Abstract
Background
Inappropriate and wasteful use of health care resources is a common problem, constituting 10–34% of health services spending in the western world. Even though diagnostic imaging is vital for identifying correct diagnoses and administrating the right treatment, low-value imaging—in which the diagnostic test confers little to no clinical benefit—is common and contributes to inappropriate and wasteful use of health care resources. There is a lack of knowledge on the types and extent of low-value imaging. Accordingly, the objective of this study was to identify, characterize, and quantify the extent of low-value diagnostic imaging examinations for adults and children.
Methods
A scoping review of the published literature was performed. Medline-Ovid, Embase-Ovid, Scopus, and Cochrane Library were searched for studies published from 2010 to September 2020. The search strategy was built from medical subject headings (Mesh) for Diagnostic imaging/Radiology OR Health service misuse/Medical overuse OR Procedures and Techniques Utilization/Facilities and Services Utilization. Articles in English, German, Dutch, Swedish, Danish, or Norwegian were included.
Results
A total of 39,986 records were identified and, of these, 370 studies were included in the final synthesis. Eighty-four low-value imaging examinations were identified. Imaging of atraumatic pain, routine imaging in minor head injury, trauma, thrombosis, urolithiasis, after thoracic interventions, fracture follow-up and cancer staging/follow-up were the most frequently identified low-value imaging examinations. The proportion of low-value imaging varied between 2 and 100% inappropriate or unnecessary examinations.
Conclusions
A comprehensive list of identified low-value radiological examinations for both adults and children are presented. Future research should focus on reasons for low-value imaging utilization and interventions to reduce the use of low-value imaging internationally.
Systematic review registration: PROSPERO: CRD42020208072.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
The use of health care and health care expenditures are increasing in most countries [1]. According to the Organization for Economic Co-operation and Development (OECD) 10–34% of health service spending is inappropriate and wasteful use of health care resources [2]. Diagnostic imaging is a health care resource aiding the physician in identifying correct diagnoses and administering the right treatment for the right patient at the right time [3]. However, imaging services can also be inappropriately used or be of low clinical value. While inappropriate imaging is characterized by not being in accordance with professional norms and guidelines, low-value care is defined as services that provide little or no benefit to patients, have potential to cause harm, incur unnecessary cost to patients, or waste limited healthcare resources. Diagnostic imaging would be of low-value when the examination has little or no impact on the management of the individual patient, thus in a societal perspective increasing costs and constituting an unnecessary risk to patients due to exposure to ionizing radiation [4] and/or contrast media [5]. Earlier research found that 20–50% of radiological examinations are overused, however, this rate varies between and within countries [2, 6,7,8]. Recommendations and guidelines such as the National Institute for Health and Care Excellence’s (NICE’s) “Do-not-do list,” iRefer, iGuide and the international Choosing Wisely campaign have been introduced to reduce overutilization in health care and reduce low-value care, including diagnostic imaging [9,10,11]. So far, the impact of such efforts is reportedly low, as patient expectations of advanced diagnostic tests, lack of knowledge among health care professionals on the right use of imaging, established clinical practice, fear of malpractice, and fee-for-service reimbursement systems continue to drive the use of low-value care [6, 12,13,14,15,16]. Knowledge about low-value imaging in terms of characteristics, quantities and contexts is warranted to enable adequate prioritizing of resource utilization and designing de-implementation initiatives. A recent systematic review previously estimated the prevalence of low-value diagnostic testing, which included some radiological services, but did not provide a complete overview of which diagnostic imaging examinations that may be regarded as low-value [17]. Therefore, the objective of this scoping review was to identify, characterize, and quantify the extent of low-value diagnostic imaging examinations.
Methods
A scoping review was completed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) extension for scoping reviews [18]. The protocol for this scoping review is registered on the PROSPERO website (CRD42020208072). Medline-Ovid, Embase-Ovid, Scopus, and Cochrane Library were searched for studies published from January 2010 to September 9, 2020. The search strategy was developed in Medline-Ovid (Table 1) and adapted for the other databases with assistance/support from librarians. Terms were built from medical subject headings (Mesh) for Diagnostic imaging/Radiology OR Health service misuse/Medical overuse OR Procedures and Techniques Utilization/Facilities and Services Utilization with text word synonyms of these terms, and more specific terms not having a Mesh term. Language filters were used to include articles written in English, German, Dutch, Danish, Norwegian, and Swedish. Animal studies were excluded. The complete search strategy is available in Additional file 1.
The search was expanded through a snowballing technique of hand-searching the reference lists of articles included following full-text screening.
Selection of records
The records were archived using Thomson Reuters EndNote X9.3.3 library and duplicates were removed. All remaining records were transferred to Rayyan QCRI [19] where titles and abstracts were screened by EK, ERA, LvB-V, FC, and BMH for eligibility; 10% of citations were screened by two of the authors as quality assurance. Full-text screening was completed by EK, ERA, AMK LvB-V, LJJS and BMH after a calibration meeting for quality assurance. Disagreements with regards to inclusion or exclusion were resolved through discussion and consensus among the authors.
Eligibility criteria
The inclusion and exclusion criteria are presented in Table 2. In brief, empirical studies, including randomized controlled trials (RCTs), non-randomized controlled trials, cohort studies, descriptive qualitative studies, case studies, mixed-methods studies, and multi-methods studies assessing the value of radiological examinations for all patient groups were included.
Data extraction and synthesis
Data of the included studies were extracted using a summary table consisting of the following variables: author and year, country, design/methods, population, clinical setting, medical condition, low-value practice, reason for being low-value, alternative to low-value practice, and extent of use (when applicable). EK, ERA, AMK, and BMH extracted data after a calibration meeting where 10 publications were discussed for quality assurance. Narrative synthesis of included articles was completed. Articles were first categorized by adult or pediatric, the imaging modality, type of radiological examination evaluated, and the anatomical area imaged.
Results
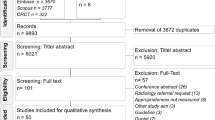
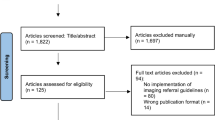
The electronic database search identified 39,986 records (findings are documented in Additional file 1) and 17,429 duplicates were removed. A total of 22,557 records were screened for titles (and abstracts) in Rayyan QCRI [19] excluding 21,907 records. Through additional searches and snowballing, 44 additional records were found, resulting in 694 articles for full-text assessment. Following full-text screening 324 articles were excluded; an overview of the excluded articles and the reason for exclusion is presented in Additional file 2. Ultimately, 370 studies were included in the final synthesis. A PRISMA flow diagram of the screening and selection process is presented in Fig. 1.
Among the 370 included studies, 84 low-value imaging examinations were identified. Studies were conducted in 35 different countries, with most from the United States (n = 215) and Europe (n = 78). In-hospital imaging was the most common clinical setting (> 65%). Fourteen different study designs were employed among the included studies; most studies were designed as retrospective chart reviews (n = 262), cohort studies (n = 39), and cross-sectional studies (n = 19). Three hundred and eight studies included adult patients, 60 studied pediatric populations, and 2 studies included both adults and children. The characteristics of the included articles are provided in Additional file 3.
Identified low-value imaging examinations
Low-value diagnostic imaging in adults was evaluated in 264 studies. Across all imaging modalities, low-value use of computed tomography (CT), magnetic resonance imaging (MRI), and X-ray were most frequently reported.
Outcomes measured for identifying low-value examinations varied across the studies and the most common were diagnostic yield (n = 213), and impact or change in treatment or management (n = 137). Importantly, the examinations defined as low-value were dependent on the clinical symptoms of patients e.g. a lumbar spine MRI is only valuable when the patient present with red flag symptoms.
In the following sections, results are stratified by body areas (neurologic (central nervous system [CNS]), thoracic, musculoskeletal, abdominopelvic, vascular, whole body, breast, cardiac, and ear, nose, and throat, and neck imaging) and population type (i.e., adult versus pediatric population).
Low-value radiological examinations in adults
Neurologic imaging
Low-value imaging of the brain was explored in 49 studies [20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66]. Specifically, routine use of head CT or repeat head CT in minor head injury and brain MRI were reported to be low-value for many clinical indications and conditions. The reason for being low-value was either low diagnostic yield where the majority of scans were reported to have no relevant findings, or a low rate in change of management for patients examined. To reduce the use of low-value neurologic imaging the studies indicated that the scan should be warranted based on patient symptoms rather than routine. Details are presented in Table 3.
Further, low-value imaging examinations of the cervical spine was identified in eleven studies [67,68,69,70,71,72,73,74,75,76,77] including routine imaging in trauma and routine follow-up after surgery in patients without symptoms (Table 4).
Thoracic imaging
Thirty-eight studies reported chest X-rays to be low-value, while four studies reported on low-value use of chest CT [78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117]. Of these, eighteen reported on chest X-rays in follow-up after procedures known to cause pneumothorax, where the X-ray did not change management in patients without symptoms [94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112]. Further, routine chest X-ray was found to not change patient management when used as a pre and post op screening, at hospital admission, in medical check-ups, or in staging of cervical and breast cancer. Repeat chest X-ray in trauma and ICU patients was found to be low-value and clinical symptoms should be used as an indicator to do an X-ray [78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93, 113, 118,119,120]. In CT, low-value examinations were found in emergency department patients, pleural effusion, and in staging of low-grade breast cancer as the diagnostic yield is low [114,115,116]. Further, repeat chest CT in Covid-19 patients showing clinical improvement was shown to be of low-value [117]. Details are presented in Table 5.
Musculoskeletal imaging
Spine and hip or pelvis
The most commonly reported low-value procedures in musculoskeletal imaging was for low back pain [121,122,123,124,125,126,127,128,129,130]. Ten studies demonstrated that X-ray, CT and MRI have a low impact on the treatment of patients without red flags, and 58.7% of MRI scans were negative [121,122,123,124,125,126,127,128,129,130,131], imaging for pain in the rest of the spine was also shown as low-value [131]. In addition, change in management were only seen in < 1% of routine post-op X-rays after cervical (c)- or lumbar (l)-spine fusion [132,133,134]. Another study found that even though 93% of the referrals for lumbar MRI were appropriate according to guidelines, only 13% of the scans showed actionable findings [125]. In cases of pelvic fracture or trauma, routine pelvic X-ray had a low impact on treatment. The same was shown for MRI or CT in pelvic ring fracture [91, 135,136,137]. In hip fracture and hemiarthroplasty, routine post-op X-ray of the hip was low-value for patients without symptoms [138, 139]. One study showed that MRI is low-value in patients with hip pain when an X-ray is already acquired [140]. Details are presented in Table 6.
Upper and lower limb
The second most common studied musculoskeletal low-value examination was MRI in knee pain without red flags, reported in eight studies [121, 141,142,143,144,145,146,147]. In addition, MRI of acute Achilles tendon rupture, X-ray of adjoined joints in ankle fracture, and CT of lower extremities stress fractures were also reported as low-value examinations [148,149,150]. X-ray of the knee changed management in 0–0.7% of patients after ligament reconstructions, tibia plateau fixation, and partial or total knee arthroplasty [151,152,153,154,155,156]. In the upper limb, shoulder MRI in patients with shoulder pain or rotator cuff tear had a low impact on treatment [157,158,159]. X-ray of the shoulder in atraumatic shoulder pain or frozen shoulder had a low impact on clinical management [160, 161]. Further, orthopedic trauma, post-op, or post-splinting X-ray gave little to no change in management [162,163,164,165,166,167,168,169]. MRI of the wrist in ligamentous injury changed the surgical plan in 28% of patients and was thus low-value for many patients [170]. On general use of imaging in the musculoskeletal system, four studies showed that skeletal CT for peri-articular fractures (post-op) [171], and long bone cartilaginous lesions (also MRI) [172] were of low-value. Details are presented in Table 7.
Abdominopelvic imaging
In abdominopelvic imaging, eighteen studies reported imaging with low-value in typical emergency or general medicine conditions [175,176,177,178,179,180,181,182,183,184,185,186,187,188,189,190,191]. X-rays for abdominal pain and upper gastrointestinal imaging (UGI) for reflux resulted in a change in management in only 4% of patients and is often of poor diagnostic quality [187,188,189]. In acute pancreatitis, < 1.2% of CT and MRI examinations yielded relevant findings [175,176,177,178]. Low-value imaging related to surgery or other invasive procedure in the abdomen was reported in seven studies [192,193,194,195,196,197,198]. Contrast esophagogram had a low impact on treatment in suspected esophageal perforation, and anastomotic leaks after esophagectomy [195, 197, 198]. In addition, staging of cancer using a different kind of MRI or CT in the abdominal/pelvic area was described as low-value in six studies for various types of cancer [199,200,201,202,203]. In urology, abdominal CT in urolithiasis had a low impact on the treatment of patients with self-limiting episodes or at follow-up [190, 204,205,206]. Renal ultrasound in new-onset acute kidney injury to screen for hydronephrosis led to changes in management in just 1.8% of patients in one study [207]. In addition, retrograde urethrography in penile fracture had a low impact on treatment in patients without hematuria or urethrorrhagia [208]. An overview of low-value imaging in abdominopelvic imaging is given in Table 8.
Vascular imaging
The two most reported low-value vascular imaging examinations were CTA of the chest in patients with low risk of pulmonary embolism (7 studies) and ultrasound in patients with low risk for deep venous thrombosis (5 studies). Negative result was demonstrated in 97% of examinations [210,211,212,213,214,215,216,217,218,219,220,221]. Further, CTA of the abdominal aorta after endovascular aneurysm repair (EVAR) in patients without endoleak 1 month after the EVAR procedure, was identified as low-value [222,223,224]. Ultrasound was reported to be better as surveillance for EVAR patients as ultrasound increased the negative predictive value to 97.6% [222,223,224]. In addition, CTA was shown to be of low-value in patients with blunt vertebral artery injuries and vascular injuries of the lower limbs [225, 226]. Details are presented in Table 9.
Whole body imaging
Whole body imaging examinations were identified as low-value in trauma and oncology in six studies. Whole body scanning in trauma should be made only when clinically indicated [227,228,229,230,231,232]. In addition, one study identified CT in soft tissue infections as low-value, with the exception of intra-abdominal abscesses [233]. In oncology, whole body imaging used for staging and follow-up was identified as low-value in 18 studies [58, 234,235,236,237,238,239,240,241,242,243,244,245,246,247,248,249,250]. Details on low-value whole body imaging in oncology is presented in Table 10.
Breast imaging
In breast cancer follow-up, mammography or MRI of the breasts less than 1-year after treatment were described as low-value [255,256,257,258,259,260,261,262]. Follow-up of benign breast tumors with short intervals showed only 0–0.5% identified malignancy in three studies, thus low-value to the majority of patients [260,261,262]. According to one study [263] on male patients only, 0.9% of breast ultrasound or mammography found malignancy. Details are presented in Table 11.
Cardiac imaging
Stress imaging such as myocardial perfusion imaging (MPI) and echocardiography were described as low-value in low risk patients, and patients with more than one risk factor for cardiac disease [264, 265]. In patients with infective endocarditis, only 10% of the findings in FDG PET/CT of the heart led to changes in treatment [266]. Routine transthoracic echocardiography in acute ischemic stroke patients had relevant findings in 38% of patients, however only 8.5% of patients had additional work-up [267]. Elective coronary angiography investigating coronary heart disease had relevant findings in 40% of patients in one study [268]. Yet another study found that during coronary angiography left ventriculography is of poor quality [269]. An overview of low-value cardiac imaging is given in Table 12.
Neck and ear, nose, and throat imaging
Post-operative thyroid cancer ultrasound was found to be low-value as 98% of the scans were negative [270] and the risk for relapse is small [271]. Furthermore, increased use of ultrasound uncovered more benign and low-risk cancers [272, 273]. Radioactive iodine scanning found 17% concordant findings with earlier examinations. Thus, fine needle aspiration should be used in diagnostics instead of imaging [274]. Thyroid ultrasound as follow-up after lobectomy found tumor or recurrence in only 1.5% of patients [275]. According to one study, in patients with secondary hyperparathyroidism routine pre-op Tc-99 m-sestamibi scans are unnecessary as nodules are found during surgery [276].
X-ray and CT of the sinuses in acute rhinosinusitis did not change patient management [277].
In patients with facial fractures, X-ray and CT was identified as low-value in five studies [278,279,280,281,282], as imaging did not change the management of the patient. One study introduced the use of ultrasound combined with an X-ray, instead of CT in zygomatic arch and mandibular fractures [281]. Another study described MRI of the face for juvenile ossifying fibroma as low-value [283].
Imaging of templar bones was described as low-value in patients with chronic Eustachian tube dysfunction and pre-op for cochlear implants [284, 285]. Details are presented in Table 13.
Low-value imaging examinations in children
The use of low-value imaging in pediatric patients was reported in 62 studies presented in Table 14 [168, 286,287,288,289,290,291,292,293,294,295,296,297,298,299,300,301,302,303,304,305,306,307,308,309,310,311,312,313,314,315,316,317,318,319,320,321,322,323,324,325,326,327,328,329,330,331,332,333,334,335,336,337,338,339,340,341,342,343,344,345]. The most frequently reported low-value examinations were CT and MRI of the head/brain, CT and X-ray related to trauma, chest X-ray, and musculoskeletal X-rays in fracture follow-up.
The quantity in use of low-value examinations
The proportion of low-value examinations varied greatly in the 103 included studies reporting proportion. Seven studies explored low-value imaging in adults on an overarching level with several medical conditions and modalities, showing an overall rate of low-value imaging of 2–31% [346,347,348,349,350,351,352].
Quantity of low-value imaging in adults
The proportion of low-value imaging examinations in specific body areas differed from 4 to 100% (86 studies], and varied both between and within different countries and clinical settings. The results are presented in Fig. 2 [20,21,22,23, 26,27,28,29, 35, 40,41,42, 54, 64, 68, 69, 122, 123, 125, 127,128,129,130, 140, 141, 143, 145,146,147, 157,158,159, 172,173,174, 176, 177, 179, 182, 190, 210, 211, 213, 215, 216, 229, 242, 252, 277, 284, 353,354,355,356,357,358,359,360,361,362,363,364,365,366,367,368,369,370,371,372,373,374,375,376,377,378,379,380,381,382,383,384,385,386,387]. From these studies, imaging examinations with a high proportion of low-value examinations (more than 50% inappropriate use reported) was: Head CT (routine and repeat), routine trauma scan, MRI in musculoskeletal pain, dual-energy x-ray absorptiometry (DEXA) in low risk patients or low interval DEXA follow-ups, echocardiography, carotid imaging, chest X-ray, X-ray in acute rhinosinusitis, CTA in pulmonary embolism, early-stage breast cancer staging, acute pancreatitis, and special imaging for pre-op templar bone CT in cochlear implantation, and CT/MRI in long bone cartilaginous lesions. In addition, one study reported a sevenfold increase in knee MRI, while there was a reduction in knee arthroscopy [145].
Quantity of low-value imaging in children
In pediatrics the use of low-value examinations varied between 3.6 and 93.7% (11 studies) [286, 297, 299, 301, 314, 315, 320, 321, 356, 388, 389]. Abdominal CT in appendicitis (3.6%), repeat CT in trauma patients (5%) and C-spine CT in cervical spine injury (13%) were the least over-used examinations. Head CT (50–93.7%), CT scan in case of blunt abdominal trauma (18–80%) and pretransfer CT in trauma patients (66%) were the low-value examinations most used.
Discussion
In summary, through this scoping review, we found 84 different low-value imaging examinations performed among both adult and pediatric populations, for all imaging modalities, and body areas. Several of these examinations already have established referral criteria or have recommendations against them in the Choosing Wisely list, however this review show that these are still being used in clinical practice, and more examinations might need referral guidelines. The most commonly practices reported as low-value was head CT in several clinical queries (especially related to minor head injury [20,21,22,23,24,25,26,27,28,29,30,31,32,33, 36, 37, 40,41,42,43,44,45,46,47,48,49,50,51,52,53, 55, 56, 286,287,288,289,290,291,292,293]), chest X-ray for routine checkup or follow-ups [78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113, 118,119,120, 339,340,341,342,343], trauma CT in patients without clinical symptoms or as repeat scans [227,228,229,230,231,232, 287, 314,315,316,317,318,319,320,321,322], and skeletal X-rays in non-traumatic pain or in fracture follow-ups [132, 138, 139, 151,152,153,154,155,156, 160,161,162,163,164,165,166,167, 169, 323,324,325,326,327,328,329,330,331,332,333,334,335,336,337]. The following were the most frequently reported low-value examinations: imaging in low back pain [121,122,123,124,125,126,127,128,129,130,131] and knee MRI without red flags [121, 141,142,143,144,145,146,147], staging and follow-up in several types of cancer (X-ray, CT, MRI and nuclear medicine) [58, 116, 172, 199,200,201,202,203, 209, 234,235,236,237,238,239,240,241,242,243,244,245,246,247,248,249,250,251,252,253,254,255,256,257,258,259,260,261,262], abdominal CT in self-limiting episode of suspected urolithiasis [190, 204,205,206], chest CTA [210,211,212,213,214,215,216] and ultrasound lower limb veins in patients with low risk of thrombosis [217,218,219,220,221] were most prominent among adult populations. When analyzing the extent in use of low-value imaging additional examinations were identified; low interval DEXA screening, echocardiography in patients with low risk of cardiac disease, carotid imaging in syncope, X-ray in rhinosinusitis, and MRI for pain in the hip or upper extremities [140, 157,158,159, 173, 277, 365, 366, 369, 373, 376].
The variation in the proportion of low-value imaging was large (2–100% inappropriate or unnecessary examinations) and varied between studies of the same examination. There is no obvious threshold in proportion for when to define examinations as low-value. Even though the examinations found in this review are low-value on a group level, certain patient sub-groups or individual patients could have clinical findings justifying the use of imaging. However, in several studies there were identified a rate of ≥ 90% inappropriate imaging examinations. This provides a reason for altering the utilization of these examinations in practice. We found this to be the case in: repeat head or routine trauma CT, echocardiography, MRI in hip, knee and upper extremity pain, CT/MRI in acute pancreatitis, and pre-op templar bone CT in cochlear implantation [40,41,42, 54, 140, 141, 143, 145,146,147, 173, 176, 177, 229, 284, 357, 369, 388].
Our review found additional examinations that are potentially low-value to the examinations presented in the Choosing Wisely list [17, 390]. Additionally, we report the extent of low-value imaging. Our additional findings merit further investigation, including chest X-ray after invasive lung procedures such as CVC placement, chest tube placement/removal, biopsies, and other procedures [94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112, 339,340,341], musculoskeletal follow-ups after fractures or invasive procedures, MRI and X-ray in atraumatic shoulder or upper-extremity pain [138, 139, 151,152,153,154,155,156, 160,161,162,163,164,165,166,167, 169, 173, 323,324,325,326,327,328,329, 334, 336] and staging and follow-up procedures in cancers other than breast, cervical, prostate, and lymphoma [58, 172, 199, 202, 203, 209, 235,236,237, 239,240,241, 243,244,245, 247,248,249]. Hence, while we confirm previous findings, we also add new findings to the literature. Not all examinations in the Choosing Wisely list were included in this in this review such as cardiac imaging in asymptomatic patients or head CT in patients with sudden hearing loss [390]. This could be caused by the search being incomplete (for instants excluding screening programs), evidence of their low-value was given before 2010 or that some of the Choosing Wisely recommendations were based on clinical experience rather than research reports.
There are many ways to measure low-value imaging, including diagnostic yield, diagnostic accuracy, and impact/change in treatment or management, where diagnostic yield (n = 213) and change in patient management (n = 137) were most common. By applying the Fryback and Thornbury value model as stated by Brady et al. [391], measures of change in patient management and trends in imaging and related treatments, seems a better way to identify low-value imaging, rather than measuring diagnostic accuracy [391].
This scoping review has strengths and limitations in its methods. Although the search in databases was systematic and exhaustive, the cut-off was set at 2010, which excluded examinations identified as low-value imaging or adopted to clinical practice before 2010. Due to the large number of citations retrieved from the database searches, a wide range of inconclusive studies, studies identifying conditional low-value imaging, and articles reporting clinical practice guidelines were excluded. Hence, a wide range of supportive studies were excluded as the inclusion criteria were strict. Therefore, it is likely that there are several studies of low-value examinations that are not included in this review. Accordingly, the excluded studies in Additional file 2 may provide useful information for those who want to pursue specific examinations. The quality of included studies was also not assessed; it is likely that the included studies were of variable quality, limiting the strength of the conclusions made in this review. While the strict inclusion criteria may to some extent compensate for the lack of study quality assessment, quality assessment is not required [392] as the purpose of a scoping review is to identify and map the available evidence. While this review provides a valuable overview of identified low-value imaging, especially useful for clinicians and policymakers to be able to take actions to reduce overuse of diagnostic imaging. However, contextual assessment is needed before changing clinical practice. In addition, the risk of ionizing radiation or contrast media has not been considered in this analysis, this would be interesting issues to consider in later studies. There is also need for research on barriers and facilitators for reducing low-value imaging care to assess where to target policy changes, guidelines, and clinical practice.
Conclusions
In this study, we provide a comprehensive list of low-value radiological examinations for both adults and children. Our overview reaches beyond earlier published lists and adds information on the quantity of low-value imaging utilization, which reportedly varied from 2 to 100% among included studies. Imaging of atraumatic pain, routine imaging in minor head injury, trauma, thrombosis, urolithiasis, after chest interventions, fracture follow-up and cancer staging, or follow-up were the most frequently identified low-value imaging examinations. This overview can be of great value for clinicians, policymakers, and researchers for revising appropriateness criteria and planning de-implementation. Efforts should be made to reduce the extension and variation of inappropriate imaging which generates huge opportunity costs and is potentially harmful to patients.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Abbreviations
- CT:
-
Computed tomography
- CTA:
-
Computed tomography angiography
- DEXA:
-
Dual-energy X-ray absorptiometry
- EVAR:
-
Endovascular aneurysm repair
- MRI:
-
Magnetic resonance imaging
- PET:
-
Positron emission tomography
- US:
-
Ultrasound
- XR:
-
X-ray
References
Expert Panel on effective ways of investing in Health (EXPH). Defining value in “value-based healthcare. 2019.
Socha K, Couffinhal A, Forde I, Nader C, Cecchini M, Lee S, et al. Tackling wasteful spending on health. OECD 2017. 2017.
Brady A, Brink J, Slavotinek J. Radiology and value-based health care. JAMA. 2020;324(13):1286–7. https://doi.org/10.1001/jama.2020.14930.
Brenner DJ, Doll R, Goodhead DT, Hall EJ, Land CE, Little JB, et al. Cancer risks attributable to low doses of ionizing radiation: assessing what we really know. Proc Natl Acad Sci. 2003;100(24):13761. https://doi.org/10.1073/pnas.2235592100.
Andreucci M, Solomon R, Tasanarong A. Side effects of radiographic contrast media: pathogenesis, risk factors, and prevention. Biomed Res Int. 2014;2014: 741018. https://doi.org/10.1155/2014/741018.
Hendee WR, Becker GJ, Borgstede JP, Bosma J, Casarella WJ, Erickson BA, et al. Addressing overutilization in medical imaging. Radiology. 2010;257(1):240–5. https://doi.org/10.1148/radiol.10100063.
Sheng AY, Castro A, Lewiss RE. Awareness, utilization, and education of the ACR appropriateness criteria: a review and future directions. J Am Coll Radiol. 2016;13(2):131–6. https://doi.org/10.1016/j.jacr.2015.08.026.
Ingraham B, Miller K, Iaia A, Sneider MB, Naqvi S, Evans K, et al. Reductions in high-end imaging utilization with radiology review and consultation. J Am Coll Radiol. 2016;13(9):1079–82. https://doi.org/10.1016/j.jacr.2016.04.016.
Choosing Wisely [Internet]. 2021. https://www.choosingwisely.org/getting-started/lists/.
Improving health and social care through evidence-based guidance [Internet]. 2021. https://www.nice.org.uk/.
Ryan JW, Hollywood A, Stirling A, Glynn M, MacMahon PJ, Bolster F. Evidenced-based radiology? A single-institution review of imaging referral appropriateness including monetary and dose estimates for inappropriate scans. Ir J Med Sci. 2019;188(4):1385–9. https://doi.org/10.1007/s11845-019-02005-8.
Chandra K, Atkinson PR, Chatur H, Fraser J, Adams CL. To choose or not to choose: evaluating the effect of a choosing wisely knowledge translation initiative for imaging in low back pain by emergency physicians. Cureus. 2019;11(2): e4002. https://doi.org/10.7759/cureus.4002.
Barth JH, Misra S, Aakre KM, Langlois MR, Watine J, Twomey PJ, et al. Why are clinical practice guidelines not followed? Clin Chem Lab Med. 2016;54(7):1133–9. https://doi.org/10.1515/cclm-2015-0871.
DeAngelis J, Lou V, Li T, Tran H, Bremjit P, McCann M, et al. Head CT for minor head injury presenting to the emergency department in the era of choosing wisely. West J Emerg Med. 2017;18(5):821–9. https://doi.org/10.5811/westjem.2017.6.33685.
Anderson TS, Leonard S, Zhang AJ, Madden E, Mowery D, Chapman WW, et al. Trends in low-value carotid imaging in the veterans health administration from 2007 to 2016. JAMA Netw Open. 2020;3(9):e2015250-e.
Berezin L, Thompson C, Rojas-Luengas V, Borgundvaag B, McLeod SL. Lumbosacral spinal imaging for patients presenting to the emergency department with nontraumatic low back pain. J Emerg Med. 2020;58(2):269–74. https://doi.org/10.1016/j.jemermed.2019.12.017.
Müskens JLJM, Kool RB, van Dulmen SA, Westert GP. Overuse of diagnostic testing in healthcare: a systematic review. BMJ Qual Saf. 2021. https://doi.org/10.1136/bmjqs-2020-012576.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73. https://doi.org/10.7326/m18-0850.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210. https://doi.org/10.1186/s13643-016-0384-4.
Cellina M, Panzeri M, Floridi C, Martinenghi CMA, Clesceri G, Oliva G. Overuse of computed tomography for minor head injury in young patients: an analysis of promoting factors. Radiol Med. 2018;123(7):507–14. https://doi.org/10.1007/s11547-018-0871-x.
Parma C, Carney D, Grim R, Bell T, Shoff K, Ahuja V. Unnecessary head computed tomography scans: a level 1 trauma teaching experience. Am Surg. 2014;80(7):664–8. https://doi.org/10.1177/000313481408000720.
Shobeirian F, Ghomi Z, Soleimani R, Mirshahi R, Sanei Taheri M. Overuse of brain CT scan for evaluating mild head trauma in adults. Emerg Radiol. 2020. https://doi.org/10.1007/s10140-020-01846-6.
Ferorelli D, Donno F, De Giorgio G, Mele F, Favia M, Riefoli F, et al. Head CT scan in emergency room: is it still abused? Quantification and causes analysis of overprescription in an Italian Emergency Department. Radiol Med. 2020;125(6):595–9. https://doi.org/10.1007/s11547-020-01143-9.
Yildizhan S, Boyaci MG, Ozdinc S. How necessary is the computerized brain tomography in minor head trauma? Ulus Travma ve Acil Cerrahi Derg. 2019;25(4):378–82.
Yun BJ, Borczuk P, Zachrison KS, Goldstein JN, Berlyand Y, Raja AS. Utilization of head CT during injury visits to United States emergency departments: 2012–2015. Am J Emerg Med. 2018;36(8):1463–6. https://doi.org/10.1016/j.ajem.2018.05.018.
Zargar Balaye Jame S, Majdzadeh R, Akbari Sari A, Rashidian A, Arab M, Rahmani H. Indications and overuse of computed tomography in minor head trauma. Iran Red Crescent Med J. 2014;16(5):3067. https://doi.org/10.5812/ircmj.13067.
Zuzek P, Rigler I, Podnar S. Validation of clinical criteria for referral to head imaging in the neurologic emergency setting. Neurol Sci. 2019;40(12):2541–8. https://doi.org/10.1007/s10072-019-04009-9.
Theisen-Toupal J, Breu AC, Mattison ML, Arnaout R. Diagnostic yield of head computed tomography for the hospitalized medical patient with delirium. J Hosp Med. 2014;9(8):497–501. https://doi.org/10.1002/jhm.2198.
Vijayakrishnan R, Ramasubramanian A, Dhand S. Utility of head CT scan for acute inpatient delirium. Hosp Top. 2015;93(1):9–12. https://doi.org/10.1080/00185868.2015.1012928.
Ali AHA, Al-Ghamdi S, Karrar MH, Alajmi SA, Almutairi OS, Aldalbahi AM, et al. Is there a misuse of computed tomography in the diagnostic workup of headache? A retrospective record-based study in secondary health-care facility in Saudi Arabia. J Family Med Prim Care. 2018;7(2):357–61. https://doi.org/10.4103/jfmpc.jfmpc_338_17.
Wang R, Liu R, Dong Z, Su H, Ao R, Liu Y, et al. Unnecessary neuroimaging for patients with primary headaches. Headache. 2018;59(1):63–8. https://doi.org/10.1111/head.13397.
You JJ, Gladstone J, Symons S, Rotstein D, Laupacis A, Bell CM. Patterns of care and outcomes after computed tomography scans for headache. Am J Med. 2011;124(1):58-63.e1. https://doi.org/10.1016/j.amjmed.2010.08.010.
Campiglio L, Bianchi F, Cattalini C, Belvedere D, Rosci CE, Casellato CL, et al. Mild brain injury and anticoagulants: less is enough. Neurol Clin Pract. 2017;7(4):296–305. https://doi.org/10.1212/CPJ.0000000000000375.
Kumar S, Modi R, Bhandari BM, Sass DA, Rothstein KD. A head CT is unnecessary in the initial evaluation of a cirrhotic patient with recurrent hepatic encephalopathy. Ann Hepatol. 2018;17(5):810–4. https://doi.org/10.5604/01.3001.0012.3141.
Nagra I, Wee B, Short J, Banerjee AK. The role of cranial CT in the investigation of meningitis. JRSM Short Rep. 2011;2(3):20. https://doi.org/10.1258/shorts.2011.010113.
Maniar H, McPhillips K, Torres D, Wild J, Suk M, Horwitz DS. Clinical indications of computed tomography (CT) of the head in patients with low-energy geriatric hip fractures. Injury. 2015;46(11):2185–9. https://doi.org/10.1016/j.injury.2015.06.036.
Danielson K, Hall T, Endres T, Jones C, Sietsema D. Clinical indications of computed tomography (CT) of the head in patients with low-energy geriatric hip fractures: a follow-up study at a community hospital. Geriatr Orthop Surg Rehabil. 2019;10:2151459319861562. https://doi.org/10.1177/2151459319861562.
Owlia M, Yu L, Deible C, Hughes MA, Jovin F, Bump GM. Head CT scan overuse in frequently admitted medical patients. Am J Med. 2014;127(5):406–10. https://doi.org/10.1016/j.amjmed.2014.01.023.
Ramey P, Osborn M, Kirshner H, Abou-Khalil B. Misdiagnosis of lamotrigine toxicity as posterior circulation transient ischemic attack or stroke. Epilepsy Behav. 2020;111:107284.
Connon FF, Namdarian B, Ee JL, Drummond KJ, Miller JA. Do routinely repeated computed tomography scans in traumatic brain injury influence management? A prospective observational study in a level 1 trauma center. Ann Surg. 2011;254(6):1028–31. https://doi.org/10.1097/SLA.0b013e318219727f.
Befeler AR, Gordon W, Khan N, Fernandez J, Muhlbauer MS, Sorenson JM. Results of delayed follow-up imaging in traumatic brain injury. J Neurosurg. 2016;124(3):703–9. https://doi.org/10.3171/2015.4.JNS141257.
Almenawer SA, Bogza I, Yarascavitch B, Sne N, Farrokhyar F, Murty N, et al. The value of scheduled repeat cranial computed tomography after mild head injury: single-center series and meta-analysis. Neurosurgery. 2013;72(1):56–62. https://doi.org/10.1227/NEU.0b013e318276f899 (discussion 3-4).
AbdelFattah KR, Eastman AL, Aldy KN, Wolf SE, Minei JP, Scott WW, et al. A prospective evaluation of the use of routine repeat cranial CT scans in patients with intracranial hemorrhage and GCS score of 13 to 15. J Trauma Acute Care Surg. 2012;73(3):685–8. https://doi.org/10.1097/TA.0b013e318265ccd9.
Rosen CB, Luy DD, Deane MR, Scalea TM, Stein DM. Routine repeat head CT may not be necessary for patients with mild TBI. Trauma Surg Acute Care Open. 2018;3(1):e000129.
Stippler M, Smith C, McLean AR, Carlson A, Morley S, Murray-Krezan C, et al. Utility of routine follow-up head CT scanning after mild traumatic brain injury: a systematic review of the literature. Emerg Med J. 2012;29(7):528–32. https://doi.org/10.1136/emermed-2011-200162.
Kaen A, Jimenez-Roldan L, Arrese I, Amosa Delgado M, Lopez PG, Alday R, et al. The value of sequential computed tomography scanning in anticoagulated patients suffering from minor head injury. J Trauma. 2010;68(4):895–8. https://doi.org/10.1097/TA.0b013e3181b28a76.
McCammack KC, Sadler C, Guo Y, Ramaswamy RS, Farid N. Routine repeat head CT may not be indicated in patients on anticoagulant/antiplatelet therapy following mild traumatic brain injury. West J Emerg Med. 2015;16(1):43–9. https://doi.org/10.5811/westjem.2014.10.19488.
Reljic T, Mahony H, Djulbegovic B, Etchason J, Paxton H, Flores M, et al. Value of repeat head computed tomography after traumatic brain injury: systematic review and meta-analysis. J Neurotrauma. 2014;31(1):78–98. https://doi.org/10.1089/neu.2013.2873.
Sifri ZC, Nyak N, Homnick AT, Mohr AA, Yonclas P, Livingston DH. Utility of repeat head computed tomography in patients with an abnormal neurologic examination after minimal head injury. J Trauma. 2011;71(6):1605–10. https://doi.org/10.1097/TA.0b013e31822b3728.
Washington CW, Grubb RL. Are routine repeat imaging and intensive care unit admission necessary in mild traumatic brain injury? J Neurosurg. 2012;116(3):549–57.
Peck KA, Sise CB, Shackford SR, Sise MJ, Calvo RY, Sack DI, et al. Delayed intracranial hemorrhage after blunt trauma: are patients on preinjury anticoagulants and prescription antiplatelet agents at risk? J Trauma. 2011;71(6):1600–4. https://doi.org/10.1097/TA.0b013e31823b9ce1.
Uccella L, Zoia C, Perlasca F, Bongetta D, Codecà R, Gaetani P. Mild traumatic brain injury in patients on long-term anticoagulation therapy: do they really need repeated head CT scan? World Neurosurg. 2016;93:100–3. https://doi.org/10.1016/j.wneu.2016.05.061.
Flaherty BF, Moore HE, Riva-Cambrin J, Bratton SL. Repeat head CT for expectant management of traumatic epidural hematoma. Pediatrics. 2018;142(3):e20180385. https://doi.org/10.1542/peds.2018-0385.
Behmanesh B, Keil F, Dubinski D, Won SY, Quick-Weller J, Seifert V, et al. The value of computed tomography imaging of the head after ventriculoperitoneal shunt surgery in adults. World Neurosurg. 2019;121:e159–64. https://doi.org/10.1016/j.wneu.2018.09.063.
Ng HY, Ng WH, King NK. Value of routine early post-operative computed tomography in determining short-term functional outcome after drainage of chronic subdural hematoma: an evaluation of residual volume. Surg Neurol Int. 2014;5(1):136. https://doi.org/10.4103/2152-7806.141299.
Nadimi S, Caballero N, Carpenter P, Sowa L, Cunningham R, Welch KC. Immediate postoperative imaging after uncomplicated endoscopic approach to the anterior skull base: is it necessary? Int Forum Allergy Rhinol. 2014;4(12):1024–9.
Abboud H, Mente K, Seay M, Kim J, Ali A, Bermel R, et al. Triaging patients with multiple sclerosis in the emergency department: room for improvement. Int J MS Care. 2017;19(6):290–6. https://doi.org/10.7224/1537-2073.2016-069.
Cho H, Lee HY, Kim J, Kim HK, Choi JY, Um SW, et al. Pure ground glass nodular adenocarcinomas: are preoperative positron emission tomography/computed tomography and brain magnetic resonance imaging useful or necessary? J Thorac Cardiovasc Surg. 2015;150(3):514–20. https://doi.org/10.1016/j.jtcvs.2015.06.024.
Eroukhmanoff J, Tejedor I, Potorac I, Cuny T, Bonneville JF, Dufour H, et al. MRI follow-up is unnecessary in patients with macroprolactinomas and long-term normal prolactin levels on dopamine agonist treatment. Eur J Endocrinol. 2017;176(3):323–8. https://doi.org/10.1530/EJE-16-0897.
Viau JA, Chaudry H, Hannigan A, Boutet M, Mukarram M, Thiruganasambandamoorthy V. The yield of computed tomography of the head among patients presenting with syncope: a systematic review. Acad Emerg Med. 2019;26(5):479–90. https://doi.org/10.1111/acem.13568.
Johnson PC, Ammar H, Zohdy W, Fouda R, Govindu R. Yield of diagnostic tests and its impact on cost in adult patients with syncope presenting to a community hospital. South Med J. 2014;107(11):707–14. https://doi.org/10.14423/SMJ.0000000000000184.
Peres MFP, Swerts DB, de Oliveira AB, Silva-Neto RP. Migraine patients’ journey until a tertiary headache center: an observational study. J Headache Pain. 2019;20(1):88. https://doi.org/10.1186/s10194-019-1039-3.
Shuaib W, Johnson JO, Pande V, Salastekar N, Kang J, He Q, et al. Ventriculoperitoneal shunt malfunction: cumulative effect of cost, radiation, and turnaround time on the patient and the health care system. AJR Am J Roentgenol. 2014;202(1):13–7. https://doi.org/10.2214/AJR.13.11176.
Raza SA, Javalkar V, Dehkharghani S, Kudrimoti A, Saindane A, Mullins M, et al. Utility of repeat cerebrovascular imaging among hospitalized stroke patients. J Stroke Cerebrovasc Dis. 2017;26(7):1588–93. https://doi.org/10.1016/j.jstrokecerebrovasdis.2017.02.029.
Al Shakarchi J, Lowry D, Nath J, Khawaja AZ, Inston N, Tiwari A. Duplex ultrasound surveillance after carotid artery endarterectomy. J Vasc Surg. 2016;63(6):1647–50. https://doi.org/10.1016/j.jvs.2016.01.054.
Scott JW, Schwartz AL, Gates JD, Gerhard-Herman M, Havens JM. Choosing wisely for syncope: low-value carotid ultrasound use. J Am Heart Assoc. 2014;3(4):e001063. https://doi.org/10.1161/JAHA.114.001063.
Rose MK, Rosal LM, Gonzalez RP, Rostas JW, Baker JA, Simmons JD, et al. Clinical clearance of the cervical spine in patients with distracting injuries: it is time to dispel the myth. J Trauma Acute Care Surg. 2012;73(2):498–502. https://doi.org/10.1097/TA.0b013e3182587634.
Uriell ML, Allen JW, Lovasik BP, Benayoun MD, Spandorfer RM, Holder CA. Yield of computed tomography of the cervical spine in cases of simple assault. Injury. 2017;48(1):133–6. https://doi.org/10.1016/j.injury.2016.10.031.
Benayoun MD, Allen JW, Lovasik BP, Uriell ML, Spandorfer RM, Holder CA. Utility of computed tomographic imaging of the cervical spine in trauma evaluation of ground-level fall. J Trauma Acute Care Surg. 2016;81(2):339–44. https://doi.org/10.1097/TA.0000000000001073.
Novick D, Wallace R, DiGiacomo JC, Kumar A, Lev S, Angus LDG. The cervical spine can be cleared without MRI after blunt trauma: a retrospective review of a single level 1 trauma center experience over 8 years. Am J Surg. 2018;216(3):427–30. https://doi.org/10.1016/j.amjsurg.2018.03.003.
Subramanian M, Hranjec T, Liu L, Hodgman EI, Minshall CT, Minei JP. A case for less workup in near hanging. J Trauma Acute Care Surg. 2016;81(5):925–30. https://doi.org/10.1097/TA.0000000000001231.
Ghaffarpasand F, Paydar S, Foroughi M, Saberi A, Abbasi H, Karimi AA, et al. Role of cervical spine radiography in the initial evaluation of stable high-energy blunt trauma patients. J Orthop Sci. 2011;16(5):498–502. https://doi.org/10.1007/s00776-011-0132-5.
Bartels RHMA, Beems T, Schutte PJ, Verbeek ALM. The rationale of postoperative radiographs after cervical anterior discectomy with stand-alone cage for radicular pain. J Neurosurg Spine. 2010;12(3):275–9. https://doi.org/10.3171/2009.9.SPINE09263.
Grimm BD, Leas DP, Glaser JA. The utility of routine postoperative radiographs after cervical spine fusion. Spine J. 2013;13(7):764–9. https://doi.org/10.1016/j.spinee.2013.01.018.
Shau DN, Bible JE, Samade R, Gadomski SP, Mushtaq B, Wallace A, et al. Utility of postoperative radiographs for cervical spine fusion a comprehensive evaluation of operative technique, surgical indication, and duration since surgery. Spine. 2012;37(24):1994–2000. https://doi.org/10.1097/BRS.0b013e31825c0130.
Martin SC, Dabbous BO, Ridgeon EE, Magdum SA, Cadoux-Hudson TA, Pereira EA. Routine radiographs one day after anterior cervical discectomy and fusion are neither necessary nor cost-effective. Br J Neurosurg. 2017;31(1):50–3. https://doi.org/10.1080/02688697.2016.1233320.
Tran B, Saxe JM, Ekeh AP. Are flexion extension films necessary for cervical spine clearance in patients with neck pain after negative cervical CT scan? J Surg Res. 2013;184(1):411–3. https://doi.org/10.1016/j.jss.2013.05.100.
Ali IS, Khan M, Khan MA. Routine preoperative chest x-ray and its impact on decision making in patients undergoing elective surgical procedures. J Ayub Med Coll Abbottabad. 2013;25(1–2):23–5.
Kröner A, Beenen L, du Raan M, Meijer P, Spronk PE, Stoker J, et al. The clinical value of routinely obtained postoperative chest radiographs in post-anaesthesia care unit patients seems poor-a prospective observational study. Ann Transl Med. 2018;6(18):360. https://doi.org/10.21037/atm.2018.08.33.
Loggers SAI, Giannakopoulos GF, Vandewalle E, Erwteman M, Berger F, Zuidema WP. Preoperative chest radiographs in hip fracture patients: is there any additional value? Eur J Orthop Surg Traumatol. 2017;27(7):953–9. https://doi.org/10.1007/s00590-017-1971-3.
Thanh NX, Rashiq S, Jonsson E. Routine preoperative electrocardiogram and chest x-ray prior to elective surgery in Alberta, Canada. Can J Anaesth. 2010;57(2):127–33. https://doi.org/10.1007/s12630-009-9233-4.
De La Pena H, Sharma A, Glicksman C, Joseph J, Subesinghe M, Traill Z, et al. No longer any role for routine follow-up chest x-rays in men with stage I germ cell cancer. Eur J Cancer. 2017;84:354–9. https://doi.org/10.1016/j.ejca.2017.07.005.
Hovgaard TB, Nymark T, Skov O, Petersen MM. Follow-up after initial surgical treatment of soft tissue sarcomas in the extremities and trunk wall. Acta Oncol. 2017;56(7):1004–12. https://doi.org/10.1080/0284186X.2017.1299937.
Hoogendam JP, Zweemer RP, Verkooijen HM, de Jong PA, van den Bosch MA, Verheijen RH, et al. No value for routine chest radiography in the work-up of early stage cervical cancer patients. PLoS ONE. 2015;10(7): e0131899. https://doi.org/10.1371/journal.pone.0131899.
Louie RJ, Tonneson JE, Gowarty M, Goodney PP, Barth RJ, Rosenkranz KM. Complete blood counts, liver function tests, and chest x-rays as routine screening in early-stage breast cancer: value added or just cost? Breast Cancer Res Treat. 2015;154(1):99–103. https://doi.org/10.1007/s10549-015-3593-y.
Izamin I, Rizal AM. Chest x-ray as an essential part of routine medical examination: is it necessary? Med J Malaysia. 2012;67(6):606–9.
Shimoni Z, Rosenberg M, Amit L, Froom P. Chest radiography should be requested only on admission based on clinical grounds. South Med J. 2020;113(1):20–2. https://doi.org/10.14423/Smj.0000000000001051.
Verma V, Vasudevan V, Jinnur P, Nallagatla S, Majumdar A, Arjomand F, et al. The utility of routine admission chest X-ray films on patient care. Eur J Intern Med. 2011;22(3):286–8. https://doi.org/10.1016/j.ejim.2010.12.007.
Alazzawi S, De Rover WS, Morris-Stiff G, Lewis MH. Erect chest radiography in the setting of the acute abdomen: essential tool or an unnecessary waste of resources? Ann R Coll Surg Engl. 2010;92(8):697–9. https://doi.org/10.1308/003588410X12699663904998.
Paydar S, Johari HG, Ghaffarpasand F, Shahidian D, Dehbozorgi A, Ziaeian B, et al. The role of routine chest radiography in initial evaluation of stable blunt trauma patients. Am J Emerg Med. 2012;30(1):1–4. https://doi.org/10.1016/j.ajem.2010.08.010.
Zieleskiewicz L, Fresco R, Duclos G, Antonini F, Mathieu C, Medam S, et al. Integrating extended focused assessment with sonography for trauma (eFAST) in the initial assessment of severe trauma: impact on the management of 756 patients. Injury. 2018;49(10):1774–80. https://doi.org/10.1016/j.injury.2018.07.002.
Greig CJ, Keiser AM, Cleary MA, Stitelman DH, Christison-Lagay ER, Ozgediz DE, et al. Routine postnatal chest x-ray and intensive care admission are unnecessary for a majority of infants with congenital lung malformations. J Pediatr Surg. 2019;54(4):670–4. https://doi.org/10.1016/j.jpedsurg.2018.10.063.
Lemmers M, Saltzherr TP, Beenen LF, Ponsen KJ, Goslings JC. Are routine repeat chest x-rays before leaving the trauma room useful? Emerg Med J. 2010;27(7):522–5. https://doi.org/10.1136/emj.2009.078519.
Bjerregaard LS, Jensen K, Petersen RH, Hansen HJ. Routinely obtained chest X-rays after elective video-assisted thoracoscopic surgery can be omitted in most patients; a retrospective, observational study. Gen Thorac Cardiovasc Surg. 2015;63(8):465–71. https://doi.org/10.1007/s11748-015-0560-9.
Leschber G, May CJ, Simbrey-Chryselius N. Do thoracic surgery patients always need a postoperative chest X-ray? Zentralbl Chir. 2014;139(Suppl 1):S43–9. https://doi.org/10.1055/s-0034-1383034.
Chui J, Saeed R, Jakobowski L, Wang W, Eldeyasty B, Zhu F, et al. Is routine chest X-ray after ultrasound-guided central venous catheter insertion choosing wisely?: A population-based retrospective study of 6875 patients. Chest. 2018;154(1):148–56. https://doi.org/10.1016/j.chest.2018.02.017.
Cunningham JP, Knott EM, Gasior AC, Juang D, Snyder CL, St. Peter SD, et al. Is routine chest radiograph necessary after chest tube removal? J Pediatr Surg. 2014;49(10):1493–5. https://doi.org/10.1016/j.jpedsurg.2014.01.004.
Dalton BGA, Gonzalez KW, Keirsy MC, Rivard DC, St. Peter SD. Chest radiograph after fluoroscopic guided line placement: no longer necessary. J Pediatr Surg. 2016;51(9):1490–1. https://doi.org/10.1016/j.jpedsurg.2016.02.003.
Eisenberg RL, Khabbaz KR. Are chest radiographs routinely indicated after chest tube removal following cardiac surgery? AJR Am J Roentgenol. 2011;197(1):122–4. https://doi.org/10.2214/AJR.10.5856.
Farzan R, Shojaee R, Haghdoost A, Mobayen M. Comparison of chest X-ray and clinical findings in trauma patients after chest tube removal. J Clin Diagn Res. 2018;12(7):Pc19–21. https://doi.org/10.7860/Jcdr/2018/31989.11833.
Goodman MD, Huber NL, Johannigman JA, Pritts TA. Omission of routine chest x-ray after chest tube removal is safe in selected trauma patients. Am J Surg. 2010;199(2):199–203. https://doi.org/10.1016/j.amjsurg.2009.03.011.
Hourmozdi JJ, Markin A, Johnson B, Fleming PR, Miller JB. Routine chest radiography is not necessary after ultrasound-guided right internal jugular vein catheterization. Crit Care Med. 2016;44(9):e804–8. https://doi.org/10.1097/CCM.0000000000001737.
Izbicki G, Romem A, Arish N, Cahan C, Azulai H, Chen-Shuali C, et al. Avoiding routine chest radiography after transbronchial biopsy is safe. Respiration. 2016;92(3):176–81. https://doi.org/10.1159/000448688.
Johnson B, Rylander M, Beres AL. Do X-rays after chest tube removal change patient management? J Pediatr Surg. 2017;52(5):813–5. https://doi.org/10.1016/j.jpedsurg.2017.01.047.
Miccini M, Cassini D, Gregori M, Gazzanelli S, Cassibba S, Biacchi D. Ultrasound-guided placement of central venous port systems via the right internal jugular vein: are chest X-ray and/or fluoroscopy needed to confirm the correct placement of the device? World J Surg. 2016;40(10):2353–8. https://doi.org/10.1007/s00268-016-3574-2.
Porter ED, Fay KA, Hasson RM, Millington TM, Finley DJ, Phillips JD. Routine chest X-rays after thoracic surgery are unnecessary. J Surg Res. 2020;250:188–92. https://doi.org/10.1016/j.jss.2019.12.030.
Woodland DC, Randall Cooper C, Farzan Rashid M, Rosario VL, Weyker PD, Weintraub J, et al. Routine chest X-ray is unnecessary after ultrasound-guided central venous line placement in the operating room. J Crit Care. 2018;46:13–6.
Cerfolio RJ, Bryant AS. Daily chest roentgenograms are unnecessary in nonhypoxic patients who have undergone pulmonary resection by thoracotomy. Ann Thorac Surg. 2011;92(2):440–3. https://doi.org/10.1016/j.athoracsur.2011.04.002.
Eisenmann S, Winantea J, Karpf-Wissel R, Funke F, Stenzel E, Taube C, et al. Thoracic ultrasound for immediate exclusion of pneumothorax after interventional bronchoscopy. J Clin Med. 2020;9(5):1486. https://doi.org/10.3390/jcm9051486.
Farach SM, Danielson PD, Chandler NM. The role of chest radiography following pectus bar removal. Pediatr Surg Int. 2016;32(7):705–8. https://doi.org/10.1007/s00383-016-3905-2.
Knudsen MR, Nyboe C, Hjortdal VE, Pilegaard HK. Routine postoperative chest X-ray is unnecessary following the Nuss procedure for pectus excavatum. Interact Cardiovasc Thorac Surg. 2013;16(6):830–3. https://doi.org/10.1093/icvts/ivt052.
Sola R, Yu YR, Friske TC, Jamal AR, Rosenfeld EH, Mazziotti MV, et al. Repetitive imaging following minimally invasive repair of pectus excavatum is unnecessary. Eur J Pediatr Surg. 2019;29(5):408–11. https://doi.org/10.1055/s-0038-1660868.
Velicković JV, Hajdarević SA, Palibrk IG, Janić NR, Djukanović M, Miljković B, et al. Routine chest radiographs in the surgical intensive care unit: can we change clinical habits with no proven benefit? Acta Chir Iugosl. 2013;60(3):39–44.
Pathak T, Parmar MS. (F)utility of computed tomography of the chest in the presence of pleural effusion. Pleura Peritoneum. 2017;2(4):181–6. https://doi.org/10.1515/pp-2017-0019.
Fatihoglu E, Aydin S, Gokharman FD, Ece B, Kosar PN. X-ray use in chest imaging in emergency department on the basis of cost and effectiveness. Acad Radiol. 2016;23(10):1239–45. https://doi.org/10.1016/j.acra.2016.05.008.
Kim H, Han W, Moon H-G, Min J, Ahn S-K, Kim T-Y, et al. The value of preoperative staging chest computed tomography to detect asymptomatic lung and liver metastasis in patients with primary breast carcinoma. Breast Cancer Res Treat. 2011;126(3):637–41. https://doi.org/10.1007/s10549-011-1368-7.
Zhou Y, Zheng Y, Yang Q, Hu L, Liao J, Li X. Cohort study of chest CT and clinical changes in 29 patients with coronavirus disease 2019 (COVID-19). Eur Radiol. 2020;30(11):6213–20. https://doi.org/10.1007/s00330-020-07007-0.
Bjurlin MA, O’Grady T, Kim R, Jordan MD, Goble SM, Hollowell CM. Is routine postoperative chest radiography needed after percutaneous nephrolithotomy? Urology. 2012;79(4):791–5. https://doi.org/10.1016/j.urology.2011.08.053.
Mikhael A, Patell R, Tabet M, Bena J, Berber E, Nasr C. Chest X-ray prior to thyroidectomy: is it really needed? World J Surg. 2018;42(5):1403–7. https://doi.org/10.1007/s00268-017-4357-0.
Cruz J, Ferra M, Kasarabada A, Gasperino J, Zigmund B. Evaluation of the clinical utility of routine daily chest radiography in intensive care unit patients with tracheostomy tubes: a retrospective review. J Intensive Care Med. 2016;31(5):333–7. https://doi.org/10.1177/0885066614538393.
Karel YH, Verkerk K, Endenburg S, Metselaar S, Verhagen AP. Effect of routine diagnostic imaging for patients with musculoskeletal disorders: a meta-analysis. Eur J Intern Med. 2015;26(8):585–95. https://doi.org/10.1016/j.ejim.2015.06.018.
Khanduja S, Loomba V, Salama-Hannah J, Upadhyay A, Khanduja N, Chauhan G. Retrospective review of magnetic resonance imaging of the lumbosacral spine: are we overinvestigating? Neurospine. 2018;15(4):383–7. https://doi.org/10.14245/ns.1836110.055.
Salari H, Ostovar R, Esfandiari A, Keshtkaran A, Akbari Sari A, Yousefi Manesh H, et al. Evidence for policy making: clinical appropriateness study of lumbar spine MRI prescriptions using RAND appropriateness method. Int J Health Policy Manag. 2013;1(1):17–21. https://doi.org/10.15171/ijhpm.2013.04.
Tan AL, Zhou J, Kuo YF, Goodwin JS. Variation among primary care physicians in the use of imaging for older patients with acute low back pain. J Gen Intern Med. 2016;31(2):156–63. https://doi.org/10.1007/s11606-015-3475-3.
Wnuk NM, Alkasab TK, Rosenthal DI. Magnetic resonance imaging of the lumbar spine: determining clinical impact and potential harm from overuse. Spine J. 2018;18(9):1653–8. https://doi.org/10.1016/j.spinee.2018.04.005.
Yu LD, Wang XW, Lin XJ, Wang Y. The use of lumbar spine magnetic resonance imaging in eastern China: appropriateness and related factors. PLoS ONE. 2016;11(1):e0146369. https://doi.org/10.1371/journal.pone.0146369.
Zargar BJS, Sari AA, Majdzadeh R, Rashidian A, Arab M, Rahmani H. The extent of inappropriate use of magnetic resonance imaging in low back pain and its contributory factors. Int J Prev Med. 2014;5(8):1029–36.
Jahanmehr N, Bigdeli AS, Salari H, Mokarami H, KhodaKarim S, Damiri S. Analyzing inappropriate magnetic resonance imaging (MRI) prescriptions and resulting economic burden on patients suffering from back pain. Int J Health Plann Manag. 2019;34(4):e1437–47. https://doi.org/10.1002/hpm.2806.
Logan GS, Pike A, Copsey B, Parfrey P, Etchegary H, Hall A. What do we really know about the appropriateness of radiation emitting imaging for low back pain in primary and emergency care? A systematic review and meta-analysis of medical record reviews. PLoS ONE. 2019;14(12):e0225414. https://doi.org/10.1371/journal.pone.0225414.
Schlemmer E, Mitchiner JC, Brown M, Wasilevich E. Imaging during low back pain ED visits: a claims-based descriptive analysis. Am J Emerg Med. 2015;33(3):414–8. https://doi.org/10.1016/j.ajem.2014.12.060.
Leichtle UG, Wunschel M, Socci M, Kurze C, Niemeyer T, Leichtle CI. Spine radiography in the evaluation of back and neck pain in an orthopaedic emergency clinic. J Back Musculoskelet Rehabil. 2015;28(1):43–8. https://doi.org/10.3233/BMR-140488.
Molinari RWMD, Hunter JGMD, McAssey RWBS. In-hospital postoperative radiographs for instrumented single-level degenerative spinal fusions: utility after intraoperative fluoroscopy. Spine J. 2012;12(7):559–67. https://doi.org/10.1016/j.spinee.2012.06.005.
Simpson AK, Osler P, Wood KB. Utility of postoperative radiographs after anterior lumbar interbody fusion with or without posterior instrumentation. Spine. 2013;38(23):2038–42. https://doi.org/10.1097/BRS.0b013e3182a81f67.
Yamashita T, Steinmetz MP, Lieberman IH, Modic MT, Mroz TE. The utility of repeated postoperative radiographs after lumbar instrumented fusion for degenerative lumbar spine. Spine. 2011;36(23):1955–60. https://doi.org/10.1097/BRS.0b013e31820125b5.
Natoli RM, Fogel HA, Holt D, Schiff A, Bernstein M, Summers HD, et al. Advanced imaging lacks clinical utility in treating geriatric pelvic ring injuries caused by low-energy trauma. J Orthop Trauma. 2017;31(4):194–9. https://doi.org/10.1097/BOT.0000000000000761.
Bolt C, O’Keeffe F, Finnegan P, Dickson K, Smit V, Fitzgerald MC, et al. Straight leg elevation to rule out pelvic injury. Injury. 2018;49(2):279–83. https://doi.org/10.1016/j.injury.2017.10.009.
van Trigt J, Schep NWL, Peters RW, Goslings JC, Schepers T, Halm JA. Routine pelvic X-rays in asymptomatic hemodynamically stable blunt trauma patients: a meta-analysis. Injury. 2018;49(11):2024–31. https://doi.org/10.1016/j.injury.2018.09.009.
Lechtig A, Barghi A, Wolf BT, Weaver M, Wixted JJ, Rodriguez EK, et al. The utility of post-operative hip radiographs in patients treated with hip hemiarthroplasty for femoral neck fractures. Injury. 2019;50(8):1448–51. https://doi.org/10.1016/j.injury.2019.07.005.
Westerterp M, Emous M, Vermeulen MC, Eerenberg JP, van Geloven AA. No additional value of routine check X-rays after internal fixation of hip fractures. Eur J Trauma Emerg Surg. 2013;39(2):163–5. https://doi.org/10.1007/s00068-012-0244-4.
Issa K, Jauregui JJ, McElroy M, Banerjee S, Kapadia BH, Mont MA. Unnecessary magnetic resonance imaging of hips: an economic burden to patients and the healthcare system. J Arthroplasty. 2014;29(10):1911–4. https://doi.org/10.1016/j.arth.2014.05.022.
Adelani MA, Mall NA, Brophy RH, Halstead ME, Smith MV, Wright RW. The use of MRI in evaluating knee pain in patients aged 40 years and older. J Am Acad Orthop Surg. 2016;24(9):653–9. https://doi.org/10.5435/JAAOS-D-15-00681.
Parent ME, Vezina F, Carrier N, Masetto A. Indications for and clinical procedures resulting from magnetic resonance imaging of the knee in older patients: are we choosing wisely? Can Fam Physician. 2018;64(3):e126–32.
Refahi S, Kachooei AR, Farsadpour M, Shahrayeni R, Goudarzian M, Taleghani YM, et al. Is prescription of knee MRI according to standard clinical guideline? Acta Medica Mediterranea. 2016;32:1207–11.
Sheridan GA, Bisseru A, Glynn AA. The utility of MRI scans for a painful knee in the elderly patient. Ir J Med Sci. 2020. https://doi.org/10.1007/s11845-020-02261-z.
Smith L, Barratt A, Buchbinder R, Harris IA, Doust J, Bell K. Trends in knee magnetic resonance imaging, arthroscopies and joint replacements in older Australians: still too much low-value care? ANZ J Surg. 2020;90(5):833–9. https://doi.org/10.1111/ans.15712.
Solivetti FM, Guerrisi A, Salducca N, Desiderio F, Graceffa D, Capodieci G, et al. Appropriateness of knee MRI prescriptions: clinical, economic and technical issues. Radiol Med. 2016;121(4):315–22. https://doi.org/10.1007/s11547-015-0606-1.
Gomez-Garcia JM, Gomez-Romero FJ, Arencibia-Jimenez M, Navarro-Gracia JF, Sanchez-Molla M. Appropriateness of magnetic resonance imaging requested by primary care physicians for patients with knee pain. Int J Qual Health Care. 2018;30(7):565–70. https://doi.org/10.1093/intqhc/mzy067.
Wright AA, Hegedus EJ, Lenchik L, Kuhn KJ, Santiago L, Smoliga JM. Diagnostic accuracy of various imaging modalities for suspected lower extremity stress fractures. Am J Sports Med. 2015;44(1):255–63.
Garras DN, Raikin SM, Bhat SB, Taweel N, Karanjia H. MRI is unnecessary for diagnosing acute Achilles tendon ruptures: clinical diagnostic criteria. Clin Orthop Relat Res. 2012;470(8):2268–73. https://doi.org/10.1007/s11999-012-2355-y.
Antoci V Jr, Patel SP, Weaver MJ, Kwon JY. Relevance of adjacent joint imaging in the evaluation of ankle fractures. Injury. 2016;47(10):2366–9. https://doi.org/10.1016/j.injury.2016.07.025.
Werner BC, Burrus MT, Kew ME, Dempsey IJ, Gwathmey FW, Miller MD, et al. Limited utility of routine early postoperative radiography after primary ACL reconstruction. Knee. 2016;23(2):237–40. https://doi.org/10.1016/j.knee.2015.09.006.
Jaecker V, Neumann L, Shafizadeh S, Koenen P, Kanakamedala AC, Tjardes T. Radiographic images are inapplicable for a precise evaluation of the femoral tunnel position following MPFL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2019;27(11):3432–40. https://doi.org/10.1007/s00167-019-05378-6.
Jennewine B, Fiorino D, Kew M, Byrne A, Yarboro S. Routine postoperative radiographs after tibia plateau fixation have minimal impact on patient care. Injury. 2019;50(11):2093–6. https://doi.org/10.1016/j.injury.2019.07.025.
Longenecker AS, Kazarian GS, Boyer GP, Lonner JH. Radiographic imaging in the postanesthesia care unit is unnecessary after partial knee arthroplasty. J Arthroplasty. 2017;32(5):1431–3. https://doi.org/10.1016/j.arth.2016.11.033.
Moussa ME, Malchau H, Freiberg AA, Kwon YM. Effect of immediate postoperative portable radiographs on reoperation in primary total knee arthroplasty. Orthopedics. 2014;37(9):e817–21. https://doi.org/10.3928/01477447-20140825-59.
Sambandam SN, Khanna V, Rohinikumar G, Mounasamy V. Pre-discharge postoperative radiographs after primary total knee replacement: tradition or science? Acta Orthop Belg. 2017;83(1):132–9.
Sheehan SE, Coburn JA, Singh H, Vanness DJ, Sittig DF, Moberg DP, et al. Reducing unnecessary shoulder MRI examinations within a capitated health care system: a potential role for shoulder ultrasound. J Am Coll Radiol. 2016;13(7):780–7. https://doi.org/10.1016/j.jacr.2016.03.015.
Freeman R, Khanna S, Ricketts D. Inappropriate requests for magnetic resonance scans of the shoulder. Int Orthop. 2013;37(11):2181–4. https://doi.org/10.1007/s00264-013-1968-4.
Cortes A, Quinlan NJ, Nazal MR, Upadhyaya S, Alpaugh K, Martin SD. A value-based care analysis of magnetic resonance imaging in patients with suspected rotator cuff tendinopathy and the implicated role of conservative management. J Shoulder Elbow Surg. 2019;28(11):2153–60. https://doi.org/10.1016/j.jse.2019.04.003.
Feder OI, Levy BJ, Gruson KI. Routine plain radiographs in the setting of atraumatic shoulder pain: are they useful? J Am Acad Orthop Surg. 2018;26(8):287–93. https://doi.org/10.5435/JAAOS-D-16-00884.
Roberts S, Dearne R, Keen S, Littlewood C, Taylor S, Deacon P. Routine X-rays for suspected frozen shoulder offer little over diagnosis based on history and clinical examination alone. Musculoskelet Care. 2019;17(2):288–92. https://doi.org/10.1002/msc.1396.
Karamitopoulos MS, Dean E, Littleton AG, Kruse R. Postoperative radiographs after pinning of supracondylar humerus fractures: are they necessary? J Pediatr Orthop. 2012;32(7):672–4. https://doi.org/10.1097/BPO.0b013e31824b2b37.
Dempsey IJ, Kew ME, Cancienne JM, Werner BC, Brockmeier SF. Utility of postoperative radiography in routine primary total shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26(7):e222–6. https://doi.org/10.1016/j.jse.2016.11.035.
Eastley N, Aujla R, Khan Z. Radiographs late in the follow up of uncomplicated distal radius fractures: are they worth it? Clinical outcome and financial implications. Orthop Rev (Pavia). 2012;4(2): e20. https://doi.org/10.4081/or.2012.e20.
Sharma V, Witney-Lagen C, Cullen S, Kim E, Haider Z, Davy A, et al. The role of early post-operative radiographs following distal radius fracture fixation with a volar locking plate: time for change? J Hand Surg Asian Pac. 2019;24(4):435–9. https://doi.org/10.1142/S2424835519500553.
Stone JD, Vaccaro LM, Brabender RC, Hess AV. Utility and cost analysis of radiographs taken 2 weeks following plate fixation of distal radius fractures. J Hand Surg Am. 2015;40(6):1106–9. https://doi.org/10.1016/j.jhsa.2015.02.013.
Van Gerven P, El Moumni M, Zuidema WP, Rubinstein SM, Krijnen P, Van Tulder MW, et al. Omitting routine radiography of traumatic distal radial fractures after initial 2-week follow-up does not affect outcomes. J Bone Joint Surg Am Vol. 2019;101(15):1342–50.
Imerci A, Kaya A, Bozoglan M, Adam G, Canbek U, Savran A. Evaluation of computed tomography use in emergency department orthopedic trauma patients. Turk J Emerg Med. 2013;13(2):75–80.
Chaudhry S, DelSole EM, Egol KA. Post-splinting radiographs of minimally displaced fractures: good medicine or medicolegal protection? J Bone Joint Surg Am. 2012;94(17): e128. https://doi.org/10.2106/JBJS.K.00944.
Michelotti BF, Mathews A, Chung KC. Appropriateness of the use of magnetic resonance imaging in the diagnosis and treatment of wrist soft tissue injury. Plast Reconstr Surg. 2018;141(2):410–9. https://doi.org/10.1097/PRS.0000000000004023.
Stott S, Balogh ZJ. Postoperative computed tomography for articular fractures: a systematic review. J Orthop Trauma. 2017;31(1):56–61. https://doi.org/10.1097/BOT.0000000000000660.
Wilson RJ, Zumsteg JW, Hartley KA, Long JH, Mesko NW, Halpern JL, et al. Overutilization and cost of advanced imaging for long-bone cartilaginous lesions. Ann Surg Oncol. 2015;22(11):3466–73. https://doi.org/10.1245/s10434-014-4325-y.
Babbel D, Rayan G. Magnetic resonance imaging in evaluating workers’ compensation patients. J Hand Surg Am. 2012;37(4):811–5. https://doi.org/10.1016/j.jhsa.2011.12.008.
Nystrom LM, Reimer NB, Dean CW, Bush CH, Scarborough MT, Gibbs CP Jr. Evaluation of imaging utilization prior to referral of musculoskeletal tumors: a prospective study. J Bone Joint Surg Am. 2015;97(1):10–5. https://doi.org/10.2106/JBJS.N.00186.
Kothari S, Kalinowski M, Kobeszko M, Almouradi T. Computed tomography scan imaging in diagnosing acute uncomplicated pancreatitis: usefulness vs cost. World J Gastroenterol. 2019;25(9):1080–7. https://doi.org/10.3748/wjg.v25.i9.1080.
Shinagare AB, Ip IK, Raja AS, Sahni VA, Banks P, Khorasani R. Use of CT and MRI in emergency department patients with acute pancreatitis. Abdom Imaging. 2015;40(2):272–7. https://doi.org/10.1007/s00261-014-0210-1.
Spanier BW, Nio Y, van der Hulst RW, Tuynman HA, Dijkgraaf MG, Bruno MJ. Practice and yield of early CT scan in acute pancreatitis: a Dutch Observational Multicenter Study. Pancreatology. 2010;10(2–3):222–8. https://doi.org/10.1159/000243731.
Reynolds PT, Brady EK, Chawla S. The utility of early cross-sectional imaging to evaluate suspected acute mild pancreatitis. Ann Gastroenterol. 2018;31(5):628–32. https://doi.org/10.20524/aog.2018.0291.
Benarroch-Gampel J, Boyd CA, Sheffield KM, Townsend CM Jr, Riall TS. Overuse of CT in patients with complicated gallstone disease. J Am Coll Surg. 2011;213(4):524–30. https://doi.org/10.1016/j.jamcollsurg.2011.07.008.
Bhangu A, Richardson C, Winter H, Bleetman A. Value of initial radiological investigations in patients admitted to hospital with appendicitis, acute gallbladder disease or acute pancreatitis. Emerg Med J. 2010;27(10):754–7. https://doi.org/10.1136/emj.2009.083188.
Creeden SG, Rao AG, Eklund MJ, Hill JG, Thacker PG. Pre-procedural scout radiographs are unnecessary for routine pediatric fluoroscopic examinations. Pediatr Radiol. 2017;47(3):290–3. https://doi.org/10.1007/s00247-016-3754-0.
de Burlet KJ, MacKay M, Larsen P, Dennett ER. Appropriateness of CT scans for patients with non-traumatic acute abdominal pain. Br J Radiol. 2018;91(1088):20180158. https://doi.org/10.1259/bjr.20180158.
Driver BE, Chittineni C, Kartha G, Cole JB, Klein LR, Rischall M. Utility of plain abdominal radiography in adult ED patients with suspected constipation. Am J Emerg Med. 2020;38(6):1092–6. https://doi.org/10.1016/j.ajem.2019.158377.
Jackson K, Taylor D, Judkins S. Emergency department abdominal x-rays have a poor diagnostic yield and their usefulness is questionable. Emerg Med J. 2011;28(9):745–9. https://doi.org/10.1136/emj.2010.094730.
Maurer MH, Winkler A, Wichlas F, Powerski MJ, Elgeti F, Huppertz A, et al. Costs and role of ultrasound follow-up of polytrauma patients after initial computed tomography. Rofo. 2012;184(1):53–8. https://doi.org/10.1055/s-0031-1281638.
Nojkov B, Duffy MC, Cappell MS. Utility of repeated abdominal CT scans after prior negative CT scans in patients presenting to ER with nontraumatic abdominal pain. Dig Dis Sci. 2013;58(4):1074–83. https://doi.org/10.1007/s10620-012-2473-0.
Sreedharan S, Fiorentino M, Sinha S. Plain abdominal radiography in acute abdominal pain–is it really necessary? Emerg Radiol. 2014;21(6):597–603. https://doi.org/10.1007/s10140-014-1244-y.
Valusek PA, St Peter SD, Keckler SJ, Laituri CA, Snyder CL, Ostlie DJ, et al. Does an upper gastrointestinal study change operative management for gastroesophageal reflux? J Pediatr Surg. 2010;45(6):1169–72. https://doi.org/10.1016/j.jpedsurg.2010.02.083.
van Randen AMD, Laméris W, Luitse JSKMD, Gorzeman MMD, Hesselink EJMD, Dolmans DEJGJMDP, et al. The role of plain radiographs in patients with acute abdominal pain at the ED. Am J Emerg Med. 2011;29(6):582–9.e2. https://doi.org/10.1016/j.ajem.2009.12.020.
Westphalen AC, Hsia RY, Maselli JH, Wang R, Gonzales R. Radiological imaging of patients with suspected urinary tract stones: national trends, diagnoses, and predictors. Acad Emerg Med. 2011;18(7):699–707. https://doi.org/10.1111/j.1553-2712.2011.01103.x.
Wu J, Zhang T, Zhu YS, Gong NM. Diagnostic value of ultrasound compared to CT in patients with suspected acute appendicitis. Int J Clin Exp Med. 2017;10(10):14377–85.
Brockmeyer JR, Simon TE, Jacob RK, Husain F, Choi Y. Upper gastrointestinal swallow study following bariatric surgery: institutional review and review of the literature. Obes Surg. 2012;22(7):1039–43. https://doi.org/10.1007/s11695-012-0658-4.
Diaz Vico T, Elli EF. Utility of immediate postoperative upper gastrointestinal contrast study in bariatric surgery. Obes Surg. 2019;29(4):1130–3. https://doi.org/10.1007/s11695-018-03639-w.
Abou Hussein BM, Khammas A, Makki M, Makki M, Al Bastaki U, Al Mazrouei A, et al. Role of routine abdominal ultrasound before bariatric surgery: review of 937 patients. Obes Surg. 2018;28(9):2696–9. https://doi.org/10.1007/s11695-018-3210-3.
Hu Z, Wang X, An X, Li W, Feng Y, You Z. The diagnostic value of routine contrast esophagram in anastomotic leaks after esophagectomy. World J Surg. 2017;41(8):2062–7. https://doi.org/10.1007/s00268-017-3923-9.
Mittermair R, Sucher R, Perathoner A, Wykypiel H. Routine upper gastrointestinal swallow studies after laparoscopic sleeve gastrectomy are unnecessary. Am J Surg. 2014;207(6):897–901. https://doi.org/10.1016/j.amjsurg.2013.06.015.
Wu CH, Chen CM, Chen CC, Wong YC, Wang CJ, Lo WC, et al. Esophagography after pneumomediastinum without CT findings of esophageal perforation: is it necessary? Am J Roentgenol. 2013;201(5):977–84.
Yonis G, Cabalag CS, Link E, Duong CP. Utility of routine oral contrast study for detecting postesophagectomy anastomotic leak—a systematic review and meta-analysis. Dis Esophagus. 2019. https://doi.org/10.1093/dote/doz011.
Baker W, Pelkofski E, Te Paske J, Erickson S, Duska L. Preoperative imaging of uterine malignancy: a low-value service. Gynecol Oncol. 2015;137(2):285–90. https://doi.org/10.1016/j.ygyno.2015.02.015.
Lavery HJ, Brajtbord JS, Levinson AW, Nabizada-Pace F, Pollard ME, Samadi DB. Unnecessary imaging for the staging of low-risk prostate cancer is common. Urology. 2011;77(2):274–8. https://doi.org/10.1016/j.urology.2010.07.491.
Drangsholt S, Walter D, Ciprut S, Lepor A, Sedlander E, Curnyn C, et al. Quantifying downstream impact of inappropriate staging imaging in a cohort of veterans with low- and intermediate-risk incident prostate cancer. Urol Oncol. 2019;37(2):145–9. https://doi.org/10.1016/j.urolonc.2018.11.022.
Han K, Park SH, Kim KW, Kim HJ, Lee SS, Kim JC, et al. Use of liver magnetic resonance imaging after standard staging abdominopelvic computed tomography to evaluate newly diagnosed colorectal cancer patients. Ann Surg. 2015;261(3):480–6. https://doi.org/10.1097/SLA.0000000000000708.
Lou I, Schneider DF, Leverson GE, Sippel RS, Chen H. Do additional imaging studies change operative management in patients undergoing adrenalectomy? Surgery. 2015;158(4):1003–9. https://doi.org/10.1016/j.surg.2015.05.031 (discussion 9-11).
Rosenlund IM, Forde OH, Revhaug A. Routine deferred computed tomography for patients with suspected urolithiasis is low-value healthcare. Scand J Urol. 2017;51(1):62–7. https://doi.org/10.1080/21681805.2016.1254680.
Wilhelm K, Hahn O, Schoenthaler M, Hein S, Neubauer J, Schnabel M, et al. Stone-free rate after treating kidney stones exceeding 10 mm via flexible ureteroscopy: can endoscopic assessment replace low-dose computed tomography control? Urol Int. 2019;103(3):326–30.
Dyer J, Syratt T, Singh G. Is CTKUB the gold standard in assessing flank pain with diagnostic uncertainty? A one-year review of 228 cases. J Clin Urol. 2013;6(2):114–8.
Gamss R, Stein MW, Rispoli JM, Cohen HW, Roberts JH, Koenigsberg M, et al. What is the appropriate use of renal sonography in an inner-city population with new-onset acute kidney injury? J Ultrasound Med. 2015;34(9):1639–44. https://doi.org/10.7863/ultra.15.14.04026.
Ahmadnia H, Rostami MY, Kamalati A, Imani MM. Penile fracture and its treatment: is retrograde urethrograghy necessary for management of penile fracture? Chin J Traumatol Engl Ed. 2014;17(6):338–40.
Li J, Tan Y, Zhang D, Li J, Shen S, Jiang Y, et al. Value and necessity of pelvic CT in gastric cancer staging: an observational study. Scand J Gastroenterol. 2018;53(9):1097–9. https://doi.org/10.1080/00365521.2018.1498121.
Coco AS, O’Gurek DT. Increased emergency department computed tomography use for common chest symptoms without clear patient benefits. J Am Board Fam Med. 2012;25(1):33–41. https://doi.org/10.3122/jabfm.2012.01.110039.
Alhassan S, Bihler E, Patel K, Lavudi S, Young M, Balaan M. Assessment of the current D-dimer cutoff point in pulmonary embolism workup at a single institution: retrospective study. J Postgrad Med. 2018;64(3):150–4. https://doi.org/10.4103/jpgm.JPGM_217_17.
Abaluck J, Agha L, Kabrhel C, Raja A, Venkatesh A. The determinants of productivity in medical testing: intensity and allocation of care. Am Econ Rev. 2016;106(12):3730–64. https://doi.org/10.1257/aer.20140260.
Kline JA, Garrett JS, Sarmiento EJ, Strachan CC, Courtney DM. Over-testing for suspected pulmonary embolism in American emergency departments: the continuing epidemic. Circ Cardiovasc Qual Outcomes. 2020;13(1):e005753. https://doi.org/10.1161/CIRCOUTCOMES.119.005753.
Mittadodla PS, Kumar S, Smith E, Badireddy M, Turki M, Fioravanti GT. CT pulmonary angiography: an over-utilized imaging modality in hospitalized patients with suspected pulmonary embolism. J Community Hosp Intern Med Perspect. 2013. https://doi.org/10.3402/jchimp.v3i1.20240.
Osman M, Subedi SK, Ahmed A, Khan J, Dawood T, Rios-Bedoya CF, et al. Computed tomography pulmonary angiography is overused to diagnose pulmonary embolism in the emergency department of academic community hospital. J Community Hosp Intern Med Perspect. 2018;8(1):6–10. https://doi.org/10.1080/20009666.2018.1428024.
Perera M, Aggarwal L, Scott IA, Cocks N. Underuse of risk assessment and overuse of computed tomography pulmonary angiography in patients with suspected pulmonary thromboembolism. Intern Med J. 2017;47(10):1154–60. https://doi.org/10.1111/imj.13524.
Gunderson CG, Chang JJ. Overuse of compression ultrasound for patients with lower extremity cellulitis. Thromb Res. 2014;134(4):846–50. https://doi.org/10.1016/j.thromres.2014.08.002.
Le Gal G, Robert-Ebadi H, Carrier M, Kearon C, Bounameaux H, Righini M. Is it useful to also image the asymptomatic leg in patients with suspected deep vein thrombosis? J Thromb Haemost. 2015;13(4):563–6. https://doi.org/10.1111/jth.12851.
Rahiminejad M, Rastogi A, Prabhudesai S, McClinton D, MacCallum P, Platton S, et al. Evaluating the use of a negative D-dimer and modified low wells score in excluding above knee deep venous thrombosis in an outpatient population, assessing need for diagnostic ultrasound. ISRN Radiol. 2014;2014:519875. https://doi.org/10.1155/2014/519875.
Rozman PA, Kurland DB, Golub D, Trang M, Rothstein A, Lewis A, et al. Venous duplex ultrasound surveillance in the neurosurgical population: a single-center quality improvement initiative. World Neurosurg. 2020;3:03. https://doi.org/10.1016/j.wneu.2020.07.207.
Yoo T, Aggarwal R, Brathwaite S, Satiani B, Haurani MJ. Four-extremity venous duplex ultrasound for suspected deep venous thrombosis is an anachronism. J Vasc Surg-Venous Lymphat Disord. 2019;7(3):325. https://doi.org/10.1016/j.jvsv.2018.11.004.
Kirkpatrick VE, Wilson SE, Williams RA, Gordon IL. Surveillance computed tomographic arteriogram does not change management before 3 years in patients who have a normal post-EVAR study. Ann Vasc Surg. 2014;28(4):831–6. https://doi.org/10.1016/j.avsg.2013.09.017.
Garg T, Baker LC, Mell MW. Postoperative surveillance and long-term outcomes after endovascular aneurysm repair among medicare beneficiaries. JAMA Surg. 2015;150(10):957–63. https://doi.org/10.1001/jamasurg.2015.1320.
Patel MS, Carpenter JP. The value of the initial post-EVAR computed tomography angiography scan in predicting future secondary procedures using the Powerlink stent graft. J Vasc Surg. 2010;52(5):1135–9. https://doi.org/10.1016/j.jvs.2010.06.019.
Nally MC, Kling C, Hocking KM, Lillemoe H, Boll JM, Curci JA, et al. Follow-up imaging of traumatic vertebral artery dissections is unnecessary in asymptomatic patients. J Vasc Surg. 2019;69(6):1704–9. https://doi.org/10.1016/j.jvs.2018.09.051.
Protack C, Wengerter B, Jean RA, Liu S, Mojibian H, Sumpio B, et al. Overutilization of cross-sectional imaging in the lower extremity trauma setting. Int J Angiol. 2018;27(1):23–8. https://doi.org/10.1055/s-0037-1612622.
Moussavi N, Ghani H, Davoodabadi A, Atoof F, Moravveji A, Saidfar S, et al. Routine versus selective chest and abdominopelvic CT-scan in conscious blunt trauma patients: a randomized controlled study. Eur J Trauma Emerg Surg. 2018;44(1):9–14. https://doi.org/10.1007/s00068-017-0842-2.
Gupta R, Greer SE, Martin ED. Inefficiencies in a rural trauma system: the burden of repeat imaging in interfacility transfers. J Trauma. 2010;69(2):253–5. https://doi.org/10.1097/TA.0b013e3181e4d579.
Heller MT, Kanal E, Almusa O, Schwarz S, Papachristou M, Shah R, et al. Utility of additional CT examinations driven by completion of a standard trauma imaging protocol in patients transferred for minor trauma. Emerg Radiol. 2014;21(4):341–7. https://doi.org/10.1007/s10140-014-1200-x.
Lavingia KS, Collins JN, Soult MC, Terzian WH, Weireter LJ, Britt LD. Torso computed tomography can be bypassed after thorough trauma bay examination of patients who fall from standing. Am Surg. 2015;81(8):798–801.
Rodriguez RM, Hawthorne N, Murphy SP, Theus M, Haase D, Chuku C, et al. Blunt trauma abdominal and pelvic computed tomography has low yield for injuries in more than one anatomic region. Western J Emerg Med. 2018;19(5):768–73. https://doi.org/10.5811/westjem.2018.6.37646.
Thornburg DA, Paulson WE, Thompson PA, Bjordahl PM. Pretransfer CT scans are frequently performed, but rarely helpful in rural trauma systems. Am J Surg. 2017;214(6):1061–4.
Evans J, Vandiver L, Morrow C, Hunt J, Dissanaike S. The increased use of computed tomography scanning for diagnosing superficial soft tissue infections: a disturbing trend of increased radiation with no benefit. Am J Surg. 2012;204(6):988–94. https://doi.org/10.1016/j.amjsurg.2012.05.029 (discussion 94-5).
Alberts AR, Schoots IG, Bokhorst LP, van Leenders GJ, Bangma CH, Roobol MJ. Risk-based patient selection for magnetic resonance imaging-targeted prostate biopsy after negative transrectal ultrasound-guided random biopsy avoids unnecessary magnetic resonance imaging scans. Eur Urol. 2016;69(6):1129–34. https://doi.org/10.1016/j.eururo.2015.11.018.
Aljubran AH, Badran A, Alshaer O, Alhashem H, Omar A, Eldali A. Pattern of use of positron emission tomography/computed tomography (PET/CT) scan in non-colorectal gastrointestinal cancers at KFSHRC, Riyadh, Saudi Arabia. Egypt J Radiol Nucl Med. 2019;50(1):60. https://doi.org/10.1186/s43055-019-0067-y.
Barsky M, Cherkassky L, Vezeridis M, Miner TJ. The role of preoperative positron emission tomography/computed tomography (PET/CT) in patients with high-risk melanoma. J Surg Oncol. 2014;109(7):726–9. https://doi.org/10.1002/jso.23549.
Cuellar SL, Carter BW, Macapinlac HA, Ajani JA, Komaki R, Welsh JW, et al. Clinical staging of patients with early esophageal adenocarcinoma: does FDG-PET/CT have a role? J Thorac Oncol. 2014;9(8):1202–6. https://doi.org/10.1097/JTO.0000000000000222.
Debald M, Wolfgarten M, Kreklau P, Abramian A, Kaiser C, Holler T, et al. Staging of primary breast cancer is not indicated in asymptomatic patients with early tumor stages. Oncol Res Treat. 2014;37(7–8):400–5. https://doi.org/10.1159/000363528.
Hartridge-Lambert SK, Schoder H, Lim RC, Maragulia JC, Portlock CS. ABVD alone and a PET scan complete remission negates the need for radiologic surveillance in early-stage, nonbulky Hodgkin lymphoma. Cancer. 2013;119(6):1203–9. https://doi.org/10.1002/cncr.27873.
Healy MA, Yin H, Reddy RM, Wong SL. Use of positron emission tomography to detect recurrence and associations with survival in patients with lung and esophageal cancers. J Natl Cancer Inst. 2016. https://doi.org/10.1093/jnci/djv429.
Holtkamp LHJ, Read RL, Emmett L, Thompson JF, Nieweg OE. Futility of imaging to stage melanoma patients with a positive sentinel lymph node. Melanoma Res. 2017;27(5):457–62. https://doi.org/10.1097/CMR.0000000000000362.
Kamal A, Zhang T, Power S, Marcom PK. Is advanced imaging in early-stage breast cancer ever warranted? Reconciling clinical judgment with common quality measures. J Natl Compr Cancer Netw. 2016;14(8):993–8. https://doi.org/10.6004/jnccn.2016.0106.
Pappas SG, Christians KK, Tolat PP, Mautz AP, Lal A, McElroy L, et al. Staging chest computed tomography and positron emission tomography in patients with pancreatic adenocarcinoma: utility or futility? HPB (Oxford). 2014;16(1):70–4. https://doi.org/10.1111/hpb.12074.
Park JY, Lee JJ, Choi HJ, Song IH, Sung CO, Kim HO, et al. The value of preoperative positron emission tomography/computed tomography in node-negative endometrial cancer on magnetic resonance imaging. Ann Surg Oncol. 2017;24(8):2303–10. https://doi.org/10.1245/s10434-017-5901-8.
Sabate-Llobera A, Cortes-Romera M, Mercadal S, Hernandez-Ganan J, Pomares H, Gonzalez-Barca E, et al. Low-dose PET/CT and full-dose contrast-enhanced CT at the initial staging of localized diffuse large B-cell lymphomas. Clin Med Insights-Blood Disord. 2016;9:29–32. https://doi.org/10.4137/Cmbd.S38468.
Simos D, Catley C, van Walraven C, Arnaout A, Booth CM, McInnes M, et al. Imaging for distant metastases in women with early-stage breast cancer: a population-based cohort study. CMAJ. 2015;187(12):E387–97. https://doi.org/10.1503/cmaj.150003.
Taghipour M, Marcus C, Sheikhbahaei S, Mena E, Prasad S, Jha AK, et al. Clinical indications and impact on management: fourth and subsequent posttherapy follow-up (18)F-FDG PET/CT scans in oncology patients. J Nucl Med. 2017;58(5):737–43. https://doi.org/10.2967/jnumed.116.183111.
Thompson CA, Ghesquieres H, Maurer MJ, Cerhan JR, Biron P, Ansell SM, et al. Utility of routine post-therapy surveillance imaging in diffuse large B-cell lymphoma. J Clin Oncol. 2014;32(31):3506–12. https://doi.org/10.1200/jco.2014.55.7561.
Truong Q, Shah N, Knestrick M, Curley B, Hu Y, Craig M, et al. Limited utility of surveillance imaging for detecting disease relapse in patients with non-Hodgkin lymphoma in first complete remission. Clin Lymphoma Myeloma Leuk. 2014;14(1):50–5. https://doi.org/10.1016/j.clml.2013.08.009.
Wallace AS, Nelson JP, Wang Z, Dale PS, Biedermann GB. In support of the Choosing Wisely campaign: perceived higher risk leads to unnecessary imaging in accelerated partial breast irradiation? Breast J. 2016;24(1):12–5. https://doi.org/10.1111/tbj.12832.
Jaukovic L, Ajdinovic B, Cerovic S, Joksimovic M, Soldatovic Z. Is bone scintigraphy necessary in initial staging of prostate cancer patients? Hellenic J Nucl Med. 2011;14(2):126-30+96.
Falchook AD, Salloum RG, Hendrix LH, Chen RC. Use of bone scan during initial prostate cancer workup, downstream procedures, and associated Medicare costs. Int J Radiat Oncol Biol Phys. 2014;89(2):243–8. https://doi.org/10.1016/j.ijrobp.2013.10.023.
Soydal C, Nak D, Araz M, Akkus P, Urun Y, Ozkan E, et al. Comparison of bone scintigraphy and Ga-68 prostate-specific membrane antigen positron emission tomography/computed tomography in the detection of bone metastases of prostate carcinoma. Nucl Med Commun. 2019;40(12):1243–9. https://doi.org/10.1097/MNM.0000000000001106.
Kirk PS, Borza T, Caram MEV, Shumway DA, Makarov DV, Burns JA, et al. Characterising potential bone scan overuse amongst men treated with radical prostatectomy. BJU Int. 2019;124(1):55–61. https://doi.org/10.1111/bju.14551.
Turnbull L, Brown S, Harvey I, Olivier C, Drew P, Napp V, et al. Comparative effectiveness of MRI in breast cancer (COMICE) trial: a randomised controlled trial. Lancet. 2010;375(9714):563–71. https://doi.org/10.1016/S0140-6736(09)62070-5.
Wang SY, Long JB, Killelea BK, Evans SB, Roberts KB, Silber A, et al. Preoperative breast magnetic resonance imaging and contralateral breast cancer occurrence among older women with ductal carcinoma in situ. Breast Cancer Res Treat. 2016;158(1):139–48. https://doi.org/10.1007/s10549-016-3858-0.
Wang SY, Long JB, Killelea BK, Evans SB, Roberts KB, Silber A, et al. Preoperative breast magnetic resonance imaging and contralateral breast cancer occurrence among older women with breast cancer. J Clin Oncol. 2016;34(4):321–8.
Barron M, Kuckelman J, Davison J, Mosier A, Sohn V. The role of early post-treatment mammography after breast conservation therapy. Am J Surg. 2016;211(5):850–3. https://doi.org/10.1016/j.amjsurg.2016.01.005.
Hymas RVPD, Gaffney DKMDPD, Parkinson BTMD, Belnap TWBS, Sause WTMD. Is short-interval mammography necessary after breast conservation surgery and radiation treatment in breast cancer patients? Int J Radiat Oncol Biol Phys. 2012;83(2):519–24. https://doi.org/10.1016/j.ijrobp.2011.07.029.
Mateo AM, Frankel AM. Is 6-month radiologic imaging necessary after benign breast biopsy? Review of literature and multicenter experience. Am Surg. 2015;81(12):1224–7.
Manjoros DT, Collett AE, Alberty-Oller JJ, Frazier TG, Barrio AV. The value of 6-month interval imaging after benign radiologic-pathologic concordant minimally invasive breast biopsy. Ann Surg Oncol. 2013;20(10):3163–8. https://doi.org/10.1245/s10434-013-3114-3.
Maldonado S, Gandhi N, Ha T, Choi P, Khalkhali I, Kalantari BN, et al. Utility of short-interval follow-up mammography after a benign-concordant stereotactic breast biopsy result. Breast. 2018;42:50–3. https://doi.org/10.1016/j.breast.2018.08.101.
Lapid O, Siebenga P, Zonderland HM. Overuse of imaging the male breast-findings in 557 patients. Breast J. 2015;21(3):219–23. https://doi.org/10.1111/tbj.12393.
Galvao De Lima JJ, Wolff Gowdak LH, de Paula FJ, Franchini Ramires JA, Bortolotto LA. The role of myocardial scintigraphy in the assessment of cardiovascular risk in patients with end-stage chronic kidney disease on the waiting list for renal transplantation. Nephrol Dial Transplant. 2012;27(7):2979–84. https://doi.org/10.1093/ndt/gfr770.
Foy A, Rier J, Kozak M. High numbers of false-positive stress tests are the result of inappropriate testing. Am J Med Qual. 2014;29(2):153–9. https://doi.org/10.1177/1062860613489726.
Holle SLK, Andersen MH, Klein CF, Bruun NE, Tonder N, Haarmark C, et al. Clinical usefulness of FDG-PET/CT for identification of abnormal extra-cardiac foci in patients with infective endocarditis. Int J Cardiovasc Imaging. 2020;36(5):939–46. https://doi.org/10.1007/s10554-020-01787-8.
Harris J, Yoon J, Salem M, Selim M, Kumar S, Lioutas VA. Utility of transthoracic echocardiography in diagnostic evaluation of ischemic stroke. Front Neurol. 2020;11:103. https://doi.org/10.3389/fneur.2020.00103.
Patel MR, Peterson ED, Dai D, Brennan JM, Redberg RF, Anderson HV, et al. Low diagnostic yield of elective coronary angiography. N Engl J Med. 2010;362(10):886–95. https://doi.org/10.1056/NEJMoa0907272.
Witteles RM, Knowles JW, Perez M, Morris WM, Spettell CM, Brennan TA, et al. Use and overuse of left ventriculography. Am Heart J. 2012;163(4):617-23.e1. https://doi.org/10.1016/j.ahj.2011.12.018.
Haymart MR, Banerjee M, Reyes-Gastelum D, Caoili E, Norton EC. Thyroid ultrasound and the increase in diagnosis of low-risk thyroid cancer. J Clin Endocrinol Metab. 2019;104(3):785–92. https://doi.org/10.1210/jc.2018-01933.
Mohammadi M, Betel C, Burton KR, Higgins KM, Ghorab Z, Halperin IJ. Follow-up of benign thyroid nodules-can we do less? Can Assoc Radiol J. 2019;70(1):62–7. https://doi.org/10.1016/j.carj.2018.10.001.
Baek HJ, Kim DW, Lee CY, Huh JY, Sung JY, Choi YJ. Analysis of postoperative ultrasonography surveillance after hemithyroidectomy in patients with papillary thyroid microcarcinoma: a multicenter study. Endocr Pract. 2017;23(7):794–802. https://doi.org/10.4158/EP161723.OR.
Baek HJ, Kim DW, Lee S, Ryoo I, Lee CY, Choi YJ, et al. Postoperative ultrasonography surveillance in patients with follicular thyroid carcinoma: a multicenter study. Radiol Med. 2017;122(7):530–7. https://doi.org/10.1007/s11547-017-0753-7.
Panneerselvan R, Schneider DF, Sippel RS, Chen H. Radioactive iodine scanning is not beneficial but its use persists for euthyroid patients. J Surg Res. 2013;184(1):269–73. https://doi.org/10.1016/j.jss.2013.03.092.
Kim DW. Long-term follow-up ultrasonography after lobectomy in papillary thyroid microcarcinoma patients: a single-center study. Endocr Res. 2016;41(3):213–7. https://doi.org/10.3109/07435800.2015.1137583.
Jones BA, Lindeman B, Chen H. Are Tc-99m-sestamibi scans in patients with secondary hyperparathyroidism and renal failure needed? J Surg Res. 2019;243:380–3. https://doi.org/10.1016/j.jss.2019.04.084.
Jaume F, Quinto L, Alobid I, Mullol J. Overuse of diagnostic tools and medications in acute rhinosinusitis in Spain: a population-based study (the PROSINUS study). BMJ Open. 2018;8(1): e018788. https://doi.org/10.1136/bmjopen-2017-018788.
Huang LK, Tu HF, Jiang LD, Chen YY, Fu CY. Evaluation of concomitant orbital floor fractures in patients with head trauma using conventional head CT scan: a retrospective study at a level II trauma center. J Clin Med. 2019;8(11):1852. https://doi.org/10.3390/jcm8111852.
Dewi F, Henry A, Bhatia S. Postoperative radiographs after open reduction and internal fixation of mandibular fractures: clinical need or unnecessary radiation? Br J Oral Maxillofac Surg. 2016;54(3):312–5. https://doi.org/10.1016/j.bjoms.2015.12.019.
Sener MT, Kok AN, Kara C, Anci Y, Sahingoz S, Emet M. Diagnosing isolated nasal fractures in the emergency department: are they missed or overdiagnosed? Ten years experience of 535 forensic cases. Eur J Trauma Emerg Surg. 2014;40(6):715–9. https://doi.org/10.1007/s00068-014-0373-z.
Singh KS, Jayachandran S. A comparative study on the diagnostic utility of ultrasonography with conventional radiography and computed tomography scan in detection of zygomatic arch and mandibular fractures. Contemp Clin Dent. 2014;5(2):166–9. https://doi.org/10.4103/0976-237X.132306.
van den Bergh B, Goey Y, Forouzanfar T. Postoperative radiographs after maxillofacial trauma: sense or nonsense? Int J Oral Maxillofac Surg. 2011;40(12):1373–6. https://doi.org/10.1016/j.ijom.2011.08.008.
Owosho AA, Hughes MA, Prasad JL, Potluri A, Costello BJ, Branstetter BF. Is computed tomography an adequate imaging modality for the evaluation of juvenile ossifying fibroma? A comparison of 2 imaging modalities (computed tomography and magnetic resonance imaging). J Oral Maxillofac Surg. 2015;73(7):1304–13.
Kenway B, Vlastarakos PV, Kasbekar AV, Axon PR, Donnelly N. Are routine preoperative CT scans necessary in adult cochlear implantation? Implications for the allocation of resources in cochlear implant programs. Ear Nose Throat J. 2016;95(8):318–22.
Tisch M, Storrle P, Danz B, Maier H. Role of imaging before Eustachian tube dilation using the Bielefeld balloon catheter. HNO. 2013;61(6):488–91. https://doi.org/10.1007/s00106-013-2712-5.
Agarwal S, Choudhury PR, Baro A, Baruah P. Is there over use of computed tomography scan in paediatric head injury patients? J Clin Diagn Res. 2018;12(9):1–4.
Strait L, Sussman R, Ata A, Edwards MJ. Utilization of CT imaging in minor pediatric head, thoracic, and abdominal trauma in the United States. J Pediatr Surg. 2020;55(9):1766–72. https://doi.org/10.1016/j.jpedsurg.2020.01.006.
Zhu H, Gao Q, Xia X, Xiang J, Yao H, Shao J. Clinically-important brain injury and CT findings in pediatric mild traumatic brain injuries: a prospective study in a Chinese reference hospital. Int J Environ Res Public Health. 2014;11(4):3493–506. https://doi.org/10.3390/ijerph110403493.
Gunes A, Oncel IH, Gunes SO, Birbilen AZ, Hanalioglu S. Use of computed tomography and diffusion weighted imaging in children with ventricular shunt. Childs Nerv Syst. 2019;35(3):477–86. https://doi.org/10.1007/s00381-018-04046-3.
Zulfiqar M, Kim S, Lai JP, Zhou Y. The role of computed tomography in following up pediatric skull fractures. Am J Surg. 2017;214(3):483–8. https://doi.org/10.1016/j.amjsurg.2016.07.020.
Hentzen AS, Helmer SD, Nold RJ, Grundmeyer RW, Haan JM. Necessity of repeat head computed tomography after isolated skull fracture in the pediatric population. Am J Surg. 2015;210(2):322–5. https://doi.org/10.1016/j.amjsurg.2014.11.011.
Dawson EC, Montgomery CP, Frim D, Koogler T. Is repeat head computed tomography necessary in children admitted with mild head injury and normal neurological exam? Pediatr Neurosurg. 2012;48(4):221–4. https://doi.org/10.1159/000346697.
Howe J, Fitzpatrick CM, Lakam DR, Gleisner A, Vane DW. Routine repeat brain computed tomography in all children with mild traumatic brain injury may result in unnecessary radiation exposure. J Trauma Acute Care Surg. 2014;76(2):292–5. https://doi.org/10.1097/TA.0000000000000119 (discussion 5-6).
Rho YI, Chung HJ, Suh ES, Lee KH, Eun BL, Nam SO, et al. The role of neuroimaging in children and adolescents with recurrent headaches—multicenter study. Headache J Head Face Pain. 2011;51(3):403–8. https://doi.org/10.1111/j.1526-4610.2011.01845.x.
Ahmed M, Grossman S, Rafique B, Momoh OA. Site locked headaches in paediatric patients do not require routine brain imaging and rarely have a serious aetiology. Acta Paediatr. 2017;106(5):791–5. https://doi.org/10.1111/apa.13743.
Gandhi R, Lewis EC, Evans JW, Sell E. Investigating the necessity of computed tomographic scans in children with headaches: a retrospective review. CJEM. 2015;17(2):148–53. https://doi.org/10.2310/8000.2014.141409.
Trofimova AV, Kishore D, Urquia L, Tewkesbury G, Duszak R Jr, Levy MD, et al. Imaging utilization in children with headaches: current status and opportunities for improvement. J Am Coll Radiol. 2020;17(5):574–83. https://doi.org/10.1016/j.jacr.2020.01.008.
Anne S, Juarez JM, Shaffer A, Eleff D, Kitsko D, Sydlowski S, et al. Utility of intraoperative and postoperative radiographs in pediatric cochlear implant surgery. Int J Pediatr Otorhinolaryngol. 2017;99:44–8. https://doi.org/10.1016/j.ijporl.2017.05.018.
Kim W, Ahn N, Ata A, Adamo MA, Entezami P, Edwards M. Pediatric cervical spine injury in the United States: defining the burden of injury, need for operative intervention, and disparities in imaging across trauma centers. J Pediatr Surg. 2020. https://doi.org/10.1016/j.jpedsurg.2020.05.009.
Zeechan M, Hamidi M, O’Keeffe T, Hanna K, Kulvatunyou N, Tang A, et al. Pediatric liver injury: physical examination, fast and serum transaminases can serve as a guide. J Surg Res. 2019;242:151–6. https://doi.org/10.1016/j.jss.2019.04.021.
Biondi E, Macduff S, Capucilli P, Tsuboyama M, Wu S, Beck C, et al. Using patient characteristics to predict usefulness of abdominal computed tomography in children. Hosp Pediatr. 2013;3(3):226–32. https://doi.org/10.1542/hpeds.2013-0006.
Gaither TW, Awad MA, Leva NV, Murphy GP, Breyer BN, Copp HL. Missed opportunities to decrease radiation exposure in children with renal trauma. J Urol. 2018;199(2):552–7. https://doi.org/10.1016/j.juro.2017.09.001.
Sincavage J, Buonpane C, Benyamen B, Benya E, Lautz T, Helenowski I, et al. Alvarado scores predict additive value of magnetic resonance imaging in workup of suspected appendicitis in children. J Surg Res. 2019;244:42–9. https://doi.org/10.1016/j.jss.2019.06.038.
Abdullah S, Shet N, Watkins R, Kim JS. Is the scout out? The utility of scout radiographs in the pediatric upper gastrointestinal examination. J Pediatr Gastroenterol Nutr. 2018;67(5):576–9. https://doi.org/10.1097/MPG.0000000000002117.
Berger MY, Tabbers MM, Kurver MJ, Boluyt N, Benninga MA. Value of abdominal radiography, colonic transit time, and rectal ultrasound scanning in the diagnosis of idiopathic constipation in children: a systematic review. J Pediatr. 2012;161(1):44-50.e2. https://doi.org/10.1016/j.jpeds.2011.12.045.
Ul Haq MMA, Lyons H, Halim M. Pediatric abdominal X-rays in the acute care setting—are we overdiagnosing constipation? Cureus. 2020;12(3):7283. https://doi.org/10.7759/cureus.7283.
El-Maadawy SM, El-Atawi KM, Elhalik MS. Role of bedside ultrasound in determining the position of umbilical venous catheters. J Clin Neonatol. 2015;4(3):173–7. https://doi.org/10.4103/2249-4847.159878.
Acker SN, Trinh BB, Partrick DA, Stewart CL, Bensard DD. Is Routine upper gastrointestinal contrast study necessary prior to laparoscopic gastrostomy tube placement in children? Eur J Pediatr Surg. 2016;26(1):29–33. https://doi.org/10.1055/s-0035-1563675.
Abbas PI, Naik-Mathuria BJ, Akinkuotu AC, Pimpalwar AP. Routine gastrostomy tube placement in children: does preoperative screening upper gastrointestinal contrast study alter the operative plan? J Pediatr Surg. 2015;50(5):715–7. https://doi.org/10.1016/j.jpedsurg.2015.02.022.
Khan ZA, Ahmad S, Sheikh MY. Gastro esophageal reflux: an over investigated entity in neonates and infants. J Pak Med Assoc. 2010;60(12):984–6.
Kanaroglou N, To T, Zhu J, Braga LH, Wehbi E, Hajiha M, et al. Inappropriate use of ultrasound in management of pediatric cryptorchidism. Pediatrics. 2015;136(3):479–86. https://doi.org/10.1542/peds.2015-0222.
Wong NC, Bansal RK, Lorenzo AJ, DeMaria J, Braga LH. Misuse of ultrasound for palpable undescended testis by primary care providers: a prospective study. Can Urol Assoc J. 2015;9(11–12):387–90. https://doi.org/10.5489/cuaj.3242.
Whittam BM, Calaway A, Szymanski KM, Carroll AE, Misseri R, Kaefer M, et al. Ultrasound diagnosis of multicystic dysplastic kidney: is a confirmatory nuclear medicine scan necessary? J Pediatr Urol. 2014;10(6):1059–62.
Cook SH, Fielding JR, Phillips JD. Repeat abdominal computed tomography scans after pediatric blunt abdominal trauma: missed injuries, extra costs, and unnecessary radiation exposure. J Pediatr Surg. 2010;45(10):2019–24. https://doi.org/10.1016/j.jpedsurg.2010.06.007.
Streck CJ, Vogel AM, Zhang J, Huang EY, Santore MT, Tsao K, et al. Identifying children at very low risk for blunt intra-abdominal injury in whom CT of the abdomen can be avoided safely. J Am Coll Surg. 2017;224(4):449-58.e3. https://doi.org/10.1016/j.jamcollsurg.2016.12.041.
Zagory JA, Dossa A, Golden J, Jensen AR, Goodhue CJ, Upperman JS, et al. Re-evaluation of liver transaminase cutoff for CT after pediatric blunt abdominal trauma. Pediatr Surg Int. 2017;33(3):311–6. https://doi.org/10.1007/s00383-016-4026-7.
Shahi V, Brinjikji W, Cloft HJ, Thomas KB, Kallmes DF. Trends in CT utilization for pediatric fall patients in US emergency departments. Acad Radiol. 2015;22(7):898–903. https://doi.org/10.1016/j.acra.2015.02.016.
Moore HB, Faulk LW, Moore EE, Pierraci F, Cothren Burlew C, Holscher CM, et al. Mechanism of injury alone is not justified as the sole indication for computed tomographic imaging in blunt pediatric trauma. J Trauma Acute Care Surg. 2013;75(6):995–1001. https://doi.org/10.1097/TA.0b013e3182ab065b.
Holscher CM, Faulk LW, Moore EE, Cothren Burlew C, Moore HB, Stewart CL, et al. Chest computed tomography imaging for blunt pediatric trauma: not worth the radiation risk. J Surg Res. 2013;184(1):352–7. https://doi.org/10.1016/j.jss.2013.04.044.
Benedict LA, Paulus JK, Rideout L, Chwals WJ. Are CT scans obtained at referring institutions justified prior to transfer to a pediatric trauma center? J Pediatr Surg. 2014;49(1):184–7. https://doi.org/10.1016/j.jpedsurg.2013.09.056 (discussion 7-8).
Farach SM, Danielson PD, Amankwah EK, Chandler NM. Repeat computed tomography scans after pediatric trauma: results of an institutional effort to minimize radiation exposure. Pediatr Surg Int. 2015;31(11):1027–33. https://doi.org/10.1007/s00383-015-3757-1.
Voss SD, Chen L, Constine LS, Chauvenet A, Fitzgerald TJ, Kaste SC, et al. Surveillance computed tomography imaging and detection of relapse in intermediate- and advanced-stage pediatric Hodgkin’s lymphoma: a report from the Children’s Oncology Group. J Clin Oncol. 2012;30(21):2635–40. https://doi.org/10.1200/JCO.2011.40.7841.
Schlechter JA, Dempewolf M. The utility of radiographs prior to pin removal after operative treatment of supracondylar humerus fractures in children. J Child Orthop. 2015;9(4):303–6. https://doi.org/10.1007/s11832-015-0673-9.
Tuomilehto N, Kivisaari R, Sommarhem A, Nietosvaara AY. Outcome after pin fixation of supracondylar humerus fractures in children: postoperative radiographic examinations are unnecessary a retrospective study of 252 Gartland-III and 12 flexion-type supracondylar humerus fractures. Acta Orthop. 2017;88(1):109–15. https://doi.org/10.1080/17453674.2016.1250058.
Karalius VP, Stanfield J, Ashley P, Lewallen LW, DeDeugd CM, Walker J, et al. The utility of routine postoperative radiographs after pinning of pediatric supracondylar humerus fractures. J Pediatr Orthop. 2017;37(5):e309–12. https://doi.org/10.1097/bpo.0000000000001000.
Acosta AM, Li YJ, Bompadre V, Mortimer A, Trask M, Steinman SE. The utility of the early postoperative follow-up and radiographs after operative treatment of supracondylar humerus fractures in children. J Pediatr Orthop. 2020;40(5):218–22. https://doi.org/10.1097/BPO.0000000000001432.
Golding LP, Yasin Y, Singh J, Gyr BM, Gardner A, Anthony E. Imaging of the elbow in children with wrist fracture: an unnecessary source of radiation and use of resources? Pediatr Radiol. 2015;45(8):1169–73. https://doi.org/10.1007/s00247-015-3304-1.
Rooke G, Phillips FTS. Does early radiography alter remanipulation rates in paediatric forearm fractures? ANZ J Surg. 2015;85(1):38–43.
Ling SJ, Cleary AJ. Are unnecessary serial radiographs being ordered in children with distal radius buckle fractures? Radiol Res Pract. 2018;2018:5143639. https://doi.org/10.1155/2018/5143639.
Wong AT, Brady KB, Caldwell AM, Graber NM, Rubin DH, Listman DA. Low-risk criteria for pelvic radiography in pediatric blunt trauma patients. Pediatr Emerg Care. 2011;27(2):92–6. https://doi.org/10.1097/PEC.0b013e3182094355.
Misiura AK, Nanassy AD, Urbine J. Usefulness of pelvic radiographs in the initial trauma evaluation with concurrent CT: is additional radiation exposure necessary? Int J Pediatr. 2018;2018:6260954. https://doi.org/10.1155/2018/6260954.
Aydın S, Fatihoğlu E. Family history in developmental dysplasia of the hip: should we follow-up? Eur Res J. 2019;5(6):957–61.
Tafazal S, Flowers MJ. Do we need to follow up an early normal ultrasound with a later plain radiograph in children with a family history of developmental dysplasia of the hip? Eur J Orthop Surg Traumatol. 2015;25(7):1171–5. https://doi.org/10.1007/s00590-015-1668-4.
Stenroos A, Kosola J, Puhakka J, Laaksonen T, Ahonen M, Nietosvaara Y. Routine radiographic follow-up is not necessary after physeal fractures of the distal tibia in children. Acta Orthop. 2019;90(6):610–3.
Kose O, Celiktas M, Yigit S, Kisin B. Can we make a diagnosis with radiographic examination alone in calcaneal apophysitis (Sever’s disease)? J Pediatr Orthop B. 2010;19(5):396–8. https://doi.org/10.1097/BPB.0b013e32833a5fa7.
Tournemine S, Angelliaume A, Simon AL, Ilharreborde B. Are postoperative standing radiographs relevant before hospital discharge in adolescent idiopathic scoliosis? Eur Spine J. 2019;28(6):1363–70.
Garg S, Kipper E, LaGreca J, Carry P, Erickson M. Are routine postoperative radiographs necessary during the first year after posterior spinal fusion for idiopathic scoliosis? A retrospective cohort analysis of implant failure and surgery revision rates. J Pediatr Orthop. 2015;35(1):33–8. https://doi.org/10.1097/BPO.0000000000000219.
Mahalik SK, Sodhi KS, Narasimhan KL, Rao KL. Role of preoperative 3D CT reconstruction for evaluation of patients with esophageal atresia and tracheoesophageal fistula. Pediatr Surg Int. 2012;28(10):961–6. https://doi.org/10.1007/s00383-012-3111-9.
Woodward CS, Dowling D, Taylor RP, Savin C. The routine use of chest radiographs after chest tube removal in children who have had cardiac surgery. J Pediatr Health Care. 2013;27(3):189–94. https://doi.org/10.1016/j.pedhc.2011.09.003.
McGrath E, Ranstrom L, Lajoie D, McGlynn L, Mooney D. Is a chest radiograph required after removal of chest tubes in children? J Pediatr Health Care. 2017;31(5):588–93. https://doi.org/10.1016/j.pedhc.2017.04.014.
Raffaele A, Segal A, Romano P, Vatta F, Boghen S, Bonetti F, et al. Intracavitary electrocardiography-guided positioning of central vascular access device can spare unnecessary ionizing radiation exposure in pediatric patients. J Vasc Access. 2020. https://doi.org/10.1177/1129729820923936.
Biagi C, Pierantoni L, Baldazzi M, Greco L, Dormi A, Dondi A, et al. Lung ultrasound for the diagnosis of pneumonia in children with acute bronchiolitis. BMC Pulm Med. 2018;18(1):191. https://doi.org/10.1186/s12890-018-0750-1.
Wrotek A, Czajkowska M, Jackowska T. Chest radiography in children hospitalized with bronchiolitis. Adv Exp Med Biol. 2019;1222:55–62. https://doi.org/10.1007/5584_2019_435.
Lang SM, Bolin E, Daily JA, Tang X, Thomas Collins R. Appropriateness and diagnostic yield of inpatient pediatric echocardiograms. Congenit Heart Dis. 2017;12(2):210–7. https://doi.org/10.1111/chd.12428.
Vernon MM, Powell D, Schultz AH, Simon TD, Doherty D. Is routine preoperative transthoracic echocardiography necessary in newborns with myelomeningocele? J Perinatol. 2015;35(10):842–5.
Lehnert BE, Bree RL. Analysis of appropriateness of outpatient CT and MRI referred from primary care clinics at an academic medical center: how critical is the need for improved decision support? J Am Coll Radiol. 2010;7(3):192–7. https://doi.org/10.1016/j.jacr.2009.11.010.
Landry BA, Barnes D, Keough V, Watson A, Rowe J, Mallory A, et al. Do family physicians request ultrasound scans appropriately? Can Fam Physician. 2011;57(8):e299–304.
Martins R, Raimundo P, Alves P, Monteiro R, Silva LD, Gomes A, et al. Appropriateness of radiology test requests by an emergency department: a retrospective study. Acta Med Port. 2020;33(1):7–14. https://doi.org/10.20344/amp.12075.
Oikarinen H, Karttunen A, Paakko E, Tervonen O. Survey of inappropriate use of magnetic resonance imaging. Insights Imaging. 2013;4(5):729–33. https://doi.org/10.1007/s13244-013-0276-2.
Sobiecka A, Bekiesinska-Figatowska M, Rutkowska M, Latos T, Walecki J. Clinically unjustified diagnostic imaging—a worrisome tendency in today’s medical practice. Pol J Radiol. 2016;81:325–30. https://doi.org/10.12659/PJR.896847.
Vanderby S, Pena-Sanchez JN, Kalra N, Babyn P. Finding the truth in medical imaging: painting the picture of appropriateness for magnetic resonance imaging in Canada. Can Assoc Radiol J. 2015;66(4):323–31.
Vilar-Palop J, Hernandez-Aguado I, Pastor-Valero M, Vilar J, Gonzalez-Alvarez I, Lumbreras B. Appropriate use of medical imaging in two Spanish public hospitals: a cross-sectional analysis. BMJ Open. 2018;8(3):e019535. https://doi.org/10.1136/bmjopen-2017-019535.
Delnevo A, Tritella S, Carbonaro LA, Bobrechova O, Di Leo G, Sardanelli F. The use of bedside chest radiography at a university hospital. Data on a two-week period. Eur J Radiol. 2012;81(3):e260–3. https://doi.org/10.1016/j.ejrad.2011.02.009.
Gershengorn HB, Wunsch H, Scales DC, Rubenfeld GD. Trends in use of daily chest radiographs among US adults receiving mechanical ventilation. JAMA Netw Open. 2018;1(4): e181119. https://doi.org/10.1001/jamanetworkopen.2018.1119.
Kirkham KR, Wijeysundera DN, Pendrith C, Ng R, Tu JV, Laupacis A, et al. Preoperative testing before low-risk surgical procedures. CMAJ. 2015;187(11):E349–58. https://doi.org/10.1503/cmaj.150174.
Leventer-Roberts M, Lev Bar-Or R, Gofer I, Rosenbaum Z, Hoshen M, Feldman B, et al. Choosing wisely: determining performance of unjustified imaging in a large healthcare system. Int J Clin Pract. 2020. https://doi.org/10.1111/ijcp.13644.
Vejdani M, Taleghani Y, Kachoei A, Hosseini R, Salehi S, Foji S, et al. Appropriateness of knee MRI prescriptions in a hospital of Birjand, 2014. Int J Sci Rep. 2015;1:299. https://doi.org/10.18203/issn.2454-2156.IntJSciRep20151498.
Bouck Z, Pendrith C, Chen XK, Frood J, Reason B, Khan T, et al. Measuring the frequency and variation of unnecessary care across Canada. BMC Health Serv Res. 2019;19(1):446. https://doi.org/10.1186/s12913-019-4277-9.
Kool RB, Verkerk EW, Meijs J, van Gorp N, Maessen M, Westert G, et al. Assessing volume and variation of low-value care practices in the Netherlands. Eur J Public Health. 2020;30(2):236–40. https://doi.org/10.1093/eurpub/ckz245.
Perez-Cajaraville J, Abejon Gonzalez D, Romero Esmerats D, Parron Cambero R, Neira Reina F, Ceberio Balda F, et al. Prevalence of the different lumbar back pain etiologies in Spain: results from a large observational study in 306 centers (the SMILE study). Eur Orthop Traumatol. 2015;6(4):451–9.
Linder R, Horenkamp-Sonntag D, Engel S, Schneider U, Verheyen F. Quality assurance using routine data: overdiagnosis by radiological imaging for back pain. Dtsch Med Wochenschr. 2016;141(10):e96–103. https://doi.org/10.1055/s-0042-101467.
Jenkins HJ, Downie AS, Maher CG, Moloney NA, Magnussen JS, Hancock MJ. Imaging for low back pain: is clinical use consistent with guidelines? A systematic review and meta-analysis. Spine J. 2018;18(12):2266–77. https://doi.org/10.1016/j.spinee.2018.05.004.
Kamper SJ, Logan G, Copsey B, Thompson J, Machado GC, Abdel-Shaheed C, et al. What is usual care for low back pain? A systematic review of health care provided to patients with low back pain in family practice and emergency departments. Pain. 2020;161(4):694–702. https://doi.org/10.1097/j.pain.0000000000001751.
Downie A, Hancock M, Jenkins H, Buchbinder R, Harris I, Underwood M, et al. How common is imaging for low back pain in primary and emergency care? Systematic review and meta-analysis of over 4 million imaging requests across 21 years. Br J Sports Med. 2020;54(11):642–51. https://doi.org/10.1136/bjsports-2018-100087.
Lasser EC, Pfoh ER, Chang HY, Chan KS, Bailey JC, Kharrazi H, et al. Has Choosing Wisely(R) affected rates of dual-energy X-ray absorptiometry use? Osteoporos Int. 2016;27(7):2311–6. https://doi.org/10.1007/s00198-016-3511-0.
Morden NE, Schpero WL, Zaha R, Sequist TD, Colla CH. Overuse of short-interval bone densitometry: assessing rates of low-value care. Osteoporos Int. 2014;25(9):2307–11. https://doi.org/10.1007/s00198-014-2725-2.
Wang X, Chang SM, Yu GR, Rao ZT. Clinical value of the Ottawa ankle rules for diagnosis of fractures in acute ankle injuries. PLoS ONE. 2013;8(4): e63228. https://doi.org/10.1371/journal.pone.0063228.
Milligan MG, Cronin AM, Colson Y, Kehl K, Yeboa DN, Schrag D, et al. Overuse of diagnostic brain imaging among patients with stage IA non-small cell lung cancer. J Natl Compr Cancer Netw. 2020;18(5):547–54. https://doi.org/10.6004/jnccn.2019.7384.
O’Sullivan JW, Albasri A, Nicholson BD, Perera R, Aronson JK, Roberts N, et al. Overtesting and undertesting in primary care: a systematic review and meta-analysis. BMJ Open. 2018;8(2):e018557. https://doi.org/10.1136/bmjopen-2017-018557.
Abelhad NI, Kiser KJ, Hughes A, Hust MA, Sayan EG, Prakash SK. Prevalence and clinical characteristics of inappropriate myocardial perfusion imaging tests at a community hospital. BMJ Open Qual. 2019;8(3):e000487. https://doi.org/10.1136/bmjoq-2018-000487.
Aks R, Peleg Hasson S, Sivan A, Kohen T, Rivo L, Yerushalmi R, et al. Diagnostic workup of early-stage breast cancer: can we choose more wisely? Breast Cancer Res Treat. 2020;183(3):741–8. https://doi.org/10.1007/s10549-020-05813-0.
Alsamarah A, Bansari A, Nasser H, Raza W, Alsamarah I, Bagrova A, et al. Comparison of the appropriateness of myocardial perfusion imaging in men versus women. Am J Cardiol. 2017;120(2):191–5. https://doi.org/10.1016/j.amjcard.2017.04.006.
Anderson TS, Leonard S, Zhang AJ, Madden E, Mowery D, Chapman WW, et al. Trends in low-value carotid imaging in the veterans health administration from 2007 to 2016. JAMA Netw Open. 2020;3(9):e2015250. https://doi.org/10.1001/jamanetworkopen.2020.15250.
Backhus LM, Farjah F, Varghese TK, Cheng AM, Zhou XH, Wood DE, et al. Appropriateness of imaging for lung cancer staging in a national cohort. J Clin Oncol. 2014;32(30):3428–35. https://doi.org/10.1200/JCO.2014.55.6589.
Choi WW, Williams SB, Gu X, Lipsitz SR, Nguyen PL, Hu JC. Overuse of imaging for staging low risk prostate cancer. J Urol. 2011;185(5):1645–9. https://doi.org/10.1016/j.juro.2010.12.033.
Keyhani S, Cheng EM, Naseri A, Halm EA, Williams LS, Johanning J, et al. Common reasons that asymptomatic patients who are 65 years and older receive carotid imaging. JAMA Intern Med. 2016;176(5):626–33. https://doi.org/10.1001/jamainternmed.2016.0678.
Liu TW, Hung YN, Soong TC, Tang ST. Increasing receipt of high-tech/high-cost imaging and its determinants in the last month of taiwanese patients with metastatic cancer, 2001–2010: a retrospective cohort study. Medicine (Baltimore). 2015;94(32): e1354. https://doi.org/10.1097/MD.0000000000001354.
Lupichuk S, Tilley D, Surgeoner B, King K, Joy AA. Unwarranted imaging for distant metastases in patients with newly diagnosed ductal carcinoma in situ and stage I and II breast cancer. Can J Surg. 2020;63(2):E100–9. https://doi.org/10.1503/cjs.003519.
Makarov DV, Soulos PR, Gold HT, Yu JB, Sen S, Ross JS, et al. Regional-level correlations in inappropriate imaging rates for prostate and breast cancers: potential implications for the choosing wisely campaign. JAMA Oncol. 2015;1(2):185–94. https://doi.org/10.1001/jamaoncol.2015.37.
Moralidis E, Papadimitriou N, Stathaki M, Xourgia X, Spyridonidis T, Fotopoulos A, et al. A multicenter evaluation of the appropriate use of single-photon emission tomography myocardial perfusion imaging in Greece. J Nucl Cardiol. 2013;20(2):275–83. https://doi.org/10.1007/s12350-012-9664-0.
Peterson T, Askew JW, Bell M, Crusan D, Hodge D, Gibbons RJ. Low yield of stress imaging in a population-based study of asymptomatic patients after percutaneous coronary intervention. Circ Cardiovasc Imaging. 2014;7(3):438–45. https://doi.org/10.1161/CIRCIMAGING.113.000833.
Prasad SM, Gu X, Lipsitz SR, Nguyen PL, Hu JC. Inappropriate utilization of radiographic imaging in men with newly diagnosed prostate cancer in the United States. Cancer. 2012;118(5):1260–7. https://doi.org/10.1002/cncr.26416.
Schumacher JR, Neuman HB, Chang GJ, Kozower BD, Edge SB, Yu M, et al. A national study of the use of asymptomatic systemic imaging for surveillance following breast cancer treatment (AFT-01). Ann Surg Oncol. 2018;25(9):2587–95. https://doi.org/10.1245/s10434-018-6496-4.
Thiriez C, Itti E, Fenelon G, Evangelista E, Meignan M, Cesaro P, et al. Clinical routine use of dopamine transporter imaging in 516 consecutive patients. J Neurol. 2015;262(4):909–15. https://doi.org/10.1007/s00415-014-7634-y.
Solivetti FM, Elia F, Guerrisi A, Desiderio F, Santaguida M, Sperduti I, et al. Cutaneous melanoma follow-up: appropriateness of requests for ultrasound tests–the S.Gallicano National Referral Centre Experience. J Exp Clin Cancer Res. 2013;32(1):73. https://doi.org/10.1186/1756-9966-32-73.
Remfry A, Abrams H, Dudzinski DM, Weiner RB, Bhatia RS. Assessment of inpatient multimodal cardiac imaging appropriateness at large academic medical centers. Cardiovasc Ultrasound. 2015. https://doi.org/10.1186/s12947-015-0037-0.
Wymer KM, Pearce SM, Harris KT, Pierorazio PM, Daneshmand S, Eggener SE. Adherence to national comprehensive cancer network(R) guidelines for testicular cancer. J Urol. 2017;197(3 Pt 1):684–9. https://doi.org/10.1016/j.juro.2016.09.073.
Gulsen I, Ak H, Karadas S, Demir I, Bulut MD, Yaycioglu S. Indications of brain computed tomography scan in children younger than 3 years of age with minor head trauma. Emerg Med Int. 2014;2014:248967. https://doi.org/10.1155/2014/248967.
Weiss AR, Lyden ER, Anderson JR, Hawkins DS, Spunt SL, Walterhouse DO, et al. Histologic and clinical characteristics can guide staging evaluations for children and adolescents with rhabdomyosarcoma: a report from the Children’s Oncology Group Soft Tissue Sarcoma Committee. J Clin Oncol. 2013;31(26):3226–32. https://doi.org/10.1200/JCO.2012.44.6476.
Levin DC, Rao VM. Reducing Inappropriate use of diagnostic imaging through the choosing wisely initiative. J Am Coll Radiol. 2017;14(9):1245–52. https://doi.org/10.1016/j.jacr.2017.03.012.
Brady AP, Bello JA, Derchi LE, Fuchsjäger M, Goergen S, Krestin GP, et al. Radiology in the era of value-based healthcare: a multi-society expert statement from the ACR, CAR, ESR, IS3R, RANZCR, and RSNA. Radiology. 2021;298(3):486–91. https://doi.org/10.1148/radiol.2020209027.
Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):143. https://doi.org/10.1186/s12874-018-0611-x.
Acknowledgements
We would like to thank Senior Research Librarian Karen Marie Øvern at NTNU and academic librarian Jana Myrvold at University of South-Eastern Norway for helping with the development of the search strategy.
Funding
This project received financial support from The Research council of Norway (Project number 302503).
Author information
Authors and Affiliations
Contributions
EK—planning and searching, screening, full-text screening, analysis, drafting, and revision of manuscript. ERA—planning, full-text and quality assessment, snowballing, analysis, and revision of manuscript. AMK—full-text screening, analysis, and revision of manuscript. LJJS—planning, full-text and quality assessment, analysis, and revision of manuscript. LvB-V—planning, full-text screening, analysis, and revision of manuscript. FMC—planning, screening, and revision of manuscript of manuscript. BMH—planning, screening, full-text screening, quality assessment, analysis, and revision of manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. Search strategy and hits.
Additional file 2
. Excluded studies.
Additional file 3
. Characteristics of the included studies.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visithttp://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kjelle, E., Andersen, E.R., Krokeide, A.M. et al. Characterizing and quantifying low-value diagnostic imaging internationally: a scoping review. BMC Med Imaging 22, 73 (2022). https://doi.org/10.1186/s12880-022-00798-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12880-022-00798-2