Abstract
Background
The debridement, antibiotics, and implant retention (DAIR) procedure is an established therapeutic option for periprosthetic knee infections (PKI). However, the efficacy and the indication for this procedure are still controversial.
Methods
All the relevant literatures were systematically reviewed and analyzed. The present study aimed to assess the success rate of DAIR in the management of PKI, identify the factors associated with prognosis of DAIR, and establish a simple algorithm for predicting a high success rate of DAIR.
Results
Totally, 33 studies with 1266 cases were included. The overall success rate following DAIR in the management of PKI was 57.11%. In the subgroup analyses, the factors of “the time from symptoms to debridement was < 3 weeks” and “the bacterial species other than methicillin-resistant Staphylococcus aureus” significantly improved the success rate of DAIR and thus were defined as the major criteria. The statistically insignificant factors of “the open debridement and liner exchange” and “the comorbidity of rheumatoid arthritis” were set as the minor criteria. The success rate of DAIR for PKI meeting all the major criteria and no less than one minor criterion was 80.98%, which was significantly higher than the overall success rate of DAIR (p < 0.05).
Conclusion
PKI cases meeting two major criteria and no less than one minor criterion may confer a high success rate of DAIR. This simple algorithm may contribute to identifying the appropriate PKI patient for DAIR treatment and predicting the prognosis of DAIR.
Similar content being viewed by others

Introduction
Periprosthetic knee infections (PKI) are disastrous complications after joint arthroplasty. The two-stage revision is the gold standard for chronic PKI [1, 2]. However, the patients have to bear two or more major surgeries, which means great sufferings and heavy economic burdens for patients [3]. Current guidelines recommend the procedure of debridement, antibiotics, and implant retention (DAIR) for the early postoperative PKI and the acute hematogenous PKI [4]. However, the success rates varied from 23 to 100% among different studies [4]. One of the plausible explanations is that the preoperative characteristics of patients, such as the timing of DAIR, the bacterial species, and the immunocompetence, are inconsistent among the studies [5, 6]. Moreover, the specific procedure of treatment, like the open debridement or the arthroscopic debridement and the liner exchange or not, may also influence the prognosis of DAIR [7]. The sensitivity of these criteria in determining outcomes is still questionable. The different preoperative characteristics of patients and the varying procedure of DAIR probably account for the inconsistent results among the literatures [5, 8].
The aims of present pooling analysis were to systematically assess the success rate of DAIR in the management of PKI, identify the factors associated with prognosis of DAIR, and establish a simple algorithm for predicting a high success rate of DAIR. To our knowledge, no such analysis has ever been made.
Materials and methods
Literature search
The following sources of data were searched by two reviewers: EMBASE, PubMed, Web of Science, Cochrane Central Register of Controlled Trials, and Cochrane Database of Systematic Reviews. A comprehensive search of these database was performed using the following combinations of the keywords: “knee,” “prosthesis,” “arthroplasty,” “periprosthetic,” “infection,” “debridement,” and “replacement.” No language or date restriction was applied to the search. The final search was conducted on Jan 1, 2018.
Selection criteria
The inclusion criteria for these studies were as follows: (1) the success rate of debridement and prosthesis retaining procedure, (2) infected knee prosthesis, and (3) the data of knee DAIR which could be extracted.
The exclusion criteria were as follows: (1) prolonged suppressive antibiotic therapy after DAIR procedure, (2) sample size was < 5, (3) abstract or conference presentation without peer review, (4) the smaller series from redundant publications, and (5) two-stage revision, arthrodesis, or other therapies were included.
Data extraction and analysis
Three authors (QGX, ZCH, and CXZ) independently screened titles and abstracts, included studies, extracted relevant data, and checked them. Any discrepancy was resolved by discussion. The following data were extracted: first author’s last name, period of the study, patient demographics, symptom duration, surgical procedure, antibiotic therapy, and outcomes.
Assessment of trial quality
Two authors (QGX and ZCH) independently assessed the methodological quality of each study using the Newcastle-Ottawa Scale (NOS) [9]. The NOS with a maximum score of nine is validated for assessing the quality of non-randomized studies, including case-control studies and observational studies [9]. Only studies with a score of > 7 were included in the analysis. The NOS score of each study was shown in Table 1.
Pooling analysis
The pooled mean proportion of success following DAIR procedure in the management of PKI was calculated. We tried to establish a simple algorithm for predicting a high success rate of DAIR. Firstly, the factors associated with prognosis of DAIR were identified based on the included studies. Secondly, the subgroup analyses were made on those identified factors. If statistical difference was obtained, the factor was defined as the major criterion, which meant that this criterion was obligatory for the algorithm. If no statistical difference was found, the factor was defined as the minor criterion. Then, we calculated and compared the success rate of DAIR cases meeting all the major criteria and different quantity of the minor criteria. Finally, we judged how many minor criteria were needed for the algorithm.
Statistical analysis
Information on the number of treated patients was collected. Data were calculated with the SPSS statistical software version 20.0 (SPSS Inc., Chicago, Illinois) and Microsoft Excel 2013 (Microsoft, Redmond, Washington). The data of all the outcomes conformed to the Bernoulli distribution. The weighted mean difference was calculated with 95% confidence intervals (CI) for continuous outcomes. The subgroup analysis was evaluated using a chi-squared test and Fisher’s exact test. The statistical significance was set at p < 0.05.
Results
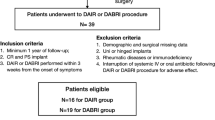
The literature search initially yielded 1328 papers, of which 1266 papers were excluded and the full texts of the remaining 62 papers were reviewed. After careful review, 33 studies of 1266 cases were included in the present analysis (Fig. 1). The characteristics of the included studies were shown in Table 1. The mean NOS score of included studies was 8.06 (7–9). The pooled mean proportion of success following DAIR procedure in the management of PKI was 57.11% (723/1266 cases, 95% CI: 54.4–59.8%) [5, 6, 8, 10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39] (Table 1).
The time from infection symptoms to debridement was found to be associated with the difference in the success rate of DAIR (Fig. 2). In the studies where the mean time from symptoms to debridement was < 7 days, the pooled success rate was 71.62% (159/222 cases, 95% CI: 65.6–77.6%). Similarly, in the studies where the mean time from symptoms to debridement was < 3 weeks, the pooled success rate was 71.15% (254/357 cases, 95% CI: 66–76%) [5, 15, 28, 29, 34, 37,38,39]. However, the pooled rate of success where the mean time from symptoms to debridement was > 3 weeks was only 35.09% (20/57 cases, 95% CI: 23–47%) [15, 32, 38, 39]. Since the difference was statistically significant (p < 0.05), “the time from symptoms to debridement was < 3 weeks” was set as the major criterion (Table 2).
Six studies reported the success rates of cases with infection of methicillin-resistant Staphylococcus aureus (MRSA) and non-MRSA bacteria [12, 15, 17, 24, 29, 40]. The overall proportion of success for MRSA and non-MRSA bacteria was 35% (14/40 cases, 95% CI: 19.6–50.4%) and 68.5% (115/168 cases, 95% CI: 61.4–75.6%), respectively. This difference was statistically significant (p < 0.05). As a consequence, “the non-MRSA bacterial species” was also set as the major criterion (Table 2).
Eleven studies chose open debridement and liner exchange [17, 20, 32, 41] while four studies performed arthroscopic debridement and liner retention [17, 20, 32, 41]. The success rate was 74% (128/173 cases, 95% CI: 67–81) and 66.67% (36/54 cases, 95% CI: 54–79), respectively. The difference was not statistically significant (p = 0.301). Accordingly, “the open debridement and liner exchange” was set as the minor criterion (Table 2).
Five studies reported the success rates of patients with rheumatoid arthritis (RA) [5, 15, 29, 36, 38]. The success rate of RA and non-RA was 44.74% (17/38 cases, 95% CI: 29–61) and 57.6% (87/151 cases, 95% CI: 50–65), respectively. No statistical difference was found (p = 0.201). So “the comorbidity of RA” was also set as the minor criterion (Table 2).
After inclusion of the studies meeting two major criteria and no less than one minor criterion, the success rate of DAIR was 80.98% (149/184 cases, 95% CI: 75.3–86.7) [5, 6, 8, 12, 17, 20, 28, 29, 34, 37,38,39]. If the studies meeting two major criteria and two minor criteria were only included, the success rate of DAIR was 80.9% (72/89 cases, 95% CI: 73–89%) [5, 12, 29, 37]. Both the success rates were not statistically different (p = 0.94).
Fourteen studies were analyzed based on Tsukayama’s classification [42]. The success rate of DAIR for type II (the early infection within 30 days after the index arthroplasty) and type III (the acute hematogenous infection) was 79.17% (95/120 cases, 95% CI: 71.8–86.5) and 61.65% (164/266 cases, 95% CI: 55.8–67.5), respectively. The difference was statistically different (p < 0.05) [5, 8, 15, 17, 18, 20, 24, 26, 28, 29, 32,33,34, 36] (Table 3).
Multiple debridements were chosen in ten studies if a single debridement fail [14, 17, 18, 20, 28, 29, 32,33,34, 43]. The success rate of a single debridement and multiple debridements was 57.23% (190/332 cases, 95% CI: 51.9–62.6) and 49.25% (33/67 cases, 95% CI: 37.0–61.5), respectively. The difference was not statistically different (p = 0.281).
Discussion
There are controversies about the therapeutic efficacy of DAIR on PKI. This pooling analysis is the first to establish a simple algorithm for predicting a high success rate of DAIR in treatment of PKI. The most important finding was that the PKI cases meeting two major criteria (“the time from symptoms to debridement was < 3 weeks” and “the non-MRSA bacterial species”), and no less than one minor criterion (“the open debridement and liner exchange” and “the comorbidity of RA”) conferred a success rate of 80.98% of DAIR. Additionally, the success rate of DAIR is significantly higher for the Tsukayama’s type II infection compared with the type III infection.
Although it is agreed that DAIR should be carried out as soon as possible for fear of biofilm formation, the deadline of DAIR is controversial. Hartman et al. [36] performed DAIR within 4 weeks from symptom onset to debridement. Cury et al. [6] started DAIR within 3 weeks after onset of infection symptoms. In a previous meta-analysis, Tsang et al. [44] reported a similar success rate of 64.7% in infected hip arthroplasty treated with DAIR. They found that the success rate was significantly higher when the time from symptoms to debridement was < 7 days compared with > 7 days. In clinical practice, however, it is difficult to perform DAIR timely within 7 days after symptoms of PKI. In the present analysis, we showed that there was no significant difference in the success rate of DAIR between < 7 days and < 3 weeks. The success rate sharply dropped after 3 weeks. Resultingly, we suggest that the time limit of DAIR for PKI could be prolonged to 3 weeks. “The time from symptoms to debridement was < 3 weeks” was set as the major criterion of the algorithm for predicting a high success rate of DAIR. It is assumed that the difference in infection site may partly account for the difference of time limit between Tsang’s analysis and the present study.
It is well accepted that the infection of MRSA is associated with a high failure rate of DAIR. The study by Bradbury et al. [40] showed that the success rate of DAIR against antibiotic-resistance bacteria including MRSA was strikingly lower than that against antibiotic-sensitive bacteria. Even in antibiotic-resistance bacteria, Peel et al. [45] found that MRSA was more likely to fail treatment than methicillin-resistant coagulase-negative staphylococci. Duque et al. [12] reported only 20% of the success rate of DAIR for MRSA infections. Our present analysis demonstrated that MRSA had a relative risk of treatment failure of 2.06 compared with non-MRSA bacteria, which agrees with the previous literatures. Since “non-MRSA infection” is an independent predicting factor for success of DAIR treatment, it was chosen as the major criterion.
Previous studies showed that open debridement and liner exchange could reduce bacterial load and increase the success rate of DAIR [7, 44]. Furthermore, it is reported that liner exchange was a strong predictor for treatment success of DAIR [46]. In the present pooling analysis, the success rate of DAIR with open debridement and liner exchange was slightly higher than that with arthroscopic debridement and liner retention though the difference was statistically insignificant. We note that the times from symptoms to debridement were both less than 1 week for two groups, which may bias the comparison. Thus, “open debridement and liner exchange” was set as the minor criterion of DAIR success.
It is believed that the patients with poor immunocompetence, such as RA, had an inferior resistance to PKI. Berbari et al. [47] reported only 32% of success rate of DAIR for prosthetic joint infections in patients with RA. In the present study, the patients with RA presented a lower success rate of DAIR compared with those without RA. Considering no statistical significance for the factor of RA, “the comorbidity of RA” was set as the minor criterion of DAIR success.
The present analysis conferred a low success proportion of 57.11% for PKI treated with DAIR, which is similar to what was reported in previous meta-analyses. Romano et al. [48] reported a low success rate of 45.9% after DAIR in hip and knee prosthesis infections. Tsang et al. [44] showed that the success rate following DAIR in the management of an infected hip arthroplasty was 64.7%. We aimed to establish a practical and simple algorithm as a tool for improving the success rate of DAIR. After selecting patients who meet two major criteria and no less than one minor criterion, the success rate of DAIR increased to over 80%. The algorithm may provide a reference of choosing the appropriate patient for DAIR treatment.
Our subgroup analysis showed that the early postoperative infection presented a higher success rate of DAIR than the acute hematogenous infection, which accords with the previous reports [15, 49]. Two reasons possibly account for it: (1) the actual duration of symptoms in the acute hematogenous infection is always longer than what is recalled by the patient, and (2) some acute hematogenous infection was essentially the acute exacerbation of a latent chronic infection.
There were limitations in our study. Firstly, the results were limited by the relative low quality and the heterogeneity of the available data. Ignoring this source of data would have underpowered the analysis and influenced the accuracy of our findings. Therefore, the present data have to be interpreted with caution, given the biases. Secondly, due to the relatively small sample size in subgroup analyses, further robust researches like randomized controlled trials and case-control trials will be indispensable for confirming the criteria and algorithm.
Conclusion
The overall success proportion of DAIR for treating PKI is 57.11%. In our established algorithm, PKI cases meeting two major criteria (“the time from symptoms to debridement was < 3 weeks” and “the non-MRSA bacterial species”) and no less than one minor criterion (“the open debridement and liner exchange” and “the comorbidity of RA”) conferred a success rate of 80.98% of DAIR. This simple algorithm may contribute to identifying the appropriate patient for DAIR treatment and predicting the prognosis of DAIR in clinical practice.
Availability of data and materials
The data of the manuscript was presented in the paper and additional files.
Abbreviations
- DAIR:
-
Antibiotics and implant retention
- MRSA:
-
Methicillin-resistant Staphylococcus aureus
- PKI:
-
Periprosthetic knee infections
- RA:
-
Rheumatoid arthritis
References
Puhto AP, Puhto TM, Niinimaki TT, Leppilahti JI, Syrjala HP. Two-stage revision for prosthetic joint infection: outcome and role of reimplantation microbiology in 107 cases. J Arthroplast. 2014;29(6):1101.
Bryan AJ, Abdel MP, Sanders TL, Fitzgerald SF, Hanssen AD, Berry DJ. Irrigation and debridement with component retention for acute infection after hip arthroplasty: improved results with contemporary management. J Bone Joint Surg Am. 2011;99(23):2017.
Cahill JL, Shadbolt B, Scarvell JM, Smith PN. Quality of life after infection in total joint replacement. J Orthop Surg. 2008;16(1):58.
Osmon DR, Berbari EF, Berendt AR, Lew D, Zimmerli W, Steckelberg JM, Rao N, Hanssen A, Wilson WR. Diagnosis and management of prosthetic joint infection: clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis. 2013;56(1):e1.
Son WS, Shon OJ, Lee DC, Park SJ, Yang HS. Efficacy of open debridement and polyethylene exchange in strictly selected patients with infection after total knee arthroplasty. Knee Surg Related Res. 2017;29(3):172.
Cury Rde P, Cinagawa EH, Camargo OP, Honda EK, Klautau GB, Salles MJ. Treatment of infection after total knee arthroplasty. Acta Ortop Brasileira. 2015;23(5):239.
Qasim SN, Swann A, Ashford R. The DAIR (debridement, antibiotics and implant retention) procedure for infected total knee replacement - a literature review. Sicot-J. 2017;3:2.
He R, Yang L, Guo L, Chen H, Zhang Y, Jiang DM. Management of acute hematogenous infection following total knee arthroplasty: a case series of 11 patients. Orthop Surg. 2016;8(4):475.
BS GAW, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of non-randomized studies in meta-analyses; 2016.
Urish KL, Bullock AG, Kreger AM, Shah NB, Jeong K, Rothenberger SD. A multicenter study of irrigation and debridement in total knee arthroplasty periprosthetic joint infection: treatment failure is high. J Arthroplast. 2017.
Riesgo AM, Park BK, Herrero CP, Yu S, Schwarzkopf R, Iorio R. Vancomycin povidone-iodine protocol improves survivorship of periprosthetic joint infection treated with irrigation and debridement. J Arthroplasty. 2017.
Duque AF, Post ZD, Lutz RW, Orozco FR, Pulido SH, Ong AC. Is there still a role for irrigation and debridement with liner exchange in acute periprosthetic total knee infection? J Arthroplast. 2017;32(4):1280.
Nakano N, Matsumoto T, Ishida K, Tsumura N, Muratsu H, Hiranaka T, Kuroda R, Kurosaka M. Factors influencing the outcome of deep infection following total knee arthroplasty. Knee. 2015;22(4):328.
Lizaur-Utrilla A, Gonzalez-Parreno S, Gil-Guillen V, Lopez-Prats FA. Debridement with prosthesis retention and antibiotherapy vs. two-stage revision for periprosthetic knee infection within 3 months after arthroplasty: a case-control study. Clin Microbiol Infect. 2015;21(9):851.e11.
Koh IJ, Han SB, In Y, Oh KJ, Lee DH, Kim TK. Open debridement and prosthesis retention is a viable treatment option for acute periprosthetic joint infection after total knee arthroplasty. Arch Orthop Trauma Surg. 2015;135(6):847.
Tornero E, Martinez-Pastor JC, Bori G, Garcia-Ramiro S, Morata L, Bosch J, Mensa J, Soriano A. Risk factors for failure in early prosthetic joint infection treated with debridement. Influence Etiol Antibiot Treat J Appl Biomater Funct Mater. 2014;12(3):129.
Chung JY, Ha CW, Park YB, Song YJ, Yu KS. Arthroscopic debridement for acutely infected prosthetic knee: any role for infection control and prosthesis salvage? Arthroscopy. 2014;30(5):599.
Stryker LS, Abdel MP, Hanssen AD. Predictive value of inflammatory markers for irrigation and debridement of acute TKA infection. Orthopedics. 2013;36(6):765.
Royo A, Bertrand ML, Ramos L, Fernandez-Gordillo F, Guerado E. Is there still a place for continuous closed irrigation in the management of periprosthetic total knee infection? Open Orthop J. 2013;7:205.
Liu CW, Kuo CL, Chuang SY, Chang JH, Wu CC, Tsai TY, Lin LC. Results of infected total knee arthroplasty treated with arthroscopic debridement and continuous antibiotic irrigation system. Indian J Orthop. 2013;47(1):93.
Kuiper JW, Vos SJ, Saouti R, Vergroesen DA, Graat HC, Debets-Ossenkopp YJ, Peters EJ, Nolte PA. Prosthetic joint-associated infections treated with DAIR (debridement, antibiotics, irrigation, and retention): analysis of risk factors and local antibiotic carriers in 91 patients. Acta Orthop. 2013;84(4):380.
Fehring TK, Odum SM, Berend KR, Jiranek WA, Parvizi J, Bozic KJ, Della Valle CJ, Gioe TJ. Failure of irrigation and debridement for early postoperative periprosthetic infection. Clin Orthop Relat Res. 2013;471(1):250.
Koyonos L, Zmistowski B, Della Valle CJ, Parvizi J. Infection control rate of irrigation and debridement for periprosthetic joint infection. Clin Orthop Relat Res. 2011;469(11):3043.
Gardner J, Gioe TJ, Tatman P. Can this prosthesis be saved?: implant salvage attempts in infected primary TKA. Clin Orthop Relat Res. 2011;469(4):970.
Cobo J, Miguel LGS, Euba G, Rodríguez D, García-Lechuz JM, Riera M, Falgueras L, Palomino J, Benito N, del Toro MD, Pigrau C, Ariza J. Early prosthetic joint infection: outcomes with debridement and implant retention followed by antibiotic therapy. Clin Microbiol Infect. 1632;17(11):2011.
Choi H-R, von Knoch F, Zurakowski D, Nelson SB, Malchau H. Can implant retention be recommended for treatment of infected TKA? Clinical orthopaedics and related research® 469(4): 961; 2011.
Byren I, Bejon P, Atkins BL, Angus B, Masters S, McLardy-Smith P, Gundle R, Berendt A. One hundred and twelve infected arthroplasties treated with ‘DAIR’ (debridement, antibiotics and implant retention): antibiotic duration and outcome. J Antimicrob Chemother. 2009;63(6):1264.
Aboltins CA, Page MA, Buising KL, Jenney AW, Daffy JR, Choong PF, Stanley PA. Treatment of staphylococcal prosthetic joint infections with debridement, prosthesis retention and oral rifampicin and fusidic acid. Clin Microbiol Infect. 2007;13(6):586.
Tsumura H, Ikeda S, Ono T, Itonaga I, Taira H, Torisu T. Synovectomy, debridement, and continuous irrigation for infected total knee arthroplasty. Int Orthop. 2005;29(2):113.
Berdal JE, Skra°mm I, Mowinckel P, Gulbrandsen P, Bjørnholt JV Use of rifampicin and ciprofloxacin combination therapy after surgical debridement in the treatment of early manifestation prosthetic joint infections Clin Microbiol Infect 11(10): 843, 2005.
Deirmengian C, Greenbaum J, Stern J, Braffman M, Lotke PA, Booth RE Jr, Lonner JH. Open debridement of acute gram-positive infections after total knee arthroplasty. Clin Orthop Relat Res. 2003;129(416).
Waldman BJ, Hostin E, Mont MA, Hungerford DS. Infected total knee arthroplasty treated by arthroscopic irrigation and debridement. J Arthroplast. 2000;15(4):430.
Segawa H, Tsukayama DT, Kyle RF, Becker DA, Gustilo RB. Infection after total knee arthroplasty. A retrospective study of the treatment of eighty-one infections. J Bone Joint Surg Am. 1999;81(10):1434.
Mont MA, Waldman B, Banerjee C, Pacheco IH, Hungerford DS. Multiple irrigation, debridement, and retention of components in infected total knee arthroplasty. J Arthroplast. 1997;12(4):426.
Wasielewski RC, Barden RM, Rosenberg AG. Results of different surgical procedures on total knee arthroplasty infections. J Arthroplast. 1996;11(8):931.
Hartman MB, Fehring TK, Jordan L, Norton HJ. Periprosthetic knee sepsis. The role of irrigation and debridement. Clin Orthop Relat Res. 1991;113(273).
Burger RR, Basch T, Hopson CN. Implant salvage in infected total knee arthroplasty. Clin Orthop Relat Res. 1991;(273):105.
Schoifet SD, Morrey BF. Treatment of infection after total knee arthroplasty by debridement with retention of the components. J Bone Joint Surg Am. 1990;72(9):1383.
Ivey FM, Hicks CA, Calhoun JH, Mader JT. Treatment options for infected knee arthroplasties. Rev Infect Dis. 1990;12(3):468.
Bradbury T, Fehring TK, Taunton M, Hanssen A, Azzam K, Parvizi J, Odum SM. The fate of acute methicillin-resistant Staphylococcus aureus periprosthetic knee infections treated by open debridement and retention of components. J Arthroplasty. 2009;24(6, Supplement):101.
Ilahi OA, Al-Habbal GA, Bocell JR, Tullos HS, Huo MH. Arthroscopic debridement of acute periprosthetic septic arthritis of the knee. Arthroscopy. 2005;21(3):303.
Tsukayama D, Estrada R, Gustilo R. Infection after total hip arthroplasty. A study of the treatment of one hundred and six infections. J Bone Joint Surg Am. 1996;78(4):512.
Aboltins CA, Dowsey MM, Buising KL, Peel TN, Daffy JR, Choong PF, Stanley PA. Gram-negative prosthetic joint infection treated with debridement, prosthesis retention and antibiotic regimens including a fluoroquinolone. Clin Microbiol Infect. 2011;17(6):862.
Tsang SJ, Ting J, Simpson A, Gaston P. Outcomes following debridement, antibiotics and implant retention in the management of periprosthetic infections of the hip: a review of cohort studies. Bone Joint J. 2017;99-b(11):1458.
Peel TN, Buising KL, Dowsey MM, Aboltins CA, Daffy JR, Stanley PA, Choong PF. Outcome of debridement and retention in prosthetic joint infections by methicillin-resistant staphylococci, with special reference to rifampin and fusidic acid combination therapy. Antimicrob Agents Chemother. 2013;57(1):350.
Wouthuyzen-Bakker M, Sebillotte M, Lomas J, Taylor A, Palomares EB, Murillo O, Parvizi J, Shohat N, Reinoso JC, Sanchez RE, Fernandez-Sampedro M, Senneville E, Huotari K, Barbero JM, Garcia-Canete J, Lora-Tamayo J, Ferrari MC, Vaznaisiene D, Yusuf E, Aboltins C, Trebse R, Salles MJ, Benito N, Vila A, MDD T, Kramer TS, Petersdorf S, Diaz-Brito V, Tufan ZK, Sanchez M, Arvieux C, Soriano A. Clinical outcome and risk factors for failure in late acute prosthetic joint infections treated with debridement and implant retention. J Infect. 2019;78(1):40.
Berbari EF, Osmon DR, Duffy MC, Harmssen RN, Mandrekar JN, Hanssen AD, Steckelberg JM. Outcome of prosthetic joint infection in patients with rheumatoid arthritis: the impact of medical and surgical therapy in 200 episodes. Clin Infect Dis. 2006;42(2):216.
Romano CL, Manzi G, Logoluso N, Romano D. Value of debridement and irrigation for the treatment of peri-prosthetic infections. A systematic review. Hip Int. 2012;22(Suppl 8):S19.
Fink B, Schuster P, Schwenninger C, Frommelt L, Oremek D. A standardized regimen for the treatment of acute postoperative infections and acute hematogenous infections associated with hip and knee arthroplasties. J Arthroplast. 2017;32(4):1255.
Acknowledgements
We thank all the authors of the included literatures for their contribution to our systematic review. And we thank the National Natural Science Foundation of China for the support of this work.
Funding
This work was supported by the National Natural Science Foundation of China (81472113).
Author information
Authors and Affiliations
Contributions
XZC contributed to design the experiments, extract and analyze data, and write the manuscript. QGX contributed to retrieve literatures, extract and analyze data, and write the manuscript. ZCH contributed to retrieve literatures and extract and analyze data. And YSG participated in the design of the experiments. All authors listed read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
No benefits in any forms have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript. And the authors declare that they have no non-financial or financial conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Qu, GX., Zhang, CH., Yan, SG. et al. Debridement, antibiotics, and implant retention for periprosthetic knee infections: a pooling analysis of 1266 cases. J Orthop Surg Res 14, 358 (2019). https://doi.org/10.1186/s13018-019-1378-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-019-1378-4