use of Ringer’s solution or other balanced electrolytes solutions, consider hypertonic saline in hypotonic patients
-
adequate ventilation: normoventilation (monitored by capnography)
-
early thrombelastometry (TEM) to optimize coagulation in all patients >60 years and/or on anticoagulants
-
medication: avoidance of steroids
This document (in German) was available via the INRO website (www.igeh.org), and was distributed to all centers. The local study managers of each center were responsible for convening meetings with the EMS providers in their regions to make the EMS staff familiar with the important aspects of these recommendations. All centers were supposed to implement these recommendations by 02/2011. In addition, the findings of phase 1 were presented at all national EMS, trauma- or anesthesia congresses in Austria in 2011.
Second data collection phase (Phase 2)
The second data collection phase started in 04/2011 and lasted 10 months. This phase was shorter than the first one due to funding restrictions, however, the monthly patient enrollment rate was similar. Enrollment criteria and data collection were identical to the first phase. Data on 325 patients collected in 14 participating centers were analyzed. Again, patient folders were collected at regular intervals, data was entered as before, and GOSE scores at 6 months after the injury were obtained by phone interviews.
Final data analysis
Data was exported from the online database to an ExcelTM file. As before, data were checked for completeness and consistency, implausible values were corrected, missing information was retrieved, and calculations (intervals, probabilities) were made. Differences in epidemiology, treatment and outcomes between Phase 1 and Phase 2 patients were analyzed.
Statistical analysis
Means with respective standard deviations or medians with inter-quartile ranges were used as central measures of continuous variables, and counts with percentages were used as frequency measures of categorical variables. For the statistical analysis of continuous variables the Student’s T-test was used when analyzing means, and the Wilcoxon test when analyzing medians. For the analysis of categorical variables the Chi2-Test was used. In case of ‘Unknown’ (missing) cases the tests were applied only on known values. Logistic regression was used for multivariable analysis of factors influencing the outcome of patients. Variables that had significant influence on the outcome in univariate analysis were used for the logistic regression model. Treatment center was also used as a predictor, thus the presented results took the ‘center effect’ into the account. Odds ratios are presented with 95 % confidence intervals.
A p-value of <0.05 was considered statistically significant.
Results
Demographic data of patients from Phase 1 versus Phase 2 are given in Table 1. The two groups were similar; there were no significant differences regarding mean age, male: female ratio, and mechanisms of trauma.
Severity of trauma, CT scan findings, and expected outcomes are given in Table 2. The initial GCS was significantly higher in Phase 2 patients; the median, however, indicated that in both groups most patients had severe TBI. The ISS was also significantly higher in Phase 2 patients. The proportion of patients with prehospital hypotension and/or hypoxia was similar in both groups. Phase 2 sample had a significantly lower rate of patients with normal pupillary reflex. Regarding CT scan findings compressed or closed basal cisterns as well as greater midline shift were seen significantly more frequently in Phase 2 patients. The predominant type of brain lesion was not significantly different between the 2 groups. Phase 2 patients had higher trauma severity, worse CT findings, and worse pupillary reactivity. Expected mortality rates and the expected rates of unfavorable outcome were similar in both groups.
The treatment options that had been recommended based on association with improved outcomes are listed in Table 3. All of them were used more frequently during Phase 2. Direct transportation to the participating centers occurred significantly more frequently (87 vs. 78 %). Regarding time intervals, in Phase 2 significantly more patients reached the hospital within 60 min after EMS arrival (61 vs. 41 %), had their first CT scan within 60 min after hospital arrival (74 vs. 66 %), and – if required – had neurosurgical operations started within 120 min of hospital arrival (36 vs. 32 %). Prehospital monitoring (pulse oximetry, blood pressure monitoring, and capnography) was used more frequently in Phase 2. Prehospital ventilation was improved, as fewer patients were hyperventilated and more patients had optimal ventilation. Regarding prehospital fluid resuscitation Ringer’s lactate solutions as well as colloids (mainly hydroxy ethyl starch) were used less frequently, while Ringer’s and other balanced electrolyte solutions were used more frequently. Prehospital infusion volumes were not significantly different: 700 (SD 698 ml) in Phase 1 vs. 800 (SD 737 ml) in Phase 2, and were given on average within the time frame of EMS care (50 ± 25) minutes. Within in-hospital treatment in Phase 2 thrombelastometry (TEM) was used more frequently (in 40 % vs. 24 %), and corticosteroids were given significantly less frequently: 2 of the 3 cases that received corticosteroids during Phase 2 had concomitant spinal cord injuries, and the corticosteroids were used due to that.
During Phase 2 neurosurgical procedures were required more frequently (67 % vs. 59 %), ICP was monitored more often (in 60 % vs. 51 %), but for shorter periods (8 [IQR 5–14] vs. 9 days [IQR 5–13]), and the duration of ventilation was longer (10 days [IQR 3–18] vs. 8 [IQR 2–15]). No significant differences between Phase 2 and Phase 1 were observed regarding rates of prehospital intubation (62 % vs. 60 %), of prehospital management by helicopter crews (48 % vs. 46 %), and of therapeutic hypothermia (14 % vs. 21 %).
Outcomes were significantly better in Phase 2 (Table 4). Hospital mortality was 22 % in Phase 2 vs. 29 % in Phase 1, and the rate of patients with unfavorable outcome was 32 % in Phase 2 vs. 38 % in Phase 1.
Comparison of expected and observed outcomes is presented in Table 5. There were significantly more unexpected survivors as well as patients with unexpected favorable outcomes.
Table 6 presents the results of multivariable analysis of factors influencing the outcome of patients. For the logistic regression model the variables that had significant influence on the outcome in univariate analysis were used. Patients in Phase 2 had significantly higher odds of ICU survival (OR 2.92, CI95%: 1.35–6.31) and hospital survival (OR 3.01, 1.41–6.38) and higher odds of favorable outcome (OR 3.14, 1.72–5.73). These findings have been adjusted for age, indicators of severity and treatment, and for “center effect” (by including the treatment center as one of the independent variables in the model).
Discussion
To the best of our knowledge this is the first project that tried to identify the most important treatment options, summarized these in a short document, and began implementing them. The results demonstrated that outcomes of patients with TBI can be improved if the recommended treatment options are used more frequently. Predicted mortality and predicted rate of unfavorable outcome were identical in both phases. There were no other differences in treatment options (e.g., increased use of tranexamic acid etc.). Thus, we believe the significantly better outcomes observed in Phase 2 were probably due to the achieved improvements in early TBI care.
The impact of time factors after TBI seems to be well known; yet there is conflicting evidence, whether duration (“golden hour”) or quality of emergency care has more influence on the outcome of TBI patients [20]. Some studies suggest that direct transport to an appropriate center is associated with improved outcomes [21]. The importance of in-hospital time factors has been shown in other studies, too [22, 23]. Our project successfully significantly reduced rates of secondary transfers and significantly increased proportion of those patients who got to the hospital within 60 min from EMS arrival. Regarding the time intervals hospital admission – ‘first CT in less than 60 min after admission’ and ‘from hospital admission to operation room in less than 120 min’ the project was less successful; the improvements were statistically not significant.
The use of capnography in patients who need prehospital intubation has been shown to reduce the rate of hyperventilation [24]. It has also been shown that end-tidal CO2 correlates well with ventilation in patients with isolated TBI [25]. However, the same study showed that end-tidal pCO2 shows poor correlation to ventilation in patients with major trauma and shock. This is due to the fact that end-tidal pCO2 may be related to pulmonary perfusion rather than to ventilation in these states. Therefore, the target range of end-tidal pCO2 has to be chosen according to the status of the trauma patient. Our recommendations included a target range of 30–35 mmHg (corresponding to an arterial pCO2 of 35–40 mmHg in patients with normal perfusion). Our data show that the use of capnography reduced the rate of hyperventilation. This part of the project was implemented successfully.
Fluid resuscitation is an important option in patients with TBI. Resuscitation with isotonic crystalloids is considered standard care. It has been shown that resuscitation using albumin is associated with worse outcomes in TBI patients [26], and that hypertonic saline is not superior to normal saline [27] in hypotensive patients with TBI. Our recommendations were to avoid hypotonic crystalloids (e.g., Ringer’s lactate), use isotonic crystalloids, and to add colloids and/or hypertonic saline in hypotensive patients. These recommendations were followed in the majority of patients.
The recommendation to use TEM as early as possible to optimize coagulation in all patients >60 years and/or on anticoagulants is a new aspect. This recommendation was based on the finding that during Phase 1, patients who had had TEM in the Trauma Room had higher hospital survival (51 % vs. 38 %) and a higher rate of favorable outcome (40 % vs. 28 %). A number of recent studies suggest that the use of TEM to guide coagulation management may be beneficial after multiple trauma [28, 29] as well as after TBI [30]. The significant increase in early use of TEM during Phase 2 may have contributed to the better outcomes of the Phase 2 patients.
The recommendation not to use steroids was made because during the first Phase 15 patients received corticosteroids; the mortality of these patients was significantly higher (15 % vs. 0 %) – thus, the use of corticosteroids more than doubled the odds for mortality. The recommendations not to use corticosteroids was one of the few “standards” in the 1996 BTF guidelines [12], and is still a “Level 1” recommendation in the 2007 version. The CRASH trial [31] has shown that use of corticosteroids is associated with increased mortality. It is unclear why corticosteroids were used so frequently during Phase 1; only 1/15 patients had a concomitant spinal cord injury.
Regarding epidemiology, >70 % of the patients were male; this is the typical male: female ratio for moderate and severe TBI [32]. The mean age was rather high; almost one third of the patients were > 65 years old. This mirrors a clear trend during the last decades: a high rate of geriatric TBI has been observed in other European studies, too [9]. Thus, traffic accidents were a leading cause of injury, but same-level falls (i.e., the typical mechanism of TBI in geriatric patients) were the cause of accident in almost one third of all cases.
Limitations
It is important to address the study limitations. The hospital selection may have introduced bias as the treatment centers participated in our study based on their own decision upon the invitation.
Despite the thorough monitoring we were not able to prevent missing data in the prehospital setting and outcome follow-up. Loss to follow-up is prominent mainly in Phase 1 with 44 % of unknown outcome. The main reason was the absence of contact information and that was better taken care of in Phase 2.
Conclusions
In conclusion, in a study done in 14 Austrian centers we have identified prehospital and early hospital treatment options that were potentially associated with better outcomes. Based on these results, recommendations were drafted and implemented with the support of participating hospitals and EMS. These recommendations dealt with time factors, monitoring and treatment options. We were able to demonstrate that these recommendations led to reduction of time delays and improved quality of care, both pre- and in-hospital in Phase 2 of our study. Patients treated in participating treatment centers after the implementation of recommended changes had three-fold chance of survival and favorable long-term outcome.
Thus, improvement in early TBI care was followed by a significant improvement in patient outcomes.
Abbreviations
- AIS:
-
Abbreviated Injury Scale
- AUVA:
-
Austrian Worker’s Compensation Board
- BTF:
-
Brain Trauma Foundation
- CI:
-
Confidence interval
- CO2:
-
Carbon dioxide
- CT:
-
Computed Tomography
- EMS:
-
Emergency medical services
- GCS:
-
Glasgow Coma Scale
- GOSE:
-
Extended Glasgow Outcome Scale
- ICU:
-
Intensive care unit
- IQR:
-
Interquartile range
- ICP:
-
Intracranial pressure
- ISS:
-
Injury Severity Score
- INRO:
-
International Neurotrauma Research Organization
- O/E:
-
Observed versus expected
- OR:
-
Odds Ratio
- p CO2:
-
Partial pressure of carbon dioxide
- SD:
-
Standard Deviation
- TEM:
-
Thrombelastometry
- TR:
-
Trauma Room
- TBI:
-
Traumatic Brain Injury
References
Ghajar J. Traumatic brain injury. Lancet. 2000;356(9233):923–9. doi:10.1016/s0140-6736(00)02689-1.
Tagliaferri F, Compagnone C, Korsic M, Servadei F, Kraus J. A systematic review of brain injury epidemiology in Europe. Acta Neurochir (Wien). 2006;148(3):255–68. doi:10.1007/s00701-005-0651-y. discussion 68.
Ackery A, Hagel BE, Provvidenza C, Tator CH. An international review of head and spinal cord injuries in alpine skiing and snowboarding. Inj Prev. 2007;13(6):368–75. doi:10.1136/ip.2007.017285.
Auman KM, Kufera JA, Ballesteros MF, Smialek JE, Dischinger PC. Autopsy study of motorcyclist fatalities: the effect of the 1992 Maryland motorcycle helmet use law. Am J Public Health. 2002;92(8):1352–5.
Bowman SM, Aitken ME, Helmkamp JC, Maham SA, Graham CJ. Impact of helmets on injuries to riders of all-terrain vehicles. Inj Prev. 2009;15(1):3–7. doi:10.1136/ip.2008.019372.
Steudel WI, Cortbus F, Schwerdtfeger K. Epidemiology and prevention of fatal head injuries in Germany--trends and the impact of the reunification. Acta Neurochir. 2005;147(3):231–42. doi:10.1007/s00701-004-0441-y. discussion 42.
WHO. World Report on Road Traffic Injury Prevention. Geneva: World Health Organization; 2004.
Maas AI, Stocchetti N, Bullock R. Moderate and severe traumatic brain injury in adults. Lancet Neurol. 2008;7(8):728–41. doi:10.1016/s1474-4422(08)70164-9.
Stocchetti N, Paterno R, Citerio G, Beretta L, Colombo A. Traumatic brain injury in an aging population. J Neurotrauma. 2012;29(6):1119–25. doi:10.1089/neu.2011.1995.
Bulger EM, Nathens AB, Rivara FP, Moore M, MacKenzie EJ, Jurkovich GJ. Management of severe head injury: institutional variations in care and effect on outcome. Crit Care Med. 2002;30(8):1870–6.
Fakhry SM, Trask AL, Waller MA, Watts DD. Management of brain-injured patients by an evidence-based medicine protocol improves outcomes and decreases hospital charges. J Trauma. 2004;56(3):492–9. discussion 9-500.
Bullock R, Chesnut RM, Clifton G, Ghajar J, Marion DW, Narayan RK, et al. Guidelines for the management of severe head injury. Brain Trauma Foundation. Eur J Emerg Med. 1996;3(2):109–27.
Rusnak M, Janciak I, Majdan M, Wilbacher I, Mauritz W. Severe traumatic brain injury in Austria VI: effects of guideline-based management. Wien Klin Wochenschr. 2007;119(1-2):64–71. doi:10.1007/s00508-006-0765-0.
Gabriel EJ, Ghajar J, Jagoda A, Pons PT, Scalea T, Walters BC. Guidelines for prehospital management of traumatic brain injury. J Neurotrauma. 2002;19(1):111–74.
Teasdale G, Jennett B. Assessment and prognosis of coma after head injury. Acta Neurochir. 1976;34(1-4):45–55.
Bull JP. Measures of severity of injury. Injury. 1978;9(3):184–7.
Wilson JT, Pettigrew LE, Teasdale GM. Structured interviews for the Glasgow Outcome Scale and the extended Glasgow Outcome Scale: guidelines for their use. J Neurotrauma. 1998;15(8):573–85.
Perel P, Arango M, Clayton T, Edwards P, Komolafe E, Poccock S, et al. Predicting outcome after traumatic brain injury: practical prognostic models based on large cohort of international patients. Br Med J. 2008;336(7641):425–9. doi:10.1136/bmj.39461.643438.25.
Majdan M, Lingsma HF, Nieboer D, Mauritz W, Rusnak M, Steyerberg EW. Performance of IMPACT, CRASH and Nijmegen models in predicting six months outcome of patients with severe or moderate TBI: an external validation study. Scand J Trauma Resusc Emerg Med. 2014;22(1):68. doi:10.1186/s13049-014-0068-9.
Tohme S, Delhumeau C, Zuercher M, Haller G, Walder B. Prehospital risk factors of mortality and impaired consciousness after severe traumatic brain injury: an epidemiological study. Scand J Trauma Resusc Emerg Med. 2014;22:1. doi:10.1186/1757-7241-22-1.
Hartl R, Gerber LM, Iacono L, Ni Q, Lyons K, Ghajar J. Direct transport within an organized state trauma system reduces mortality in patients with severe traumatic brain injury. J Trauma. 2006;60(6):1250–6. doi:10.1097/01.ta.0000203717.57821.8d. discussion 6.
Weninger P, Mauritz W, Fridrich P, Spitaler R, Figl M, Kern B, et al. Emergency room management of patients with blunt major trauma: evaluation of the multislice computed tomography protocol exemplified by an urban trauma center. J Trauma. 2007;62(3):584–91. doi:10.1097/01.ta.0000221797.46249.ee.
Fung Kon Jin PH, Penning N, Joosse P, Hijdra AH, Bouma GJ, Ponsen KJ, et al. The effect of the introduction of the Amsterdam Trauma Workflow Concept on mortality and functional outcome of patients with severe traumatic brain injury. J Neurotrauma. 2008;25(8):1003–9. doi:10.1089/neu.2007.0463.
Helm M, Schuster R, Hauke J, Lampl L. Tight control of prehospital ventilation by capnography in major trauma victims. Br J Anaesth. 2003;90(3):327–32.
Warner KJ, Cuschieri J, Garland B, Carlbom D, Baker D, Copass MK, et al. The utility of early end-tidal capnography in monitoring ventilation status after severe injury. J Trauma. 2009;66(1):26–31. doi:10.1097/TA.0b013e3181957a25.
Myburgh J, Cooper DJ, Finfer S, Bellomo R, Norton R, Bishop N, et al. Saline or albumin for fluid resuscitation in patients with traumatic brain injury. N Engl J Med. 2007;357(9):874–84. 357/9/874.
Cooper DJ, Myles PS, McDermott FT, Murray LJ, Laidlaw J, Cooper G, et al. Prehospital hypertonic saline resuscitation of patients with hypotension and severe traumatic brain injury: a randomized controlled trial. JAMA. 2004;291(11):1350–7. doi:10.1001/jama.291.11.1350.
Lier H, Krep H, Schochl H. Coagulation management in the treatment of multiple trauma. Anaesthesist. 2009;58(10):1010–26. doi:10.1007/s00101-009-1595-z.
Schochl H, Nienaber U, Hofer G, Voelckel W, Jambor C, Scharbert G, et al. Goal-directed coagulation management of major trauma patients using thromboelastometry (ROTEM)-guided administration of fibrinogen concentrate and prothrombin complex concentrate. Crit Care. 2010;14(2):R55. doi:10.1186/cc8948.
Schochl H, Solomon C, Traintinger S, Nienaber U, Tacacs-Tolnai A, Windhofer C, et al. Thromboelastometric (ROTEM) findings in patients suffering from isolated severe traumatic brain injury. J Neurotrauma. 2011;28(10):2033–41. doi:10.1089/neu.2010.1744.
Edwards P, Arango M, Balica L, Cottingham R, El-Sayed H, Farrell B, et al. Final results of MRC CRASH, a randomised placebo-controlled trial of intravenous corticosteroid in adults with head injury-outcomes at 6 months. Lancet. 2005;365(9475):1957–9. doi:10.1016/S0140-6736(05)66552-X.
Masson F, Thicoipe M, Aye P, Mokni T, Senjean P, Schmitt V, et al. Epidemiology of severe brain injuries: a prospective population-based study. J Trauma. 2001;51(3):481–9.
Baker SP, O'Neill B, Haddon Jr W, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14(3):187–96.
Source of Funding
The project was funded jointly by the Austrian Ministry of Health (Contract Oct. 15, 2008) and by the Austrian Worker’s Compensation Board (AUVA; FK 11/2008 and FK 11/2010). Data analysis was supported by a grant from AUVA (FK 09/13). INRO is supported by an annual grant from Mrs. Ala Auersperg-Isham and Mr. Ralph Isham through Neurotrauma Foundation, and by small donations from various sources.
Members of the “Austrian Working Group on Improvement of Early TBI Care”
International Neurotrauma Research Organisation (Alexandra Brazinova MD PhD MPH, Marek Majdan PhD, Johannes Leitgeb MD, Walter Mauritz Prof. MD), Amstetten hospital (Alexandra Frisch MD, Andreas Liedler MD, Harald Schmied MD); Feldkirch hospital (Reinhard Folie MD, Reinhard Germann MD PhD, Jürgen Graber RN ICU), Graz University hospital (Kristina Michaeli MD, Rene Florian Oswald MD, Andreas Waltensdorfer MD), Graz trauma hospital (Thomas Haidacher MD, Johannes Menner MD), Horn hospital (Anna Hüblauer MD, Elisabeth Nödl MD), Innsbruck University hospital (Christian Freund MD, Karl-Heinz Stadlbauer MD), Klagenfurt hospital (Michel Oher MD, Ernst Trampitsch MD, Annemarie Zechner MD), Linz hospital (Franz Gruber MD, Walter Mitterndorfer MD, Sandra Rathmaier MS), Linz trauma hospital (Norbert Bauer MD), Salzburg hospital (Peter Hohenauer MD), Salzburg trauma hospital (Josef Lanner MD, Wolfgang Voelckel Prof. MD), Sankt Poelten hospital (Claudia Mirth MD), Schwarzach hospital (Hubert Artmann MD, Bettina Cudrigh MD), Wiener Neustadt hospital (Daniel Csomor MD, Günther Herzer MD, Andreas Hofinger MD, Helmut Trimmel MD), Wien Meidling trauma hospital (Veit Lorenz MD, Heinz Steltzer Prof. MD), Wien „Lorenz Boehler“trauma hospital (Walter Mauritz Prof. MD).
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
AB was project manager of the study, participated in its conception and design, coordinated its implementation, performed the statistical analysis, drafted the manuscript. She established and maintained contacts with local study managers in participating hospitals; carried out preparation, distribution and pick up of the data collection patient folders; organized and supervised data transcription into electronic database; managed the database: controlled for missing information and retrieved these from the local study managers, cleaned the data; supervised follow-up; performed data analysis; drafted the manuscript. MM participated in data management and statistical analysis, participated in critical revision of the manuscript. JL reviewed CT scan data, participated in critical revision of the manuscript. HT participated in drafting and critical revision of the recommendations, participated in critical revision of the manuscript. WM is the author of the study concept, made substantial contribution to the design, participated in critical revision of the manuscript. All authors read and approve the final manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Brazinova, A., Majdan, M., Leitgeb, J. et al. Factors that may improve outcomes of early traumatic brain injury care: prospective multicenter study in Austria. Scand J Trauma Resusc Emerg Med 23, 53 (2015). https://doi.org/10.1186/s13049-015-0133-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13049-015-0133-z