Abstract
Background
Traumatic brain injury (TBI) remains one of the main causes of mortality and long-term disability worldwide. Maintaining physiology of brain tissue to the greatest extent possible through optimal management of blood pressure, airway, ventilation, and oxygenation, improves patient outcome. We studied the quality of prehospital care in severe TBI patients by analyzing adherence to recommended target ranges for ventilation and blood pressure, prehospital time expenditure, and their effect on mortality, as well as quality of prehospital ventilation assessed by arterial partial pressure of CO2 (PaCO2) at hospital admission.
Methods
This is a retrospective cohort study of all TBI patients requiring tracheal intubation on scene who were transported to one of two major level 1 trauma centers in Switzerland between January 2014 and December 2019 by Swiss Air Rescue (Rega). We assessed systolic blood pressure (SBP), end-tidal partial pressure of CO2 (PetCO2), and PaCO2 at hospital admission as well as prehospital and on-scene time. Quality markers of prehospital care (PetCO2, SBP, prehospital times) and prehospital ventilation (PaCO2) are presented as descriptive analysis. Effect on mortality was calculated by multivariable regression analysis and a logistic general additive model.
Results
Of 557 patients after exclusions, 308 were analyzed. Adherence to blood pressure recommendations was 89%. According to PetCO2, 45% were normoventilated, and 29% had a SBP ≥ 90 mm Hg and were normoventilated. Due to the poor correlation between PaCO2 and PetCO2, only 33% were normocapnic at hospital admission. Normocapnia at hospital admission was strongly associated with reduced probability of mortality. Prehospital and on-scene times had no impact on mortality.
Conclusions
PaCO2 at hospital admission is strongly associated with mortality risk, but normocapnia is achieved only in a minority of patients. Therefore, the time required for placement of an arterial cannula and prehospital blood gas analysis may be warranted in severe TBI patients requiring on-scene tracheal intubation.
Similar content being viewed by others
Introduction
Traumatic brain injury (TBI) remains one of the main causes of mortality and long-term disability, affecting 50 million people worldwide per year and costing € 325 billion [1, 2]. In Europe, crude incidence rates of TBI range from 47 to 694 per 100,000 population per year, with mortality rates ranging from 9 to 28 per 100,000 population per year [3].
TBI is caused by an initial traumatic insult to the brain, which disrupts normal physiology of the tissues involved. These non-physiological states may then lead to secondary damage [1, 2, 4,5,6,7]. Hypotension, inadequate ventilation, and hypoxemia are among the non-physiological states that increase mortality after severe TBI [6, 8,9,10]. Early tracheal intubation and controlled ventilation in the prehospital setting can improve outcomes of patients with severe TBI [11,12,13].
Guidelines on resuscitation of TBI patients recommend a partial pressure of end-tidal carbon dioxide (PetCO2) between 4.4 and 5.4 kPa in intubated patients (“normoventilation”) and maintenance of systolic blood pressure (SBP) ≥ 90 mm Hg (“normotension”), despite weak evidence and controversy surrounding this concept of a unique threshold for hypotension in severe TBI [14,15,16,17]. While optimizing brain tissue physiology seems to reduce mortality, the time required for treatment of trauma is also considered an important factor influencing outcome of trauma patients [18, 19]. Therefore, we studied the quality of prehospital care in severe TBI patients by analyzing adherence to recommended target ranges for ventilation and blood pressure, prehospital time expenditure, and their effect on mortality.
Methods
We reviewed data from all patients in the Swiss Air Ambulance (Rega) mission archives who were suspected to have severe TBI in the prehospital setting, requiring tracheal intubation on scene and were transported to one of two level 1 trauma centers (Cantonal Hospital St. Gallen and Bern University Hospital, Switzerland) between January 2014 and December 2019. Prehospital management was performed according to current treatment protocols used by the helicopter emergency medical service (HEMS) of Rega. These include rapid sequence induction and tracheal intubation at a Glasgow Coma Scale (GCS) Score ≤ 8. Capnography was used to guide ventilation with a target PetCO2 between 4.4 and 5.7 kPa (33–43 mm Hg). Whether the patients were ventilated manually using a bag valve mask or mechanically could not be ascertained from the mission reports. Target SBP of ≥ 90 mm Hg was achieved—if necessary—by intravenous administration of crystalloid volume or catecholamine support. Capnography and non-invasive blood pressure monitoring were performed using a Propaq® Multifunction Monitor (ZOLL Medical Corporation, MA, USA).
Recorded data included patient characteristics, initial GCS score, first SBP at admission to the hospital, first PetCO2 at admission, arterial partial pressure of carbon dioxide (PaCO2) within the first 5 min of admission, injury severity score (ISS), and on-scene time, as well as total prehospital time (defined as interval between alert of the helicopter emergency medical service crew and hospital arrival). Mission information was transferred from paper logs into a spreadsheet (Microsoft Excel, Microsoft Corporation, Redmond, WA, USA). Patients were then matched to hospital records using date of birth and admission date and time.
Statistical methods
In terms of summary statistics, categorical variables are presented with counts and percentages. Continuous variables are presented as median and interquartile range (IQR) or mean and standard deviation (STD) as appropriate. Unadjusted univariable group comparisons in Table 2 were based on the chi-square test (categorical variables), Student’s t-test (continuous, normally distributed) and unpaired two-samples Wilcoxon test (continuous, skewed).
Correlation between PetCO2 and PaCO2 was evaluated by the Pearson correlation coefficient. Univariable, non-linear associations of the outcome mortality with the covariates systolic blood pressure, PetCO2 and PaCO2 were graphically examined by a logistic general additive model. To analyze the effect of time expenditure in the prehospital setting, we performed a multivariable logistic regression to examine the association of a set of known predictors of outcome after severe TBI with mortality. The discrimination capacity of the logistic regression models was evaluated by means of the area under the receiver operating curve (AUROC). Model fit was evaluated by means of Nagelkerke's pseudo-R-squared. All computations were performed with R Version 4.0.2.
Ethics
The study was conducted in accordance with ethical standards as laid down in the Declaration of Helsinki and all national guidelines. The local ethics committees of Bern and St. Gallen (EKOS) approved the study. Both granted permission to use patient data without individual informed consent according to the federal act on research involving human beings and the ordinance on human research with the exception of clinical trials. The permission also covered the use of patient data regarding HEMS operations (ethics committee Bern: BASEC nr. 2020-01737, study nr. 4690 and EKOS: BASEC nr. 2020-01737, 20/122).
Results
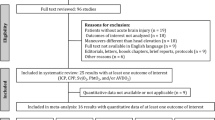
From January 2014 to December 2019 a total of 557 patients requiring tracheal intubation after suspected TBI were transported to the two participating trauma centers by Rega HEMS crews. A total of 110 patients were excluded due to a missing paper mission log (1), no documented intubation (1), being on an inter-hospital transfer (2), no description of the mission available (missing or illegible) (7) or no confirmation of intracranial injuries after diagnostic imaging (99). Of the remaining 447 patients, 139 patients could not be matched to corresponding hospital records. The remaining 308 patients were included for analysis (Fig. 1).
Patient characteristics are shown in Table 1. The majority of TBI were sustained in road traffic accidents (45%), with accidents at home being the second most common cause (31%). Sporting accidents (13%) and accidents at work (8%) were lower in proportion, and classification of mechanism of injury was not available for eight patients (3%). The mortality rate was 36% (111/308). The median age of this cohort of patients was 52 years (IQR 27–71), and patients who survived were significantly younger. Median SBP in the resuscitation room was 122 mm Hg (IQR 104–138 mm Hg), with surviving patients having a higher median systolic blood pressure than those who died (unadjusted p = 0.045). SBP at handoff was ≥ 90 mm Hg in 89% of all patients. Vasopressors were administered to 24% of patients. Normoventilation according to the measured PetCO2 at arrival in the resuscitation room was achieved in 45% of the patients, and 29% were both normoventilated and had a systolic blood pressure ≥ 90 mm Hg (Fig. 2A).
Scatter plot showing end-tidal partial pressure of CO2 (PetCO2) and systolic blood pressure at arrival in the resuscitation room for surviving and deceased patients, shaded area: normoventilation and systolic blood pressure ≥ 90 mm Hg (A). Probability of mortality depending on systolic blood pressure (B), arterial partial pressure of CO2 (PaCO2) (C) and PetCO2 (D) at arrival in the resuscitation room. Blue shaded area: Recommended treatment target. Grey shaded are: 95% confidence interval
As measured in the first arterial blood gas analysis in the emergency department, 33% of the patients had normocapnia at hospital admission. In surviving patients, PetCO2 was significantly higher (p < 0.001) and PaCO2 significantly lower (p = 0.019) compared to deceased patients. Correlation between PetCO2 and PaCO2 was weak with an r = 0.14 (Fig. 3, p = 0.02), and the mean difference was 1.81 kPa (SD 1.46 kPa). No difference in on-scene or total prehospital time was seen between surviving and deceased patients.
Factors significantly associated with in-hospital mortality in our multivariable regression analysis (Table 2) were greater age (OR 1.04, CI 1.03–1.06, p < 0.001), lower GCS (GCS 3 compared to GCS 4–8 OR 5.17, CI 2.31–12.3, p < 0.001), and higher ISS (OR 1.03, CI 1.00–1.06, p < 0.001). SBP at handover in the resuscitation room did not show any significant association with mortality (OR 1.0, CI 0.99–1.01, p = 0.5). Neither did on-scene time (OR 1.04, CI 0.99–1.09, p = 0.2) or total prehospital time (OR 0.97, CI 0.94–1.00, p = 0.079). These results are robust under multiple imputations that were performed as a sensitivity analysis (Additional file 1).
Discussion
The pre-hospital phase is a very critical period for patients with severe TBI. Outcome after severe TBI is influenced by rapid interventions and early stabilization of ventilation and circulation, which together can prevent secondary brain damage [11, 12, 20, 21].
In our cohort upon hospital admission, recommended values for ventilation and blood pressure management according to the guidelines were achieved in only 29% of the patients after pre-hospital tracheal intubation. More importantly, however, we showed that PetCO2 does not reliably reflect PaCO2. In our patients, this led to 67% of the patients not being ventilated appropriately despite their PetCO2 being within the recommended range on hospital admission. The majority of these patients were hypercapnic (64%), whereas hypocapnia only occurred in 3% of cases.
The physiological causes of a gap between PaCO2 and PetCO2 are dead space ventilation and ventilation/perfusion mismatch. A gap of 0.4–0.7 kPa (3–5 mm Hg) is considered physiologic. In trauma patients, however, this gap can be markedly increased by hypovolemia and reduced cardiac output (due to hemorrhage, e.g.) as well as severe thoracic injuries. The proportion of normocapnic patients at hospital arrival in our study was even worse than in a study conducted before the availability of prehospital capnography, at a time in which ventilation was simply guided by estimated body weight [22]. This poor correlation is also clinically relevant when ventilation is performed in the pre-hospital setting with a self-inflating bag (e.g., during on-scene treatment and transfer from helipad to the emergency department) is typically titrated to PetCO2 and not with a ventilator with spirometry analysis. Hypocapnia may aggravate cerebral ischemia, and hypercapnia can increase intracranial pressure; both are known to negatively affect outcome of severe TBI patients [9].
Our findings underscore the tremendous importance of maintaining normocapnia already in the prehospital setting, before hospital admission (Fig. 2C). Hyperventilating patients (guided by PetCO2) seems to be independently associated with increased mortality (Fig. 2B, Table 2). This is in good accordance with and a potential explanation for the findings of a previous study by our group showing that the size of the CO2-gap between end-tidal and arterial measurements is significantly associated with mortality [23]. However, these results should not question the reliability of PetCO2 measurements altogether. Clinicians should consider the physiological causes of the CO2-gap and its potential increase in patients with hemodynamic instability or severe chest trauma. According to the results of another study, aiming for a PetCO2 of 3.3–4.0 kPa (25–30 mm Hg) in these patients could significantly increase the proportion of normocapnic patients upon arrival at the hospital [24]. Of course, in times of widespread availability of ultrasound and physicians that are well trained in prehospital emergency medicine, arterial blood gas analysis would be ideal and feasible.
The negative influence of hypotension on outcome in patients suffering from severe TBI has been proven in numerous studies, and recommendations for blood pressure management are integrated in all guidelines on emergency management of TBI [4, 8, 10, 14, 15, 25, 26]. Rega’s standard operating procedure for severe TBI patients uses a hypotension threshold of 90 mm Hg. Median SBP upon arrival at the trauma centers in our study was 122 mm Hg, and 89% of all patients had a SBP of ≥ 90 mm Hg, indicating good adherence to treatment recommendations for blood pressure.
Juelsgaard et al. analyzed adherence to company treatment recommendations for a Danish HEMS organization showing a SBP ≥ 90 mm Hg in 91% of TBI cases analyzed [4]. Further literature and guidelines recommend targeting higher SBP values between ≥ 100 mm Hg and ≥ 120 mm Hg [5, 27,28,29,30]. A SBP ≥ 120 mm Hg was achieved in only 55% of patients by Juelsgaard and colleagues, and 51% in another Danish study, exactly corresponding to our rate of 55% [4, 31]. However, the concept of a hypotension threshold as defined in international guidelines has been questioned recently, as these numbers are based on studies that mainly focused on dichotomous comparison of low and high blood pressure groups with arbitrary cutoffs [16].
New data show that mortality after TBI does not drop off at the proposed cut-off values for SBP. Spaite et al. found a rather linear association of lowest prehospital SBP and mortality, without any detectable threshold between 40 and 119 mm Hg [17]. Our unadjusted data supports this finding (Fig. 2B). After adjusting for several other factors, we found no significant association between blood pressure at hospital admission and mortality. One explanation for this could be that we only evaluated the blood pressure value at a certain point in time; however, the episodes of hypotension during the entire phase of emergency medical care are probably much more decisive for the outcome [4, 8]. We only evaluated the blood pressure values at hospital admission that were automatically recorded and documented in the resuscitation rooms. Blood pressure values during the prehospital phase were documented manually using paper mission logs which are known to be unreliable in terms of data quality. Additionally, more than 90% of patients had the recommended SBP of ≥ 90 mm Hg at hospital admission. These factors might also explain the lack of association between blood pressure and mortality in the regression analysis of our study.
In our cohort, we saw no significant association between on-scene or prehospital time and mortality. This might seem counterintuitive at first glance, as longer duration of prehospital times prolongs the timespan before severe TBI patients have access to more comprehensive diagnostic and treatment options in a critical care setting [32]. This potential delay can be hypothesized to increase the likelihood of secondary brain damage, and a shorter time on the scene before diagnosis could help improve outcomes [33,34,35]. However, the concept of the shortest possible time to definitive treatment being the sole indicator of outcome has been called into question [36,37,38,39]. More than simply increasing the speed at which patients are brought to definitive care, it seems that the impact of HEMS on mortality in severe TBI patients is a multifactorial process involving pre-hospital interventions which slow the development of secondary brain damage before transport [40]. In severe TBI patients in particular, adherence to physiological treatment targets as well as direct transport to level 1 trauma centers may have led to better outcomes, and not necessarily short prehospital times [1, 13, 41, 42].
In a comparison of physician- and non-physician-based HEMS services, Pakkanen and colleagues showed higher rates of pre-hospital interventions and conversely lower rates of non-physiologic vital parameters at admission. They interpreted this as being at least partially responsible for the observed improvement in mortality in the physician-based HEMS group [33, 43]. This might also help explain improved outcomes despite there being no time benefit or in some cases even longer prehospital times in other studies on physician-staffed HEMS [43,44,45]. One must also consider that indicated invasive emergency procedures in the prehospital setting do not increase total resuscitation time (i.e., time to surgery or an intensive care unit), as these procedures must be made up in the resuscitation room anyway [46]. Moreover, even though patients required rapid sequence induction and tracheal intubation, this study showed on-scene times of only 30 min. Finally, the high density of trauma centers in Switzerland, with relatively short approaches and transport times compared to other countries (interval from alerting the HEMS crew to arrival at the hospital was < 68 min for the vast majority of our patients) could also explain the lack of association between prehospital time and mortality [47].
Limitations
Our study has several limitations. First, it was conducted in a retrospective fashion, which affected availability of data in some cases. Second, paper logs were used for HEMS missions. It is reasonable to assume that there was significant variability in the quality of logged data in the setting of severely injured patients requiring tracheal intubation, which represents a high workload for the entire team. We used the first values recorded in-hospital for SBP and PetCO2, as these were automatically recorded every minute and more reliable compared to the prehospital values recorded manually. Therefore, we cannot make any statement about the course of these parameters during prehospital care. However, we used the most valid data available. In the future, electronic recording of vital signs during prehospital care (as now introduced by Rega) may allow studies that are more accurate. Third, data may be difficult to compare due to the countries and regions with a lower density of hospitals and trauma centers, as well as different geographical challenges in prehospital missions. Forth, 139 out of eligible 447 patients could not be matched to corresponding hospital records (31%). The most common reason was that the patient's personal details were not stored or not correctly stored in the electronic documentation system during resuscitation room care and subsequently the data from resuscitation room care is missing in the patient record. This was certainly by chance and is therefore unlikely to have biased our results. And finally, neurological outcome at discharge could not be analyzed as it was not readily available for a majority of patients.
Conclusion
In conclusion, we saw adherence to guideline recommendations in patients with severe TBI requiring tracheal intubation on scene, which was good for blood pressure management, but only moderate on normoventilation. However, due to the poor correlation between PetCO2 and PaCO2, only a minority of patients were normocapnic on hospital admission. Our results, although limited by the univariate exploratory analysis in this study, suggest that striving for normocapnia already in the prehospital phase may reduce patient mortality. As on-scene time did not have a significant impact on in-hospital mortality, the time required for placement of an arterial cannula and prehospital blood gas analysis may be beneficial to severe TBI patients requiring prehospital tracheal intubation.
Availability of data and materials
The datasets generated and/or analysed during this study can be obtained from the corresponding author on reasonable request.
References
Juratli TA, Stephan SE, Stephan AE, Sobottka SB. Acute treatment of patients with severe traumatic brain injury. Anaesthesist. 2015;64:159–74.
Ng SY, Lee AYW. Traumatic brain injuries: pathophysiology and potential therapeutic targets. Front Cell Neurosci. 2019. https://doi.org/10.3389/fncel.2019.00528.
Brazinova A, Rehorcikova V, Taylor MS, Buckova V, Majdan M, Psota M, et al. Epidemiology of traumatic brain injury in Europe: a living systematic review. J Neurotrauma. 2021;38:1411–40.
Juelsgaard J, Rognås L, Knudsen L, Hansen TM, Rasmussen M. Prehospital treatment of patients with acute intracranial pathology: adherence to guidelines and blood pressure recommendations by the Danish Air Ambulance. Scand J Trauma Resusc Emerg Med. 2018;26:4–9.
Brenner M, Stein DM, Hu PF, Aarabi B, Sheth K, Scalea TM. Traditional systolic blood pressure targets underestimate hypotension-induced secondary brain injury. J Trauma Acute Care Surg. 2012;72:1135–9.
Stein NR, McArthur DL, Etchepare M, Vespa PM. Early cerebral metabolic crisis after TBI influences outcome despite adequate hemodynamic resuscitation. Neurocrit Care. 2012;17:49–57.
Manley G, Knudson MM, Morabito D, Damron S, Erickson V, Pitts L. Hypotension, hypoxia, and head injury frequency, duration, and consequences. Arch Surg. 2001;136:1118–23.
Rice AD, Hu C, Spaite DW, Barnhart BJ, Chikani V, Gaither JB, et al. Correlation between prehospital and in-hospital hypotension and outcomes after traumatic brain injury. Am J Emerg Med. 2023;65:95–103.
Dumont TM, Visioni AJ, Rughani AI, Tranmer BI, Crookes B. Inappropriate prehospital ventilation in severe traumatic brain injury increases in-hospital mortality. J Neurotrauma. 2010;27:1233–41.
Spaite DW, Hu C, Bobrow BJ, Chikani V, Barnhart B, Gaither JB, et al. The impact of combined prehospital hypotension and hypoxia on mortality in major traumatic brain injury. Ann Emerg Med. 2017;69:62–72.
Winchell RJ, Hoyt DB. Endotracheal intubation in the field improves survival in patients with severe head injury. Arch Surg. 1997;132:592–7.
Trupka A, Waydhas C, Nast-Kolb D, Schweiberer L. Early intubation in severely injured patients. Eur J Emerg Med. 1994;1:1–8.
Gomes E, Araújo R, Carneiro A, Dias C, Costa-Pereira A, Lecky FE. The importance of pre-trauma centre treatment of life-threatening events on the mortality of patients transferred with severe trauma. Resuscitation. 2010;81:440–5.
Badjatia N, Carney N, Crocco TJ, Fallat ME, Hennes HMA, Jagoda AS, et al. Guidelines for prehospital management of traumatic brain injury 2nd edition. Prehosp Emerg Care. 2008;12:S1-52.
Carney N, Totten AM, O’Reilly C, Ullman JS, Hawryluk GWJ, Bell MJ, et al. Guidelines for the management of severe traumatic brain injury, fourth edition. Neurosurgery. 2017;80:6–15.
Spaite DW, Hu C, Bobrow BJ, Chikani V, Sherrill D, Barnhart B, et al. Mortality and prehospital blood pressure in patients with major traumatic brain injury: implications for the hypotension threshold. JAMA Surg. 2017;152:360–8.
Spaite DW, Hu C, Bobrow BJ, Barnhart B, Chikani V, Gaither JB, et al. Optimal out-of-hospital blood pressure in major traumatic brain injury: a challenge to the current understanding of hypotension. Ann Emerg Med. 2022;80:46–59.
Sampalis JS, Lavoie A, Williams JI, Mulder DS, Kalina M. Impact of on-site care, prehospital time, and level of in-hospital care on survival in severely injured patients. J Trauma. 1993;34:252–61.
Andruszkow H, Schweigkofler U, Lefering R, Frey M, Horst K, Pfeifer R, et al. Impact of helicopter emergency medical service in traumatized patients: which patient benefits most? PLoS ONE. 2016. https://doi.org/10.1371/journal.pone.0146897.
Miller JD, Sweet RC, Narayan R, Becker DP. Early insults to the injured brain. JAMA. 1978;240:439–42.
Chesnut RM. Avoidance of hypotension: conditio sine qua non of successful severe head-injury management. J Trauma Acute Care Surg. 1997;42:S4-9.
Helm M, Hauke J, Lampl L. A prospective study of the quality of pre-hospital emergency ventilation in patients with severe head injury. Br J Anaesth. 2002;88:345–9.
Doppmann P, Meuli L, Sollid SJM, Filipovic M, Knapp J, Exadaktylos A, et al. End-tidal to arterial carbon dioxide gradient is associated with increased mortality in patients with traumatic brain injury: a retrospective observational study. Sci Rep. 2021;11:10391.
Helm M, Schuister R, Hauke J, Lampl L. Tight control of prehospital ventilation by Capnography in major trauma victims. Br J Anaesth. 2003;90:327–32.
Chesnut RM, Marshall LF, Klauber MR, Blunt BA, Baldwin N, Eisenberg HM, et al. The role of secondary brain injury in determining outcome from severe head injury. J Trauma. 1993;34:216–22.
Wang HE, Peitzman AB, Cassidy LD, Adelson PD, Yealy DM. Out-of-hospital endotracheal intubation and outcome after traumatic brain injury. Ann Emerg Med. 2004;44:439–50.
Berry C, Ley EJ, Bukur M, Malinoski D, Margulies DR, Mirocha J, et al. Redefining hypotension in traumatic brain injury. Injury. 2012;43:1833–7.
Maas AIR, Dearden M, Teasdale GM, Braakman R, Cohadon F, Iannotti F, et al. EBIC-guidelines for management of severe head injury in adults. Acta Neurochir (Wien). 1997;139:286–94.
Moppett IK. Traumatic brain injury: assessment, resuscitation and early management. Br J Anaesth. 2007;99:18–31.
Murray GD, Butcher I, McHugh GS, Lu J, Mushkudiani NA, Maas AIR, et al. Multivariable prognostic analysis in traumatic brain injury: results from the IMPACT study. J Neurotrauma. 2007;24:329–37.
Rognås L, Hansen TM, Kirkegaard H, Tønnesen E. Anaesthesiologist-provided prehospital airway management in patients with traumatic brain injury: an observational study. Eur J Emerg Med. 2014;21:418–23.
Kim HW, Yun J-H. Treatment experiences of traumatic brain injury patients using doctor-helicopter emergency medical service: early data in a regional trauma center. Korean J Neurotrauma. 2020;16:157–65.
Gravesteijn BY, Sewalt CA, Stocchetti N, Citerio G, Ercole A, Lingsma HF, et al. Prehospital management of traumatic brain injury across Europe: a CENTER-TBI study. Prehosp Emerg Care. 2021;25:629–43.
Pakkanen T, Kämäräinen A, Huhtala H, Silfvast T, Nurmi J, Virkkunen I, et al. Physician-staffed helicopter emergency medical service has a beneficial impact on the incidence of prehospital hypoxia and secured airways on patients with severe traumatic brain injury. Scand J Trauma Resusc Emerg Med. 2017. https://doi.org/10.1186/s13049-017-0438-1.
Davis DP, Idris AH, Sise MJ, Kennedy F, Eastman AB, Velky T, et al. Early ventilation and outcome in patients with moderate to severe traumatic brain injury. Crit Care Med. 2006;34:1202–8.
Lerner EB, Moscati RM. The golden hour: scientific fact or medical ‘urban legend’? Acad Emerg Med. 2001;8:758–60.
Rogers FB, Rittenhouse KJ, Gross BW. The golden hour in trauma: dogma or medical folklore? Injury. 2015;46:525–7.
Nirula R, Maier R, Moore E, Sperry J, Gentilello L. Scoop and run to the trauma center or stay and play at the local hospital: Hospital transfer’s effect on mortality. J Trauma. 2010;69:595–9.
Smith RM, Conn AK. Prehospital care—Scoop and run or stay and play? Injury. 2009. https://doi.org/10.1016/j.injury.2009.10.033.
Hosomi S, Kitamura T, Sobue T, Nakagawa Y, Ogura H, Shimazu T. Association of pre-hospital helicopter transport with reduced mortality in traumatic brain injury in Japan: a nationwide retrospective cohort study. J Neurotrauma. 2022;39:76–85.
Berlot G, La Fata C, Bacer B, Biancardi B, Viviani M, Lucangelo U, et al. Influence of prehospital treatment on the outcome of patients with severe blunt traumatic brain injury: a single-centre study. Eur J Emerg Med. 2009;16:312–7.
Mcconnell KJ, Newgard CD, Mullins RJ, Arthur M, Hedges JR. Mortality benefit of transfer to level I versus level II trauma centers for head-injured patients. Health Serv Res. 2005;40:435–58.
Knapp J, Häske D, Böttiger BW, Limacher A, Stalder O, Schmid A, et al. Influence of prehospital physician presence on survival after severe trauma: systematic review and meta-analysis. J Trauma Acute Care Surg. 2019;87:978–89.
Franschman G, Verburg N, Brens-Heldens V, Andriessen TMJC, Van Der Naalt J, Peerdeman SM, et al. Effects of physician-based emergency medical service dispatch in severe traumatic brain injury on prehospital run time. Injury. 2012;43:1838–42.
Penner K. Fly or drive to stay alive? A systematic review evaluating outcomes following ground versus helicopter prehospital transport in rural patients with moderate to severe traumatic brain injury. Air Med J. 2022;41:33–6.
Kulla M, Helm M, Lefering R, Walcher F. Prehospital endotracheal intubation and chest tubing does not prolong the overall resuscitation time of severely injured patients: a retrospective, multicentrestudy of the Trauma Registry of the German Society of Trauma Surgery. Emerg Med J. 2012;29:497–501.
Meuli L, Zimmermann A, Menges AL, Tissi M, Becker S, Albrecht R, et al. Helicopter emergency medical service for time critical interfacility transfers of patients with cardiovascular emergencies. Scand J Trauma Resusc Emerg Med. 2021. https://doi.org/10.1186/s13049-021-00981-4.
Acknowledgements
We thank Ms. Jeannie Wurz (medical editor, Department of Anaesthesiology and Pain Medicine, Inselspital, Bern University Hospital, University of Bern, Switzerland) for proofreading and linguistic correction of our manuscript.
Funding
None.
Author information
Authors and Affiliations
Contributions
JK and PD wrote the main manuscript text. JK, PD and UP collected and analysed data. MH did the statistical analysis and prepared Fig. 2, Tables 1 and 2. RA supervised the process of creating this paper. LM and SS contributed substantially to conception and discussion. All authors revised the manuscript critically for important intellectual content and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The local ethics committees of Bern and St. Gallen approved the study protocol (Ethics committee Bern: BASEC nr. 2020-01737, study nr. 4690 and St. Gallen: BASEC nr. 2020-01737, 20/122). The local ethics committees granted permission to use patient data without individual informed consent according to the federal act on research involving human beings and the ordinance on human research with the exception of clinical trials. The permission also covered the use of patient data regarding HEMS operations. The investigation was carried out in accordance with the Helsinki declaration and all relevant national guidelines and recommendations.
Consent for publication
Not applicable.
Competing interests
The authors have no competing interests to declare that are relevant to the content of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. Sensitivity analysis of multivariable regression analysis using multiple imputations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Knapp, J., Doppmann, P., Huber, M. et al. Pre-hospital endotracheal intubation in severe traumatic brain injury: ventilation targets and mortality—a retrospective analysis of 308 patients. Scand J Trauma Resusc Emerg Med 31, 46 (2023). https://doi.org/10.1186/s13049-023-01115-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13049-023-01115-8