Abstract
Interleukin-6 is an inflammatory cytokine with wide-ranging biological effects. It has been widely demonstrated that neuroinflammation plays a critical role in the development of pathological pain. Recently, various pathological pain models have shown elevated expression levels of interleukin-6 and its receptor in the spinal cord and dorsal root ganglia. Additionally, the administration of interleukin-6 could cause mechanical allodynia and thermal hyperalgesia, and an intrathecal injection of anti-interleukin-6 neutralizing antibody alleviated these pain-related behaviors. These studies indicated a pivotal role of interleukin-6 in pathological pain. In this review, we summarize the recent progress in understanding the roles and mechanisms of interleukin-6 in mediating pathological pain associated with bone cancer, peripheral nerve injury, spinal cord injury, chemotherapy-induced peripheral neuropathy, complete Freund’s adjuvant injection, and carrageenan injection. Understanding and regulating interleukin-6 could be an interesting lead to novel therapeutic strategies for pathological pain.
Similar content being viewed by others
Background
Pathological pain is characterized by a low threshold and an exaggerated response to noxious stimuli, and it can be categorized as cancer pain, neuropathic pain, or inflammatory pain [1, 2]. Although physiological pain is essential for the elimination of damaging stimuli, pathological pain significantly affects the quality of life [3–5]. Currently, pathological pain is thought to be mainly induced by a combination of peripheral drives and central processing [6–9]. Despite growing knowledge of the mechanisms of pathological pain, this type of pain still represents a major challenge in clinical practice and basic science. Cytokines have been reported to participate in the regulation of numerous cellular functions including the inflammatory response and expression of cell surface proteins [10–12]. In addition, we previously reported that several cytokines could potentially serve as targets for the management of bone cancer pain (BCP) [13–19]. Recently, mounting evidence has suggested that one cytokine in particular, interleukin-6 (IL-6), may play a critical role in the development of pathological pain [20–24].
IL-6 is an inflammatory cytokine with wide-ranging biological effects. It was first described as B-stimulatory factor 2, which induces B lymphocytes to produce immunoglobulin [25]. IL-6 exerts its biological effect on target cells by interacting with the non-signaling membrane-bound IL-6 receptor (mIL-6R) [26, 27]. The IL-6 and mIL-6R complex then associates with the signal transducing membrane protein gp130, promoting its dimerization and the subsequent activation of intracellular signaling including the Janus-activated kinase/signal transducer activator of transcription (JAK/STAT), mitogen-activated protein kinase/extracellular signal-regulated kinase (MAPK/ERK), and phosphatidylinositol 3-kinase/protein kinase B (PI3K/Akt) signaling pathways [28–30]. This manner of IL-6 signaling is often referred to as “classical IL-6 signaling.” gp130 is expressed by almost all cells in the body, whereas the mIL-6R has a highly restricted expression profile, and is mainly expressed by hepatocytes, neutrophils, monocytes/macrophages and certain other leukocytes [31, 32]. Only cells expressing mIL-6R can bind and respond to IL-6. Thus, until the discovery of a naturally occurring soluble form of IL-6R (sIL-6R), it was difficult to understand how IL-6 could elicit wide-ranging biological responses by interacting with a limited number of cell types. sIL-6R has been found in various body fluids and has been shown to be generated by two independent mechanisms: limited proteolytic cleavage from mIL-6R and translation from a differentially spliced messenger RNA (mRNA) [33–35]. A complex comprising IL-6 and sIL-6R is also able to bind to gp130 and to initiate intracellular signaling [36, 37]. Through this so-called “trans-signaling” mechanism, IL-6 is capable of stimulating cells that lack endogenous mIL-6R [38]. Additionally, it has been shown that the soluble form of gp130 (sgp130) exclusively inhibits IL-6 responses mediated via the IL-6/sIL-6R complexes (i.e., trans-signaling) and does not affect stimulation via mIL-6R (i.e., classical IL-6 signaling) [39–41]. Therefore, sgp130 can be used as a molecular tool to discriminate between classical signaling and trans-signaling.
Various pathological pain models have shown elevated expression levels of IL-6, IL-6R, and gp130 in the spinal cord and dorsal root ganglia (DRG). Additionally, the administration of IL-6 could cause mechanical allodynia or thermal hyperalgesia, and an intrathecal injection of anti-IL-6 neutralizing antibody alleviated these pain-related behaviors. Furthermore, IL-6 was reported to be intimately linked to nociceptive plasticity by enhancing translation in sensory neurons [42, 43]. IL-6 was also demonstrated to contribute to nociceptor sensitization and central sensitization [44–47]. These studies suggested an important role of IL-6 in pathological pain, indicating that the targeting of IL-6 or its receptor may reveal novel therapeutic interventions for the management of pathological pain. Moreover, humanized anti-IL-6R monoclonal antibody has exhibited excellent efficacy and safety against numerous diseases [48–50]. Therefore, here we review the current evidence of the role of IL-6 in the generation of pathological pain caused by bone cancer, peripheral nerve injury, spinal cord injury, chemotherapy-induced peripheral neuropathy, complete Freund’s adjuvant (CFA) injection, or carrageenan injection.
IL-6 and cancer pain
Advanced prostate, lung, and breast cancer frequently metastasize to the bone, which causes 75–90 % of these patients to experience severe pain [51–53]. There is growing body of evidence demonstrating that IL-6 plays a vital role in various aspects of tumor behaviors including cell proliferation, migration, invasion, differentiation, and angiogenesis [54–57]. In this review, we focus on the critical role of IL-6 in pain caused by bone metastasis.
The involvement of IL-6 in BCP was first reported by Dong et al. [58], who used a rat model of BCP. In this study, the reverse transcription polymerase chain reaction (RT-PCR) results showed that the mRNA levels of IL-6 were considerably increased on 16 days after tumor cell implantation (TCI). Furthermore, intrathecal administration of EphB1-Fc significantly suppressed the mRNA levels of IL-6 in the spinal cord, indicating a downstream role of IL-6 in the analgesic effect of EphB1-Fc. In another study, immunohistochemistry and enzyme-linked immuno-sorbent assay (ELISA) work revealed that spinal IL-6 levels were significantly increased on day 12 after TCI [59]. It was found that propentofylline (PPF), a glial modulating agent, could alleviate pain hypersensitivity after TCI; in addition, the intrathecal injection of PPF markedly inhibited the expression of IL-6. Recently, it was shown that the intrathecal injection of tanshinone IIA, an ingredient in a traditional Chinese medicine, attenuated thermal hyperalgesia in a mouse model of BCP by inhibiting the release of pro-inflammatory cytokines [60]. More recently, Lu et al. [61] provided evidence for the persistent involvement of inflammation in the development of BCP; JWH-015, a selective cannabinoid receptor agonist, reduced the expression of pro-inflammatory cytokines in a time-dependent manner, thereby exerting an anti-nociceptive effect. Using conditional knockout mice lacking gp130 specifically in nociceptors, Andratsch et al. [62] uncovered that gp130 expressed in peripheral pain sensing neurons is critically required for the development of cancer pain. In addition, Quarta et al. [63] have shown the first genetic evidence that gp130 in Nav1.8 expressing primary afferents contributes to the maintenance of nociceptor sensitization in a mouse model of cancer pain. They found that mice with a null mutation of gp130 (gp130−/−) showed signs of nociceptor sensitization and hypersensitivity to mechanical stimuli in the early stage. However, gp130−/− mice significantly recovered from hypersensitivity in the later stage, indicating that gp130 signal transducer plays a substantial role in regulating mechanical hypersensitivity particularly in the maintenance phase of cancer pain. The findings from the studies above implicate a role of IL-6 in the progression of cancer pain. However, the underlying mechanisms of IL-6 in the development of BCP were not investigated until Fang et al. [20]. Using RT-PCR and Western blotting, the expression levels of IL-6 and sIL-6R in the ipsilateral L4 and L5 DRG were found to be remarkably higher in BCP rats than in sham rats. Additionally, the intrathecal administration of FIL-6, a mixture of IL-6 and sIL-6R, induced hyperexcitability of nociceptive DRG neurons acutely isolated from naive rats and caused mechanical allodynia and thermal hyperalgesia in naive rats, suggesting that increased IL-6 contributed to the pathogenesis of BCP. Furthermore, both pretreatment and posttreatment with sgp130, a potent IL-6/sIL-6R trans-signaling inhibitor, remarkably attenuated the bone cancer induced overexcitability of DRG neurons and hyperalgesia in BCP rats, indicating that IL-6/sIL-6R trans-signaling was involved in the development of BCP by inducing DRG neurons hyperexcitability. More importantly, they found that transient receptor potential vanilloid channel type 1 (TRPV1) was the downstream target on which the enhanced expression of IL-6 in DRG neurons exerted its effects associated with the development of BCP. Activation of the JAK/PI3K signaling pathway was required for both the FIL-6-induced functional upregulation of TRPV1 in DRG neurons and pain hypersensitivity in naive rats. This study provided various lines of evidence for a novel intracellular pathway, the IL-6/JAK/PI3K/TRPV1 signaling cascade, which may underlie the development of peripheral sensitization and BCP.
IL-6 and neuropathic pain
Neuropathic pain is a chronic pain condition caused by a primary lesion in or dysfunction of the nervous system and is characterized by spontaneous and evoked pain [64–66]. This type of pain is commonly observed in patients with cancer, diabetic peripheral neuropathy, herpes infection, spinal cord injury (SCI), or multiple sclerosis [67, 68]. Although there is no systematic classification system, neuropathic pain could be classified based on the etiology of the insult to the nervous system or the anatomical distribution of the pain [69]. Various animal models have been established to explore the mechanisms of neuropathic pain of different etiologies, including peripheral nerve injury, SCI, and chemotherapy-induced peripheral neuropathy. Using these animal models, a great deal of basic research has been performed to elucidate the mechanisms of neuropathic pain, which are complex and involve both peripheral and central pathophysiological phenomena. Following peripheral nerve injury, A-δ fiber and C-fiber primary afferent neurons become abnormally sensitive and develop pathological spontaneous activity, leading to peripheral sensitization [70]. This sensitization triggers the production of mediators, alteration of ion channels, and sprouting of nerves endings. These activities provoke secondary changes in central sensory processing, thereby contributing to spinal cord hyperexcitability and central sensitization [71]. Recently, converging lines of evidence have indicated that IL-6 plays a critical role in neuropathic pain caused by peripheral nerve injury, SCI, and chemotherapy-induced peripheral neuropathy.
IL-6 and peripheral nerve injury
Most studies have used an animal model of peripheral nerve injury to explore the relationship between IL-6 and neuropathic pain. A growing body of research has demonstrated that IL-6 plays a role in the pathogenesis of neuropathic pain. The involvement of IL-6 in peripheral neuropathy was first found in a rat model of sciatic cryoneurolysis (SCN), in which the sciatic nerve was frozen to induce nerve injury [72]. The immunohistochemical data resulting from this model showed that IL-6-like immunoreactivity was significantly higher in both the dorsal and ventral horns in SCN rats than in those of normal rats. Furthermore, intrathecal administration of recombinant human IL-6 could mimic and even potentiate pain behavior after SCN. These results provided evidence that IL-6 may be involved in the development of neuropathic pain following SCN. In a subsequent study, they demonstrated that IL-6 mRNA was significantly elevated in both the dorsal and ventral horns in a neuropathic pain model of spinal nerve cryoneurolysis and spinal nerve tight ligation using in situ hybridization and a digoxigenin-labeled oligonucleotide [73]. In addition, they further demonstrated that an intrathecal injection of anti-IL-6 antibody could attenuate L5 spinal nerve transection-induced mechanical allodynia [74], providing further evidence for the role of central IL-6 in the etiology of mechanical allodynia following peripheral nerve injury. In another study, Ramera et al. [75] reported that spinal nerve lesion-induced mechanical allodynia was attenuated and delayed in IL-6 knockout mice, indicating a role of IL-6 in the initiation of neuropathic pain. Similar results were reported in IL-6−/− mice using chronic constriction injury (CCI) model [76]. Using in situ hybridization, Brazda et al. [77] were the first group to show that IL-6 and IL-6R synthesis was increased in remote cervical DRG not associated with the nerve injury following CCI. They found that unilateral CCI induced the bilateral elevation of IL-6 and IL-6R mRNAs not only in L4–L5 DRG but also in remote cervical DRG, suggesting a general neuro-inflammatory reaction of the nervous system to local nerve injury. They further confirmed their hypothesis in a subsequent study [78].
The above studies demonstrated the participation of IL-6 in the pathogenesis of peripheral nerve injury-induced neuropathic pain. However, the underlying molecular and cellular mechanisms were not investigated. In an in vivo and in vitro study, Ma et al. [79] reported the involvement of prostaglandin E2 (PGE2) in the upregulated expression of IL-6 by invading macrophages following partial sciatic nerve ligation (PSNL). The immunostaining results of the in vivo study confirmed the dramatically increased number of IL-6-immunoreactive cells in the injured nerve of PSNL rats. The in vitro results showed that the levels of both PGE2 and IL-6 released from cultured cells derived from injured nerves were significantly increased, as well as that these elevated levels could be suppressed by non-selective and selective COX2 inhibitors. Interestingly, although PGE2 treatment did not remarkably increase the level of IL-6 released from cultured cells derived from uninjured nerve, it did increase the level of IL-6 released from injured nerve-derived cells in a concentration- and time-dependent manner. Moreover, both a selective PGE2 receptor 4 (EP4) antagonist (L-161982) and a protein kinase C (PKC) inhibitor (calphostin C) dramatically suppressed IL-6 release. These findings suggested that PGE2 was involved in mediating the upregulation of IL-6 occurring in invading macrophages via the EP4 receptor and the PKC pathway. In a subsequent study, they also demonstrated the role of PGE2 in the synthesis of IL-6 in primary sensory neurons following PSNL [80]. The in vivo data showed that injured nerve-derived PGE2 contributed to the de novo synthesis of IL-6 in damaged medium and large size DRG neurons following PSNL by activating the EP4 receptors. The in vitro data showed that EP4 receptor, PKA, PKC, ERK/MAPK, CREB, and NF-kB signaling pathways were involved in PGE2-induced IL-6 production in DRG neurons. These results provided evidence that facilitating the de novo synthesis of IL-6 in injured medium and large size DRG neurons was a new mechanism underlying the role of injured nerve-derived PGE2 in the development of neuropathic pain.
As IL-6 mainly activates the JAK/STAT transduction pathway, Dominguez et al. [81] investigated the possible activation of this signaling system in the spinal cord using an SNL model. It was shown that phospho-STAT3 (p-STAT3) in microglial cells of the spinal cord dorsal horn was significantly increased in SNL rats compared with sham rats and that inhibiting the STAT3 pathway attenuated both mechanical allodynia and thermal hyperalgesia in SNL rats. In line with previous studies, they found a massive induction of IL-6 mRNA expression in DRG and an increased concentration of IL-6 in the spinal cord dorsal horn. In addition, the intrathecal injection of anti-rat IL-6 antibodies prevented the SNL-induced accumulation of p-STAT3 in the spinal cord. Together, these data suggest that IL-6 plays a major role in the activation of the spinal JAK/STAT3 pathway after SNL and that this transduction pathway participates in the development of neuropathic pain.
It was reported that tumor necrosis factor-α (TNF-α), which binds to tumor necrosis factor receptor 1 (TNFR1) and induces NF-kB and p38 MAPK activation, was also upregulated following peripheral nerve injury [82, 83]. Therefore, Lee et al. [84] investigated whether TNFR1 regulates IL-6 expression through NF-kB or p38 MAPK activation in the spinal cord and DRG using a CCI model. They found that the CCI-induced upregulation of IL-6 expression was suppressed by intrathecal injection of a TNFR1 antisense oligonucleotide and an NF-kB decoy, but not by a p38 MAPK inhibitor, suggesting that TNFR1 induces IL-6 upregulation through NF- kB activation, but not p38 MAPK activation, in a CCI model. In a subsequent study, they further examined whether IL-6 regulates CX3CR1 expression through p38 MAPK activation in the spinal cord of CCI rats [21]. It was shown that CX3CR1 expression and p38 MAPK activation in the ipsilateral spinal dorsal horn were significantly increased following CCI and that an intrathecal injection of anti-IL-6 neutralizing antibody dramatically decreased both CX3CR1 expression and p38 MAPK activation. Additionally, naïve rats treated with exogenous recombinant rat IL-6 (rrIL-6) showed increased spinal CX3CR1 expression and p38 MAPK activation. Furthermore, treatment with a p38 MAPK-specific inhibitor, SB203580, suppressed the increase in CX3CR1 expression induced by either CCI or rrIL-6 treatment. These results indicated that IL-6 induces microglial CX3CR1 expression in the spinal cord after peripheral nerve injury through p38 MAPK activation, which demonstrates a new mechanism of neuropathic pain.
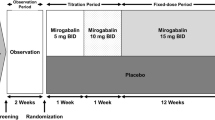
Several drugs have been reported to alleviate neuropathic pain, and this alleviation was accompanied by decreased serum level of IL-6 [85–87]. Recently, the clinical involvement of IL-6 in peripheral nerve injury-induced pain was also reported. Ohtori et al. [88] found that an epidural injection of an anti-IL-6R monoclonal antibody, tocilizumab, onto the spinal nerve alleviated radicular leg pain, numbness, and low back pain without causing adverse events in 60 patients with lumbar spinal stenosis-induced sciatica.
IL-6 and spinal cord injury
Approximately 70 % of SCI patients have been reported to have chronic pain, and the pathogenesis of which remains largely unknown [89, 90]. Guptarak et al. [22] conducted a study to investigate the role of IL-6 in spinal cord injury pain (SCIP) using a clinically relevant rat contusion model. They found that only SCI rats that developed mechanical allodynia showed elevated IL-6 levels. Their immunocytochemistry results showed that increased IL-6 was predominantly co-localized with reactive astrocytes. Furthermore, one systemic injection of neutralizing IL-6 receptor antibody (IL-6R Ab) abolished the SCI-induced allodynia. As the humanized IL-6R Ab tocilizumab is approved by the Food and Drug Administration, they proposed that tocilizumab may become a novel and potentially effective means of managing SCIP. In another study, Murakami et al. [91] reported the beneficial effects of an anti-mouse IL-6R Ab (MR16-1) on neuropathic pain. The ELISA data showed that IL-6 levels between 24 and 72 h after SCI were significantly decreased in mice treated with MR16-1. Additionally, their behavioral data suggested that MR16-1 could alleviate hyperalgesia in SCI mice. The findings from these two studies indicate that IL-6/IL-6R trans-signaling may be a potential target for the treatment of SCIP.
IL-6 and chemotherapy-induced peripheral neuropathy
Chemotherapy-induced peripheral neuropathy (CIPN) is a common consequence of several antineoplastic agents and can severely impact patients’ long-term quality of life [92, 93]. However, contradictory results have been reported, and the mechanisms of CIPN have remained unclear. In an in vivo study, three animal models of CIPN (i.e., rats treated with cisplatin or vincristine and mice treated with paclitaxel) were used to study the peripheral roles of IL-6 in painful CIPN [94]. This study first reported that IL-6 treatment could prevent the painful behavior of CIPN without interfering with the anti-tumor activity of these chemotherapeutic regimens, suggesting a potential neuroprotective effect of IL-6 on CIPN. In another study, the role IL-6 in vincristine-induced mechanical allodynia was examined using a mouse model of CIPN [95]. It was found that the expression of IL-6 was increased in CIPN mice and was co-localized with macrophage, as indicated by double immunostaining. Moreover, IL-6 neutralizing antibody considerably reduced vincristine-induced mechanical allodynia. In addition, the incidence of vincristine-induced mechanical allodynia was lower in IL-6 knockout mice than in wild-type mice. All of these results suggest that IL-6 plays a vital role in vincristine-induced mechanical allodynia. However, further investigation is required to determine whether IL-6, IL-6 neutralizing antibody or both can alleviate hyperalgesia and the associated underlying mechanisms. These conflicting results may be due to the different drug administration methods and animals used. Recently, a clinical study reported that IL-6 and sIL-6R levels were significantly higher after the conclusion of chemotherapy in breast cancer patients with CIPN than in those without CIPN, providing the first clinical evidence of the involvement of IL-6 in CIPN [96].
IL-6 and inflammatory pain
Inflammatory pain is a common clinical symptom of inflammatory diseases and is characterized by hyperalgesia due to the sensitization of primary nociceptive neurons [97, 98]. Our previous study revealed that cannabinoid CB2 receptors (CB2Rs) are involved in the anti-nociceptive effect of electroacupuncture (EA) on inflammatory pain [99–101]. However, it was not clear how CB2R activation contributed to the anti-nociceptive effect of EA. Therefore, we conducted a study to investigate the effects of CB2R activation and EA on the expression level of several cytokines including IL-6 in a CFA rat model of inflammatory pain [24]. Using RT-PCR and Western blotting, we found that the mRNA and protein levels of IL-1β, IL-6, and TNF-α were significantly higher in CFA rats than in control rats. Moreover, treatment with EA or the selective CB2R agonist AM1241 significantly decreased the mRNA and protein levels of IL-1β, IL-6, and TNF-α in CFA rats. In addition, pretreatment with the specific CB2R antagonist AM630 significantly reversed the inhibitory effect of EA on IL-1β, IL-6, and TNF-α in CFA rats. These results suggested that EA suppressed the expression of IL-1β, IL-6, and TNF-α through CB2R activation, resulting in an analgesic effect. In another study, Sun et al. [102] found that tanshinone IIA attenuated the development of CFA-induced mechanical and thermal hypersensitivity, which was concomitant with downregulation of the spinal IL-6 level. Recently, Xu et al. [103] reported that triptolide, a traditional Chinese medicine ingredient, attenuated CFA-induced inflammatory pain by inhibiting spinal glia activation in rats. Pro-inflammatory cytokine levels were significantly increased after CFA injection. Furthermore, triptolide treatment reduced the levels of pro-inflammatory cytokines in the spinal cord. These results suggested that IL-6 may play a role in the pain-suppression effect of triptolide. More recently, Yang et al. [104] explored the possible mechanisms of the analgesic effect of oxysophocarpin, an alkaloid extracted from Sophora alopecuroides, on carrageenan induced inflammatory pain in mice. They found that IL-1β, IL-6, TNF-α, and PGE2 was significantly higher in mice with induced inflammatory pain than in sham mice and that the oxysophocarpin treatment markedly decreased their production. These findings demonstrated that IL-6 could potentially serve as a downstream target of several drugs to relieve inflammatory pain. However, it is still unclear how IL-6 suppression contributes to the alleviation of inflammatory pain. Therefore, further studies are needed to explore the molecular and cellular mechanisms of IL-6 in inflammatory pain. Our recent studies have shown that JAK2/STAT3 signaling may be involved.
Conclusions
By reviewing the current evidence, we discussed the relationship between IL-6 and pathological pain (Figs. 1 and 2). These studies provided robust evidence that IL-6 plays a critical role in the pathogenesis of BCP, neuropathic pain, and inflammatory pain. Treatment with anti-IL-6 or anti-IL-6R neutralizing antibody attenuates mechanical allodynia and thermal hyperalgesia caused by pathological pain, indicating that inhibitors of IL-6 or its receptors may be novel and beneficial therapeutic tools for pathological pain management. Although IL-6 plays vital roles in host defense and homeostasis maintenance, the overproduction of IL-6 causes the onset or development of several diseases. Therefore, novel therapeutic strategies using IL-6 or its receptors have been developed and successfully used for the treatment of numerous diseases. It was reported that tocilizumab, a humanized anti-IL-6R monoclonal antibody, improved the signs and symptoms of rheumatoid arthritis [105–110], juvenile idiopathic arthritis [111–113], and Castleman disease [114–116]. Furthermore, a recent prospective comparative cohort study provided evidence that single intradiscal injection of tocilizumab exerted a short-term analgesic effect in patients with discogenic low back pain [117]. Therefore, inhibitors of IL-6 or its receptors may be useful for the management of pathological pain. However, further research is warranted to extensively explore the exact role of IL-6 in pathological pain.
Schematic representation of the downstream mechanism of IL-6 in the processing of bone cancer pain and neuropathic pain. IL-6 interleukin-6, IL-6R interleukin-6 receptor, JAK Janus-activated kinase, PI3K phosphoinositide 3-kinase, TRPV1 transient receptor potential vanilloid channel type 1, MAPK mitogen-activated protein kinase, STAT3 signal transducer activator of transcription 3
Schematic representation of the possible upstream mechanism of IL-6 in the processing of neuropathic pain and inflammatory pain. PGE2 prostaglandin E2, EP4R prostaglandin E2 receptor 4, PKA protein kinase A, PKC protein kinase C, ERK extracellular signal-regulated kinase, MAPK mitogen-activated protein kinase, CREB cAMP-response element binding protein, NF-kB nuclear factor kappa B, TNF-α tumor necrosis factor-α, TNFR1 tumor necrosis factor receptor 1, IL-6 interleukin-6, CB2R cannabinoid CB2 receptor
Abbreviations
Akt, protein kinase B; BCP, bone cancer pain; CB2Rs, cannabinoid CB2 receptors; CCI, chronic constriction injury; CFA, complete Freund’s adjuvant; CIPN, chemotherapy-induced peripheral neuropathy; DRG, dorsal root ganglia; EA, electroacupuncture; ELISA, enzyme-linked immune-sorbent assay; EP4, PGE2 receptor 4; ERK, extracellular signal-regulated kinase; gp130−/−, null mutation of glycoprotein 130; IL-6, interleukin-6; IL-6R Ab, IL-6 receptor antibody; JAK, Janus-activated kinase; MAPK, mitogen-activated protein kinase; mIL-6R, membrane-bound IL-6 receptor; PI3K, phosphatidylinositol 3-kinase; PGE2, prostaglandin E2; PKC, protein kinase C; PPF, propentofylline; PSNL, partial sciatic nerve ligation; p-STAT3, phospho-signal transducer activator of transcription 3; rrIL-6, recombinant rat IL-6; RT-PCR, reverse transcription polymerase chain reaction; SCI, spinal cord injury; SCN, sciatic cryoneurolysis; sgp130, soluble form of gp130; sIL-6R, soluble form of IL-6R; TCI, tumor cell implantation; TNF-α, tumor necrosis factor-α; TNFR1, tumor necrosis factor receptor 1; TRPV1, transient receptor potential vanilloid channel type 1
References
Kuner R. Central mechanisms of pathological pain. Nat Med. 2010;16:1258–66.
Luo C, Kuner T, Kuner R. Synaptic plasticity in pathological pain. Trends Neurosci. 2014;37:343–55.
Woolf CJ, Salter MW. Neuronal plasticity: increasing the gain in pain. Science. 2000;288:1765–9.
Lorenz J, Casey KL. Imaging of acute versus pathological pain in humans. Eur J Pain. 2005;9:163–5.
Ke C, Gao F, Tian X, Li C, Shi D, He W, Tian Y. Slit2/Robo1 mediation of synaptic plasticity contributes to bone cancer pain. Mol Neurobiol. 2016. http://www.ncbi.nlm.nih.gov/pubmed/26738857?dopt=Citation.
Latremoliere A, Woolf CJ. Central sensitization: a generator of pain hypersensitivity by central neural plasticity. J Pain. 2009;10:895–926.
Basbaum AI, Bautista DM, Scherrer G, Julius D. Cellular and molecular mechanisms of pain. Cell. 2009;139:267–84.
Ji RR, Kohno T, Moore KA, Woolf CJ. Central sensitization and LTP: do pain and memory share similar mechanisms? Trends Neurosci. 2003;26:696–705.
Hua B, Gao Y, Kong X, Yang L, Hou W, Bao Y. New insights of nociceptor sensitization in bone cancer pain. Expert Opin Ther Targets. 2015;19:227–43.
Clark AK, Old EA, Malcangio M. Neuropathic pain and cytokines: current perspectives. J Pain Res. 2013;6:803–14.
Stow JL, Murray RZ. Intracellular trafficking and secretion of inflammatory cytokines. Cytokine Growth Factor Rev. 2013;24:227–39.
Han D, Wu C, Xiong Q, Zhou L, Tian Y. Anti-inflammatory mechanism of bone marrow mesenchymal stem cell transplantation in rat model of spinal cord injury. Cell Biochem Biophys. 2015;71:1341–7.
Bu H, Shu B, Gao F, Liu C, Guan X, Ke C, Cao F, Hinton AO, Jr., Xiang H, Yang H, et al. Spinal IFN-gamma-induced protein-10 (CXCL10) mediates metastatic breast cancer-induced bone pain by activation of microglia in rat models. Breast Cancer Res Treat. 2014;143:255–63.
Guan XH, Fu QC, Shi D, Bu HL, Song ZP, Xiong BR, Shu B, Xiang HB, Xu B, Manyande A,. Activation of spinal chemokine receptor CXCR3 mediates bone cancer pain through an Akt-ERK crosstalk pathway in rats. Exp Neurol. 2015;263:39–49.
Liu X, Bu H, Liu C, Gao F, Yang H, Tian X, Xu A, Chen Z, Cao F, Tian Y. Inhibition of glial activation in rostral ventromedial medulla attenuates mechanical allodynia in a rat model of cancer-induced bone pain. J Huazhong Univ Sci Technolog Med Sci. 2012;32:291–8.
Ye D, Bu H, Guo G, Shu B, Wang W, Guan X, Yang H, Tian X, Xiang H, Gao F. Activation of CXCL10/CXCR3 signaling attenuates morphine analgesia: involvement of Gi protein. J Mol Neurosci. 2014;53:571–9.
Zhou YQ, Gao HY, Guan XH, Yuan X, Fang GG, Chen Y, Ye DW. Chemokines and their receptors: potential therapeutic targets for bone cancer pain. Curr Pharm Des. 2015;21:5029–33.
Song ZP, Xiong BR, Guan XH, Cao F, Manyande A, Zhou YQ, Zheng H, Tian YK. Minocycline attenuates bone cancer pain in rats by inhibiting NFkappaB in spinal astrocytes. Acta Pharmacol Sin. 2016;37:753–62.
Guan X, Fu Q, Xiong B, Song Z, Shu B, Bu H, Xu B, Manyande A, Cao F, Tian Y. Activation of PI3Kgamma/Akt pathway mediates bone cancer pain in rats. J Neurochem. 2015;134:590–600.
Fang D, Kong LY, Cai J, Li S, Liu XD, Han JS, Xing GG. Interleukin-6-mediated functional upregulation of TRPV1 receptors in dorsal root ganglion neurons through the activation of JAK/PI3K signaling pathway: roles in the development of bone cancer pain in a rat model. Pain. 2015;156:1124–44.
Lee KM, Jeon SM, Cho HJ. Interleukin-6 induces microglial CX3CR1 expression in the spinal cord after peripheral nerve injury through the activation of p38 MAPK. Eur J Pain. 2010;14:682. e681-612.
Guptarak J, Wanchoo S, Durham-Lee J, Wu Y, Zivadinovic D, Paulucci-Holthauzen A, Nesic O. Inhibition of IL-6 signaling: a novel therapeutic approach to treating spinal cord injury pain. Pain. 2013;154:1115–28.
Kiguchi N, Maeda T, Kobayashi Y, Kishioka S. Up-regulation of tumor necrosis factor-alpha in spinal cord contributes to vincristine-induced mechanical allodynia in mice. Neurosci Lett. 2008;445:140–3.
Su TF, Zhao YQ, Zhang LH, Peng M, Wu CH, Pei L, Tian B, Zhang J, Shi J, Pan HL, Li M. Electroacupuncture reduces the expression of proinflammatory cytokines in inflamed skin tissues through activation of cannabinoid CB2 receptors. Eur J Pain. 2012;16:624–35.
Hirano T, Yasukawa K, Harada H, Taga T, Watanabe Y, Matsuda T, Kashiwamura S, Nakajima K, Koyama K, Iwamatsu A, et al. Complementary DNA for a novel human interleukin (BSF-2) that induces B lymphocytes to produce immunoglobulin. Nature. 1986;324:73–6.
Scheller J, Garbers C, Rose-John S. Interleukin-6: from basic biology to selective blockade of pro-inflammatory activities. Semin Immunol. 2014;26:2–12.
Tanaka T, Kishimoto T. The biology and medical implications of interleukin-6. Cancer Immunol Res. 2014;2:288–94.
Kishimoto T. Interleukin-6: from basic science to medicine—40 years in immunology. Annu Rev Immunol. 2005;23:1–21.
Heinrich PC, Behrmann I, Haan S, Hermanns HM, Muller-Newen G, Schaper F. Principles of interleukin (IL)-6-type cytokine signalling and its regulation. Biochem J. 2003;374:1–20.
Boulanger MJ, Chow DC, Brevnova EE, Garcia KC. Hexameric structure and assembly of the interleukin-6/IL-6 alpha-receptor/gp130 complex. Science. 2003;300:2101–4.
Wolf J, Rose-John S, Garbers C. Interleukin-6 and its receptors: a highly regulated and dynamic system. Cytokine. 2014;70:11–20.
Neurath MF, Finotto S. IL-6 signaling in autoimmunity, chronic inflammation and inflammation-associated cancer. Cytokine Growth Factor Rev. 2011;22:83–9.
Horiuchi S, Koyanagi Y, Zhou Y, Miyamoto H, Tanaka Y, Waki M, Matsumoto A, Yamamoto M, Yamamoto N. Soluble interleukin-6 receptors released from T cell or granulocyte/macrophage cell lines and human peripheral blood mononuclear cells are generated through an alternative splicing mechanism. Eur J Immunol. 1994;24:1945–8.
Mullberg J, Schooltink H, Stoyan T, Gunther M, Graeve L, Buse G, Mackiewicz A, Heinrich PC, Rose-John S. The soluble interleukin-6 receptor is generated by shedding. Eur J Immunol. 1993;23:473–80.
Rivera M, Talens-Visconti R, Sirera R, Bertomeu V, Salvador A, Cortes R, Garcia de Burgos F, Climent V, Paya R, Martinez-Dolz L, et al. Soluble TNF-alpha and interleukin-6 receptors in the urine of heart failure patients. Their clinical value and relationship with plasma levels. Eur J Heart Fail. 2004;6:877–82.
Rose-John S, Scheller J, Elson G, Jones SA. Interleukin-6 biology is coordinated by membrane-bound and soluble receptors: role in inflammation and cancer. J Leukoc Biol. 2006;80:227–36.
Rose-John S, Waetzig GH, Scheller J, Grotzinger J, Seegert D. The IL-6/sIL-6R complex as a novel target for therapeutic approaches. Expert Opin Ther Targets. 2007;11:613–24.
Rose-John S. IL-6 trans-signaling via the soluble IL-6 receptor: importance for the pro-inflammatory activities of IL-6. Int J Biol Sci. 2012;8:1237–47.
Metz S, Wiesinger M, Vogt M, Lauks H, Schmalzing G, Heinrich PC, Muller-Newen G. Characterization of the interleukin (IL)-6 Inhibitor IL-6-RFP: fused receptor domains act as high affinity cytokine-binding proteins. J Biol Chem. 2007;282:1238–48.
Garbers C, Thaiss W, Jones GW, Waetzig GH, Lorenzen I, Guilhot F, Lissilaa R, Ferlin WG, Grotzinger J, Jones SA, et al. Inhibition of classic signaling is a novel function of soluble glycoprotein 130 (sgp130), which is controlled by the ratio of interleukin 6 and soluble interleukin 6 receptor. J Biol Chem. 2011;286:42959–70.
Jostock T, Mullberg J, Ozbek S, Atreya R, Blinn G, Voltz N, Fischer M, Neurath MF, Rose-John S. Soluble gp130 is the natural inhibitor of soluble interleukin-6 receptor transsignaling responses. Eur J Biochem. 2001;268:160–7.
Melemedjian OK, Asiedu MN, Tillu DV, Peebles KA, Yan J, Ertz N, Dussor GO, Price TJ. IL-6- and NGF-induced rapid control of protein synthesis and nociceptive plasticity via convergent signaling to the eIF4F complex. J Neurosci. 2010;30:15113–23.
Melemedjian OK, Tillu DV, Moy JK, Asiedu MN, Mandell EK, Ghosh S, Dussor G, Price TJ. Local translation and retrograde axonal transport of CREB regulates IL-6-induced nociceptive plasticity. Mol Pain. 2014;10:45.
Vazquez E, Kahlenbach J, Segond von Banchet G, Konig C, Schaible HG, Ebersberger A. Spinal interleukin-6 is an amplifier of arthritic pain in the rat. Arthritis Rheum. 2012;64:2233–42.
Brenn D, Richter F, Schaible HG. Sensitization of unmyelinated sensory fibers of the joint nerve to mechanical stimuli by interleukin-6 in the rat: an inflammatory mechanism of joint pain. Arthritis Rheum. 2007;56:351–9.
Obreja O, Schmelz M, Poole S, Kress M. Interleukin-6 in combination with its soluble IL-6 receptor sensitises rat skin nociceptors to heat, in vivo. Pain. 2002;96:57–62.
Cunha FQ, Poole S, Lorenzetti BB, Ferreira SH. The pivotal role of tumour necrosis factor alpha in the development of inflammatory hyperalgesia. Br J Pharmacol. 1992;107:660–4.
Miyagawa I, Nakayamada S, Saito K, Hanami K, Nawata M, Sawamukai N, Nakano K, Yamaoka K, Tanaka Y. Study on the safety and efficacy of tocilizumab, an anti-IL-6 receptor antibody, in patients with rheumatoid arthritis complicated with AA amyloidosis. Mod Rheumatol. 2014;24:405–9.
Araki M, Matsuoka T, Miyamoto K, Kusunoki S, Okamoto T, Murata M, Miyake S, Aranami T, Yamamura T. Efficacy of the anti-IL-6 receptor antibody tocilizumab in neuromyelitis optica: a pilot study. Neurology. 2014;82:1302–6.
Imagawa T, Yokota S, Mori M, Miyamae T, Takei S, Imanaka H, Nerome Y, Iwata N, Murata T, Miyoshi M, et al. Safety and efficacy of tocilizumab, an anti-IL-6-receptor monoclonal antibody, in patients with polyarticular-course juvenile idiopathic arthritis. Mod Rheumatol. 2012;22:109–15.
Coleman RE. Clinical features of metastatic bone disease and risk of skeletal morbidity. Clin Cancer Res. 2006;12:6243s–9s.
Costantini M, Ripamonti C, Beccaro M, Montella M, Borgia P, Casella C, Miccinesi G. Prevalence, distress, management, and relief of pain during the last 3 months of cancer patients’ life. Results of an Italian mortality follow-back survey. Ann Oncol. 2009;20:729–35.
Yeh DC, Chen DR, Chao TY, Chen SC, Wang HC, Rau KM, Feng YH, Chang YC, Lee KD, Ou-Yang F, et al. EORTC QLQ-BM22 quality of life evaluation and pain outcome in patients with bone metastases from breast cancer treated with zoledronic acid. In Vivo. 2014;28:1001–4.
Chavele KM, Merry E, Ehrenstein MR. Cutting edge: circulating plasmablasts induce the differentiation of human T follicular helper cells via IL-6 production. J Immunol. 2015;194:2482–5.
Sun W, Liu DB, Li WW, Zhang LL, Long GX, Wang JF, Mei Q, Hu GQ. Interleukin-6 promotes the migration and invasion of nasopharyngeal carcinoma cell lines and upregulates the expression of MMP-2 and MMP-9. Int J Oncol. 2014;44:1551–60.
Tzeng HE, Tsai CH, Chang ZL, Su CM, Wang SW, Hwang WL, Tang CH. Interleukin-6 induces vascular endothelial growth factor expression and promotes angiogenesis through apoptosis signal-regulating kinase 1 in human osteosarcoma. Biochem Pharmacol. 2013;85:531–40.
Santer FR, Malinowska K, Culig Z, Cavarretta IT. Interleukin-6 trans-signalling differentially regulates proliferation, migration, adhesion and maspin expression in human prostate cancer cells. Endocr Relat Cancer. 2010;17:241–53.
Dong Y, Mao-Ying QL, Chen JW, Yang CJ, Wang YQ, Tan ZM. Involvement of EphB1 receptor/ephrinB1 ligand in bone cancer pain. Neurosci Lett. 2011;496:163–7.
Yao M, Chang XY, Chu YX, Yang JP, Wang LN, Cao HQ, Liu MJ, Xu QN. Antiallodynic effects of propentofylline elicited by interrupting spinal glial function in a rat model of bone cancer pain. J Neurosci Res. 2011;89:1877–86.
Ren BX, Ji Y, Tang JC, Sun DP, Hui X, Yang DQ, Zhu XL. Effect of tanshinone IIA intrathecal injections on pain and spinal inflammation in mice with bone tumors. Genet Mol Res. 2015;14:2133–8.
Lu C, Liu Y, Sun B, Sun Y, Hou B, Zhang Y, Ma Z, Gu X. Intrathecal injection of JWH-015 attenuates bone cancer pain via time-dependent modification of pro-inflammatory cytokines expression and astrocytes activity in spinal cord. Inflammation. 2015;38:1880–90.
Andratsch M, Mair N, Constantin CE, Scherbakov N, Benetti C, Quarta S, Vogl C, Sailer CA, Uceyler N, Brockhaus J, et al. A key role for gp130 expressed on peripheral sensory nerves in pathological pain. J Neurosci. 2009;29:13473–83.
Quarta S, Vogl C, Constantin CE, Uceyler N, Sommer C, Kress M. Genetic evidence for an essential role of neuronally expressed IL-6 signal transducer gp130 in the induction and maintenance of experimentally induced mechanical hypersensitivity in vivo and in vitro. Mol Pain. 2011;7:73.
Nightingale S. The neuropathic pain market. Nat Rev Drug Discov. 2012;11:101–2.
Tsuda M, Inoue K. Neuron-microglia interaction by purinergic signaling in neuropathic pain following neurodegeneration. Neuropharmacol. 2016:104:76–81.
Baron R, Binder A, Wasner G. Neuropathic pain: diagnosis, pathophysiological mechanisms, and treatment. Lancet Neurol. 2010;9:807–19.
Smith EM, Bridges CM, Kanzawa G, Knoerl R, Kelly JP, Berezovsky A, Woo C. Cancer treatment-related neuropathic pain syndromes—epidemiology and treatment: an update. Curr Pain Headache Rep. 2014;18:459.
van Hecke O, Austin SK, Khan RA, Smith BH, Torrance N. Neuropathic pain in the general population: a systematic review of epidemiological studies. Pain. 2014;155:654–62.
Gilron I, Baron R, Jensen T. Neuropathic pain: principles of diagnosis and treatment. Mayo Clin Proc. 2015;90:532–45.
Bridges D, Thompson SW, Rice AS. Mechanisms of neuropathic pain. Br J Anaesth. 2001;87:12–26.
Baron R. Mechanisms of disease: neuropathic pain—a clinical perspective. Nat Clin Pract Neurol. 2006;2:95–106.
DeLeo JA, Colburn RW, Nichols M, Malhotra A. Interleukin-6-mediated hyperalgesia/allodynia and increased spinal IL-6 expression in a rat mononeuropathy model. J Interferon Cytokine Res. 1996;16:695–700.
Arruda JL, Colburn RW, Rickman AJ, Rutkowski MD, DeLeo JA. Increase of interleukin-6 mRNA in the spinal cord following peripheral nerve injury in the rat: potential role of IL-6 in neuropathic pain. Brain Res Mol Brain Res. 1998;62:228–35.
Arruda JL, Sweitzer S, Rutkowski MD, DeLeo JA. Intrathecal anti-IL-6 antibody and IgG attenuates peripheral nerve injury-induced mechanical allodynia in the rat: possible immune modulation in neuropathic pain. Brain Res. 2000;879:216–25.
Ramer MS, Murphy PG, Richardson PM, Bisby MA. Spinal nerve lesion-induced mechanoallodynia and adrenergic sprouting in sensory ganglia are attenuated in interleukin-6 knockout mice. Pain. 1998;78:115–21.
Murphy PG, Ramer MS, Borthwick L, Gauldie J, Richardson PM, Bisby MA. Endogenous interleukin-6 contributes to hypersensitivity to cutaneous stimuli and changes in neuropeptides associated with chronic nerve constriction in mice. Eur J Neurosci. 1999;11:2243–53.
Brazda V, Klusakova I, Hradilova Svizenska I, Dubovy P. Dynamic response to peripheral nerve injury detected by in situ hybridization of IL-6 and its receptor mRNAs in the dorsal root ganglia is not strictly correlated with signs of neuropathic pain. Mol Pain. 2013;9:42.
Dubovy P, Brazda V, Klusakova I, Hradilova-Svizenska I. Bilateral elevation of interleukin-6 protein and mRNA in both lumbar and cervical dorsal root ganglia following unilateral chronic compression injury of the sciatic nerve. J Neuroinflammation. 2013;10:55.
Ma W, Quirion R. Up-regulation of interleukin-6 induced by prostaglandin E from invading macrophages following nerve injury: an in vivo and in vitro study. J Neurochem. 2005;93:664–73.
St-Jacques B, Ma W. Role of prostaglandin E2 in the synthesis of the pro-inflammatory cytokine interleukin-6 in primary sensory neurons: an in vivo and in vitro study. J Neurochem. 2011;118:841–54.
Dominguez E, Rivat C, Pommier B, Mauborgne A, Pohl M. JAK/STAT3 pathway is activated in spinal cord microglia after peripheral nerve injury and contributes to neuropathic pain development in rat. J Neurochem. 2008;107:50–60.
Milligan ED, Twining C, Chacur M, Biedenkapp J, O'Connor K, Poole S, Tracey K, Martin D, Maier SF, Watkins LR. Spinal glia and proinflammatory cytokines mediate mirror-image neuropathic pain in rats. J Neurosci. 2003;23:1026–40.
Gerard E, Spengler RN, Bonoiu AC, Mahajan SD, Davidson BA, Ding H, Kumar R, Prasad PN, Knight PR, Ignatowski TA. Chronic constriction injury-induced nociception is relieved by nanomedicine-mediated decrease of rat hippocampal tumor necrosis factor. Pain. 2015;156:1320–33.
Lee KM, Jeon SM, Cho HJ. Tumor necrosis factor receptor 1 induces interleukin-6 upregulation through NF-kappaB in a rat neuropathic pain model. Eur J Pain. 2009;13:794–806.
Zanjani TM, Sabetkasaei M, Mosaffa N, Manaheji H, Labibi F, Farokhi B. Suppression of interleukin-6 by minocycline in a rat model of neuropathic pain. Eur J Pharmacol. 2006;538:66–72.
Chao PK, Lu KT, Lee YL, Chen JC, Wang HL, Yang YL, Cheng MY, Liao MF, Ro LS. Early systemic granulocyte-colony stimulating factor treatment attenuates neuropathic pain after peripheral nerve injury. PLoS One. 2012;7:e43680.
Ebisawa S, Andoh T, Shimada Y, Kuraishi Y. Yokukansan improves mechanical allodynia through the regulation of interleukin-6 expression in the spinal cord in mice with neuropathic pain. Evid Based Complement Alternat Med. 2015;2015:870687.
Ohtori S, Miyagi M, Eguchi Y, Inoue G, Orita S, Ochiai N, Kishida S, Kuniyoshi K, Nakamura J, Aoki Y, et al. Efficacy of epidural administration of anti-interleukin-6 receptor antibody onto spinal nerve for treatment of sciatica. Eur Spine J. 2012;21:2079–84.
Finnerup NB. Pain in patients with spinal cord injury. Pain. 2013;154 Suppl 1:S71–76.
Finnerup NB, Johannesen IL, Sindrup SH, Bach FW, Jensen TS. Pain and dysesthesia in patients with spinal cord injury: a postal survey. Spinal Cord. 2001;39:256–62.
Murakami T, Kanchiku T, Suzuki H, Imajo Y, Yoshida Y, Nomura H, Cui D, Ishikawa T, Ikeda E, Taguchi T. Anti-interleukin-6 receptor antibody reduces neuropathic pain following spinal cord injury in mice. Exp Ther Med. 2013;6:1194–8.
Miltenburg NC, Boogerd W. Chemotherapy-induced neuropathy: a comprehensive survey. Cancer Treat Rev. 2014;40:872–82.
Seretny M, Currie GL, Sena ES, Ramnarine S, Grant R, MacLeod MR, Colvin LA, Fallon M. Incidence, prevalence, and predictors of chemotherapy-induced peripheral neuropathy: a systematic review and meta-analysis. Pain. 2014;155:2461–70.
Callizot N, Andriambeloson E, Glass J, Revel M, Ferro P, Cirillo R, Vitte PA, Dreano M. Interleukin-6 protects against paclitaxel, cisplatin and vincristine-induced neuropathies without impairing chemotherapeutic activity. Cancer Chemother Pharmacol. 2008;62:995–1007.
Kiguchi N, Maeda T, Kobayashi Y, Kondo T, Ozaki M, Kishioka S. The critical role of invading peripheral macrophage-derived interleukin-6 in vincristine-induced mechanical allodynia in mice. Eur J Pharmacol. 2008;592:87–92.
Starkweather A. Increased interleukin-6 activity associated with painful chemotherapy-induced peripheral neuropathy in women after breast cancer treatment. Nurs Res Pract. 2010;2010:281531.
Millan MJ. The induction of pain: an integrative review. Prog Neurobiol. 1999;57:1–164.
Fan QQ, Li L, Wang WT, Yang X, Suo ZW, Hu XD. Activation of alpha2 adrenoceptors inhibited NMDA receptor-mediated nociceptive transmission in spinal dorsal horn of mice with inflammatory pain. Neuropharmacology. 2014;77:185–92.
Su TF, Zhang LH, Peng M, Wu CH, Pan W, Tian B, Shi J, Pan HL, Li M. Cannabinoid CB2 receptors contribute to upregulation of beta-endorphin in inflamed skin tissues by electroacupuncture. Mol Pain. 2011;7:98.
Zhang J, Chen L, Su T, Cao F, Meng X, Pei L, Shi J, Pan HL, Li M. Electroacupuncture increases CB2 receptor expression on keratinocytes and infiltrating inflammatory cells in inflamed skin tissues of rats. J Pain. 2010;11:1250–8.
Chen L, Zhang J, Li F, Qiu Y, Wang L, Li YH, Shi J, Pan HL, Li M. Endogenous anandamide and cannabinoid receptor-2 contribute to electroacupuncture analgesia in rats. J Pain. 2009;10:732–9.
Sun S, Yin Y, Yin X, Cao F, Luo D, Zhang T, Li Y, Ni L. Anti-nociceptive effects of tanshinone IIA (TIIA) in a rat model of complete Freund’s adjuvant (CFA)-induced inflammatory pain. Brain Res Bull. 2012;88:581–8.
Xu F, Li Y, Li S, Ma Y, Zhao N, Liu Y, Qian N, Zhao H, Li Y. Complete Freund’s adjuvant-induced acute inflammatory pain could be attenuated by triptolide via inhibiting spinal glia activation in rats. J Surg Res. 2014;188:174–82.
Yang Y, Li YX, Wang HL, Jin SJ, Zhou R, Qiao HQ, Du J, Wu J, Zhao CJ, Niu Y, et al. Oxysophocarpine ameliorates carrageenan-induced inflammatory pain via inhibiting expressions of prostaglandin E2 and cytokines in mice. Planta Med. 2015;81:791–7.
Choy EH, Isenberg DA, Garrood T, Farrow S, Ioannou Y, Bird H, Cheung N, Williams B, Hazleman B, Price R, et al. Therapeutic benefit of blocking interleukin-6 activity with an anti-interleukin-6 receptor monoclonal antibody in rheumatoid arthritis: a randomized, double-blind, placebo-controlled, dose-escalation trial. Arthritis Rheum. 2002;46:3143–50.
Nishimoto N, Yoshizaki K, Miyasaka N, Yamamoto K, Kawai S, Takeuchi T, Hashimoto J, Azuma J, Kishimoto T. Treatment of rheumatoid arthritis with humanized anti-interleukin-6 receptor antibody: a multicenter, double-blind, placebo-controlled trial. Arthritis Rheum. 2004;50:1761–9.
Alten R. Tocilizumab: a novel humanized anti-interleukin 6 receptor antibody for the treatment of patients with rheumatoid arthritis. Ther Adv Musculoskelet Dis. 2011;3:133–49.
Tanaka E, Inoue E, Hoshi D, Shimizu Y, Kobayashi A, Sugimoto N, Shidara K, Sato E, Seto Y, Nakajima A, et al. Cost-effectiveness of tocilizumab, a humanized anti-interleukin-6 receptor monoclonal antibody, versus methotrexate in patients with rheumatoid arthritis using real-world data from the IORRA observational cohort study. Mod Rheumatol. 2015;25:503–13.
Tanaka T, Hishitani Y, Ogata A. Monoclonal antibodies in rheumatoid arthritis: comparative effectiveness of tocilizumab with tumor necrosis factor inhibitors. Biologics. 2014;8:141–53.
Schiff MH, Kremer JM, Jahreis A, Vernon E, Isaacs JD, van Vollenhoven RF. Integrated safety in tocilizumab clinical trials. Arthritis Res Ther. 2011;13:R141.
Yokota S, Imagawa T, Mori M, Miyamae T, Aihara Y, Takei S, Iwata N, Umebayashi H, Murata T, Miyoshi M, et al. Efficacy and safety of tocilizumab in patients with systemic-onset juvenile idiopathic arthritis: a randomised, double-blind, placebo-controlled, withdrawal phase III trial. Lancet. 2008;371:998–1006.
De Benedetti F, Brunner HI, Ruperto N, Kenwright A, Wright S, Calvo I, Cuttica R, Ravelli A, Schneider R, Woo P, et al. Randomized trial of tocilizumab in systemic juvenile idiopathic arthritis. N Engl J Med. 2012;367:2385–95.
Brunner HI, Ruperto N, Zuber Z, Keane C, Harari O, Kenwright A, Lu P, Cuttica R, Keltsev V, Xavier RM, et al. Efficacy and safety of tocilizumab in patients with polyarticular-course juvenile idiopathic arthritis: results from a phase 3, randomised, double-blind withdrawal trial. Ann Rheum Dis. 2015;74:1110–7.
Nishimoto N, Sasai M, Shima Y, Nakagawa M, Matsumoto T, Shirai T, Kishimoto T, Yoshizaki K. Improvement in Castleman’s disease by humanized anti-interleukin-6 receptor antibody therapy. Blood. 2000;95:56–61.
Nishimoto N, Kanakura Y, Aozasa K, Johkoh T, Nakamura M, Nakano S, Nakano N, Ikeda Y, Sasaki T, Nishioka K, et al. Humanized anti-interleukin-6 receptor antibody treatment of multicentric Castleman disease. Blood. 2005;106:2627–32.
Higuchi T, Nakanishi T, Takada K, Matsumoto M, Okada M, Horikoshi H, Suzuki K. A case of multicentric Castleman’s disease having lung lesion successfully treated with humanized anti-interleukin-6 receptor antibody, tocilizumab. J Korean Med Sci. 2010;25:1364–7.
Sainoh T, Orita S, Miyagi M, Inoue G, Yamauchi K, Suzuki M, Sakuma Y, Kubota G, Oikawa Y, Inage K, et al. Single intradiscal injection of the interleukin-6 receptor antibody tocilizumab provides short-term relief of discogenic low back pain; prospective comparative cohort study. J Orthop Sci. 2016;21:2–6.
Acknowledgements
Not applicable.
Funding
This work was supported by grants from National Natural Science Foundation of People’s Republic China 81371250, 81400917, and 81571053, National Natural Science Foundation of Hubei Province 2014CFB449, Shenzhen Science and Technology Innovation Committee GJHZ20140414170821201, and Specialized Research Fund for the Doctoral Program of Higher Education No.20130142120102, HUST No. 2014QT021.
Availability of data and materials
The data supporting the conclusions of this article is included within the “References” section.
Authors’ contributions
YQZ, ZL, ZHL, and SPC involved in acquisition of data, analysis of data, and drafting of the manuscript. DWY, ML, AS, and YKT involved in study concept and critical revision of the manuscript. YQZ, ZL, and ZHL contributed equally to this work. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Not applicable.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Zhou, YQ., Liu, Z., Liu, ZH. et al. Interleukin-6: an emerging regulator of pathological pain. J Neuroinflammation 13, 141 (2016). https://doi.org/10.1186/s12974-016-0607-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12974-016-0607-6