Abstract
Background
There is growing urgency to tackle issues of equity and justice in the USA and worldwide. Health equity, a framing that moves away from a deficit mindset of what society is doing poorly (disparities) to one that is positive about what society can achieve, is becoming more prominent in health research that uses implementation science approaches. Equity begins with justice—health differences often reflect societal injustices. Applying the perspectives and tools of implementation science has potential for immediate impact to improve health equity.
Main text
We propose a vision and set of action steps for making health equity a more prominent and central aim of implementation science, thus committing to conduct implementation science through equity-focused principles to achieve this vision in U.S. research and practice. We identify and discuss challenges in current health disparities approaches that do not fully consider social determinants. Implementation research challenges are outlined in three areas: limitations of the evidence base, underdeveloped measures and methods, and inadequate attention to context. To address these challenges, we offer recommendations that seek to (1) link social determinants with health outcomes, (2) build equity into all policies, (3) use equity-relevant metrics, (4) study what is already happening, (5) integrate equity into implementation models, (6) design and tailor implementation strategies, (7) connect to systems and sectors outside of health, (8) engage organizations in internal and external equity efforts, (9) build capacity for equity in implementation science, and (10) focus on equity in dissemination efforts.
Conclusions
Every project in implementation science should include an equity focus. For some studies, equity is the main goal of the project and a central feature of all aspects of the project. In other studies, equity is part of a project but not the singular focus. In these studies, we should, at a minimum, ensure that we “leave no one behind” and that existing disparities are not widened. With a stronger commitment to health equity from funders, researchers, practitioners, advocates, evaluators, and policy makers, we can harvest the rewards of the resources being invested in health-related research to eliminate disparities, resulting in health equity.
Similar content being viewed by others
Background
There is growing urgency to tackle issues of equity and justice [1, 2], which is driven by greater awareness of decades-long increases in income and wealth inequality [3] and the visibility and impacts of structural racism and associated societal problems [4]. Longstanding socioeconomic and racial/ethnic disparities in numerous health outcomes are prominent among these societal challenges and are now exacerbated by the impacts of the COVID-19 pandemic [5]. The focus on equity is spreading quickly across many sectors and in very public ways [6]. A renewed focus on social and structural determinants of health, including racism and discrimination, is also advancing within the scientific community [7].
Health equity is a framing that moves away from a deficit mindset of what society is doing poorly (disparities) to one that is positive about what society can achieve [8]. Beginning in Europe, there has been growing attention on health equity—the commitment to reduce and ultimately eliminate health disparities [9,10,11,12]. In the UK, Whitehead framed health inequities as not only avoidable but also unjust [13]. Braveman and colleagues pointed out that achieving health equity involves closing health gaps between those less and those more advantaged while also improving the health of the population overall [9]. Health inequity is addressed through a range of approaches: changing large-scale policies to offset historical injustices, changing policies and practices within healthcare settings, and changing organizational or community contexts that influence health.
A clear distinction is needed between systems, programs, or policies that are equitable, that is, accounting for systematic social disadvantage and injustice, and those that might seem fair because they use the language of equality. Viewing everyone equally assumes, incorrectly, that all population groups have similar circumstances, resources, and opportunities for achieving good health. For example, changing policies that target longstanding injustices fosters equity by improving social and economic conditions, such as poverty and the opportunity structure for education, housing, employment, and access to healthcare.
Implementation science is an area of research with particular potential to accelerate progress toward achieving health equity goals [14]. Implementation science seeks to understand and influence how scientific evidence is put into practice for health improvement [15]. It offers an explicit response to the decades of scientific progress that generally have not translated into equitable improvements in population health [16]. Applying the perspectives and tools of implementation science has potential for immediate improvement of health equity. Moreover, a greater emphasis on health equity could attract new and more diverse scientific talent to fully invest in implementation science solutions.
Although a focus on disparities and/or health equity has long been an emphasis of implementation science, a more explicit priority on health equity is timely [14, 17,18,19,20]. Elements of health equity are now being more prominently considered in implementation science models (aka, frameworks, theories), in the context of implementation of interventions, and in study methods. Recent conceptual models, such as the Health Equity Implementation Framework [20], have begun to examine more deeply a broad array of social determinants of health, rather than simply adding a disparities component to the large set of existing implementation science frameworks [21]. Incorporating a strong equity focus in implementation science requires not only a deliberate emphasis on the needs, culture, and history of the populations and communities [22, 23], but also more critical analyses and deeper understanding of systems and policies, including care delivery and provider attitudes from which inequities might arise. Equity-centered research relies on meaningful engagement and partnership with multiple stakeholders, builds on existing resources, develops shared goals, and integrates knowledge and action that lead to a fairer distribution of power and the benefits of an intervention for all partners [23,24,25].
In this article, we propose a vision for making health equity the highest priority in implementation science, and thus a central indicator of the field’s success. This means actively seeking and positively addressing issues of diversity and disadvantage to improve the relevance, effectiveness, equity, and impact of implementation science. We identify and discuss challenges in current approaches to addressing health disparities in the context of implementation science and provide recommendations to move the field forward to achieve health equity. While our article is focused largely on public health and health equity challenges in the USA, we draw upon literature and experiences from other regions of the globe.
Key challenges
Here, we address three important challenges for health equity in implementation science. We propose that each can be overcome, and provide a set of recommendations with specific steps to address them.
To identify relevant literature for this article, a review of reviews was conducted using searches for English-language documents published between January 2015 and February 2021. Electronic databases searched included PubMed, Google, and Google Scholar. Keywords included “health equity,” “heath disparities,” “health inequalities,” “implementation,” and “social determinants of health.” Following screening of titles and abstracts, full papers were reviewed and examined for the following information: focus of the study; type of review (i.e., narrative review, review of systematic reviews, scoping review, systematic review, umbrella review); and selected findings of relevance to health equity and implementation science.
Limitations of the evidence base
There are at least two important limitations of current scientific evidence that must be overcome to achieve health equity goals: (1) too few evidence-based interventions (EBIs) adequately include a systems approach or address upstream social determinants and (2) the lack of diversity in study samples and settings limits applicability of research findings in ways that unintentionally benefit some populations more than others, potentially exacerbating health inequities.
In implementation research, an EBI is central [26]—often addressing some well-established risk factor (e.g., tobacco use, lack of cancer screening) [27, 28]. However, the origins of many risk behaviors and exposures are shaped by adverse social determinants of health and root causes of inequities (e.g., structural racism, unjust allocation of power and resources). Even though we have a deep literature on the importance of social determinants [8, 10, 29, 30], most repositories of EBIs are organized around downstream diseases and risk factors, with inadequate attention to upstream factors and solutions [31].
Approaches for developing EBIs characteristically follow a reductionist tradition, where the objective is to reconstruct reality by its linear, cause and effect parts [32], not acknowledging or attending to broader systems in which the risk behavior is embedded [33]. Typically, EBI deployment involves developing and testing an intervention by researchers in a specific population, identifying discordance between where and with whom the EBI was originally tested and a new setting and population of interest (contextual differences), and then adapting the EBI to fit [34]. A more practice-based, systems approach is needed for achieving equity. For example, a health equity approach recognizes that race-based discrimination through one system (e.g., housing) is reinforced in other interlocking systems (e.g., transportation, education) and identifies how these systems can undercut the effectiveness, in real-world practice, of an intervention developed in a best-case, controlled efficacy study. A systems-based approach identifies the leverage points within and across societal sectors with the highest potential for impact on health equity [35, 36].
There is also evidence for an “inverse prevention law,” which suggests that those in most need of benefiting from an EBI may be the least likely to receive it [37]. When an EBI improves health across the general population, it may have an unintended consequence of increasing health inequities for some groups (e.g., low-income populations, certain minority groups) who were less likely to be reached or reached effectively [37,38,39]. Widening of disparities is a clear indication of the failure of science, practice, and policy to adequately achieve equity. In a review of public health interventions in high-income countries, Lorenc and colleagues found that certain interventions (media campaigns, workplace smoking bans) showed evidence of increasing inequities affecting lower socioeconomic groups [37]. In a policy-focused umbrella review, Thomas and colleagues studied a wide range of policy approaches across seven public health areas: tobacco, alcohol, food and nutrition, reproductive health services, the control of infectious diseases, the environment, and workplace regulations [39]. While most policies were shown to either reduce inequities or were neutral toward inequities, some appear to increase inequities (e.g., folic acid mass media campaigns, low emission zones in cities). Implementation of broad policy approaches thought to be universal may require adjustments to aspects of disadvantaged settings and populations to achieve equitable effects.
Underdeveloped measures and methods
The measures and methods for implementation science are evolving but to date with a limited emphasis on equity and, therefore, a lack of methods that are sensitive to equity issues. For example, upstream interventions which are often focused on policy changes are likely to decrease inequities if appropriately designed [37], but a review of measures of policy implementation found that none of the 170 measures used in a diverse set of studies had an explicit focus on equity [40].
Policy and other interventions that address fundamental health equity issues should be studied with the strongest designs possible. In some cases, the biomedical “gold standard” designs (e.g., the randomized controlled trial) can be used, including cluster-randomized trials [41] and stepped-wedge designs [42]. There is growing literature on how to conduct randomized trials that are equity-relevant [43,44,45]. In other cases, particularly when the independent variable (e.g., a policy) cannot be randomized, non-randomized designs and methods are appropriate (e.g., time-series designs, quasi-experiments, natural experiments, difference in difference studies) [41, 46]. This range of study methods can help with understanding and addressing policies and equity-related issues in various contexts [41]. Also relevant are pragmatic trials that address issues of importance to key stakeholders by conducting research in real-world conditions, seeking to enhance external validity and other information relevant to transferability to other settings [47]. Such pragmatic approaches facilitate equity-driven implementation science due to their ability to assess multilevel impacts and an emphasis on who benefits and who does not benefit from an EBI [48].
Inadequate attention to context
Context is a central feature of implementation science, yet it is frequently poorly defined or goes unreported [49]. Often context relates to characteristics of a priority population of focus or the setting within which an EBI is being delivered [50, 51]. Failure to fully account for context limits the applicability and generalizability of study findings to different populations, settings, and time periods [51]. Gaps in our current approaches to context include (1) inadequate attention to macro forces that shape implementation and (2) a need to re-visit the role of EBI adaptation.
To advance equity, we need to more fully account for (macro-level) historical, cultural, economic, and political forces that shape implementation in low-resource settings and communities within the USA and in other countries [14, 52]. When implementing or scaling up an EBI, contexts should be conceptualized in terms of aspects of the intervention and its delivery that are likely to differ from those of the original study population in populations affected by inequities, focusing on those factors that are likely to influence intervention uptake, salience, and effectiveness. First, during implementation planning, a community assessment should account for historical, cultural, and system factors such as structural racism and mistrust of health systems [53]. Second, selection of an EBI is a critical part of implementation and should avoid the assumption that any EBI is good for anyone in any context [54]. And third, it is useful to consider contextual issues across all levels of a socio-ecological framework (individual, interpersonal, organizational, community, policy) [52]. Table 1 summarizes reviews of equity-relevant studies describing essential implementation contextual elements for interventions among disadvantaged populations and low-resource settings [55,56,57,58,59].
Contextual conditions drive adaptation—e.g., how an EBI needs to be adapted for a population different from the one with which it was originally developed [60]. However, it is worth re-examining the very concept of adaptation, which one could argue illustrates the relative failure of science to develop relevant solutions for disadvantaged populations. Too often, adaptation is an exercise in retrofitting EBIs to underserved populations and under-resourced settings. In a true equity approach to implementation, a goal might be a steady reduction in the need for EBI adaptation when more and more EBIs are developed in circumstances with the least, rather than the most resources.
Recommendations
To tackle these and related challenges, we offer 10 recommendations (Table 2). Each is directly linked to the challenges noted and is based on the existing literature and the authors’ experiences.
Improving the evidence base
Link social determinants with health outcomes
Many funders of research in public health and healthcare delivery (including those in implementation science) tend to require studies that show effects on traditional clinical and behavioral outcomes (e.g., cancer screening rates, rates of depression, rates of infectious disease) [61]. A clear need for health equity in implementation science is the ability to understand pathways between social determinants of health and outcomes of relevance to various stakeholders, recognizing that the impact may be neither direct nor immediate, but still profound and measurable. There is a substantial and growing body of evidence linking interventions on social determinants of health to a broad range of health outcomes (Table 3) [4, 38, 39, 62,63,64,65,66,67,68]. In primary care studies, there are multiple ways in which social determinants of health are increasingly being addressed (e.g., screening for social risk factors, linking patients with local resources) [69]. In addition, it is important to consider social determinants as potential moderators of health behavior change [70].
There are opportunities for researchers to more fully consider social determinants of health as they design studies. To inform future studies and to synthesize existing literature, several useful guidelines and evidence frameworks can be applied. For example, equity and social determinants are included in the APEASE criteria [71], the GRADE Evidence to Decision framework [72, 73], and an expanded version of CONSORT [74,75,76,77].
Build equity into all policies
Policies, in the form of laws and administrative regulations, have profound effects on population health and health equity. Policy implementation is an under-studied area, particularly in the USA [78, 79]. Research on policy implementation seeks to understand the complexity of the policy process to increase the likelihood that research evidence is a meaningful part of policy decisions. In this section, we focus on “Big P” policies (i.e., laws, administrative rules, and regulations), although in a later section, “small p” policies (i.e., organizational changes, non-governmental professional guidelines) are briefly considered.
Lessons can be drawn from the Health in All Policies (HiAP) movement which recognizes that our greatest health challenges are complex and strongly determined by policy and social determinants [80, 81]. The HiAP approach seeks to incorporate health considerations in decision-making across sectors and policy topics. We propose a new framing as Equity in All Policies (EiAP), in which equity is a primary consideration, not merely one of many considerations. An EiAP approach would include analyzing barriers to policy change, the impacts of policy decisions on equity, both retrospectively and prospectively, with a particular emphasis on aspects of policy design that can privilege or disadvantage certain population groups [39, 82, 83]. Lack of evidence often is not the main barrier to policy action to address equity, more often political will is the biggest challenge [30]. To build political will, new approaches are also needed for framing and communicating the health equity benefits to various segments of policy audiences (e.g., progressive versus conservative) via audience research studies [84].
Improving measures and methods
Use equity-relevant metrics
A public health adage is “what gets measured, gets done” [85]. Most existing measures focus on ultimate outcomes, such as disparities in health status, and do not directly measure factors that lie along the pathway to inequity or equity. Equity measurement should include three elements (1) an indicator of health or a modifiable determinant of health (e.g., living conditions, policies), (2) an indicator of social position (e.g., economic stability, educational attainment), and (3) a method for comparing health or a health determinant across social strata (e.g., a ratio of rates) [86]. Two groups of metrics need to be developed and used: (1) broad equity measures of social determinants of health that could be used to measure progress in communities and (2) measures specific to equity and implementation science for use in research studies.
At a population level, representing the success or failure of implementation, we need to expand our usual surveillance metrics (e.g., behavioral risk factors, mortality) and crude area-level measures (e.g., the Area Deprivation Index) to concentrate more on upstream factors. For example, surveillance systems should track social determinants such as third grade reading literacy, unemployment rates, incarceration rates, and the percentage of households that pay over 30% of their income for housing.
Within implementation research studies, we need to go deeper into the underlying causes of disparities, identify new metrics, and include these in our studies. For example, to measure disadvantage, many studies measure household income but few measure household wealth. The Black-White difference in median household income is 1.7-fold yet the difference in Black-White median household wealth is 10-fold [87, 88]. To more fully measure equity, researchers need to develop measures that account for historical or life course disadvantage and metrics within multiple levels that account for the context for implementation [89, 90]. A measurement approach for equity in implementation science assesses both quantity and quality—the simplest measurement occurs in quadrant 1 and the most comprehensive in quadrant 4 (Fig. 1) [91].
Four categories of measurement for equity and implementation science (adapted from MCH Evidence [91])
As equity-relevant measures are developed and refined, it will be helpful to apply existing taxonomies such as the set of eight outcomes developed by Proctor and colleagues (i.e., acceptability, adoption, appropriateness, feasibility, fidelity, implementation cost, penetration, and sustainability) [92]. Measures and methods within these eight categories will need to be adapted to account for contexts where disparities are developed and maintained (e.g., how to document feasibility in a low-resource setting).
Study what is already happening—more practice-based evidence
The importance of context is often devalued relative to the presumed “superiority” of the intervention itself. Our funding mechanisms tend to favor innovation over replication, even when many stakeholders are largely seeking to apply existing knowledge [93]. The research process does not always align with priorities of those experiencing inequities and often moves more slowly than innovations in practice and policy. In a study of implementation of mental health services, Aby found three important themes showing how participants experienced implementation: invisibility (e.g., not enough mental health providers of color), isolation (e.g., separation and lack of collaboration among key stakeholder), and inequity (e.g., feeling tokenized or unwelcome) [94].
To address these issues, it will be useful to place much more emphasis on studying implementation of ongoing health equity projects, often via natural experiments. Experience in low-resource settings shows that novel approaches sometimes thrive under constraints (i.e., creativity can thrive when choices are restricted) [56]. These real-world studies often involve natural experiments [95, 96], which are particularly useful in studying social determinants designed to address inequities and enhance external validity [97]. Multiple state and local agencies across the USA are conducting health equity projects [98]. As an example, the Rhode Island Department of Health supports nine Health Equity Zones across the state to improve socioeconomic and environmental conditions across the state [99]. In Canada, as part of the Canadian Coalitions Linking Action and Science for Prevention (CLASP) initiative, First Nations, Inuit, and Métis community partners brought unique and important community perspectives and relationships to implementation projects [100, 101]. These projects develop so-called “tacit knowledge” or “colloquial evidence” (pragmatic information based on direct experience and action in practice) [102, 103]. They also contribute to the process of tailored implementation, which builds on real-world experiences to identify the most important determinants to address [104, 105].
Integrate equity into implementation models
Models provide a roadmap—a systematic structure for the development, management, and evaluation of all parts of a study [21]. While there are over 100 models to guide implementation science research, only a handful explicitly include health equity [20, 90, 94, 106,107,108,109]. These frameworks are informed by development and use of a larger set of models on health and equity [110].
To advance equity and implementation science, we need to identify gaps among existing models which in turn can guide model improvement. This analysis could assess (1) whether equity is an explicit focus of models (e.g., Is it an end goal?), (2) the degree to which social determinants are represented, (3) whether a set of core equity constructs could be identified within models, (4) whether models apply equally well to lower and higher resource settings, and (5) the degree of representation of disadvantaged groups and community stakeholders in the model. Model selection and adaptation can benefit by interactive webtools such as Dissemination and Implementation Models in Health Research and Practice [111].
Design and tailor implementation strategies
Implementation strategies are methods to enhance the adoption, implementation, sustainment, and scale-up of an innovation (often in the form of an EBI) [112]. Multiple taxonomies describe and organize commonly used implementation strategies that can target a range of stakeholders and multilevel contextual factors across different phases of implementation [113, 114]. The design of implementation strategies should be guided by the growing body of evidence, pertinent theories and frameworks, and relevant stakeholders, including those from communities in which health disparities have been identified [113, 115]. Ultimately, the goal is to understand who needs to do what in order to implement and sustain an innovation, what factors are likely to facilitate or impede those changes, and what strategies need to be in place in order to address anticipated or emergent challenges [116, 117]. The implementation and scale-up of the U.K. Diabetes Prevention Programme show the importance of stakeholder engagement, addressing contextual conditions (e.g., staff turnover), and the value of incentives [118].
Development and use of implementation strategies should include explicit consideration of disparities, contextual conditions that may lead to inequitable outcomes (e.g., resources, history), and opportunities to promote equity by carefully designing and/or tailoring strategies. To date, relatively little emphasis has been placed on how well implementation strategies are responsive to health equity needs. There is ample opportunity to examine the extent to which strategies identified in prevailing taxonomies can be leveraged to address determinants of equity, and to develop and test novel strategies at multiple levels (e.g., individual, provider, organization, community) that may promote health equity. Adaptive designs for developing equity-relevant implementation strategies, such as the Sequential Multiple Assignment Randomized Trial (SMART) design [119], are likely to be useful in accounting for changing real-world conditions.
Giving greater attention to context
Connect to systems and sectors outside of health
Many of the most important influences on health status and disparities occur in sectors outside of healthcare and public health (e.g., schools, housing, education, labor) [120]. These settings are crucial for implementation science in at least four ways: (1) they are highly experienced delivering services to underserved populations and thus have deep knowledge of how to do it well, (2) many of these sectors are already delivering exactly the kinds of non-health interventions that address social needs (as described in Table 3), (3) they provide access to high-risk populations where a health intervention might be added to a service (e.g., adding a smoking cessation intervention to services designed to meet social needs), and (4) the setting itself might be the focus for change and a secondary benefit is a health outcome (e.g., lower use of the emergency department among those who receive permanent supportive housing). Often, the missions and cultures of agencies in these sectors do not focus on health [121]. Therefore, our traditional approaches for forming partnerships need to be re-examined and altered [122].
Three principles show promise. First, an underlying premise is that justice is essential to achieving health equity [123, 124]—not only justice in the health sector but justice across all sectors including housing and neighborhoods, safety, education, and economics and employment. Second, we need more “disease-agnostic interventions,” which are structural interventions, often outside the health sector, that address common risk factors that are linked with multiple disparities [125]. And third, systems science approaches that link sectors have been increasingly applied in public health to study and develop EBIs to address areas as diverse as global pandemics, vaccination system, cancer, and obesity [126]. To date, systems approaches have not been widely applied in health equity, although they show promise [127].
Engage organizations in internal and external equity efforts
Organizations are one of several central entities of influence in implementation science [128]. They may directly deliver health services or may involve community-level partnerships to influence disparities and population health. While health equity is a high priority for many public health organizations, there is sparse empirical data on the organizational commitment to equity issues and how that commitment is operationalized. For example, in a nationwide survey of U.S. practitioners in state health departments, only 2% reported working primarily on health equity and 9% reported that health equity was one of their multiple priority areas [129].
There are opportunities to more fully address issues in equity and implementation science in organizations [121]—both internally and externally. Within an organization, assessments of climate and culture can be conducted with an equity lens. For example, one could assess the perception of the commitment of leaders to equity; employee attitudes, motivations, performance on equity issues (including the presence of hidden biases [130]); internal policies supporting equity; and the diversity of an organization. Organizations could also evaluate existing programs and policies for their reach and impact on health equity. Externally, organizations can bring on new partners who have a shared commitment to equity, develop organizational policies that share decision-making and power with partners, make equity a stated goal of partnerships, and break down funding silos to address root causes. Equity-driven practice for organizations directs resources for those most in need [131].
Addressing cross-cutting issues
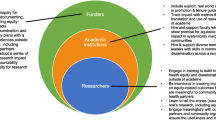
Build capacity for equity in implementation science
Recent reviews of initiatives to build capacity in implementation science have shown a growing number of training opportunities across eight countries [132,133,134]. Capacity building for implementation science occurs in multiple formats including university degree programs, summer training institutes, workshops, and conferences [133]. Nearly all training programs to date have focused on capacity building among researchers (the “push” for implementation science) with little emphasis on practitioners or implementers (the “pull” for implementation science) [133, 135], with few featuring an explicit focus on equity [136].
A full vision for equity-related training needs to be centered on who is being trained, how they are being trained, and where the work is occurring. To address the “who” element in training, programs need to include a larger percentage of early-career scholars who are from under-represented minority groups [137] and those working in disciplines outside of health. The “how” can include multiple parts including (1) how training is delivered to reach all audiences (including those outside the health sector), (2) whether equity is featured as an explicit part of core competencies, (3) how principles of community engagement are included in training [23], and (4) how progress toward equity is evaluated. The “where” issues include where research is occurring and how diverse communities, which are the settings for studies, are engaged in meaningful ways.
Focus on equity in dissemination efforts
Designing for dissemination is defined as “an active process that helps to ensure that public health interventions, often evaluated by researchers, are developed in ways that match well with adopters’ needs, assets, and time frames” [138]. There is a well-documented disconnect between how researchers disseminate their findings and how practitioners and policy makers learn about the latest evidence [93]. Experience in the population or setting of focus also matters—public health researchers with practice or policy experience are over four times more likely to report good or excellent skills in dissemination [139].
Equity-focused dissemination of research findings could include several core elements. At a systems level, funders should provide incentives for researchers to engage in meaningful ways with audiences experiencing disparities (e.g., through requirements for dissemination, supplemental funding). To improve dissemination processes, researchers should engage with equity-focused partners early and often in the research process [140]. Products for dissemination could be improved by refining messages that resonate with key stakeholders and developing communications materials in collaboration with the audience of focus that reflect the images, narratives, and outcomes of interest to populations experiencing disparities.
Conclusions
Approaches to achieving health equity are critical to ameliorating disparities resulting from social, economic, and racial injustice. Given that implementation science is a relatively young field [141, 142], often focused on narrowly-defined EBIs, the lack of explicit attention on equity is not unexpected. As a new field, it is more malleable and should embrace the challenge of equity, a highly ambitious but critically important responsibility that would unquestionably demonstrate its value and provide an identity distinct from the many disciplines it draws upon.
Our premise is that every project in implementation science should include an equity focus. Equity begins with justice—health differences often reflect social injustices [123]. For some studies, equity is the main goal of the project and a central feature of the research questions, the conceptual model, project activities, and dissemination of findings. In other studies, equity is part of a project but not the singular focus. In these projects, we should, at a minimum, ensure that we “leave no one behind” and that existing disparities are not inadvertently widened.
Our recommendations offer a pathway for advancing health equity through implementation science. The ideas provided are critical but far from a complete “playbook” on what needs to happen and how goals might be accomplished. Along with other recent calls to action [14, 20], we view these as first-generation concepts to immediately address health equity—ideas on which others can further advance and build upon. With a stronger commitment to equity from funders, researchers, practitioners, advocates, and policy makers, we can harvest the rewards of the resources being invested in health-related research to eliminate disparities, resulting in health justice.
Availability of data and materials
Not applicable.
Abbreviations
- APEASE:
-
Acceptability, Practicability, Effectiveness, Affordability, Side-effects, and Equity
- CONSORT:
-
Consolidated Standards of Reporting Trials
- COVID-19:
-
Coronavirus disease 2019
- EBI:
-
Evidence-based intervention
- GRADE:
-
Grading Recommendations Assessment and Development Evidence
- HiAP:
-
Health in All Policies
- EiAP:
-
Equity in All Policies
- SMART:
-
Sequential Multiple Assignment Randomized Trial
- U.S.:
-
United States
References
Farrer L, Marinetti C, Cavaco YK, Costongs C. Advocacy for health equity: a synthesis review. Milbank Q. 2015;93(2):392–437. https://doi.org/10.1111/1468-0009.12112.
Morton S, Pencheon D, Squires N. Sustainable Development Goals (SDGs), and their implementation: a national global framework for health, development and equity needs a systems approach at every level. Br Med Bull. 2017;124(1):81–90. https://doi.org/10.1093/bmb/ldx031.
Bor J, Cohen GH, Galea S. Population health in an era of rising income inequality: USA, 1980-2015. Lancet. 2017;389(10077):1475–90. https://doi.org/10.1016/S0140-6736(17)30571-8.
Bailey ZD, Krieger N, Agenor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. Lancet. 2017;389(10077):1453–63. https://doi.org/10.1016/S0140-6736(17)30569-X.
Lancet Covid-19 Commissioners TFC, Commission S. Lancet COVID-19 Commission Statement on the occasion of the 75th session of the UN General Assembly. Lancet. 2020;396(10257):1102–24. https://doi.org/10.1016/S0140-6736(20)31927-9.
Weber L. Companies have promised $35 billion toward racial equity. Where is the money going? New York: Almar Latour; 2020.
Jones NL, Breen N, Das R, Farhat T, Palmer R. Cross-cutting themes to advance the science of minority health and health disparities. Am J Public Health. 2019;109(S1):S21–4. https://doi.org/10.2105/AJPH.2019.304950.
Kumanyika SK. Health equity is the issue we have been waiting for. J Public Health Manag Pract. 2016;22(Suppl 1):S8–S10. https://doi.org/10.1097/PHH.0000000000000363.
Braveman P. What are health disparities and health equity? We need to be clear. Public Health Rep. 2014;129(Suppl 2):5–8. https://doi.org/10.1177/00333549141291S203.
Haire-Joshu D, Hill-Briggs F. The next generation of diabetes translation: a path to health equity. Annu Rev Public Health. 2019;40(1):391–410. https://doi.org/10.1146/annurev-publhealth-040218-044158.
Yao Q, Li X, Luo F, Yang L, Liu C, Sun J. The historical roots and seminal research on health equity: a referenced publication year spectroscopy (RPYS) analysis. Int J Equity Health. 2019;18(1):152. https://doi.org/10.1186/s12939-019-1058-3.
Alcaraz KI, Wiedt TL, Daniels EC, Yabroff KR, Guerra CE, Wender RC. Understanding and addressing social determinants to advance cancer health equity in the United States: a blueprint for practice, research, and policy. CA Cancer J Clin. 2020;70(1):31–46. https://doi.org/10.3322/caac.21586.
Whitehead M. The concepts and principles of equity and health. Int J Health Serv. 1992;22(3):429–45. https://doi.org/10.2190/986L-LHQ6-2VTE-YRRN.
Baumann AA, Cabassa LJ. Reframing implementation science to address inequities in healthcare delivery. BMC Health Serv Res. 2020;20(1):190. https://doi.org/10.1186/s12913-020-4975-3.
Brownson R, Colditz G. Proctor E (Eds.): Dissemination and implementation research in health: translating science to practice, 2nd edition. New York: Oxford University Press; 2018.
Lenfant C. Shattuck lecture--clinical research to clinical practice--lost in translation? N Engl J Med. 2003;349(9):868–74. https://doi.org/10.1056/NEJMsa035507.
Chinman M, Woodward EN, Curran GM, Hausmann LRM, et al. Med Care. 2017;55(Suppl 9 Suppl 2):S16–23.
Galaviz KI, Breland JY, Sanders M, Breathett K, Cerezo A, Gil O, Hollier JM, Marshall C, Wilson JD, Essien UR. Implementation science to address health disparities during the coronavirus pandemic. Health Equity. 2020;4(1):463–7. https://doi.org/10.1089/heq.2020.0044.
Sterling MR, Echeverria SE, Commodore-Mensah Y, Breland JY, Nunez-Smith M. Health equity and implementation science in heart, lung, blood, and sleep-related research: emerging themes from the 2018 Saunders-Watkins Leadership Workshop. Circ Cardiovasc Qual Outcomes. 2019;12:e005586.
Woodward EN, Matthieu MM, Uchendu US, Rogal S, Kirchner JE. The health equity implementation framework: proposal and preliminary study of hepatitis C virus treatment. Implement Sci. 2019;14(1):26. https://doi.org/10.1186/s13012-019-0861-y.
Tabak RG, Khoong EC, Chambers DA, Brownson RC. Bridging research and practice: models for dissemination and implementation research. Am J Prev Med. 2012;43(3):337–50. https://doi.org/10.1016/j.amepre.2012.05.024.
Clarke AR, Goddu AP, Nocon RS, Stock NW, Chyr LC, Akuoko JA, Chin MH. Thirty years of disparities intervention research: what are we doing to close racial and ethnic gaps in health care? Med Care. 2013;51(11):1020–6. https://doi.org/10.1097/MLR.0b013e3182a97ba3.
Minkler M, Salvatore A, Chang C. Participatory approaches for study design and analysis in dissemination and implementation research. In: Brownson R, Colditz G, Proctor E, editors. Dissemination and Implementation Research in Health: Translating Science to Practice. 2nd ed. New York: Oxford University Press; 2018. p. 175–90.
Israel BA, Coombe CM, Cheezum RR, Schulz AJ, McGranaghan RJ, Lichtenstein R, Reyes AG, Clement J, Burris A. Community-based participatory research: a capacity-building approach for policy advocacy aimed at eliminating health disparities. Am J Public Health. 2010;100(11):2094–102. https://doi.org/10.2105/AJPH.2009.170506.
Ramanadhan S, Davis MM, Armstrong R, Baquero B, Ko LK, Leng JC, Salloum RG, Vaughn NA, Brownson RC. Participatory implementation science to increase the impact of evidence-based cancer prevention and control. Cancer Causes Control. 2018;29(3):363–9. https://doi.org/10.1007/s10552-018-1008-1.
National Institutes of Health. Dissemination and implementation research in health (R01 Clinical Trial Optional). vol. PAR-19-274. Bethesda: National Institutes of Health; 2019.
Guide to Community Preventive Services. http://www.thecommunityguide.org. Accessed 14 Mar 2021.
The Cochrane Collaboration. http://www.cochrane.org/. Accessed 14 Mar 2021.
Marmot M. Social determinants of health inequalities. Lancet. 2005;365(9464):1099–104. https://doi.org/10.1016/S0140-6736(05)71146-6.
Braveman P, Egerter S, Williams DR. The social determinants of health: coming of age. Annu Rev Public Health. 2011;32(1):381–98. https://doi.org/10.1146/annurev-publhealth-031210-101218.
Aves T, Kredo T, Welch V, Mursleen S, Ross S, Zani B, Motaze NV, Quinlan L, Mbuagbaw L. Equity issues were not fully addressed in Cochrane human immunodeficiency virus systematic reviews. J Clin Epidemiol. 2017;81:96–100. https://doi.org/10.1016/j.jclinepi.2016.09.008.
Hoffmann I. Transcending reductionism in nutrition research. Am J Clin Nutr. 2003;78(3):514S–6S. https://doi.org/10.1093/ajcn/78.3.514S.
Ahn AC, Tewari M, Poon CS, Phillips RS. The limits of reductionism in medicine: could systems biology offer an alternative? PLoS Med. 2006;3(6):e208. https://doi.org/10.1371/journal.pmed.0030208.
Chambers DA, Norton WE. The Adaptome: advancing the science of intervention adaptation. Am J Prev Med. 2016;51(4):S124–31. https://doi.org/10.1016/j.amepre.2016.05.011.
Jayasinghe S. Social determinants of health inequalities: towards a theoretical perspective using systems science. Int J Equity Health. 2015;14(1):71. https://doi.org/10.1186/s12939-015-0205-8.
Reskin B. The race discrimination system. Annu Rev Sociol. 2012;38(1):17–35. https://doi.org/10.1146/annurev-soc-071811-145508.
Lorenc T, Petticrew M, Welch V, Tugwell P. What types of interventions generate inequalities? Evidence from systematic reviews. J Epidemiol Community Health. 2013;67(2):190–3. https://doi.org/10.1136/jech-2012-201257.
Naik Y, Baker P, Ismail SA, Tillmann T, Bash K, Quantz D, Hillier-Brown F, Jayatunga W, Kelly G, Black M, Gopfert A, Roderick P, Barr B, Bambra C. Going upstream - an umbrella review of the macroeconomic determinants of health and health inequalities. BMC Public Health. 2019;19(1):1678. https://doi.org/10.1186/s12889-019-7895-6.
Thomson K, Hillier-Brown F, Todd A, McNamara C, Huijts T, Bambra C. The effects of public health policies on health inequalities in high-income countries: an umbrella review. BMC Public Health. 2018;18(1):869. https://doi.org/10.1186/s12889-018-5677-1.
Allen P, Walsh-Bailey C, Purtle J, Pilar M, Hooley C, Brownson R. Implications for policy implementation measurement from a systematic review. In: 13th Annual Conference on the Science of Dissemination and Implementation in Health. Washington, DC: AcademyHealth; 2020.
Brown C, Curran G, Palinkas L, et al. An overview of research and evaluation designs for dissemination and implementation. Annu Rev Public Health. 2017;38(1):1–22. https://doi.org/10.1146/annurev-publhealth-031816-044215.
Hemming K, Haines TP, Chilton PJ, Girling AJ, Lilford RJ. The stepped wedge cluster randomised trial: rationale, design, analysis, and reporting. BMJ. 2015;350(feb06 1):h391. https://doi.org/10.1136/bmj.h391.
Jull J, Whitehead M, Petticrew M, Kristjansson E, Gough D, Petkovic J, Volmink J, Weijer C, Taljaard M, Edwards S, et al. When is a randomised controlled trial health equity relevant? Development and validation of a conceptual framework. BMJ Open. 2017;7:e015815.
Mbuagbaw L, Aves T, Shea B, Jull J, Welch V, Taljaard M, Yoganathan M, Greer-Smith R, Wells G, Tugwell P. Considerations and guidance in designing equity-relevant clinical trials. Int J Equity Health. 2017;16(1):93. https://doi.org/10.1186/s12939-017-0591-1.
Wester G, Baeroe K, OF N. Towards theoretically robust evidence on health equity: a systematic approach to contextualising equity-relevant randomised controlled trials. J Med Ethics. 2019;45(1):54–9. https://doi.org/10.1136/medethics-2017-104610.
Wing C, Simon K, Bello-Gomez RA. Designing difference in difference studies: best practices for public health policy research. Annu Rev Public Health. 2018;39(1):453–69. https://doi.org/10.1146/annurev-publhealth-040617-013507.
Glasgow RE. What does it mean to be pragmatic? Pragmatic methods, measures, and models to facilitate research translation. Health Educ Behav. 2013;40(3):257–65. https://doi.org/10.1177/1090198113486805.
Glasgow RE, Askew S, Purcell P, Levine E, Warner ET, Stange KC, Colditz GA, Bennett GG. Use of RE-AIM to address health inequities: application in a low-income community health center based weight loss and hypertension self-management program. Transl Behav Med. 2013;3(2):200–10. https://doi.org/10.1007/s13142-013-0201-8.
Simpson A, Furlong A, Jetha N. At-a-glance - bringing equity into the fold: a review of interventions to improve mental health. Health Promot Chronic Dis Prev Can. 2018;38(10):380–4. https://doi.org/10.24095/hpcdp.38.10.04.
May CR, Johnson M, Finch T. Implementation, context and complexity. Implement Sci. 2016;11(1):141. https://doi.org/10.1186/s13012-016-0506-3.
Nilsen P, Bernhardsson S. Context matters in implementation science: a scoping review of determinant frameworks that describe contextual determinants for implementation outcomes. BMC Health Serv Res. 2019;19(1):189. https://doi.org/10.1186/s12913-019-4015-3.
Glasgow RE, Emmons KM. How can we increase translation of research into practice? Types of evidence needed. Annu Rev Public Health. 2007;28(1):413–33. https://doi.org/10.1146/annurev.publhealth.28.021406.144145.
George S, Duran N, Norris K. A systematic review of barriers and facilitators to minority research participation among African Americans, Latinos, Asian Americans, and Pacific Islanders. Am J Public Health. 2014;104(2):e16–31. https://doi.org/10.2105/AJPH.2013.301706.
Baumann A, Cabassa L, Wiltsey Stirman S. Adaptation in dissemination and implementation science. In: Brownson R, Colditz G, Proctor E, editors. Dissemination and Implementation Research in Health: Translating Science to Practice. 2nd ed. New York: Oxford University Press; 2018. p. 285–300.
Pinto RM, Berringer KR, Melendez R, Mmeje O. Improving PrEP implementation through multilevel interventions: a synthesis of the literature. AIDS Behav. 2018;22(11):3681–91. https://doi.org/10.1007/s10461-018-2184-4.
Yapa HM, Barnighausen T. Implementation science in resource-poor countries and communities. Implement Sci. 2018;13(1):154. https://doi.org/10.1186/s13012-018-0847-1.
Alonge O, Rodriguez DC, Brandes N, Geng E, Reveiz L, Peters DH. How is implementation research applied to advance health in low-income and middle-income countries? BMJ Glob Health. 2019;4(2):e001257. https://doi.org/10.1136/bmjgh-2018-001257.
Harding T, Oetzel J. Implementation effectiveness of health interventions for indigenous communities: a systematic review. Implement Sci. 2019;14(1):76. https://doi.org/10.1186/s13012-019-0920-4.
Wali S, Superina S, Mashford-Pringle A, Ross H, Cafazzo JA. What do you mean by engagement? - evaluating the use of community engagement in the design and implementation of chronic disease-based interventions for Indigenous populations - scoping review. Int J Equity Health. 2021;20(1):8. https://doi.org/10.1186/s12939-020-01346-6.
Cabassa LJ, Baumann AA. A two-way street: bridging implementation science and cultural adaptations of mental health treatments. Implement Sci. 2013;8(1):90. https://doi.org/10.1186/1748-5908-8-90.
Kerner JF. Integrating research, practice, and policy: what we see depends on where we stand. J Public Health Manag Pract. 2008;14(2):193–8. https://doi.org/10.1097/01.PHH.0000311899.11197.db.
Paradies Y, Ben J, Denson N, Elias A, Priest N, Pieterse A, Gupta A, Kelaher M, Gee G. Racism as a determinant of health: a systematic review and meta-analysis. Plos One. 2015;10(9):e0138511. https://doi.org/10.1371/journal.pone.0138511.
Purnell TS, Calhoun EA, Golden SH, Halladay JR, Krok-Schoen JL, Appelhans BM, Cooper LA. Achieving health equity: closing the gaps in health care disparities, interventions, and research. Health Aff (Millwood). 2016;35(8):1410–5. https://doi.org/10.1377/hlthaff.2016.0158.
Taylor LA, Tan AX, Coyle CE, Ndumele C, Rogan E, Canavan M, Curry LA, Bradley EH. Leveraging the social determinants of health: What Works? Plos One. 2016;11(8):e0160217. https://doi.org/10.1371/journal.pone.0160217.
Asare M, Flannery M, Kamen C. Social determinants of health: a framework for studying cancer health disparities and minority participation in research. Oncol Nurs Forum. 2017;44:20–3.
Dendup T, Feng X, Clingan S, Astell-Burt T. Environmental risk factors for developing type 2 diabetes mellitus: a systematic review. Int J Environ Res Public Health. 2018;15(1). https://doi.org/10.3390/ijerph15010078.
Suleman S, Garber KD, Rutkow L. Xenophobia as a determinant of health: an integrative review. J Public Health Policy. 2018;39(4):407–23. https://doi.org/10.1057/s41271-018-0140-1.
Martinez-Cardoso A, Jang W, Baig AA. Moving diabetes upstream: the social determinants of diabetes management and control among immigrants in the US. Curr Diab Rep. 2020;20(10):48. https://doi.org/10.1007/s11892-020-01332-w.
Allen LN, Smith RW, Simmons-Jones F, Roberts N, Honney R, Currie J. Addressing social determinants of noncommunicable diseases in primary care: a systematic review. Bull World Health Organ. 2020;98(11):754–765B. https://doi.org/10.2471/BLT.19.248278.
Alcantara C, Diaz SV, Cosenzo LG, Loucks EB, Penedo FJ, Williams NJ. Social determinants as moderators of the effectiveness of health behavior change interventions: scientific gaps and opportunities. Health Psychol Rev. 2020;14(1):132–44. https://doi.org/10.1080/17437199.2020.1718527.
Public Health England. Achieving behaviour change. A guide for local government and partners. London: Public Health England; 2019.
Moberg J, Oxman AD, Rosenbaum S, Schunemann HJ, Guyatt G, Flottorp S, Glenton C, Lewin S, Morelli A, Rada G, et al. The GRADE Evidence to Decision (EtD) framework for health system and public health decisions. Health Res Policy Syst. 2018;16(1):45. https://doi.org/10.1186/s12961-018-0320-2.
Pottie K, Welch V, Morton R, Akl EA, Eslava-Schmalbach JH, Katikireddi V, Singh J, Moja L, Lang E, Magrini N, Thabane L, Stanev R, Matovinovic E, Snellman A, Briel M, Shea B, Tugwell P, Schunemann H, Guyatt G, Alonso-Coello P. GRADE equity guidelines 4: considering health equity in GRADE guideline development: evidence to decision process. J Clin Epidemiol. 2017;90:84–91. https://doi.org/10.1016/j.jclinepi.2017.08.001.
Welch V, Jull J, Petkovic J, Armstrong R, Boyer Y, Cuervo LG, Edwards S, Lydiatt A, Gough D, Grimshaw J, Kristjansson E, Mbuagbaw L, McGowan J, Moher D, Pantoja T, Petticrew M, Pottie K, Rader T, Shea B, Taljaard M, Waters E, Weijer C, Wells GA, White H, Whitehead M, Tugwell P. Protocol for the development of a CONSORT-equity guideline to improve reporting of health equity in randomized trials. Implement Sci. 2015;10(1):146. https://doi.org/10.1186/s13012-015-0332-z.
Welch VA, Norheim OF, Jull J, Cookson R, Sommerfelt H, Tugwell P, Equity C, Boston Equity S. CONSORT-Equity 2017 extension and elaboration for better reporting of health equity in randomised trials. BMJ. 2017;359:j5085.
Boutron I, Altman DG, Moher D, Schulz KF, Ravaud P, Group CN. CONSORT statement for randomized trials of nonpharmacologic treatments: a 2017 update and a CONSORT extension for nonpharmacologic trial abstracts. Ann Intern Med. 2017;167(1):40–7. https://doi.org/10.7326/M17-0046.
Glasgow RE, Huebschmann AG, Brownson RC. Expanding the CONSORT figure: increasing transparency in reporting on external validity. Am J Prev Med. 2018;55(3):422–30. https://doi.org/10.1016/j.amepre.2018.04.044.
Purtle J, Peters R, Brownson RC. A review of policy dissemination and implementation research funded by the National Institutes of Health, 2007-2014. Implement Sci. 2016;11:1.
Emmons K, Chambers D. Commentary: policy implementation science--an unexplored stragegy to address social determinants of health. Ethn Dis. 2021;31(1):133–8. https://doi.org/10.18865/ed.31.1.133.
Puska P. Health in all policies. Eur J Public Health. 2007;17(4):328. https://doi.org/10.1093/eurpub/ckm048.
Williams DR, Costa MV, Odunlami AO, Mohammed SA. Moving upstream: how interventions that address the social determinants of health can improve health and reduce disparities. J Public Health Manag Pract. 2008;14(Suppl):S8–17. https://doi.org/10.1097/01.PHH.0000338382.36695.42.
Hahn RA. Two paths to health in all policies: the traditional public health path and the path of social determinants. Am J Public Health. 2019;109(2):253–4. https://doi.org/10.2105/AJPH.2018.304884.
Pollack Porter KM, Lindberg R, McInnis-Simoncelli A. Considering health and health disparities during state policy formulation: examining Washington state Health Impact Reviews. BMC Public Health. 2019;19(1):862. https://doi.org/10.1186/s12889-019-7165-7.
Purtle J, Dodson E, Brownson R. Policy dissemination research. In: Brownson R, Colditz G, Proctor E, editors. Dissemination and Implementation Research in Health: Translating Science to Practice. 2nd ed. New York: Oxford University Press; 2018. p. 433–47.
Thacker SB. Public health surveillance and the prevention of injuries in sports: what gets measured gets done. J Athl Train. 2007;42(2):171–2.
Braveman P. Health disparities and health equity: concepts and measurement. Annu Rev Public Health. 2006;27(1):167–94. https://doi.org/10.1146/annurev.publhealth.27.021405.102103.
McIntosh R, Moss E, Nunn R, Shambaugh J. Examining the Black-white wealth gap, vol. 2020. Washington, DC: Brookings; 2020.
Wilson V, Williams J. Racial and ethnic income gaps persist amid uneven growth in household incomes. In: Working Economics Blog, vol. 2020. Washington, DC: Economic Policy Institute; 2019.
Penman-Aguilar A, Talih M, Huang D, Moonesinghe R, Bouye K, Beckles G. Measurement of health disparities, health inequities, and social determinants of health to support the advancement of health equity. J Public Health Manag Pract. 2016;22(Suppl 1):S33–42. https://doi.org/10.1097/PHH.0000000000000373.
Dover DC, Belon AP. The health equity measurement framework: a comprehensive model to measure social inequities in health. Int J Equity Health. 2019;18(1):36. https://doi.org/10.1186/s12939-019-0935-0.
MCH Evidence: ESM review & resources. https://www.mchevidence.org/documents/ESM-Review-National-Summary.pdf. Accessed 14 Mar 2021.
Proctor E, Silmere H, Raghavan R, Hovmand P, Aarons G, Bunger A, Griffey R, Hensley M. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health. 2010;38:65–76.
Brownson RC, Fielding JE, Green LW. Building capacity for evidence-based public health: reconciling the pulls of practice and the push of research. Annu Rev Public Health. 2018;39(1):27–53. https://doi.org/10.1146/annurev-publhealth-040617-014746.
Aby MJ. Race and equity in statewide implementation programs: an application of the policy ecology of implementation framework. Adm Policy Ment Health. 2020;47(6):946–60. https://doi.org/10.1007/s10488-020-01033-2.
Bauer MS, Damschroder L, Hagedorn H, Smith J, Kilbourne AM. An introduction to implementation science for the non-specialist. BMC Psychol. 2015;3(1):32. https://doi.org/10.1186/s40359-015-0089-9.
Rabin B, Brownson R. Terminology for dissemination and implementation research. In: Brownson R, Colditz G, Proctor E, editors. Dissemination and Implementation Research in Health: Translating Science to Practice. 2nd ed. New York: Oxford University Press; 2018. p. 19–45.
Petticrew M, Cummins S, Ferrell C, Findlay A, Higgins C, Hoy C, Kearns A, Sparks L. Natural experiments: an underused tool for public health? Public Health. 2005;119(9):751–7. https://doi.org/10.1016/j.puhe.2004.11.008.
HealthEquityGuide.org. https://healthequityguide.org/. Accessed 14 Mar 2021.
Health Equity Zones (HEZ) Initiative. https://health.ri.gov/programs/detail.php?pgm_id=1108. Accessed 14 Mar 2021.
Lobb R, Petermann L, Manafo E, Keen D, Kerner J. Networking and knowledge exchange to promote the formation of transdisciplinary coalitions and levels of agreement among transdisciplinary peer reviewers. J Public Health Manag Pract. 2013;19(1):E9–20. https://doi.org/10.1097/PHH.0b013e31823991c2.
Manafo E, Petermann L, Lobb R, Keen D, Kerner J. Research, practice, and policy partnerships in pan-Canadian coalitions for cancer and chronic disease prevention. J Public Health Manag Pract. 2011;17(6):E1–E11. https://doi.org/10.1097/PHH.0b013e318215a4ae.
Kothari A, Rudman D, Dobbins M, Rouse M, Sibbald S, Edwards N. The use of tacit and explicit knowledge in public health: a qualitative study. Implement Sci. 2012;7(1):20. https://doi.org/10.1186/1748-5908-7-20.
Sharma T, Choudhury M, Kaur B, Naidoo B, Garner S, Littlejohns P, Staniszewska S. Evidence informed decision making: the use of “colloquial evidence” at nice. Int J Technol Assess Health Care. 2015;31(3):138–46. https://doi.org/10.1017/S0266462314000749.
Krause J, Van Lieshout J, Klomp R, Huntink E, Aakhus E, Flottorp S, Jaeger C, Steinhaeuser J, Godycki-Cwirko M, Kowalczyk A, et al. Identifying determinants of care for tailoring implementation in chronic diseases: an evaluation of different methods. Implement Sci. 2014;9(1):102. https://doi.org/10.1186/s13012-014-0102-3.
Wensing M, Oxman A, Baker R, Godycki-Cwirko M, Flottorp S, Szecsenyi J, Grimshaw J, Eccles M. Tailored implementation for chronic diseases (TICD): a project protocol. Implement Sci. 2011;6(1):103. https://doi.org/10.1186/1748-5908-6-103.
Napoles AM, Stewart AL. Transcreation: an implementation science framework for community-engaged behavioral interventions to reduce health disparities. BMC Health Serv Res. 2018;18(1):710. https://doi.org/10.1186/s12913-018-3521-z.
Eslava-Schmalbach J, Garzon-Orjuela N, Elias V, Reveiz L, Tran N, Langlois EV. Conceptual framework of equity-focused implementation research for health programs (EquIR). Int J Equity Health. 2019;18(1):80. https://doi.org/10.1186/s12939-019-0984-4.
Shelton RC, Chambers DA, Glasgow RE. An extension of RE-AIM to enhance sustainability: addressing dynamic context and promoting health equity over time. Front Public Health. 2020;8:134. https://doi.org/10.3389/fpubh.2020.00134.
Yousefi Nooraie R, Kwan BM, Cohn E, AuYoung M, Clarke Roberts M, Adsul P, Shelton RC. Advancing health equity through CTSA programs: opportunities for interaction between health equity, dissemination and implementation, and translational science. J Clin Transl Sci. 2020;4(3):168–75. https://doi.org/10.1017/cts.2020.10.
Givens ML, Catlin BB, Johnson SP, Pollock EA, Faust VN, Inzeo PT, Kindig DA. What do we know about the drivers of health and equity? a narrative review of graphic representations. Health Equity. 2020;4(1):446–62. https://doi.org/10.1089/heq.2020.0013.
Dissemination and implementation models in health research and practice. https://dissemination-implementation.org/index.aspx. Accessed 14 Mar 2021.
Proctor EK, Powell BJ, McMillen JC. Implementation strategies: recommendations for specifying and reporting. Implement Sci. 2013;8(1):139. https://doi.org/10.1186/1748-5908-8-139.
Powell BJ, Fernandez ME, Williams NJ, Aarons GA, Beidas RS, Lewis CC, McHugh SM, Weiner BJ. Enhancing the impact of implementation strategies in healthcare: a research agenda. Front Public Health. 2019;7:3. https://doi.org/10.3389/fpubh.2019.00003.
Powell BJ, Waltz TJ, Chinman MJ, Damschroder LJ, Smith JL, Matthieu MM, Proctor EK, Kirchner JE. A refined compilation of implementation strategies: results from the Expert Recommendations for Implementing Change (ERIC) project. Implement Sci. 2015;10(1):21. https://doi.org/10.1186/s13012-015-0209-1.
Powell BJ, Beidas RS, Lewis CC, Aarons GA, McMillen JC, Proctor EK, Mandell DS. Methods to improve the selection and tailoring of implementation strategies. J Behav Health Serv Res. 2015;44:177–94.
Fernandez ME, Ten Hoor GA, van Lieshout S, Rodriguez SA, Beidas RS, Parcel G, Ruiter RAC, Markham CM, Kok G. Implementation mapping: using intervention mapping to develop implementation strategies. Front Public Health. 2019;7:158. https://doi.org/10.3389/fpubh.2019.00158.
Powell BJ, Haley AD, Patel SV, Amaya-Jackson L, Glienke B, Blythe M, Lengnick-Hall R, McCrary S, Beidas RS, Lewis CC, et al. Improving the implementation and sustainment of evidence-based practices in community mental health organizations: a study protocol for a matched-pair cluster randomized pilot study of the Collaborative Organizational Approach to Selecting and Tailoring Implementation Strategies (COAST-IS). Implement Sci Commun. 2020;1:9.
Stokes J, Gellatly J, Bower P, Meacock R, Cotterill S, Sutton M, Wilson P. Implementing a national diabetes prevention programme in England: lessons learned. BMC Health Serv Res. 2019;19(1):991. https://doi.org/10.1186/s12913-019-4809-3.
Kilbourne AM, Almirall D, Eisenberg D, Waxmonsky J, Goodrich DE, Fortney JC, Kirchner JE, Solberg LI, Main D, Bauer MS, et al. Protocol: Adaptive Implementation of Effective Programs Trial (ADEPT): cluster randomized SMART trial comparing a standard versus enhanced implementation strategy to improve outcomes of a mood disorders program. Implement Sci. 2014;9(1):132. https://doi.org/10.1186/s13012-014-0132-x.
National Prevention Council. National Prevention Strategy. Washington, DC: US Department of Health and Human Services, Office of the Surgeon General; 2011.
Mazzucca S, Arredondo EM, Hoelscher DM, Haire-Joshu D, Tabak RG, Kumanyika SK, Brownson RC. Expanding implementation research to prevent chronic diseases in community settings. Annu Rev Public Health. 2021. p. 4.
Mensah GA. New partnerships to advance global health research for NCD. Glob Heart. 2016;11(4):473–8. https://doi.org/10.1016/j.gheart.2016.10.022.
Braveman PA, Kumanyika S, Fielding J, Laveist T, Borrell LN, Manderscheid R, Troutman A. Health disparities and health equity: the issue is justice. Am J Public Health. 2011;101(Suppl 1):S149–55. https://doi.org/10.2105/AJPH.2010.300062.
Krieger N. ENOUGH: COVID-19, structural racism, police brutality, plutocracy, climate change-and time for health justice, democratic governance, and an equitable, sustainable future. Am J Public Health. 2020;110(11):1620–3. https://doi.org/10.2105/AJPH.2020.305886.
Brown AF, Ma GX, Miranda J, Eng E, Castille D, Brockie T, Jones P, Airhihenbuwa CO, Farhat T, Zhu L, Trinh-Shevrin C. Structural interventions to reduce and eliminate health disparities. Am J Public Health. 2019;109(S1):S72–8. https://doi.org/10.2105/AJPH.2018.304844.
Luke DA, Stamatakis KA. Systems science methods in public health: dynamics, networks, and agents. Annu Rev Public Health. 2012;33(1):357–76. https://doi.org/10.1146/annurev-publhealth-031210-101222.
McNulty M, Smith JD, Villamar J, Burnett-Zeigler I, Vermeer W, Benbow N, Gallo C, Wilensky U, Hjorth A, Mustanski B, Schneider J, Brown CH. Implementation research methodologies for achieving scientific equity and health equity. Ethn Dis. 2019;29(Suppl 1):83–92. https://doi.org/10.18865/ed.29.S1.83.
Aarons G, Moullin J, Ehrhart M. The role of organizational processes in dissemination and implementation research. In: Brownson R, Colditz G, Proctor E, editors. Dissemination and Implementation Research in Health: Translating Science to Practice. 2nd ed. New York: Oxford University Press; 2018. p. 121–42.
Furtado KS, Brownson C, Fershteyn Z, Macchi M, Eyler A, Valko C, Brownson RC. Health departments with a commitment to health equity: a more skilled workforce and higher-quality collaborations. Health Aff (Millwood). 2018;37(1):38–46. https://doi.org/10.1377/hlthaff.2017.1173.
Wangari Walter A, Ruiz Y, Welch R, Tourse C, Kress H, Morningstar B, MacArthur B, Daniels A. Leadership matters: how hidden biases perpetuate institutional racism in organizations. Hum Serv Organ. 2016;41:213–21.
Gron S, Loblay V, Conte KP, Green A, Innes-Hughes C, Milat A, Mitchell J, Persson L, Thackway S, Williams M, Hawe P. Key performance indicators for program scale-up and divergent practice styles: a study from NSW, Australia. Health Promot Int. 2020;35(6):1415–26. https://doi.org/10.1093/heapro/daaa001.
Darnell D, Dorsey CN, Melvin A, Chi J, Lyon AR, Lewis CC. A content analysis of dissemination and implementation science resource initiatives: what types of resources do they offer to advance the field? Implement Sci. 2017;12(1):137. https://doi.org/10.1186/s13012-017-0673-x.
Chambers DA, Proctor EK, Brownson RC, Straus SE. Mapping training needs for dissemination and implementation research: lessons from a synthesis of existing D&I research training programs. Transl Behav Med. 2016;7:593–601.
Davis R, D'Lima D. Building capacity in dissemination and implementation science: a systematic review of the academic literature on teaching and training initiatives. Implement Sci. 2020;15(1):97. https://doi.org/10.1186/s13012-020-01051-6.
Rabin BA, Brownson RC, Kerner JF, Glasgow RE. Methodologic challenges in disseminating evidence-based interventions to promote physical activity. Am J Prev Med. 2006;31(4 Suppl):S24–34. https://doi.org/10.1016/j.amepre.2006.06.009.
Boyce CA, Barfield W, Curry J, Shero S, Green Parker M, Cox H, Bustillo J, Price LN. Building the next generation of implementation science careers to advance health equity. Ethn Dis. 2019;29(Suppl 1):77–82. https://doi.org/10.18865/ed.29.S1.77.
Kreuter MW, Griffith DJ, Thompson V, Brownson RC, McClure S, Scharff DP, Clark EM, Haire-Joshu D. Lessons learned from a decade of focused recruitment and training to develop minority public health professionals. Am J Public Health. 2011;101(Suppl 1):S188–95. https://doi.org/10.2105/AJPH.2011.300122.
Brownson RC, Jacobs JA, Tabak RG, Hoehner CM, Stamatakis KA. Designing for dissemination among public health researchers: findings from a national survey in the United States. Am J Public Health. 2013;103(9):1693–9. https://doi.org/10.2105/AJPH.2012.301165.
Tabak RG, Stamatakis KA, Jacobs JA, Brownson RC. What predicts dissemination efforts among public health researchers in the United States? Public Health Rep. 2014;129(4):361–8. https://doi.org/10.1177/003335491412900411.
Lee K, van Nassau F, Grunseit A, Conte K, Milat A, Wolfenden L, Bauman A. Scaling up population health interventions from decision to sustainability - a window of opportunity? A qualitative view from policy-makers. Health Res Policy Syst. 2020;18:118.
Eccles MP, Mittman B. Welcome to implementation science. Implement Sci. 2006;1(1):1. https://doi.org/10.1186/1748-5908-1-1.
Chambers D. Foreword. In: Brownson R, Colditz G, Proctor E, editors. Dissemination and Implementation Research in Health: Translating Science to Practice. New York: Oxford University Press; 2012. p. vii–x.
Acknowledgements
We thank Ana Baumann, Carol Brownson, Leopoldo Cabassa, Russell Glasgow, Jon Kerner, Byron Powell, and Rachel Tabak for helpful comments on the manuscript.
Disclaimer
The findings and conclusions in this paper are those of the authors and do not necessarily represent the official positions of the National Institutes of Health, or the Centers for Disease Control and Prevention.
Funding
This work was supported in part by the National Cancer Institute (number P50CA244431), the National Institute of Diabetes and Digestive and Kidney Diseases (numbers P30DK092950 and R25DK123008), the Centers for Disease Control and Prevention (number U48DP006395), and the Foundation for Barnes-Jewish Hospital.
Author information
Authors and Affiliations
Contributions
RCB conceptualized the original ideas and wrote the first draft of the paper. SKK, MWK, and DHJ provided input on the original outline, contributed text to the draft manuscript, and provided intellectual content to the manuscript. All authors provided critical edits on drafts of the article and approved the final version. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Brownson, R.C., Kumanyika, S.K., Kreuter, M.W. et al. Implementation science should give higher priority to health equity. Implementation Sci 16, 28 (2021). https://doi.org/10.1186/s13012-021-01097-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13012-021-01097-0