Abstract
Gliomas are the common type of brain tumors originating from glial cells. Epidemiologically, gliomas occur among all ages, more often seen in adults, which males are more susceptible than females. According to the fifth edition of the WHO Classification of Tumors of the Central Nervous System (WHO CNS5), standard of care and prognosis of gliomas can be dramatically different. Generally, circumscribed gliomas are usually benign and recommended to early complete resection, with chemotherapy if necessary. Diffuse gliomas and other high-grade gliomas according to their molecule subtype are slightly intractable, with necessity of chemotherapy. However, for glioblastoma, feasible resection followed by radiotherapy plus temozolomide chemotherapy define the current standard of care. Here, we discuss novel feasible or potential targets for treatment of gliomas, especially IDH-wild type glioblastoma. Classic targets such as the p53 and retinoblastoma (RB) pathway and epidermal growth factor receptor (EGFR) gene alteration have met failure due to complex regulatory network. There is ever-increasing interest in immunotherapy (immune checkpoint molecule, tumor associated macrophage, dendritic cell vaccine, CAR-T), tumor microenvironment, and combination of several efficacious methods. With many targeted therapy options emerging, biomarkers guiding the prescription of a particular targeted therapy are also attractive. More pre-clinical and clinical trials are urgently needed to explore and evaluate the feasibility of targeted therapy with the corresponding biomarkers for effective personalized treatment options.
Similar content being viewed by others

Introduction
The most common malignant primary brain tumor in adults is glioma. Based on the previous histological classification of gliomas from grade I to IV in WHO classification in 2016 [1], molecular biomarkers of different tumor types were updated in WHO CNS5 in 2021, bringing more benefits and meaningful instructions to clinic. Generally, gliomas are divided into circumscribed gliomas and diffuse gliomas, with the former one being benign and curable after complete surgical resection and the latter one being more malignant and unable to be cured following surgical resection alone. According to that the fifth-edition WHO Blue Books have emphasized, use of Arabic numerals for grading is recommended [2]. In addition, WHO CNS5 has proclaimed the importance of grading within tumor type. Thus 4 different families are divided: 1) Adult-type diffuse gliomas; 2) Pediatric-type diffuse low-grade gliomas; 3) Pediatric-type diffuse high-grade gliomas; and 4) Circumscribed astrocytic gliomas. Nevertheless, for convenience, here we review targeted therapy of gliomas still in an order of summing up different types of tumors in a certain grade. Thus overall, low-grade glioma (LGG) contains CNS WHO grades 1–2, while high-grade glioma (HGG) contains CNS WHO grades 3–4. LGG, accounting for 6% of CNS primary tumors in adult, usually presents more promising prognosis [3]. The more common CNS WHO grade 1 LGG in child have the best prognosis [4], while grade 2 LGG usually relapses and progresses to HGG [5]. Besides diffuse midline glioma H3 K27M-altered, glioblastoma (GBM) is the majority of WHO grade 4. GBM is one of the most lethal and prone to recurrence malignant solid tumor, accounting for 57% of all gliomas and 48% of primary CNS malignant tumors [6], with median survival time less than 2 years. Currently, standard magnetic resonance imaging could provide the most initial and sensitive diagnosis to GBM, while GBM diagnosed with such method have usually developed into advanced stage [7].
Both The 2016 WHO classification and WHO CNS5 have declared the mutational status of isocitrate dehydrogenase (IDH) should be considered regarding LGG, which emphasized IDH-wildtype (IDH-WT) as the critical biomarker of high-risk LGG since the molecular characteristics and clinical manifestations of IDH-WT LGG are similar to those of GBM. Analogously, glioblastomas with mutant IDH are characteristically similar to anaplastic astrocytoma (though nomenclature “anaplastic astrocytoma” is no longer included in WHO CNS5 classification), thus treatment of glioma much relying on molecular diagnosis and classification.
Except for IDH status, MGMT methylation is hitherto regarded as another significantly prognostic biomarker. Other markers in CNS5 are merely related to grade and further estimate prognosis, such as CDKN2A/B homozygous deletion in IDH-mutant astrocytoma, as well as 1p/19q co-deleted, TERT promoter mutation, EGFR amplification or mutation, and + 7/ − 10 copy number changes in IDH-wildtype diffuse astrocytoma [2]. Among those, only EGFRvIII mutation is unequivocally clinically instructional (see below). Recently researchers have also concentrated on mismatch repair (MMR) protein as a novel biomarker due to its high relevant association with tumor mutational burden (TMB) [8], though it appears MMR status in recurrence GBM is not a prognostic marker. Thus, treatment of glioma much relying on molecular biomarkers as criteria of diagnosis and classification.
Histologically, LGG tumor cells present nuclear atypia and increased mitotic activity, while GBM cells characteristically remain areas of microvascular proliferation, focal necrosis, or both [9]. Histological distinction does not make a difference to the current clinical treatment. However, the variety of molecular subtypes is often related to the treatment and prognosis of patients. Specifically, IDH-WT glioblastoma usually contains higher level of epidermal growth factor receptor (EGFR) amplification, TERT promoter mutation and PTEN deletion, etc. [10]. Meanwhile, patients with MGMT promoter methylation, observed in 30% to 50% of IDH-WT glioblastoma [11, 12], may present better prognosis and treatment response. Pediatric LGGs and those in adults are distinct in molecular characteristics, though similarities on histology exist a lot. Pediatric LGGs were thought to carry mutations of FGFR1 and BRAF, both concentrating on MAPK pathway, although recently in WHO CNS5 pediatric-type low-grade diffuse gliomas include Diffuse astrocytoma, MYB- or MYBL1-altered; Angiocentric glioma; Polymorphous low-grade neuroepithelial tumor of the young; and Diffuse LGG, MAPK pathway-altered. Adult LGGs are characterized by mutations of IDH1/2 and ATRX, with 1p/19q codeletion sometimes. TERT promoter mutation was also found in LGG, which has to do with oligodendroglioma. Moreover, Epithelioid glioblastoma, as a newly discovered GBM tissue subtype, often carries BRAFV600E mutations. Since the consensus treatment currently is restricted to limited number of patients (as mentioned below) and most of gliomas failed to meet completely recovery, including either unexpected relapse or worse progression in LGGs and poor survival particularly in GBM, original insights into therapies are pressing. With regard to molecular heterogeneity, the importance of varying and adequate targeted therapy is self-evident in order to open up more possibility to treatment of gliomas, to say nothing of the fact that since the discovery of PD1/PDL1 awarded as Nobel Prize more and more immunotherapy options have been proposed and developing. Correspondingly, predictive biomarkers are strongly recommended to be identified for optimizing the efficacy of immunotherapy. For instance, MHC class I-negative glioma cells were found to be associated with inactivation and resistance to immunotherapy [8].
Current standard of care
As discussed above, the prognosis of WHO grade 1 and 2 glioma is the most promising [13], whereas differing from classification of molecular phenotype. IDH mutation and 1p/19q codeletion tumor (corresponding to oligodendroglioma) has the best prognosis, followed by IDH mutation and 1p/19q intact tumor, and IDH wild type tumor [14]. Although it is previously thought that "wait and see" approach could be used safely and appropriately for LGGs, recent trials have found that surgical resection should be performed on patients as soon as possible to avoid subsequent malignant progression of the tumor and meanwhile to accurately identify the molecular subtypes of the tumor [15]. For high-risk LGG, due to the high possibility of recurrence, the standard of postoperative care is necessary, including 50-54 Gy local radiotherapy, followed by 6 cycles of adjuvant procarbazine or Lomustine or vincristine (PCV), in which Lomustine is usually selected, due to its respectively mild toxicity and blood–brain barrier limitations [14]. Recent decades, the replacement or combination of radiotherapy with chemotherapy and target therapy and individualized treatment for different patients have been gradually proposed [16,17,18]. For instance, for some patients with unresectable pediatric LGG, carboplatin and vincristine are regarded as standard treatment [19].
For GBM, a gross total resection, radiotherapy in the focal tumor area and concomitant Temozolomide (TMZ) chemotherapy and certain dose of radiotherapy should be taken as the standard treatment (Stupp treatment) [20, 21]. Tumor-treating field, as a novel strategy of care, improves progression-free survival (PFS) and overall survival (OS) [22], whereas not included in the current general consensus on GBM treatment. All glioblastomas will eventually progress or relapse, and there is no standard treatment for recurrent GBM (rGBM). Lomustine, another alkylating agent, most widely used in recurrent GBM and also in “control group” in the lately recurrent GBM randomized trial [23], is partially considered to be the standard choice for rGBM, but only effective in patients with MGMT methylation [6]. European association of neuro-oncology (EANO) proposed for patients with rGBM to continue using TMZ or Bevacizumab [20]. However, TMZ often produces drug resistance due to the non-methylated MGMT promoter in tumor cells of patients [24], and bevacizumab could only prolong the PFS of rGBM. Notably, the combined therapy presents better effect.
Glioblastoma
Alkylating agent and MGMT promoter methylation
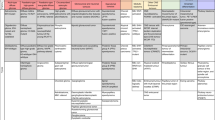
Temozolomide, currently used in the standard treatment of GBM, is an alkylating agent that induces tumor cell death by alkylating DNA at multiple sites. O6-methylguanine DNA methyltransferase (MGMT) functions as a sort of repairing protein [25, 26], which is encoded by MGMT and could reverse this alkylation process by consuming itself. Hence, MGMT promoter methylation is a strong prognostic biomarker and brings benefits, at least theoretically, to patients treated with TMZ combined with radiotherapy [25, 27] (Table 1).
Studies have confirmed that it’s better to initiate post-surgery TMZ chemotherapy within 6 months [28, 29]. Since the effect of TMZ combined with radiotherapy differs among patients, evaluating the status of MGMT promoter has been recognized for its significance. Though there is no such thing as international consensus on the best diagnostic method of measuring MGMT promoter [30], there have been various development to evaluate the level of MGMT methylation in patients with GBM [30,31,32,33]. There is occasionally no predictive relationship between the methylation level of MGMT promoter and the level of the corresponding protein. Clinical trial showed that TMZ might lead to recurrence of GBM with high expression of MGMT [34], and resistance to TMZ was presumed related to MGMT gene fusion or rearrangement mutation [35]. Thus, more effective target therapies are urgently needed.
Recently, animal models present that Bortezomib could increase the sensitivity of GBM to temozolomide by reducing MGMT mRNA and protein [36]. Newly discovered enhancer, namely K-M enhancer, increases MGMT expression thus inducing TMZ resistance despite of the hypermethylated MRMT promoter [37]. Therefore, the combination of TMZ and K-M enhancer inhibitors could be a potent treatment modality. Besides, Frenel et al. proved that the combination of folic acid, TMZ and radiotherapy in the treatment of unmethylated MGMT patients was feasible, suggesting the prospect of inducing MGMT methylation in GBM therapy (NCT01700569) [38].
Tyrosine kinase receptor
Epidermal growth factor receptor (EGFR)
Two measures are usually considered for treatment of GBM with EGFR as the target: one is to use EGFR inhibitors, and the other is to use antibodies, vaccines, CAR-T and other therapies to limit the content of EGFR (Fig. 1). EGFR is one of the most common oncogenic mutation sites in IDH-WT GBM [10], relevant to proliferation, migration and escape from apoptosis of tumor cells [39]. EGFR mutations occur in about 50% of all GBM samples, of which more than 40% are gene amplification, and the rest include gene mutations, rearrangements, splicing site changes, etc. [10, 40,41,42,43]. The most common gene mutation of EGFR is EGFRvIII (deletion of exons 2–7) [10], as a potential marker of treatment for GBM.
EGFR inhibitors, Gefitinib and Dacomitinib, are not so effective in the treatment of EGFR-amplification GBM patients (NCT01520870, NCT02447419) [44, 45], which is conjectured to be related to the blockage of blood–brain barrier (BBB). Osimertinib, as the third generation of inhibitor targeting EGFR in non-small-cell lung cancer (NSCLC), with better ability in BBB penetration, needs to be further verified before clinical application [46]. Recently, Osimertinib could not only inhibit EGFR-negative glioblastoma patient-derived xenograft (PDX), possibly via regulation of MAPK pathway [47], but also inhibit transcription factor EGFR-TAZ [48], providing a novel insight for drug reuse of EGFR-targeted inhibitors.
Antibodies of EGFR mostly failed in trials out of expectation [49, 50]. However, Nimotuzumab was more effective with patients carrying activated akt/mTOR [51]. Depatuxizumab (formerly ABT-806) showed limited efficacy, but Depatuxizumab mafodotin (formerly ABT-414), an antibody–drug conjugate using EGFR antibody as receptor-direction, seemed to be effective in recurrent GBM (rGBM) after standard treatment of TMZ [52, 53], but ineffective in newly-diagnosed GBM (NCT02573324) [54]. Novel methods are proposed to overcome the problem of BBB blockage with their feasibility to be verified before clinical application [55, 56]. Vaccination Rindopepimut combined with TMZ in rGBM patients carrying EGFR-VIII is relatively active (originally NCT00458601) [57], but it failed to present effectiveness in a phase III trial (NCT01480479) [58]. CAR-T therapy is still under phase I trial and demonstrates expected effect (NCT02209376) [59, 60].
PI3K/AKT/mTOR pathway
PI3K/mTOR is one of the most common mutation pathways in patients with IDH-WT GBM [10]. Activation of PI3K in GBM is mainly due to the mutation of phosphatase and tensin homolog on chromosome ten (PTEN) [61, 62]. Early in 2005, it was proved that the mTOR inhibitor temsirolimus was inactive as a single drug in rGBM [63]. A recent phase I clinical trial exploring the combined Temsirolimus and AKT inhibitor perifosine demonstrated disappointing results, but it was observed that patients had higher tolerance to Temsirolimus, which was speculated to be related to the use of corticosteroids in the experiment (NCT01051557) [64]. As a new PI3K pan-inhibitor, Buparlisib was also proved to be ineffective against rGBM in experiments, either as a single dose [65] or combined with carboplatin or Lomustine (NCT01339052, NCT01934361) [66]. Further research for an oral PI3K inhibitor, Bevacizumab with BKM120, was terminated due to low tolerance in patients (NCT01349660) [67]. Combination of Perifosine and Temsirolimus for rGBM is under test in an ongoing trial (NCT02238496).
The mTOR inhibitor Everolimus was not effective in patients with newly diagnosed MGMT promoter-unmethylated GBM, either used alone (NCT01019434) [68] or combined with radiotherapy or TMZ (NCT00553150) [69]. A recent phase I trial of Buparlisib combined with TMZ and radiotherapy in newly diagnosed GBM patients was interrupted due to adverse events and dose-limiting toxicities of Buparlisib, suggesting the deficiency of this combined treatment (NCT01473901) [70].
In short, PI3K pathway as a therapy target in GBM is often ineffective and followed with relatively low patient tolerance, which may be related to the complex molecular regulation of PI3K/AKT/mTOR. Some trials have shown that the tolerance of inhibitors will increase significantly under certain conditions that have not yet been explored, and it is possible to find ways to help patients tolerate higher doses in the future to ensure effects of targeted therapy. In addition, the current effect of PI3K inhibitors combined with other treatments is not ideal, which more combination strategies should be explored in the future.
MET
MET gene encodes hepatocyte growth factor receptor (also known as scatter factor), which is thought to play an important role in the migration, invasion, drug resistance and recurrence of glioma cells, especially in radiation resistance, inhibition of angiogenesis and hypoxia [71, 72]. About 30% GBM patients are charactered by MET hyper-expression [73]. The use of AMG102 (Rilotumumab) antibody alone had no effect on inhibiting the progression of GBM [74]. A clinical trial of combined antibody Onartuzumab and antivascular drugs confirmed that there was no significant benefit for rGBM patients but those with high expression of HGF (NCT01632228) [75]. Cabozantinib, an inhibitor of MET, whether in combination with antiangiogenic drugs or not, was mildly active in patients with rGBM (NCT00704288) [76, 77]. Combined Buparlisib and MET inhibitor Capmatinib failed to prolong the survival of PTEN-loss recurrence GBM patients (NCT01870726) [78]. Since mutations in c-MET often lead to drug resistance in GBM patients, influencing the efficacy of PI3K targeted therapy, the combination of MET inhibitors and PI3K inhibitors can be considered in follow-up trials.
Fibroblast growth factor receptor (FGFR)
FGFR is widely expressed in GBM, but its therapeutic value may be limited to a small number of patients with FGFR-TACC fusion [79]. One case with stable disease and one case with partial response were reported in 2 FGFR3-TACC3-positive rGBM patients treated with oral pan-FGFR kinase inhibitor Erdafitinib [80]. Similarly, only partial response in FGFR3-TACC3 positive GBM patients treated with this inhibitor was reported in another phase I trial (NCT01703481) [81]. In recent trials, the use of Dovitinib, an oral inhibitor of FGFR and VEGFR, whether combined with anti-vascular therapy or not, was ineffective in prolonging survival in patients (NCT01753713) [82].
BRAF mutation
BRAF, a member of Raf kinase family, participates in activation of Mek/Erk signaling pathway and promotes cell proliferation [83]. Mutations of BRAF, particularly BRAFV600E missense mutation, are observed in multiple types of cancer and have been proved to be a reliable target [84,85,86,87]. Although BRAF mutation was observed in several glioma subtypes, it was rare in high grade gliomas including GBM [88]. The low mutation rate of BRAF in GBM limited the therapeutic effect [89,90,91,92].
Neurotrophic tyrosine receptor kinases (NTRK)
NTRK is encoded by three different genes, namely NTRK1, NTRK2 and NTRK3. The genomic rearrangement of NTRK gene leads to gene fusion [93], which may trigger the activation of carcinogenic TRK signaling pathway. The incidence of NTRK gene fusion seems to be quite rare in glioblastoma [94]. An adult GBM patient with IDH-WT and NTRK2 rearrangement was treated with Larotrectinib and Entrectinib successively, showed a robust but temporary response. Re-biopsy after disease progression showed that the tumor cells carrying rearranged NTRK2 were eliminated and the tumor cells with amplification of PDGFRA survived [95]. Larotrectinib was also used in a female patient with infantile GBM, and the curative effect was significant [96]. Entrectinib was also effective in the treatment of infantile GBM [97], indicating the potential therapeutic value and diagnostic value of NTRK fusion for GBM.
Cell cycle control and apoptosis regulating pathways
The retinoblastoma (pRB) pathway
In most IDH wild-type GBM, the cell cycle control of pRB pathway is alternated due to homozygous deletion of CDKN2A/B, amplification of CDK4/6, and change of RB1 gene (Fig. 2). Challenging abstacles appears when applying pRB pathway as clinical target, due to the extensive existence of this pathway in normal cells [98]. CDK4/6 inhibitor Palbociclib for GBM was disappointing in a phase II trial (NCT01227434) [99]. Ribociclib as a single agent was also ineffective (NCT02933736) [100, 101]. SPH3643, as a newly-discovered inhibitor of CDK4/6 has not been tested in clinical trials, but its BBB permeability may indicate better clinical benefits than Palbpciclib [102]. TG02 is a multi-CDK inhibitor mainly targeting CDK9 rather than CDK4/6, currently being tested in clinical trials for rGBM and newly diagnosed GBM (NCT02942264, NCT03224104).
The p53 pathway
TP53, as a tumor suppressor, has been deeply elucidated in GBM. Given the key function of p53 in blocking cells in G0/1 and in inducing apoptosis in response to genotoxic stress [103, 104], how to restore the function of p53 has been widely studied. Although drugs for promoting the refolding of mutant proteins into wild-type conformations have not been successful, continuous efforts have been put in inhibiting the negative regulatory proteins of p53, MDM2 and MDM4, which aims at neutralizing defective MDM2 and MDM4 produced by amplification of MDM2 and MDM4 gene in GBM patients [105, 106]. The MDM2 inhibitor AMG 232 suppressed tumor progression in the course of the trial (NCT01723020) [107]. AZD1775, an inhibitor of Wee1 kinase, showed better brain tumor penetration but further trials are needed to prove its curative effect [108].
TERT promoter mutation
TERT promoter mutation is one of the most common molecular markers in IDH wild-type GBM [10, 109]. Two hot spots of TERT mutation produce new E-twenty-six transcription factors binding sites and increase TERT transcription, thus increasing TERT activity [110].
It was previously thought that the effect of MGMT promoter methylation on chemotherapy sensitivity and prognosis may be different in tumors with and without telomerase reverse transcriptase (TERT) promoter mutation [111]. However, recent studies have found that when patients with MGMT promoter methylation are treated with standard TMZ chemotherapy, TERT is likely to exert a positive effect [112].
TERT promoter mutation has not yet become the main pharmacological target for tumor therapy. Tubulin polymerization inhibitor Eribulin exerts TERT inhibitory activity in GBM model, which proves the rationality of its clinical application [113]. The mutation of TERT promoter creates a binding site for GABP transcription factor complex. Down-regulation of GABPB1L, an isomer of a subunit of GABP, could significantly improve the survival rates when combined with TMZ in GBM model, shedding light on the significance of finding its inhibitor [114]. Bases editing by CRISPR/Cas9 could correct TERT mutation and reduce the binding activity of ETS transcription factors to slow down tumor growth [115], but the prospect of gene therapy in clinic is still open to question.
Proteasome
As the vital mediator of intracellular degradation of useless or/and toxic proteins [116], proteasome promotes apoptosis by regulating p53 and ER stress, which critically regulates cell cycle and affects drug resistance of tumor cells [117]. Currently, bortezomib, Ixazomib, and Marizomib have been the clinically approved proteasome inhibitors.
Bortezomib combined with Vorinostat, a histone deacetylase inhibitor, was ineffective in rGBM (NCT00641706) [118], while Bortezomib combined with standard radiotherapy was well-tolerated and presented promising survival rates (NCT00998010) [119]. Marizomib combined with TMZ is ongoing a phase III trial (NCT03345095), and Marizomib combined with Bevacizumab is ongoing a phase I/II trial (NCT02330562). Ixazomib has distinct permeability to tumor tissues preclinically with its efficacy trials to be further verified [120].
Disulfiram not only restricts the proteasome from peripheral blood cells to a certain extent, but also has favorable BBB penetration ability and better drug resistance to exert its anti-tumor effects [121] in newly-diagnosed GBM and rGBM models. However, a phase II trial reported that Disulfiram was limited in sensitizing TMZ (NCT03034135) [122].
Microenvironmental targets—Angiogenesis
Vascular Endothelial Growth Factor (VEGF)
GBM is characterized by the abnormality in vascular proliferation (Fig. 3). VEGF is highly expressed in glioblastoma and promotes the abnormal proliferation of tumor blood vessels. VEGFR1 and VEGFR2 signaling pathways are suggested as the critical factor of tumor survival in GBM [123]. Hypothetically, vascular normalization could increase tumor blood perfusion and help improve patient survival (NCT00035656) [124].
Bevacizumab, a humanized monoclonal antibody against the VEGF-A ligand, binds to endothelial cells and inhibits angiogenesis [125]. In Phase II clinical non-controlled trials, Bevacizumab presents significant biological activity, anti-glioma activity, high radiation response rate (RR), high overall survival (OS) and 6 months PFS(PFS-6) in newly diagnosed and rGBM [126,127,128]. In Phase III clinical trials, Bevacizumab could also significantly improve PFS (NCT00884741) [129]. However, it did not improve OS even with the adjuvant chemoradiotherapy or lomustine and was reported with high frequency of adverse events (NCT00943826, NCT01290939) [23, 129, 130], and the quality of life raised, declined or remained the same which reached opposite results in different trials [129, 130]. IDH1-wildtype GBM patients exhibited prolonged OS after receiving Bevacizumab therapy (NCT00943826) [131]. Bevacizumab could develop drug resistance within months. The efficacy of multi-kinase inhibitor Ponatinib in GBM patients is very limited in Bevacizumab-refractory GBM (NCT02478164) [132]. Also, patients who progress on VEGF R-TKi with Bevacizumab only benefit modestly [133]. The latest research showed that the response to Bevacizumab in some patients might correlate with antibody dependent cytotoxicity(ADCC) [134].
Bevacizumab plus Temozolomide exhibits great efficacy and tolerance [135]. In some trials, Bevacizumab plus Trebananib had less effect than single agent (NCT01609790, NCT01609790) [136, 137]. Bevacizumab plus erlotinib or metronomic Etoposide had a similar effect to Bevacizumab monotherapy and Etoposide showed a greater toxicity (NCT00671970, NCT00612430) [138, 139]. The efficacy of small dose Bevacizumab plus Lomustine was not improved [140]. Bevacizumab combined with CCNU radiotherapy significantly improved PFS in IGS-18 GBM [141]. Although Bevacizumab plus Rilotumumab showed 3–4 months improvement in median OS over single agents in rGBM, PFS was not increased (NCT01113398) [142]. Administration of concurrent Bevacizumab and Erlotinib presented significantly higher RR and PFS-6 [143].
Other VEGF inhibitor like Cediranib, a pan-VEGF receptor tyrosine kinase inhibitor, showed significant efficacy and PFS-6 in phase II clinical trial of rGBM (NCT00305656) [144]. In newly-diagnosed GBM patients, Cediranib promoted the blood perfusion and prolonged the OS (NCT00662506) [145]. Cediranib also declined the tumor-associated angiogenic brain edema (NCT00254943) [146]. However, it failed to prolong the PFS in phase III clinical trial of rGBM (NCT00777153) [147].
Pazopanib and Tivozanib have in situ bioactivity and similar tolerance to other anti-VEGF drugs, but they failed to prolong PFS and OS in phase II trials ((NCT00459381, NCT01846871, NCT00350727)) [148,149,150]. Phase I trial of Aflibercept showed great toxic side effect to rGBM while the efficacy is very limited [151]. A phase II trial suggested that Aflibercept binds to VEGF with a greater affinity than Bevacizumab, whereas, without greater efficacy [152]. Axitinib, a tyrosine kinase inhibitor (TKI) against VEGFR-1, 2 and 3, could be a potential combination partner with immunotherapy (NCT01562197) [153]. Other inhibitors like Aflibercept could also down-regulate the activity of VEGF and needs to be further studied (NCT00369590) [154].
Integrin
Integrins are a family of 24 heterodimeric cell surface receptors that participate in signal transduction involved in many cellular processes. They also mediate cellular communication within the extracellular matrix during adhesion, motility, migration, invasion and angiogenesis. Integrins αvβ3 and αvβ5 are highly expressed in endothelial cells and identified as preclinical therapeutic targets in GBM [155, 156].
Cilengitide is a selective integrin inhibitor targeting αvβ3 and αvβ5, which its combination with Cediranib had a great tolerance to rGBM patients in a phase I trial (NCT00979862) [157]. In a phase II trial, Cilengitide has a moderate efficacy which could be transported and accumulated in rGBM cell through binding with avβ3 and αvβ5 [158, 159]. TMZ/RT-TMZ plus Cilengitide with great tolerance and efficacy could not improve invasiveness or recurrent rate of newly-diagnosed GBM (NCT00813943) [160, 161]. In GBM patients with MGMT promoter methylation, Cilengitide had good performance as adjuvant administration with standard treatment (NCT00689221, NCT00689221) [162, 163]. But Cilengitide failed to reach the primary endpoint in non- methylated patients (NCT01124240) [164]. In phase I and II trials, Cilengitide was proved incapable of being the monotherapy in children with GBM [165, 166]. A phase III trial showed limitation on the efficacy of Cilengitide (NCT00689221) [167]. Although Cilengitide has not exhibited remarkable potential as monotherapy, integrins remain to be the important target.
Transforming growth factor (TGF)-β
The TGF-β protein family has complex functions in a wide range of regulatory pathways [168, 169], among which TGFβ2 is a T cell suppressor in tumor microenvironment of GBM [170] and is expressed in about 90% of GBM tumor cells. However, although TGFβ1/2 inhibitors have been used in treatment of other cancers, they are still difficult to be used as GBM clinical treatment targets.
As a TGF-β receptor(R)1 kinase inhibitor, Galunisertib was ineffective with combined Lumostine (NCT01582269) [171]. TGF-β2-specific antisense oligonucleotides, Trabedersen was effective in particular to patients whose KPS are above 80% and age are under 55, but generally the therapy efficacy was far from expectations (NCT00431561) [172]. Similarly, antisense oligonucleotides, namely ISTH1047 and ISTH0047, exhibit anti-tumor properties and can be further tested in clinical trials [173].
Gene therapy focusing on hematopoietic stem cell (HSC) that expresses TGF-β blocking peptides enhanced the sensitivity of GBM to chemotherapy in animal model [174]. Given that, further clinical treatment can be considered. Recent trials have also pointed out that TGF-β is related to TMZ resistance and MGMT expression [175]. Therefore, the combination of TMZ and TGF-β inhibitors are promising.
Immunotherapy
Programmed cell death protein (PD)-1
One strategy of cancer immunotherapy is to prevent the interaction between PD-1 ligand (PD-L1) on tumor cells or host cells and PD-1 on T cells (Fig. 4). Pembrolizumab, an antibody that blocks PD-1, has poor efficacy in previous treatments of GBM [176], except in cases with specific mismatch repair defects [177,178,179]. Thus, mismatch repair defects are expected to be a novel biomarker of targeting PD-1/PD-L1, with classic markers as TMB, tumor infiltrating lymphocyte (TIL) and microsatellite instability (MSI) [180,181,182]. However, standard therapy with neoadjuvant Pembrolizumab demonstrates significant survival benefits [183].
In a randomized clinical trial, Nivolumab combined with Bevacizumab [184] and Nivolumab combined with chemoradiotherapy in newly-diagnosed GBM patients with MGMT promoter unmethylation (CHECKMATE 498, NCT02617589) were both ineffective. Preclinic animal models confirmed that PD-1 blockade could reverse peripheral T cell exhaustion induced by TMZ but could not affect tumor infiltrating lymphocytes [185], which partly accounts for its ineffectiveness. The phase II trial of Nivolumab as neoadjuvant therapy also failed to show clinical benefits (NCT02550249) [186].
Lymphocyte activation gene 3 (LAG-3)
LAG-3, mainly found on activated immune cells [187, 188], leads to immune escape of tumor cells similar to that of PD-1 [189]. In tumor tissues, LAG-3 is usually expressed in T cells with lost functions, called exhausted T cells. Thus, inhibitor of LAG-3 become an attractive immune-modulating agent alone or in combination with other immune checkpoint inhibitors [190, 191].
In GBM, LAG-3 rather than PD-1 is co-expressed with CD8A [192], indicating that LAG-3 targeted therapy in GBM with abundant CD8 + T cells infiltration may be promising. A phase I trial (NCT02658981) of the LAG-3 antibody BMS-986016 is ongoing.
Cytotoxic T-lymphocyte–associated antigen 4 (CTLA-4)
CTLA-4 shares common receptors CD80/CD86 with CD28, and binding of CTLA-4 to those receptors are antagonistic to T cell activation and proliferation [193, 194]. CTLA-4 antibody Ipilimumab is the first clinically approved immune checkpoint inhibitor, in addition to Tremelimumab, etc. [182].
Combined anti-CTLA-4 and anti-PD-1/PD-L1 therapy is active in multiple kinds of cancers. Intracerebral injection of Ipilimumab plus Nivolumab is safe and feasible, and has a certain effect for rGBM (NCT03233152) [195]. Other trials for combined anti-PD-I and anti-CTLA-4 therapy are ongoing (NCT04323046, NCT04606316). The effectiveness of CTLA-4/PD-1/IDO triple therapy is also confirmed in animal model [196], further ensuring the prospect of combined immune therapy. The clinical benefits of Ipilimumab combined with standard chemoradiotherapy are observed in a phase II clinical trial (ISRCTN84434175) [197]. Intratumorally injection of IL-12 combined with systemic administration of CTLA-4 antibody is also effective in animal model [198], providing the robust basis for further clinical research.
Vaccination aimed at enhancing anti-glioma immunity by injecting autologous glioma cells mixed with GM-K562 cells that are inactivated via irradiation has been proved safety and modestly feasible [199]. Meanwhile, CAR-T therapy combined with Ipilimumab for the treatment of rGBM is also in the preliminary stage (NCT04003649).
CD73
CD73, an extracellular nucleotidase, catalyzes the production of adenosine from extracellular AMP [200], which exerts an immunosuppressive effect on GBM and induces drug resistance of vincristine presumedly via regulating multiple drug associated protein 1 (Mrp1) [201, 202].
Nasal administration of cationic nanoemulsion mixed with CD73-siRNA presented promising anti-CD73 effect in GBM model [203]. This anti-CD73 effect promotes, subsequently, alteration in tumor microenvironment and suppressing the tumor proliferation [204]. Whereas the feasibility of cationic nanoemulsion to clinic is under studied. Anti-PD-1 combined with anti-CTLA-4 showed a favorable effect in CD73-deficient GBM model [205]. Currently, there are still few clinical trials of CD73 inhibitors with GBM. Although CD73 inhibitor AB680 is discovered, it has not been used in treatment of GBM [206].
CD161
CD161, as the marker of GBM tumor infiltrating lymphocytes, is widely expressed on the plasma membrane surface of NK cells, CD8 + and CD4 + T cells [207], binding to the ligand CLEC2/Lectin like transcript-1(LLT1) mainly expressed in GBM myeloid cells [208]. Previous studies have confirmed that CD161 directly interacts with intracellular acid sphingomyelinase to regulate Akt signaling pathway and then inhibits activity of NK cell. Notably, CD161 simultaneously exerts the property of stimulating immunity and inhibiting immunity: when CD161 binds to LLT1 and is co-stimulated by CD3, the expression of TNF-α in T cells is promoted, when CD161 is stimulated on CD8 T cells alone, the expression of TNF-α in T cells is inhibited [209]. CD161 has been regarded as a critical regulator for immunosuppression in GBM [210]. So far, inhibition of CD161 is proved with enhanced anti-tumor effect of T cells in preclinic model.
IDO1
Indoleamine 2,3-dioxygenase 1 (IDO1), an Trp dioxygenase extensively detected in mammalian tissues except the liver [211,210,213], usually degrades Trp into L- kynurenine that subsequently activates aryl hydrocarbon receptor (AhR) via the Kyn–AhR–AQP4 signaling pathway, which promotes cell motility and increases malignancy of gliomas. Furthermore, IDO1 is regarded as a significant mediator in immunotolerance and immunosuppression of cancer via its non-enzyme activity, though the potential mechanisms remains to be fully elucidated [214]. Thus IDO1 is becoming an attractive target of immunotherapy in grade IV gliomas, especially GBM.
1-methyl-l-tryptophan (1-MT, also known as Indoximod), the inhibitor of IDO1, was effective with combined TMZ in animal models of malignant gliomas (exclusively corresponding to WHO grade IV gliomas) [215], hence several phase I/II trails exploring the safety and efficacy of combined 1-MT and chemotherapy in both pediatric and adult patients with gliomas are ongoing. (NCT02052648, NCT02502708, NCT04049669).
Given that some trials indicated inactivity of IDO1 inhibitor as a single agent, combination of IDO1 inhibitor and PD-1/PD-L1, CTLA-4 blockade [216], or other treatments such as anti-angiogenesis is proposed. Also, Erik Ladomersky et al. discovered that older patients with GBM experienced an age-related immunosuppression hypothetically resulted from the increase of IDO accumulation in elderly brain [217]. Since immunosuppression could be induced by Trp depletion and Kyn activation that are initiated by three enzymes namely IDO1, IDO2 and TDO while IDO1 and TDO are more vital than IDO2 in pathologic grade of gliomas [214], the application of IDO1 and TDO inhibitors simultaneously, excluding IDO2, is advised. Additionally, according to the fact that compared to the physiological situation systemic Kyn decreases while intratumoral Kyn increases in GBM patients, exploration on Kyn pathway modulation is still in its infancy [218]. Nevertheless, recent study has found that IDO induces the expression of complement factor H (CFH) and its isoform, factor H like protein 1 (FHL-1) independent of its enzymatic activity, which contributes to poor survival of GBM patients [219]. This finding would help explore the novel targets of IDO inhibition.
Hepatitis A virus cellular receptor 2 (HAVCR2)
HAVCR2 is a specific cell surface protein encoded by homonymous gene. It is also named T cell immunoglobulin and mucin-domain containing-3 (TIM3) [220] that belongs to immunoglobulin superfamily. TIM3 participates in regulation of macrophage, induction of immunological tolerance, inhibition of Th1-mediated auto- and alloimmune responses, which becomes a promising target for immunotherapy.
Generally, TIM3 interacts with HLA-B-associated transcript 3 (BAT3) and subsequently recruits kinase LCK to maintain T cell activation. However, Galectin 9, mainly found in tumor cells and antigen-presenting cells, binds to TIM3 that phosphorylates intracellular domain of TIM3 and recruits kinase FYN, contributing to apoptotic and anergic T cells. So far, various ligands of TIM3 have been discovered, such as carcinoembryonic antigen-related cell adhesion molecule 1 (CEACAM1), phosphatidylserine (PtdSer), and high mobility group protein B1 (HMGB1) [221].
Almost all anti-TIM3 antibodies presenting antitumor activity are designed to interfere with the binding between TIM3 and CEACAM1, PtdSer [222]. In particular, TIM3 is widely expressed in GBM and IDH-WT gliomas, regulating inflammatory activation especially after anti-PD-1 therapy [223, 224]. Thus, combined anti-TIM3 inhibitor and other immunotherapy is getting promising. Combination of anti-TIM3 therapy, anti-PD-1 therapy, and radiotherapy in animal models has reported promising efficacy [225]. Besides, MBG-453 is an antibody against TIM3 in an ongoing phase I trial (NCT03961971).
V-set domain containing T cell activation inhibitor 1 (VTCN1)
Commonly known as B7-H4, VTCN1 is a highly revolutionarily conserved type-I transmembrane protein [226]. Interaction of B7-H4 with the unknown receptors has the capability of negatively regulating activity of T cells. Moreover, VTCN1 not only inhibits production of cytokines but also arrests cell cycle in G0/Gi phase [227]. B7-H4 is found in a wide range of lymphocytes, including NK cells, T cells, and cancer cells, including partial glioma cells [228,227,230]
Previous study has declared that patient with high B7-H4 expression specifically experienced deficiency in tumor-infiltrating lymphocytes, suggesting its critical role in immunosuppression [230]. However, antibodies or inhibitors against B7-H4 remain to be developed for gliomas.
V-domain immunoglobulin suppressor of T cell activation (VISTA)
VISTA has been initially recognized for its significant role in immunosuppression [231]. VISTA complicatedly and conversely functions as both ligand and receptor in the negative or positive regulation of cancer immunity. Notably, several recent studies using anti-VISTA methods, VISTA-deficient models or computer simulation have confirmed its suppressive role and upregulation of immune response [232, 233].
One of the known ligands of VITSA, the immunoglobulin superfamily 11 gene (IgSF11), is found with elevated expression particularly in high grade glioma (also named HGG) and correlates with worse prognosis [234], suggesting the potential prognostic value of VISTA and IgSF11. However, clinical trials on targeting VISTA alone or as adjuvant therapy with gliomas are still scarce to date。
CD27/CD70
As a member of the tumor necrosis factor receptor (TNFR) superfamily widely expressed on resting T cells [235], NK cells [236], and memory B cells [237], CD27 interacts with its ligand CD70 to stimulate T cell activity [238]. Nevertheless, early finding also showed that CD27 correlates with apoptosis of CD27-bearing cells [239], indicating its two-sided role in regulating immune response [240].
CD70 is overexpressed in primary and recurrent glioma cells in contrast to normal tissue and lymphocytes, and is associated with poor survival. Thus, CD70 on tumor cells is proposed to induce T cell (especially CD8 + T cell) exhaustion or apoptosis and activate regulatory T cells (Tregs) to mediate immunosuppression [241,240,241,244]. Since CD27 stimulates T cell activity, and also induces cytotoxicity and then apoptosis of CD27-bearing lymphocytes under pathological cases, the combined CD27 agonist and CD70 inhibitor is promising.
Previous study has shown that agonist anti-CD27 mAbis capable of recruiting CD8 + T cells and promoting anti-tumor response in animal model [245]. CD27 agonist, Varlilumab, has been tested in combination with anti-PD-1 therapy in a phase I/II trial (NCT02335918), with the results to be reported. Other trials exploring anti-CD27 inhibitor as neoadjuvant or in combination with other immunotherapy options are ongoing (NCT02924038, NCT03688178). CAR-T cells target at CD70 alone or at both CD70 and B7-H3 present promising perspective, however not applied to clinical trials hitherto [244, 246].
B and T lymphocyte attenuator (BTLA)
As a member of CD28 superfamily, BTLA shares a similar molecule structure with PD-1 and CTLA-4. Functionally, as the only identified ligand of BTLA, herpes virus entry mediator (HVEM) [247, 248] interacts with BTLA to negatively regulate activity and proliferation of T cells.
It has been confirmed that BTLA influences T cell signaling through SHP1/2, similar to that of PD-1. But compared with PD-1 that prefers to recruit SHP2, BTLA mainly recruits SHP1. Surprisingly, under SHP1/2 deficient condition, BTLA still presents inhibitory effect of cell proliferation and cytokine production in primary T cells. Thus, combination of PD-1 blockade and BTLA blockade is promising and attractive, with some potent signaling pathways by which BTLA and PD-1 inhibit activity of T cell remain to be further elucidated [249, 250]. Preclinic model proved that anti-BTLA and anti-PD-1 immunotherapy mainly promotes the activation of CD4 + T cells, CD8 + T cells and the secretion of IFN-γ that correlates with favorable survival [251]. However, there is still a long way to go before this combination therapy could be applied clinically.
CD39
CD39 predicts worse survival for GBM and anaplastic astrocytoma patients [252]. As an ecto-enzyme hydrolyzing extracellular ATP (eATP) into AMP, CD39 and CD73 sequentially convert eATP to immunosuppressive adenosine (ADO) in the tumor microenvironment (TME), as one portion of the ATP–adenosine axis [253]. In the TME, eATP is released and accumulated due to hypoxia, subsequentially to stimulate inflammation activity or be converted to ADO by CD39 and CD73. ADO could be also generated by sequential catabolism of NAD + by CD38-CD203a-CD73 [253], and by alkaline phosphatase independently [254]. High level of extracellular ADO is beneficial to suppress immune response via ADO binding to low-affinity adenosine receptor namely A2A and A2B that are broadly expressed on lymphocytes and myeloid cells [255]. CD73 is proved to be preferentially expressed on glioma cells and has the synergetic effect with CD39 expressed on tumor-infiltration T cells on inducing immunosuppression [256, 257].
Researchers have revealed that CD39 expressed on tumor-associated macrophage could contribute to dysfunction of CD8 + T cell [258]. However, inhibitor for the adenosine pathway failed in preclinic model, with presumed explanation such as irreversible exhaustion of T cells [257], or different affinity and distribution of adenosine receptors on glioma cells or lymphocytes. Given that, the specific mechanism involved in the modulation of ADO in tumor microenvironment of glioma needs to be further revealed.
CD276
CD276, also known as B7-H3, is one of the B7 ligand family. CD276 is believed to provide a negative costimulatory signal both on donor T cells and host cells during transplantation [259, 260]. CD276 expressed on antigen-presenting cells also conveys an immunosuppression signal. Besides, CD276 is also detected on DCs, NK cells and epithelial cells.
CD276 is extensively overexpressed on tumor cells and tumor vasculature [261, 262], and serves as a hazardous marker in GBM as it mediates immunosuppression via inhibiting activity of NK cells, inducing invasion and differentiation of tumor cells [263,262,265]. Considering its relatively low expression in normal tissues, bringing potential safety and presumed tolerance in patients, thus CD276/B7-H3 becomes an attractive target for immunotherapy.
CAR-T therapy targeting CD276 both in vitro and in xenograft model demonstrated promising survival benefits [266]. Using antibody–drug conjugates to ablate CD276 + glioma cells simultaneously impaired tumor vescular [262], indicating a novel insight on the combination of anti-CD276 with anti-angiogenesis, which was supported when CD276 was confirmed to positively be related with VEGFA and MMP2 [267].
The immunotherapy value of CD276 has not been fully determined partially due to the un-defined isoforms, intracellular domain and ligands of CD276 [268]. Although such a type I transmembrane protein has almost 90% homologous amino acid sequence between human and murine [269], different and opposing outcomes were sometimes reported in murine tumor model compared with human tumor model [270], making the clinical trials in gliomas challenging.
CD47
CD47, also called integrin-associated protein (IAP) or MER6 [271], is ubiquitously expressed in astrocytoma cells as different isoforms [272, 273]. CD47 promotes GBM invasion and progression [274, 275], and also delivers a special “don’t eat me” signal by binding to signal-regulatory protein α (SIRPα or CD172a) on macrophages or DCs. Thus, anti-CD47 is suggested efficacious by promoting immune response ablating tumor cells via macrophage and/or DCs [276, 277], even through microglia [278].
Apart from integrins and SIRPγ (CD172b) [279], expression of SIRPα is also observed in brain tissues [280], astrocytomas [281]. SIRPα, also called CD172a, is vital to the “CD47-SIRPα axis”, which is more significant since SIRPα is only expressed on certain cells including myeloid cells and neurons leading to relatively high safety and efficacy.
In vitro experiment and murine model proved that anti-CD47 induces the M1-polarization of macrophages that promotes an immune active tumor microenvironment [282]. Hu5F9-G4, a humanized anti-CD47 antibody, manifested efficacy both in pediatric GBM and diffuse intrinsic pontine glioma cells [283]. Anti-CD47 was also proved to increase tumor-infiltrating CD8 + T cells that suppressed glioma cells and cancer stem cells [284]. SIRPα-Fc blocks CD47-SIRPα impressively, also triggering autophagy of glioma cells thus promoting survival in GBM models, and the prognosis is better with chloroquine [285]. Given that TMZ induced ER stress response in GBM then beneficial to phagocytosis, studies found that combination of TMZ and anti-CD47 therapy was with drastically improved efficacy in GBM model [286]. Since SIRPα polymorphism has become the obstacle to anti-CD47 therapy, other studies are urgently needed to elucidate the entire mechanism of CD47-SIRPα axis.
Cytokine therapy
Cytokines, produced by the immune microenvironment, could both be employed by tumors to suppress immune response and be employed by immune system to induce immune response [287]. Among the multiple cytokines, interleukins and interferons have been most widely used in cancer therapy with high efficiency.
IL-2 was first studied in glioma patients in 1986 [288], which the combined IL-2 and tumor vaccination was observed with remarkable side effects [289]. Notably, tumor responses were detected in 50% rGBM patients receiving the combined therapy of IL-2-encoding genes and herpes simplex virus type 1 thymidine kinase (HSV-TK) genes. In a phase I trial, HGG patients receiving the glioma cell vaccine admixed with IL-4-encoding genes transfected fibroblasts showed favorable clinical responses [290]. The safety of recombinant protein IL-13-PE38QQR was confirmed in a phase I trial [291]. In a subsequent phase III trial, IL-13-PE38QQR significantly increased PFS but not OS in rGBM patients (NCT00076986) [292].
In two phase II trials, TMZ with combined IFN-α exhibited improved efficacy in rGBM patients [293]. IFN-β also enhanced sensitivity to TMZ by inhibiting MGMT transcription preclinically [294, 295]. Besides, the combined IFN-β and standard chemoradiotherapy prolonged the survival of GBM patients in a phase I trial [296]. However, the combined IFN-γ and standard chemoradiotherapy failed to demonstrate clinical benefits in GBM patients [297, 298].
TAM therapy
Tumor-associated macrophages (TAMs), a significant component of tumor microenvironment, in glioma, are commonly defined as macrophages of peripheral origin and microglia, to regulate immune response and promote tumor progression [299, 300]. A recent study demonstrated that despite of inducing T cell and DC activation, neoadjuvant PD-1 blockade failed to overcome the immunosuppressive TAMs in rGBM, indicating the important role of TAM in resistance to treatment [301].
Previous study revealed immunosuppressive M2 macrophages populating TAM in glioma tissues, are associated with histological grade of glioma. Researchers also suggested macrophage colony-stimulating factor (M-CSF) is vital to shift of microglia/macrophage to M2 subtype, inducing tumor proliferation [302, 303]. Thus BLZ945, a CSF inhibitor, has been tested to target TAMs in mouse models of GBM with satisfactory survival with elimination of tumor cells and decrease of M2 in TAM [304]. Pyonteck et al. also pointed out GBM classification (proneural GBM in this case) and TAM phenotype rather than TAM number as a potential biomarker for anti-CSF therapy. Given that combination of PI3K and BLZ495 showed better OS, further clinical trials are needed [305]. PLX3397 is another efficacious CSF inhibitor in GBM models [306], however, the result of a phase II trial showed PLX3397 barely presented therapeutic effect (NCT01349036). Moreover, biomimetic tumor-on-a-chip on GBM have predicted promising outcome of co-targeting M2-TAM combined with anti-PD-1 [307]. In epithelioid GBM (with markers of the BRAF‐V600E and TERT C228T promoter mutations and the absence of IDH1 and IDH2 mutations), CSF-1R is also detected broadly on epithelioid GBM cells and combination of inhibiting BRAF-V600E and BLZ945 reduces cell viabilities [308]. Those recent studies in vitro indicate potential efficacy of targeting TAM with other immunotherapies.
As a lipophilic molecule, antibiotic minocycline could suppress the expression of microglial MMPs and attenuate the invasion of glioma [309], which minocycline could also be safely combined with radiation and bevacizumab [310]. Besides, cyclosporine A displayed efficacy in attenuating the survival and angiogenesis of glioma by inhibiting the infiltration of microglia [311]. Propentofylline was also proved to reduce tumor growth in GBM by directly targeting microglia [312].
Dendritic cell vaccine
DC vaccine (DCV), composed of powerful antigen-presenting cells (APCs), could induce effective immune responses.
In most of the clinical studies on DCVs, autologous tumor lysate and tumor-associated peptides were chosen as the antigen [313]. In two phase I trials (NCT00068510 NCT00612001), autologous tumor lysate (ATL)-pulsed DCV was proved with higher patient eligibility than glioma-associated antigen (GAA) peptide-pulsed DCV [314]. GBM6-AD/DC vaccine was well tolerated and induced immune response in rGBM patients [315](NCT01171469). In a phase I/II trial (NCT00766753), DVC with EphA2, IL-13Rα2, YKL-40, and gp100 as GAAs was also well tolerated and induced potent immune response, contributing to the progression free status in 9 out of 22 glioma patients [316]. In a phase I trial (NCT00576641), DVC with HER2, TRP-2, gp100, MAGE-1, IL-13Rα2, and AIM-2 as antigens significantly prolonged OS and PFS in newly diagnosed GBM patients [317]. In a subsequent phase II trial of the same DCV (NCT01280552), ICT-107, remarkable antitumor activity was observed and ICT-107-treated GBM patients presented improved PFS [318]. Immune responses and clinical benefits of GBM patients receiving DCV were reported in another phase II trial (NCT00576537) [319]. Tumor lysate-pulsed DCV in combination with standard chemoradiotherapy was proved feasible and safe in newly diagnosed GBM patients in two phase II trials (NCT01006044, NCT00323115) [320, 321].
Other studies explored the feasibility of mRNA-transfected DCV. The mRNA-transfected DCV was suggested to be safe, well-tolerated, and significantly prolonged the PFS of GBM patients by 2.9 times (NCT00846456) [322]. In addition, despite the increased Treg proportions, pp65-transfected DCV admixed with GM-CSF and TMZ significantly prolonged the PFS and OS of GBM patients [323].
Low-grade glioma (LGG)
Notably, there was no significant difference in PFS and health-related quality of life of LGG patients receiving radiotherapy alone or temozolomide alone [16, 324]. Correspondingly, the combined radiotherapy and TMZ presented better clinical benefits [325, 326], with certain better prognosis when MGMT promoter methylation exists [327]. Hence, TMZ or radiotherapy as the single therapy for LGG is not recommended. Generally, most of the median overall survival of LGG patients are more than 10 years, only those with diffuse astrocytoma with IDH-WT are around 5 years [14, 328]. As discussed above, WHO grade I glioma, most of which is pilocytic astrocytoma, presents excellent prognosis, with reported 10 years overall survival as high as 100% after standard gross total resection [1, 14]. To WHO grade II glioma, 5 years survival rate of oligodendroglioma reaches 81%, while diffuse astrocytoma only reaches 50%.
Alkylating agent
IDH mutation and consequently increased D-2-hydroxyglutarate level inhibit the expression of some DNA repair genes and anti-apoptotic proteins, such as MGMT, MLH3, RAD21 and SMC4 [329], which downregulates the intracellular glutathione level, apoptosis threshold of LGG and upregulates the sensitivity of LGG to alkylating agent [330] (Fig. 5, Table 2). Similarly, 1p/19q codeletion also correlates with the sensitivity of LGG to alkylating agent [331].
Tyrosine kinase receptor pathway
tyrosine kinase receptor
Erlotinib, a kind of EGFR inhibitor, was mildly effective combined with rapamycin in pediatric LGG (pLGG), and disease stability was observed especially in patients with neurofibromatosis type 1 (NF1) [332]. Erdafitinib, a kind of FGFR inhibitor, was tested in LGG patients in a phase II clinical trial (NCT03210714).
Ras/Mek/Erk pathway
Abnormal activation of Ras/Mek/Erk pathway is the most common and major cause of genetic/epigenetic alterations in LGG. Different LGG subtypes activate this pathway in distinct ways, inducing carcinogenesis and tumor progression. Therefore, inhibiting this pathway is becoming a promising treatment option.
BRAF mutation
BRAF–KIAA1549 fusion and BRAFV600E mutation are the most prevalent genetic alternation in pLGG that are being increasingly focused as the therapeutic targets.
Sorafenib is a multi-kinase inhibitor targeting BRAF, VEGFR, PDGFR, and c-kit, which unexpectedly promotes the proliferation of the tumor cells in low grade astrocytoma [333]. Dabrafenib, a selectively robust inhibitor of BRAFV600 was mildly effective in patients with BRAF V600–mutant pLGG (NCT01677741) [334]. MEK inhibitor, Selumetinib, prolonged the survival of LGG patients (NCT01089101) [335,334,337]. Another inhibitor of MEK, Trametinib, is still being tested in a phase II trial (NCT03363217) [338].
NF1
Neurofibromatosis type 1 is an essential autosomal dominant genetic disorder resulted from loss-of-function mutations in gene neurofibromatosis type 1 that encodes a negative regulator of Ras GTPases under physiological condition [339] and influences the MAPK signaling. The loss-of-function mutation is usually found in anaplastic astrocytoma [340], which NF1 subsequently leads to the diffuse or pilocytic phenotype of pLGG [341]. When treated with carboplatin and vincristine, LGG patients with NF1 experienced prolonged PFS, OS and decreased toxicity [342]. Selumetinib was proved with high effectiveness in pLGG patients with NF1 [336]. A phase II trial exploring double-strain RNA as Toll-like receptor-3 agonist [343] to cure pLGG patients with NF1 is ongoing (NCT04544007). NCT03871257 and NCT04166409 are two simultaneous phase III studies investigating the efficacy of Selumetinib in LGG patients with or without NF1.
PI3K/AKT/mTOR pathway
Everolimus, the mTOR inhibitor, is promising and effective in recurrent/progressive NF1-associated LGG [344]. Nevertheless, for most LGG patients, Everolimus was only associated with a high degree of disease stability and unexpected tumor vascular alternations [345].
IDH-mutation
Compared with children, IDH-mutation is more common in adult LGG. IDH-mutation was first detected from the exome sequencing of GBM [346]. Many follow-up studies proved that patients with IDH-mutation had better prognosis [347]. The mutant IDH1 with a neo-enzymatic activity could produce D-2-hydroxyglutarate whose accumulation in cells facilitates tumor proliferation and growth, increases the ROS level, and promotes hypermethylation in certain DNA sequence. As an inhibitor of IDH1, AG5198 suppressed proliferation of IDH-mutant tumor cells in animal model [348]. Inhibitors of D-2-hydroxyglutaratethat is the production of mutant IDH1 is under explored as a novel treatment for LGG (NCT03343197). Nevertheless, IDH-mutation as a significant early mutation site of glioma has also been proposed to no longer regulates tumor proliferation and invasion after tumor formation [349], So, the prospect of IDH-mutation as a therapeutic target in LGG remains controversial.
PD-1
PD-1 is widely detected among LGG patients, but most of their tumor tissue are positive with PD-1 in a small proportion (< 5%). In some cases, over 50% cells were detected with PD-1 positive [350], which may be related to the methylation of PD-1 promoter in patients with LGG [351]. The expression of PD-1 by immune infiltrating cells in LGG indicates immune escape, while the methylation of PD-1 promoter indicates better prognosis of LGG. Besides, the expression of PD-1 may facilitate adjuvant therapy in patients with radiotherapy tolerance [352].
Conclusion
Due to its relatively lower tumor malignancy, better prognosis, and higher chemotherapy sensitivity brought by IDH-mutation, researches for therapy of LGG are limited. However, some high-risk LGGs incompletely cured by surgical resection are prone to relapse and turn into high-grade gliomas with malignant and aggressive characteristics, which more postoperative adjuvant treatment modalities are necessary. The most common mutation in LGG is the abnormal activation of the Raf/MEK/Erk pathway. Therefore, there are many target inhibitors of this pathway and most of them are very effective. Different LGG subtypes have different genetic/epigenetic alterations, such as amplification and/or rearrangement of MYB/MYBL1, 1p/19q co-deletion, ATRX, and CDKN2A loss. These molecular changes are valuable prognosis signal and/or potential targets for the treatment of LGG. For instance, 1p/19q co-deletion is beneficial for LGG sensitivity to alkylating agent. Additionally, early enough resection combined with chemotherapy or adjuvant around surgery if necessary is gradually advocated instead of MRI every 3–6 months and resection only after tumor progression. As a majority of chemotherapy of LGG are carried out after surgical operation, instant molecular diagnosis is necessary in order to provide prognostic evidence and more precise target therapy. Combination of alkylating agent and inhibitor against Ras/Mek/Erk pathway is worthy of attempting.
For newly diagnosed GBM, the current standard therapy is alkylating agent chemotherapy combined with radiotherapy. Owing to the fact that standard therapy is limited to patients with MGMT promoter hypermethylation and there is no standard therapy for patients with rGBM, more effective target treatment modalities are urgently needed. In recent years, researchers have mostly adopted the scheme of combining therapies targeting different pathways in GBM. However, the therapy efficacy is often unsatisfactory mainly due to the existence of BBB, the complexity of tumor microenvironment, the heterogeneity of tumor tissues, and the tolerance of drugs. Therefore, some potential attempts could be made: 1) developing more effective drug delivery system to cross BBB, such as nanoemulsion for nasal administration or direct intracranial administration, 2) identifying and elucidating more complicated pathways such as PI3K for development of novel drugs 3) more timely and precisely molecular diagnosis of tumor cells [353]. With the publishing of WHO CNS5, gene and protein nomenclature is formally recommended and proved to be more effective and beneficial to clinic. And CNS5 has listed newly-discovered types of gliomas recently, also with a method of grading within types and combining histological and molecular grading, pointing out a legible way to diagnosis and associated treatment. Additionally, studies have confirmed few prognostic or (and) predictive biomarkers remain steady between GBM at the time of diagnosis and relapse because of the evolution of tumor. For instance, loss of expression of MSH6, a mutation of mismatch repair gene, is more frequently found among relapsed GBM than newly diagnosed GBM as a result of standard chemoradiotherapy (Stupp protocol), with mild decrease of MGMT methylation in recurrence as well [8]. Thus combination of molecular diagnostics and precise therapy is supposed to be executed both before and after a defined course of treatment. Furthermore, since Shepherd et al. discovered the elimination of the NTRK2-fusion-harboring cells by Larotrectinib promoted the predominance of untargeted subclone at relapse [95], it is presumed this certain alteration of molecular target might occur much more commonly in recurrence GBM, no matter which treatment we implement, indicating potential obstacles on future glioma therapy. Therefore, targeted therapies are indeed ideal weapons for precision and personalized medicine based on the detection of biomarkers throughout the management of glioma patients.
Moreover, immunotherapy has been an emerging field of tumor therapy. Various immune checkpoints inhibitors have performed well in several cancers. PD-1/PD-L1, CTLA4, TIM3 and other classic checkpoints have made remarkable progress in both pre-clinic and clinical trials. Given the complexity of tumor microenvironment and regulation of immune response, combination therapy is proposed, especially when the combination of anti-PD-1 and anti-CTLA4 presents promising efficacy on rGBM. Classic anti-PD-1 could be combined with various targets such as TIM3 and BTLA. Based on the ATP-ADO axis discussed above, combination of CD39 and CD73 and further exploration on regulation of local ADO concentration are also worth pursuing. Similarly, it is appealing to combine immunotherapy and other targetable pathway. Since CD276/B7-H3 is confirmed associated with angiogenesis, trials on anti-CD276 combined with Bevacizumab is attractive. EGFRvIII mutation leads to the unique extracellular domain of EGFR, becoming an ideal specific antigen for both vaccine and CAR-T therapy. As discussed above, given that single-target therapy induces recurrence and subsequently resistance to original treatment due to molecular heterogeneity and evolution of tumor, implementation of targeting multiple antigens or with antagonism of immunosuppressive cytokines is recommended. In short, more laboratorial and clinical effort is required when it comes to combination therapy (Table 3).
Availability of data and materials
Not applicable
References
Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, Ohgaki H, Wiestler OD, Kleihues P, Ellison DW. The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary. Acta Neuropathol. 2016;131(6):803–20.
Louis DN, Perry A, Wesseling P, Brat DJ, Cree IA, Figarella-Branger D, Hawkins C, Ng HK, Pfister SM, Reifenberger G, et al. The 2021 WHO Classification of Tumors of the Central Nervous System: a summary. Neuro Oncol. 2021;23(8):1231–51.
Ostrom QT, Cioffi G, Gittleman H, Patil N, Waite K, Kruchko C, Barnholtz-Sloan JS: CBTRUS Statistical Report: Primary Brain and Other Central Nervous System Tumors Diagnosed in the United States in 2012–2016. Neuro-oncology 2019;21(Suppl 5).
Campian J, Gutmann DH. CNS Tumors in Neurofibromatosis. J Clin Oncol. 2017;35(21):2378–85.
Duffau H, Taillandier L. New concepts in the management of diffuse low-grade glioma: Proposal of a multistage and individualized therapeutic approach. Neuro Oncol. 2015;17(3):332–42.
Weller M, Le Rhun E. How did lomustine become standard of care in recurrent glioblastoma? Cancer treatment reviews. 2020;87:102029.
Alexander BM, Cloughesy TF. Adult Glioblastoma. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2017;35(21):2402–9.
Indraccolo S, Lombardi G, Fassan M, Pasqualini L, Giunco S, Marcato R, Gasparini A, Candiotto C, Nalio S, Fiduccia P, et al. Genetic, Epigenetic, and Immunologic Profiling of MMR-Deficient Relapsed Glioblastoma. Clin Cancer Res. 2019;25(6):1828–37.
Tan AC, Ashley DM, López GY, Malinzak M, Friedman HS, Khasraw M. Management of glioblastoma: State of the art and future directions. CA a cancer journal for clinicians. 2020;70(4):299–312.
Brennan CW, Verhaak RGW, McKenna A, Campos B, Noushmehr H, Salama SR, Zheng S, Chakravarty D, Sanborn JZ, Berman SH, et al. The somatic genomic landscape of glioblastoma. Cell. 2013;155(2):462–77.
Na K, Kim HS, Shim HS, Chang JH, Kang SG, Kim SH. Targeted next-generation sequencing panel (TruSight Tumor 170) in diffuse glioma: a single institutional experience of 135 cases. J Neurooncol. 2019;142(3):445–54.
Capper D, Jones DTW, Sill M, Hovestadt V, Schrimpf D, Sturm D, Koelsche C, Sahm F, Chavez L, Reuss DE, et al. DNA methylation-based classification of central nervous system tumours. Nature. 2018;555(7697):469–74.
Jakola AS, Myrmel KS, Kloster R, Torp SH, Lindal S, Unsgård G, Solheim O. Comparison of a strategy favoring early surgical resection vs a strategy favoring watchful waiting in low-grade gliomas. JAMA. 2012;308(18):1881–8.
Lapointe S, Perry A, Butowski NA. Primary brain tumours in adults. Lancet (London, England). 2018;392(10145):432–46.
Jakola AS, Skjulsvik AJ, Myrmel KS, Sjåvik K, Unsgård G, Torp SH, Aaberg K, Berg T, Dai HY, Johnsen K, et al. Surgical resection versus watchful waiting in low-grade gliomas. Ann Oncol. 2017;28(8):1942–8.
Baumert BG, Hegi ME, Van Den Bent MJ, Von Deimling A, Gorlia T, Hoang-Xuan K, Brandes AA, Kantor G, Taphoorn MJB, Hassel MB, et al. Temozolomide chemotherapy versus radiotherapy in high-risk low-grade glioma (EORTC 22033–26033): a randomised, open-label, phase 3 intergroup study. Lancet Oncol. 2016;17(11):1521–32.
Buckner JC, Shaw EG, Pugh SL, Chakravarti A, Gilbert MR, Barger GR, Coons S, Ricci P, Bullard D, Brown PD, et al. Radiation plus Procarbazine, CCNU, and Vincristine in Low-Grade Glioma. N Engl J Med. 2016;374(14):1344–55.
Lassaletta A, Scheinemann K, Zelcer SM, Hukin J, Wilson BA, Jabado N, Carret AS, Lafay-Cousin L, Larouche V, Hawkins CE, et al. Phase II Weekly Vinblastine for Chemotherapy-Naïve Children With Progressive Low-Grade Glioma: A Canadian Pediatric Brain Tumor Consortium Study. J Clin Oncol. 2016;34(29):3537–43.
Nellan A, Wright E, Campbell K, Davies KD, Donson AM, Amani V, Judd A, Hemenway MS, Raybin J, Foreman NK, et al. Retrospective analysis of combination carboplatin and vinblastine for pediatric low-grade glioma. J Neurooncol. 2020;148(3):569–75.
Weller M, van den Bent M, Tonn JC, Stupp R, Preusser M, Cohen-Jonathan-Moyal E, Henriksson R, Le Rhun E, Balana C, Chinot O, et al. European Association for Neuro-Oncology (EANO) guideline on the diagnosis and treatment of adult astrocytic and oligodendroglial gliomas. Lancet Oncol. 2017;18(6):e315–29.
Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, Belanger K, Brandes AA, Marosi C, Bogdahn U, et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med. 2005;352(10):987–96.
Stupp R, Taillibert S, Kanner A, Read W, Steinberg D, Lhermitte B, Toms S, Idbaih A, Ahluwalia MS, Fink K, et al. Effect of Tumor-Treating Fields Plus Maintenance Temozolomide vs Maintenance Temozolomide Alone on Survival in Patients With Glioblastoma: A Randomized Clinical Trial. JAMA. 2017;318(23):2306–16.
Wick W, Gorlia T, Bendszus M, Taphoorn M, Sahm F, Harting I, Brandes AA, Taal W, Domont J, Idbaih A, et al. Lomustine and Bevacizumab in Progressive Glioblastoma. N Engl J Med. 2017;377(20):1954–63.
Hegi ME, Diserens A-C, Gorlia T, Hamou M-F, de Tribolet N, Weller M, Kros JM, Hainfellner JA, Mason W, Mariani L, et al. MGMT gene silencing and benefit from temozolomide in glioblastoma. The New England journal of medicine. 2005;352(10):997–1003.
Hegi ME, Diserens AC, Gorlia T, Hamou MF, de Tribolet N, Weller M, Kros JM, Hainfellner JA, Mason W, Mariani L, et al. MGMT gene silencing and benefit from temozolomide in glioblastoma. N Engl J Med. 2005;352(10):997–1003.
Brigliadori G, Foca F, Dall’Agata M, Rengucci C, Melegari E, Cerasoli S, Amadori D, Calistri D, Faedi M. Defining the cutoff value of MGMT gene promoter methylation and its predictive capacity in glioblastoma. J Neurooncol. 2016;128(2):333–9.
Esteller M, Hamilton SR, Burger PC, Baylin SB, Herman JG. Inactivation of the DNA repair gene O6-methylguanine-DNA methyltransferase by promoter hypermethylation is a common event in primary human neoplasia. Can Res. 1999;59(4):793–7.
Sun MZ, Oh T, Ivan ME, Clark AJ, Safaee M, Sayegh ET, Kaur G, Parsa AT, Bloch O. Survival impact of time to initiation of chemoradiotherapy after resection of newly diagnosed glioblastoma. J Neurosurg. 2015;122(5):1144–50.
Balana C, Vaz MA, Manuel Sepúlveda J, Mesia C, Del Barco S, Pineda E, Muñoz-Langa J, Estival A, de Las PR, Fuster J, et al. A phase II randomized, multicenter, open-label trial of continuing adjuvant temozolomide beyond 6 cycles in patients with glioblastoma (GEINO 14–01). Neuro Oncol. 2020;22(12):1851–61.
McAleenan A, Kelly C, Spiga F, Kernohan A, Cheng HY, Dawson S, Schmidt L, Robinson T, Brandner S, Faulkner CL, et al. Prognostic value of test(s) for O6-methylguanine-DNA methyltransferase (MGMT) promoter methylation for predicting overall survival in people with glioblastoma treated with temozolomide. Cochrane Database Syst Rev. 2021;3(3):Cd013316.
Mansouri A, Hachem LD, Mansouri S, Nassiri F, Laperriere NJ, Xia D, Lindeman NI, Wen PY, Chakravarti A, Mehta MP, et al. MGMT promoter methylation status testing to guide therapy for glioblastoma: refining the approach based on emerging evidence and current challenges. Neuro Oncol. 2019;21(2):167–78.
Raghavan S, Baskin DS, Sharpe MA. A “Clickable” Probe for Active MGMT in Glioblastoma Demonstrates Two Discrete Populations of MGMT. Cancers. 2020;12(2):453.
Tzaridis T, Schafer N, Weller J, Steinbach JP, Schlegel U, Seidel S, Sabel M, Hau P, Seidel C, Krex D, et al. MGMT promoter methylation analysis for allocating combined CCNU/TMZ chemotherapy: Lessons learned from the CeTeG/NOA-09 trial. Int J Cancer. 2021;148(7):1695–707.
Brandner S, von Deimling A. Diagnostic, prognostic and predictive relevance of molecular markers in gliomas. Neuropathol Appl Neurobiol. 2015;41(6):694–720.
Oldrini B, Vaquero-Siguero N, Mu QH, Kroon P, Zhang Y, Galan-Ganga M, Bao ZS, Wang Z, Liu HJ, Sa JK, et al. MGMT genomic rearrangements contribute to chemotherapy resistance in gliomas. Nature Communications. 2020;11(1):1–10.
Rahman MA, Gras Navarro A, Brekke J, Engelsen A, Bindesbøll C, Sarowar S, Bahador M, Bifulco E, Goplen D, Waha A, et al. Bortezomib administered prior to temozolomide depletes MGMT, chemosensitizes glioblastoma with unmethylated MGMT promoter and prolongs animal survival. Br J Cancer. 2019;121(7):545–55.
Chen X, Zhang M, Gan H, Wang H, Lee J-H, Fang D, Kitange GJ, He L, Hu Z, Parney IF, et al. A novel enhancer regulates MGMT expression and promotes temozolomide resistance in glioblastoma. Nature Communications. 2018;9(1):1–14.
Frenel JS, Cartron PF, Gourmelon C, Campion L, Aumont M, Augereau P, Ducray F, Loussouarn D, Lallier L, Robert M, et al. FOLAGLI: A phase I study of folinic acid combined with temozolomide and radiotherapy to modulate MGMT gene promoter methylation in newly diagnosed MGMT non-methytated glioblastoma. Ann Oncol. 2020;31:S400–S400.
Voldborg BR, Damstrup L, Spang-Thomsen M, Poulsen HS. Epidermal growth factor receptor (EGFR) and EGFR mutations, function and possible role in clinical trials. Annals of oncology : official journal of the European Society for Medical Oncology. 1997;8(12):1197–206.
Libermann TA, Razon N, Bartal AD, Yarden Y, Schlessinger J, Soreq H. Expression of epidermal growth factor receptors in human brain tumors. Can Res. 1984;44(2):753–60.
Libermann TA, Nusbaum HR, Razon N, Kris R, Lax I, Soreq H, Whittle N, Waterfield MD, Ullrich A, Schlessinger J. Amplification, enhanced expression and possible rearrangement of EGF receptor gene in primary human brain tumours of glial origin. Nature. 1985;313(5998):144–7.
Furnari FB, Cloughesy TF, Cavenee WK, Mischel PS. Heterogeneity of epidermal growth factor receptor signalling networks in glioblastoma. Nat Rev Cancer. 2015;15(5):302–10.
Lassman AB, Aldape KD, Ansell PJ, Bain E, Curran WJ, Eoli M, French PJ, Kinoshita M, Looman J, Mehta M, et al. Epidermal growth factor receptor (EGFR) amplification rates observed in screening patients for randomized trials in glioblastoma. J Neurooncol. 2019;144(1):205–10.
Sepúlveda-Sánchez JM, Vaz MÁ, Balañá C, Gil-Gil M, Reynés G, Gallego Ó, Martínez-García M, Vicente E, Quindós M, Luque R, et al. Phase II trial of dacomitinib, a pan-human EGFR tyrosine kinase inhibitor, in recurrent glioblastoma patients with EGFR amplification. Neuro Oncol. 2017;19(11):1522–31.
Byeon S, Hong JY, Lee J, Nam DH, Park SH, Park JO, Park YS, Lim HY, Kang WK, Kim ST. Use of Gefitinib in EGFR-Amplified Refractory Solid Tumors: An Open-Label, Single-Arm. Single-Center Prospective Pilot Study Target Oncol. 2020;15(2):185–92.
Liu X, Chen X, Shi L, Shan Q, Cao Q, Yue C, Li H, Li S, Wang J, Gao S, et al. The third-generation EGFR inhibitor AZD9291 overcomes primary resistance by continuously blocking ERK signaling in glioblastoma. Journal of experimental & clinical cancer research : CR. 2019;38(1):219.
Chen C, Cheng C-D, Wu H, Wang Z-W, Wang L, Jiang Z-R, Wang A-L, Hu C, Dong Y-F, Niu W-X, et al. Osimertinib successfully combats EGFR-negative glioblastoma cells by inhibiting the MAPK pathway. Acta Pharmacol Sin. 2021;42(1):108–14.
Gao M, Fu Y, Zhou W, Gui G, Lal B, Li Y, Xia S, Ji H, Eberhart CG, Laterra J, et al. EGFR Activates a TAZ-Driven Oncogenic Program in Glioblastoma. Can Res. 2021;81(13):3580–92.
Neyns B, Sadones J, Joosens E, Bouttens F, Verbeke L, Baurain JF, D’Hondt L, Strauven T, Chaskis C, In’t Veld P, et al. Stratified phase II trial of cetuximab in patients with recurrent high-grade glioma. Annals of oncology : official journal of the European Society for Medical Oncology. 2009;20(9):1596–603.
Gan HK, Burgess AW, Clayton AHA, Scott AM. Targeting of a conformationally exposed, tumor-specific epitope of EGFR as a strategy for cancer therapy. Can Res. 2012;72(12):2924–30.
Ronellenfitsch MW, Zeiner PS, Mittelbronn M, Urban H, Pietsch T, Reuter D, Senft C, Steinbach JP, Westphal M, Harter PN. Akt and mTORC1 signaling as predictive biomarkers for the EGFR antibody nimotuzumab in glioblastoma. Acta Neuropathol Commun. 2018;6(1):81.
van den Bent M, French P, Eoli M, Sepulvado J, Walenkamp A, Weller M, Looman J, Ansell P, Gorlia T, Golfinopoulos V. UPDATED RESULTS OF THE INTELLANCE 2/EORTC TRIAL 1410 RANDOMIZED PHASE II STUDY ON DEPATUX -M ALONE, DEPATUX-M IN COMBINATION WITH TEMOZOLOMIDE (TMZ) AND EITHER TMZ OR LOMUSTINE (LOM) IN RECURRENT EGFR AMPLIFIED GLIOBLASTOMA (NCT02343406). Neuro Oncol. 2018;20:241–241.
Lassman AB, van den Bent MJ, Gan HK, Reardon DA, Kumthekar P, Butowski N, Lwin Z, Mikkelsen T, Nabors LB, Papadopoulos KP, et al. Safety and efficacy of depatuxizumab mafodotin + temozolomide in patients with EGFR-amplified, recurrent glioblastoma: results from an international phase I multicenter trial. Neuro Oncol. 2019;21(1):106–14.
Marin B-M, Porath KA, Jain S, Kim M, Conage-Pough JE, Oh J-H, Miller CL, Talele S, Kitange GJ, Tian S et al: Heterogeneous delivery across the blood-brain barrier limits the efficacy of an EGFR-targeting antibody drug conjugate in glioblastoma. Neuro-oncology 2021.
Rizzuto MA, Dal Magro R, Barbieri L, Pandolfi L, Sguazzini-Viscontini A, Truffi M, Salvioni L, Corsi F, Colombo M, Re F, et al. H-Ferritin nanoparticle-mediated delivery of antibodies across a BBB in vitro model for treatment of brain malignancies. Biomaterials science. 2021;9(6):2032–42.
Ferreira NN, de Oliveira Junior E, Granja S, Boni FI, Ferreira LMB, Cury BSF, Santos LCR, Reis RM, Lima EM, Baltazar F, et al. Nose-to-brain co-delivery of drugs for glioblastoma treatment using nanostructured system. International journal of pharmaceutics. 2021;603:120714.
Schuster J, Lai RK, Recht LD, Reardon DA, Paleologos NA, Groves MD, Mrugala MM, Jensen R, Baehring JM, Sloan A, et al. A phase II, multicenter trial of rindopepimut (CDX-110) in newly diagnosed glioblastoma: the ACT III study. Neuro Oncol. 2015;17(6):854–61.
Weller M, Butowski N, Tran DD, Recht LD, Lim M, Hirte H, Ashby L, Mechtler L, Goldlust SA, Iwamoto F, et al. Rindopepimut with temozolomide for patients with newly diagnosed, EGFRvIII-expressing glioblastoma (ACT IV): a randomised, double-blind, international phase 3 trial. Lancet Oncol. 2017;18(10):1373–85.
O'Rourke DM, Nasrallah MP, Desai A, Melenhorst JJ, Mansfield K, Morrissette JJD, Martinez-Lage M, Brem S, Maloney E, Shen A et al: A single dose of peripherally infused EGFRvIII-directed CAR T cells mediates antigen loss and induces adaptive resistance in patients with recurrent glioblastoma. Science translational medicine 2017, 9(399).
Johnson LA, Scholler J, Ohkuri T, Kosaka A, Patel PR, McGettigan SE, Nace AK, Dentchev T, Thekkat P, Loew A, et al. Rational development and characterization of humanized anti-EGFR variant III chimeric antigen receptor T cells for glioblastoma. Science translational medicine. 2015;7(275):275ra222.
Hoxhaj G, Manning BD. The PI3K-AKT network at the interface of oncogenic signalling and cancer metabolism. Nat Rev Cancer. 2020;20(2):74–88.
Zhao H-F, Wang J, Shao W, Wu C-P, Chen Z-P. To S-ST, Li W-P: Recent advances in the use of PI3K inhibitors for glioblastoma multiforme: current preclinical and clinical development. Mol Cancer. 2017;16(1):100.
Chang SM, Wen P, Cloughesy T, Greenberg H, Schiff D, Conrad C, Fink K, Robins HI, De Angelis L, Raizer J, et al. Phase II study of CCI-779 in patients with recurrent glioblastoma multiforme. Invest New Drugs. 2005;23(4):357–61.
Kaley TJ, Panageas KS, Pentsova EI, Mellinghoff IK, Nolan C, Gavrilovic I, DeAngelis LM, Abrey LE, Holland EC, Omuro A, et al. Phase I clinical trial of temsirolimus and perifosine for recurrent glioblastoma. Ann Clin Transl Neurol. 2020;7(4):429–36.
Wen PY, Touat M, Alexander BM, Mellinghoff IK, Ramkissoon S, McCluskey CS, Pelton K, Haidar S, Basu SS, Gaffey SC, et al. Buparlisib in Patients With Recurrent Glioblastoma Harboring Phosphatidylinositol 3-Kinase Pathway Activation: An Open-Label, Multicenter, Multi-Arm. Phase II Trial J Clin Oncol. 2019;37(9):741–50.
Rosenthal M, Clement PM, Campone M, Gil-Gil MJ, DeGroot J, Chinot O, Idbaih A, Gan H, Raizer J, Wen PY, et al. Buparlisib plus carboplatin or lomustine in patients with recurrent glioblastoma: a phase Ib/II, open-label, multicentre, randomised study. ESMO Open. 2020;5(4):e000672.
Hainsworth JD, Becker KP, Mekhail T, Chowdhary SA, Eakle JF, Wright D, Langdon RM, Yost KJ, Padula GDA, West-Osterfield K, et al. Phase I/II study of bevacizumab with BKM120, an oral PI3K inhibitor, in patients with refractory solid tumors (phase I) and relapsed/refractory glioblastoma (phase II). J Neurooncol. 2019;144(2):303–11.
Wick W, Gorlia T, Bady P, Platten M, van den Bent MJ, Taphoorn MJB, Steuve J, Brandes AA, Hamou M-F, Wick A, et al. Phase II Study of Radiotherapy and Temsirolimus versus Radiochemotherapy with Temozolomide in Patients with Newly Diagnosed Glioblastoma without MGMT Promoter Hypermethylation (EORTC 26082). Clinical cancer research : an official journal of the American Association for Cancer Research. 2016;22(19):4797–806.
Ma DJ, Galanis E, Anderson SK, Schiff D, Kaufmann TJ, Peller PJ, Giannini C, Brown PD, Uhm JH, McGraw S, et al. A phase II trial of everolimus, temozolomide, and radiotherapy in patients with newly diagnosed glioblastoma: NCCTG N057K. Neuro Oncol. 2015;17(9):1261–9.
Wen PY, Rodon JA, Mason W, Beck JT, DeGroot J, Donnet V, Mills D, El-Hashimy M, Rosenthal M. Phase I, open-label, multicentre study of buparlisib in combination with temozolomide or with concomitant radiation therapy and temozolomide in patients with newly diagnosed glioblastoma. ESMO Open. 2020;5(4):e000673.
Dean M, Park M, Le Beau MM, Robins TS, Diaz MO, Rowley JD, Blair DG, Vande Woude GF. The human met oncogene is related to the tyrosine kinase oncogenes. Nature. 1985;318(6044):385–8.
Cheng F, Guo D. MET in glioma: signaling pathways and targeted therapies. Journal of Experimental & Clinical Cancer Research. 2019;38(1):1–13.
Xie Q, Bradley R, Kang L, Koeman J, Ascierto ML, Worschech A, De Giorgi V, Wang E, Kefene L, Su Y, et al. Hepatocyte growth factor (HGF) autocrine activation predicts sensitivity to MET inhibition in glioblastoma. Proc Natl Acad Sci USA. 2012;109(2):570–5.
Wen PY, Schiff D, Cloughesy TF, Raizer JJ, Laterra J, Smitt M, Wolf M, Oliner KS, Anderson A, Zhu M, et al. A phase II study evaluating the efficacy and safety of AMG 102 (rilotumumab) in patients with recurrent glioblastoma. Neuro Oncol. 2011;13(4):437–46.
Cloughesy T, Finocchiaro G, Belda-Iniesta C, Recht L, Brandes AA, Pineda E, Mikkelsen T, Chinot OL, Balana C, Macdonald DR, et al. Randomized, Double-Blind, Placebo-Controlled, Multicenter Phase II Study of Onartuzumab Plus Bevacizumab Versus Placebo Plus Bevacizumab in Patients With Recurrent Glioblastoma: Efficacy, Safety, and Hepatocyte Growth Factor and O(6)-Methylguanine-DNA Methyltransferase Biomarker Analyses. J Clin Oncol. 2017;35(3):343–51.
Wen PY, Drappatz J, de Groot J, Prados MD, Reardon DA, Schiff D, Chamberlain M, Mikkelsen T, Desjardins A, Holland J, et al. Phase II study of cabozantinib in patients with progressive glioblastoma: subset analysis of patients naive to antiangiogenic therapy. Neuro Oncol. 2018;20(2):249–58.
Cloughesy TF, Drappatz J, de Groot J, Prados MD, Reardon DA, Schiff D, Chamberlain M, Mikkelsen T, Desjardins A, Ping J, et al. Phase II study of cabozantinib in patients with progressive glioblastoma: subset analysis of patients with prior antiangiogenic therapy. Neuro Oncol. 2018;20(2):259–67.
van den Bent M, Azaro A, De Vos F, Sepulveda J, Yung WKA, Wen PY, Lassman AB, Joerger M, Tabatabai G, Rodon J, et al. A Phase Ib/II, open-label, multicenter study of INC280 (capmatinib) alone and in combination with buparlisib (BKM120) in adult patients with recurrent glioblastoma. J Neurooncol. 2020;146(1):79–89.
Singh D, Chan JM, Zoppoli P, Niola F, Sullivan R, Castano A, Liu EM, Reichel J, Porrati P, Pellegatta S, et al. Transforming fusions of FGFR and TACC genes in human glioblastoma. Science (New York, NY). 2012;337(6099):1231–5.
Di Stefano AL, Fucci A, Frattini V, Labussiere M, Mokhtari K, Zoppoli P, Marie Y, Bruno A, Boisselier B, Giry M, et al. Detection, Characterization, and Inhibition of FGFR-TACC Fusions in IDH Wild-type Glioma. Clinical cancer research : an official journal of the American Association for Cancer Research. 2015;21(14):3307–17.
Tabernero J, Bahleda R, Dienstmann R, Infante JR, Mita A, Italiano A, Calvo E, Moreno V, Adamo B, Gazzah A, et al. Phase I Dose-Escalation Study of JNJ-42756493, an Oral Pan-Fibroblast Growth Factor Receptor Inhibitor, in Patients With Advanced Solid Tumors. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2015;33(30):3401–8.
Sharma M, Schilero C, Peereboom DM, Hobbs BP, Elson P, Stevens GHJ, McCrae K, Nixon AB, Ahluwalia MS. Phase II study of Dovitinib in recurrent glioblastoma. J Neurooncol. 2019;144(2):359–68.
Davies H, Bignell GR, Cox C, Stephens P, Edkins S, Clegg S, Teague J, Woffendin H, Garnett MJ, Bottomley W, et al. Mutations of the BRAF gene in human cancer. Nature. 2002;417(6892):949–54.
Planchard D, Besse B, Groen HJM, Souquet P-J, Quoix E, Baik CS, Barlesi F, Kim TM, Mazieres J, Novello S, et al. Dabrafenib plus trametinib in patients with previously treated BRAF(V600E)-mutant metastatic non-small cell lung cancer: an open-label, multicentre phase 2 trial. Lancet Oncol. 2016;17(7):984–93.
Brose MS, Cabanillas ME, Cohen EEW, Wirth LJ, Riehl T, Yue H, Sherman SI, Sherman EJ. Vemurafenib in patients with BRAF(V600E)-positive metastatic or unresectable papillary thyroid cancer refractory to radioactive iodine: a non-randomised, multicentre, open-label, phase 2 trial. Lancet Oncol. 2016;17(9):1272–82.
Subbiah V, Kreitman RJ, Wainberg ZA, Cho JY, Schellens JHM, Soria JC, Wen PY, Zielinski C, Cabanillas ME, Urbanowitz G, et al. Dabrafenib and Trametinib Treatment in Patients With Locally Advanced or Metastatic BRAF V600-Mutant Anaplastic Thyroid Cancer. Journal of clinical oncology official journal of the American Society of Clinical Oncology. 2018;36(1):7.
Robert C, Grob JJ, Stroyakovskiy D, Karaszewska B, Hauschild A, Levchenko E, Chiarion Sileni V, Schachter J, Garbe C, Bondarenko I, et al. Five-Year Outcomes with Dabrafenib plus Trametinib in Metastatic Melanoma. N Engl J Med. 2019;381(7):626–36.
Kaley T, Touat M, Subbiah V, Hollebecque A, Rodon J, Lockhart AC, Keedy V, Bielle F, Hofheinz R-D, Joly F, et al. BRAF Inhibition in -Mutant Gliomas: Results From the VE-BASKET Study. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2018;36(35):3477–84.
Schreck KC, Guajardo A, Lin DDM, Eberhart CG, Grossman SA. Concurrent BRAF/MEK Inhibitors in V600-Mutant High-Grade Primary Brain Tumors. Journal of the National Comprehensive Cancer Network : JNCCN. 2018;16(4):343–7.
Wen P, De Greve J, Mason W, Hofheinz R-D, Dietrich S, de Vos F, van den Bent M, Mookerjee B, Boran A, Burgess P, et al. RARE-11. EFFICACY AND SAFETY OF DABRAFENIB + TRAMETINIB IN PATIENTS WITH RECURRENT/REFRACTORY BRAF V600E–MUTATED LOW-GRADE GLIOMA (LGG). Neuro-Oncology. 2018;20(suppl_6):vi238–9.
Wen P, Alexander S, Yung-Jue B, van den Bent M, Gazzah A, Dietrich S, de Vos F, van Linde M, Lai A, Chi A, et al. RARE-09. EFFICACY AND SAFETY OF DABRAFENIB + TRAMETINIB IN PATIENTS WITH RECURRENT/REFRACTORY BRAF V600E–MUTATED HIGH-GRADE GLIOMA (HGG). Neuro-Oncology. 2018;20(suppl_6):vi238–vi238.
Schreck KC, Grossman SA, Pratilas CA. BRAF Mutations and the Utility of RAF and MEK Inhibitors in Primary Brain Tumors. Cancers. 2019;11(9):1262.
Woo HY, Na K, Yoo J, Chang JH, Park YN, Shim HS, Kim SH. Glioblastomas harboring gene fusions detected by next-generation sequencing. Brain Tumor Pathol. 2020;37(4):136–44.
Ferguson SD, Zhou S, Huse JT, de Groot JF, Xiu J, Subramaniam DS, Mehta S, Gatalica Z, Swensen J, Sanai N, et al. Targetable Gene Fusions Associate With the IDH Wild-Type Astrocytic Lineage in Adult Gliomas. J Neuropathol Exp Neurol. 2018;77(6):437–42.
Shepherd DJ, Miller TE, Forst DA, Jones P, Nardi V, Martinez-Lage M, Stemmer-Rachamimov A, Gonzalez RG, Iafrate AJ, Ritterhouse LL: Mosaicism for Receptor Tyrosine Kinase Activation in a Glioblastoma Involving Both PDGFRA Amplification and NTRK2 Fusion. Oncologist 2021.
Alharbi M, Mobark NA, Balbaid AAO, Alanazi FA, Aljabarat WAR, Bakhsh EA, Ramkissoon SH, Abedalthagafi M: Regression of ETV6-NTRK3 Infantile Glioblastoma After First-Line Treatment With Larotrectinib. JCO precision oncology 2020, 4:PO.20.00017.
Ku DT-L, Shing MM-K, Chan GC-F, Fu E, Yau P-W, Luk C-W, Cheng K-F, Ho WW-S, Ng H-K, Po Y-C, et al. HGG-48. ROS1 INHIBITOR ENTRECTINIB USE IN RELAPSE/REFRACTORY INFANTILE GLIOBLASTOMA WITH POSITIVE ROS1 FUSION - A CASE REPORT WITH PROMISING RESPONSE. Neuro-Oncology. 2020;22(Supplement_3):iii352–iii352.
Dyson NJ. RB1: a prototype tumor suppressor and an enigma. Genes Dev. 2016;30(13):1492–502.
Taylor JW, Parikh M, Phillips JJ, James CD, Molinaro AM, Butowski NA, Clarke JL, Oberheim-Bush NA, Chang SM, Berger MS, et al. Phase-2 trial of palbociclib in adult patients with recurrent RB1-positive glioblastoma. J Neurooncol. 2018;140(2):477–83.
Miller TW, Traphagen NA, Li J, Lewis LD, Lopes B, Asthagiri A, Loomba J, De Jong J, Schiff D, Patel SH, et al. Tumor pharmacokinetics and pharmacodynamics of the CDK4/6 inhibitor ribociclib in patients with recurrent glioblastoma. J Neurooncol. 2019;144(3):563–72.
Tien AC, Li J, Bao X, Derogatis A, Kim S, Mehta S, Sanai N. A Phase 0 Trial of Ribociclib in Recurrent Glioblastoma Patients Incorporating a Tumor Pharmacodynamic- and Pharmacokinetic-Guided Expansion Cohort. Clin Cancer Res. 2019;25(19):5777–86.
Liao X, Hong Y, Mao Y, Chen N, Wang Q, Wang Z, Zhang L, Wang L, Shi C, Shi W, et al. SPH3643: A novel cyclin-dependent kinase 4/6 inhibitor with good anticancer efficacy and strong blood-brain barrier permeability. Cancer Sci. 2020;111(5):1761–73.
Levine AJ. p53, the Cellular Gatekeeper for Growth and Division. Cell. 1997;88(3):323–31.
Hernández Borrero LJ, El-Deiry WS. Tumor suppressor p53 Biology signaling pathways and therapeutic targeting. Biochimica et Biophysica Acta (BBA) Reviews on Cancer. 2021;1876(1):188556.
Wick W, Dettmer S, Berberich A, Kessler T, Karapanagiotou-Schenkel I, Wick A, Winkler F, Pfaff E, Brors B, Debus J et al: N2M2 (NOA-20) phase I/II trial of molecularly matched targeted therapies plus radiotherapy in patients with newly diagnosed non-MGMT hypermethylated glioblastoma. Neuro-oncology 2019, 21(1).
Miles X, Vandevoorde C, Hunter A, Bolcaen J. MDM2/X Inhibitors as Radiosensitizers for Glioblastoma Targeted Therapy. Frontiers in oncology. 2021;11:703442.
Gluck WL, Gounder MM, Frank R, Eskens F, Blay JY, Cassier PA, Soria JC, Chawla S, de Weger V, Wagner AJ, et al. Phase 1 study of the MDM2 inhibitor AMG 232 in patients with advanced P53 wild-type solid tumors or multiple myeloma. Invest New Drugs. 2020;38(3):831–43.
Sanai N, Li J, Boerner J, Stark K, Wu J, Kim S, Derogatis A, Mehta S, Dhruv HD, Heilbrun LK, et al. Phase 0 Trial of AZD1775 in First-Recurrence Glioblastoma Patients. Clin Cancer Res. 2018;24(16):3820–8.
Killela PJ, Reitman ZJ, Jiao Y, Bettegowda C, Agrawal N, Diaz LA, Friedman AH, Friedman H, Gallia GL, Giovanella BC, et al. TERT promoter mutations occur frequently in gliomas and a subset of tumors derived from cells with low rates of self-renewal. Proc Natl Acad Sci USA. 2013;110(15):6021–6.
Horn S, Figl A, Rachakonda PS, Fischer C, Sucker A, Gast A, Kadel S, Moll I, Nagore E, Hemminki K, et al. TERT promoter mutations in familial and sporadic melanoma. Science (New York, NY). 2013;339(6122):959–61.
Nguyen HN, Lie A, Li T, Chowdhury R, Liu F, Ozer B, Wei B, Green RM, Ellingson BM, Wang H-J, et al. Human TERT promoter mutation enables survival advantage from MGMT promoter methylation in IDH1 wild-type primary glioblastoma treated by standard chemoradiotherapy. Neuro Oncol. 2017;19(3):394–404.
Gramatzki D, Felsberg J, Hentschel B, Wolter M, Schackert G, Westphal M, Regli L, Thon N, Tatagiba M, Wick W, et al. Telomerase reverse transcriptase promoter mutation- and O(6)-methylguanine DNA methyltransferase promoter methylation-mediated sensitivity to temozolomide in isocitrate dehydrogenase-wild-type glioblastoma: is there a link? Eur J Cancer. 2021;147:84–94.
Takahashi M, Miki S, Fujimoto K, Fukuoka K, Matsushita Y, Maida Y, Yasukawa M, Hayashi M, Shinkyo R, Kikuchi K, et al. Eribulin penetrates brain tumor tissue and prolongs survival of mice harboring intracerebral glioblastoma xenografts. Cancer Sci. 2019;110(7):2247–57.
Amen AM, Fellmann C, Soczek KM, Ren SM, Lew RJ, Knott GJ, Park JE, McKinney AM, Mancini A, Doudna JA et al: Cancer-specific loss of TERT activation sensitizes glioblastoma to DNA damage. Proc Natl Acad Sci U S A 2021, 118(13).
Li X, Qian X, Wang B, Xia Y, Zheng Y, Du L, Xu D, Xing D, Depinho RA, Lu Z. Programmable base editing of mutated TERT promoter inhibits brain tumour growth. Nat Cell Biol. 2020;22(3):282–8.
Goldberg AL. Protein degradation and protection against misfolded or damaged proteins. Nature. 2003;426(6968):895–9.
Narayanan S, Cai C-Y, Assaraf YG, Guo H-Q, Cui Q, Wei L, Huang J-J, Ashby CR, Chen Z-S. Targeting the ubiquitin-proteasome pathway to overcome anti-cancer drug resistance. Drug Resistance Updates. 2020;48:100663.
Friday BB, Anderson SK, Buckner J, Yu C, Giannini C, Geoffroy F, Schwerkoske J, Mazurczak M, Gross H, Pajon E, et al. Phase II trial of vorinostat in combination with bortezomib in recurrent glioblastoma: a north central cancer treatment group study. Neuro Oncol. 2012;14(2):215–21.
Kong XT, Nguyen NT, Choi YJ, Zhang G, Nguyen HN, Filka E, Green S, Yong WH, Liau LM, Green RM, et al. Phase 2 Study of Bortezomib Combined With Temozolomide and Regional Radiation Therapy for Upfront Treatment of Patients With Newly Diagnosed Glioblastoma Multiforme: Safety and Efficacy Assessment. Int J Radiat Oncol Biol Phys. 2018;100(5):1195–203.
Quillin J, Patel R, Herzberg E, Alton D, Bikzhanova G, Geisler L, Olson J. A phase 0 analysis of ixazomib in patients with glioblastoma. Molecular and clinical oncology. 2020;13(5):43.
Huang J, Campian JL, Gujar AD, Tsien C, Ansstas G, Tran DD, Dewees TA, Lockhart AC, Kim AH. Final results of a phase I dose-escalation, dose-expansion study of adding disulfiram with or without copper to adjuvant temozolomide for newly diagnosed glioblastoma. J Neurooncol. 2018;138(1):105–11.
Huang J, Chaudhary R, Cohen AL, Fink K, Goldlust S, Boockvar J, Chinnaiyan P, Wan L, Marcus S, Campian JL. A multicenter phase II study of temozolomide plus disulfiram and copper for recurrent temozolomide-resistant glioblastoma. J Neurooncol. 2019;142(3):537–44.
Szabo E, Schneider H, Seystahl K, Rushing EJ, Herting F, Weidner KM, Weller M. Autocrine VEGFR1 and VEGFR2 signaling promotes survival in human glioblastoma models in vitro and in vivo. Neuro Oncol. 2016;18(9):1242–52.
Sorensen AG, Emblem KE, Polaskova P, Jennings D, Kim H, Ancukiewicz M, Wang M, Wen PY, Ivy P, Batchelor TT, et al. Increased survival of glioblastoma patients who respond to antiangiogenic therapy with elevated blood perfusion. Cancer Res. 2012;72(2):402–7.
Ferrara N, Hillan KJ, Novotny W. Bevacizumab (Avastin), a humanized anti-VEGF monoclonal antibody for cancer therapy. Biochem Biophys Res Commun. 2005;333(2):328–35.
Friedman HS, Prados MD, Wen PY, Mikkelsen T, Schiff D, Abrey LE, Yung WKA, Paleologos N, Nicholas MK, Jensen R, et al. Bevacizumab Alone and in Combination With Irinotecan in Recurrent Glioblastoma. J Clin Oncol. 2009;27(28):4733–40.
Kreisl TN, Kim L, Moore K, Duic P, Royce C, Stroud I, Garren N, Mackey M, Butman JA, Camphausen K, et al. Phase II Trial of Single-Agent Bevacizumab Followed by Bevacizumab Plus Irinotecan at Tumor Progression in Recurrent Glioblastoma. J Clin Oncol. 2009;27(5):740–5.
Raizer JJ, Grimm S, Chamberlain MC, Nicholas MK, Chandler JP, Muro K, Dubner S, Rademaker AW, Renfrow J, Bredel M. A phase 2 trial of single-agent bevacizumab given in an every-3-week schedule for patients with recurrent high-grade gliomas. Cancer. 2010;116(22):5297–305.
Gilbert MR, Dignam JJ, Armstrong TS, Wefel JS, Blumenthal DT, Vogelbaum MA, Colman H, Chakravarti A, Pugh S, Won M, et al. A randomized trial of bevacizumab for newly diagnosed glioblastoma. N Engl J Med. 2014;370(8):699–708.
Chinot OL, Wick W, Mason W, Henriksson R, Saran F, Nishikawa R, Carpentier AF, Hoang-Xuan K, Kavan P, Cernea D, et al. Bevacizumab plus radiotherapy-temozolomide for newly diagnosed glioblastoma. N Engl J Med. 2014;370(8):709–22.
Sandmann T, Bourgon R, Garcia J, Li C, Cloughesy T, Chinot OL, Wick W, Nishikawa R, Mason W, Henriksson R, et al. Patients With Proneural Glioblastoma May Derive Overall Survival Benefit From the Addition of Bevacizumab to First-Line Radiotherapy and Temozolomide: Retrospective Analysis of the AVAglio Trial. J Clin Oncol. 2015;33(25):2735–44.
Lee EQ, Muzikansky A, Duda DG, Gaffey S, Dietrich J, Nayak L, Chukwueke UN, Beroukhim R, Doherty L, Laub CK, et al. Phase II trial of ponatinib in patients with bevacizumab-refractory glioblastoma. Cancer Med. 2019;8(13):5988–94.
Scott BJ, Quant EC, McNamara MB, Ryg PA, Batchelor TT, Wen PY. Bevacizumab salvage therapy following progression in high-grade glioma patients treated with VEGF receptor tyrosine kinase inhibitors. Neuro Oncol. 2010;12(6):603–7.
Lallemand C, Ferrando-Miguel R, Auer M, Iglseder S, Czech T, Gaber-Wagener A, Di Pauli F, Deisenhammer F, Tovey MG. Quantification of Bevacizumab Activity Following Treatment of Patients With Ovarian Cancer or Glioblastoma. Front Immunol. 2020;11:515556.
Gilbert MR, Pugh SL, Aldape K, Sorensen AG, Mikkelsen T, Penas-Prado M, Bokstein F, Kwok Y, Lee RJ, Mehta M. NRG oncology RTOG 0625: a randomized phase II trial of bevacizumab with either irinotecan or dose-dense temozolomide in recurrent glioblastoma. J Neurooncol. 2017;131(1):193–9.
Lee EQ, Zhang P, Wen PY, Gerstner ER, Reardon DA, Aldape KD, deGroot JF, Pan E, Raizer JJ, Kim LJ, et al. NRG/RTOG 1122: A phase 2, double-blinded, placebo-controlled study of bevacizumab with and without trebananib in patients with recurrent glioblastoma or gliosarcoma. Cancer. 2020;126(12):2821–8.
Reardon DA, Lassman AB, Schiff D, Yunus SA, Gerstner ER, Cloughesy TF, Lee EQ, Gaffey SC, Barrs J, Bruno J, et al. Phase 2 and biomarker study of trebananib, an angiopoietin-blocking peptibody, with and without bevacizumab for patients with recurrent glioblastoma. Cancer. 2018;124(7):1438–48.
Sathornsumetee S, Desjardins A, Vredenburgh JJ, McLendon RE, Marcello J, Herndon JE, Mathe A, Hamilton M, Rich JN, Norfleet JA, et al. Phase II trial of bevacizumab and erlotinib in patients with recurrent malignant glioma. Neuro Oncol. 2010;12(12):1300–10.
Reardon DA, Desjardins A, Vredenburgh JJ, Gururangan S, Sampson JH, Sathornsumetee S, McLendon RE, Herndon JE 2nd, Marcello JE, Norfleet J, et al. Metronomic chemotherapy with daily, oral etoposide plus bevacizumab for recurrent malignant glioma: a phase II study. Br J Cancer. 2009;101(12):1986–94.
Weathers SP, Han X, Liu DD, Conrad CA, Gilbert MR, Loghin ME, O’Brien BJ, Penas-Prado M, Puduvalli VK, Tremont-Lukats I, et al. A randomized phase II trial of standard dose bevacizumab versus low dose bevacizumab plus lomustine (CCNU) in adults with recurrent glioblastoma. J Neurooncol. 2016;129(3):487–94.
Erdem-Eraslan L, van den Bent MJ, Hoogstrate Y, Naz-Khan H, Stubbs A, van der Spek P, Böttcher R, Gao Y, de Wit M, Taal W, et al. Identification of Patients with Recurrent Glioblastoma Who May Benefit from Combined Bevacizumab and CCNU Therapy: A Report from the BELOB Trial. Cancer Res. 2016;76(3):525–34.
Affronti ML, Jackman JG, McSherry F, Herndon JE 2nd, Massey EC Jr, Lipp E, Desjardins A, Friedman HS, Vlahovic G, Vredenburgh J, et al. Phase II Study to Evaluate the Efficacy and Safety of Rilotumumab and Bevacizumab in Subjects with Recurrent Malignant Glioma. Oncologist. 2018;23(8):889-e898.
D’Alessandris QG, Montano N, Cenci T, Martini M, Lauretti L, Bianchi F, Larocca LM, Maira G, Fernandez E, Pallini R. Targeted therapy with bevacizumab and erlotinib tailored to the molecular profile of patients with recurrent glioblastoma. Preliminary experience Acta Neurochir (Wien). 2013;155(1):33–40.
Batchelor TT, Duda DG, di Tomaso E, Ancukiewicz M, Plotkin SR, Gerstner E, Eichler AF, Drappatz J, Hochberg FH, Benner T, et al. Phase II study of cediranib, an oral pan-vascular endothelial growth factor receptor tyrosine kinase inhibitor, in patients with recurrent glioblastoma. J Clin Oncol. 2010;28(17):2817–23.
Batchelor TT, Gerstner ER, Emblem KE, Duda DG, Kalpathy-Cramer J, Snuderl M, Ancukiewicz M, Polaskova P, Pinho MC, Jennings D, et al. Improved tumor oxygenation and survival in glioblastoma patients who show increased blood perfusion after cediranib and chemoradiation. Proc Natl Acad Sci U S A. 2013;110(47):19059–64.
Batchelor TT, Sorensen AG, di Tomaso E, Zhang WT, Duda DG, Cohen KS, Kozak KR, Cahill DP, Chen PJ, Zhu M, et al. AZD2171, a pan-VEGF receptor tyrosine kinase inhibitor, normalizes tumor vasculature and alleviates edema in glioblastoma patients. Cancer Cell. 2007;11(1):83–95.
Batchelor TT, Mulholland P, Neyns B, Nabors LB, Campone M, Wick A, Mason W, Mikkelsen T, Phuphanich S, Ashby LS, et al. Phase III randomized trial comparing the efficacy of cediranib as monotherapy, and in combination with lomustine, versus lomustine alone in patients with recurrent glioblastoma. J Clin Oncol. 2013;31(26):3212–8.
Iwamoto FM, Lamborn KR, Robins HI, Mehta MP, Chang SM, Butowski NA, Deangelis LM, Abrey LE, Zhang WT, Prados MD, et al. Phase II trial of pazopanib (GW786034), an oral multi-targeted angiogenesis inhibitor, for adults with recurrent glioblastoma (North American Brain Tumor Consortium Study 06–02). Neuro Oncol. 2010;12(8):855–61.
Kalpathy-Cramer J, Chandra V, Da X, Ou Y, Emblem KE, Muzikansky A, Cai X, Douw L, Evans JG, Dietrich J, et al. Phase II study of tivozanib, an oral VEGFR inhibitor, in patients with recurrent glioblastoma. J Neurooncol. 2017;131(3):603–10.
Reardon DA, Groves MD, Wen PY, Nabors L, Mikkelsen T, Rosenfeld S, Raizer J, Barriuso J, McLendon RE, Suttle AB, et al. A phase I/II trial of pazopanib in combination with lapatinib in adult patients with relapsed malignant glioma. Clin Cancer Res. 2013;19(4):900–8.
Nayak L, de Groot J, Wefel JS, Cloughesy TF, Lieberman F, Chang SM, Omuro A, Drappatz J, Batchelor TT, DeAngelis LM, et al. Phase I trial of aflibercept (VEGF trap) with radiation therapy and concomitant and adjuvant temozolomide in patients with high-grade gliomas. J Neurooncol. 2017;132(1):181–8.
de Groot JF, Lamborn KR, Chang SM, Gilbert MR, Cloughesy TF, Aldape K, Yao J, Jackson EF, Lieberman F, Robins HI, et al. Phase II study of aflibercept in recurrent malignant glioma: a North American Brain Tumor Consortium study. J Clin Oncol. 2011;29(19):2689–95.
Du Four S, Maenhout SK, Benteyn D, De Keersmaecker B, Duerinck J, Thielemans K, Neyns B, Aerts JL. Disease progression in recurrent glioblastoma patients treated with the VEGFR inhibitor axitinib is associated with increased regulatory T cell numbers and T cell exhaustion. Cancer Immunol Immunother. 2016;65(6):727–40.
de Groot JF, Piao Y, Tran H, Gilbert M, Wu HK, Liu J, Bekele BN, Cloughesy T, Mehta M, Robins HI, et al. Myeloid biomarkers associated with glioblastoma response to anti-VEGF therapy with aflibercept. Clin Cancer Res. 2011;17(14):4872–81.
Schnell O, Krebs B, Carlsen J, Miederer I, Goetz C, Goldbrunner RH, Wester HJ, Haubner R, Pöpperl G, Holtmannspötter M, et al. Imaging of integrin alpha(v)beta(3) expression in patients with malignant glioma by [18F] Galacto-RGD positron emission tomography. Neuro Oncol. 2009;11(6):861–70.
Mikkelsen T, Brodie C, Finniss S, Berens ME, Rennert JL, Nelson K, Lemke N, Brown SL, Hahn D, Neuteboom B, et al. Radiation sensitization of glioblastoma by cilengitide has unanticipated schedule-dependency. Int J Cancer. 2009;124(11):2719–27.
Gerstner ER, Ye X, Duda DG, Levine MA, Mikkelsen T, Kaley TJ, Olson JJ, Nabors BL, Ahluwalia MS, Wen PY, et al. A phase I study of cediranib in combination with cilengitide in patients with recurrent glioblastoma. Neuro Oncol. 2015;17(10):1386–92.
Gilbert MR, Kuhn J, Lamborn KR, Lieberman F, Wen PY, Mehta M, Cloughesy T, Lassman AB, Deangelis LM, Chang S, et al. Cilengitide in patients with recurrent glioblastoma: the results of NABTC 03–02, a phase II trial with measures of treatment delivery. J Neurooncol. 2012;106(1):147–53.
Reardon DA, Fink KL, Mikkelsen T, Cloughesy TF, O’Neill A, Plotkin S, Glantz M, Ravin P, Raizer JJ, Rich KM, et al. Randomized phase II study of cilengitide, an integrin-targeting arginine-glycine-aspartic acid peptide, in recurrent glioblastoma multiforme. J Clin Oncol. 2008;26(34):5610–7.
Eisele G, Wick A, Eisele AC, Clément PM, Tonn J, Tabatabai G, Ochsenbein A, Schlegel U, Neyns B, Krex D, et al. Cilengitide treatment of newly diagnosed glioblastoma patients does not alter patterns of progression. J Neurooncol. 2014;117(1):141–5.
Nabors LB, Fink KL, Mikkelsen T, Grujicic D, Tarnawski R, Nam DH, Mazurkiewicz M, Salacz M, Ashby L, Zagonel V, et al. Two cilengitide regimens in combination with standard treatment for patients with newly diagnosed glioblastoma and unmethylated MGMT gene promoter: results of the open-label, controlled, randomized phase II CORE study. Neuro Oncol. 2015;17(5):708–17.
Stupp R, Hegi ME, Neyns B, Goldbrunner R, Schlegel U, Clement PM, Grabenbauer GG, Ochsenbein AF, Simon M, Dietrich PY, et al. Phase I/IIa study of cilengitide and temozolomide with concomitant radiotherapy followed by cilengitide and temozolomide maintenance therapy in patients with newly diagnosed glioblastoma. J Clin Oncol. 2010;28(16):2712–8.
Weller M, Nabors LB, Gorlia T, Leske H, Rushing E, Bady P, Hicking C, Perry J, Hong YK, Roth P, et al. Cilengitide in newly diagnosed glioblastoma: biomarker expression and outcome. Oncotarget. 2016;7(12):15018–32.
Khasraw M, Lee A, McCowatt S, Kerestes Z, Buyse ME, Back M, Kichenadasse G, Ackland S, Wheeler H. Cilengitide with metronomic temozolomide, procarbazine, and standard radiotherapy in patients with glioblastoma and unmethylated MGMT gene promoter in ExCentric, an open-label phase II trial. J Neurooncol. 2016;128(1):163–71.
MacDonald TJ, Stewart CF, Kocak M, Goldman S, Ellenbogen RG, Phillips P, Lafond D, Poussaint TY, Kieran MW, Boyett JM, et al. Phase I clinical trial of cilengitide in children with refractory brain tumors: Pediatric Brain Tumor Consortium Study PBTC-012. J Clin Oncol. 2008;26(6):919–24.
MacDonald TJ, Vezina G, Stewart CF, Turner D, Pierson CR, Chen L, Pollack IF, Gajjar A, Kieran MW. Phase II study of cilengitide in the treatment of refractory or relapsed high-grade gliomas in children: a report from the Children’s Oncology Group. Neuro Oncol. 2013;15(10):1438–44.
Stupp R, Hegi ME, Gorlia T, Erridge SC, Perry J, Hong YK, Aldape KD, Lhermitte B, Pietsch T, Grujicic D, et al. Cilengitide combined with standard treatment for patients with newly diagnosed glioblastoma with methylated MGMT promoter (CENTRIC EORTC 26071–22072 study): a multicentre, randomised, open-label, phase 3 trial. Lancet Oncol. 2014;15(10):1100–8.
Massagué J. TGFbeta in Cancer. Cell. 2008;134(2):215–30.
Chen W, Ten Dijke P. Immunoregulation by members of the TGFβ superfamily. Nat Rev Immunol. 2016;16(12):723–40.
Kuppner MC, Hamou MF, Bodmer S, Fontana A, de Tribolet N. The glioblastoma-derived T-cell suppressor factor/transforming growth factor beta 2 inhibits the generation of lymphokine-activated killer (LAK) cells. Int J Cancer. 1988;42(4):562–7.
Brandes AA, Carpentier AF, Kesari S, Sepulveda-Sanchez JM, Wheeler HR, Chinot O, Cher L, Steinbach JP, Capper D, Specenier P, et al. A Phase II randomized study of galunisertib monotherapy or galunisertib plus lomustine compared with lomustine monotherapy in patients with recurrent glioblastoma. Neuro Oncol. 2016;18(8):1146–56.
Bogdahn U, Hau P, Stockhammer G, Venkataramana NK, Mahapatra AK, Suri A, Balasubramaniam A, Nair S, Oliushine V, Parfenov V, et al. Targeted therapy for high-grade glioma with the TGF-β2 inhibitor trabedersen: results of a randomized and controlled phase IIb study. Neuro Oncol. 2011;13(1):132–42.
Papachristodoulou A, Silginer M, Weller M, Schneider H, Hasenbach K, Janicot M, Roth P. Therapeutic Targeting of TGF beta Ligands in Glioblastoma Using Novel Antisense Oligonucleotides Reduces the Growth of Experimental Gliomas. Clin Cancer Res. 2019;25(23):7189–201.
Andreou T, Williams J, Brownlie RJ, Salmond RJ, Watson E, Shaw G, Melcher A, Wurdak H, Short SC, Lorger M. Hematopoietic stem cell gene therapy targeting TGFβ enhances the efficacy of irradiation therapy in a preclinical glioblastoma model. Journal for ImmunoTherapy of Cancer. 2021;9(3):e001143.
Nie E, Jin X, Miao F, Yu T, Zhi T, Shi Z, Wang Y, Zhang J, Xie M, You Y. TGF-β1 modulates temozolomide resistance in glioblastoma via altered microRNA processing and elevated MGMT. Neuro Oncol. 2021;23(3):435–46.
Blumenthal DT, Yalon M, Vainer GW, Lossos A, Yust S, Tzach L, Cagnano E, Limon D, Bokstein F. Pembrolizumab: first experience with recurrent primary central nervous system (CNS) tumors. J Neurooncol. 2016;129(3):453–60.
Bouffet E, Larouche V, Campbell BB, Merico D, de Borja R, Aronson M, Durno C, Krueger J, Cabric V, Ramaswamy V, et al. Immune Checkpoint Inhibition for Hypermutant Glioblastoma Multiforme Resulting From Germline Biallelic Mismatch Repair Deficiency. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2016;34(19):2206–11.
Johanns TM, Miller CA, Dorward IG, Tsien C, Chang E, Perry A, Uppaluri R, Ferguson C, Schmidt RE, Dahiya S, et al. Immunogenomics of Hypermutated Glioblastoma: A Patient with Germline POLE Deficiency Treated with Checkpoint Blockade Immunotherapy. Cancer Discov. 2016;6(11):1230–6.
Lukas RV, Rodon J, Becker K, Wong ET, Shih K, Touat M, Fassò M, Osborne S, Molinero L, O’Hear C, et al. Clinical activity and safety of atezolizumab in patients with recurrent glioblastoma. J Neurooncol. 2018;140(2):317–28.
Zhang H, Dai Z, Wu W, Wang Z, Zhang N, Zhang L, Zeng WJ, Liu Z, Cheng Q. Regulatory mechanisms of immune checkpoints PD-L1 and CTLA-4 in cancer. J Exp Clin Cancer Res. 2021;40(1):184.
Wu W, Liu Y, Zeng S, Han Y, Shen H. Intratumor heterogeneity: the hidden barrier to immunotherapy against MSI tumors from the perspective of IFN-gamma signaling and tumor-infiltrating lymphocytes. J Hematol Oncol. 2021;14(1):160.
Zhang H, Dai Z, Wu W, Wang Z, Zhang N, Zhang L, Zeng W-J, Liu Z, Cheng Q. Regulatory mechanisms of immune checkpoints PD-L1 and CTLA-4 in cancer. Journal of experimental & clinical cancer research : CR. 2021;40(1):184.
Cloughesy TF, Mochizuki AY, Orpilla JR, Hugo W, Lee AH, Davidson TB, Wang AC, Ellingson BM, Rytlewski JA, Sanders CM, et al. Neoadjuvant anti-PD-1 immunotherapy promotes a survival benefit with intratumoral and systemic immune responses in recurrent glioblastoma. Nat Med. 2019;25(3):477–86.
Reardon DA, Brandes AA, Omuro A, Mulholland P, Lim M, Wick A, Baehring J, Ahluwalia MS, Roth P, Bähr O, et al. Effect of Nivolumab vs Bevacizumab in Patients With Recurrent Glioblastoma: The CheckMate 143 Phase 3 Randomized Clinical Trial. JAMA Oncol. 2020;6(7):1003–10.
Karachi A, Yang C, Dastmalchi F, Sayour EJ, Huang J, Azari H, Long Y, Flores C, Mitchell DA, Rahman M. Modulation of temozolomide dose differentially affects T-cell response to immune checkpoint inhibition. Neuro Oncol. 2019;21(6):730–41.
Schalper KA, Rodriguez-Ruiz ME, Diez-Valle R, López-Janeiro A, Porciuncula A, Idoate MA, Inogés S, de Andrea C, de Cerio López-Diaz A, Tejada S, et al. Neoadjuvant nivolumab modifies the tumor immune microenvironment in resectable glioblastoma. Nature Medicine. 2019;25(3):470–6.
Workman CJ, Rice DS, Dugger KJ, Kurschner C, Vignali DAA. Phenotypic analysis of the murine CD4-related glycoprotein, CD223 (LAG-3). Eur J Immunol. 2002;32(8):2255–63.
Triebel F, Jitsukawa S, Baixeras E, Roman-Roman S, Genevee C, Viegas-Pequignot E, Hercend T. LAG-3, a novel lymphocyte activation gene closely related to CD4. J Exp Med. 1990;171(5):1393–405.
Maruhashi T, Sugiura D, Okazaki I-M, Okazaki T: LAG-3: from molecular functions to clinical applications. Journal for immunotherapy of cancer 2020, 8(2).
Harris-Bookman S, Mathios D, Martin AM, Xia Y, Kim E, Xu H, Belcaid Z, Polanczyk M, Barberi T, Theodros D, et al. Expression of LAG-3 and efficacy of combination treatment with anti-LAG-3 and anti-PD-1 monoclonal antibodies in glioblastoma. Int J Cancer. 2018;143(12):3201–8.
Mair MJ, Kiesel B, Feldmann K, Widhalm G, Dieckmann K, Wöhrer A, Müllauer L, Preusser M, Berghoff AS. LAG-3 expression in the inflammatory microenvironment of glioma. J Neurooncol. 2021;152(3):533–9.
Panda A, Rosenfeld JA, Singer EA, Bhanot G, Ganesan S. Genomic and immunologic correlates of LAG-3 expression in cancer. Oncoimmunology. 2020;9(1):1756116.
Egen JG, Kuhns MS, Allison JP. CTLA-4: new insights into its biological function and use in tumor immunotherapy. Nat Immunol. 2002;3(7):611–8.
Rowshanravan B, Halliday N, Sansom DM. CTLA-4: a moving target in immunotherapy. Blood. 2018;131(1):58–67.
Duerinck J, Schwarze JK, Awada G, Tijtgat J, Vaeyens F, Bertels C, Geens W, Klein S, Seynaeve L, Cras L, et al. Intracerebral administration of CTLA-4 and PD-1 immune checkpoint blocking monoclonal antibodies in patients with recurrent glioblastoma: a phase I clinical trial. J Immunother Cancer. 2021;9(6).
Wainwright DA, Chang AL, Dey M, Balyasnikova IV, Kim CK, Tobias A, Cheng Y, Kim JW, Qiao J, Zhang L, et al. Durable therapeutic efficacy utilizing combinatorial blockade against IDO, CTLA-4, and PD-L1 in mice with brain tumors. Clin Cancer Res. 2014;20(20):5290–301.
Brown NF, Ng SM, Brooks C, Coutts T, Holmes J, Roberts C, Elhussein L, Hoskin P, Maughan T, Blagden S, et al. A phase II open label, randomised study of ipilimumab with temozolomide versus temozolomide alone after surgery and chemoradiotherapy in patients with recently diagnosed glioblastoma: the Ipi-Glio trial protocol. BMC Cancer. 2020;20(1):198.
Vom Berg J, Vrohlings M, Haller S, Haimovici A, Kulig P, Sledzinska A, Weller M, Becher B. Intratumoral IL-12 combined with CTLA-4 blockade elicits T cell-mediated glioma rejection. J Exp Med. 2013;210(13):2803–11.
Curry WT, Gorrepati R, Piesche M, Sasada T, Agarwalla P, Jones PS, Gerstner ER, Golby AJ, Batchelor TT, Wen PY, et al. Vaccination with Irradiated Autologous Tumor Cells Mixed with Irradiated GM-K562 Cells Stimulates Antitumor Immunity and T Lymphocyte Activation in Patients with Recurrent Malignant Glioma. Clinical cancer research : an official journal of the American Association for Cancer Research. 2016;22(12):2885–96.
Resta R, Yamashita Y, Thompson LF: Ecto-enzyme and signaling functions of lymphocyte CD73. Immunological reviews 1998, 161.
Allard B, Pommey S, Smyth MJ, Stagg J. Targeting CD73 enhances the antitumor activity of anti-PD-1 and anti-CTLA-4 mAbs. Clinical cancer research : an official journal of the American Association for Cancer Research. 2013;19(20):5626–35.
Quezada C, Garrido W, Oyarzún C, Fernández K, Segura R, Melo R, Casanello P, Sobrevia L, San Martín R. 5’-ectonucleotidase mediates multiple-drug resistance in glioblastoma multiforme cells. J Cell Physiol. 2013;228(3):602–8.
Azambuja JH, Schuh RS, Michels LR, Gelsleichter NE, Beckenkamp LR, Iser IC, Lenz GS, de Oliveira FH, Venturin G, Greggio S, et al. Nasal Administration of Cationic Nanoemulsions as CD73-siRNA Delivery System for Glioblastoma Treatment: a New Therapeutical Approach. Mol Neurobiol. 2020;57(2):635–49.
Azambuja JH, Schuh RS, Michels LR, Iser IC, Beckenkamp LR, Roliano GG, Lenz GS, Scholl JN, Sévigny J, Wink MR, et al. Blockade of CD73 delays glioblastoma growth by modulating the immune environment. Cancer Immunol Immunother. 2020;69(9):1801–12.
Goswami S, Walle T, Cornish AE, Basu S, Anandhan S, Fernandez I, Vence L, Blando J, Zhao H, Yadav SS, et al. Immune profiling of human tumors identifies CD73 as a combinatorial target in glioblastoma. Nat Med. 2020;26(1):39–46.
Lawson KV, Kalisiak J, Lindsey EA, Newcomb ET, Leleti MR, Debien L, Rosen BR, Miles DH, Sharif EU, Jeffrey JL, et al. Discovery of AB680: A Potent and Selective Inhibitor of CD73. J Med Chem. 2020;63(20):11448–68.
Zhou X, Du J, Liu C, Zeng H, Chen Y, Liu L, Wu D. A Pan-Cancer Analysis of CD161 a Potential New Immune Checkpoint. Frontiers in immunology. 2021;12:688215.
Mathewson ND, Ashenberg O, Tirosh I, Gritsch S, Perez EM, Marx S, Jerby-Arnon L, Chanoch-Myers R, Hara T, Richman AR, et al. Inhibitory CD161 receptor identified in glioma-infiltrating T cells by single-cell analysis. Cell. 2021;184(5):1281-1298.e1226.
Konduri V, Oyewole-Said D, Vazquez-Perez J, Weldon SA, Halpert MM, Levitt JM, Decker WK. CD8(+)CD161(+) T-Cells: Cytotoxic Memory Cells With High Therapeutic Potential. Front Immunol. 2021;11:613204–613204.
Roth P, Mittelbronn M, Wick W, Meyermann R, Tatagiba M, Weller M. Malignant glioma cells counteract antitumor immune responses through expression of lectin-like transcript-1. Can Res. 2007;67(8):3540–4.
Uyttenhove C, Pilotte L, Théate I, Stroobant V, Colau D, Parmentier N, Boon T, Van den Eynde BJ. Evidence for a tumoral immune resistance mechanism based on tryptophan degradation by indoleamine 2,3-dioxygenase. Nat Med. 2003;9(10):1269–74.
Zhai L, Ladomersky E, Lenzen A, Nguyen B, Patel R, Lauing KL, Wu M, Wainwright DA. IDO1 in cancer: a Gemini of immune checkpoints. Cell Mol Immunol. 2018;15(5):447–57.
Munn DH, Zhou M, Attwood JT, Bondarev I, Conway SJ, Marshall B, Brown C, Mellor AL. Prevention of allogeneic fetal rejection by tryptophan catabolism. Science (New York, NY). 1998;281(5380):1191–3.
Du L, Xing Z, Tao B, Li T, Yang D, Li W, Zheng Y, Kuang C, Yang Q. Both IDO1 and TDO contribute to the malignancy of gliomas via the Kyn-AhR-AQP4 signaling pathway. Signal Transduct Target Ther. 2020;5(1):10.
Hanihara M, Kawataki T, Oh-Oka K, Mitsuka K, Nakao A, Kinouchi H. Synergistic antitumor effect with indoleamine 2,3-dioxygenase inhibition and temozolomide in a murine glioma model. J Neurosurg. 2016;124(6):1594–601.
Ladomersky E, Zhai L, Lenzen A, Lauing KL, Qian J, Scholtens DM, Gritsina G, Sun X, Liu Y, Yu F, et al. IDO1 Inhibition Synergizes with Radiation and PD-1 Blockade to Durably Increase Survival Against Advanced Glioblastoma. Clinical cancer research : an official journal of the American Association for Cancer Research. 2018;24(11):2559–73.
Ladomersky E, Zhai L, Lauing KL, Bell A, Xu J, Kocherginsky M, Zhang B, Wu JD, Podojil JR, Platanias LC, et al. Advanced Age Increases Immunosuppression in the Brain and Decreases Immunotherapeutic Efficacy in Subjects with Glioblastoma. Clinical cancer research : an official journal of the American Association for Cancer Research. 2020;26(19):5232–45.
Zhai L, Bell A, Ladomersky E, Lauing KL, Bollu L, Sosman JA, Zhang B, Wu JD, Miller SD, Meeks JJ, et al. Immunosuppressive IDO in Cancer: Mechanisms of Action, Animal Models, and Targeting Strategies. Front Immunol. 2020;11:1185.
Zhai L, Bell A, Ladomersky E, Lauing KL, Bollu L, Nguyen B, Genet M, Kim M, Chen P, Mi X, et al. Tumor cell IDO enhances immune suppression and decreases survival independent of tryptophan metabolism in glioblastoma. Clinical cancer research : an official journal of the American Association for Cancer Research. 2021;27(23):6514–28.
Monney L, Sabatos CA, Gaglia JL, Ryu A, Waldner H, Chernova T, Manning S, Greenfield EA, Coyle AJ, Sobel RA, et al. Th1-specific cell surface protein Tim-3 regulates macrophage activation and severity of an autoimmune disease. Nature. 2002;415(6871):536–41.
Wolf Y, Anderson AC, Kuchroo VK. TIM3 comes of age as an inhibitory receptor. Nat Rev Immunol. 2020;20(3):173–85.
Sabatos-Peyton CA, Nevin J, Brock A, Venable JD, Tan DJ, Kassam N, Xu F, Taraszka J, Wesemann L, Pertel T, et al. Blockade of Tim-3 binding to phosphatidylserine and CEACAM1 is a shared feature of anti-Tim-3 antibodies that have functional efficacy. Oncoimmunology. 2018;7(2):e1385690.
Li G, Wang Z, Zhang C, Liu X, Cai J, Wang Z, Hu H, Wu F, Bao Z, Liu Y, et al. Molecular and clinical characterization of TIM-3 in glioma through 1,024 samples. Oncoimmunology. 2017;6(8):e1328339.
Das M, Zhu C, Kuchroo VK. Tim-3 and its role in regulating anti-tumor immunity. Immunological reviews. 2017;276(1):97–111.
Kim JE, Patel MA, Mangraviti A, Kim ES, Theodros D, Velarde E, Liu A, Sankey EW, Tam A, Xu H, et al. Combination Therapy with Anti-PD-1, Anti-TIM-3, and Focal Radiation Results in Regression of Murine Gliomas. Clin Cancer Res. 2017;23(1):124–36.
Sica GL, Choi IH, Zhu G, Tamada K, Wang SD, Tamura H, Chapoval AI, Flies DB, Bajorath J, Chen L. B7–H4, a molecule of the B7 family, negatively regulates T cell immunity. Immunity. 2003;18(6):849–61.
Podojil JR, Miller SD. Potential targeting of B7–H4 for the treatment of cancer. Immunol Rev. 2017;276(1):40–51.
Yao Y, Wang X, Jin K, Zhu J, Wang Y, Xiong S, Mao Y, Zhou L. B7–H4 is preferentially expressed in non-dividing brain tumor cells and in a subset of brain tumor stem-like cells. J Neurooncol. 2008;89(2):121–9.
Mo LJ, Ye HX, Mao Y, Yao Y, Zhang JM. B7–H4 expression is elevated in human U251 glioma stem-like cells and is inducible in monocytes cultured with U251 stem-like cell conditioned medium. Chin J Cancer. 2013;32(12):653–60.
Chen D, Li G, Ji C, Lu Q, Qi Y, Tang C, Xiong J, Hu J, Yasar FBA, Zhang Y et al: Enhanced B7-H4 expression in gliomas with low PD-L1 expression identifies super-cold tumors. Journal for immunotherapy of cancer 2020, 8(1).
Wang L, Rubinstein R, Lines JL, Wasiuk A, Ahonen C, Guo Y, Lu L-F, Gondek D, Wang Y, Fava RA, et al. VISTA, a novel mouse Ig superfamily ligand that negatively regulates T cell responses. J Exp Med. 2011;208(3):577–92.
Huang X, Zhang X, Li E, Zhang G, Wang X, Tang T, Bai X, Liang T. VISTA: an immune regulatory protein checking tumor and immune cells in cancer immunotherapy. J Hematol Oncol. 2020;13(1):83.
Flies DB, Han X, Higuchi T, Zheng L, Sun J, Ye JJ, Chen L. Coinhibitory receptor PD-1H preferentially suppresses CD4+ T cell-mediated immunity. J Clin Investig. 2014;124(5):1966–75.
Ghouzlani A, Rafii S, Karkouri M, Lakhdar A, Badou A. The Promising IgSF11 Immune Checkpoint Is Highly Expressed in Advanced Human Gliomas and Associates to Poor Prognosis. Frontiers in oncology. 2020;10:608609.
van Lier RA, Borst J, Vroom TM, Klein H, Van Mourik P, Zeijlemaker WP, Melief CJ. Tissue distribution and biochemical and functional properties of Tp55 (CD27), a novel T cell differentiation antigen. Journal of immunology (Baltimore, Md : 1950). 1987;139(5):1589–96.
Sugita K, Robertson MJ, Torimoto Y, Ritz J, Schlossman SF, Morimoto C. Participation of the CD27 antigen in the regulation of IL-2-activated human natural killer cells. J Immunol. 1992;149(4):1199–203.
Xiao Y, Hendriks J, Langerak P, Jacobs H, Borst J. CD27 Is Acquired by Primed B Cells at the Centroblast Stage and Promotes Germinal Center Formation. J Immunol. 2004;172(12):7432–41.
Buchan SL, Rogel A, Al-Shamkhani A. The immunobiology of CD27 and OX40 and their potential as targets for cancer immunotherapy. Blood. 2018;131(1):39–48.
Prasad KVS, Ao Z, Yoon Y, Wu MX, Rizk M, Jacquot S, Schlossman SF. CD27, a member of the tumor necrosis factor receptor family, induces apoptosis and binds to Siva, a proapoptotic protein. Proc Natl Acad Sci. 1997;94(12):6346–51.
Borst J, Hendriks J, Xiao Y. CD27 and CD70 in T cell and B cell activation. Curr Opin Immunol. 2005;17(3):275–81.
Held-Feindt J, Mentlein R. CD70/CD27 ligand, a member of the TNF family, is expressed in human brain tumors. Int J Cancer. 2002;98(3):352–6.
Wischhusen J, Jung G, Radovanovic I, Beier C, Steinbach JP, Rimner A, Huang H, Schulz JB, Ohgaki H, Aguzzi A, et al. Identification of CD70-mediated apoptosis of immune effector cells as a novel immune escape pathway of human glioblastoma. Can Res. 2002;62(9):2592–9.
Claus C, Riether C, Schürch C, Matter MS, Hilmenyuk T, Ochsenbein AF. CD27 signaling increases the frequency of regulatory T cells and promotes tumor growth. Can Res. 2012;72(14):3664–76.
Jin L, Ge H, Long Y, Yang C, Chang YE, Mu L, Sayour EJ, De Leon G, Wang QJ, Yang JC, et al. CD70, a novel target of CAR T-cell therapy for gliomas. Neuro Oncol. 2018;20(1):55–65.
Turaj AH, Hussain K, Cox KL, Rose-Zerilli MJJ, Testa J, Dahal LN, Chan HTC, James S, Field VL, Carter MJ, et al. Antibody Tumor Targeting Is Enhanced by CD27 Agonists through Myeloid Recruitment. Cancer cell. 2017;32(6):777–91.
Yang M, Tang X, Zhang Z, Gu L, Wei H, Zhao S, Zhong K, Mu M, Huang C, Jiang C, et al. Tandem CAR-T cells targeting CD70 and B7–H3 exhibit potent preclinical activity against multiple solid tumors. Theranostics. 2020;10(17):7622–34.
Gonzalez LC, Loyet KM, Calemine-Fenaux J, Chauhan V, Wranik B, Ouyang W, Eaton DL. A coreceptor interaction between the CD28 and TNF receptor family members B and T lymphocyte attenuator and herpesvirus entry mediator. Proc Natl Acad Sci USA. 2005;102(4):1116–21.
Sedy JR, Gavrieli M, Potter KG, Hurchla MA, Lindsley RC, Hildner K, Scheu S, Pfeffer K, Ware CF, Murphy TL, et al. B and T lymphocyte attenuator regulates T cell activation through interaction with herpesvirus entry mediator. Nat Immunol. 2005;6(1):90–8.
Xu X, Hou B, Fulzele A, Masubuchi T, Zhao Y, Wu Z, Hu Y, Jiang Y, Ma Y, Wang H et al: PD-1 and BTLA regulate T cell signaling differentially and only partially through SHP1 and SHP2. The Journal of cell biology 2020, 219(6).
Celis-Gutierrez J, Blattmann P, Zhai Y, Jarmuzynski N, Ruminski K, Grégoire C, Ounoughene Y, Fiore F, Aebersold R, Roncagalli R, et al. Quantitative Interactomics in Primary T Cells Provides a Rationale for Concomitant PD-1 and BTLA Coinhibitor Blockade in Cancer Immunotherapy. Cell reports. 2019;27(11):3315–30.
Choi J, Medikonda R, Saleh L, Kim T, Pant A, Srivastava S, Kim Y-H, Jackson C, Tong L, Routkevitch D, et al. Combination checkpoint therapy with anti-PD-1 and anti-BTLA results in a synergistic therapeutic effect against murine glioblastoma. Oncoimmunology. 2021;10(1):1956142.
Mostafa H, Pala A, Högel J, Hlavac M, Dietrich E, Westhoff MA, Nonnenmacher L, Burster T, Georgieff M, Wirtz CR, et al. Immune phenotypes predict survival in patients with glioblastoma multiforme. J Hematol Oncol. 2016;9(1):77.
Moesta AK, Li X-Y, Smyth MJ. Targeting CD39 in cancer. Nat Rev Immunol. 2020;20(12):739–55.
Vijayan D, Young A, Teng MWL, Smyth MJ. Targeting immunosuppressive adenosine in cancer. Nat Rev Cancer. 2017;17(12):709–24.
Mittal D, Sinha D, Barkauskas D, Young A, Kalimutho M, Stannard K, Caramia F, Haibe-Kains B, Stagg J, Khanna KK, et al. Adenosine 2B Receptor Expression on Cancer Cells Promotes Metastasis. Can Res. 2016;76(15):4372–82.
Xu S, Shao Q-Q, Sun J-T, Yang N, Xie Q, Wang D-H, Huang Q-B, Huang B, Wang X-Y, Li X-G, et al. Synergy between the ectoenzymes CD39 and CD73 contributes to adenosinergic immunosuppression in human malignant gliomas. Neuro Oncol. 2013;15(9):1160–72.
Ott M, Tomaszowski K-H, Marisetty A, Kong L-Y, Wei J, Duna M, Blumberg K, Ji X, Jacobs C, Fuller GN et al: Profiling of patients with glioma reveals the dominant immunosuppressive axis is refractory to immune function restoration. JCI insight 2020, 5(17).
Takenaka MC, Gabriely G, Rothhammer V, Mascanfroni ID, Wheeler MA, Chao C-C, Gutiérrez-Vázquez C, Kenison J, Tjon EC, Barroso A, et al. Control of tumor-associated macrophages and T cells in glioblastoma via AHR and CD39. Nat Neurosci. 2019;22(5):729–40.
Veenstra RG, Flynn R, Kreymborg K, McDonald-Hyman C, Saha A, Taylor PA, Osborn MJ, Panoskaltsis-Mortari A, Schmitt-Graeff A, Lieberknecht E, et al. B7–H3 expression in donor T cells and host cells negatively regulates acute graft-versus-host disease lethality. Blood. 2015;125(21):3335–46.
Steinberger P. B7–H3 ameliorates GVHD. Blood. 2015;125(21):3219–21.
Chapoval AI, Ni J, Lau JS, Wilcox RA, Flies DB, Liu D, Dong H, Sica GL, Zhu G, Tamada K, et al. B7–H3: a costimulatory molecule for T cell activation and IFN-gamma production. Nat Immunol. 2001;2(3):269–74.
Seaman S, Zhu Z, Saha S, Zhang XM, Yang MY, Hilton MB, Morris K, Szot C, Morris H, Swing DA, et al. Eradication of Tumors through Simultaneous Ablation of CD276/B7-H3-Positive Tumor Cells and Tumor Vasculature. Cancer cell. 2017;31(4):501–15.
Lemke D, Pfenning P-N, Sahm F, Klein A-C, Kempf T, Warnken U, Schnölzer M, Tudoran R, Weller M, Platten M, et al. Costimulatory protein 4IgB7H3 drives the malignant phenotype of glioblastoma by mediating immune escape and invasiveness. Clinical cancer research : an official journal of the American Association for Cancer Research. 2012;18(1):105–17.
Zhang J, Wang J, Marzese DM, Wang X, Yang Z, Li C, Zhang H, Zhang J, Chen CC, Kelly DF, et al. B7H3 regulates differentiation and serves as a potential biomarker and theranostic target for human glioblastoma. Lab Invest. 2019;99(8):1117–29.
Wang Z, Wang Z, Zhang C, Liu X, Li G, Liu S, Sun L, Liang J, Hu H, Liu Y, et al. Genetic and clinical characterization of B7–H3 (CD276) expression and epigenetic regulation in diffuse brain glioma. Cancer Sci. 2018;109(9):2697–705.
Nehama D, Di Ianni N, Musio S, Du H, Patané M, Pollo B, Finocchiaro G, Park JJH, Dunn DE, Edwards DS, et al. B7-H3-redirected chimeric antigen receptor T cells target glioblastoma and neurospheres. EBioMedicine. 2019;47:33–43.
Zhang M, Zhang H, Fu M, Zhang J, Zhang C, Lv Y, Fan F, Zhang J, Xu H, Ye D, et al. The Inhibition of B7H3 by 2-HG Accumulation Is Associated With Downregulation of VEGFA in IDH Mutated Gliomas. Front Cell Dev Biol. 2021;9:670145.
Kontos F, Michelakos T, Kurokawa T, Sadagopan A, Schwab JH, Ferrone CR, Ferrone S. B7–H3: An Attractive Target for Antibody-based Immunotherapy. Clinical cancer research : an official journal of the American Association for Cancer Research. 2021;27(5):1227–35.
Sun M, Richards S, Prasad DVR, Mai XM, Rudensky A, Dong C. Characterization of mouse and human B7-H3 genes. Journal of immunology (Baltimore, Md 1950). 2002;168(12):6294–7.
Leitner J, Klauser C, Pickl WF, Stöckl J, Majdic O, Bardet AF, Kreil DP, Dong C, Yamazaki T, Zlabinger G, et al. B7–H3 is a potent inhibitor of human T-cell activation: No evidence for B7–H3 and TREML2 interaction. Eur J Immunol. 2009;39(7):1754–64.
Brown E, Hooper L, Ho T, Gresham H. Integrin-associated protein: a 50-kD plasma membrane antigen physically and functionally associated with integrins. J Cell Biol. 1990;111(6 Pt 1):2785–94.
Logtenberg MEW, Scheeren FA, Schumacher TN. The CD47-SIRPα Immune Checkpoint. Immunity. 2020;52(5):742–52.
Sick E, Boukhari A, Deramaudt T, Rondé P, Bucher B, André P, Gies JP, Takeda K. Activation of CD47 receptors causes proliferation of human astrocytoma but not normal astrocytes via an Akt-dependent pathway. Glia. 2011;59(2):308–19.
Daubon T, Léon C, Clarke K, Andrique L, Salabert L, Darbo E, Pineau R, Guérit S, Maitre M, Dedieu S, et al. Deciphering the complex role of thrombospondin-1 in glioblastoma development. Nat Commun. 2019;10(1):1146.
Liu X, Wu X, Wang Y, Li Y, Chen X, Yang W, Jiang L. CD47 Promotes Human Glioblastoma Invasion Through Activation of the PI3K/Akt Pathway. Oncol Res. 2019;27(4):415–22.
Liu X, Pu Y, Cron K, Deng L, Kline J, Frazier WA, Xu H, Peng H, Fu Y-X, Xu MM. CD47 blockade triggers T cell–mediated destruction of immunogenic tumors. Nat Med. 2015;21(10):1209–15.
Tseng D, Volkmer J-P, Willingham SB, Contreras-Trujillo H, Fathman JW, Fernhoff NB, Seita J, Inlay MA, Weiskopf K, Miyanishi M, et al. Anti-CD47 antibody–mediated phagocytosis of cancer by macrophages primes an effective antitumor T-cell response. Proc Natl Acad Sci. 2013;110(27):11103–8.
Hutter G, Theruvath J, Graef CM, Zhang M, Schoen MK, Manz EM, Bennett ML, Olson A, Azad TD, Sinha R, et al. Microglia are effector cells of CD47-SIRPα antiphagocytic axis disruption against glioblastoma. Proc Natl Acad Sci U S A. 2019;116(3):997–1006.
Brown EJ, Frazier WA. Integrin-associated protein (CD47) and its ligands. Trends Cell Biol. 2001;11(3):130–5.
Uhlén M, Fagerberg L, Hallström BM, Lindskog C, Oksvold P, Mardinoglu A, Sivertsson Å, Kampf C, Sjöstedt E, Asplund A, et al. Proteomics. Tissue-based map of the human proteome. Science (New York, NY). 2015;347(6220):1260419.
Chen TT, Brown EJ, Huang EJ, Seaman WE. Expression and activation of signal regulatory protein alpha on astrocytomas. Cancer Res. 2004;64(1):117–27.
Zhang M, Hutter G, Kahn SA, Azad TD, Gholamin S, Xu CY, Liu J, Achrol AS, Richard C, Sommerkamp P, et al. Anti-CD47 Treatment Stimulates Phagocytosis of Glioblastoma by M1 and M2 Polarized Macrophages and Promotes M1 Polarized Macrophages In Vivo. PLoS One. 2016;11(4):e0153550.
Gholamin S, Mitra SS, Feroze AH, Liu J, Kahn SA, Zhang M, Esparza R, Richard C, Ramaswamy V, Remke M et al: Disrupting the CD47-SIRPα anti-phagocytic axis by a humanized anti-CD47 antibody is an efficacious treatment for malignant pediatric brain tumors. Sci Transl Med 2017, 9(381).
Li F, Lv B, Liu Y, Hua T, Han J, Sun C, Xu L, Zhang Z, Feng Z, Cai Y, et al. Blocking the CD47-SIRPα axis by delivery of anti-CD47 antibody induces antitumor effects in glioma and glioma stem cells. Oncoimmunology. 2018;7(2):e1391973.
Zhang X, Chen W, Fan J, Wang S, Xian Z, Luan J, Li Y, Wang Y, Nan Y, Luo M, et al. Disrupting CD47-SIRPα axis alone or combined with autophagy depletion for the therapy of glioblastoma. Carcinogenesis. 2018;39(5):689–99.
von Roemeling CA, Wang Y, Qie Y, Yuan H, Zhao H, Liu X, Yang Z, Yang M, Deng W, Bruno KA, et al. Therapeutic modulation of phagocytosis in glioblastoma can activate both innate and adaptive antitumour immunity. Nat Commun. 2020;11(1):1508.
Dranoff G. Cytokines in cancer pathogenesis and cancer therapy. Nat Rev Cancer. 2004;4(1):11–22.
Jacobs SK, Wilson DJ, Kornblith PL, Grimm EA. Interleukin-2 or autologous lymphokine-activated killer cell treatment of malignant glioma: phase I trial. Can Res. 1986;46(4 Pt 2):2101–4.
Holladay FP, Heitz-Turner T, Bayer WL, Wood GW. Autologous tumor cell vaccination combined with adoptive cellular immunotherapy in patients with grade III/IV astrocytoma. J Neurooncol. 1996;27(2):179–89.
Okada H, Lieberman FS, Walter KA, Lunsford LD, Kondziolka DS, Bejjani GK, Hamilton RL, Torres-Trejo A, Kalinski P, Cai Q, et al. Autologous glioma cell vaccine admixed with interleukin-4 gene transfected fibroblasts in the treatment of patients with malignant gliomas. J Transl Med. 2007;5:67.
Kunwar S, Prados MD, Chang SM, Berger MS, Lang FF, Piepmeier JM, Sampson JH, Ram Z, Gutin PH, Gibbons RD, et al. Direct intracerebral delivery of cintredekin besudotox (IL13-PE38QQR) in recurrent malignant glioma: a report by the Cintredekin Besudotox Intraparenchymal Study Group. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2007;25(7):837–44.
Kunwar S, Chang S, Westphal M, Vogelbaum M, Sampson J, Barnett G, Shaffrey M, Ram Z, Piepmeier J, Prados M, et al. Phase III randomized trial of CED of IL13-PE38QQR vs Gliadel wafers for recurrent glioblastoma. Neuro Oncol. 2010;12(8):871–81.
Groves MD, Puduvalli VK, Gilbert MR, Levin VA, Conrad CA, Liu VH, Hunter K, Meyers C, Hess KR, Alfred Yung WK. Two phase II trials of temozolomide with interferon-alpha2b (pegylated and non-pegylated) in patients with recurrent glioblastoma multiforme. Br J Cancer. 2009;101(4):615–20.
Natsume A, Ishii D, Wakabayashi T, Tsuno T, Hatano H, Mizuno M, Yoshida J. IFN-beta down-regulates the expression of DNA repair gene MGMT and sensitizes resistant glioma cells to temozolomide. Can Res. 2005;65(17):7573–9.
Natsume A, Wakabayashi T, Ishii D, Maruta H, Fujii M, Shimato S, Ito M, Yoshida J. A combination of IFN-beta and temozolomide in human glioma xenograft models: implication of p53-mediated MGMT downregulation. Cancer Chemother Pharmacol. 2008;61(4):653–9.
Wakabayashi T, Kayama T, Nishikawa R, Takahashi H, Hashimoto N, Takahashi J, Aoki T, Sugiyama K, Ogura M, Natsume A, et al. A multicenter phase I trial of combination therapy with interferon-β and temozolomide for high-grade gliomas (INTEGRA study): the final report. J Neurooncol. 2011;104(2):573–7.
Färkkilä M, Jääskeläinen J, Kallio M, Blomstedt G, Raininko R, Virkkunen P, Paetau A, Sarelin H, Mäntylä M. Randomised, controlled study of intratumoral recombinant gamma-interferon treatment in newly diagnosed glioblastoma. Br J Cancer. 1994;70(1):138–41.
Wolff JEA, Wagner S, Reinert C, Gnekow A, Kortmann RD, Kühl J, Van Gool SW. Maintenance treatment with interferon-gamma and low-dose cyclophosphamide for pediatric high-grade glioma. J Neurooncol. 2006;79(3):315–21.
Hambardzumyan D, Gutmann DH, Kettenmann H. The role of microglia and macrophages in glioma maintenance and progression. Nat Neurosci. 2016;19(1):20–7.
Singh S, Mehta N, Lilan J, Budhthoki MB, Chao F, Yong L. Initiative action of tumor-associated macrophage during tumor metastasis. Biochim Open. 2017;4:8–18.
Lee AH, Sun L, Mochizuki AY, Reynoso JG, Orpilla J, Chow F, Kienzler JC, Everson RG, Nathanson DA, Bensinger SJ, et al. Neoadjuvant PD-1 blockade induces T cell and cDC1 activation but fails to overcome the immunosuppressive tumor associated macrophages in recurrent glioblastoma. Nat Commun. 2021;12(1):6938.
Hussain SF, Yang D, Suki D, Aldape K, Grimm E, Heimberger AB. The role of human glioma-infiltrating microglia/macrophages in mediating antitumor immune responses. Neuro Oncol. 2006;8(3):261–79.
Komohara Y, Ohnishi K, Kuratsu J, Takeya M. Possible involvement of the M2 anti-inflammatory macrophage phenotype in growth of human gliomas. J Pathol. 2008;216(1):15–24.
Pyonteck SM, Akkari L, Schuhmacher AJ, Bowman RL, Sevenich L, Quail DF, Olson OC, Quick ML, Huse JT, Teijeiro V, et al. CSF-1R inhibition alters macrophage polarization and blocks glioma progression. Nat Med. 2013;19(10):1264–72.
Quail DF, Bowman RL, Akkari L, Quick ML, Schuhmacher AJ, Huse JT, Holland EC, Sutton JC, Joyce JA. The tumor microenvironment underlies acquired resistance to CSF-1R inhibition in gliomas. Science. 2016;352(6288):aad3018.
Coniglio SJ, Eugenin E, Dobrenis K, Stanley ER, West BL, Symons MH, Segall JE. Microglial stimulation of glioblastoma invasion involves epidermal growth factor receptor (EGFR) and colony stimulating factor 1 receptor (CSF-1R) signaling. Mol Med. 2012;18(1):519–27.
Cui X, Ma C, Vasudevaraja V, Serrano J, Tong J, Peng Y, Delorenzo M, Shen G, Frenster J, Morales RTT, et al. Dissecting the immunosuppressive tumor microenvironments in Glioblastoma-on-a-Chip for optimized PD-1 immunotherapy. eLife. 2020;9:e52253.
Nakagomi N, Sakamoto D, Hirose T, Takagi T, Murase M, Nakagomi T, Yoshimura S, Hirota S. Epithelioid glioblastoma with microglia features: potential for novel therapy. Brain Pathol. 2020;30(6):1119–33.
Hu F, Ku M-C, Markovic D. Dzaye ODa, Lehnardt S, Synowitz M, Wolf SA, Kettenmann H: Glioma-associated microglial MMP9 expression is upregulated by TLR2 signaling and sensitive to minocycline. Int J Cancer. 2014;135(11):2569–78.
Cohen AL, Anker CJ, Salzman K, Jensen RL, Shrleve DC, Colman H. A phase 1 study of repeat radiation, minocycline, and bevacizumab in patients with recurrent glioma (RAMBO). Journal of Clinical Oncology. 2014;32(15):2066–2066.
Gabrusiewicz K, Ellert-Miklaszewska A, Lipko M, Sielska M, Frankowska M, Kaminska B. Characteristics of the alternative phenotype of microglia/macrophages and its modulation in experimental gliomas. PLoS One. 2011;6(8):e23902.
Jacobs VL, Landry RP, Liu Y, Romero-Sandoval EA, De Leo JA. Propentofylline decreases tumor growth in a rodent model of glioblastoma multiforme by a direct mechanism on microglia. Neuro Oncol. 2012;14(2):119–31.
Eagles ME, Nassiri F, Badhiwala JH, Suppiah S, Almenawer SA, Zadeh G, Aldape KD. Dendritic cell vaccines for high-grade gliomas. Ther Clin Risk Manag. 2018;14:1299–313.
Prins RM, Wang X, Soto H, Young E, Lisiero DN, Fong B, Everson R, Yong WH, Lai A, Li G, et al. Comparison of glioma-associated antigen peptide-loaded versus autologous tumor lysate-loaded dendritic cell vaccination in malignant glioma patients. J Immunother. 2013;36(2):152–7.
Olin MR, Low W, McKenna DH, Haines SJ, Dahlheimer T, Nascene D, Gustafson MP, Dietz AB, Clark HB, Chen W, et al. Vaccination with dendritic cells loaded with allogeneic brain tumor cells for recurrent malignant brain tumors induces a CD4(+)IL17(+) response. J Immunother Cancer. 2014;2:4.
Okada H, Kalinski P, Ueda R, Hoji A, Kohanbash G, Donegan TE, Mintz AH, Engh JA, Bartlett DL, Brown CK, et al. Induction of CD8+ T-cell responses against novel glioma-associated antigen peptides and clinical activity by vaccinations with {alpha}-type 1 polarized dendritic cells and polyinosinic-polycytidylic acid stabilized by lysine and carboxymethylcellulose in patients with recurrent malignant glioma. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2011;29(3):330–6.
Phuphanich S, Wheeler CJ, Rudnick JD, Mazer M, Wang H, Nuño MA, Richardson JE, Fan X, Ji J, Chu RM, et al. Phase I trial of a multi-epitope-pulsed dendritic cell vaccine for patients with newly diagnosed glioblastoma. Cancer immunology, immunotherapy : CII. 2013;62(1):125–35.
Wen PY, Reardon DA, Phuphanich S, Aiken R, Landolfl JC, Curry WT, Zhu JJ, Glantz MJ, Peereboom DM, Markert J, et al. A randomized, double-blind, placebo-controlled phase 2 trial of dendritic cell (DC) vaccination with ICT-107 in newly diagnosed glioblastoma (GBM) patients. Journal of Clinical Oncology. 2014;32(15):2005–2005.
Wheeler CJ, Black KL, Liu G, Mazer M, Zhang X-x, Pepkowitz S, Goldfinger D, Ng H, Irvin D, Yu JS. Vaccination elicits correlated immune and clinical responses in glioblastoma multiforme patients. Can Res. 2008;68(14):5955–64.
Fadul CE, Fisher JL, Hampton TH, Lallana EC, Li Z, Gui J, Szczepiorkowski ZM, Tosteson TD, Rhodes CH, Wishart HA, et al. Immune response in patients with newly diagnosed glioblastoma multiforme treated with intranodal autologous tumor lysate-dendritic cell vaccination after radiation chemotherapy. J Immunother. 2011;34(4):382–9.
Inogés S, Tejada S, de Cerio ALD, Gállego Pérez-Larraya J, Espinós J, Idoate MA, Domínguez PD, de Eulate RG, Aristu J, Bendandi M, et al. A phase II trial of autologous dendritic cell vaccination and radiochemotherapy following fluorescence-guided surgery in newly diagnosed glioblastoma patients. J Transl Med. 2017;15(1):104.
Vik-Mo EO, Nyakas M, Mikkelsen BV, Moe MC, Due-Tønnesen P, Suso EMI, Sæbøe-Larssen S, Sandberg C, Brinchmann JE, Helseth E, et al. Therapeutic vaccination against autologous cancer stem cells with mRNA-transfected dendritic cells in patients with glioblastoma. Cancer immunology, immunotherapy : CII. 2013;62(9):1499–509.
Batich KA, Reap EA, Archer GE, Sanchez-Perez L, Nair SK, Schmittling RJ, Norberg P, Xie W, Herndon JE, Healy P, et al. Long-term Survival in Glioblastoma with Cytomegalovirus pp65-Targeted Vaccination. Clinical cancer research : an official journal of the American Association for Cancer Research. 2017;23(8):1898–909.
Reijneveld JC, Taphoorn MJB, Coens C, Bromberg JEC, Mason WP, Hoang-Xuan K, Ryan G, Hassel MB, Enting RH, Brandes AA, et al. Health-related quality of life in patients with high-risk low-grade glioma (EORTC 22033–26033): a randomised, open-label, phase 3 intergroup study. Lancet Oncol. 2016;17(11):1533–42.
Wahl M, Phillips JJ, Molinaro AM, Lin Y, Perry A, Haas-Kogan DA, Costello JF, Dayal M, Butowski N, Clarke JL, et al. Chemotherapy for adult low-grade gliomas: clinical outcomes by molecular subtype in a phase II study of adjuvant temozolomide. Neuro Oncol. 2017;19(2):242–51.
Fisher BJ, Pugh SL, Macdonald DR, Chakravatri A, Lesser GJ, Fox S, Rogers CL, Werner-Wasik M, Doyle T, Bahary JP, et al. Phase 2 Study of a Temozolomide-Based Chemoradiation Therapy Regimen for High-Risk, Low-Grade Gliomas: Long-Term Results of Radiation Therapy Oncology Group 0424. Int J Radiat Oncol Biol Phys. 2020;107(4):720–5.
Bell EH, Zhang P, Fisher BJ, Macdonald DR, McElroy JP, Lesser GJ, Fleming J, Chakraborty AR, Liu Z, Becker AP, et al. Association of MGMT Promoter Methylation Status With Survival Outcomes in Patients With High-Risk Glioma Treated With Radiotherapy and Temozolomide: An Analysis From the NRG Oncology/RTOG 0424 Trial. JAMA Oncol. 2018;4(10):1405–9.
Laack NN, Sarkaria JN, Buckner JC. Radiation Therapy Oncology Group 9802: Controversy or Consensus in the Treatment of Newly Diagnosed Low-Grade Glioma? Seminars in Radiation Oncology. 2015;25(3):197–202.
Bady P, Kurscheid S, Delorenzi M, Gorlia T, van den Bent MJ, Hoang-Xuan K, Vauléon É, Gijtenbeek A, Enting R, Thiessen B, et al. The DNA methylome of DDR genes and benefit from RT or TMZ in IDH mutant low-grade glioma treated in EORTC 22033. Acta Neuropathol. 2018;135(4):601–15.
Youssef G, Miller JJ. Lower Grade Gliomas. Current Neurology and Neuroscience Reports. 2020;20(7):1–9.
Rudà R, Pellerino A, Pace A, Carapella CM, Dealis C, Caroli M, Faedi M, Bello L, Migliore E, Marchese G, et al. Efficacy of initial temozolomide for high-risk low grade gliomas in a phase II AINO (Italian Association for Neuro-Oncology) study: a post-hoc analysis within molecular subgroups of WHO 2016. J Neurooncol. 2019;145(1):115–23.
Yalon M, Rood B, MacDonald TJ, McCowage G, Kane R, Constantini S, Packer RJ. A feasibility and efficacy study of rapamycin and erlotinib for recurrent pediatric low-grade glioma (LGG). Pediatr Blood Cancer. 2013;60(1):71–6.
Karajannis MA, Legault G, Fisher MJ, Milla SS, Cohen KJ, Wisoff JH, Harter DH, Goldberg JD, Hochman T, Merkelson A, et al. Phase II study of sorafenib in children with recurrent or progressive low-grade astrocytomas. Neuro Oncol. 2014;16(10):1408–16.
Hargrave DR, Bouffet E, Tabori U, Broniscer A, Cohen KJ, Hansford JR, Geoerger B, Hingorani P, Dunkel IJ, Russo MW, et al. Efficacy and Safety of Dabrafenib in Pediatric Patients with BRAF V600 Mutation-Positive Relapsed or Refractory Low-Grade Glioma: Results from a Phase I/IIa Study. Clin Cancer Res. 2019;25(24):7303–11.
Banerjee A, Jakacki RI, Onar-Thomas A, Wu S, Nicolaides T, Young Poussaint T, Fangusaro J, Phillips J, Perry A, Turner D, et al. A phase I trial of the MEK inhibitor selumetinib (AZD6244) in pediatric patients with recurrent or refractory low-grade glioma: a Pediatric Brain Tumor Consortium (PBTC) study. Neuro Oncol. 2017;19(8):1135–44.
Fangusaro J, Onar-Thomas A, Young Poussaint T, Wu S, Ligon AH, Lindeman N, Banerjee A, Packer RJ, Kilburn LB, Goldman S, et al. Selumetinib in paediatric patients with BRAF-aberrant or neurofibromatosis type 1-associated recurrent, refractory, or progressive low-grade glioma: a multicentre, phase 2 trial. Lancet Oncol. 2019;20(7):1011–22.
Campagne O, Yeo KK, Fangusaro J, Stewart CF. Clinical Pharmacokinetics and Pharmacodynamics of Selumetinib. Clin Pharmacokinet. 2021;60(3):283–303.
Perreault S, Larouche V, Tabori U, Hawkin C, Lippé S, Ellezam B, Décarie JC, Théoret Y, Métras M, Sultan S, et al. A phase 2 study of trametinib for patients with pediatric glioma or plexiform neurofibroma with refractory tumor and activation of the MAPK/ERK pathway: TRAM-01. BMC Cancer. 2019;19(1):1250.
Rasmussen SA, Friedman JM. NF1 Gene and Neurofibromatosis 1. Am J Epidemiol. 2000;151(1):33–40.
De Blank P, Fouladi M, Huse JT. Molecular markers and targeted therapy in pediatric low-grade glioma. J Neurooncol. 2020;150(1):5–15.
Rabab’h O, Gharaibeh A, Al-Ramadan A, Ismail M, Shah J. Pharmacological Approaches in Neurofibromatosis Type 1-Associated Nervous System Tumors. Cancers. 2021;13(15):3880.
Ater JL, Xia C, Mazewski CM, Booth TN, Freyer DR, Packer RJ, Sposto R, Vezina G, Pollack IF. Nonrandomized comparison of neurofibromatosis type 1 and non-neurofibromatosis type 1 children who received carboplatin and vincristine for progressive low-grade glioma: A report from the Children’s Oncology Group. Cancer. 2016;122(12):1928–36.
Kyi C, Roudko V, Sabado R, Saenger Y, Loging W, Mandeli J, Thin TH, Lehrer D, Donovan M, Posner M, et al. Therapeutic Immune Modulation against Solid Cancers with Intratumoral Poly-ICLC: A Pilot Trial. Clinical cancer research : an official journal of the American Association for Cancer Research. 2018;24(20):4937–48.
Ullrich NJ, Prabhu SP, Reddy AT, Fisher MJ, Packer R, Goldman S, Robison NJ, Gutmann DH, Viskochil DH, Allen JC, et al. A phase II study of continuous oral mTOR inhibitor everolimus for recurrent, radiographic-progressive neurofibromatosis type 1-associated pediatric low-grade glioma: a Neurofibromatosis Clinical Trials Consortium study. Neuro Oncol. 2020;22(10):1527–35.
Wahl M, Chang SM, Phillips JJ, Molinaro AM, Costello JF, Mazor T, Alexandrescu S, Lupo JM, Nelson SJ, Berger M, et al. Probing the phosphatidylinositol 3-kinase/mammalian target of rapamycin pathway in gliomas: A phase 2 study of everolimus for recurrent adult low-grade gliomas. Cancer. 2017;123(23):4631–9.
Parsons DW, Jones S, Zhang X, Lin JCH, Leary RJ, Angenendt P, Mankoo P, Carter H, Siu IM, Gallia GL, et al. An integrated genomic analysis of human glioblastoma multiforme. Science (New York, NY). 2008;321(5897):1807–12.
Olar A, Wani KM, Alfaro-Munoz KD, Heathcock LE, van Thuijl HF, Gilbert MR, Armstrong TS, Sulman EP, Cahill DP, Vera-Bolanos E, et al. IDH mutation status and role of WHO grade and mitotic index in overall survival in grade II-III diffuse gliomas. Acta Neuropathol. 2015;129(4):585–96.
Rohle D, Popovici-Muller J, Palaskas N, Turcan S, Grommes C, Campos C, Tsoi J, Clark O, Oldrini B, Komisopoulou E, et al. An inhibitor of mutant IDH1 delays growth and promotes differentiation of glioma cells. Science (New York, NY). 2013;340(6132):626–30.
Johannessen TCA, Mukherjee J, Viswanath P, Ohba S, Ronen SM, Bjerkvig R, Pieper RO. Rapid Conversion of Mutant IDH1 from Driver to Passenger in a Model of Human Gliomagenesis. Molecular cancer research MCR. 2016;14(10):976–83.
Martin AM, Bell WR, Yuan M, Harris L, Poore B, Arnold A, Engle EL, Asnaghi L, Lim M, Raabe EH, et al. PD-L1 Expression in Pediatric Low-Grade Gliomas Is Independent of BRAF V600E Mutational Status. J Neuropathol Exp Neurol. 2020;79(1):74–85.
Röver LK, Gevensleben H, Dietrich J, Bootz F, Landsberg J, Goltz D, Dietrich D. PD-1 (PDCD1) Promoter Methylation Is a Prognostic Factor in Patients With Diffuse Lower-Grade Gliomas Harboring Isocitrate Dehydrogenase (IDH) Mutations. EBioMedicine. 2018;28:97–104.
Jang BS, Kim IA. A radiosensitivity gene signature and PD-L1 predict the clinical outcomes of patients with lower grade glioma in TCGA. Radiother Oncol. 2018;128(2):245–53.
Berzero G, Di Stefano AL, Ronchi S, Bielle F, Villa C, Guillerm E, Capelle L, Mathon B, Laurenge A, Giry M, et al. IDH-wildtype lower-grade diffuse gliomas: the importance of histological grade and molecular assessment for prognostic stratification. Neuro Oncol. 2021;23(6):955–66.
Acknowledgements
Not applicable
Funding
This work was supported by the National Natural Science Foundation of China (NO.82073893, 82172685, 81873635, 81703622). China Postdoctoral Science Foundation (NO. 2018M633002), Hunan Provincial Natural Science Foundation of China (NO. 2018SK2101, 2018JJ3838), Hunan Provincial Health Committee Foundation of China (C2019186). Xiangya Hospital Central South University postdoctoral foundation.
Author information
Authors and Affiliations
Contributions
Keyang Yang, Zhijing Wu, Hao Zhang drafted the manuscript and prepared the figures. Keyang Yang, Zhijing Wu, Hao Zhang, Nan Zhang, Wantao Wu, Zeyu Wang, Ziyu Dai, Xun Zhang, Yun Peng, Weijie Ye, Wenjing Zeng, Liyang Zhang collected the related references and participated in discussion. Hao Zhang, Zhixiong Liu, and Quan Cheng designed this review and revised the manuscript. All authors contributed to this manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yang, K., Wu, Z., Zhang, H. et al. Glioma targeted therapy: insight into future of molecular approaches. Mol Cancer 21, 39 (2022). https://doi.org/10.1186/s12943-022-01513-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12943-022-01513-z